Abstract
Objectives
The spinopelvic relationship (including pelvic incidence) has been shown to influence pelvic orientation, but its potential association with femoroacetabular impingement has not been thoroughly explored. The purpose of this study was to prove the hypothesis that decreasing pelvic incidence is associated with increased risk of cam morphology.
Methods
Two matching cohorts were created from a collection of cadaveric specimens with known pelvic incidences: 50 subjects with the highest pelvic incidence (all subjects > 60°) and 50 subjects with the lowest pelvic incidence (all subjects < 35°). Femoral version, acetabular version, and alpha angles were directly measured from each specimen bilaterally. Cam morphology was defined as alpha angle > 55°. Differences between the two cohorts were analysed with a Student’s t-test and the difference in incidence of cam morphology was assessed using a chi-squared test. The significance level for all tests was set at p < 0.05.
Results
Cam morphology was identified in 47/100 (47%) femurs in the cohort with pelvic incidence < 35° and in only 25/100 (25%) femurs in the cohort with pelvic incidence > 60° (p = 0.002). The mean alpha angle was also greater in the cohort with pelvic incidence < 35° (mean 53.7°, sd 10.7° versus mean 49.7°, sd 10.6°; p = 0.008).
Conclusions
Decreased pelvic incidence is associated with development of cam morphology. We propose a novel theory wherein subjects with decreased pelvic incidence compensate during gait (to maintain optimal sagittal balance) through anterior pelvic tilt, creating artificial anterior acetabular overcoverage and recurrent impingement that increases risk for cam morphology.
Cite this article: W. Z. Morris, C. A. Fowers, R. T. Yuh, J. J. Gebhart, M. J. Salata, R. W. Liu. Decreasing pelvic incidence is associated with greater risk of cam morphology. Bone Joint Res 2016;5:387–392. DOI: 10.1302/2046-3758.59.BJR-2016-0028.R1.
Article focus
-
The spinopelvic relationship influences pelvic tilt to achieve sagittal balance.
-
Pelvic tilt affects relative acetabular coverage and may increase the risk of mechanical impingement.
-
The purpose of the study was to assess whether pelvic incidence affects the risk for development of cam morphology.
Key messages
-
Low pelvic incidence was associated with an increased risk of concurrent cam morphology.
-
Low pelvic incidence may lead to compensatory anterior pelvic tilt, causing relative anterior acetabular overcoverage and an increased risk of impingement.
Strengths and limitations
-
This large cadaveric study permits unique evaluation of the anatomic contribution of pelvic incidence on cam morphology.
-
Cadaveric studies do not provide clinical or kinematic data.
Introduction
Investigation of risk factors that predispose patients to femoroacetabular impingement (FAI) have focused on morphological parameters about the hip including relative femoral or acetabular retroversion1,2 and slipped capital femoral epiphysis (SCFE).3,4 However, little attention has been paid to the influence of sagittal balance of the spine and the spinopelvic relationship on the development of FAI.
The spinopelvic relationship is determined by both morphologic and functional parameters which combine to influence the kinematics of the hip. The goal of this relationship is highlighted by Lazennec, Brusson and Rousseau5 who illustrated that the spinopelvic relationship uses a postural strategy in order to maintain sagittal balance by positioning the centre of gravity of the trunk such that it is supported by the femoral heads relative to the pelvic base. This strategy allows for the most economical standing posture6 and relies on interplay between lumbar lordosis (LL) and pelvic incidence.
