Abstract
Aims
Assessment of bone mineral density (BMD) with dual-energy X-ray absorptiometry (DXA) is a well-established clinical technique, but it is not available in the acute trauma setting. Thus, it cannot provide a preoperative estimation of BMD to help guide the technique of fracture fixation. Alternative methods that have been suggested for assessing BMD include: 1) cortical measures, such as cortical ratios and combined cortical scores; and 2) aluminium grading systems from preoperative digital radiographs. However, limited research has been performed in this area to validate the different methods. The aim of this study was to investigate the evaluation of BMD from digital radiographs by comparing various methods against DXA scanning.
Methods
A total of 54 patients with distal radial fractures were included in the study. Each underwent posteroanterior (PA) and lateral radiographs of the injured wrist with an aluminium step wedge. Overall 27 patients underwent routine DXA scanning of the hip and lumbar spine, with 13 undergoing additional DXA scanning of the uninjured forearm. Analysis of radiographs was performed on ImageJ and Matlab with calculations of cortical measures, cortical indices, combined cortical scores, and aluminium equivalent grading.
Results
Cortical measures showed varying correlations with the forearm DXA results (range: Pearson correlation coefficient (r) = 0.343 (p = 0.251) to r = 0.521 (p = 0.068)), with none showing statistically significant correlations. Aluminium equivalent grading showed statistically significant correlations with the forearm DXA of the corresponding region of interest (p < 0.017).
Conclusion
Cortical measures, cortical indices, and combined cortical scores did not show a statistically significant correlation to forearm DXA measures. Aluminium-equivalent is an easily applicable method for estimation of BMD from digital radiographs in the preoperative setting.
Cite this article: Bone Joint Res 2021;10(12):830–839.
Article focus
-
There is no routinely administered, standardized preoperative method of bone mineral density (BMD) assessment in the trauma setting.
-
This paper compares methods of BMD evaluation from digital radiographs against results obtained from dual-energy X-ray absorptiometry (DXA) scanning.
Key messages
-
Cortical measures, cortical indices, and combined cortical scores did not show a statistically significant correlation to forearm DXA measures.
-
Use of aluminium phantoms can prove to be an accurate assessment of bone density in the wrist.
-
This method is easy to implement and can be corrected for soft-tissue.
Strengths and limitations
-
A limited number of participants were able to provide both hip and wrist DXA assessment.
-
An aluminium step wedge is a low-cost, easy-to-use phantom that is combatable with trauma radiological equipment.
Introduction
Bone mineral density (BMD) is defined as the amount of bone minerals per unit area of bone.1 This is often used as a proxy measure of bone strength, providing a preoperative indication of the quality of bone prior to fracture repair.2
The standard method for assessing BMD is dual-energy X-ray absorptiometry (DXA), as recommended by the National Institute for Health and Care Excellence (NICE) and Scottish Intercollegiate Guidelines Network (SIGN) guidelines.3,4 This technique is based on the process by which an X-ray source produces two X-ray beams, each of different energy levels, to correct for soft-tissue.1 DXA provides an ‘area density’ (g/cm2), i.e. the bone mineral contained in a given projected area of bone.5
DXA assessment is routinely used for postoperative diagnosis of osteoporosis following low-energy fracture. However, as BMD assessment is not carried out on an emergency or urgent basis, it is not available preoperatively.4 However, knowledge of the bone strength before surgery would provide very useful information to surgeons in order to allow them to choose the optimal implant and method for fracture fixation for each patient.2
For example, with fractures of the distal radius that require surgical fixation, there are a number of techniques available. These include Kirschner wire fixation of the fracture segments, plating (both locked and unlocked) or external fixation of the fracture.6 The biomechanical strength and quality of the bone plays a crucial role in the stability of the constructs used for fixation.7 Preoperative quantitative values for BMD would allow surgeons to select the fixation method based on the bone quality, increasing the likelihood of successful fixation and rapid healing.
Radiographs are routinely taken before fracture fixation. However, a well-defined and consistently quantifiable method to assess BMD and bone quality preoperatively from digital radiographs is not presently available in the standard clinical setting. Techniques currently used clinically centre on subjective, qualitative assessment of the radiograph by the surgeon and the patient characteristics.2 These, combined with personal experience and preference, often form the basis for the choice of fixation technique.2 Such subjective assessment of bone density from radiographs is variable, unreliable, and strongly influenced by user experience and interpretation.8-10 In contrast, quantitative tools that allow assessment of BMD and bone quality from digital radiography2 would provide a more accurate and objective assessment and help to optimize fracture fixation techniques and materials.
Digital radiography systems offer potential in enhancing existing radiograph techniques due to their high-quality digital output and post-processing control.11 This allows for more accurate measurements of bone geometry and trabecular patterns as potential methods for estimating BMD,12 as well as digital quantification of gray level.11
Currently available methods for assessment of BMD on preoperative radiographs include cortical measures and ratios,13,14 simple textural analysis methods,15 and more complex textural analyses.12 The use of an aluminium step wedge in radiographs to establish aluminium equivalent (AlEq) densities has been well validated in the fields of dentistry and archaeological science,16-18 but not for limb fractures in a clinical setting.
The aim of this study was to investigate the use of digital radiograph images for providing a preoperative estimation of BMD of the distal radius. Two methods were assessed: 1) measurements of cortical thicknesses with associated cortical indices and combined cortical scores – referred to as cortical measures; and 2) AlEq thickness grading, achieved by inclusion of an aluminium step wedge in the digital radiographs – referred to as AlEq measures.
Methods
Patients
Ethical approval was obtained from the South East Scotland (NHS Lothian) Research Ethics Committee to assess an additional region (i.e. the wrist) during the routine DXA examination.
All adult patients with an isolated distal radius fracture presenting at the Emergency Department (ED) were considered for inclusion in the study. Patients excluded from the study were: those with substantial other injuries in addition to their wrist fracture; those with pathological fractures; and those with notable cognitive impairment or any other condition which would prevent them from being eligible for further DXA investigation.
