Abstract
Objectives
To investigate psychosocial and biomedical outcomes following total hip replacement (THR) and to identify predictors of recovery from THR.
Methods
Patients with osteoarthritis (OA) on the waiting list for primary THR in North West England were assessed pre-operatively and at six and 12 months post-operatively to investigate psychosocial and biomedical outcomes. Psychosocial outcomes were anxiety and depression, social support and health-related quality of life (HRQoL). Biomedical outcomes were pain, physical function and stiffness. The primary outcome was the Short-Form 36 (SF-36) Health Survey Total Physical Function. Potential predictors of outcome were age, sex, body mass index, previous joint replacement, involvement in the decision for THR, any comorbidities, any complications, type of medication, and pre-operative ENRICHD Social Support Instrument score, Hospital Anxiety and Depression scores and Western Ontario and McMaster Universities osteoarthritis index score.
Results
The study included 206 patients undergoing THR. There were 88 men and 118 women with a mean age of 66.3 years (sd 10.4;36 to 89). Pain, stiffness and physical function, severity of OA, HRQoL, anxiety and depression all improved significantly from pre-operative to 12-month assessment (all p < 0.001), with the greatest improvement occurring in the first six months (all p < 0.001). The predictors that were found to influence recovery six months after THR were: pain (p < 0.001), anxiety (p = 0.034), depression (p = 0.001), previous joint replacement (p = 0.006) and anti-inflammatory drugs (p = 0.012).
Conclusions
The study identified the key psychosocial and biomedical predictors of recovery following THR. By identifying these predictors, we are able to identify and provide more support for patients at risk of poor recovery following THR.
Cite this article: Bone Joint Res 2013;2:248–54.
Article focus
To investigate the biomedical and psychosocial outcomes following total hip replacement (THR) in patients with osteoarthritis
To determine which predictors are associated with better outcomes of recovery from THR
Key messages
Having social support does affect an individual’s mental well-being, but does not influence recovery following THR
Patients with anxiety and depression are at risk of poorer recovery following THR
Health professionals need to be aware of patients who are more at risk of poor recovery from THR, so that advice and targeted interventions can be delivered
Strengths and limitations
Adequate sample size and low attrition rate during follow-up
Use of valid and reliable tools to measure osteoarthritis symptoms and severity, social support, anxiety and depression and health-related quality of life
Follow-up limited to 12 months after THR
Introduction
Total hip replacement (THR) for osteoarthritis (OA) is one of the most common operations carried out in England.1 A total of 76 970 THRs were performed in England in the period from 2007 to 2008, which had increased to 86 076 for the period 2011 to 2012.1,2 THRs are a considerable cost to the health service, both in terms of the operation costs and the care and rehabilitation that patients require. The National Institute for Health and Care Excellence (NICE) recommends surgery when there is prolonged and established limitation and severe pain.3 Pain and restriction of internal rotation of the hip are found to be the major clinical predictors of being placed on a waiting list for hip replacement.4
Joint replacement for severe OA of the hip is an effective treatment.5 Improvements are found early in the post-operative period, but a follow-up of 12 months is required to gain the full benefit of THR.6 Recovery following THR often focuses on the long-term clinical outcomes and there is strong evidence that biomedical factors, such as pain and physical function, improve after joint replacement.6-12 Despite successes in reduction of pain after THR, a recent systematic review found that between 7% and 23% of patients report long-term pain after THR for OA.13
Psychosocial outcomes, such as health-related quality of life (HRQoL), are found to improve following THR.10,11,14 However, a systematic review showed that THR was effective resulting in an improvement in HRQoL, but not regarding the social dimension,15 with another study showing little or no change in HRQoL following THR.9 Comorbidity may be an issue and can interfere with improvements in HRQoL following hip replacement.15
Anxiety and depression are prevalent in individuals with osteoarthritis.16,17 Whether these psychosocial outcomes improve post-hip replacement is an under-researched area and a focus of this study. Pre-operative depression and somatisation have been found to influence outcome after THR18and pre-operative anxiety and depression may influence post-operative pain and HRQoL.19
There is also evidence that social support has an influence on improvements in quality of life after joint replacement, although there was a limitation as to how social support was measured.10 Qualitative research has shown that recovery in the early stages is influenced by patients’ relationships and social support.20
It is important to identify factors that may influence outcomes following THR so that health professionals are able to identify those patients who may be more at risk of poorer recovery following THR. The overall aim of this study was to investigate the biomedical and psychosocial outcomes following THR in patients with OA and to determine which predictors are associated with better outcomes of recovery from THR.
Patients and Methods
The study was longitudinal, with a postal questionnaire completed pre-operatively and at six and 12 months after THR. Ethical approval was obtained from an NHS research ethics committee (Wrightington, Wigan & Leigh LREC: 08/H1014/40) and research governance arrangements in NHS Trusts were followed.
