Abstract
Objectives
Deep bone and joint infections (DBJI) are directly intertwined with health, demographic change towards an elderly population, and wellbeing.
The elderly human population is more prone to acquire infections, and the consequences such as pain, reduced quality of life, morbidity, absence from work and premature retirement due to disability place significant burdens on already strained healthcare systems and societal budgets.
DBJIs are less responsive to systemic antibiotics because of poor vascular perfusion in necrotic bone, large bone defects and persistent biofilm-based infection. Emerging bacterial resistance poses a major threat and new innovative treatment modalities are urgently needed to curb its current trajectory.
Materials and Methods
We present a new biphasic ceramic bone substitute consisting of hydroxyapatite and calcium sulphate for local antibiotic delivery in combination with bone regeneration. Gentamicin release was measured in four setups: 1) in vitro elution in Ringer’s solution; 2) local elution in patients treated for trochanteric hip fractures or uncemented hip revisions; 3) local elution in patients treated with a bone tumour resection; and 4) local elution in patients treated surgically for chronic corticomedullary osteomyelitis.
Results
The release pattern in vitro was comparable with the obtained release in the patient studies. No recurrence was detected in the osteomyelitis group at latest follow-up (minimum 1.5 years).
Conclusions
This new biphasic bone substitute containing antibiotics provides safe prevention of bone infections in a range of clinical situations. The in vitro test method predicts the in vivo performance and makes it a reliable tool in the development of future antibiotic-eluting bone-regenerating materials.
Cite this article: M. Stravinskas, P. Horstmann, J. Ferguson, W. Hettwer, M. Nilsson, S. Tarasevicius, M. M. Petersen, M. A. McNally, L. Lidgren. Pharmacokinetics of gentamicin eluted from a regenerating bone graft substitute: In vitro and clinical release studies. Bone Joint Res 2016;5:427–435. DOI: 10.1302/2046-3758.59.BJR-2016-0108.R1.
Article focus
-
To investigate a new commercially available bone substitute that elutes antibiotics, with an initial high local release and a sustainable antibiotic level to effectively prevent recurrence of infection.
-
To compare the elution of gentamicin from a synthetic bone substitute in vitro with elution and efficacy in clinical applications.
Key messages
-
The in vitro antibiotic elution test method presented in this study predicts the local antibiotic elution in vivo and makes it a reliable tool in the research and development of future antibiotic-eluting bone-regenerating materials.
-
Local elution of antibiotics from a regenerating bone substitute effectively prevents recurrence of infection and supports bone healing.
Strengths and limitations
-
Strengths: This study compares in vitro data with in vivo performance in three different clinical settings.
-
Limitations: The local concentration of gentamicin was not measured in the osteomyelitis patients, and the detection limit of the equipment measuring the gentamicin concentrations in the drainage, serum and urine of studied patients prevented measurements of concentrations below 0.2 mg/L.
Introduction
Local delivery of antibiotics has been shown to be successful in treating active infections1-3 as well as for prophylactic use.4 Many different carriers have been used with different results5 and the ideal delivery material is yet to be found.
The first local antibacterial treatments were performed by Joseph Lister and published in The Lancet in 1867.6 Lister used carbolic acid and other local antiseptics in open fracture treatments, in addition to aseptic covering, thereby significantly decreasing the morbidity caused by infection.
Deep bone and joint infections (DBJI) still constitute a significant and costly societal burden globally. Whether caused by trauma, tumour surgery or joint replacement, DBJIs may require repeated invasive revision surgery and extensive systemic antimicrobial treatment that can last for years. In addition to potentially serious side effects, aggressive long-term systemic antibiotic treatments contribute to emerging bacterial resistance. Although major advances in aseptic and antiseptic routines have been achieved, approximately 30% of open fractures and 5% of closed fractures treated with fixation devices still become infected.5,7
The ongoing demographic changes in an ageing world have an impact on health care with 2.5 million artificial joints being inserted yearly.8,9 The most feared early complication is deep prosthetic joint infection, which occurs in 1% to 2% of patients who undergo joint replacement.10 As the typical patient tends to be an older individual with substantial comorbidity, an infection often results in prolonged and repeated surgeries, secondary complications, chronic morbidity, and even mortality related to the systemic antibiotic treatment and immobilisation.10,11 This patient group is especially susceptible to highly contagious and potentially life-threatening Clostridium difficile enteritis caused by long-term systemic treatment using the few remaining effective antibiotics. Clostridium enteritis, the leading cause of hospital-acquired diarrhoea, has a mortality rate ranging from 60% to 83%, and 40 000 deaths are reported yearly in the US alone.12
From a cost perspective, the increased direct cost for a patient with a prosthetic joint infection is five to seven times higher than for a primary procedure, corresponding to an additional € 40 000 per patient.13 Substantial suffering could be prevented and resources saved if more efficient treatment and prevention existed.
Local antibiotic delivery is an attractive option if it can be shown that it can be delivered safely with no systemic adverse effects. It may act synergistically with systemic antimicrobial therapy and may be better able to perfuse poorly vascularised bone in chronic osteomyelitis. Carriers for local antibiotic treatment currently or previously in use may be divided into six categories: non-biodegradable polymers; bone grafts; bone graft substitutes; collagen; gels; and aqueous solutions. Non-biodegradable carriers are mainly represented by polymethyl methacrylate (PMMA), usually in the form of blocks or beads. The antibiotic release from PMMA occurs from the surface by diffusion, and is therefore controlled by the surface area and the concentration gradient between the material surface and the surrounding tissue.14 This results in a high local level of antibiotics for the first one to three days post-operatively, followed by a sustained slow release that steadily decreases over weeks.15 Elution has been reported up to five years after PMMA bead implantation.16,17 The long elution time of low levels of antibiotics is a major disadvantage, as it may cause bacterial resistance when the antibiotic release falls below therapeutic levels. At this point, the PMMA will act as a foreign body and will be a source of recurrent infection due to colonisation of the surface and biofilm formation.17,18
A biodegradable carrier such as a bone graft substitute, collagen or a gel would theoretically decrease the risk of recurrence of infection and generation of resistance since it resorbs quickly and completely and all the antibiotic is released.5 However, the release from this group of carriers has repeatedly been reported as very fast and at a relatively uncontrolled rate.19
Morselised bone grafts, with the addition of antibiotics in powder form or soaked in an antibiotic solution,20 have been used as local antibiotic carriers since 1984.19 Good results have been achieved21-25 with up to a 90% success rate in hip revisions,22 and healing in infected nonunions within four to five months.23 The drawback presented with autograft is that it needs additional surgery to collect the graft. Allograft often presents a large variability in bone quality, and the antibiotic loading and dosing varies with loading technique and the antibiotic used.
Injections of aqueous solutions as a carrier for antibiotics may be effective in treatment of areas close to articulations26 but the sustained antibiotic level is poor, making it inefficient in any application other than as prophylaxis of surgical site infections.5
There is a great need for better, more efficient and more predictable delivery systems for successful local antibiotic delivery, especially in view of the emerging development of bacterial resistance worldwide. The main aim of this study was to investigate a new commercially available bone substitute that elutes antibiotics, combining an initial high local release with a sustainable antibiotic level for a sufficiently long time to effectively prevent infection (CERAMENT G, BONESUPPORT AB, Lund, Sweden). The product was developed by adding antibiotics to a clinically well documented bone-regenerating biphasic ceramic bone graft substitute.27-30 It is hypothesised that adequate antibiotic release may be achieved, as well as new bone ingrowth, to manage the dead space created during bone debridement. The gentamicin will prevent colonisation of gentamicin-sensitive organisms in order to protect bone healing.