Pelvic incidence (PI), a static, position-independent sacropelvic parameter introduced by Legaye et al,7 is defined as the angle formed between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axis of the femoral heads (Fig. 1). Legaye et al7 introduced this concept and also demonstrated its close association with lumbar lordosis. Boulay et al8 further examined the relationship between PI and LL and found a direct association wherein subjects with lower PI had a lower LL in the upright position. While PI is a static, position-independent sacropelvic parameter, it is composed of two positional parameters, pelvic tilt and sacral slope (Fig. 1), which may change dynamically in response to postural changes to maintain sagittal balance. Pelvic tilt is defined as the angle between the vertical line and the line connecting the midpoint of the sacral plate and the femoral axis.7 Previous work has demonstrated that pelvic tilt may act as a compensatory mechanism in the PI-LL relationship. Furthermore, in patients with increased PI (and consequently increased LL), posterior pelvic tilt occurs in order to maintain sagittal alignment.9
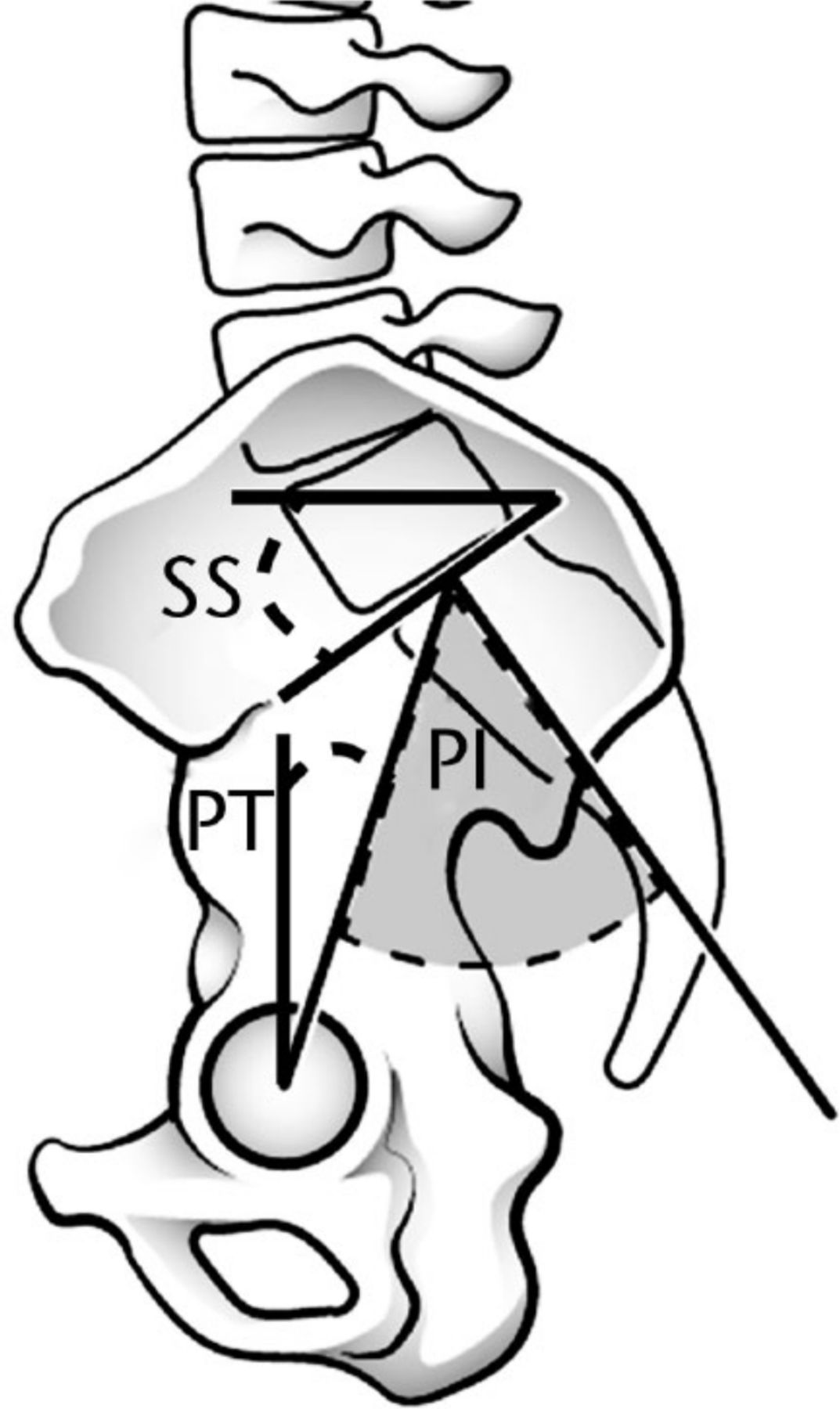
Fig. 1
Illustration of a lateral view of the pelvis and lumbar spine demonstrating the non-positional sacropelvic parameter, pelvic incidence (PI), and its positional components, sacral slope (SS) and pelvic tilt (PT). PI is defined as the angle formed between the line perpendicular to the sacral plate at its midpoint and the line connecting this point to the axis of the femoral heads. PT is defined as the angle between the vertical and the line connecting the midpoint of the sacral plate and the femoral axis. SS is defined as the angle between the superior plate of S1 and a horizontal line.
Given the evidence that the body posturally compensates to maintain appropriate LL, we hypothesised that patients with lower PI (and consequently lower LL) would compensate to maintain sagittal balance by increasing anterior pelvic tilt (and consequently increasing LL), causing relative anterior acetabular overcoverage of the hip. Anterior pelvic tilt has previously been shown to cause this overcoverage and decrease the hip range of motion prior to impingement.10 Although the aetiology of cam remains unclear, a theoretical model recently revealed that recurrent mechanical impingement could lead to growth plate alterations and development of cam.11 Growth plate alterations have subsequently been identified prior to cam development in adolescents.12-14 Relative anterior acetabular overcoverage (as a consequence of low pelvic incidence) would similarly increase the risk for repetitive mechanical impingement, and could subsequently lead to cam formation through this mechanism. A preliminary study supported this theory as it demonstrated that patients with bilateral cam morphology had lower PI than matched controls.15 However, this study was limited by a small sample size (20 specimens with bilateral cam morphology) and did not examine the potential association of femoral version in cam morphology. The purpose of our study was to further validate the relationship between low PI and the incidence of cam morphology and to propose a novel theory of a kinematic mechanism through which femoroacetabular impingement may occur in patients with low PI.
Materials and Methods
For our investigation, we used cadaveric pelvises and femurs from the Hamann-Todd Osteological Collection. The collection is comprised of approximately 3000 well-preserved, disarticulated skeletons obtained between 1912 and 1938 from the unclaimed dead of Cleveland-area morgues. We identified two cohorts from a pool of 598 randomly selected skeletons for whom PI was previously measured (see below). All specimens were in good condition and any specimens with evidence of deformity or fracture were excluded from this study. The two cohorts consisted of: 50 pelvises with the lowest measured PI of the sample population (all specimens with PI < 35°) and 50 pelvises with the highest measured PI of the sample population (all specimens with PI > 60°) within the group.