Sample size was based on having a form of multiple regression as the main analysis to estimate associations with a continuous HRQoL outcome.21 Assuming moderate effect sizes, a significance level of 0.05 and power of 0.80, a model involving ten predictors required a sample size of 163, allowing for attrition of up to 20% during follow-up. While this was the initial target, the final sample size supported the estimation of models with up to 14 predictors.
Patients with OA who were placed on the waiting list for a primary THR from three hospitals in the North West of England were recruited for the study. Written consent was obtained from each participant. A total of 438 individuals were invited to participate during October 2008 to July 2009, with follow-up continuing until 12 months after THR. As there was a delay with some operations, follow-up was not completed until mid-2011.
Data were collected pre-operatively and at six and 12 months post-operatively by post using a structured questionnaire to collect information on demographics, medication, consultation episodes, history of OA, and pre- and post-operative complications.
Assessment of psychosocial factors
Social support was measured by the ENRICHD Social Support Instrument (ESSI).22 The ESSI is a seven-item measure, with items summed to provide a total score between 8 and 34; a higher score is indicative of greater social support. Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS).23-25 The HADS anxiety and depression scores range between 0 and 21: scores from 0 to 7 are ‘normal’, from 8 to 10 ‘mild’, from 11 to 15 considered ‘moderate’ and from 16 to 21 ‘severe’. HRQoL was assessed using the Short-Form 36 Health Survey (SF-36v2), which provides two summary scores (total physical and total mental scores), each ranging from 0 to 100, with higher scores indicating better quality of life. Version 2 allows for norm-based scoring with a mean of 50 (sd 10).26
Assessment of biomedical factors
Pain, stiffness and physical function were assessed using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).27 The WOMAC pain score ranges between 0 and 20, the stiffness score between 0 and 8 and the physical function range between 0 and 68, with lower scores in each being indicative of better function. The Oxford Hip Score (OHS) was used to measure outcome following THR.28,29 It ranges from 0 to 48, with a higher score indicative of a better outcome.
The measurement tools were chosen for their validity, reliability and responsiveness to detect change. At six and 12 months following hip replacement, participants completed the WOMAC, OHS, SF-36v2 and HADS.
Statistical analysis
Data from the questionnaires were entered into Microsoft Excel (Microsoft Corp., Redmond, Washington) and SPSS v20 (IBM Corp., Armonk, New York). Descriptive and inferential statistics were used, with a conventional significance level of α = 0.05 used to determine statistical significance. Linear mixed models were fitted to analyse the change in outcome measures from pre-operative to 12-month assessment, and to see which variables were independently associated with better outcomes at six and 12 months post-operatively. This approach uses data from all participants, whether or not they had responded at each time-point.30 For simplicity, only main effects terms were included in the model; time was treated as a covariate and an unstructured covariance type was used. The outcome of main interest was the change in the SF-36 Total Physical Score at six months post-operatively. The predictor variables for investigation were chosen from a study of the literature. They included age, gender, body mass index (BMI), previous joint replacement, involvement in decision to undergo THR, comorbidity, complications, taking opioids, taking non-steroidal anti-inflammatory drugs (NSAIDs) or COX-2 inhibitors, and baseline scores (including ENRICHD social support score, HADS anxiety score, HADs depression score and WOMAC pain level).
Results
Of the 400 eligible patients, 215 completed the baseline questionnaire (baseline participation rate 53.8%). Of these, nine did not go on to have their operation, leaving 206 patients included in the study. A total of 188 patients completed the six-month follow-up and 182 completed the 12-month follow-up (Fig. 1).