The second aim with this study was to compare the in vitro and the in vivo elution rate to identify a test method that is able to predict the local antibiotic release pattern in vivo and thereby make the development of new antibiotic delivery systems more effective in the future.
Materials and Methods
Gentamicin release was measured from a synthetic bone graft substitute (CERAMENT G) consisting of 40 wt% hydroxyapatite particles in a calcium sulphate matrix. The bone graft substitute contained 175 mg gentamicin per 10 mL.
Gentamicin release was measured in four setups: in vitro elution in Ringer’s solution; local elution in patients treated for trochanteric hip fractures or uncemented hip revisions; local elution in patients treated with a bone tumour resection; and local elution in patients treated surgically for chronic corticomedullary osteomyelitis.
Each study was approved by the local independent ethics committee and informed consent was obtained from all patients.
In vitro elution in Ringer’s solution
For elution in Ringer’s solution, the material was studied either as paste or as pre-set beads with high or low surface areas,31 >100 cm2 and 24 cm2, respectively. The material was prepared according to the instructions for use, each sample consisting of 10 mL material. The samples were prepared in triplicate and immersed in 200 mL polypropylene beakers with 50 mL Ringer’s solution. The pre-set beads were allowed to cure before immersion, while the paste hardened in the solution. The samples were kept at 37 °C in an incubator.
The amount of Ringer’s solution used (50 mL) was calculated from the assumption that in an in vivo condition the minimal inhibitory concentration (MIC) levels for pseudomonas and other gentamicin-sensitive micro-organisms (4 mg/L)32 should be reached in all of the tissue surrounding the device up to a distance of approximately 1 cm (see Fig. 1). It should be noted that therapeutically much higher concentrations are needed to reach bactericidal effect, e.g. four to eight times the MIC.33
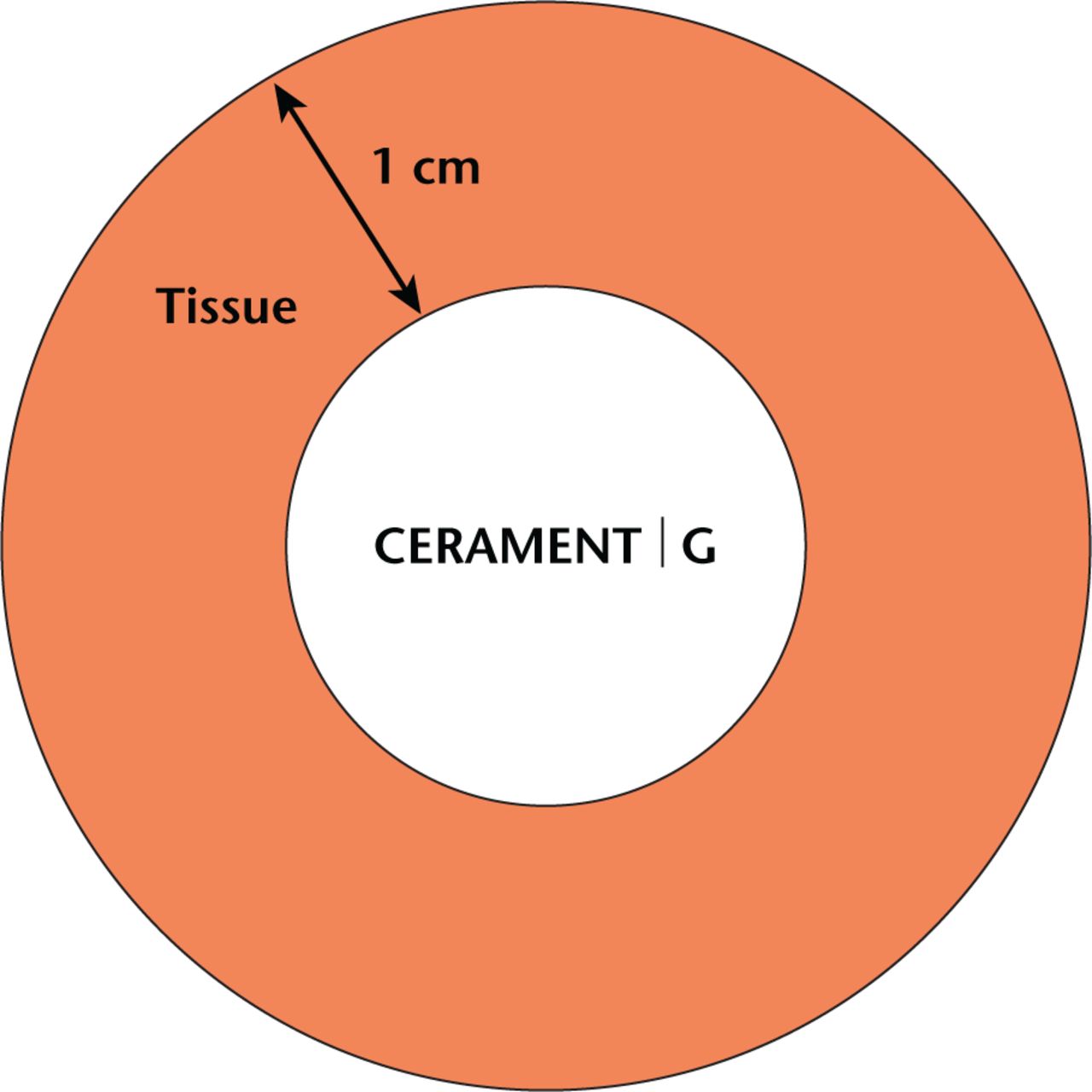
Fig. 1
Illustration of the local release model used for the in vitro release test. In an in vivo condition the minimal inhibitory concentration levels for gentamicin-sensitive microorganisms should be reached in all the tissue surrounding the device up to a distance of approximately 1 cm. Since the volume of the implant is 10 mL, the surrounding volume of a distance up to 1.09 cm is approximately 50 mL.
Since the volume of the implant is 10 mL, the surrounding volume of a distance up to 1.09 cm is approximately 50 mL according to Vsurrounding = Vtotal – Vimplant = 4/3 * π(1.34 + 1.09)3 – 10 = 60 -10 = 50 mL.
Samples were taken every 24 hours ± 2 for eight days, then once a week for four weeks. Samples of 10 mL (or 20%) of the solution were exchanged for fresh Ringer’s solution in order to simulate the situation in vivo where both a liquid/tissue flow and diffusion of gentamicin from the tissue surrounding the implant will take place. The gentamicin concentration in the samples was analysed by cloned enzyme donor immunoassay (CEDIA) on Roche Cobas, C501 (Roche Diagnostics, Risch-Rotkreuz, Switzerland).
Before the weekly collections, there was an exchange of the solution according to:
where n is the number of times the liquid should have been replaced if it was still replaced daily. Thereafter, the sample outtake and replacement were made as before (10 mL).