A total of 54 consecutive consenting patients (46 female; eight male), who met the above criteria, were included in the study (Figure 1). The mean age was 73.9 years (57 to 95; standard deviation (SD) 11). Each underwent posteroanterior (PA) and lateral digital radiographs of their injured wrist in the ED, with an aluminium step wedge placed at the side of the wrist (Figure 2).
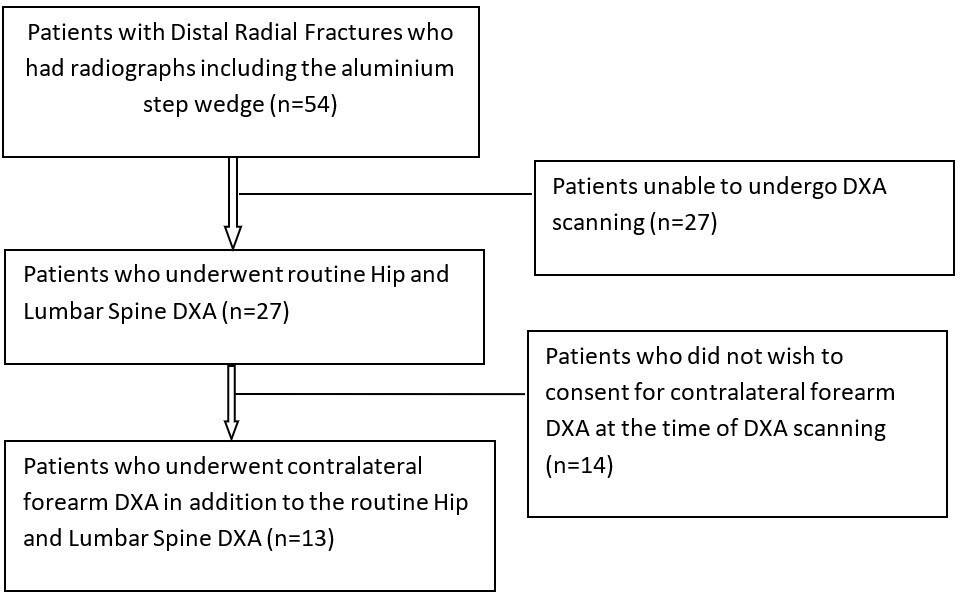
Fig. 1
Recruitment process for the study patients. DXA, dual-energy X-ray absorptiometry.
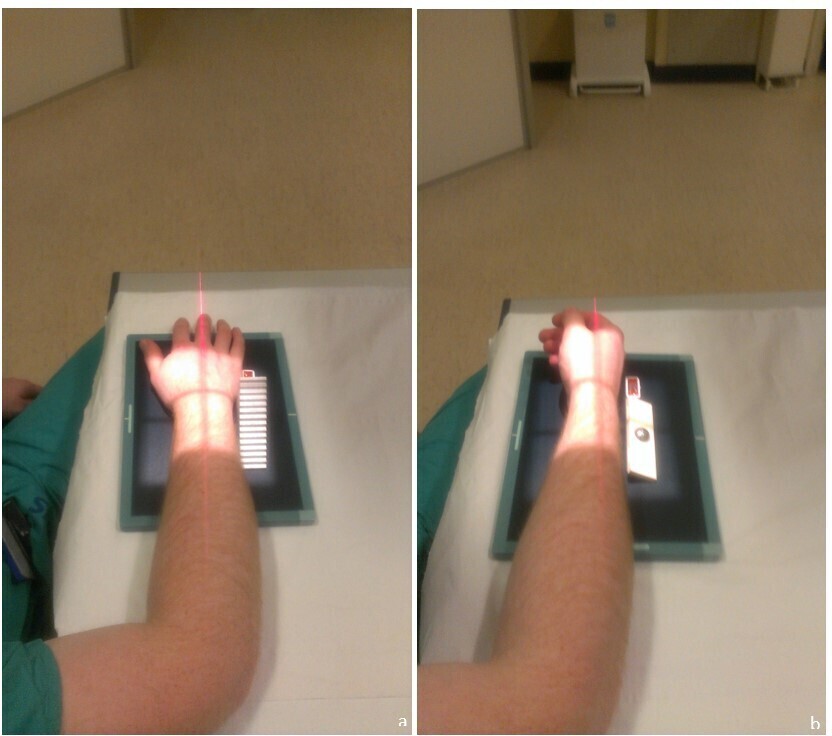
Fig. 2
Wrist radiograph set-up: a) posteroanterior (PA) view (note aluminium step wedge to the right of the wrist); b) lateral view (note stainless steel ball within plastic holder to the right of the wrist).
Radiographs
All radiographs were taken using the FUJI XG5000 Calculated Radiography System, with Fuji FCR type CC IP Cassettes at a focal distance of 1 m. The mean voltage used for the radiographs was 59.4 kV (52 to 60; SD 2.0). The mean current used for the radiographs was 2.0 mA (1.6 to 2.5; SD 0.3).
The aluminium step wedge was incorporated into the PA radiographs (Figure 2), enabling AlEq values of bone to be derived and also acting as a known length for calibration of the PA X-rays. The step wedge was placed at the level of the radiocarpal joint, as close to the patient as possible. A stainless steel ball bearing of diameter 20 mm was included in the lateral radiograph, to allow calculation of the depth of the soft-tissue and bone through which the radiograph beams travel. This was placed adjacent to the injured forearm, as close to the forearm as possible, one hand breadth (of the operating radiographer) proximal to the radiocarpal joint (Figure 2). The soft-tissue and bone thickness dimensions were required for the technique of establishing AlEq measures of the distal radius, as described by Dawson.19
The automatic gain control of the Digital Processing System was disabled on the FUJI electronic radiograph system. This allowed provision of unprocessed radiographs for subsequent analysis in MATLAB (2013a; MathWorks, USA) and ImageJ (2012; National Institutes of Health (NIH), USA).