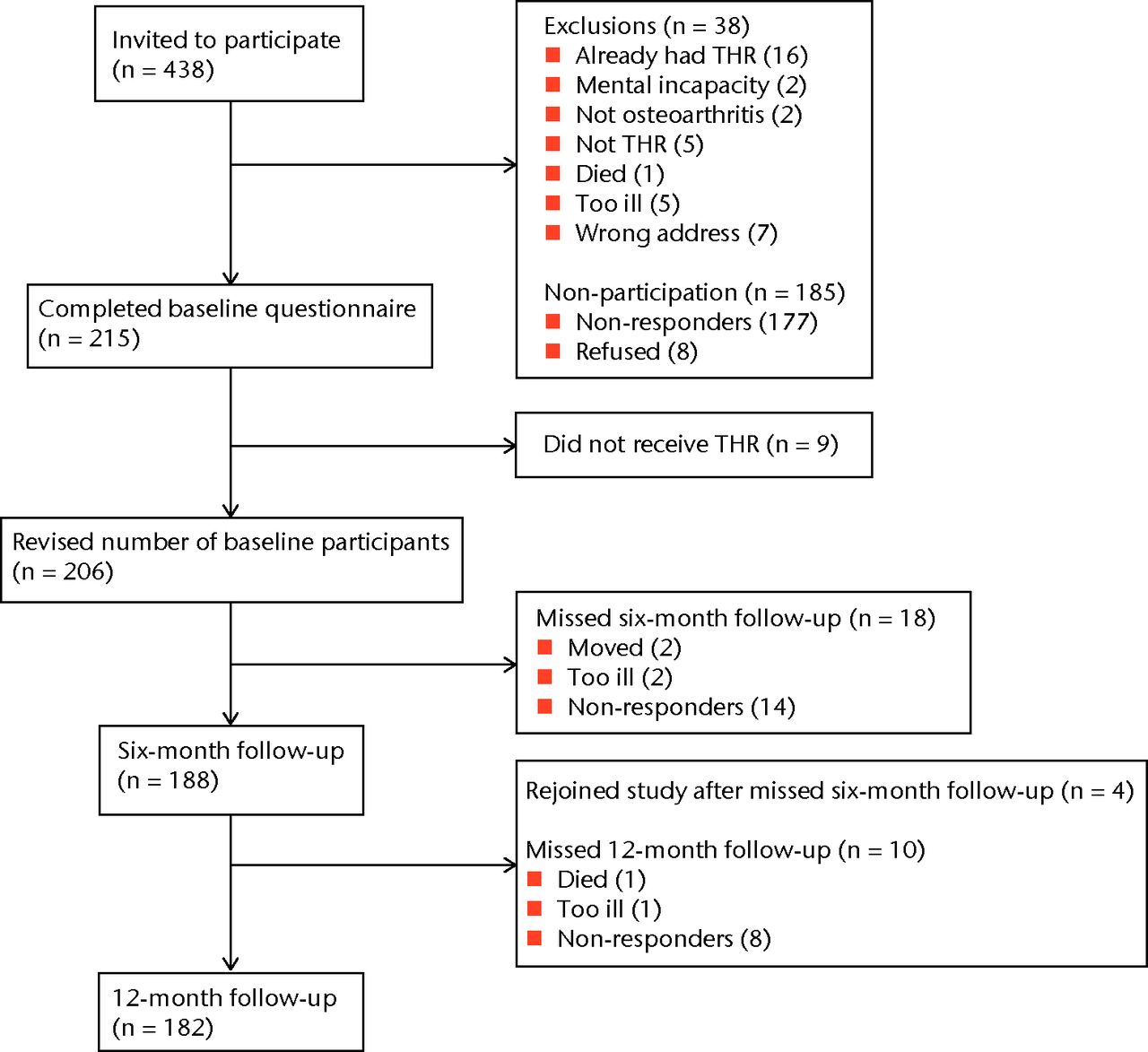
Fig. 1
Recruitment flowchart.
Baseline characteristics for all 206 participants who had a THR are given in Table I. There were 88 men and 118 women with a mean age of 66.3 years (sd 10.4; 36 to 89), of whom 135 (66.2%) were overweight (BMI > 25 kg/m2), with 51 (25.0%) classified as obese (BMI > 30 kg/m2) according to the World Health Organization (WHO) classification.31 Of the 206 participants, 178 (86.4%) completed the questionnaires pre-operatively and at both follow-up time-points, and 188 patients (91.3%) provided both pre-operative and six-month data. Compared with participants with complete data, those with incomplete data showed no significant difference in their baseline characteristics, but they had significantly worse WOMAC scores (pain p = 0.006, stiffness p = 0.024, physical function p = 0.010), SF-36 Total Mental Score (p = 0.017) and HADS depression scores (p = 0.039) at baseline.
Table I
Baseline characteristics of all participants
| Characteristic | |
|---|---|
| Patients (n) | 206 |
| Male (n, %) | 88 (42.7) |
| Mean age (yrs) (sd; range) | 66.3 (10.4; 36 to 89) |
| Married/living together (n, %) | 142 (68.9) |
| Mean body mass index (kg/m2) (sd; range) | 27.5 (5.3; 13.0 to 47.9) |
| Smoker (n, %) | 24 (11.7) |
| Mean cigarettes/day (sd; range) | 10.7 (5.7; 0 to 20) |
| Comorbidities (n, %) | 159 (77.2) |
| Mean number (sd; range) | 1.4 (1.3; 1 to 7) |
| Median number | 1 |
| Angina | 20 (9.7) |
| Ankylosing spondylitis | 9 (4.4) |
| Anxiety-related | 14 (6.8) |
| Asthma | 23 (11.2) |
| Bronchitis | 7 (3.4) |
| Depression-related | 16 (7.8) |
| Diabetes | 22 (10.7) |
| Gastro-intestinal | 25 (12.1) |
| Hypertension | 86 (41.7) |
| Rheumatoid arthritis | 17 (8.3) |
| Other illness(es) | 46 (22.3) |
Social support was measured using the ESSI at baseline. The median score was 27 (interquartile range (IQR) 22 to 30), with 18 (8.4%) scoring ≤ 15 and 79 (38.9%) scoring 29 or 30. At baseline, the median ESSI was significantly higher for males than females (28 (IQR 24 to 30) vs 26 (IQR 21 to 29)); p = 0.003, Mann–Whitney U test), and significantly correlated with HADS anxiety (Kendall’s τ = -0.15, p = 0.004) and depression scores (τ = -0.17, p = 0.001). In particular, it was not significantly associated with the SF-36 Total Physical Score at baseline, six or 12 months (p = 0.891, 0.478 and 0.539, respectively), although it was significantly associated with the SF-36 Total Mental Score (p < 0.001, p = 0.001 and p = 0.004, respectively).