The pH of the liquid surrounding the CERAMENT G samples was measured using a pH meter (inoLab pH Level 2P, WTW GmbH, Weilheim, Germany) at each sampling occasion to ensure a stable and physiological pH value needed to maintain the activity of the pH-sensitive gentamicin.34-37
Local elution in patients treated for trochanteric hip fractures or uncemented hip revisions
A total of 11 patients underwent bone augmentation with CERAMENT G during the surgical management of a trochanteric fracture with internal fixation (six patients) and uncemented hip revision (five patients).The aim was to prevent infections, and the hypothesis was that the local concentration of gentamicin would reach bactericidal level, while the systemic concentration would be kept below toxic levels.
The 11 patients (two men, nine women) with a mean age of 75 years, (62 to 90; standard deviation (sd) 10) underwent the surgery. A mean of 7.3 mL of CERAMENT G was implanted (5 to 9; sd 1.1). A rigorous analysis of the antibiotic release followed: intra-articular drainage, from passive, open drain procedure placed close to the surgical site, was assessed at six, 12, 24, 30 and 36 hours post-operatively; urine was collected daily during the hospital stay (seven days); and blood serum assessed every hour for the first six hours post-operatively and every six hours (sd 1) thereafter, up to 96 hours post-operatively (21 samples per patient in total).
The total volume of the drainage was measured for each time point. A maximum of 10 mL drainage was collected for each sample and centrifuged for ten minutes at 2200 × g or 4000 rpm at room temperature. The supernatant was then separated from the rest and deep frozen at -80°C prior to analysis.
The urine was sampled daily from a urinary catheter for the first four days and thereafter morning urine was collected. The samples were homogenised, transferred into two 50 mL tubes and kept cool in a refrigerator.
A minimum of 4 mL of blood was withdrawn at each time point and placed in a 5 mL heparin tube. Blood samples were centrifuged for ten minutes at 2200 × g and the supernatant was transferred to two 5 mL polypropylene tubes and deep frozen at -80°C until analysis.
None of the patients were prescribed systemic gentamicin during the study period. Gentamicin concentrations were analysed using a validated antibody technique (QMS Gentamicin Assay, Indiko Thermo Scientific, Thermo Fisher Scientific, Waltham, Massachusetts).
Local elution in patients treated with a bone tumour resection
A total of eight patients (five men, three women) with a mean age of 54 years (37 to 79; sd 14) underwent bone defect reconstruction with the use of a temporary drain. A mean of 12.1 mL of CERAMENT G was implanted (4 to 20; sd 5.5) and both drainage and blood serum were collected daily until two days post-operatively. Indications for surgery were metastatic bone disease (n = 3, proximal humerus), giant cell tumour (n = 2, distal femur) and chondroid tumour (n = 3, distal femur, proximal femur, pelvis). Additional endoprosthetic reconstruction with a tumour prosthesis was performed in two patients (two proximal humerus). Drainage and blood were collected immediately post-operatively and on each post-operative day until the drain was removed. In two cases it was not possible to collect drainage directly post-operatively due to minimal fluid production. None of the patients were prescribed systemic gentamicin during the study period. Gentamicin concentrations were analysed using a validated antibody technique (QMS Gentamicin Assay, Indiko Thermo Scientific).
Local elution in patients treated surgically for chronic corticomedullary osteomyelitis
A total of 13 patients (seven men, six women) with a mean age of 47 years (2 to 65; sd 12) with Cierny-Mader stage III and IV chronic osteomyelitis38 were treated by resecting the affected areas and filling the dead space with a mean of 10.6 mL of CERAMENT G (2 to 20; sd 6). Blood serum was collected on the morning after surgery, on day two and on day five post-operatively. All operations were performed by two surgeons. At the time of osteomyelitis excision surgery, tissue samples were collected and cultured to identify the causative bacteria. None of the patients were prescribed systemic gentamicin during the study period.
Results
In vitro elution in Ringer’s solution
In the elution study in vitro, there was a high initial peak in the gentamicin concentration for all the samples, with a maintained level above 4 mg/L during the whole test period of 28 days, which is the MIC breakpoint for most gentamicin-sensitive microorganisms (Figs 2a and 2b). The maximum gentamicin concentration for pre-set beads with high surface area was (mean and sd 2879 mg/L; sd 105) obtained on the first day (Fig. 2a). For the pre-set beads with low surface area and for the paste, the maximum gentamicin concentration was 2420 mg/L (sd 45) and 2354 mg/L (sd 100), respectively, obtained on the second day (Fig. 2a). The gentamicin concentrations at day 28 were 43 mg/L; sd 8 for the high surface samples, 43 mg/L; sd 11 for the low surface samples and 65 mg/L; sd 8 for the paste (Fig. 2b). All gentamicin was released during the test period and more than 95% had been released after two to four days independently of the surface area of the material, or whether it was pre-set or paste.
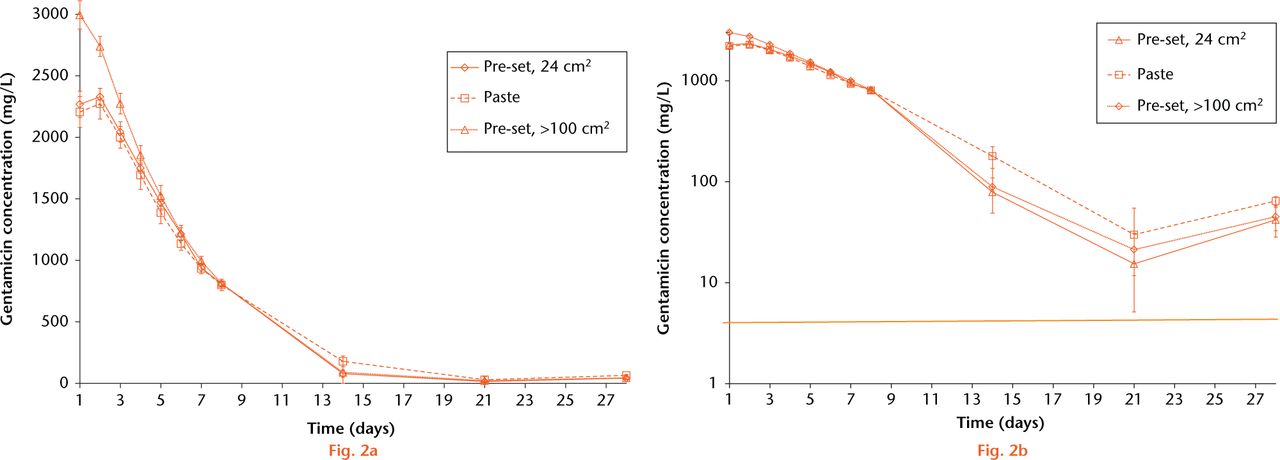
Fig. 2
Graphs showing a) gentamicin concentration over time in Ringer’s solution, no difference was observed between pre-set beads with high and low surface area and paste; and b) on log scale over time: same results as in Fig 2a, clearly showing levels over 4 mg/L, which is the minimal inhibitory concentration break point for most gentamicin-sensitive microorganisms. Line = mean values.