Acetabular version and PI were previously measured in the nearly 600 specimens in a standardised fashion after reassembling the pelvises in a method previously described in other osteological studies.15-18 The two hemipelvises were re-attached to the sacrum with rubber bands with a 12 mm piece of foam used to represent the cartilage of the pubic symphysis (Fig. 2). The sacroiliac joints were visually inspected to confirm congruous reconstruction. Reassembled specimens were all placed with the anterior superior iliac spines and pubic crest resting on the laboratory table in order to establish the anatomic frontal plane of the pelvis.16,19 The central acetabular version was measured for each of the 200 hips (100 hips per cohort) as the complement to the angle formed between the laboratory table (representing the horizontal plane) and a line connecting the anterior and posterior ridges of the acetabulum using a goniometer (Prestige Medical, Northridge, California) (Fig. 2). The measured acetabular version (AV) was therefore referenced from the perpendicular to the anatomic frontal plane of the pelvis. Attention was then moved to determination of pelvic incidence. After reassembly, pelvises were repositioned to rest on the sacrum and ischial tuberosities. A quilter’s ruler (Dritz, Spartanburg, South Carolina) was then used to mark both the centre and the slope of the S1 endplate. Standardised direct lateral photographs were obtained of the pelvis with the ruler in place. All images were processed and angles measured using Image J software (National Institutes of Health, Bethesda, Maryland). A best-fit ellipse was drawn to fit the acetabular rim. Pelvic incidence was then measured based on the technique by Legaye et al7 as the angle formed between a line perpendicular to the midpoint of the sacral endplate and a line connecting the centre of the sacral endplate and the centre of the best-fit ellipse of the acetabular rim (Fig. 3). It is important to note that the relationship between the sacral endplate and the acetabulum is static and will not change regardless of the position of the pelvis in space. Therefore, pelvic incidence is a static measurement that is independent of the position of the pelvis.
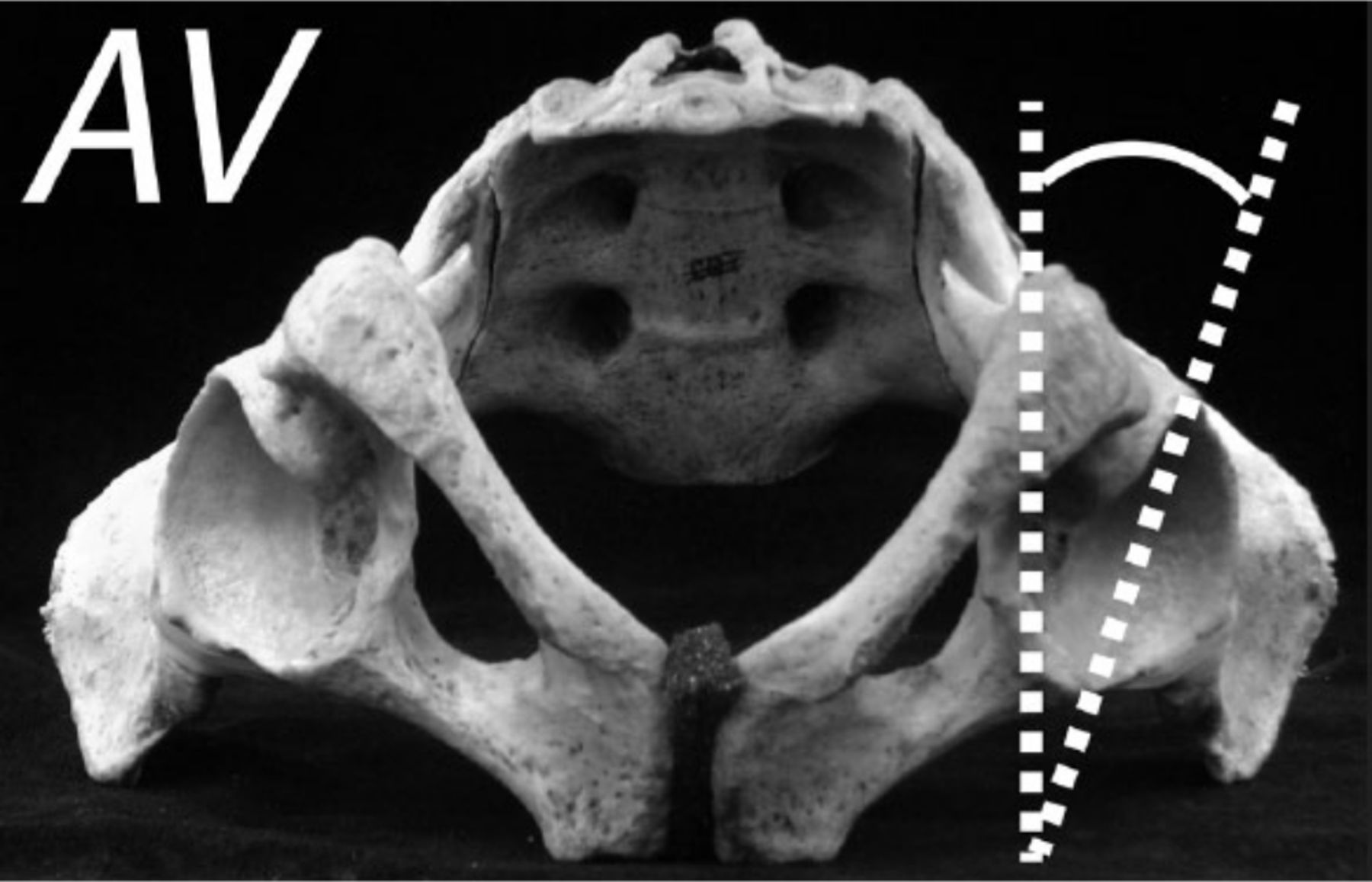
Fig. 2
Measurement of acetabular version. The central acetabular version (AV) is defined as the complement to the angle formed between the horizontal plane (represented by the laboratory table) and a line connecting the anterior and posterior ridges of the acetabulum.