The median hospital stay was six days (IQR 3 to 42). Of the 198 responding to the question, 62 patients (31.3%) reported a delay in being discharged and of these, only three had anticipated this delay. A total of 22 patients (10.7%) had post-operative complications (infection in nine, bleeding in nine, dislocation in three and thrombosis in one).
WOMAC pain, stiffness and physical function scores, OHS, SF-36 Total Physical and Mental Scores, and HADS anxiety and depression scores all showed a significant improvement from before the operation to 12 months after the operation (all p < 0.001), with most improvement occurring in the first six months (all p < 0.001) (Table II). The OHS was the only measure which approached a statistically significant change from six months to 12 months (p = 0.089).
Table II
Changes in validated measures from pre-operative assessment to six and 12 months post-operatively using linear mixed model (n = 206)
| Mean (sd) score | Change over time | p-values (Sidak-corrected) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome measure | Pre-operative (n = 206) | 6 months (n = 188) | 12 months (n = 181) | F | df | p-value | Pre vs 6 mths | Pre vs 12 mths | 6 vs 12 mths | ||
| WOMAC* | |||||||||||
| Pain | 11.4 (3.7) | 3.1 (3.8) | 2.7 (3.7) | 375.62 | 2, 660.66 | < 0.001 | < 0.001 | < 0.001 | 0.280 | ||
| Stiffness | 4.9 (1.6) | 2.2 (1.6) | 2.0 (1.7) | 281.77 | 2, 383.37 | < 0.001 | < 0.001 | < 0.001 | 0.224 | ||
| Physical function | 40.5 (12.7) | 15.7 (13.6) | 15.3 (14.0) | 370.65 | 2, 370.65 | < 0.001 | < 0.001 | < 0.001 | 0.751 | ||
| OHS† | 18.5 (8.1) | 36.8 (9.6) | 37.9 (9.5) | 631.28 | 2, 374.50 | < 0.001 | < 0.001 | < 0.001 | 0.089 | ||
| SF-36‡ | |||||||||||
| Total Physical Score | 28.2 (8.5) | 40.1 (11.1) | 40.9 (11.6) | 233.15 | 2, 375.70 | < 0.001 | < 0.001 | < 0.001 | 0.471 | ||
| Total Mental Score | 47.2 (14.0) | 50.7 (12.1) | 50.4 (13.3) | 9.70 | 2, 369.77 | < 0.001 | < 0.001 | 0.002 | 0.933 | ||
| HADS§ | |||||||||||
| Anxiety score | 7.6 (4.6) | 4.8 (4.3) | 4.9 (4.5) | 81.19 | 2, 372.72 | < 0.001 | < 0.001 | < 0.001 | 0.698 | ||
| Depression score | 7.4 (3.9) | 4.1 (3.8) | 3.8 (3.8) | 132.16 | 2, 369.14 | < 0.001 | < 0.001 | < 0.001 | 0.846 | ||
-
* WOMAC, Western Ontario and McMaster Universities osteoarthritis index: pain (0 to 20), stiffness (0 to 8) and physical function (0 to 68) subscores, with lower scores indicating better function † OHS, Oxford hip score (0 to 48, higher score indicating better outcome following THR) ‡ SF-36, Short-Form 36: Total Physical and Total Mental Scores (both from 0 to 100), with higher scores indicating better quality of life and norm-based scoring with a mean of 50 (sd 10) § HADS, Hospital Anxiety and Depression Scale: anxiety (0 to 21) and depression (0 to 21), each graded as normal (0 to 7), mild (8 to 10), moderate (11 to 15) and severe (16 to 21)
A number of variables were identified as important predictors of the SF-36 Total Physical Score at six months (Table III). In addition to the expected relationship with the pre-operative Total Physical Score (p < 0.001), change in Total Physical Score at six months was significantly and negatively associated with baseline HADS anxiety and depression scores and WOMAC pain score at baseline (p = 0.034, p = 0.001 and p < 0.001, respectively). Those with previous experience of joint replacement surgery also had significantly worse outcomes (p = 0.006), while those taking NSAIDs or COX-2 inhibitors had significantly better outcomes (p = 0.012). The association between change in Total Physical Score at six months and taking opioids was negative but just failed to reach significance (p = 0.054). There was a similar pattern of association at 12 months, with a less significant association between change in Total Physical Score at six months and taking opioids (p = 0.176).