Aluminium step wedge
The dimensions of the step wedge were 75 mm (height) by 75 mm (length) by 30 mm (thickness), with 15 steps on its surface each 5 mm in height (Figure 3). The step wedge was manufactured from Duralumin, an aluminium alloy, containing aluminium, copper, magnesium, and manganese. The step wedge was deburred to remove sharp edges and was suitable for autoclave sterilization.
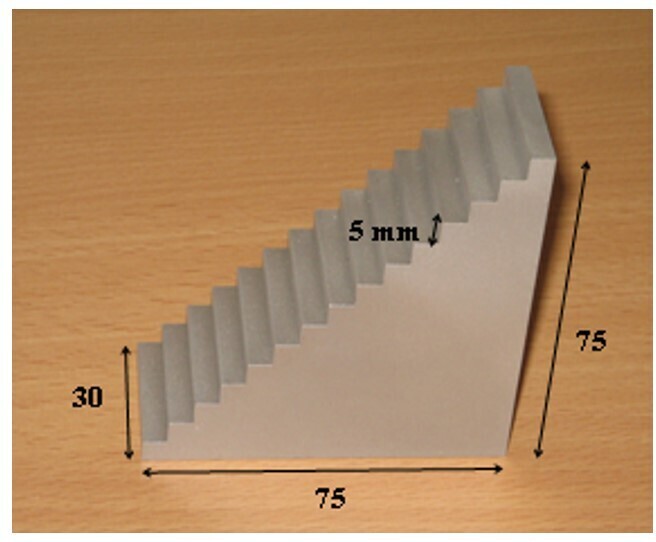
Fig. 3
The aluminium step wedge (all measurements in millimetres).
DXA measurements
In total, 27 of the patients underwent routine DXA scanning of their hip and lumbar spine, following their fracture. Of these, 13 consented to the additional DXA analysis of the contralateral forearm, as shown in Figure 4. All of these patients had adequate PA and lateral radiographs to allow full cortical measurement assessment and AlEq measure analysis. Demographic data for the patient cohorts are presented in Table I.
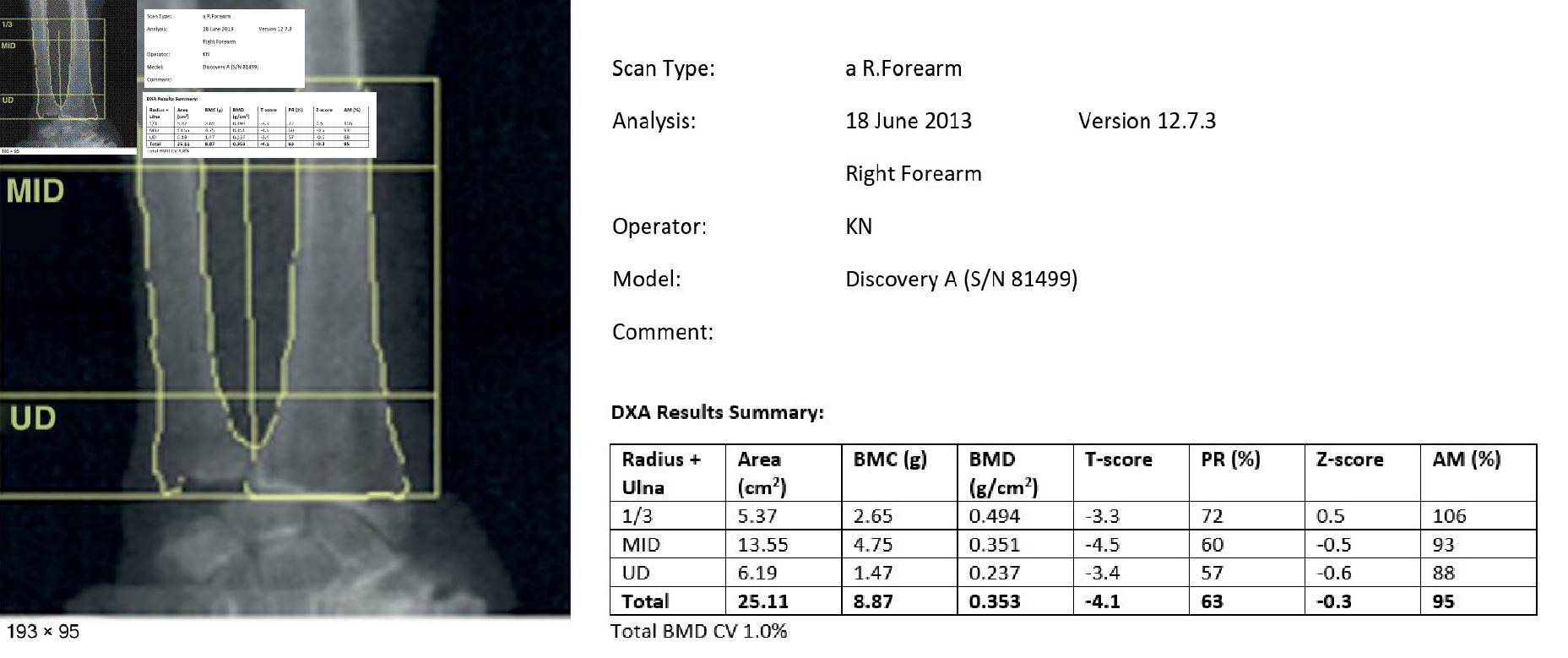
Fig. 4
Forearm dual-energy X-ray absorptiometry (DXA) result – DXA scan of the contralateral forearm to the fracture side, demonstrating the bone mineral density (BMD) measures of the three regions of interest. AM, age-matched; BMC, bone mineral content; MID, mid distal; PR, peak reference; UD, ultra-distal.
Table I.