The pH in the liquid surrounding the samples was a mean of 7.00 (sd 0.13) during the 28 days of measurements, assuring good activity and predictability of the gentamicin against Staphylococcus aureus, Escherichia coli and Salmonella entericae.34-37
Local elution in patients treated for trochanteric hip fractures, uncemented hip revisions and after bone tumour resection
In the clinical studies similar results were found, with high initial levels of gentamicin detected in the drainage, followed by a decreasing concentration (Fig. 3). Gentamicin was detected in the serum in most patients during the first post-operative days, although always well below the maximum recommended systemic level of 10 mg/L (Fig. 4). It was even less than 2 mg/L, to which the serum concentration should decline between doses to avoid toxicity during systemic administration. Gentamicin concentrations in both drainage and serum were higher in the bone tumour patients, which probably reflects the larger volume of CERAMENT G used. Gentamicin was detected in urine during the first post-operative week (Fig. 5).
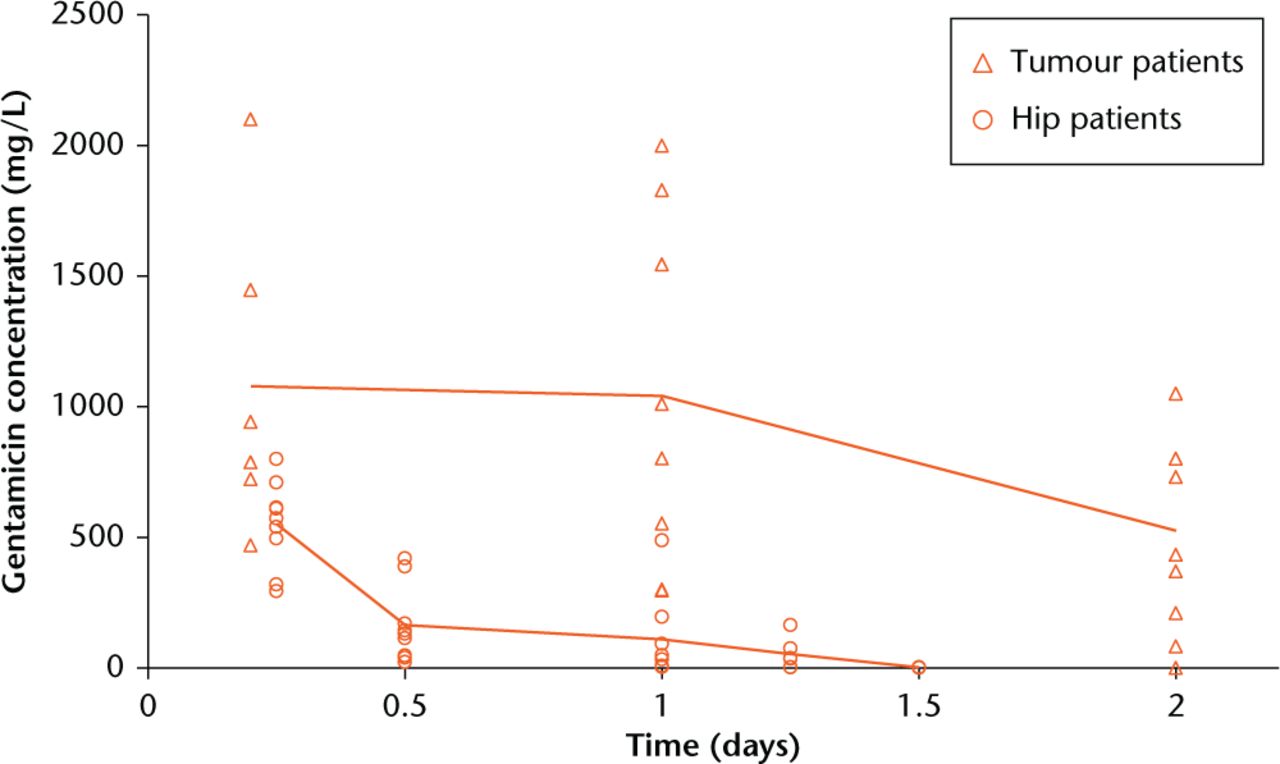
Fig. 3
Graph showing gentamicing concentrations in wound drainage from patients undergoing tumour surgery or hip surgery. High initial local concentrations of gentamicin were observed (100 times minimal inhibitory concentration (MIC) at six hours and still ten times the MIC at 30 hours), with a rapid decrease during the following days. Line = mean values.
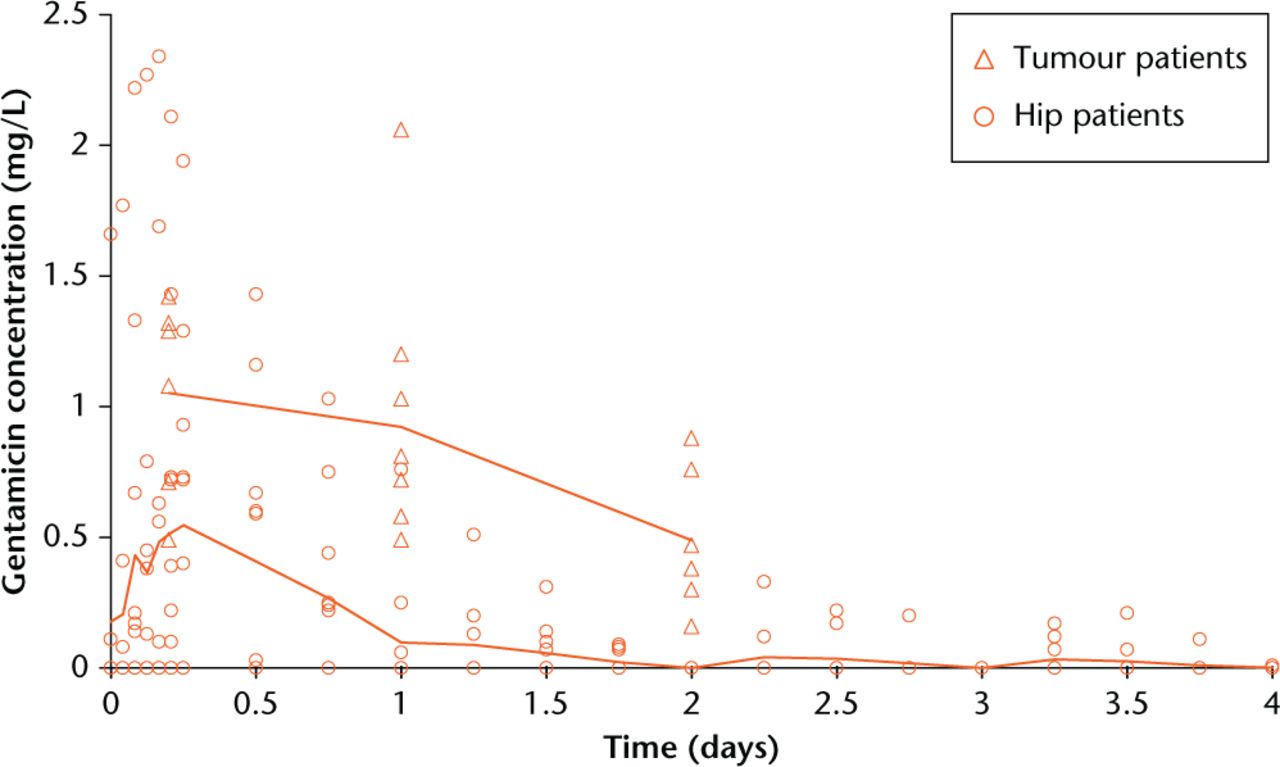
Fig. 4
Graph showing detectable levels of gentamicin in serum from tumour and hip patients for the first two days post-operatively. The local levels of gentamicin are generally 1000 times higher than systemic levels. Line = mean values.