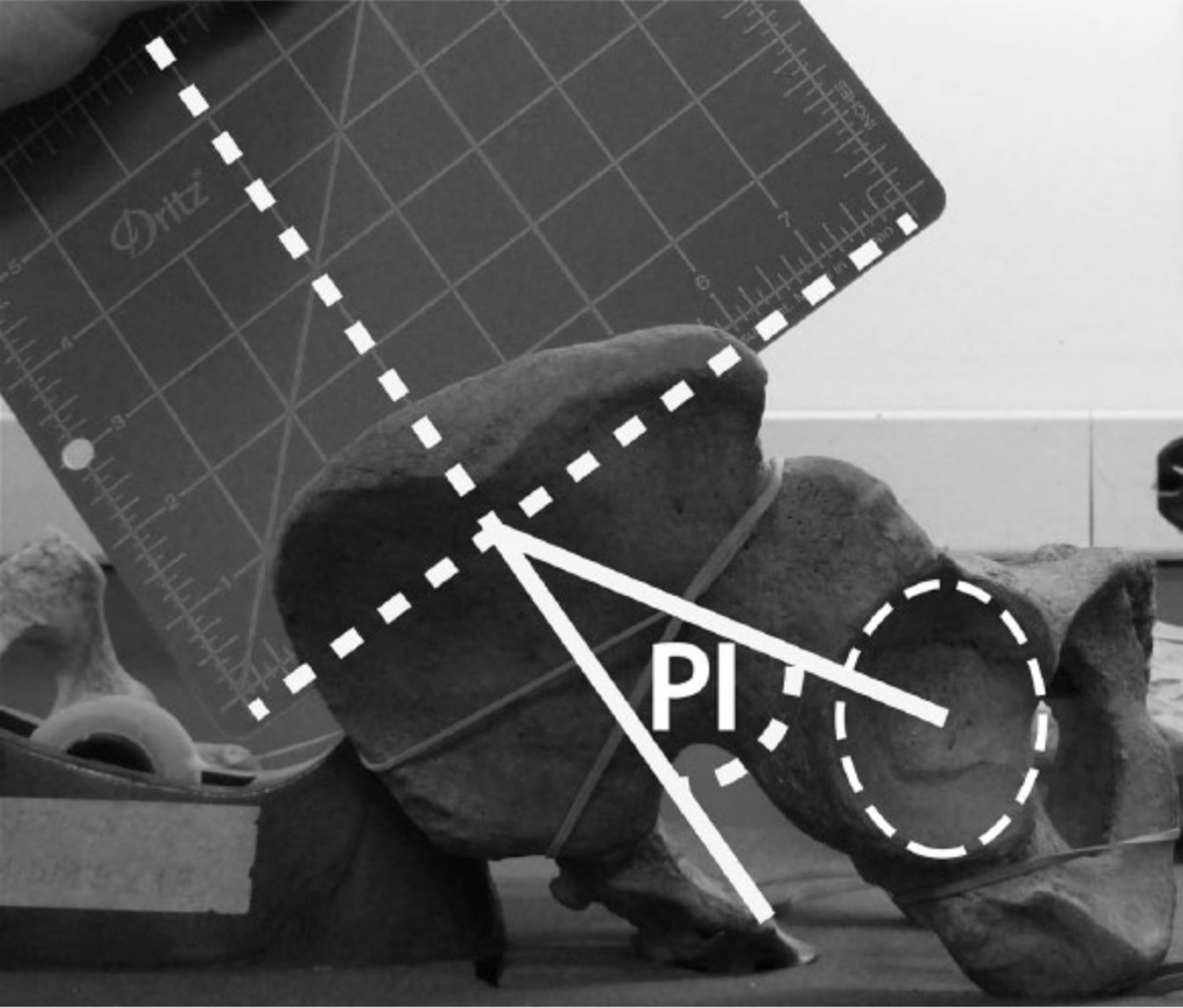
Fig. 3
Measurement of pelvic incidence (PI), which was defined as the angle formed between a line perpendicular to the midpoint of the sacral endplate and a line connecting the centre of the sacral endplate and the centre of the best-fit ellipse of the acetabular rim. The best fit ellipse of the acetabular rim serves as a surrogate marker of the femoral head axis.