Demographic data of the patient cohorts.
| AlEq region in forearm | Corrected for soft-tissue (n = 27) | Non-corrected for soft-tissue (n = 27) | Paired t-test (p-value: 95% CI) | Intraobserver reliability (ICC) |
|---|---|---|---|---|
| ‘Ultra-distal’ region AlEq, AlEq/mm2 (range) | 1.25 (0.91 to 1.58) | 5.43 (3.95 to 6.86) | 0.001: 3.442 to 4.929 | 0.902 |
| ‘Mid-distal’ region AlEq, AlEq/mm2 (range) | 1.89 (1.43 to 2.07) | 9.02 (6.47 to 9.37) | 0.001: 5.878 to 8.390 | 0.857 |
| ‘One-third’ region AlEq, AlEq/mm2 (range) | 3.39 (1.83 to 4.74) | 17.93 (3.11 to 10.57) | 0.001: 12.052 to 17.025 | 0.813 |
-
AlEq, aluminium equivalent; CI, confidence interval; ICC, intraclass correlation.
The forearm DXA analysis provided areal BMD readings (grams per cm2) from the ‘ultra-distal’ region (distal juxta-articular region of radius and ulna), the ‘mid-distal’ region (metaphyseal region of radius and ulna), and the ‘one-third’ region (distal diaphyseal region of radius and ulna), as well as the whole forearm region, as per the standard protocol recommended by the manufacturer (Figure 4).
Image analysis for cortical measures
ImageJ was used to assess the following geometrical parameters for the cortical measures on the PA wrist radiograph shown in Figure 5. All measures were performed three times by the same person (GR) and the mean obtained: a) second metacarpal – mid-diaphyseal width, lateral cortical width, and medial cortical width; b) radial diaphysis – diaphyseal width, lateral cortical width, and medial cortical width; and c) ulnar diaphysis – diaphyseal width, lateral cortical width, and medial cortical width.
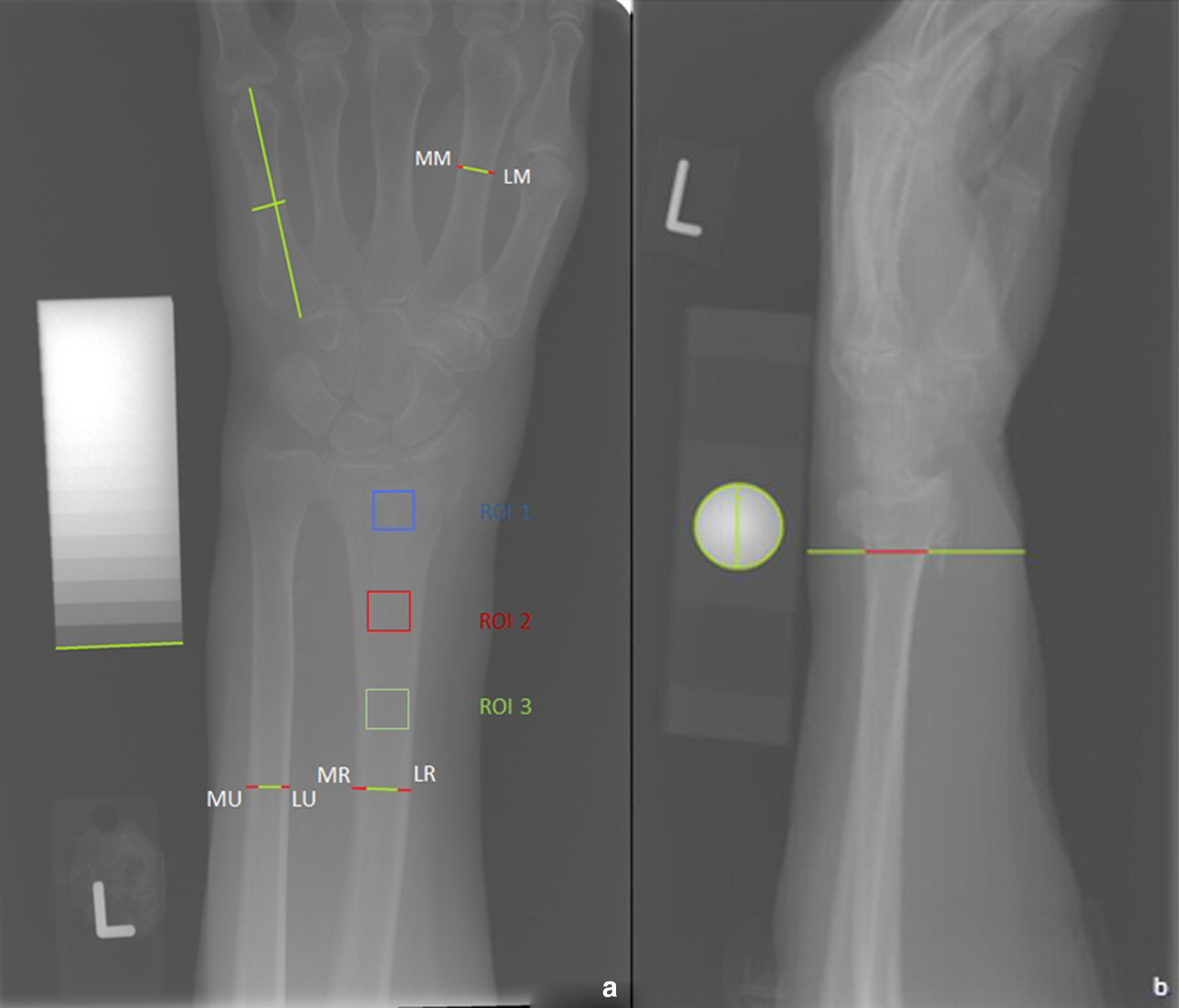
Fig. 5
a) Preoperative posteroanterior (PA) wrist radiograph of a 73-year-old female, demonstrating cortical measures (LR – lateral cortex of the distal radial diaphysis, MR – medial cortex of the distal radial diaphysis, LU – lateral cortex of the distal ulnar diaphysis, MU – medial cortex of the distal ulnar diaphysis, LM – lateral cortex of the second metacarpal mid-diaphyseal, MM – medial cortex of the second metacarpal mid-diaphyseal), cortical ratios, and region of interest (ROI) for the aluminium equivalent values (ROI 1 – ultra-distal ROI; ROI 2 – mid-distal ROI; ROI 3 – one-third ROI); b) preoperative lateral wrist radiograph of a 73-year-old female, demonstrating soft-tissue measurement.
