Abstract
Aims
Unicompartmental knee arthroplasty (UKA) has become a popular method of treating knee localized osteoarthritis (OA). Additionally, the posterior cruciate ligament (PCL) is essential to maintaining the physiological kinematics and functions of the knee joint. Considering these factors, the purpose of this study was to investigate the biomechanical effects on PCL-deficient knees in medial UKA.
Methods
Computational simulations of five subject-specific models were performed for intact and PCL-deficient UKA with tibial slopes. Anteroposterior (AP) kinematics and contact stresses of the patellofemoral (PF) joint and the articular cartilage were evaluated under the deep-knee-bend condition.
Results
As compared to intact UKA, there was no significant difference in AP translation in PCL-deficient UKA with a low flexion angle, but AP translation significantly increased in the PCL-deficient UKA with high flexion angles. Additionally, the increased AP translation became decreased as the posterior tibial slope increased. The contact stress in the PF joint and the articular cartilage significantly increased in the PCL-deficient UKA, as compared to the intact UKA. Additionally, the increased posterior tibial slope resulted in a significant decrease in the contact stress on PF joint but significantly increased the contact stresses on the articular cartilage.
Conclusion
Our results showed that the posterior stability for low flexion activities in PCL-deficient UKA remained unaffected; however, the posterior stability for high flexion activities was affected. This indicates that a functional PCL is required to ensure normal stability in UKA. Additionally, posterior stability and PF joint may reduce the overall risk of progressive OA by increasing the posterior tibial slope. However, the excessive posterior tibial slope must be avoided.
Cite this article: Bone Joint Res 2020;9(9):593–600.
Article focus
-
The effect of tibial slope on the stability of medial unicompartmental knee arthroplasty (UKA) in posterior cruciate ligament (PCL)-deficient knees.
Key messages
-
The tibial slope affects the posterior kinematics and contact stress on a knee joint in the PCL-deficient UKA. The proper slope of the posterior tibia helps the stability of PCL-deficient UKA under deep-knee-bend condition.
Strengths and limitations
-
This study showed that the posterior tibial slope has a significant impact on the posterior kinematics and contact stress in PCL-deficient UKA.
-
We did not compare the actual clinical data for AP translation and contact stress.
Introduction
Unicompartmental knee arthroplasty (UKA) has been proven as a suitable surgical technique to treat unilateral osteoarthritis (OA) of knee joints, and this method has recently become popular.1-4 A greater postoperative range of motion (ROM) and the preservation of normal kinematic functions relative to total knee arthroplasty (TKA) are the functional advantages of UKA.5-9 However, less than 10% of all primary knee arthroplasties are performed using UKA, even if half of these patients are potential candidates for UKA.5
In general, the ideal patient for medial UKA is the patient suffering from medial unicompartmental knee OA with four major intact ligaments in the knee joints.10 In addition, a preserved ROM, comparable young age (more than 60 years), and low weight and activity levels are considered to be indicators for medial UKA.11-15 In addition, the medial UKA with deficient cruciate or collateral ligaments could lead to secondary opposite compartmental OA and early loosening of the implant.10 Therefore, many orthopaedic surgeons do not perform medial UKA if the ligaments are unstable; however, there is no general consensus on whether or not this is the appropriate practice.10
In the native knee, the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) are essential to maintaining the kinematics and stability in knee joints.16 During neutral tibial rotation, the ACL and PCL are the primary restraints for the anterior and posterior drawers, respectively.16 During mid-flexion, the ACL and PCL provide knee joint stability, and during high flexion the PCL is responsible for posterior femoral rollback.16-18 Ventura et al19 showed that UKA combined with ACL reconstruction is an effective therapeutic option for the treatment of combined medial unicompartmental knee OA and ACL deficiency, and confirms subjective and objective clinical improvement up to eight years after surgery. However, long-term results suggest that an insufficient PCL may promote the development of OA in knee joints due to excessive displacements between the tibia and femur. As the number of people undergoing UKA increases, high flexion activities must be carefully considered.20-22
A previous study has evaluated the effect of the tibial slope on knee stability.23,24 It has been shown that an increased tibial slope in UKA can increase anteroposterior (AP) tibiofemoral (TF) translation as well as the risk of ACL injuries.25
However, a majority of these studies focused on the effect of the posterior tibial slope on the ACL in deficient UKA.25-27 To the best of our knowledge, very few studies have focused on the effect of the slope on the PCL. In addition, finite element (FE) analysis can be used to evaluate biomechanical effect in PCL-deficient UKA with respect to posterior tibial slope. Using FE analysis for accurate in silico evaluations of UKA is valuable for clinical assessment.28,29
Therefore, the purpose of this study was to evaluate the biomechanical effect on PCL-deficient knees in medial UKA, with respect to different posterior tibial slopes. It was hypothesized that an increased posterior tibial slope facilitates positive biomechanical effects in PCL-deficient UKA.
