Abstract
Objectives
Cement augmentation of pedicle screws could be used to improve screw stability, especially in osteoporotic vertebrae. However, little is known concerning the influence of different screw types and amount of cement applied. Therefore, the aim of this biomechanical in vitro study was to evaluate the effect of cement augmentation on the screw pull-out force in osteoporotic vertebrae, comparing different pedicle screws (solid and fenestrated) and cement volumes (0 mL, 1 mL or 3 mL).
Materials and Methods
A total of 54 osteoporotic human cadaver thoracic and lumbar vertebrae were instrumented with pedicle screws (uncemented, solid cemented or fenestrated cemented) and augmented with high-viscosity PMMA cement (0 mL, 1 mL or 3 mL). The insertion torque and bone mineral density were determined. Radiographs and CT scans were undertaken to evaluate cement distribution and cement leakage. Pull-out testing was performed with a material testing machine to measure failure load and stiffness. The paired t-test was used to compare the two screws within each vertebra.
Results
Mean failure load was significantly greater for fenestrated cemented screws (+622 N; p ⩽ 0.001) and solid cemented screws (+460 N; p ⩽ 0.001) than for uncemented screws. There was no significant difference between the solid and fenestrated cemented screws (p = 0.5). In the lower thoracic vertebrae, 1 mL cement was enough to significantly increase failure load, while 3 mL led to further significant improvement in the upper thoracic, lower thoracic and lumbar regions.
Conclusion
Conventional, solid pedicle screws augmented with high-viscosity cement provided comparable screw stability in pull-out testing to that of sophisticated and more expensive fenestrated screws. In terms of cement volume, we recommend the use of at least 1 mL in the thoracic and 3 mL in the lumbar spine.
Cite this article: C. I. Leichtle, A. Lorenz, S. Rothstock, J. Happel, F. Walter, T. Shiozawa, U. G. Leichtle. Pull-out strength of cemented solid versus fenestrated pedicle screws in osteoporotic vertebrae. Bone Joint Res 2016;5:419–426.
Article focus
-
The evaluation of the pull-out force for solid and fenestrated cemented screws as well as uncemented screws from osteoporotic vertebrae.
-
The comparison of two different cement volumes (1 mL, 3 mL).
-
The consideration of vertebra level (upper thoracic, lower thoracic and lumbar) and bone mineral density.
Key messages
-
Conventional, solid pedicle screws augmented with high viscosity cement provided comparable pull-out strength as sophisticated, more expensive fenestrated screws.
-
We recommend the use of at least 1 mL cement in the thoracic and 3 mL in the lumbar spine.
-
Bone mineral density (BMD) and insertion torque might be good predictors of screw stability, particularly in the uncemented screws.
Strengths and limitations
-
Strength: three study groups, each with paired comparison of two screw types implanted in the left and right pedicle of the same vertebra.
-
Strength: randomisation with respect to BMD measured by dual-energy X-ray absorptiometry and vertebra level.
-
Limitation: use of embalmed vertebra specimens.
Introduction
Osteoporosis contributes to the risk of revision instrumented spine surgery because of failure of pedicle screw fixation from loosening or cutting out. Cement augmentation of pedicle screws could increase the mechanical strength of the interface between the screw and bone. Biomechanical studies have demonstrated an increased resistance to failure of the screw-bone interface after augmentation with bone cement.1-7 Numerous clinical follow-up studies have reported good functional outcomes and very low revision rates with poly methyl methacrylate (PMMA)-augmented screws.8-13
However, this technique may be complicated by cement leakage and embolism. Cement may leak into the spinal canal, especially with larger volumes of cement and osteoporotic bone.14,15 Low-viscosity cement may be susceptible to cement leakage and risk of embolism. Therefore, high-viscosity cement was developed but limited outcome data are available.
Although the increased mechanical stability of implants augmented with cement has been sufficiently demonstrated in terms of significantly increased axial pull-out strength, transverse bending stiffness, and resistance to toggle,3,5,6,16-18 cement augmentation raises a multitude of further questions. One major issue is the use of solid or fenestrated screws. Fenestrated screws enable the injection of cement after screw insertion and may minimise operative time and placement error compared with solid cemented screws because fenestrated screws are not removed before cement application.2 However, previous biomechanical studies have shown controversial results regarding the failure load of these screws. Compared with conventional solid pedicle screws, the fenestrated screws achieved either increased,4 were equal to16 or decreased10,19 pull-out forces.
The optimal cement volume for proper screw fixation is also controversial. A cement volume of 1 mL to 3 mL has been suggested as optimal,1 with > 3 mL providing no improvement in fixation strength6 and greater potential for cement leakage. However, the guideline of using 1 mL to 3 mL cement is approximate because of potential variations of volume needed for different spinal segments (thoracic or lumbar), bony conditions (normal or osteoporotic), vertebral body sizes, types of pedicle screw (fenestrated or solid cemented) and viscosity of cement (low or high). Systematic approaches are required to identify the minimal amount of PMMA that provides stability against screw migration and cut-out in osteoporotic bone. However, only one study20 was found where different volumes of bone cement were systematically compared for thoracic and lumbar vertebrae in separate groups. This study provided unexpected results, in particular for the lumbar area, where decreasing pull-out strength was reported for increasing cement volume, suggesting further research is required.
Another interesting issue concerning pedicle screws is the predictive ability of the expected pull-out force from the insertion torque, which can be measured intra-operatively. While many older studies demonstrated high correlations between insertion torque and pull-out force,21-23 a study from 2003 using more modern screw designs only found low and not significant correlations.24 More recent studies did not calculate correlations.4,5,10 No previous studies have examined the relationship of pull-out force and insertion torque to bone mineral density (BMD) and the influence of cement augmentation.