To standardize the images and enhance contrast, all radiographs were expanded to the full width of the screen. Bone and soft-tissue dimensions were extrapolated from the known dimensions of the aluminium step wedge in the PA wrist radiographs and the known diameter of the ball bearing in the lateral wrist radiographs, in order to correct for the distortion of length introduced by the fan-beam X-ray. These are referred to as calibrated dimensions.
Intraobserver reliability of the image analysis and measurement sequence was assessed by the same observer (GR) performing the image analysis and measurements for each of the distal radii three times, and quantified using the intraclass correlation (ICC) (two-way random model with absolute agreement) model.
To define a uniform level of assessment for the cortical measurements of the radial and ulnar diaphysis for each patient, the following method was used.
The width of the distal radial articular surface was measured, from the most distal radial aspect of the radial styloid to the most ulnar aspect of the distal radial articular surface, using the measuring tool on ImageJ. A line measuring two widths of the distal radial articular surface was drawn proximally from the midpoint of the distal radial articular surface.
The cortical indices were calculated using the following formula, developed by the authors as a method to provide cortical dimension assessment of the distal radius and ulna (Figure 5):
Cortical index = (width of lateral cortex + width of medial cortex) / width of diaphysis
The formulae for the combined cortical measure scores are provided in the Supplementary Material.
Image analysis for aluminium equivalent measures
Three regions of interest (ROIs) were chosen for analysis of AlEq measures to correspond with the forearm DXA radiological measures: ‘ultra-distal’, ‘mid-distal’, and ‘one-third’ regions. Soft-tissue and bone thickness measurements were obtained from the lateral radiographs (Figure 5). All measures were performed three times and the mean obtained.
Using the methods described by Dawson,19 MATLAB was used to correct for the differing effects of scatter and absorption in the soft-tissue, providing corrected AlEq measure values. These corrected AlEq measures were compared against all four values of the forearm DXA analysis and the hip DXA analysis.
DXA analysis
For the patients with both forearm DXA analysis and hip DXA analysis, the ‘total’ forearm DXA results were compared against all the ‘total’ hip DXA results.
Statistical analysis
Correlations between data were performed with Pearson correlation coefficient (r) models (for normally distributed data) and Spearman’s Rank correlation coefficient models (for non-normally distributed data and datasets with statistically significant outliers). Normality of datasets was assessed for using the Shapiro–Wilk test. Comparison of correlation coefficient values was performed with the Fisher r-to-z transformation (z) statistical test. Univariate comparison between continuous ‘soft tissue’ corrected and non-corrected data was performed with paired t-tests. Intraobserver reliability was calculated using the intraclass correlation (ICC) (two-way random model with absolute agreement) model. For all statistical tests, the significance level was set at p < 0.05.
Results
Cortical measures
The r values between the cortical measures and the DXA reading are provided in Figure 6 and Supplementary Table i. None of the cortical measures had a statistically significant correlation with any of the DXA results.
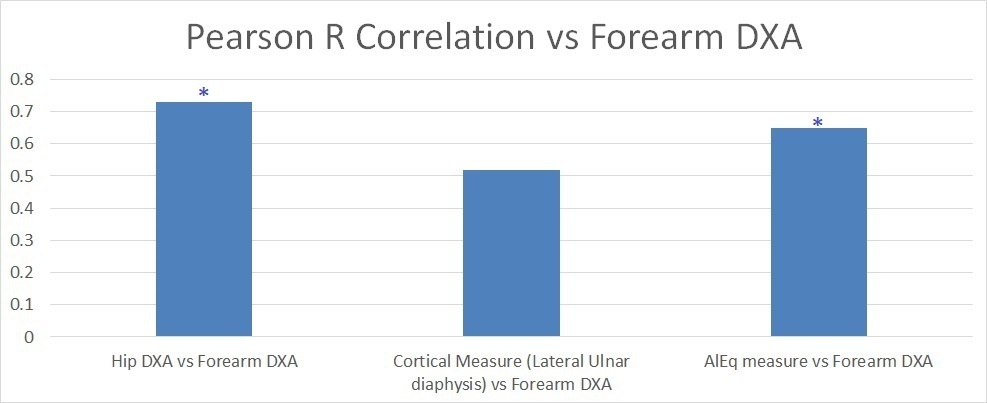
Fig. 6
The Pearson correlation coefficient (r) values with forearm dual-energy X-ray absorptiometry (DXA). Column 1: hip DXA vs forearm DXA; column 2: ulnar diaphysis lateral cortex versus forearm DXA; column 3: ‘ultra distal’ aluminium equivalent (AlEq) (corrected for soft-tissue) versus ‘ultra distal’ forearm DXA. *p < 0.05 for Pearson correlation coefficient (r) model. The correlation between the AlEq measures and the forearm DXA measures was statistically significant. The correlation between the hip DXA measures and the forearm DXA measures was also statistically significant.
The strongest correlation between cortical measures and forearm DXA was seen with the lateral cortex of the ulna diaphysis (r = 0.52 (p = 0.068)), using the Pearson correlation coefficient model.
The use of cortical indices (ulna diaphysis cortical index vs ‘forearm’ DXA: r = 0.506 (p = 0.078)) provided no statistically significant improvement over cortical measures, using the Pearson correlation coefficient model.
The use of the combined cortical scores resulted in a modest improvement (radial ulnar and second metacarpal (MCP) score vs ‘forearm’ DXA: r = 0.543 (p = 0.055)) in the correlation with DXA, using the Pearson correlation coefficient model.