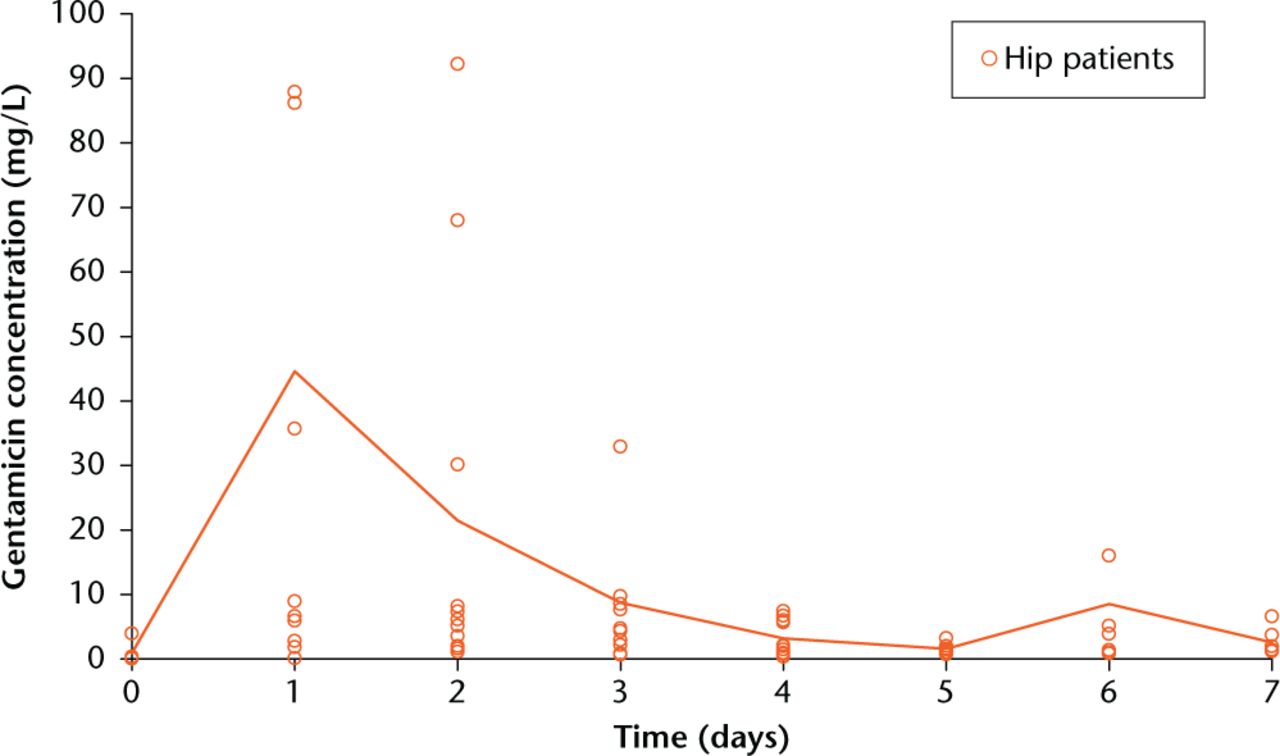
Fig. 5
Graph showing detectable gentamicin concentrations in urine from hip surgery patients for seven days post-operatively. These levels are about ten times higher than the systemic concentrations measured in serum, indicating bactericidal local levels in the region of surgery. Line = mean values.
Local elution in patients treated surgically for chronic corticomedullary osteomyelitis
The gentamicin levels in the serum of the patients treated for chronic osteomyelitis were low. In all, eight of the 13 patients had gentamicin concentrations of less than 0.2 mg/L on the day after surgery and the levels were maintained over the first five days post-operatively or for as long as samples were collected. The other five patients had slightly higher gentamicin concentrations in the serum the day after operation, at a mean of 0.54 mg/L (sd 0.43), however, thereafter the levels were as low as for the rest of the patient group. No patient had levels which would be associated with any systemic toxicity.
A breakdown of the organisms cultured at the time of osteomyelitis excision surgery is outlined in Table I. There were four cases with no growth, probably due to long-term antibiotic treatment and multiple recurrences of the osteomyelitis. Of the remaining nine cases with positive cultures, eight were monomicrobial and the final was polymicrobial. Five cases cultured gentamicin-sensitive organisms, as defined by the European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoints for resistance.
Table I.
The cultures of osteomyelitis causative bacteria showed four cases with no growth, eight cases were monomicrobial and one case was polymicrobial. Five cases cultured gentamicin-sensitive organisms and four cases demonstrated some degree of gentamicin resistance
| Organism | Patients (n) | Gentamicin resistance |
|---|---|---|
| No growth | 4 | |
| Staphylococcus aureus | 2 | Sensitive |
| Methicillin-resistant staphylococcus aureus | 1 | Resistant |
| Streptococcus agalactiae | 1 | Resistant |
| Enterobacter cloacae | 1 | Sensitive |
| Salmonella enteritidis | 1 | Intermediate |
| Clostridium difficile | 1 | Resistant |
| Corynebacterium spp. | 1 | Sensitive |
| Mixed Growth (Staphylococcus aureus and Enterobacter cloacae) | 1 | Sensitive |
The remaining four cases demonstrated some degree of gentamicin resistance, with one case showing intermediate resistance and the remaining three being fully gentamicin-resistant organisms.
No recurrence had been detected for any of the patients for the minimum follow-up time of 1.5 years.
Discussion
The initial gentamicin release in vitro from the synthetic bone graft substitute was similar to that observed in the three different clinical applications. When comparing the elution in Ringer’s solution with gentamicin concentrations in the drainage from both the hip and the tumour patients, a high local antibiotic concentration was observed. It decreased with time, slightly faster for the in vivo studies with a half-life of two days for the tumour patients and 0.5 days for the hip patients, compared with five to six days for the in vitro study. These differences in half-life may be explained by the differences of measurements and collection of samples. In the elution study, the gentamicin concentration is measured within 1 cm of the implant, which gives a truly local concentration. The in vivo studies show the concentration of gentamicin in the drainage which may be considered further away from the implant than 1 cm, giving slightly inferior values of the gentamicin concentration compared with the in vitro study. The static incubation with controlled exchange of 20% of the liquid in the in vitro study may be slower than the actual exchange, which would explain the shorter half-life in the in vivo studies. Also, dissolution of the calcium sulphate component of the bone graft substitute occurs in vitro compared with both dissolution and cellular resorption in vivo, possibly speeding up the release.
The trend is still clear, with an elution pattern that starts with a burst which decreases with time and is maintained above the MIC level for four weeks. The gentamicin release pattern observed thus confirms that the in vitro release model used was found to simulate the performance in clinical applications, which was one of the aims of this study. Having a reliable in vitro model will impact the research and development of new drug-releasing compounds significantly since in vitro tests are much more time- and cost-efficient than expensive animal trials.