The purpose of this biomechanical study was to systematically evaluate the effect of cement injection technique for different screw types (solid or fenestrated) on the screw pull-out force by means of paired comparison in individual vertebrae. We further evaluated whether increasing the volume of high-viscosity cement from 1 mL to 3 mL was sufficient to improve the pull-out strength from osteoporotic vertebrae in three separated regions: upper thoracic, lower thoracic and lumbar spine. In addition, correlations of insertion torque, pull-out force and BMD were analysed for all groups.
Materials and Methods
Specimens
After approval of the study by the local ethical committee, 54 vertebrae (38 thoracic and 16 lumbar) were obtained from five adult human spines (two males and three females; age at the time of death: 87.2 years, standard deviation 4.2 ) that had been fixed in ethanol and glycerol as previously described.25 The BMD of each vertebra was determined with dual-energy X-ray absorptiometry (DEXA) (Lunar Prodigy, GE Healthcare Medical Systems, München, Germany), with two repeated observations by different observers (mean BMD, 0.7g/cm²). All vertebrae were sorted into three study groups, each having 18 vertebrae: (A) solid uncemented versus solid cemented; (B) solid uncemented versus fenestrated cemented; and (C) solid cemented versus fenestrated cemented, and randomisation was done according to the level (T6 to L5) and the BMD. This study design allowed a paired comparison of each treatment in individual vertebra to minimise bias from variations in anatomic (BMD and bone shape) and implant (screw length and diameter) factors, and the potential influence of the embalming process. A total of six vertebrae were excluded because of pre-existing osteoporotic damage to the endplates or the pedicles and these vertebrae were replaced by vertebrae from unused levels of the same spine, including T4 and T5. Each study group had the same number of left and right pedicles instrumented, with the two screw techniques compared. In addition, the injected cement volume was varied (1 mL and 3 mL) in an alternating order (T7, 1 mL; T8, 3 mL; T9, 1 mL; etc.) for each spine, resulting in an equal mean density for each cement volume group. These cement volumes were a reasonable minimal and maximal amount as suggested from previous studies.2,11
Specimen preparation
The spines were thawed overnight and kept moistened with saline solution during the entire testing period. All instrumentations were performed by the same experienced spine surgeon (CIL). Polyaxial solid and fenestrated pedicle screws (Expedium, DePuy Spine, Kirkel, Germany) were inserted with fluoroscopic guidance to ensure correct positioning. The insertion torque was recorded for each screw with an analogue torque sensor (Stahlwille Torsiometer 760/30, Wille GmbH, Wuppertal, Germany). The thread design and the pitch were the same for the screws in the uncemented and the cemented groups. A constant screw diameter (6.0 mm) was chosen for all levels, but the screw length (40 mm, 45 mm, or 50 mm) was adjusted according to the individual vertebral anatomy.
High-viscosity bone cement (Confidence System, DePuy Spine, Kirkel, Germany) was mixed as recommended by the manufacturer. The cement applicator was placed into the fenestrated pedicle screws, or the bone cavity for the solid cemented screws, and the predetermined amount of cement (1 mL or 3 mL) was injected. Plain radiographs and CT scans were performed to assess for correct screw position, proper cement distribution and cement leakage (Fig. 1). The cement was allowed to harden at room temperature for at least two hours before mechanical testing.
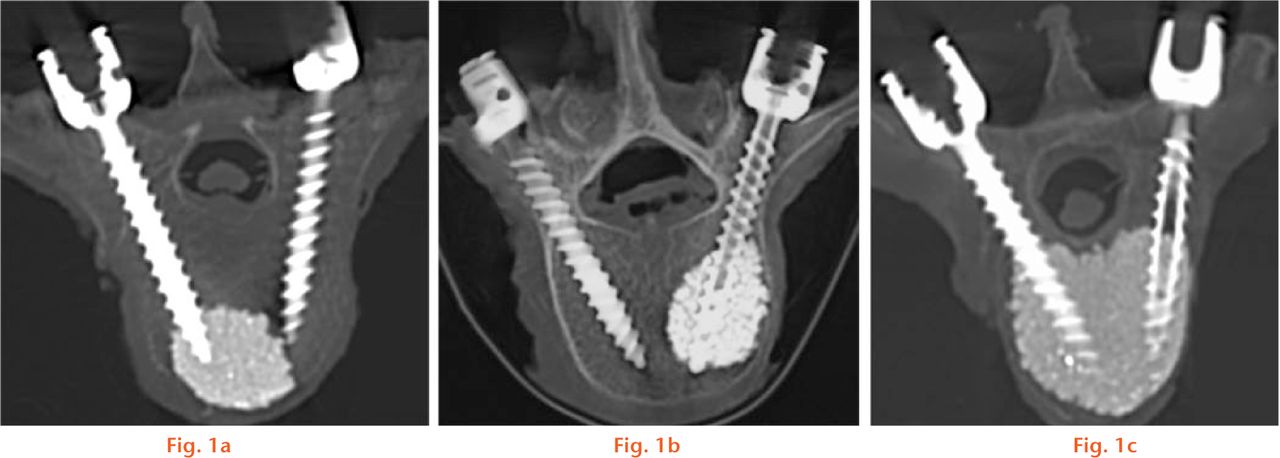
Fig.
CT scans after instrumentation and application of cement (3 mL); a) solid cemented screw (left), showing the far distal location of the cement cloud at the tip of the screw; b) fenestrated cemented screw (right), showing the cement cloud full around the screw, with good anchorage of the screw; and c) two cemented screws, showing the confluence of the cement clouds.