Methods
Computational model
A previously validated FE model of an intact knee joint was employed in this study to address our two main research questions (Figure 1).30–33 First, what biomechanical effect can the PCL-deficient UKA provide as compared to the intact PCL and the intact UKA? Second, how does an increased posterior tibial slope affect the kinematics and contact stress of the patellofemoral (PF) joint and tibial cartilage? The computational models of the intact knee consisted of subject-specific geometries of the bony structure, articular cartilage, and menisci obtained from the CT and MRI images of four male subjects (Subject 1: age 36 years, height 178 cm, mass 75 kg; Subject 2: age 34 years, height 173 cm, mass 83 kg; Subject 3: age 32 years, height 182 cm, mass 79 kg; Subject 4: age 34 years, height 173 cm, mass 71 kg) and a female subject (Subject 5: age 26 years, height 163 cm, mass 65 kg). The bony structures were modelled in rigid body. In addition, the major ligaments were modelled using non-linear and tension-only spring elements.34,35 ACL was assumed to be normal. The interfaces between the cartilage and the bones were modelled to be completely bonded. The contacts between the femoral cartilage and the meniscus, the meniscus and the tibial cartilage, and the femoral and tibial cartilages were modelled for the medial and lateral sides in six contact pairs.36 A fixed-bearing UKA (Zimmer, Warsaw, Indiana, USA) was virtually implanted in the medial compartment of the modelled intact knee models. The bone models were imported and appropriately positioned, trimmed, and meshed using rigid elements via surgical techniques.37 The neutrally aligned tibial baseplate was defined as a square (0°) inclination in the coronal plane, with a 5° posterior slope. This is because the subject's anatomy posterior tibial slope was 5°. The rotating axis was defined as a line parallel to the lateral edge of the tibial baseplate and passing through the centre of the femoral component peg. A neutral femoral component distal cut that was perpendicular to the mechanical axis of the femur and parallel to the tibial cut was reproduced. Based on the neutral position, the tibial tray and bearing were rotated about the axis, and five posterior tibial slopes were modelled while maintaining 0° in the coronal plane without changing the height of the joint surface, from 1° to 9° with 2° increments in posterior tibial slope (Figure 2). In addition, the PCL-deficient model and the posterior tibial slopes of models 1°, 3°, 5°, 7°, and 9° were included in this simulation. The polyethylene (PE) insert and the femoral component and tibial baseplate were modelled as elastoplastic and linear elastic isotropic materials, respectively.31,38,39 The materials of the femoral component, PE insert, and tibial baseplate corresponded to a cobalt chromium alloy (CoCr), ultra-high molecular weight polyethylene, and a titanium alloy (Ti6Al4V), respectively (Table I). The femoral component came into contact with the PE insert. The selected coefficient of friction between the PE and metal corresponded to 0.04.39
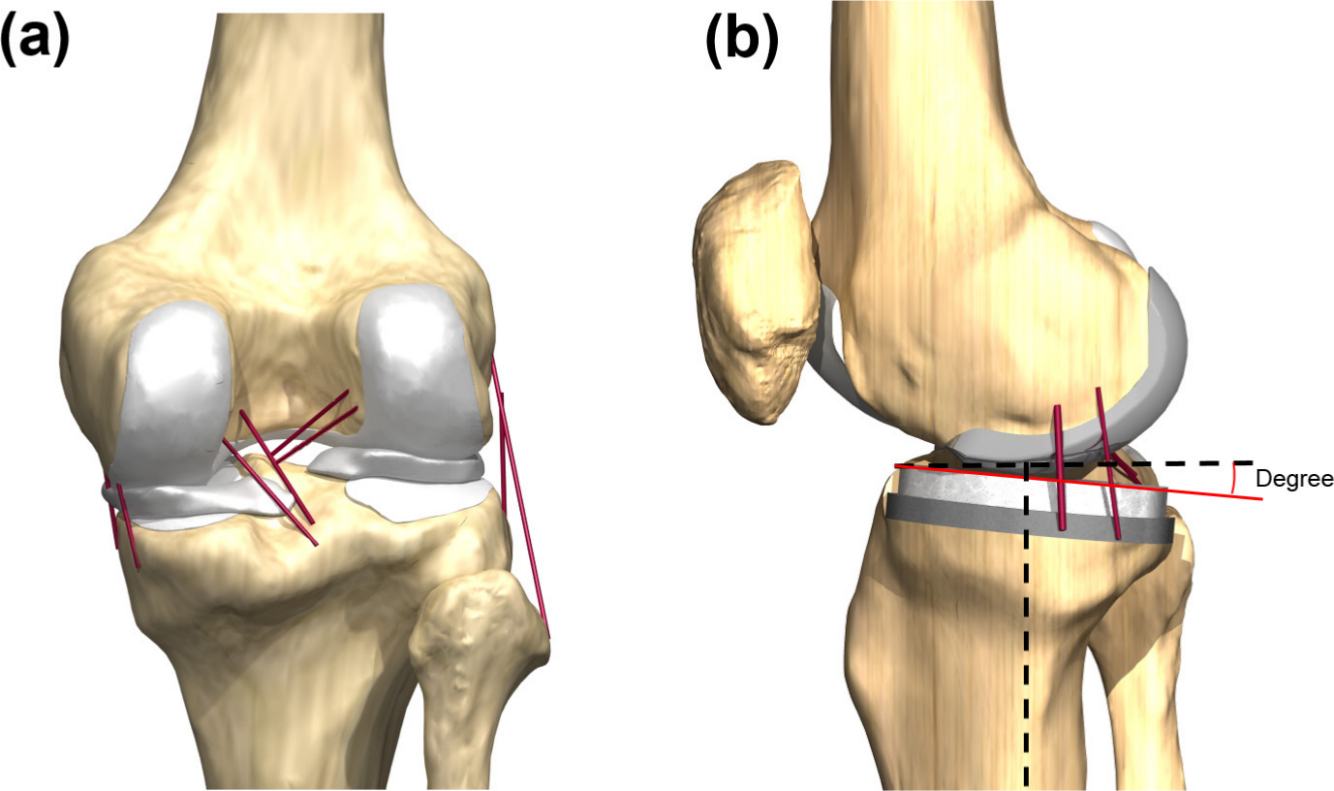
Fig. 1
Finite element models in analysis for a) intact and b) unicompartmental knee arthroplasty (UKA) model.
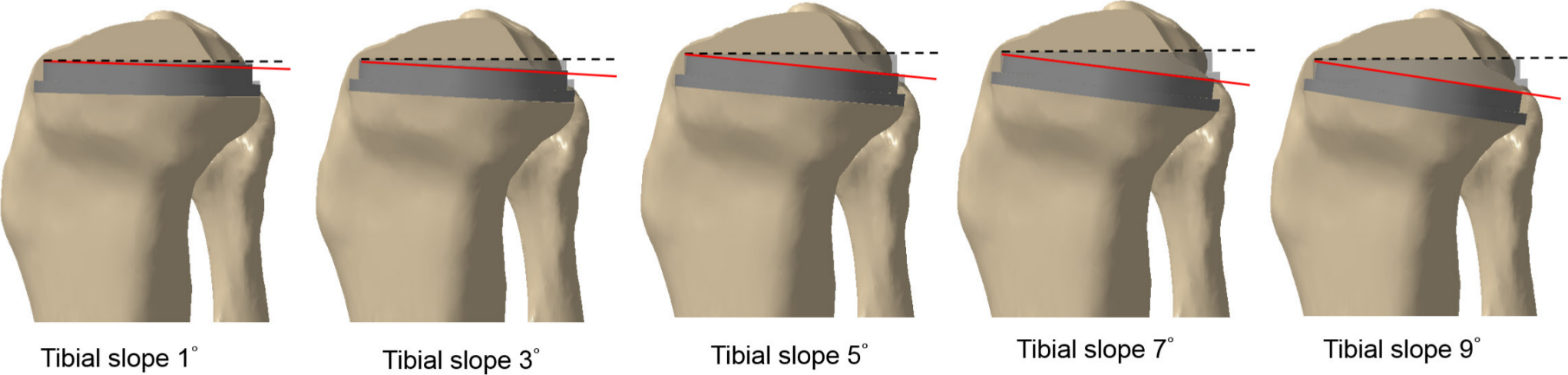
Fig. 2
Depiction of the posterior tibial slope of 1°, 3°, 5°, 7°, and 9°.