The local antibiotic concentrations in both the hip and the tumour study were 100 times the MIC at six hours and still ten times the MIC at 30 hours. This should allow eradication of any planktonic bacteria causing infection and give good preventative levels. The total amount of gentamicin-containing bone substitute implanted in the tumour patients was higher than that used for the hip patients (mean 12.1 mL versus 7.3 mL) which may explain why the gentamicin concentrations in the tumour patients were higher.
It is important that the initial release is significantly above the MIC level locally to prevent bacterial adherence leading to an established deep infection.39 Even though no data on local levels of gentamicin were collected from the clinical study in osteomyelitis patients, there was no recurrence of the infection in any of these patients for the entire 1.5 years’ follow-up time, indicating that the local levels were indeed high enough to eradicate the majority of bacteria. This has further been confirmed in a larger series of clinical cases with a very low rate of recurrence of osteomyelitis.40 The bacterial cultures from the time of osteomyelitis excision surgery showed three cases of resistant bacteria as defined by EUCAST: Methicillin-resistant staphylococcus aureus, Streptococcus agalactiae and Clostridium difficile. However, the test methods used to define the resistance do not necessarily apply here since they are designed for treatment of non-biofilm bacteria and systemic therapy. The local gentamicin concentration during elution from the bone substitute material reaches 100 to 1000 times the MIC level and may therefore be effective in preventing recurrence by eradicating gentamicin-resistant bacteria.
A detectable gentamicin concentration in urine observed for up to seven days in the hip patients indicates prolonged drug release in these cases.
The initial release pattern of antibiotics in this study, using a resorbable bone substitute, is comparable with that of gentamicin-containing PMMA beads,41 with high initial antibiotic levels followed by slower release. In Hedström’s study, 41 the peak release of gentamicin was around ten times the MIC but others have reported initial release from PMMA beads as high as 100 times the MIC value which is known to be effective.14 Ideally, the high local antibiotic concentration of 100 times the MIC should last for the first one to two days and thereafter a prolonged release at a level closer to the MIC should be maintained for another four weeks.42,43 Since PMMA only releases the antibiotics from the surface by diffusion, most of the gentamicin remains trapped in the PMMA matrix, resulting in a prolonged release at antibiotic concentrations below the therapeutic level. Walenkamp44 calculated that approximately 24% (sd 11%) of the total gentamicin amount was released from the PMMA beads over 14 days, compared with 95% for the ceramic bone substitute used in this study. Prolonged antibiotic release at low levels may induce antibiotic resistance.45 In 1989, Hope et al46 found that 90% of Staphylococcal strains isolated from infected hip replacements were resistant to gentamicin after using gentamicin-containing PMMA cement, compared with 16% if plain cement had been used. Other studies have confirmed that antibiotic-loaded PMMA cement reduces infection in total joint arthroplasty at the cost of increasing case-specific resistance.4,47 The studied bone graft substitute is porous, allowing elution from the bulk (without surface dependency) and avoiding antibiotics getting trapped in the material. In this study, it was considered that 100% of the antibiotics had been eluted at 28 days. Moreover, the bone graft substitute is biodegradable30 and will be resorbed by the body over a period of approximately two years27 depending on the amount used and the implant site.
The most severe side effects following the use of systemic gentamicin are renal failure and ototoxicity. These complications are known to occur at high systemic levels of gentamicin but may also result with prolonged gentamicin release, especially if the patient is already suffering from renal insufficiency.48 It is therefore important to use a carrier which assures complete release of the gentamicin within a short period of time to avoid the risk of prolonged and non-reversible exposure to the antibiotic.
Fleiter et al49 treated 20 patients with osteomyelitis (11 in tibia, seven in femur, one humeral head and one metatarsal bone) using local implantation of a calcium sulphate/carbonate bone void filler containing gentamicin. Collection of drainage, serum and urine showed similar gentamicin release curves to those obtained in this study. For all cases, an initial burst was observed followed by a decrease in gentamicin release over the next few days. The gentamicin concentrations were generally lower in the osteomyelitis patients studied by Fleiter et al49 than in the hip and tumour patients studied herein. These results correlate well with ours, where the highest gentamicin concentration measured in serum was 0.54 mg/L (at one day post-operatively) in the osteomyelitis patients, compared with 0.6 mg/L in Fleiter et al’s study. The mean gentamicin amount implanted by Fleiter et al49 was 187 mg versus 186 mg in the current study.
Due to a limitation in the analysis instrument used in our in vivo studies, where the minimal detectable gentamicin concentration was 0.2 mg/L, no release curves could be obtained for the osteomyelitis patients. However, comparing the results from the osteomyelitis patients studied by Fleiter et al49 with our hip and tumour patients, it is most probable that the release curves for the osteomyelitis patients in our study follow the same pattern.
Fleiter et al49 reported recurrent infections in one fifth of the study group (four patients) several weeks to months after surgery, and indicate antibiotic resistance as one possible cause due to repeated local treatment with gentamicin. In our study, no recurrence had been identified 1.5 years after implantation. Fleiter et al49 concluded that local treatment with a resorbable gentamicin-containing bone void filler is a useful option in the battle against deep bone infection. The potential for systemic side effects are minimal with local treatment, and subsequent procedures to remove implanted material and filling of the dead space are avoided by the use of a resorbable bone-regenerating carrier.
Our study highlights four important aspects regarding the elution of gentamicin from this ceramic synthetic bone graft substitute, which makes the use more predictable compared with other carriers: gentamicin is homogenously distributed in the bone substitute ensuring an even release; the elution of the antibiotic is not surface dependent, i.e. antibiotic release occurs from the material bulk as well as from the surface of the sample; the release occurs in the same way from pre-set beads or injectable in situ setting paste, making it effective irrespective of how it is applied; and all gentamicin added to the bone substitute will be eluted. The antibiotic will accumulate in the surrounding tissue of the defect and be locally present in levels above the MIC for the ensuing weeks, depending on the degree of vascularisation of the area and the degree of wound drainage.15
Results from cell cultures in vitro suggest that gentamicin might have a negative impact on the osteoblast, indicating a time-dependent impact on cell number/proliferation and a dose-dependent impact on protein synthesis and cell viability, although there is not a consensus in the results of the studies.50-55 However, animal and human in vivo data show no impact on the bone repair process, and even show a protective effect when a local bone infection exists.56-58 This has been confirmed in animal studies with CERAMENT G, showing active remodelling into bone despite the high initial gentamicin release.31,59
Dvorzhinskiy et al59 studied CERAMENT G versus CERAMENT BONE VOID FILLER without antibiotics in a rat osteomyelitis model. Empty voids were held as controls. Six weeks after debridement and implantation, the CERAMENT G group showed no infections versus 30% positive cultures in the CERAMENT BONE VOID FILLER group and 25% in the control group (p < 0.05). The bone volume/total volume ratio of the region of interest in the CERAMENT G group was 24% greater than in the CERAMENT BONE VOID FILLER group and 94% greater than in the control group (p < 0.05). The study also showed that once the infection had cleared the bone regenerated better and faster.
The ceramic bone substitute used in this study contains gentamicin, providing an efficient antibiotic release and ensuring bone remodeling at the site of debridement. The advantage of using a resorbable bone substitute over PMMA is that a one-step treatment can be performed, both preventing the reinfection by local antibiotic release and promoting new bone ingrowth without the removal of the bone substitute, as is the case with acrylic cement carriers. A second surgery to manage the bone void is avoided and a faster bone healing process is achieved.