Mechanical testing
Mechanical pull-out testing along the longitudinal axis of the screw was performed to quantify the shear stability of the screw-bone interface. Each vertebra was separated, dissected from soft tissues and embedded in resin (Technovit Universal Fluid and Powder 2060, Heraeus Kulzer GmbH, Wehrheim, Germany). The embedding line of each vertebra was below the pedicle to avoid interference with mechanical testing. During embedding, the vertebral body was aligned with both screw symmetry axes parallel to the transverse plane. The angle (α) between the screw symmetry axis and the axis vertical to the embedding (transverse) plane was measured (Fig. 2).
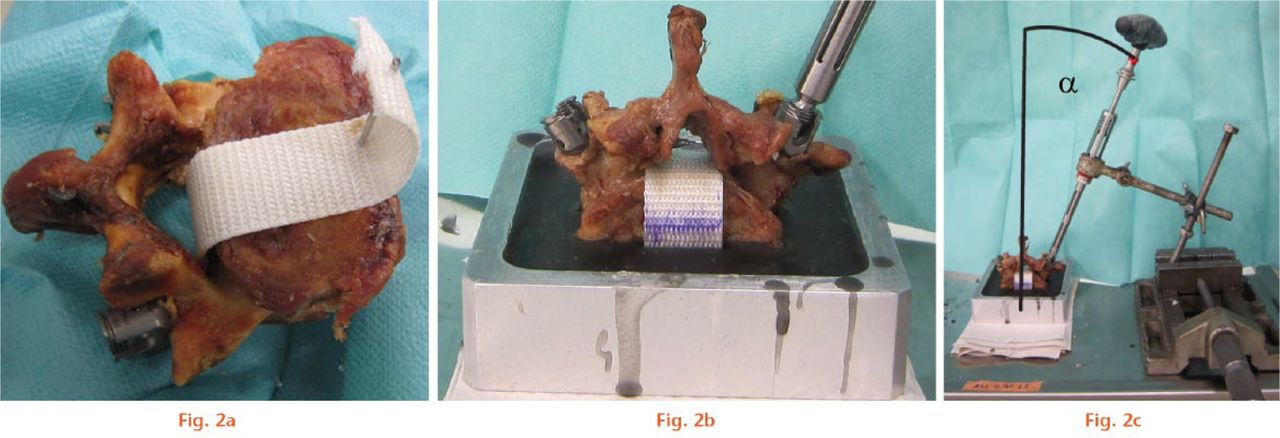
Fig.
Experimental arrangement for mechanical pull-out testing of pedicle screws; a) an inelastic band was wrapped around the vertebral body through the spinal canal and fixed with a Kirschner wire; b) the specimen was embedded in resin up to two thirds of the vertebral body anteroposterior diameter; c) the angle α (angle between the longitudinal screw axis and the vertical embedding axis) was measured in the transverse plane.
For mechanical testing, each screw was aligned parallel to the piston of a servohydraulic testing machine (MTS 858 Mini Bionix, Eden Prairie, Minnesota). A titanium rod attached to an adjustable cardan joint was connected to the pedicle screw using a grub screw to avoid additional forces or moments, and the cardan joint was locked to maintain constant pull-out direction defined by the premeasured angle (α) (Fig. 3). Pull-out testing was performed with the testing machine (25 kN load cell) in displacement controlled mode (10 mm/min and 10 Hz sample rate).

Fig. 3
Mechanical testing arrangement for an embedded vertebra: an adjustable hinge joint was used to align the screw axis parallel to the piston of the materials testing apparatus in the transverse plane at the previously measured angle (α). At the top, a titanium bar is shown connecting to an adjustable cardan joint that was fixed during testing.
For study groups A and B, the uncemented screw was always pulled out first to avoid damage to the vertebra which was more likely to occur on the cemented side. For study group C (both sides cemented), the first 25% force drop, after the peak load, was used as the stop criterion and then the contralateral side was tested before complete screw pull-out. After pull-out testing, an additional CT scan was performed to study the individual failure pattern of each screw.
Data analysis
During pull-out testing, the force-displacement curve was recorded and the maximum peak load (failure load) and the initial construct stiffness (slope of linear part of the curve) were determined. Data analysis was performed with statistical software (SPSS 19.0 for Windows, Armonk, New York). The normal distribution of the data was checked with the Shapiro-Wilk test. Within the three study groups, the failure loads were compared using the paired t-test. To examine the effect of cement volume, the data of all cemented screws were combined and then separated into lumbar, lower thoracic (T9 to T12) and upper thoracic (T4 to T8) regions. The Jonckheere-Terpstra test was performed for the resulting three groups (0 mL, 1 mL, and 3 mL) within the three regions (lumbar, lower and upper thoracic). Correlations between failure load, BMD, and insertion torque were analysed using Spearman’s rank correlation coefficient (ρ).
Results
The BMD was normally distributed and the mean BMD was similar for all study groups (Table I). The CT scans showed lateral or ventral cement leakage in 12 of 72 cemented screws (17%, eight solid and four fenestrated screws) and most frequently when 3 mL cement was used (eight of the 12 screws). There was no cement leakage into the spinal canal. Cement distribution was better around the fenestrated screws because the solid cemented screws showed cement clouding at the apex (Fig. 1).
Table I.