Table I.
Material properties of implant.
| Material | Young’s modulus, MPa | Poisson’s ratio |
|---|---|---|
| CoCr alloy | 220,000 | 0.30 |
| UHMWPE | 685 | 0.47 |
| Ti6AI4V alloy | 110,000 | 0.30 |
-
CoCr, cobalt chromium; Ti6AI4V, titanium alloy; UHMWPE, ultra-high molecular weight polyethylene.
The FE simulation included three types of loading conditions corresponding to the loads utilized in the model validation experiment and the predictions of loading scenarios during daily activities. Under the first loading condition, an axial loading of 1,150 N was applied to the model to determine the contact stresses and compare them to those reported in a published FE knee joint study.34 In addition, the validation of the UKA model with posterior tibial slope 50 was performed at flexion angles of 0°, 30°, 60°, and 90° by using a passive flexion simulation. The anterior and posterior drawer loads of 130 N were separately applied to the tibia at the knee centre in a manner similar to that in a previous experimental study.40 The third loading condition, which corresponded to the deep-knee-bend loading, was applied to evaluate knee joint mechanics. A computational simulation was performed to utilize an AP force applied to the femur, based on the compressive load applied to the hip with constrained femoral internal-external (IE) rotation, free medial-lateral translation, and knee flexion based on a combination of vertical hip and quadriceps loads. Thus, a six-degrees-of-freedom TF joint was developed.41,42 A proportional-integral-derivative controller was incorporated into the computational model to control the quadriceps in a manner similar to that utilized in a previous experiment.18 A control system was utilized to evaluate the instantaneous displacement of the quadriceps muscles to match the same target flexion profile as in the experiment. Furthermore, IE and varus-valgus torques were applied to the tibia, and the remaining tibial degrees of freedom were constrained. The FE model was analyzed using ABAQUS software (version 6.11; Simulia, Providence, Rhode Island, USA). The kinematics and contact stress of the articular cartilage in the TF joint were evaluated. The kinematics were based on Grood and Suntay’s definition of a joint coordinate system.43
Statistical analysis
In this study, we had performed the test to divide into 11 timepoints (0.0 to 1.0 phases) for single cycles of the deep-knee-bend loading conditions. To evaluate the models with various degrees of posterior tibial slope, each model’s condition was compared to the UKA’s intact model in a pairwise manner using non-parametric repeated-measure Friedman tests at each phase of the cycle. This study used a Mann-Whitney U test with Holm correction for the posthoc comparisons, to control the familywise error rate for the tests conducted within each phase of the cycle. Statistical analyses were performed using SPSS for Windows (version 20.0.0; IBM, Armonk, New York, USA). Statistical significance was set at p < 0.05 for all comparisons.
Results
Validation of intact and UKA models
For the validation of the five intact models, the contact stress acting on the menisci was compared with previous results.34 The mean contact stresses on the medial and lateral menisci were 3.1 MPa (SD 0.4) and 1.53 MPa (SD 0.6), respectively, under an axial load of 1,150 N. These values were within a mean 4% of the contact stresses reported in a study conducted by Peña et al,34 i.e. 2.9 MPa and 1.45 MPa, respectively. These minor differences can be attributed to the variations in geometry, such as the differences in the thicknesses of the cartilage and meniscus. However, the general agreement between the validation results and the results of previous studies proved the potential of the FE model to produce reasonable outcomes. The data from the UKA FE model with posterior tibial slope 50 was compared with previous experimental data for validation. In the anterior drawer test at 130 N, the mean of anterior tibial translations in the UKA model were 6.3 mm, 9.6 mm, 8.4 mm, and 8.4 mm, and those in the posterior drawer test were 6.0 mm, 4.2 mm, 3.6 mm, and 4.8 mm at knee flexion angles of 0°, 30°, 60°, and 90°, respectively (Figure 3).
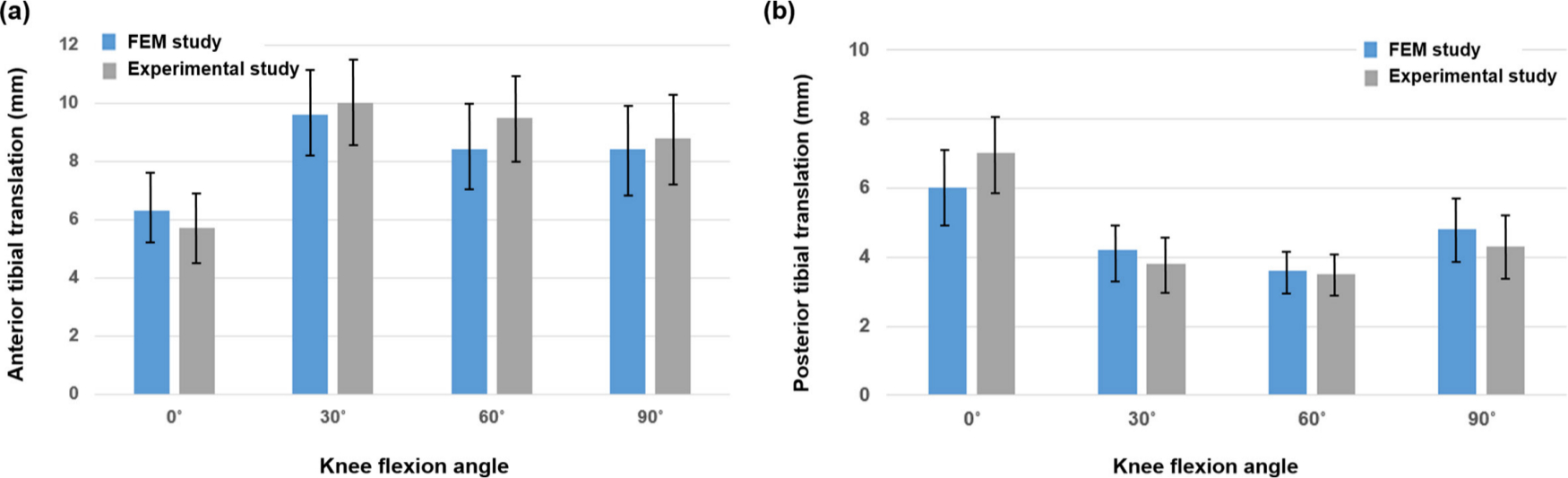
Fig. 3
Comparison of a) the anterior tibial translation and b) the posterior tibial translation for finite element method (FEM) and experiment study.