Table III
Predictors of Short-Form 36 (SF-36) Total Physical Score at six and 12 months post-operatively using linear mixed models (n = 198). Statistically significant p-values are bolded (CI, confidence interval)
| Six months | 12 months | ||||
|---|---|---|---|---|---|
| Predictor | Coefficient (95% CI) | p-value | Coefficient (95% CI) | p-value | |
| Constant | 44.19 | - | 44.88 | - | |
| Age | -0.01 (-0.10 to 0.09) | 0.871 | -0.01 (-0.10 to 0.09) | 0.916 | |
| Female | 1.63 (-0.34 to 3.61) | 0.104 | 0.98 (-1.03 to 3.00) | 0.338 | |
| Body mass index | 0.15 (-0.02 to 0.33) | 0.091 | 0.14 (-0.04 to 0.32) | 0.132 | |
| ENRICHD Social Support score | -0.08 (-0.26 to 0.09) | 0.360 | -0.09 (-0.27 to 0.09) | 0.335 | |
| Previous joint surgery | -2.98 (-5.07 to -0.88) | 0.006 | -2.71 (-4.85 to -0.57) | 0.013 | |
| Involved in decision | -1.18 (-3.18 to 0.82) | 0.247 | -1.07 (-3.11 to 0.97) | 0.301 | |
| Any comorbidities | -1.72 (-4.00 to 0.56) | 0.138 | -1.12 (-3.45 to 1.21) | 0.344 | |
| Any complications | -1.43 (-1.43 to 3.55) | 0.402 | 0.37 (-2.20 to 2.94) | 0.778 | |
| Taking opioids | -1.94 (-3.92 to 0.03) | 0.054 | -1.39 (-3.41 to 0.63) | 0.176 | |
| Taking NSAIDs or COX-2 inhibitors | 2.41 (0.55 to 4.27) | 0.012 | 2.64 (0.73 to 4.54) | 0.007 | |
| HADS anxiety score at baseline | 0.28 (0.02 to 0.54) | 0.034 | 0.38 (0.12 to 0.64) | 0.004 | |
| HADS depression score at baseline | -0.56 (-0.56 to -0.16) | 0.001 | -0.65 (-0.98 to -0.31) | < 0.001 | |
| WOMAC pain score at baseline | -1.19 (-1.48 to -0.91) | < 0.001 | -1.28 (-1.57 to -0.99) | < 0.001 | |
| SF-36 Total Physical Score over time | -11.42 (-12.82 to -10.03) | < 0.001 | -12.19 (-13.64 to -10.75) | < 0.001 | |
-
* NSAIDs, non-steroidal anti-inflammatory drugs; HADS, Hospital Anxiety and Depression Scale; WOMAC, Western Ontario and McMaster Universities osteoarthritis index; SF-36, Short-Form 36
Discussion
This study investigated the psychosocial and biomedical outcomes following THR. We were able to ascertain the predictors of recovery following THR. The predictor positively related to recovery was the taking of anti-inflammatory drug consumption and those that had a negative effect on recovery included anxiety and depression, pain and previous experience of joint replacement. There were few post-operative complications following THR in the study participants.
Biomedical outcomes such as pain, physical function, stiffness improved significantly in patients by six months’ post-operatively. Previous studies have shown improvements in pain and physical function following hip replacement,6,8,11 with one study showing that greatest improvement in pain, physical function and stiffness following THR occurred by three months.8 It is of interest that the OHS, which is validated for measuring outcome following joint replacement, was the only outcome measure for which the change from six to 12 months approached statistical significance. This may be as a result of its use as a joint-specific instrument that was developed to minimise the effects of comorbidity.29 The instrument is also sensitive to the outcome of joint replacement and is responsive to detecting changes.32 When the OHS has been compared with the WOMAC, the former appears to be less influenced by the presence of other comorbidities.33
The psychosocial outcomes such as HRQoL, anxiety and depression improved significantly at six months following THR. HRQoL has previously been found to be slower to improve post-operatively than pain or physical function.8 Our study found significant improvements in HRQoL at six months after THR. Anxiety and depression have not been investigated extensively in patients undergoing THR. The baseline levels of anxiety and depression in our study (mean HADS scores of 7.6 and 7.4, respectively) were just outside the normal range (defined as 0 to 7), thereby bordering on the category of mild anxiety and depression. Once patients had a THR, our study found that there were significant improvements in both anxiety and depression, which were also identified as predictors influencing recovery. Those patients who had higher anxiety and depression scores as measured by HADs had a worse outcome. Levels of anxiety pre-operatively may partly be due to apprehension about their impending operation, thus support and interventions aimed at reducing this anxiety could be helpful to these patients. Previously, mental health has been found to influence HRQoL outcome.34 Therefore, it is important that anxiety and depression are assessed pre-operatively to identify undiagnosed depression and anxious patients.