Effect of screw type and cement on pull-out testing of pedicle screws from human thoracic and lumbar vertebrae*
| Group | Treatment | Failure load (N) | Bone mineral density (g/cm²) | Insertion torque (Ncm) | Stiffness (N/mm) |
|---|---|---|---|---|---|
| A | Uncemented | 444 (356) | 0.70 (0.27) | 71.0 (42.7) | 266 (89) |
| Solid cemented | 904 (485) | 0.70 (0.27) | 81.3 (47.0) | 316 (128) | |
| p ⩽ | 0.001† | 0.247 | 0.050 | ||
| B | Uncemented | 611 (308) | 0.76 (0.25) | 88.7 (40.1) | 379 (91) |
| Fenestrated cemented | 1233 (546) | 0.76 (0.25) | 68.6 (33.5) | 388 (71) | |
| p ⩽ | 0.001† | 0.016† | 0.542 | ||
| C | Solid cemented | 1145 (643) | 0.68 (0.22) | 74.9 (33.3) | 285 (133) |
| Fenestrated cemented | 1070 (557) | 0.68 (0.22) | 79.5 (35.5) | 337 (122) | |
| p ⩽ | 0.509 | 0.165 | 0.276 |
-
*
data reported as mean (standard deviation). Results for different anatomic regions (thoracic and lumbar) and different cement volumes (1 mL and 3 mL) were combined
-
†
statistically significant (p < 0.05) using the paired t-test within the study group
The force-displacement curves during the pull-out experiments were usually linear at the beginning, with a distinct peak at the failure load and subsequent decreased force (Fig. 4). A total of three vertebrae of group B had to be excluded because of screw misalignment in one case and the contact of the uncemented screw to the cement cloud of the contralateral screw in two cases. The failure pattern of all uncemented screws was a straight axial pull-out of the screw without any fracture at the base of the pedicles. The cemented fenestrated screws had screw pull-out with the cement cloud adherent to the screw in 29 of 36 fenestrated screws, and the cement-bone interface was disrupted by a fracture of the pedicle. In the remaining seven screws, failure of the screw-cement interface was observed, with the cement cloud remaining in situ without breakage of the pedicle. The solid cemented screws had similar failure patterns to those of the fenestrated screws (solid cemented screws: pedicle fracture in 21 of 33 screws and failure of screw-cement interface in 12 of 33 screws).
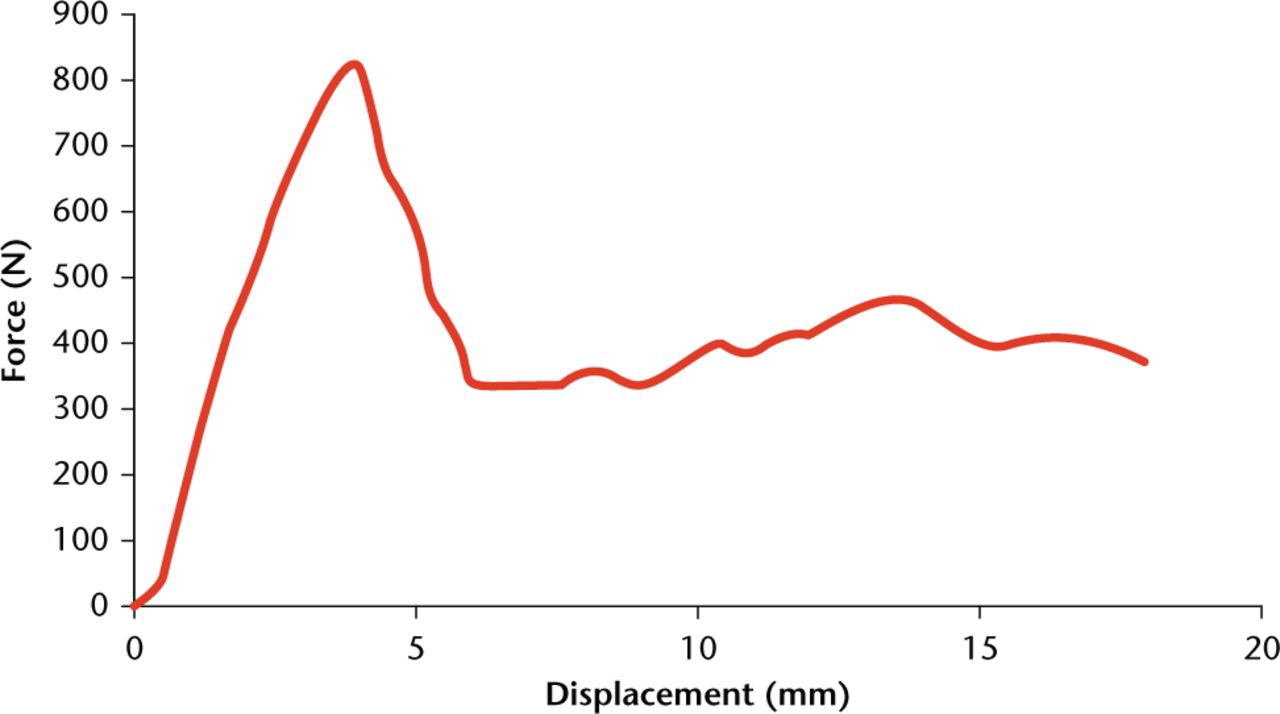
Fig. 4
Typical force-displacement curve from a screw pull-out experiment.
Mean failure load for the different screw constructs (data for groups combined) was greatest for fenestrated cemented and solid cemented screws (Table I). The differences between the paired failure loads for each vertebra were normally distributed. Mean failure load was significantly greater for solid cemented screws than uncemented screws (group A) and significantly greater for fenestrated cemented than uncemented screws (group B, Table I). There was no difference in mean failure load between solid cemented and fenestrated cemented screws (group C, Table I). There were no significant differences in mean insertion torque or stiffness between the different screw and cement constructs (Table I).