These results showed a good agreement with the results from previous experimental data within the ranges of values under anterior and posterior drawer loading conditions.
Comparison of the kinematics and the contact stress in the intact and PCL-deficient UKA models during the deep-knee-bend condition
The kinematics and contact stresses of the PF joint and the articular cartilage obtained via the UKA and PCL-deficient UKA models were compared with respect to different posterior tibial slopes.
Figure 4 presents the posterior kinematics in the intact PCL and PCL-deficient UKAs, with respect to different posterior tibial slopes under the deep-knee-bend loading conditions. It can be seen that there is no significant difference in AP translation between the intact and PCL-deficient UKAs for low flexion activities. However, significantly increased AP translation was observed in the PCL-deficient UKA for high flexion activities. In the PCL-deficient UKAs, AP translation decreased as the posterior tibial slope increased and vice versa.
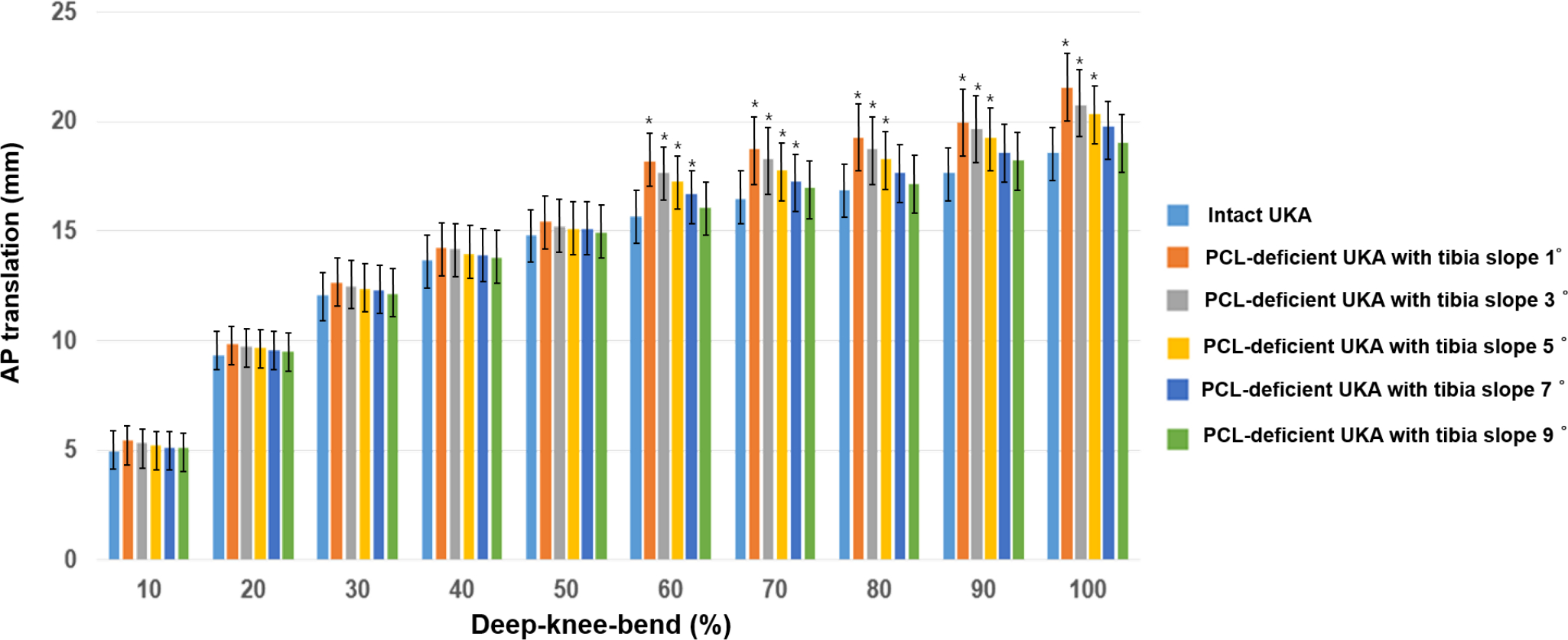
Fig. 4
Comparison of the anteroposterior (AP) translation in the intact model and posterior cruciate ligament (PCL)-deficient unicompartmental knee arthroplasties (UKAs), with respect to different posterior tibial slopes under the deep-knee-bend conditions. *p < 0.05.
Figure 5 shows the contact stress of the PF joint and the articular cartilage in the intact PCL and PCL-deficient UKAs, with respect to different posterior tibial slopes under the deep-knee-bend loading conditions. There was a significantly increased contact stress on the PF joint and the articular cartilage in the PCL-deficient UKA, as compared to the intact PCL UKA. In addition, the contact stress on the PF joint significantly decreased as the posterior tibial slope increased.