Another predictor of recovery was pain. Pain has previously been reported as a predictor of outcome following THR, with a higher level of pain associated with poorer outcome9 and this study confirms this. Previously, patients with higher baseline function have been found to have less pain and better function at six months than those with lower baseline function.35 Ensuring that patients have appropriate information as well as access to treatments to reduce pain pre-operatively and post-operatively would be useful.
Taking NSAIDs were found to be a predictor of recovery following THR but taking weak or strong opioids was not a statistically significant predictor (just missing statistical significance at six months: p = 0.054). The use of medication for OA is variable and one study of patients with end-stage OA awaiting joint replacement found that patients often do not take adequate analgesia, or are taking analgesics which are ineffective in relation to their level of pain.36 Ensuring that patients have their medication assessed regularly and understanding how to take their medication is important during recovery from THR.
In individuals who previously had another joint replaced, this was found to influence recovery negatively. Only one study was identified which looked at previous joint procedures and this study found that patients with previous knee surgery undergoing THR had significantly lower improvements in physical and social functioning, but this was not found in previous hip surgery patients.37 It has also been shown that in patients having a THR, those with OA of the non-operative hip have less long-term improvement in function.9 Therefore, it is important to recognise that those individuals who have OA in other joints or previous joint replacements, may not have as much functional improvement as individuals who only have hip OA in the joint replaced.
There were a number of variables that did not influence recovery following THR and some of these are worthy of further discussion. The concept of social support has not been extensively studied in patients with OA or what influence having social support has on recovery following joint replacement. Only one study of individuals having a hip replacement has been identified and this found that having greater social support resulted in better post-operative outcomes.10 However, the research was limited by the way social support was measured, which was: married/not married and living alone/not living alone. There has been more extensive work using ESSI as a measure of social support with cardiac patients and having social support was an important predictor of recovery following myocardial infarction.38 We hypothesised that having social support would positively influence recovery following THR. However, social support as measured by the ESSI at baseline was not a predictor of outcome following THR. Despite, the ESSI being a valid and reliable instrument to measure social support, it may not have been the best measure to use with the OA population, as the instrument has mainly been used to measure social support with cardiac patients.22,38 Perhaps the Medical Outcomes Study (MOS) Social Support Survey instrument developed for individuals with chronic diseases39 might have been more appropriate to use in our population but the ESSI was selected over this instrument because of its applicability with surgical patients. Further research is needed on social support and its influence on recovery. We have shown that there are correlations between ESSI and TMS and between ESSI and HADS, so it would be important to use mental well-being as an outcome. Previous qualitative research has found that social support is important for patients during recovery following hip replacement20,40 and it is also important to those in deciding to undergo joint replacement surgery.41,42
Weight management is important for patients with OA and guidelines from NICE recommend interventions to achieve weight loss as a core treatment for individuals with OA.3 It is of concern that two-thirds of patients undergoing THR were overweight, with around a quarter of participants classed as obese (BMI > 30 kg/m2). However, BMI was not found to be a predictor of post-operative outcome in THR and this is consistent with another study.10 However, in the longer term it is unclear in those with a THR, the effects of being obese on mobility, physical functioning and on the replaced hip joint. One study of longer-term outcomes found that a high BMI and worse physical function pre-operatively were predictors for worse function at a follow-up of 3.6 years.9
Pre-operative comorbidity did not predict worse recovery. This supports the findings of a previous study that found comorbid conditions were not predictive of worse outcome using WOMAC function as primary outcome and also with SF-36 Total Physical Score as the primary outcome.6 Other studies have shown that having comorbidity had worse outcomes following THR.19,34and influenced the longer-term functional outcome of THR.43
The strength of this study was that participants were recruited from three study sites with different procedures for patients undergoing THR, thus making the study findings more generalisable. The study used reliable and valid measurement instruments. The use of the SF-36 Total Physical Score at six months as the outcome is also a strength of the study, as it has been shown to be as responsive as the disease-specific measures (such as WOMAC or the OHS)44 and shows a better gradient with comorbidities.9 The study was adequately powered to 80% for the main analysis, with the required sample size achieved. There was a lower attrition rate than was estimated at follow-ups of six and 12 months. A limitation of the study was the 46% rate of non-participation, which was largely affected by a poor response in one of the study sites. Another limitation was the loss of patients at each time period. Follow-up was also limited to the two time-points of six and 12 months, which did not allow for early post-operative outcomes and longer-term outcomes of THR to be assessed. Finally, using another measurement tool to assess social support other than the ESSI, which has mainly been used in the cardiac population, may have been more appropriate.