For the analysis of the effect of cement volume on failure load, the data were normally distributed in all subgroups except for the uncemented group in the lumbar region and the 1 mL cement group in the thoracic region (p < .01). In all tested regions, the upper thoracic, lower thoracic and lumbar spine, screws cemented with 3 mL cement had significantly greater mean failure load than either screws cemented with 1 mL or uncemented screws (Table II). In the lower thoracic region, but not in the upper thoracic or lumbar regions, mean failure load was significantly greater for screws cemented with 1 mL cement than for uncemented screws (Table II).
Table II.
Effect of cement volume on failure load in pull-out testing of pedicle screws in human thoracic and lumbar vertebrae§
| Region | Cement volume (mL) | Failure load (N) | p-value ⩽ |
|---|---|---|---|
| Upper thoracic | 0 | 470 (356) | — |
| 1 | 720 (386) | 0.129† | |
| 3 | 1434 (398) | 0.001‡* | |
| Lower thoracic | 0 | 532 (283) | — |
| 1 | 917 (533) | 0.025†* | |
| 3 | 1395 (502) | 0.037‡* | |
| Lumbar | 0 | 604 (397) | — |
| 1 | 719 (487) | 0.628† | |
| 3 | 1496 (499) | 0.004‡* |
-
§
data reported as mean (standard deviation)
-
†
comparison between screws cemented with 1 mL cement and uncemented screws;
-
*
statistically significant (p < 0.05) using the Jonckheere-Terpstra test
-
‡
comparison between screws cemented with 3 mL cement and 1 mL cement
Significant correlations were observed between failure load, insertion torque, and BMD (Table III). The failure load was highly correlated with insertion torque for uncemented screws, with decreasing values of the correlation coefficient for increasing cement volume (Table III and Fig. 5). A stronger correlation for the dependence of failure load and insertion torque on the BMD was observed for uncemented screws more than cemented screws (Table III).
Table III.
Correlation between parameters of pull-out tests for pedicle screws in human thoracic and lumbar vertebrae (Spearman’s rank correlation coefficient ρ, all values significant, p < 0.05)
| Cement volume (mL) | |||
|---|---|---|---|
| 0 | 1 | 3 | |
| Failure load/insertion torque | 0.91 | 0.71 | 0.46 |
| Failure load/bone mineral density | 0.70 | 0.45 | 0.55 |
| Insertion torque/bone mineral density | 0.71 | 0.58 | 0.41 |
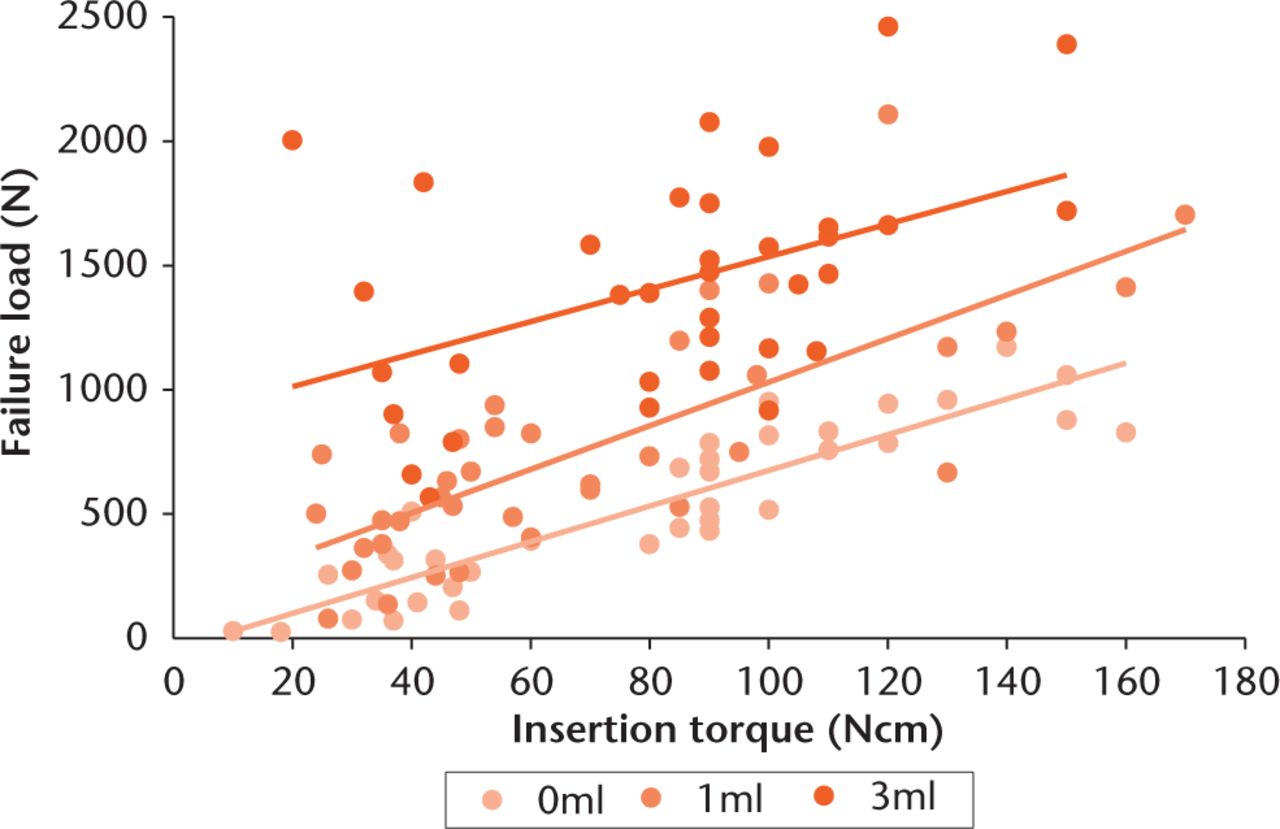
Fig. 5
Relationship between failure load and insertion torque for different cement volumes.