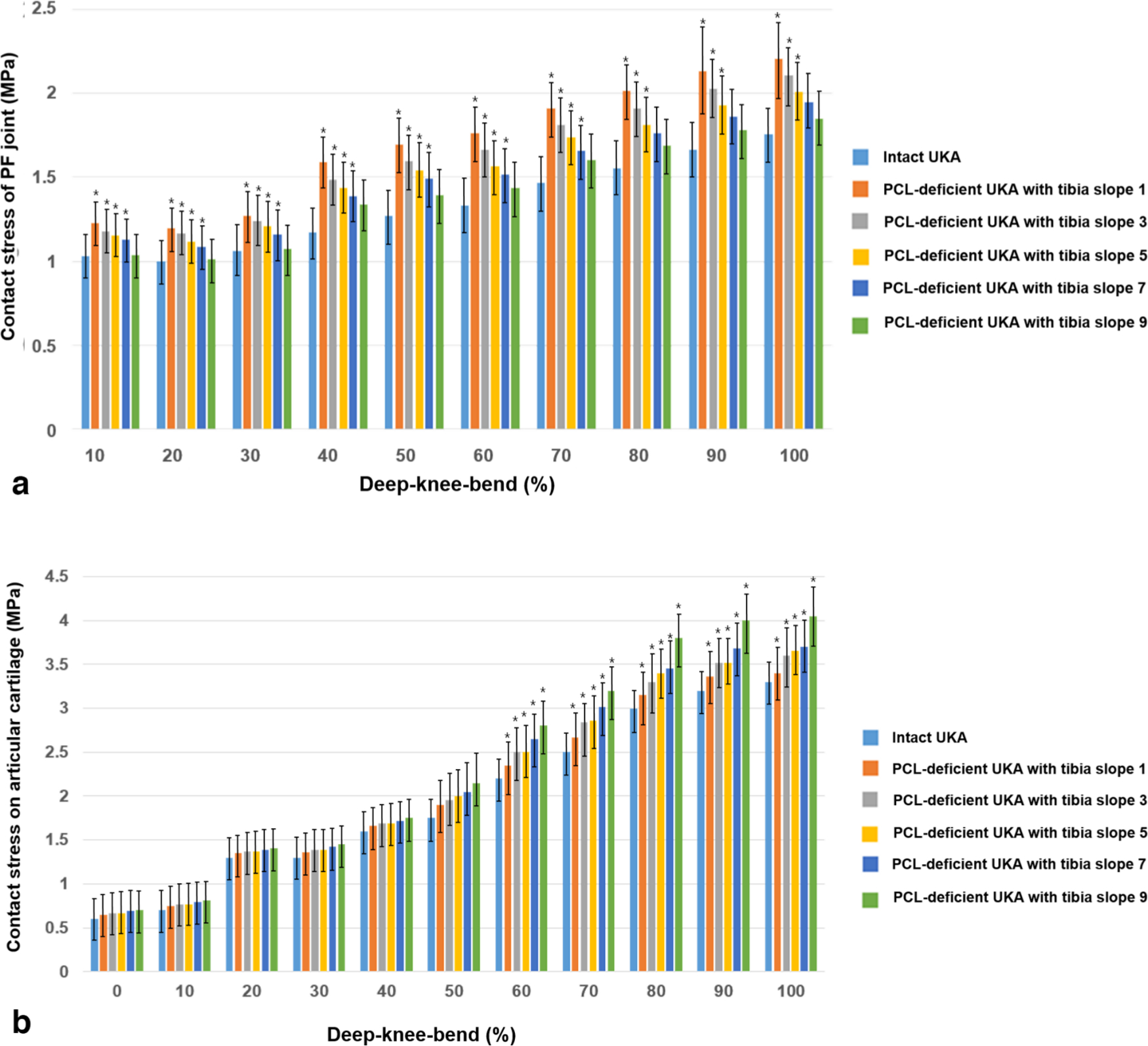
Fig. 5
Comparison of the contact stress on a) patellofemoral (PF) joint and b) articular cartilage in the intact unicompartmental knee arthroplasty (UKA) and posterior cruciate ligament (PCL)-deficient UKA models with respect to different posterior tibial slopes under the deep-knee-bend conditions. *p < 0.05.
Discussion
The most important finding of this study was that there was a significantly increased AP translation in the PCL-deficient UKA, as compared to the intact PCL UKA. In particular, it was found that the deficiency of the PCL may affect posterior stability in UKA for the high flexion activities. In addition, the contact stress on the PF joint and articular cartilage significantly increased for PCL-deficient UKA. This may increase the overall risk of progressive OA on the PF joint and the articular cartilage after UKA. Posterior stability can be ensured as the AP translation decreased on increasing the posterior tibial slope in the PCL-deficient UKA, and this may increase the overall risk of progressive OA as the contact stress on the PF joint decreased. However, an increase in the posterior tibial slope caused the contact stress on the articular cartilage to increase. Therefore, our hypothesis was partially accepted.
To the best of our knowledge, this study is the first attempt to investigate the effect of PCL-deficient UKA on knee joint mechanics. The intact and UKA models are the foundation of this study and involve a series of validation steps. The results exhibit a good agreement with those of a previous computational study.34 In addition, the UKA models were validated based on a previous experimental study.40 Therefore, the UKA models used in this study and the following analyses are considered to be reasonable. Furthermore, the contact stress on the articular cartilage and the kinematics are consistent with the results reported in previous studies.44,45 In addition, this study has two strengths compared to other studies. First, in contrast to those of previous UKA studies, the tibia, femur, and related soft tissues were included in the FE model. Second, in contrast to current biomechanical UKA models, the model used in this study included the deep-knee-bend loading as opposed to simple vertical static loading conditions.
The PCL is the primary restraint to AP translation of the tibia relative to the femur.46 This restraining function is most pronounced at a flexion angle of 90° as the secondary restraints to posterior tibial displacement, such as the posterolateral corner structures and the posteromedial capsule, become lax and cannot serve as effective checkreins during flexion.47
At full extension and low flexion, there was no significant difference in the PCL-deficient knee joints for the TF kinematics. As PCL is a functional restraint to AP translation during flexion, a limited effect of the deficient PCL might be observed during the low flexion activity.10 However, AP translation significantly increased in the PCL-deficient UKA, as compared to that in the intact condition, as flexion angle increased. Thus, it was proved that PCL injury significantly influences posterior stability during high flexion in UKA.44 Our results showed that an increased posterior tibial slope maintained posterior stability in PCL-deficient UKA. This implies that decreased posterior tibial slope maintains anterior stability in the ACL-deficient UKA.25 Theoretically, an increased posterior tibial slope may impart translational stability to PCL-deficient UKA.
