Abstract
Objectives
A patient-centred approach, usually achieved through shared decision making, has the potential to help improve decision making around knee arthroplasty surgery. However, such an approach requires an understanding of the factors involved in patient decision making. This review’s objective is to systematically examine the qualitative literature surrounding patients’ decision making in knee arthroplasty.
Methods
A systematic literature review using Medline and Embase was conducted to identify qualitative studies that examined patients’ decision making around knee arthroplasty. An aggregated account of what is known about patients’ decision making in knee arthroplasties is provided.
Results
Seven studies with 234 participants in interviews or focus groups are included. Ten themes are replicated across studies, namely: expectations of surgery; coping mechanisms; relationship with clinician; fear; pain; function; psychological implications; social network; previous experience of surgery; and conflict in opinions.
Conclusions
This review is helpful in not only directing future research to areas that are not understood, or require confirmation, but also in highlighting areas that future interventions could address. These include those aimed at delivering information, which are likely to affect the satisfaction rate, demand, and use of knee arthroplasties.
Cite this article: Bone Joint Res 2015;4;163–169.
Article focus
- Patients’ decision making plays a central role in preference-based health decisions.
- This article’s aim is to provide an aggregated account of the factors that influence patients’ decision making when considering total knee arthroplasty.
Key messages
- We identified ten themes that were replicated across studies.
- The themes interact with each other.
- The themes have varying influences across different patients and different healthcare settings.
Strengths and limitations
- Robust and reproducible search criteria were used, accepting the limitations of electronic indexing of qualitative work.
- No synthesis of included studies was conducted. This is a controversial topic, and currently no consensus exists as to the value, or the methods, in qualitative synthesis.
- All included papers only examined patients at one stage in the process of care. The stage of decision making is likely to be an important element in understanding the decision making process.
Introduction
Understanding patients’ decision making has particular relevance during patients’ deliberation over having a knee arthroplasty. It has the potential to improve the information given to patients, patient-centred care, and to inform patient decision aids. Improved pre-operative counselling could help address three problematic areas facing knee arthroplasty services: a high dissatisfaction rate; increasing demand with financial constraints; and a variation in the use of knee arthroplasties.
The rate of dissatisfaction after knee arthroplasty surgery is around 17%, although estimates vary.1 One of the potential factors implicated in the high dissatisfaction rate is patient expectations.2 Patients with unrealistically high expectations may drive a high dissatisfaction rate.2 Understanding how expectations of outcome affect the decision making process may help in understanding the dissatisfaction rate, and may even aid methods to decrease it (particularly interventions aimed at providing information).
There is increasing demand for knee arthroplasties combined with increasing financial pressure.3,4 This is not specific to knee arthroplasties, but if current trends in the use of total knee arthroplasty (TKA) hold true, we are likely to see at least a three-fold increase in demand by 2035.5 Interventions to improve patient-centred care through shared decision making (which requires an understanding of patient decision making) have demonstrated a decrease in the uptake of preference-based elective operations, but no studies have been conducted in knee arthroplasty surgery.6,7
There is a significant amount of variation in the use of knee arthroplasties. Differences in expenditure of almost four fold are demonstrated between Primary Care Trusts with regard to inpatient knee arthroplasty costs - those trusts with the highest expenditure treat patients with the best pre-operative patient-reported outcome measures (PROMs) scores.8 Some of this variation is warranted in that it reflects patient preference: Hawker et al9 report that in some groups of patients only one third that would fulfil a needs assessment would be willing to undergo a joint arthroplasty. However, it is clear that not all the variation is warranted (i.e. due to patient need or preference). For example, orthopaedic surgeons and general practitioners have been reported to be less likely to refer a woman with osteoarthritis (OA) of the knee for knee arthroplasty than they would a man.10 Therefore, the variation observed in utilisation rates is likely to be due in part to patient preference, and an understanding of how patients make decisions about having a TKA should explain some of this variation.
Various attempts at identifying how patients make decisions about knee surgery, and what factors are important to them, have been conducted. Interestingly, many studies have examined both hip and knee patients as one cohort. Additionally, historic attempts at synthesising the qualitative literature on this topic have likewise included both hip and knee patients as one patient group.11 Although there are clear similarities between these groups, there are significant differences that make combining these populations potentially unsound.
Firstly, there is the significant difference in the ‘success’ rate of hip and knee arthroplasties. TKAs have a dissatisfaction rate of around 17%.1,12 Hip arthroplasties have significantly better outcomes regarding satisfaction, pain, and function.13 Ibrahim et al14 examined the influence of expectations as an explanatory factor in some of the variation in utilisation rates of joint arthroplasty, and found that it explains some of the variation. Therefore, knee arthroplasty decision making is likely to be different to that for hip arthroplasties, as the outcome is not the same.