In conclusion, this novel antibiotic-eluting biphasic ceramic bone substitute shows promise as one of the steps in the management of chronic osteomyelitis, the prevention of infection and the healing of bone defects in a safe and effective way. A reliable in vitro test method that predicts in vivo performance has been identified for future development of additional new antibiotic-eluting bone regenerating materials.
Funding Statement
This work was supported by the Medical Faculty, Lund University, Lund, Sweden.
J. Ferguson, M. Nilsson, M. McNally, M. Peterson, W. Hettwer and P. Horstmann report grants or personal fees received from BONESUPPORT during the conduct of the study.
M. Peterson also reports funding received from Zimmer and Biomet which is not related to this article. W. Hettwer has a patent on bone reconstruction compositions pending, and a patent on bone reconstruction method pending.
L. Lidgren is a member of the board at BONESUPPORT and Orthocell.
ICMJE conflict of interest
None declared
References
1 Ostermann PA , HenrySL, SeligsonD. The role of local antibiotic therapy in the management of compound fractures. Clin Orthop Relat Res1993;295:102-111.PubMed Google Scholar
2 Ostermann PA , SeligsonD, HenrySL. Local antibiotic therapy for severe open fractures. A review of 1085 consecutive cases. J Bone Joint Surg [Br]1995;77-B:93-97.PubMed Google Scholar
3 Gogia JS , MeehanJP, Di CesarePE, et al.. Local antibiotic therapy in osteomyelitis. Semin Plast Surg2009;23:100-107.CrossrefPubMed Google Scholar
4 Wininger DA , FassRJ. Antibiotic-impregnated cement and beads for orthopedic infections. Antimicrob Agents Chemother1996;40:2675-2679.CrossrefPubMed Google Scholar
5 Cancienne JM , BurrusMT, WeissDB, et al.. Applications of Local Antibiotics in Orthopedic Trauma. Orthop Clin North [Am]2015;46:495-510.CrossrefPubMed Google Scholar
6 Pitt D , AubinJM. Joseph Lister: father of modern surgery. Can J Surg2012;55:E8-E9.CrossrefPubMed Google Scholar
7 Jenkinson RJ , KissA, JohnsonS, et al.. Delayed wound closure increases deep-infection rate associated with lower-grade open fractures: a propensity-matched cohort study. J Bone Joint Surg [Am]2014;96:380-386.CrossrefPubMed Google Scholar
8 Oleske DM , BonafedeMM, JickS, et al.. Electronic health databases for epidemiological research on joint replacements: considerations when making cross-national comparisons. Ann Epidemiol2014;24:660-665.CrossrefPubMed Google Scholar
9 Carr AJ , RobertssonO, GravesS, et al.. Knee replacement. Lancet2012;7:1331-1340.CrossrefPubMed Google Scholar
10 Jämsen E , FurnesO, EngesaeterLB, et al.. Prevention of deep infection in joint replacement surgery. Acta Orthop2010;81:660-666.CrossrefPubMed Google Scholar
11 Zimmerli W , TrampuzA, OchsnerPE. Prosthetic-joint infections. N Engl J Med2004;351:1645-1654. Google Scholar
12 Lundeen SJ , OttersonMF, BinionDG, et al.. Clostridium difficile enteritis: an early postoperative complication in inflammatory bowel disease patients after colectomy. J Gastrointest Surg2007;11:138-142.CrossrefPubMed Google Scholar
13 Borgquist L , W-DahlA, DaleH, et al.. Prosthetic joint infections: a need for health economy studies. Acta Orthop2014;85:218-220.CrossrefPubMed Google Scholar
14 Walenkamp GH , VreeTB, van RensTJ. Gentamicin-PMMA beads. Pharmacokinetic and nephrotoxicological study. Clin Orthop Relat Res1986;205:171-183.PubMed Google Scholar
15 Törholm C , LidgrenL, LindbergL, et al.. Total hip joint arthroplasty with gentamicin-impregnated cement. A clinical study of gentamicin excretion kinetics. Clin Orthop Relat Res1983;181:99-106.PubMed Google Scholar
16 Wahlig H , DingeldeinE. Antibiotics and bone cements. Experimental and clinical long-term observations. Acta Orthop Scand1980;51:49-56.CrossrefPubMed Google Scholar
17 Neut D , vande, BeltH, van HornJR, et al.. Residual gentamicin-release from antibiotic-loaded polymethylmethacrylate beads after 5 years of implantation. Biomaterials2003;24:1829-1831.CrossrefPubMed Google Scholar
18 Kendall RW , DuncanCP, SmithJA, et al.. Persistence of bacteria on antibiotic loaded acrylic depots. A reason for caution. Clin Orthop Relat Res1996;329:273-280.CrossrefPubMed Google Scholar
19 McLaren AC . Alternative materials to acrylic bone cement for delivery of depot antibiotics in orthopaedic infections. Clin Orthop Relat Res2004;427:101-106.CrossrefPubMed Google Scholar
20 Masquelet AC , FitoussiF, BegueT, et al.. Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet2000;45:346-353. (In French) Google Scholar
21 Winkler H , KaudelaK, StoiberA, et al.. Bone grafts impregnated with antibiotics as a tool for treating infected implants in orthopedic surgery - one stage revision results. Cell Tissue Bank2006;7:319-323.CrossrefPubMed Google Scholar
22 Winkler H . Bone grafting and one-stage revision of THR - biological reconstruction and effective antimicrobial treatment using antibiotic impregnated allograft bone. Hip Int2012;22:S62-S68.CrossrefPubMed Google Scholar
23 Chan YS , UengSW, WangCJ, et al.. Management of small infected tibial defects with antibiotic-impregnated autogenic cancellous bone grafting. J Trauma1998;45:758-764.CrossrefPubMed Google Scholar
24 Chan YS , UengSW, WangCJ, et al.. Antibiotic-impregnated autogenic cancellous bone grafting is an effective and safe method for the management of small infected tibial defects: a comparison study. J Trauma2000;48:246-255.CrossrefPubMed Google Scholar
25 Khoo PP , MichalakKA, YatesPJ, et al.. Iontophoresis of antibiotics into segmental allografts. J Bone Joint Surg [Br]2006;88-B:1149-1157.CrossrefPubMed Google Scholar
26 Lovallo J , HelmingJ, JafariSM, et al.. Intraoperative intra-articular injection of gentamicin: will it decrease the risk of infection in total shoulder arthroplasty?J Shoulder Elbow Surg2014;23:1272-1276.CrossrefPubMed Google Scholar
27 Abramo A , GeijerM, KopylovP, et al.. Osteotomy of distal radius fracture malunion using a fast remodeling bone substitute consisting of calcium sulphate and calcium phosphate. J Biomed Mater Res B Appl Biomater2010;92:281-286.CrossrefPubMed Google Scholar
28 Karr J . Clinical Case Presentation: Metatarsal Delayed Union Management in a Diabetic Patient with CERAMENT™|BONE VOID FILLER. The Journal of Diabetic Foot Complications2010;2:65-68. Google Scholar