The PF joint plays an important role in the function of a knee joint, especially during high flexion activities. The malfunctioning of PF joints has been associated with problems related to the extensor mechanism in UKA. In particular, high PF contact forces have been associated with wear and loosening as well as anterior knee pain and cartilage degeneration.48 Our results showed that the mean contact stress on the PF joint was higher in the PCL-deficient UKA compared with the intact PCL UKA. In addition, the contact stress on the PF joint decreased as the posterior tibial slope increased. In this study, an increase of 9° in the posterior slope led to a mean 15% decrease in the contact stress on the PF joint. Increasing the tibial posterior slope induced a more posterior position of the femoral component. A more posterior contact position in the TF joint leads to an increase in the quadriceps lever arm, which improves the movement efficiency, thereby reducing the contact stress on the PF joint. Therefore, increasing the tibial posterior slope can be expected to reduce PF contact stress required to perform deep-knee-bend activity. In addition, such a decrease of contact stress on PF joint was found more in high flexion activity.
These results of the contact stress on the articular cartilage are noteworthy. The contact stress significantly increased in PCL-deficient UKA, as compared to that in intact PCL UKA, similar to the PF joint. There was no significant difference in the contact stress on the articular cartilage of the PCL-deficient and intact PCL UKA during low flexion activities. This indicates that the deficiency of PCL does not affect the contact stress on the articular cartilage during low flexion activities, which is similar to the results reported in a previous study.10
However, unlike the contact stress on the PF joint, the increase in the posterior tibial slope caused the contact stress on the articular cartilage to increase. This was similar to the result of a previous study.49 Our results showed that posterior stability can be ensured and the contact stress on the PF joint can be decreased on increasing the posterior tibial slope in the PCL-deficient UKA. However, this may increase the contact stress on the articular cartilage. As the data were obtained under the deep-knee-bending condition, we advise caution when extrapolating the data to other functional activities. However, we believe that these findings might be useful for the design of improved treatment protocols for PCL-deficient UKA. As we did not detect any differences in the biomechanical effects between the intact and PCL-deficient UKA under the deep-knee-bend between flexion angles of 0° and 60°, our findings suggest that rehabilitation exercises might be safely performed in this ROM. However, subjects suffering from PCL deficiency should avoid repetitive deep-knee-bend activities.
There are a few limitations to this study. First, although we performed statistical analysis for five subjects, the knee joint models do not capture the variations in bony and articular morphologies as well as ligament shapes and mechanical properties across a population. However, the computational simulation is advantageous for the evaluation of the effects of the UKA with deficient PCL on the posterior tibial slope for the same person, and elimination of the effects of other variables such as weight, height, bony geometry, ligament properties, and component size.50 Second, the biphasic properties of the articular soft tissue were not modelled; however, the response of nearly incompressible elastic materials can be equivalent over short loading periods.51 Finally, this computational simulation only considered the deep-knee-bend loading condition, and future studies should focus on models incorporating actions such as rising/sitting on chairs, climbing/descending stairs, or gait cycle. However, the simulation was performed under the deep-knee-bending condition because this included a wide range of flexion-extension and significant muscular endeavour around the knee joint.50
In conclusion, our result showed that the posterior stability in low flexion activities for PCL-deficient UKA is not affected; however, the posterior stability in high flexion activities was affected. This indicates that a functional PCL is required to ensure normal stability in UKA. In addition, posterior stability and PF joint may reduce the overall risk of progressive OA by increasing the posterior tibial slope. However, this increases the contact stress on the articular cartilage. Therefore, excessive posterior tibial slope must be avoided.
References
1. Murray DW , Goodfellow JW , O'Connor JJ . The Oxford medial unicompartmental arthroplasty: a ten-year survival study . J Bone Joint Surg Br . 1998 ; 80-B ( 6 ): 983 – 989 . Crossref PubMed Google Scholar
2. Pandit H , Jenkins C , Barker K , Dodd CAF , Murray DW . The Oxford medial unicompartmental knee replacement using a minimally-invasive approach . J Bone Joint Surg Br . 2006 ; 88-B ( 1 ): 54 – 60 . Crossref PubMed Google Scholar
3. Mohammad HR , Campi S , Kennedy JA , et al. Long-term in vivo wear of different bearing types used for the Oxford Unicompartmental Knee Replacement . Bone Joint Res . 2019 ; 8 ( 11 ): 535 – 543 . Crossref PubMed Google Scholar
4. Roussot MA , Haddad FS . The evolution and role of patellofemoral joint arthroplasty: The road less travelled, but not forgotten . Bone Joint Res . 2018 ; 7 ( 12 ): 636 – 638 . Google Scholar
5. Jones LD , Palmer J , Jackson WF . Unicompartmental knee arthroplasty . Orthopaed Trauma . 2017 ; 31 ( 1 ): 8 – 15 . Crossref PubMed Google Scholar