Secondly, the population that develop hip arthritis are different to the population that develop knee arthritis. A recent study including almost 2000 participants found that body mass index (BMI) was correlated with the development and progression of OA of the knee, but not hip OA.15 This is particularly relevant to decision making, as people with higher BMIs display different psychological profiles to the general population.16
Therefore, people who develop hip and knee OA are likely to be different populations, with different psychological profiles. Additionally, the outcome, and therefore expectation, of the operations are different.
An understanding of patients’ decision making will be helpful in not only enabling high quality, patient-centred interactions, but in highlighting areas that future interventions could address (particularly interventions aimed at delivering information).
This review aggregates the qualitative literature surrounding patients’ decision making in knee arthroplasty surgery. The aim of this review was to provide an aggregation of studies (c.f. a synthesis of qualitative studies) – the difference, as Sandelowski, Barroso and Voils17 describe, is accumulation and summary, rather than transformation. This represents an approach consistent with a “lines argument synthesis”, defined as “building up a picture of the whole” and represents what Pantoja described as a realist synthesis with narrative review,18 however, the term synthesis here refers to the combination of results, rather than any second or third order interpretation of them.
Materials and Methods
We conducted a literature search of Medline and Embase in January 2015. Subject and topic terms (Knee, Knee prosthesis, Knee replacement, Knee arthroplasty and Decision making) were included, both as free text and indexed headings. A bibliographic search of all studies retrieved for full text analysis (whether included in the final review or not) was conducted. This search strategy is consistent with that used by the Evidence for Policy and Practice Information Centre.19
Studies that reported qualitative data on the decision making process in knee arthroplasties were included. The lead author selected the relevant papers, and conducted a bibliographic search. All full text papers retrieved were screened by a second author (DB) to provide consensus that papers were reporting qualitative findings on decision making. We did not specifically exclude survey data, however, such papers were required to provide insights into decision making over and above reporting descriptive or inferential statistics. The eligibility criteria were:
Inclusion
- Findings on how and why patients make decisions regarding knee arthroplasty.
- Recognised as qualitative research.
Exclusion
- Knee patients’ decision making not reported separately.
There is controversy over the quality assessment of qualitative literature, with over 100 tools currently available, however, the reliability of these tools is questionable.20 Some authors, claiming that setting standards, or following prescribed formulas, is a fruitless exercise, have questioned the entire process of quality appraisal.19 Therefore, quality assessment of included papers was not undertaken.
Synthesis of the data, which involves some form of transformation, was not performed. There are many different methodologies for the synthesis of qualitative work with differing approaches, inconsistent and confusing nomenclature, and the prolific use of modification of techniques.21 Furthermore, the synthesis of qualitative data is in itself a controversial topic, with some authors questioning if it should be attempted at all.19 Issues surrounding the synthesis include those of mixing methods and researchers.22 However, our aim here was not to synthesise or transform the studies, but to provide a map, or a picture of the whole. This is consistent with approaches described in the literature.17-19,21,22 Our approach involved identifying themes that the authors had recognised as important to decision making. Themes and, where appropriate, sub-themes are reported as per the authors’ classification. Therefore the authors’ own findings, in their own words as far as possible, are reported, and any clear consistencies or inconsistencies are discussed. The lead author completed this process, and the findings were cross-checked by another experienced qualitative researcher (AR).
Results
The electronic database search returned 556 papers. In total, 70 papers remained after a title review, and a further 50 papers were excluded on the basis of their abstract. A further 11 papers were retrieved for full text review from the bibliographic search (total 31 papers full text review). Of these, seven were included in the review. A flow diagram of the included studies is displayed in Figure 1.