Correlation values for cortical measures were stronger with forearm DXA values (lateral cortex of the ulna diaphysis: r = 0.521 (p = 0.068)) than with hip DXA values (lateral cortex of the ulna diaphysis: r = 0.354 (p = 0.070)), using the Pearson correlation coefficient model.
The intraobserver reliability for the cortical measurements ranged from 0.82 to 0.96.
Aluminium equivalent measures
The AlEq density measures of the distal radius are listed in Table II. The paired t-test results for the comparisons between corrected and non-corrected data, as well as the ICC values of intraobserver reliability are also given in Table II. There was a statistically significant difference between the AlEq values, corrected and non-corrected for the effects of soft-tissue attenuation, demonstrating the need to take the soft-tissues into account when determining the aluminium equivalence of the bone.
Table II.
The aluminium equivalent measures of the distal radius.
| Group | Total cohort | Patients with standard DXA scans | Patients with standard DXA scans and additional forearm DXA |
|---|---|---|---|
| n | 54 | 27 | 13 |
| Mean age, yrs (range) | 73.9 (57 to 95) | 73.4 (57 to 88) | 72.6 (57 to 88) |
| Sex (M:F), n | 8:46 | 4:23 | 1:12 |
-
DXA, dual X-ray absorptiometry.
The correlation coefficients of the DXA values and the AlEq density measures of the distal radius are shown in Figure 6 and Figure 7. Statistically significant correlations were seen between the AlEq (corrected for soft-tissue) and DXA values of the corresponding regions, using the Pearson correlation coefficient model (‘ultra-distal’ AlEq vs ‘ultra-distal’ DXA: r = 0.64 (p < 0.017); ‘mid-distal’ AlEq vs ‘mid-distal’ DXA: r = 0.62 (p < 0.023); ‘one-third’ AlEq vs ‘one-third’ DXA: r = 0.61 (p < 0.028).
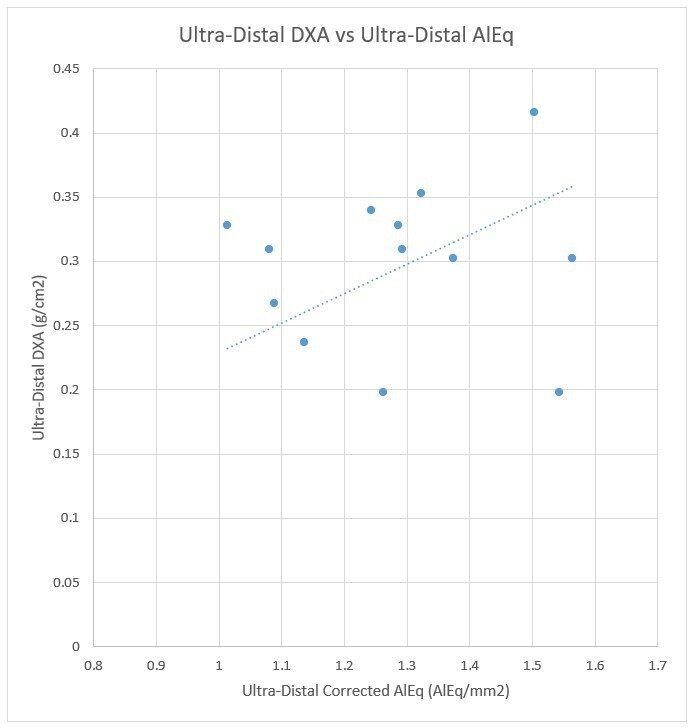
Fig. 7
Scatter plot of ‘ultra-distal DXA versus ultra-distal AlEq (corrected for soft-tissue)’. AlEq, aluminium equivalent; DXA, dual-energy X-ray absorptiometry.
Correlation values for AlEq measures were stronger with forearm DXA values, using the Pearson correlation coefficient model ('ultra-distal’ AlEq vs ‘ultra-distal’ DXA: r = 0.64 (p < 0.017)) than with hip DXA values ('ultra-distal’ AlEq vs ‘hip’ DXA: r = 0.33 (p = 0.089)).
The correlation between the forearm and hip DXA values
DXA-derived values were obtained from the forearm with a mean of 0.44 g/cm3 (0.32 to 0.56; SD 0.07) and from the hip with a mean of 0.78 g/cm3 (0.64 to 1.00; SD 0.09). The correlation between the total forearm and the total hip DXA values was 0.73 (p < 0.005), using the Pearson correlation coefficient model.
Discussion
The main finding from this study was that AlEq measures of the distal radius provided statistically significant correlations with corresponding forearm DXA BMD measures. This suggests that AlEq measures may provide an accurate method of preoperative BMD density estimation of the distal radius in digital radiographs, and so could be used to guide methods and materials of fracture fixation. In contrast, cortical measures, cortical indices, and combined cortical scores from the second metacarpal, radial, and ulnar diaphyses did not show statistically significant correlations with forearm or hip DXA values.
Use of the aluminium step wedge in plain radiography to correlate AlEq measures with BMD is a long-established and well-validated technique in the field of dentistry, where it is used to compare the density of intra-oral restorative materials against surrounding anatomical structures.20-26
However, use of the AlEq technique to assess BMD from digital radiographs of human peripheries remains limited.19 Kolbeck et al27 employed AlEq measures to assess changes of BMD during tibial osteogenesis following tibial-lengthening in pigs. They found that their method was able to quantify the density of regenerate bone throughout the healing process, with a statistically significant correlation between equivalent aluminium thickness and torsional stiffness. However, their results showed considerable variation, which may have been due to: 1) an automatic image-processing system; 2) the effects of soft-tissue attenuation and radiation scatter; and 3) a failure to normalize equivalent measures with bone thickness.19 These potential sources of error were accounted for within our study.
Our results showed no statistically significant correlations with any of the cortical measures and any of the DXA measures. Previous studies have found measures of the cortical thickness of the proximal radius to correlate with age and female sex,28 and cortical indices of the second metacarpal to correlate with vertebral DXA and forearm single photon absorptiometry readings;29 however, neither of these studies made comparisons against forearm DXA readings.