Each femur was then individually assessed by two authors to determine femoral version and alpha angle. Authors were blinded with regard to whether the femora pertained to the “high” or “low” pelvic incidence groups. Femoral anteversion was measured using the Kingsley-Olmsted method.20,21 This method involves placement of the femurs in a standardised position with the posterior aspect of the greater trochanter and distal femoral condyles resting on wood blocks. A digital axial photograph is then obtained from a craniocaudal view of the femur. The angle of anteversion is defined as the intersection of the plane of the full length of the femur (connecting the posterior aspects of the condyles to the posterior aspect of the greater trochanter) and the axis of the femoral neck. Alpha angle was measured for each femur based on a modification of the technique originally described by Notzli.22,23 Specimens were placed in the above-mentioned standardised position and photographs were taken in an angled craniocaudal view perpendicular to the femoral neck. Image J was then used to place a best-fit circle over the femoral head and a line representing the centre of the femoral neck axis. The alpha angle is defined as the angle formed by the line representing the femoral neck axis to the centre of the femoral head and a line from the centre of the femoral head to the femoral head-neck junction (Fig. 4). Specimens were considered to have cam morphology with an alpha angle > 55°.12,15
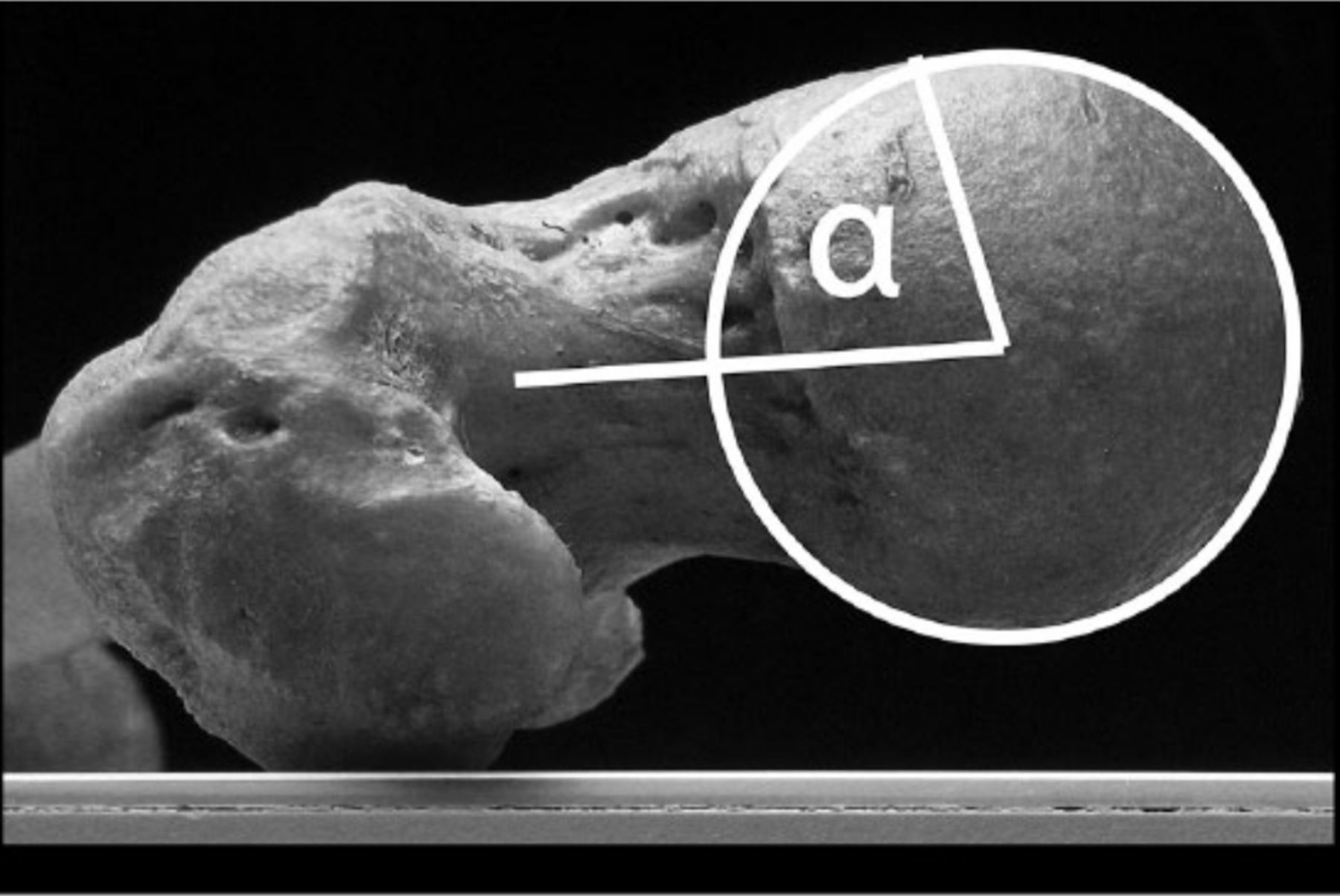
Fig. 4
Measurement of alpha angle (α), which is defined as the angle formed by the line representing the femoral neck axis to the centre of the femoral head and a line from the centre of the femoral head to the point where femoral head-neck junction exits a best-fit circle around the femoral head.
Statistical analysis
All statistical analyses were performed with SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. IBM, Armonk, New York). Pelvic incidence, acetabular version, femoral version, and alpha angle measurements among the specimens were characterised with descriptive statistics. Additionally, differences between the cohorts in acetabular version, femoral version, and alpha angle were compared using Student’s t-tests. The incidence of cam morphology between the two groups was compared using a chi-squared test. The significance level for all tests was set at p < 0.05.
Inter- and intra-observer agreement was determined for each variable through measurement of 20 specimens by the initial assessor and an additional assessor. The intraclass correlation coefficient for inter- and intra-observer reliability was then calculated. The values were interpreted as follows: < 0.40 was considered poor, 0.40 to 0.59 was considered fair, 0.60 to 0.74 was considered good, and > 0.74 was considered excellent.24,25
Results
Femurs from the cohort of 50 pelvises (100 hips) with the lowest pelvic incidence (< 35°) demonstrated an increased mean alpha angle (53.7; sd 10.7) compared with the cohort of 50 pelvises with the highest pelvic incidence (all specimens > 60°; mean alpha angle 49.7; sd 10.6; p = 0.008). We also examined conventionally held pelvic parameters believed to be associated with cam morphology: femoral and acetabular version. There was no statistically significant difference between mean femoral version of the cohort with lower pelvic incidence (10.4°, sd 9.6°) compared with the cohort with higher pelvic incidence (9.7°; sd 9.5°; p = 0.631). There was a trend towards relative acetabular retroversion in the cohort with lower pelvic incidence (17.0°; sd 6.2° versus 18.9°; sd 7.2°), but analysis revealed that this difference fell just outside of significance (p = 0.05). Furthermore, when the subjects were re-categorised to those with and without cam morphology, there was no significant difference in acetabular version in those subjects with cam morphology (n = 72; 18.4°; sd 6.9°) compared with those without cam (n = 128; 17.7°; sd 6.7°; p = 0.443).