6. Longo UG , Loppini M , Trovato U , et al. No difference between unicompartmental versus total knee arthroplasty for the management of medial osteoarthtritis of the knee in the same patient: a systematic review and pooling data analysis . Br Med Bull . 2015 ; 114 ( 1 ): 65 – 73 . Crossref PubMed Google Scholar
7. Mancuso F , Dodd CA , Murray DW , Pandit H . Medial unicompartmental knee arthroplasty in the ACL-deficient knee . J Orthop Traumatol . 2016 ; 17 ( 3 ): 267 – 275 . Crossref PubMed Google Scholar
8. Sekiguchi K , Nakamura S , Kuriyama S , et al. Effect of tibial component alignment on knee kinematics and ligament tension in medial unicompartmental knee arthroplasty . Bone Joint Res . 2019 ; 8 ( 3 ): 126 – 135 . Crossref PubMed Google Scholar
9. Danese I , Pankaj P , Scott CEH . Infographic: impact of implant materials and malalignment in unicompartmental knee arthroplasty . Bone Joint Res . 2019 ; 8 ( 6 ): 226 – 227 . Crossref PubMed Google Scholar
10. Kwon HM , Kang K-T , Kim JH , Park KK . Medial unicompartmental knee arthroplasty to patients with a ligamentous deficiency can cause biomechanically poor outcomes . Knee Surg Sports Traumatol Arthrosc . 2020 ; 28 ( 9 ): 2846-2853 . (Epub ahead of print) PMID: 31346669 . Crossref PubMed Google Scholar
11. Kozinn SC , Scott R . Unicondylar knee arthroplasty . J Bone Joint Surg Am . 1989 ; 71-A ( 1 ): 145 – 150 . PubMed Google Scholar
12. Kuroda Y , Takayama K , Ishida K , et al. Medial joint line elevation of the tibia measured during surgery has a significant correlation with the limb alignment changes following medial unicompartmental knee arthroplasty . Knee Surg Sports Traumatol Arthrosc . 2018 ; 26 ( 11 ): 3468 – 3473 . Crossref PubMed Google Scholar
13. Kwon H , Yang IH , Lee WS , et al. Reliability of intraoperative knee range of motion measurements by Goniometer compared with robot-assisted arthroplasty . J Knee Surg . 2019 ; 32 ( 03 ): 233 – 238 . Crossref PubMed Google Scholar
14. Danese I , Pankaj P , Scott CEH . The effect of malalignment on proximal tibial strain in fixed-bearing unicompartmental knee arthroplasty: A comparison between metal-backed and all-polyethylene components using a validated finite element model . Bone Joint Res . 2019 ; 8 ( 2 ): 55 – 64 . Crossref PubMed Google Scholar
15. Kayani B , Haddad FS . Robotic unicompartmental knee arthroplasty: current challenges and future perspectives . Bone Joint Res . 2019 ; 8 ( 6 ): 228 – 231 . Crossref PubMed Google Scholar
16. Butler DL , Noyes FR , Grood ES . Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study . J Bone Joint Surg Am . 1980 ; 62-A ( 2 ): 259 – 270 . PubMed Google Scholar
17. Suter L , Roth A , Angst M , et al. Is ACL deficiency always a contraindication for medial UKA? Kinematic and kinetic analysis of implanted and contralateral knees . Gait Posture . 2019 ; 68 : 244 – 251 . Crossref PubMed Google Scholar
18. Kang KT , Koh YG , Son J , et al. Finite element analysis of the biomechanical effects of 3 posterolateral corner reconstruction techniques for the knee joint . Arthroscopy . 2017 ; 33 ( 8 ): 1537 – 1550 . Crossref PubMed Google Scholar
19. Ventura A , Legnani C , Terzaghi C , Macchi V , Borgo E . Unicompartmental knee replacement combined to anterior cruciate ligament reconstruction: midterm results . J Knee Surg . 2019 . (Epub ahead of print) PMID: 31269529 . Crossref PubMed Google Scholar
20. Allen CR , Kaplan LD , Fluhme DJ , Harner CD . Posterior cruciate ligament injuries . Curr Opin Rheumatol . 2002 ; 14 ( 2 ): 142 – 149 . PubMed Google Scholar
21. Clancy WG , Shelbourne KD , Zoellner GB , et al. Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure . J Bone Joint Surg Am . 1983 ; 65-A ( 3 ): 310 – 322 . PubMed Google Scholar
22. Dejour H , Walch G , Peyrot J , Eberhard P . [The natural history of rupture of the posterior cruciate ligament] . Rev Chir Orthop Reparatrice Appar Mot . 1988 ; 74 ( 1 ): 35 – 43 . (Article in French).PubMed Google Scholar
23. Giffin JR , Stabile KJ , Zantop T , et al. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee . Am J Sports Med . 2007 ; 35 ( 9 ): 1443 – 1449 . Crossref PubMed Google Scholar
24. Giffin JR , Vogrin TM , Zantop T , Woo SL , Harner CD . Effects of increasing tibial slope on the biomechanics of the knee . Am J Sports Med . 2004 ; 32 ( 2 ): 376 – 382 . Crossref PubMed Google Scholar
25. Hernigou P , Deschamps G . Posterior slope of the tibial implant and the outcome of unicompartmental knee arthroplasty . J Bone Joint Surg Am . 2004 ; 86-A ( 3 ): 506 – 511 . Crossref PubMed Google Scholar
26. Adulkasem N , Rojanasthien S , Siripocaratana N , Limmahakhun S . Posterior tibial slope modification in osteoarthritis knees with different ACL conditions: cadaveric study of fixed-bearing UKA . J Orthop Surg . 2019 ; 27 ( 2 ): 230949901983628 . Crossref PubMed Google Scholar
27. Engh GA , Ammeen DJ . Unicondylar arthroplasty in knees with deficient anterior cruciate ligaments . Clin Orthop Relat Res . 2014 ; 472 ( 1 ): 73 – 77 . Crossref PubMed Google Scholar
28. Kwon OR , Kang KT , Son J , et al. Importance of joint line preservation in unicompartmental knee arthroplasty: finite element analysis . J Orthop Res . 2017 ; 35 ( 2 ): 347 – 352 . Crossref PubMed Google Scholar
29. Campi S , Mellon SJ , Ridley D , et al. Optimal interference of the tibial component of the cementless Oxford Unicompartmental knee replacement . Bone Joint Res . 2018 ; 7 ( 3 ): 226 – 231 . Crossref PubMed Google Scholar
30. Kang KT , Son J , Koh YG , et al. Effect of femoral component position on biomechanical outcomes of unicompartmental knee arthroplasty . Knee . 2018 ; 25 ( 3 ): 491 – 498 . Crossref PubMed Google Scholar