Achieving optimum recovery for patients following a THR is important. We have shown that patients do experience improvement in psychosocial and biomedical outcomes at six months after hip replacement. The strongest predictors of recovery were: anxiety and depression; pain, previous joint surgery and taking anti-inflammatory drugs. The identification of predictors affecting outcome of recovery will assist in providing guidance to health professionals and patients on how to enhance recovery following THR.
1 No authors listed. Health & Social Care Information Centre (HSCIC): Hospital Episode Statistics, Admitted Patient Care – England 2011-12. http://www.hscic.gov.uk/searchcatalogue?productid=9161& q=Procedures& sort=Relevance& size=10& page=1#top (date last accessed 17 April 2013). Google Scholar
2 No authors listed. Health & Social Care Information Centre (HSCIC): Hospital Episode Statistics, Admitted Patient Care – England 2007-08. http://www.hscic.gov.uk/searchcatalogue?productid=94& q=title%3a%22Hospital+Episode+Statistics%2c+Admitted+patient+care+-+England%22& sort=Relevance& size=10& page=1#top (date last accessed 17 April 2013). Google Scholar
3 National Institute for Health and Care Excellence. Osteoarthritis: the care and management of osteoarthritis in adults: Clinical Guideline 59. http://www.nice.org.uk/nicemedia/pdf/cg59niceguideline.pdf (date last accessed 16 October 2013). Google Scholar
4 Birrell F , AfzalC, NahitE, et al.Predictors of hip joint replacement in new attenders in primary care with hip pain. Br J Gen Pract2003;53:26–30.PubMed Google Scholar
5 Fitzpatrick R , ShortallE, SculpherM, et al.Primary total hip replacement surgery: a systematic review of outcomes and modelling of cost-effectiveness associated with different prosthesis. Health Technol Assess1998;2:1–64. Google Scholar
6 Nilsdotter AK , LohmanderLS. Age and waiting time as predictors of outcome after total hip replacement for osteoarthritis. Rheumatology2002;41:1261–1267.CrossrefPubMed Google Scholar
7 Dawson J , FitzpatrickR, FrostS, et al.Evidence for the validity of patient-based instrument for assessment of outcome after revision hip replacement. J Bone Joint Surg [Br]2001;83-B:1125–1129. Google Scholar
8 Bachmeier CJ , MarchLM, CrossMJ, et al.A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage2001;9:137–146.CrossrefPubMed Google Scholar
9 Nilsdotter AK , PeterssonIF, RoosEM, LohmanderLS. Predictors of patient relevant outcome after total hip replacement for osteoarthritis: a prospective study. Ann Rheum Dis2003;62:923–930.CrossrefPubMed Google Scholar
10 Fitzgerald JD , OravEJ, LeeTH, et al.Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum2004;51:100–109.CrossrefPubMed Google Scholar
11 Cushnaghan J , CoggonD, ReadingI, et al.Long-term outcome following total hip arthroplasty: a controlled longitudinal study. Arthritis Rheum2007;57:1375–1380.CrossrefPubMed Google Scholar
12 McHugh GA , CampbellM, LukerKA. Quality of care for individuals with osteoarthritis: a longitudinal study. J Eval Clin Prac2012;18:534–541.CrossrefPubMed Google Scholar
13 Beswick AD , WyldeV, Gooberman-HillR, BlomA, DieppeP. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis?: a systematic review of prospective studies in unselected patients. BMJ Open2012;2:000435. Google Scholar
14 McMurray A , GrantS, GriffithsS, LetfordA. Health-related quality of life and health service use following total hip replacement surgery. J Adv Nurs2002;40:663–672.CrossrefPubMed Google Scholar
15 Ethgen O , BruyèreO, RichyF, DardennesC, ReginsterJY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg [Am]2004;86-A:963–974. Google Scholar
16 Memel DS , KirwanJR, SharpDJ, HehirM. General practitioners miss disability and anxiety in their patients with osteoarthritis. Br J Gen Pract2000;50:645–648. Google Scholar
17 Rosemann T , GensichenJ, SauerN, LauxG, SzecsenyiJ. The impact of concomitant depression on quality of life and health service utilisation in patients with osteoarthritis. Rheumatol Int2007;27:859–863.CrossrefPubMed Google Scholar
18 Riediger W , DoeringS, KrismerM. Depression and somatisation influence the outcome of total hip replacement. Int Orthop2010;34:13–18.CrossrefPubMed Google Scholar
19 Rolfson O , DahlbergLE, NilssonJA, MalchauH, GarellickG. Variables determining outcome in total hip replacement surgery. J Bone Joint Surg [Br]2009;91-B:157–161.CrossrefPubMed Google Scholar
20 Grant S , St JohnW, PattersonE. Recovery from total hip replacement surgery: “it’s not just physical”. Qual Health Res2009;19:1612–1620. Google Scholar
21 Tabachnick BG, Fidell LS. Using multivariate statistics. Fourth ed. Needham Heights: Allyn and Bacon, 2001. Google Scholar