The data were separately analysed for the incidence of cam morphology (defined as alpha > 55°). Interestingly, although the mean difference in alpha angle between the groups with low and high pelvic incidence was small (53.7; sd 10.7 and 49.7; sd 10.6, respectively), analysis revealed that there was a greater incidence of cam morphology in the cohort with low pelvic incidence (47/100, 47%) compared with the cohort with high pelvic incidence (25/100, 25%). This difference was found to be significant using a chi-squared test (p = 0.002).
Inter- and intra-observer agreement
A total of 20 femurs, acetabula, and pelvises were remeasured by two authors (WZM, CAF). The intraclass correlation coefficient showed excellent inter-observer agreement between the two authors for alpha angle (0.81), pelvic incidence (0.91), femoral version (0.98), and acetabular version (0.88) measurements. The intraclass correlation coefficient also demonstrated excellent intra-observer agreement for alpha angle (0.94), pelvic incidence (0.95), femoral version (0.95), and acetabular version (0.96).
Discussion
Femoroacetabular impingement is increasingly recognised as a cause of hip pain in adolescents and young adults. Studies of symptomatic individuals with femoroacetabular impingement syndrome have revealed that relative femoral and acetabular retroversion are risk factors for symptomatic disease. While there has been extensive investigation of these pelvic parameters, only a preliminary study has investigated the potential role of pelvic incidence and sagittal spinal balance as a risk factor for development of cam morphology.15
Using a separate, expanded cohort of specimens, our current study confirmed the finding that decreased pelvic incidence is associated with increased risk of cam morphology. The mean alpha angle and the incidence of cam morphology were both significantly increased in the cohort with low pelvic incidence. In contrast to the preliminary study which contained 20 specimens per cohort, our follow-up expanded the cohorts to 100 hips per group (a total of 200 hips) and also examined the most commonly associated risk factors for FAI: femoral and acetabular version. We further demonstrated that there was no statistically significant difference between the cohorts’ mean femoral or acetabular version, though the cohort with low pelvic incidence trended towards relative acetabular retroversion (consistent with the previous study). Low pelvic incidence has previously been associated with acetabular retroversion.26 However, when we recategorised our subjects to those with or without cam morphology, there was no difference in acetabular version between the groups. We consequently believe that the changes seen in incidence of cam are reflective of the differences in pelvic incidence.
We believe that the association between decreased pelvic incidence and cam morphology is based on the spinopelvic postural changes the body performs to maintain sagittal balance. Previous studies, primarily in the spine literature, have demonstrated that the body effects postural changes in order maintain the centre of gravity of the trunk so that it is supported by the femoral heads relative to the pelvic base.5,27 Studies have also revealed a direct relationship between pelvic incidence and lumbar lordosis8 and that the body posturally compensates for higher lumbar lordosis with posterior pelvic tilt.9 Yoshimoto et al9 illustrated radiographically that this posterior pelvic tilt caused relative acetabular undercoverage and an increased risk for hip osteoarthritis. We propose that the converse is also true: in patients with decreased pelvic incidence (and consequently decreased lumbar lordosis), the body affects the same postural strategy to optimise lumbar lordosis through anterior pelvic tilt.
As illustrated in Figure 5, we propose that compensatory pelvic tilt may lead to relative acetabular over- or undercoverage. In patients with elevated pelvic incidence, there is increased lumbar lordosis and a postural strategy to decrease lordosis through posterior pelvic tilt. This posterior tilt causes relative acetabular undercoverage, similar to a dysplastic hip, and has been associated with increased risk of osteoarthritis.9 Conversely, in patients with decreased pelvic incidence, there is decreased lumbar lordosis and a postural strategy to increase lordosis through anterior pelvic tilt. Anterior pelvic tilt has been shown to cause relative anterior acetabular overcoverage and increase the risk of mechanical femoroacetabular impingement with hip flexion and internal rotation.10 A theoretical model suggested that recurrent mechanical impingement could lead to growth plate alterations and development of cam,11 findings which have been reinforced by recent studies demonstrating that adolescents develop concurrent growth plate changes and cam morphology.12-14 Although we have no kinematic data from our cadaveric subjects, this hypothesis is consistent with the increased incidence of cam morphology seen in the cohort with decreased pelvic incidence.