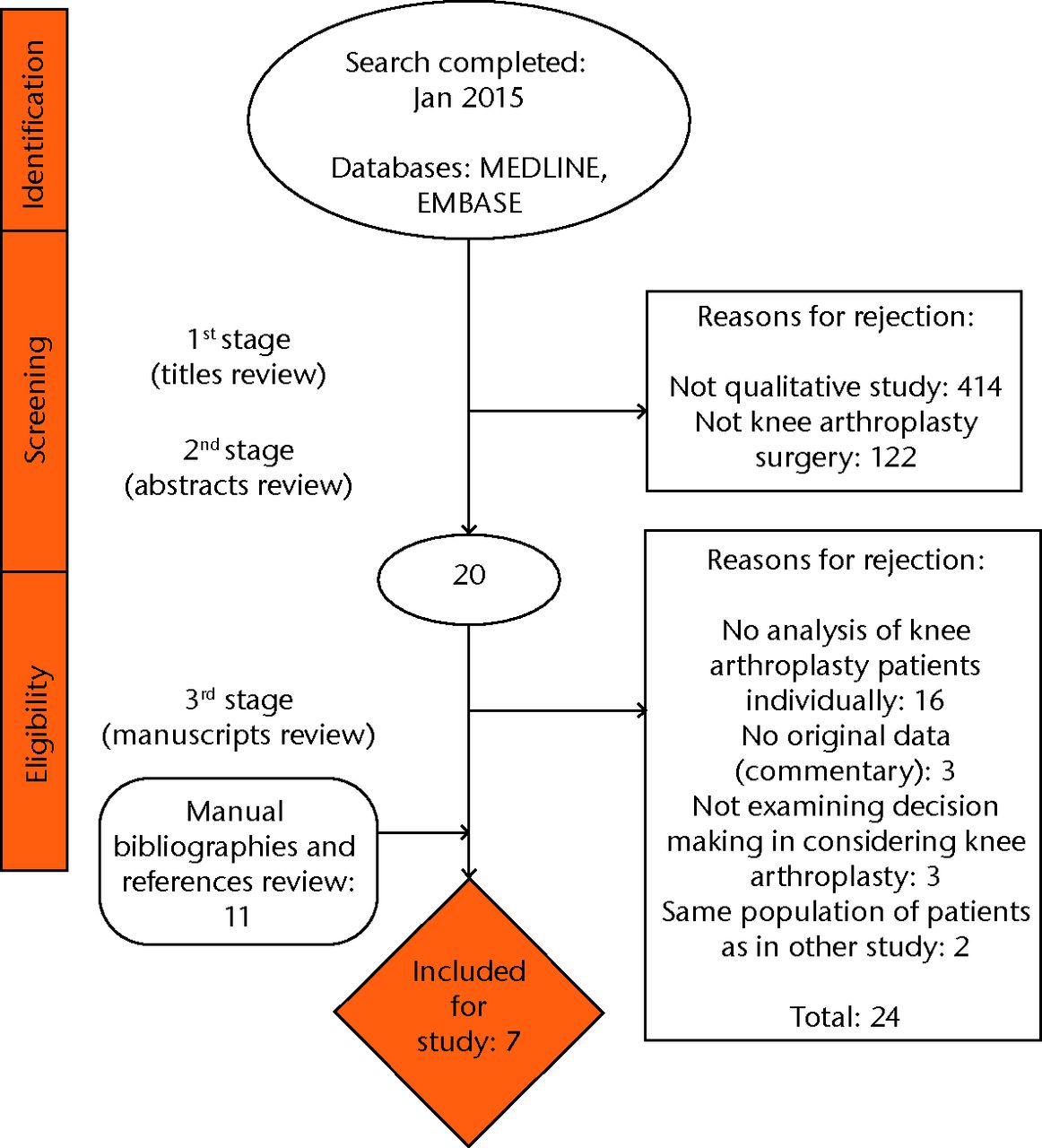
Fig. 1
Flow diagram of included studies
The basic study characteristics can be found in Table I.23-29
Table I
Basic study characteristics
| Author | Title | Setting | Sampling | Participants | Method | Analysis |
|---|---|---|---|---|---|---|
| Figaro et al23 | Preferences for Arthritis Care Amoung Urban African Americans: “I Don’t Want to Be Cut”. | Church or senior centre in Manhatton, New York. | Opt-in recruitment from patients who had pain or stiffness in one or both knees. | A total of 94 African American/black participants, (79 female, 15 male). Mean age 71 years. 82 without and 12 with knee arthroplasty. | Structured interviews | Content analysis using constant comparative method |
| Suarez-Almazor24 | A qualitative Analysis of Decision-Making for Total Knee Replacement in patients with Osteoarthritis. | Primary care setting in United States. | Patients identified as subpopulation of another study, with a diagnosis of knee OA but no TKA. | A total of 37 patients. 13 white, nine Hispanic, 15 African American (14 males, 23 females). Mean age 64 years. | Focus group | Thematic analysis using a grounded theory approach. |
| Chang et al25 | Concerns of Patients Actively Contemplating Total Knee Replacement: Differences by Race and Gender. | Othopaedic surgeon’s office, United States. | Patients actively considering knee arthroplasty. Patients were recruited in sequence of attendance. | A total of 12 male, 25 female: 20 white American, 17 African American. Mean age 60 years. | Focus group | Thematic content analysis |
| Al-Taiar et al26 | Attitudes to knee osteoarthritis and total knee replacement in Arab women: a qualitative study. | The only publicly funded orthopaedic centre in Kuwait. | Patients selected from the waiting list for knee replacement. Process not reported. | A total of 39 Kuwaiti female participants. Mean age 62.5 years. | Semi-structured focus group | Thematic analysis |
| Toye et al27 | Personal meanings in the construction of need for total knee replacement surgery. | Specialist orthopaedic centre, England, UK. | Patient on waiting list for TKA and below average need as judged by WOMAC pain and function score. Invited by letter (opt in). | A total of 18 patients (12 male, six female). Mean age and ethnicity not reported. | Semi-structured interviews | Interpretive phenomenological analysis |
| Woolhead et al28 | Who should have priority for a knee joint replacement? | Three orthopaedic surgeons’ waiting lists, UK. | Patients on the waiting list for knee replacement. Sampling across age and gender by letter (opt in). | A total of 25 participants (14 female, 11 male). Mean age 65 years. | Semi-structured interviews | Constant comparison |
| Marcinkowski et al29 | Getting Back to the Future. A Grounded Theory Study of the Patient Perspective of Total Knee Joint Arthoplasty. | A publicly funded centre in New Zealand. | Purposive sampling by age, gender, comorbidity and complications from patients who had recently had a knee arthroplasty. | A total of nine European New Zealand participants (four male, five female). Mean age 71 years. | Unstructured interview | Constant comparative analysis based in grounded theory |
-
OA, osteoarthritis; TKA, total knee arthroplasty; WOMAC, Western Ontario and McMaster Universities Arthritis Index
Study characteristics
The included studies have examined decision making in a population with knee symptoms but no diagnosis of knee pain,23 patients in primary care with a diagnosis of knee OA,24 patients actively considering knee arthroplasty in secondary care,25 patients on the waiting list,26-28 and recent post-operative patients.29 Of note, two papers had a focus that was not decision making in knee arthroplasties, but reported factors that influenced patients in making a decision, thus, both papers were included.
From the seven studies, four different countries are represented with 234 participants. Study samples range from nine to 94 participants (mean 33 participants). Of the 234 participants, 126 are African American (skewed by one large study of 94 participants),23 with 39 Kuwaiti women, 33 “white” or “white American”, nine European New Zealanders, with two studies (43 participants) not reporting ethnicity. Three studies conducted focus groups, with four conducting interviews. Analysis was reported in a variety of ways, with different nomenclature. In total, 68 out of the 234 participants (29%) were male.