31. Koh YG , Lee JA , Lee HY , et al. Anatomy-mimetic design preserves natural kinematics of knee joint in patient-specific mobile-bearing unicompartmental knee arthroplasty . Knee Surg Sports Traumatol Arthrosc . 2020 ; 28 ( 5 ): 1465 – 1472 . Crossref PubMed Google Scholar
32. Kang KT , Son J , Suh DS , et al. Patient-specific medial unicompartmental knee arthroplasty has a greater protective effect on articular cartilage in the lateral compartment: A Finite Element Analysis . Bone Joint Res . 2018 ; 7 ( 1 ): 20 – 27 . Crossref PubMed Google Scholar
33. Koh YG , Lee JA , Lee HY , et al. Reduction in tibiofemoral conformity in lateral unicompartmental knee arthroplasty is more representative of normal knee kinematics . Bone Joint Res . 2019 ; 8 ( 12 ): 593 – 600 . Crossref PubMed Google Scholar
34. Peña E , Calvo B , Martinez MA , Palanca D , Doblaré M . Why lateral meniscectomy is more dangerous than medial meniscectomy. A finite element study . J Orthop Res . 2006 ; 24 ( 5 ): 1001 – 1010 . Crossref PubMed Google Scholar
35. Mesfar W , Shirazi-Adl A . Biomechanics of the knee joint in flexion under various quadriceps forces . Knee . 2005 ; 12 ( 6 ): 424 – 434 . Crossref PubMed Google Scholar
36. Kang KT , Kim SH , Son J , Lee YH , Chun HJ . Computational model-based probabilistic analysis of in vivo material properties for ligament stiffness using the laxity test and computed tomography . J Mater Sci Mater Med . 2016 ; 27 ( 12 ): 183 . Crossref PubMed Google Scholar
37. No authors listed . Zimmer Unicompartmental high flex knee: intramedullary, spacer block option and extramedullary minimally invasive surgical techniques . Zimmer . 2005 . http://www.rpa.spot.pt/getdoc/bdb307b0-1a13-4284-9c62-a61c429b283b/ZUK.aspx (date last accessed 14 August 2020 ). Google Scholar
38. Inoue S , Akagi M , Asada S , et al. The Valgus Inclination of the Tibial Component Increases the Risk of Medial Tibial Condylar Fractures in Unicompartmental Knee Arthroplasty . J Arthroplasty . 2016 ; 31 ( 9 ): 2025 – 2030 . Crossref PubMed Google Scholar
39. Godest AC , Beaugonin M , Haug E , Taylor M , Gregson PJ . Simulation of a knee joint replacement during a gait cycle using explicit finite element analysis . J Biomech . 2002 ; 35 ( 2 ): 267 – 275 . Crossref PubMed Google Scholar
40. Suggs JF , Li G , Park SE , et al. Function of the anterior cruciate ligament after unicompartmental knee arthroplasty: an in vitro robotic study . J Arthroplasty . 2004 ; 19 ( 2 ): 224 – 229 . Crossref PubMed Google Scholar
41. Halloran JP , Clary CW , Maletsky LP , et al. Verification of predicted knee replacement kinematics during simulated gait in the Kansas knee simulator . J Biomech Eng . 2010 ; 132 ( 8 ): 081010 . Crossref PubMed Google Scholar
42. Kutzner I , Heinlein B , Graichen F , et al. Loading of the knee joint during activities of daily living measured in vivo in five subjects . J Biomech . 2010 ; 43 ( 11 ): 2164 – 2173 . Crossref PubMed Google Scholar
43. Grood ES , Suntay WJ . A joint coordinate system for the clinical description of three-dimensional motions: application to the knee . J Biomech Eng . 1983 ; 105 ( 2 ): 136 – 144 . Crossref PubMed Google Scholar
44. Kang KT , Koh YG , Son J , et al. Biomechanical influence of deficient posterolateral corner structures on knee joint kinematics: A computational study . J Orthop Res . 2018 . (Epub ahead of print) PMID: 29436742. . Crossref PubMed Google Scholar
45. Koh YG , Park KM , Kang KT . Influence of Preservation of Normal Knee Contact Stress on Other Compartments with respect to the Tibial Insert Design for Unicompartmental Knee Arthroplasty . Appl Bionics Biomech . 2019 ; 2019 : 9246379. Crossref PubMed Google Scholar
46. Amis AA , Bull AMJ , Gupte CM , et al. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments . Knee Surg Sports Traumatol Arthrosc . 2003 ; 11 ( 5 ): 271 – 281 . Crossref PubMed Google Scholar
47. Covey DC , Sapega AA . Anatomy and function of the posterior cruciate ligament . Clin Sports Med . 1994 ; 13 ( 3 ): 509 – 518 . PubMed Google Scholar
48. Andriacchi TP , Natarajan RN , Hurwitz DE . Musculoskeletal dynamics: locomotion and clinical applications . In : Mow VC , Hayes WC, eds . Basic Orthopaedic Biomechanics . 2nd ed . New York, New York : Lippincott-Raven , 1997 : 37 – 68 . Google Scholar
49. Kang KT , Park JH , Koh YG , Shin J , Park KK . Biomechanical effects of posterior tibial slope on unicompartmental knee arthroplasty using finite element analysis . Biomed Mater Eng . 2019 ; 30 ( 2 ): 133 – 144 . Crossref PubMed Google Scholar
50. Kang KT , Koh YG , Son J , et al. Influence of increased posterior tibial slope in total knee arthroplasty on knee joint biomechanics: a computational simulation study . J Arthroplasty . 2018 ; 33 ( 2 ): 572 – 579 . Crossref PubMed Google Scholar
51. Ateshian GA , Ellis BJ , Weiss JA . Equivalence between short-time biphasic and incompressible elastic material responses . J Biomech Eng . 2007 ; 129 ( 3 ): 405 – 412 . Crossref PubMed Google Scholar
Author contributions
J-A. Lee: Developed the 3D model and drafted the paper.
Y-G. Koh: Drafted the paper.
P. S. Kim: Evaluated the data.
K. W. Kang: Interpreted the data.
Y. H. Kwak: Supervised the study.
K-T. Kang: Supervised the study.
J-A. Lee and Y-G. Koh are joint first authors.
Y. H. Kwak and K-T. Kang contributed equally to this work.
J-A. Lee and Y-G. Koh contributed equally to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
No external source of funding was received for the study.
Ethical review statement
None required.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