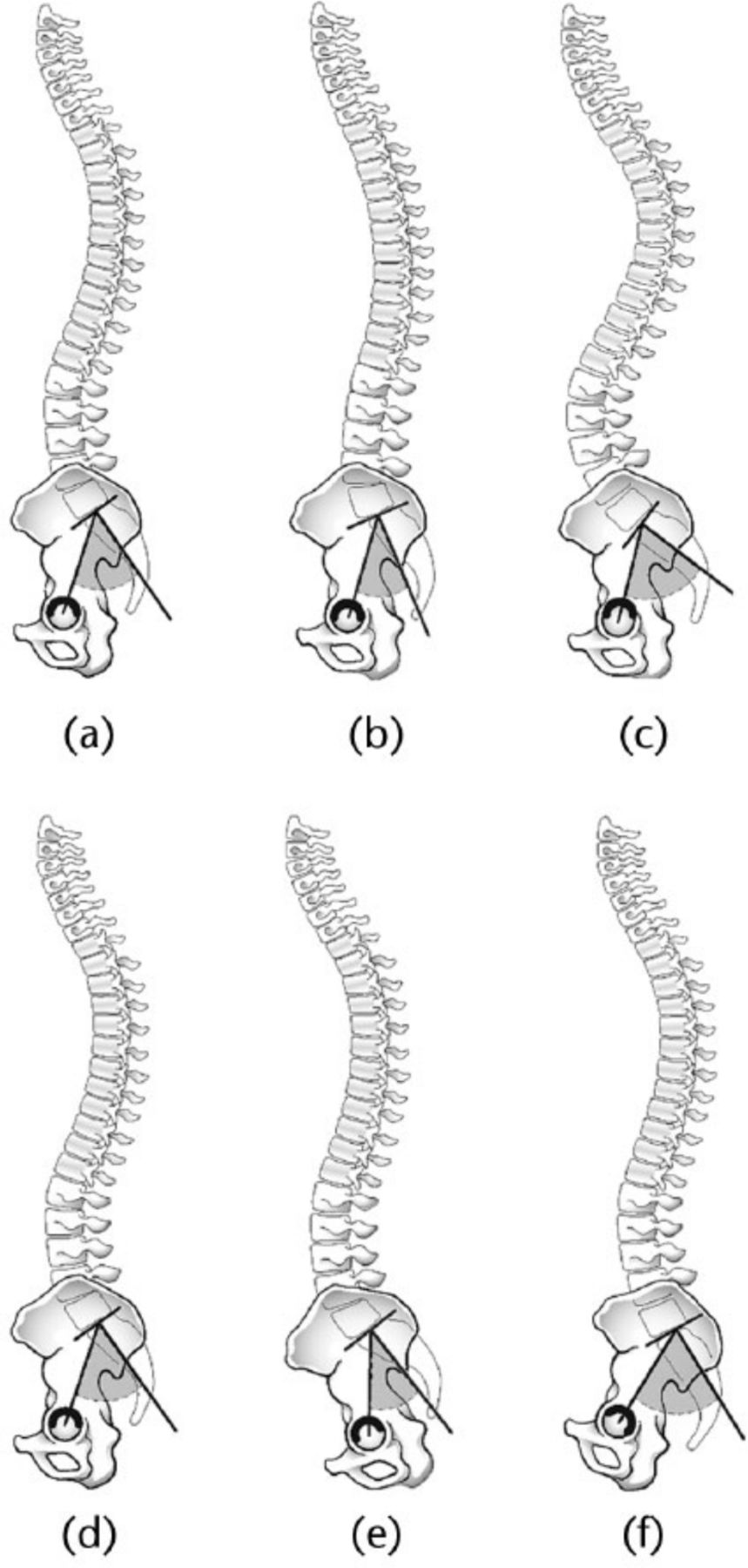
Fig. 5
Proposed kinematic mechanism for pelvic incidence influencing hip impingement. Top row: Pelvic orientation and lumbar lordosis corresponding to normal (a), low (b), and high (c) pelvic incidence. Bottom row: Proposed compensatory pelvic tilt in order to maintain appropriate sagittal balance and normalise lumbar lordosis. The pelvis with normal pelvic incidence (d) is static. The pelvises with low (e) and high (f) pelvic incidence normalise their lumbar lordosis through anterior and posterior pelvic tilt, respectively.
There are two significant limitations to our study. The first limitation is the use of disarticulated cadaveric specimens without soft tissues or cartilage. This required us to reassemble hemipelvises and sacra into a pelvic ring using a standard piece of foam to represent the pubic symphysis. This creates the potential for inaccuracies in pelvic orientation and consequent errors in our measurements. However, we methodically recreated the pelvic ring in a standardised fashion using a previously published technique15-17 to minimise the errors in reproduction of the ring. This resulted in acetabular version measurements that fell within the range of population norms of approximately 15° to 20°.28,29 The measurement of pelvic incidence was also based on a direct lateral photograph of the pelvic ring, mimicking the view of a lateral radiograph. This required us to reference the femoral head axis from the centre of a best-fit ellipse of the acetabulum. Although there may be slight positional differences between these anatomic landmarks, a large cadaveric study using the Hamann Todd osteological collection30 recently revealed that this measurement technique provided pelvic incidence measurements consistent with the other published literature.31 Consequently, we believe our technique provides a faithful recreation of the pelvic ring. Furthermore, it is important to emphasise that pelvic incidence is a static pelvic parameter and does not change depending on the orientation of the pelvis in space. Therefore, a faithful reconstruction of the pelvis provides accurate pelvic incidence measurement regardless of the manner in which the pelvis is oriented in space. The second major limitation of the study is the absence of clinical data from our subjects. We have no way of knowing whether any of these subjects had symptomatic FAI during life or whether decreased pelvic incidence has any association with increased symptomatic FAI. We are also unable to obtain any functional radiographic data to demonstrate this kinematic theory of compensatory relative anterior acetabular overcoverage.
In conclusion, our study further supports the association between decreased pelvic incidence and increased risk of cam morphology. We have proposed a novel kinematic mechanism through which decreased pelvic incidence (and consequent compensatory postural changes for sagittal balance) may lead to anterior pelvic tilt, relative anterior acetabular overcoverage, and recurrent mechanical impingement which increases the risk for cam morphology. Identification of potentially modifiable risk factors such as pelvic tilt may provide avenues for conservative management of these risk factors through treatments such as postural modifications with physical therapy. Further studies are needed in a clinical setting to investigate this association in patients with symptomatic femoroacetabular impingement.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
M. J. Salata received consultancy fees from Smith & Nephew which is not related to this article.
R. W. Liu receives royalties from Orthopaediatrics Corp which are not related to this article.
We wish to thank Lyman Jellema, Collections Manager for Physical Anthropology at the Cleveland Museum of Natural History, for his assistance with the Hamann-Todd Osteological Collection.