22 Mitchell PH , PowellL, BlumenthalJ, et al.A short social support measure for patients recovering from myocardial infarction: the ENRICHD Social Support Inventory. J Cardiopulm Rehabil2003;23:398–403.CrossrefPubMed Google Scholar
23 Zigmond AS , SnaithRP. The hospital anxiety and depression scale. Acta Psychiatr Scand1983;67:361–370. Google Scholar
24 Bjelland I , DahlAA, HaugTT, NeckelmannD. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res2002;52:69–77. Google Scholar
25 Snaith RP . The Hospital Anxiety and Depression Scale. Health Qual Life Outcomes2003;1:29. Google Scholar
26 Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey: manual and interpretation guide. Boston: The Health Institute New England Medical Centre, 1993. Google Scholar
27 Bellamy N , BuchananWW, GoldsmithCH, CampbellJ, StiffL. Validation study of WOMAC: a health status instrument for measuring clinically-important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol1988;1:95–108. Google Scholar
28 Dawson J , FitzpatrickR, FrostS, et al.Evidence for the validity of patient-based instrument for assessment of outcome after revision hip replacement. J Bone Joint Surg [Br]2001;83-B:1125–1129. Google Scholar
29 Murray DW , FitzpatrickR, RogersK, et al.The use of the Oxford hip and knee scores. J Bone Joint Surg [Br]2007;89-B:1010–1014. Google Scholar
30 Norusis MJ. SPSS 15.0 advanced statistical procedures companion. Prentice Hall: Pearson, 2007. Google Scholar
31 World Health Organization (WHO). Global database on Body Mass Index: BMI Classification. 2006. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html (date last accessed 13 November 2013). Google Scholar
32 Dawson J , FitzpatrickR, CarrA, MurrayD. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg [Br]1996;78-B:185–190.PubMed Google Scholar
33 Garbuz DS , XuM, SayreEC. Patients’ outcome after total hip arthroplasty: a comparison between the Western Ontario and McMaster Universities index and the Oxford 12-item hip score. J Arthroplasty2006;21:998–1004. Google Scholar
34 Quintana JM , EscobarA, AguirreU, LafuenteI, ArenazaJC. Predictors of health-related quality-of-life change after total hip arthroplasty. Clin Orthop Relat Res2009;467:2886–2894.CrossrefPubMed Google Scholar
35 Fortin PR , ClarkeAE, JosephL, et al.Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum1999;42:1722–1728.CrossrefPubMed Google Scholar
36 McHugh GA , LukerKA, CampbellM, KayPR, SilmanAJ. A longitudinal study exploring pain control, treatment and service provision for individuals with end-stage lower limb osteoarthritis. Rheumatology (Oxford)2007;46:631–637.CrossrefPubMed Google Scholar
37 Cleary PD , ReillyDT, GreenfieldS, et al.Using patient reports to assess health-related quality of life after total hip replacement. Qual Life Res1993;2:3–11.CrossrefPubMed Google Scholar
38 Dickens CM , McGowanL, PercivalC, et al.Lack of a close confidant, but not depression, predicts further cardiac events after myocardial infarction. Heart2004;90:518–522. Google Scholar
39 Sherbourne CD , StewartAL. The MOS social support survey. Soc Sci Med1991;32:705–714.CrossrefPubMed Google Scholar
40 McHugh GA , LukerKA. Individuals’ expectations and challenges following total hip replacement: a qualitative study. Disabil Rehabil2012;34:1351–1357. Google Scholar
41 Karlson EW , DaltroyLH, LiangMH, EatonHE, KatzJN. Gender differences in patient preferences may underlie differential utilization of elective surgery. Am J Med1997;102:524–530.CrossrefPubMed Google Scholar
42 McHugh GA , LukerKA. Influences on individuals with osteoarthritis in deciding to undergo a hip or knee joint replacement: a qualitative study. Disabil Rehabil2009;31:1257–1266.CrossrefPubMed Google Scholar
43 Gandhi R , DhotarH, DaveyJR, MahomedNN. Predicting the longer-term outcomes of total hip replacement. J Rheumatol2010;37:2573–2577.CrossrefPubMed Google Scholar
44 Marx RG , JonesEC, AtwanNC, et al.Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J Bone Joint Surg [Am]2005;87-A:1999–2005.CrossrefPubMed Google Scholar
Funding statement:
GM received funding for the study under the terms of a post-doctoral research training fellowship from the National Institute for Health Research (NIHR).
Author contributions:
G. A. McHugh: Study conception, Study design and conduct, Data collection, Data analysis, Writing the paper
M. Campbell: Design & Conduct, Data Analysis, Writing the paper
K. A. Luker: Study conception, Study design and conduct, Writing the paper
ICMJE Conflict of Interest:
None declared
©2013 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