Barnett and Nordin30 and Wishart et al29 both considered the cortical index to provide a better correlation with BMD compared to simple measures of a single cortex. However, we failed to find any statistically significant improvement in correlation with cortical indices in our results.
None of these studies28-30 assessed the effect of summation of cortical measures on the improvement of BMD estimation. Such a method has been previously reported by Tingart et al,13 who found that a combined cortical scoring system of the proximal humerus provided statistically significant correlations with corresponding proximal humeral DXA BMD measures. From the results of our study, it appears that use of such a technique in the forearm does not provide statistically significant correlations with forearm DXA BMD values, and so does not provide accurate BMD estimates.
The DXA results were taken from the contralateral forearm. This was considered justified based on the findings of Sergi et al31 and Taafe et al.32 Both assessed variations in bilateral forearm DXA readings: Sergi at al31 found no statistically significant difference between the dominant and non-dominant forearm DXA values; Taafe et al32 reported percentage differences between dominant and non-dominant forearm DXA values of 1.8% for young patients and 1.0% for elderly patients.
The findings that the hip DXA values provide good correlation with the forearm DXA values have previously been acknowledged.33 However, given the comparison of the correlation values for ‘forearm AlEq vs forearm DXA’ and ‘hip DXA vs forearm DXA’ (0.640 vs 0.730), it would appear that forearm AlEq can provide a suitable preoperative alternative to routine DXA for BMD estimate.
The main limitation of the study is the limited sample size, with only 13 patients undergoing additional forearm DXA, to allow AlEq comparison data on the distal radius. This unfortunately was due to a lack of patient willingness to undergo the additional DXA site. However, despite the limited cohort size, the simultaneous measurements performed in the same patients have allowed direct comparisons to be made between the different BMD assessments. Future studies should aim to compare AlEq measures to other density and strength measures that could be usefully interpreted by surgeons planning their surgeries.
In conclusion, this study found that the AlEq measures could be used as a reliable measure of BMD analysis on digital radiographs of the wrist. Cortical measures, cortical indices, and combined cortical scores, at the wrist, from such radiographs did not provide accurate correlations with BMD. The AlEq technique could form a useful method of preoperative BMD estimation of the distal radius, and so allow surgical methods and materials to be adapted accordingly. However, further studies would be required to confirm that such findings correlated with the stability of fixation materials within bone, in order to validate the use of this technique in clinical practice.
References
1. Ramachandran M . Basic Orthopaedic Sciences: The Stanmore Guide . Boca Raton, Florida : Taylor & Francis Group , 2006 . Google Scholar
2. Huber MB , Carballido-Gamio J , Fritscher K , et al. Development and testing of texture discriminators for the analysis of trabecular bone in proximal femur radiographs . Med Phys . 2009 ; 36 ( 11 ): 5089 – 5098 . Crossref PubMed Google Scholar
3. No authors listed . Osteoporosis: assessing the risk of fragility fracture. Clinical guideline [CG146] . National Institute for Health and Care Excellence (NICE) , 2021 . https://www.nice.org.uk/guidance/cg146 ( date last accessed 10 November 2021 ). Google Scholar
4. No authors listed . SIGN142: Management of osteoporosis and the prevention of fragility fractures: A national clinical guideline . Scottish Intercollegiate Guidelines Network (SIGN) . 2021 . https://www.sign.ac.uk/media/1812/sign-142-osteoporosis-v3.pdf ( date last accessed 3 December 2021 ). Google Scholar
5. Strømsøe K . Fracture fixation problems in osteoporosis . Injury . 2004 ; 35 ( 2 ): 107 – 113 . Crossref PubMed Google Scholar
6. Mirghasemi SA , Rashidinia S , Sadeghi MS , Talebizadeh M , Rahimi N , et al. A prospective study of a modified pin-in-plaster technique for treatment of fractures of the distal radius . Bone Joint Res . 2015 ; 4 ( 11 ): 176 – 180 . Crossref PubMed Google Scholar
7. Court-Brown C , McQueen MM , Tornetta III P . Orthopaedic Surgery Essentials Series: Trauma . Philadelphia, Pennsylvania : Lippincott Williams & Wilkins , 2006 . Google Scholar
8. Wagner S , Stäbler A , Sittek H , et al. Diagnosis of osteoporosis: visual assessment on conventional versus digital radiographs . Osteoporos Int . 2005 ; 16 ( 12 ): 1815 – 1822 . Crossref PubMed Google Scholar
9. Garton MJ , Robertson EM , Gilbert FJ , Gomersall L , Reid DM . Can radiologists detect osteopenia on plain radiographs? Clin Radiol . 1994 ; 49 ( 2 ): 118 – 122 . Crossref PubMed Google Scholar
10. Koot VC , Kesselaer SM , Clevers GJ , de Hooge P , Weits T , van der Werken C . Evaluation of the Singh index for measuring osteoporosis . J Bone Joint Surg Br . 1996 ; 78-B ( 5 ): 831 – 834 . PubMed Google Scholar
11. Nomoto R , Mishima A , Kobayashi K , et al. Quantitative determination of radio-opacity: equivalence of digital and film X-ray systems . Dent Mater . 2008 ; 24 ( 1 ): 141 – 147 . Crossref PubMed Google Scholar
12. Chappard C , Bousson V , Bergot C , et al. Prediction of femoral fracture load: cross-sectional study of texture analysis and geometric measurements on plain radiographs versus bone mineral density . Radiology . 2010 ; 255 ( 2 ): 536 – 543 . Crossref PubMed Google Scholar