Discussion
The present results showed that mean failure load was significantly greater for cemented than for uncemented pedicle screws (Table I), but there was no significant difference in mean failure load between solid cemented and fenestrated cemented screws (Table I). The current study design had the advantage that each injection technique (fenestrated or solid screws) was studied against an uncemented control and in a combined paired study group, minimising potential bias from screw design or anatomical variations.
While the enhanced failure load of cemented compared with uncemented pedicle screws is well known, the effect of fenestration is still a topic of controversy. Chen et al19 and Chang et al10 found a significantly higher failure load for solid cemented pedicle screws compared with fenestrated cemented screws in their biomechanical studies on artificial, osteoporotic-like bone. In contrast, in their study on human osteoporotic thoracic and lumbar specimens, Choma et al4 found significantly higher pull-out forces for the partially fenestrated than for the solid cemented screws. In accordance with our study, Becker et al16 reported no significant difference between the solid and fenestrated cemented screws. These differing results might be partially explained by the different screw designs. A comparative study had shown that pull-out force increases with the number of output holes in the fenestrated screws,26 which could explain the poor results of the fenestrated screws in some studies10,19 where screws with only one10 or two19 holes were used. In contrast, Choma et al4 were using the same screw type as that in our study (nine holes), and Becker et al16 were testing screws with four holes. Another reason might be the different bone conditions. While Chen et al19 and Chang et al10 were using artificial bone, where the natural variations in BMD were missing and the comparability with human bone is questionable in general, Choma et al4 were using highly osteoporotic bone but without randomisation. Adaptation of the pull-out forces according to BMD was performed by Becker et al,16 while in our study the two screw types were tested in the two pedicles of the same human vertebrae using paired comparisons. Therefore, the two testing groups had exactly the same mean BMD, while its natural variations were still considered. Thus, if testing was carried out on human vertebrae and BMD was taken into account accordingly, as it was done in our study and by Becker et al,16 no significant difference in pull-out force would be found between the solid and fenestrated cemented screws.
One remaining concern of cemented screws is the risk for cement leakage into the spinal canal which is likely to occur with larger amounts of cement, especially in osteoporotic bone.16 Using high-viscosity cement as in the present study can possibly help to decrease cement leakage, but systematic approaches are required to identify the minimal amount of PMMA which still provides stability against screw migration and cut-out in osteoporotic bone. Varied amounts of cement have been suggested and studied.1,27 A previous study6 reported no significant difference in failure of pedicle screw fixation in osteoporotic bone between two different larger cement volumes (2.8 mL and > 5.5 mL). In other laboratory studies, it had been proposed and confirmed that optimal cement volume may be between 0.5 mL and 3 mL, and larger volumes may have no beneficial effect on stability.5,9 Therefore, in the present work, minimum (1 mL) and maximum (3 mL) amounts of cement within these suggested limits were used for both thoracic and lumbar levels.
We found a significant increase of the pull-out force with 3 mL cement compared with a smaller cement volume in all considered spine regions (Table II). As pull-out force was very similar in the three regions using 3 mL cement, it seems that cement is becoming the determining factor (compared with spine level or screw length, for example) when a sufficiently large volume is used. Pedicle screws augmented with 1 mL cement had significantly greater stability compared with uncemented screws in lower thoracic vertebrae. It was interesting to see that in the upper thoracic spine, 1 mL cement could distinctly increase pull-out force by 250 N, however, this increase was not statistically significant. This might be attributed to the overall smaller force level in this region while the variation is still comparably high and the number of specimens small, but certainly in the upper thoracic region, the sustainable loads are also smaller as a smaller part of the body weight has to be carried. Furthermore, from a clinical point of view, the application of 3 mL cement in the upper thoracic region has to be considered carefully, taking into account the individual anatomical conditions and the increased risk of cement leakage with higher cement volume. With respect to these results, the usage of at least 1 mL cement in the thoracic spine and 3 mL in the lumbar spine seem to be appropriate.
Cement leakage was more commonly observed with 3 mL cement than with 1 mL cement. As we only used high-viscosity cement, no direct comparison with low-viscosity cement concerning leakage could be made. However, Bullmann et al2 reported 65% of leakage (15 of 23 screws) in a similar biomechanical study using low-viscosity cement. In contrast, the 17% of leakage (12 of 72 screws) in our study using high-viscosity cement was relatively low, indicating possible advantages of high-viscosity cement. This is also in accordance with other studies, revealing that high-viscosity cement may potentially reduce the problem of cement leakage28 while providing comparable stability.4
The main advantage of fenestrated screws is that the cement can be injected directly through the screw after instrumentation, avoiding the removal of the screw before cement application which is commonly required with solid screws. Therefore, fenestrated screws may minimise operative time, especially for multiple level instrumentations and it may be possible to stop the cement application immediately after detection of cement leakage. The analysis of the post-operative CT scans showed that the fenestrated screws used in this study, with nine holes near the screw tip (three rows separated by 120°), provided an even distribution of the cement circumferentially around the screw and not predominantly at the screw tip in the anterior part of the vertebral body, as observed with some solid screws (Fig. 1).