29 Iundusi R , GasbarraE, D’ArienzoM, et al.. Augmentation of tibial plateau fractures with an injectable bone substitute: CERAMENT™. Three year follow-up from a prospective study. BMC Musculoskelet Disord2015;16:115.CrossrefPubMed Google Scholar
30 Nilsson M , WangJ-S, WielanekL, et al.. Biodegradation and biocompatability of a calcium sulphate-hydroxyapatite bone substitute. J Bone Joint Surg [Br]2004;86-B:120-125.PubMed Google Scholar
31 Lindberg F , LidénE, SandellV. Antibiotic elution and bone remodelling with a novel bone substitute impregnated with Gentamicin [abstract]. EBJIS Conference, 2012. Google Scholar
32 No authors listed. EUCAST Clinical Breakpoint Table v. 5.0, 2015. http://www.eucast.org/clinical_breakpoints/ (date last accssed 15 September 2016).[[bibmisc]] Google Scholar
33 Tam VH , KabbaraS, VoG, et al.. Comparative pharmacodynamics of gentamicin against Staphylococcus aureus and Pseudomonas aeruginosa. Antimicrob Agents Chemother2006;50:2626-2631.CrossrefPubMed Google Scholar
34 Seral C , Van BambekeF, TulkensPM. Quantitative analysis of gentamicin, azithromycin, telithromycin, ciprofloxacin, moxifloxacin, and oritavancin (LY333328) activities against intracellular Staphylococcus aureus in mouse J774 macrophages. Antimicrob Agents Chemother2003;47:2283-2292.CrossrefPubMed Google Scholar
35 Nanavaty J , MortensenJE, ShryockTR. The effects of environmental conditions on the in vitro activity of selected antimicrobial agents against Escherichia coli. Curr Microbiol1998;36:212-215.CrossrefPubMed Google Scholar
36 Menashe O , KaganskayaE, BaasovT, et al.. Aminoglycosides affect intracellular Salmonella enterica serovars typhimurium and virchow. Antimicrob Agents Chemother2008;52:920-926.CrossrefPubMed Google Scholar
37 Baudoux P , BlesN, LemaireS, et al.. Combined effect of pH and concentration on the activities of gentamicin and oxacillin against Staphylococcus aureus in pharmacodynamic models of extracellular and intracellular infections. J Antimicrob Chemother2007;59:246-253.CrossrefPubMed Google Scholar
38 Cierny G III , MaderJT, PenninckJJ. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res2003;414:7-24.CrossrefPubMed Google Scholar
39 Howlin RP , BrayfordMJ, WebbJS, et al.. Antibiotic-loaded synthetic calcium sulfate beads for prevention of bacterial colonization and biofilm formation in periprosthetic infections. Antimicrob Agents Chemother2015;59:111-120.CrossrefPubMed Google Scholar
40 McNally MA , FergusonJY, LauCK, et al.. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite. A prospective series of 100 cases. Bone Joint J2016;98-B:1289–1296. Google Scholar
41 Hedström SÅ , LidgrenL, TörholmC, et al.. Antibiotic containing bone cement beads in the treatment of deep muscle and skeletal infections. Acta Orthop Scand1980;51:863-869.CrossrefPubMed Google Scholar
42 Rossi S , AzghaniAO, OmriA. Antimicrobial efficacy of a new antibiotic-loaded poly(hydroxybutyric-co-hydroxyvaleric acid) controlled release system. J Antimicrob Chemother2004;54:1013-1018.CrossrefPubMed Google Scholar
43 Geurts J , Chris ArtsJJ, WalenkampGH. Bone graft substitutes in active or suspected infection. Contra-indicated or not?Injury2011;42:S82-S86.CrossrefPubMed Google Scholar
44 Walenkamp G . Small PMMA beads improve gentamicin release. Acta Orthop Scand1989;60:668-669.CrossrefPubMed Google Scholar
45 Gristina AG , NaylorPT, MyrvikQN. Musculoskeletal infection, microbial adhesion, and antibiotic resistance. Infect Dis Clin North [Am]1990;4:391-408.PubMed Google Scholar
46 Hope PG , KristinssonKG, NormanP, et al.. Deep infection of cemented total hip arthroplasties caused by coagulase-negative staphylococci. J Bone Joint Surg [Br]1989;71-B:851-855.CrossrefPubMed Google Scholar
47 Oga M , ArizonoT, SugiokaY. Inhibition of bacterial adhesion by tobramycin-impregnated PMMA bone cement. Acta Orthop Scand1992;63:301-304.CrossrefPubMed Google Scholar
48 Nergelius G , VingeE, GrubbA, et al.. Renal impairment after hip or knee arthroplasty. Urinary excretion of protein markers studied in 59 patients. Acta Orthop Scand1997;68:34-40.CrossrefPubMed Google Scholar
49 Fleiter N , WalterG, BösebeckH, et al.. Clinical use and safety of a novel gentamicin-releasing resorbable bone graft substitute in the treatment of osteomyelitis/osteitis. Bone Joint Res2014;3:223-229.CrossrefPubMed Google Scholar
50 Vester H , WildemannB, SchmidmaierG, et al.. Gentamycin delivered from a PDLLA coating of metallic implants: in vivo and in vitro characterisation for local prophylaxis of implant-related osteomyelitis. Injury2010;41:1053-1059.CrossrefPubMed Google Scholar
51 Rathbone CR , CrossJD, BrownKV, et al.. Effect of various concentrations of antibiotics on osteogenic cell viability and activity. J Orthop Res2011;29:1070-1074.CrossrefPubMed Google Scholar
52 Popat KC , EltgrothM, LatempaTJ, et al.. Decreased Staphylococcus epidermis adhesion and increased osteoblast functionality on antibiotic-loaded titania nanotubes. Biomaterials2007;28:4880-4888.CrossrefPubMed Google Scholar
53 Lewis CS , KatzJ, BakerMI, et al.. Local antibiotic delivery with bovine cancellous chips. J Biomater Appl2011;26:491-506.CrossrefPubMed Google Scholar
54 Ince A , SchützeN, HendrichC, et al.. In vitro investigation of orthopedic titanium-coated and brushite-coated surfaces using human osteoblasts in the presence of gentamycin. J Arthroplasty2008;23:762-771.CrossrefPubMed Google Scholar
55 Belcarz A , GinalskaG, ZalewskaJ, et al.. Covalent coating of hydroxyapatite by keratin stabilizes gentamicin release. J Biomed Mater Res B Appl Biomater2009;89:102-113.CrossrefPubMed Google Scholar
56 Wu CC . Single-stage surgical treatment of infected nonunion of the distal tibia. J Orthop Trauma2011;25:156-161.CrossrefPubMed Google Scholar
57 Stewart RL , CoxJT, VolgasD, et al.. The use of a biodegradable, load-bearing scaffold as a carrier for antibiotics in an infected open fracture model. J Orthop Trauma2010;24:587-591.CrossrefPubMed Google Scholar
58 Alt V , BitschnauA, BöhnerF, et al.. Effects of gentamicin and gentamicin-RGD coatings on bone ingrowth and biocompatibility of cementless joint prostheses: an experimental study in rabbits. Acta Biomater2011;3:1274-1280.CrossrefPubMed Google Scholar
59 Dvorzhinskiy A , PerinoG, ChojnowskiR, et al.. Cerament bone void filler with gentamicin increases bone formation and decreases detectable infection in a rat model of debrided osteomyelitis [abstract]. EBJIS Conference, 2015. Google Scholar