13. Tingart MJ , Apreleva M , von Stechow D , Zurakowski D , Warner JJ . The cortical thickness of the proximal humeral diaphysis predicts bone mineral density of the proximal humerus . J Bone Joint Surg Br . 2003 ; 85-B ( 4 ): 611 – 617 . Crossref PubMed Google Scholar
14. Skedros JG , Mears CS , Burkhead WZ . Ultimate fracture load of cadaver proximal humeri correlates more strongly with mean combined cortical thickness than with areal cortical index, DEXA density, or canal-to-calcar ratio . Bone Joint Res . 2017 ; 6 ( 1 ): 1 – 7 . Crossref PubMed Google Scholar
15. Singh M , Nagrath AR , Maini PS . Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis . J Bone Joint Surg Am . 1970 ; 52-A ( 3 ): 457 – 467 . PubMed Google Scholar
16. No authors listed . ISO 9917-1:2007: Dentistry — Water-based cements — Part 1: Powder/liquid acid-base cements . International Organization for Standardization (ISO) . 2007 . https://www.iso.org/standard/45818.html ( date last accessed 10 November 2021 ). Google Scholar
17. No authors listed . ISO 4049. Dentistry – Polymer-based filling, restorative and luting materials . International Organization for Standardization (ISO) . 2000 . https://www.iso.org/standard/23041.html ( date last accessed 3 December 2021 ). Google Scholar
18. No authors listed . ISO 6876:2001: Dental root canal sealing materials . International Organization for Standardization (ISO) . 2001 . https://www.iso.org/standard/34965.html ( date last accessed 3 December 2021 ). Google Scholar
19. Dawson SP . Digital X-Ray Analysis for Monitoring Fracture Healing, in Edinburgh Orthopaedic Engineering Department . Edinburgh : University of Edinburgh . 2009 : 1-312 . Google Scholar
20. Beyer-Olsen EM , Orstavik D . Radiopacity of root canal sealers . Oral Surg Oral Med Oral Pathol . 1981 ; 51 ( 3 ): 320 – 328 . Crossref PubMed Google Scholar
21. Bloxom RM , Manson-Hing LR . The accuracy of an x-ray film quality-assurance step-wedge test . Oral Surg Oral Med Oral Pathol . 1986 ; 62 ( 4 ): 449 – 458 . Crossref PubMed Google Scholar
22. Willems G , Noack MJ , Inokoshi S , et al. Radiopacity of composites compared with human enamel and dentine . J Dent . 1991 ; 19 ( 6 ): 362 – 365 . Crossref PubMed Google Scholar
23. Swart TJ , Seeliger JE . Densitometric evaluation of intra-oral radiographic film-processing solution combinations . J Dent Assoc S Afr . 1989 ; 44 ( 7 ): 281 – 283 . PubMed Google Scholar
24. Matthee MJ , Seeliger JE . Densitometric evaluation of seven dental film processing solutions . J Dent Assoc S Afr . 1990 ; 45 ( 2 ): 31 – 33 . PubMed Google Scholar
25. Hedin M . Developing solutions for dental X-ray processors . Swed Dent J . 1989 ; 13 ( 6 ): 261 – 265 . PubMed Google Scholar
26. Fjellström CA , Fredholm U , Julin P , Rehnmark S , et al. Optimal processing of Ektaspeed dental film . Swed Dent J . 1986 ; 10 ( 4 ): 137 – 143 . PubMed Google Scholar
27. Kolbeck S , Bail H , Weiler A , Windhagen H , Haas N , Raschke M . Digital radiography. A predictor of regenerate bone stiffness in distraction osteogenesis . Clin Orthop Relat Res . 1999 ; 366 : 221 – 228 . PubMed Google Scholar
28. Meema HE , Bunker ML , Meema S . Loss of compact bone due to menopause . Obstet Gynecol . 1965 ; 26 : 333 – 343 . PubMed Google Scholar
29. Wishart JM , Horowitz M , Bochner M , Need AG , Nordin BE . Relationships between metacarpal morphometry, forearm and vertebral bone density and fractures in post-menopausal women . Br J Radiol . 1993 ; 66 ( 785 ): 435 – 440 . Crossref PubMed Google Scholar
30. Barnett E , Nordin BE . The radiological diagnosis of osteoporosis: a new approach . Clin Radiol . 1960 ; 11 : 166 – 174 . Crossref PubMed Google Scholar
31. Sergi G , Perissinotto E , Zucchetto M , et al. Upper limb bone mineral density and body composition measured by peripheral quantitative computed tomography in right-handed adults: the role of the dominance effect . J Endocrinol Invest . 2009 ; 32 ( 4 ): 298 – 302 . Crossref PubMed Google Scholar
32. Taaffe DR , Pruitt L , Reim J , et al. Effect of recombinant human growth hormone on the muscle strength response to resistance exercise in elderly men . J Clin Endocrinol Metab . 1994 ; 79 ( 5 ): 1361 – 1366 . Crossref PubMed Google Scholar
33. Mole PA , McMurdo ME , Paterson CR . Evaluation of peripheral dual energy X-ray absorptiometry: comparison with single photon absorptiometry of the forearm and dual energy X-ray absorptiometry of the spine or femur . Br J Radiol . 1998 ; 71 ( 844 ): 427 – 432 . Google Scholar
Author contributions
G. Robertson: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing.
R. Wallace: Formal analysis, Investigation, Methodology, Software, Validation, Writing - review & editing.
A. H. R. W. Simpson: Conceptualization, Investigation, Methodology, Resources, Supervision, Writing – review & editing.
S. P. Dawson: Conceptualization, Formal analysis, Methodology, Software, Validation, Writing – review & editing.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
A. H. R. W. Simpson is Editor-in-Chief of Bone & Joint Research.
Acknowledgements
The authors would like to acknowledge the radiography staff at the Royal Infirmary of Edinburgh for their help in producing the radiographs for the study.
Ethical review statement
Ethical approval was obtained from the South East Scotland (NHS Lothian) Research Ethics Committee to assess an additional region (i.e. the wrist) during the routine DXA examination.
Supplementary material
Includes the formulae for the combined cortical measure scores, and a table showing the Pearson correlation coefficient values between the forearm cortical measures and the dual-energy X-ray absorptiometry values.