The pull-out strength of the solid screws was greater when both sides of a vertebra were cemented (Table I). This effect appeared predominantly for vertebrae with cement volumes of 3 mL in which the cement clouds from both pedicle screws were merged into one cloud (Fig. 1c). As this could only occur in Group C, where the solid and fenestrated cemented screws were compared, it occurred just as often for both types of screws. However, it was interesting to see that for the fenestrated screws, the pull-out strength was similar with one side or both sides of the vertebra cemented (Table I). This could be attributed to the better cement distribution with fenestrated than with solid screws. Due to these results of either similar or increased pull-out forces, for clinical application, cement cloud merging is considered to be advantageous, as long as it is not connected to increased leakage, which was not the case in the current study.
In the current study, a particularly high correlation (r = 0.91) was found between failure load and insertion torque for the uncemented screws. This result is in accordance with many previous studies.21-23 However, Inceoglu, Ferrara and Mclain24 reported contrary results. Perhaps this could be attributed to the fact that, in that study, the screw holes were tapped before screw insertion. Another possible reason might be the different screw designs, which have been shown to have a large influence.29 The screws used in our study have a design which is frequently used (Expedium, DePuy). With this design, the insertion torque gives a good prediction for the pull-out force and therefore the stability of the pedicle screw. Although this good correlation decreased with the amount of cement used for augmentation, there remained considerable correlation (r = 0.46) even when 3 mL of cement was injected. We could also demonstrate high correlation between insertion torque and BMD, as well as pull-out force and BMD (r = 0.7), which might partly explain the high correlation between insertion torque and pull-out force, as both are strongly influenced by BMD. Therefore, according to our study, BMD and insertion torque may be good predictors of screw stability.
The limitations of the present study include the use of bone specimens that were embalmed which could have changed the mechanical properties of bone, e.g. absolute pull-out strength. However, this would not be expected to affect the relative comparison of the two implantation techniques during paired comparison in individual vertebrae. Furthermore, as the fixation of human tissue using ethanol and glycerol is a technique designed only to conserve tissue and does not influence the morphology and macroscopic anatomy of the bone, the impact on cement distribution should be marginal. This was also proved by the post-operational CT scans (Fig. 1) which showed similar cement distributions to those in the patients. The present results are in agreement with the results of other laboratory studies, so the present bone model may be comparable with fresh frozen bone in mechanical behaviour. Another limitation might be the use of a constant screw diameter because the screw diameter might have a larger effect on the uncemented than the cemented screws, introducing an unwanted bias. This was done to reduce the number of differing variables, as has been done in many similar studies.3,4,7,16 To clarify the specific influence of the screw diameter and the potential bias regarding cementation, further studies are needed.
In conclusion, the present study demonstrated that conventional, solid pedicle screws augmented with high-viscosity cement provided results comparable to those using sophisticated and considerably more expensive fenestrated screws with respect to stability in pull-out tests in osteoporotic bone. The data suggest that 1 mL cement may provide adequate stability for thoracic vertebrae, especially in the lower thoracic spine, while 3 mL leads to further significant improvement in all considered spine regions. Therefore, we recommend the use of at least 1 mL in the thoracic and 3 mL in the lumbar spine. Furthermore, the results of our biomechanical in vitro study propose that pre-operatively determined BMD and intra-operatively measured insertion torque might be good predictors of screw stability, particularly in uncemented screws.
Funding Statement
We acknowledge support by Deutsche Forschungsgemeinschaft and Open Access Publishing Fund of University of Tübingen.
Funding has been received from the author’s institution from DePuy Spine which is related to this article (provision of implants and cement).
T. Shiozawa has received funding from Zimmer Biomet and Storz GmbH & Co which is not related to this article.
ICMJE conflict of interest
None declared
References
1 Bullmann V , LiljenqvistUR, RodlR, et al.. Pedicle screw augmentation from a biomechanical perspective.Orthopäde2010;39:673-678. Google Scholar
2 Bullmann V , SchmoelzW, RichterM, et al.. Revision of cannulated and perforated cement-augmented pedicle screws: a biomechanical study in human cadavers. Spine (Phila Pa 1976)2010;35:932-939.CrossrefPubMed Google Scholar
3 Burval DJ , McLainRF, MilksR, et al.. Primary pedicle screw augmentation in osteoporotic lumbar vertebrae: biomechanical analysis of pedicle fixation strength. Spine (Phila Pa 1976)2007;32:1077-1083.CrossrefPubMed Google Scholar
4 Choma TJ , PfeifferFM, SwopeRW, et al.. Pedicle screw design and cement augmentation in osteoporotic vertebrae: effects of fenestrations and cement viscosity on fixation and extraction. Spine (Phila Pa 1976)2012;37:1628-1632.CrossrefPubMed Google Scholar