ICMJE conflict of interest
None declared
References
1 Ito K , MinkaMAII, LeunigM, WerlenS, GanzR. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg [Br]2001;83-B:171-176.CrossrefPubMed Google Scholar
2 Siebenrock KA , SchoenigerR, GanzR. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg [Am]2003;85-A:278-286.CrossrefPubMed Google Scholar
3 Rab GT . The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop1999;19:419-424.CrossrefPubMed Google Scholar
4 Leunig M , CasillasMM, HamletM, et al.. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand2000;71:370-375.CrossrefPubMed Google Scholar
5 Lazennec JY , BrussonA, RousseauMA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J2011;20(Suppl 5):686-698.CrossrefPubMed Google Scholar
6 Duval-Beaupère G , SchmidtC, CossonP. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng1992;20:451-462.CrossrefPubMed Google Scholar
7 Legaye J , Duval-BeaupèreG, HecquetJ, MartyC. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J1998;7:99-103.CrossrefPubMed Google Scholar
8 Boulay C , TardieuC, HecquetJ, et al.. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J2006;15:415-422.CrossrefPubMed Google Scholar
9 Yoshimoto H , SatoS, MasudaT, et al.. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976)2005;30:1650-1657.CrossrefPubMed Google Scholar
10 Ross JR , NeppleJJ, PhilipponMJ, et al.. Effect of changes in pelvic tilt on range of motion to impingement and radiographic parameters of acetabular morphologic characteristics. Am J Sports Med2014;42:2402-2409.CrossrefPubMed Google Scholar
11 Roels P , AgricolaR, OeiEH, et al.. Mechanical factors explain development of cam-type deformity. Osteoarthritis Cartilage2014;22:2074-2082.CrossrefPubMed Google Scholar
12 Siebenrock KA , BehningA, MamischTC, SchwabJM. Growth plate alteration precedes cam-type deformity in elite basketball players. Clin Orthop Relat Res2013;471:1084-1091.CrossrefPubMed Google Scholar
13 Agricola R , HeijboerMP, GinaiAZ, et al.. A cam deformity is gradually acquired during skeletal maturation in adolescent and young male soccer players: a prospective study with minimum 2-year follow-up. Am J Sports Med2014;42:798-806.CrossrefPubMed Google Scholar
14 Morris WZ , WeinbergDS, GebhartJJ, CoopermanDR, LiuRW. Capital femoral growth plate extension predicts cam deformity in a longitudinal radiographic study. J Bone Joint Surg [Am]2016;98-A:805-812. Google Scholar
15 Gebhart JJ , StreitJJ, BediA, et al.. Correlation of pelvic incidence with cam and pincer lesions. Am J Sports Med2014;42:2649-2653.CrossrefPubMed Google Scholar
16 Maruyama M , FeinbergJR, CapelloWN, D’AntonioJA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res2001;393:52-65.PubMed Google Scholar
17 Krebs V , IncavoSJ, ShieldsWH. The anatomy of the acetabulum: what is normal?Clin Orthop Relat Res2009;467:868-875.CrossrefPubMed Google Scholar
18 Gebhart JJ , BohlMS, WeinbergDS, CoopermanDR, LiuRW. Pelvic incidence and acetabular version in slipped capital femoral epiphysis. J Pediatr Orthop2015;35:565-570.CrossrefPubMed Google Scholar
19 Abel MF , SutherlandDH, WengerDR, MubarakSJ. Evaluation of CT scans and 3-D reformatted images for quantitative assessment of the hip. J Pediatr Orthop1994;14:48-53.CrossrefPubMed Google Scholar
20 Liu RW , ToogoodP, HartDE, DavyDT, CoopermanDR. The effect of varus and valgus osteotomies on femoral version. J Pediatr Orthop2009;29:666-675.CrossrefPubMed Google Scholar
21 Kingsley PC , OlmstedKL. A study to determine the angle of anteversion of the neck of the femur. J Bone Joint Surg [Am]1948;30-A:745-751.PubMed Google Scholar
22 Nötzli HP , WyssTF, StoecklinCH, et al.. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg [Br]2002;84-B:556-560.CrossrefPubMed Google Scholar
23 Toogood PA , SkalakA, CoopermanDR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res2009;467:876-885.CrossrefPubMed Google Scholar
24 Cicchetti DV , SparrowSA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adaptive behavior. Am J Ment Defic1981;86:127-137.PubMed Google Scholar
25 Shrout PE , FleissJL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull1979;86:420-428.CrossrefPubMed Google Scholar
26 Tiziani S , GautierL, Farei-CampagnaJ, et al.. Correlation of pelvic incidence with radiographical parameters for acetabular retroversion: a retrospective radiological study. BMC Med Imaging2015;15:39.CrossrefPubMed Google Scholar
27 Lazennec JY , CharlotN, GorinM, et al.. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat2004;26:136-144.CrossrefPubMed Google Scholar
28 Tönnis D , HeineckeA. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg [Am]1999;81-A:1747-1770.CrossrefPubMed Google Scholar
29 Jamali AA , MladenovK, MeyerDC, et al.. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the "cross-over-sign". J Orthop Res2007;25:758-765.CrossrefPubMed Google Scholar
30 Weinberg DS , MorrisWZ, GebhartJJ, LiuRW. Pelvic incidence: an anatomic investigation of 880 cadaveric specimens. Eur Spine J2015; Nov4 (Epub ahead of print).CrossrefPubMed Google Scholar
31 Vrtovec T , JanssenMM, LikarB, et al.. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J2012;12:433-446.CrossrefPubMed Google Scholar