5 Derincek A , WuC, MehbodA, et al.. Biomechanical comparison of anatomic trajectory pedicle screw versus injectable calcium sulfate graft-augmented pedicle screw for salvage in cadaveric thoracic bone. J Spinal Disord Tech2006;19:286-291.CrossrefPubMed Google Scholar
6 Frankel BM , D’AgostinoS, WangC. A biomechanical cadaveric analysis of polymethylmethacrylate-augmented pedicle screw fixation. J Neurosurg Spine2007;7:47-53.CrossrefPubMed Google Scholar
7 Gao M , LeiW, WuZ, LiuD, ShiL. Biomechanical evaluation of fixation strength of conventional and expansive pedicle screws with or without calcium based cement augmentation. Clin Biomech (Bristol, Avon)2011;26:238-244.CrossrefPubMed Google Scholar
8 Amendola L , GasbarriniA, FoscoM, et al.. Fenestrated pedicle screws for cement-augmented purchase in patients with bone softening: a review of 21 cases. J Orthop Traumatol2011;12:193-199.CrossrefPubMed Google Scholar
9 Aydogan M , OzturkC, KaratoprakO, et al.. The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. J Spinal Disord Tech2009;22:444-447.CrossrefPubMed Google Scholar
10 Chang MC , KaoHC, YingSH, et al.. Polymethylmethacrylate augmentation of cannulated pedicle screws for fixation in osteoporotic spines and comparison of its clinical results and biomechanical characteristics with the needle injection method. J Spinal Disord Tech2013;26:305-315.CrossrefPubMed Google Scholar
11 Chang MC , LiuCL, ChenTH. Polymethylmethacrylate augmentation of pedicle screw for osteoporotic spinal surgery: a novel technique. Spine (Phila Pa 1976)2008;33:317-324.CrossrefPubMed Google Scholar
12 Moon BJ , ChoBY, ChoiEY, et al.. Polymethylmethacrylate-augmented screw fixation for stabilization of the osteoporotic spine : a three-year follow-up of 37 patients. J Korean Neurosurg Soc2009;46:305-311.CrossrefPubMed Google Scholar
13 Pinera AR , DuranC, LopezB, et al.. Instrumented lumbar arthrodesis in elderly patients: prospective study using cannulated cemented pedicle screw instrumentation. Eur Spine J2011;20:408–414.CrossrefPubMed Google Scholar
14 Hu MH , WuHT, ChangMC, et al.. Polymethylmethacrylate augmentation of the pedicle screw: the cement distribution in the vertebral body. Eur Spine J2011;20:1281-1288.CrossrefPubMed Google Scholar
15 Kerry G , RuedingerC, SteinerHH. Cement embolism into the venous system after pedicle screw fixation: case report, literature review, and prevention tips. Orthop Rev (Pavia)2013;5:24.CrossrefPubMed Google Scholar
16 Becker S , ChavanneA, SpitalerR, et al.. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J2008;17:1462-1469.CrossrefPubMed Google Scholar
17 Choma TJ , FrevertWF, CarsonWL, et al.. Biomechanical analysis of pedicle screws in osteoporotic bone with bioactive cement augmentation using simulated in vivo multicomponent loading. Spine (Phila Pa 1976)2011;36:454-462.CrossrefPubMed Google Scholar
18 Wittenberg RH , LeeKS, SheaM, WhiteAA3rd, HayesWC. Effect of screw diameter, insertion technique, and bone cement augmentation of pedicular screw fixation strength. Clin Orthop Relat Res1993;296:278-287.PubMed Google Scholar
19 Chen LH , TaiCL, LeeDM, et al.. Pullout strength of pedicle screws with cement augmentation in severe osteoporosis: a comparative study between cannulated screws with cement injection and solid screws with cement pre-filling. BMC Musculoskelet Disord2011;12:33.CrossrefPubMed Google Scholar
20 Pare PE , ChappuisJL, RampersaudR, et al.. Biomechanical evaluation of a novel fenestrated pedicle screw augmented with bone cement in osteoporotic spines. Spine (Phila Pa 1976)2011;36:1210-1214.CrossrefPubMed Google Scholar
21 Daftari TK , HortonWC, HuttonWC. Correlations between screw hole preparation, torque of insertion, and pullout strength for spinal screws. J Spinal Disord1994;7:139-145.CrossrefPubMed Google Scholar
22 Okuyama K , SatoK, AbeE, et al.. Stability of transpedicle screwing for the osteoporotic spine. An in vitro study of the mechanical stability. Spine (Phila Pa 1976)1993;18:2240-2245.CrossrefPubMed Google Scholar
23 Yerby SA , TohE, McLainRF. Revision of failed pedicle screws using hydroxyapatite cement. A biomechanical analysis. Spine (Phila Pa 1976)1998;23:1657-1661.CrossrefPubMed Google Scholar
24 Inceoglu S , FerraraL, McLainRF. Pedicle screw fixation strength: pullout versus insertional torque. Spine J2004;4:513-518.CrossrefPubMed Google Scholar
25 Shiozawa T , HuebnerM, HirtB, et al.. Nerve-preserving sacrocolpopexy: anatomical study and surgical approach. Eur J Obstet Gynecol Reprod Biol2010;152:103-107.CrossrefPubMed Google Scholar
26 Chen L-H , TaiC-L, LaiP-L, et al.. Pullout strength for cannulated pedicle screws with bone cement augmentation in severely osteoporotic bone: influences of radial hole and pilot hole tapping. Clin Biomech (Bristol, Avon)2009;24:613-618.CrossrefPubMed Google Scholar
27 Blattert TR , GlasmacherS, RiesnerHJ, et al.. Revision characteristics of cement-augmented, cannulated-fenestrated pedicle screws in the osteoporotic vertebral body: a biomechanical in vitro investigation. Technical note. J Neurosurg Spine2009;11:23-27.CrossrefPubMed Google Scholar
28 Baroud G , CrookshankM, BohnerM. High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine (Phila Pa 1976)2006;31:2562-2568.CrossrefPubMed Google Scholar
29 Kwok AW , FinkelsteinJA, WoodsideT, et al.. Insertional torque and pull-out strengths of conical and cylindrical pedicle screws in cadaveric bone. Spine (Phila Pa 1976)1996;21:2429-2433.CrossrefPubMed Google Scholar