Study themes
A matrix of study themes has been produced, demonstrating where themes overlap, and where they do not. The description of themes is taken from the relevant papers, but summarised where necessary. No synthesis or second order interpretation took place. Some ten themes were identified in more than one study: expectations of surgery; coping mechanisms; relationship with clinician; fear; pain; function; psychological implications; social network; previous experience of surgery; and conflict in opinions.
Expectation of surgery was a theme identified in five of the seven studies. A common finding was the uncertainty surrounding the outcome of a knee arthroplasty.
Four studies identified various patterns of coping mechanisms, which were important in the decision making process. The use of alternative medicine and social support was prevalent. Two studies identified religion as part of the preferred coping mechanism. These mechanisms help people live with OA and therefore predominantly act as deterrents to operative intervention, however, they can also act as stimulators (e.g. social support in helping to make the decision).
The relationship with the clinician was recognised as important in four studies. This was almost universally seen as a major factor in decision making, however, one paper found that trust in physicians was not an important factor. Related to this theme, two papers documented the role of decisional conflict in decision making. Woolhead et al,28 who examined patients’ views on prioritisation for surgery, found that decisional conflict existed because of differences of opinion between patient and surgeon. This was consistent with findings from Suarez-Almazor et al.24 Interestingly, patients in these studies interacted with primary care physicians and surgeons, suggesting conflict continues throughout the patients’ journey to knee arthroplasty.
Many fears were identified in the studies. This was predominantly a fear of the operation (with associated anaesthesia), recovery, and outcome. One fear was related to pain, which was identified in four of the studies, with the effect on participants’ life being a major factor in decision making.
Function was reported in three studies as a decision making factor. Many authors linked function with another domain (e.g. Marcinkowski et al29 describe physical and emotional struggling as a theme).
Psychological aspects were explored in three papers. This was viewed quite consistently across papers involving participants on the waiting list, or those who had received knee arthroplasties. Feelings of frustration, vulnerability, letting others down, and self-image were discussed.
Patients’ social network functioned both as a source of perceived pressure and as an information source related to the social network’s experience of surgery. Related to this was a personal experience of surgery, identified by two studies.
Six further themes were identified in the studies, but were only identified in one sample of patients. These included surgery as a last resort, preference for continuing their current state, financial issues, different source of information, and different preferences for participation in decision making.
Discussion
We describe a heterogeneous group of studies examining the decision making process of patients when considering knee arthroplasty. Some themes are remarkably consistent, others have only been demonstrated in specific samples of patients. One theme, the relationship with the treating physician, was not found to be important in one study, contrasting with it being a major factor in four other papers. It may be that this is a result of the study samples: the study that found this theme was not important as it included patients that had been seen by many doctors in many different countries.
The themes identified within this review are consistent with the wider literature of knee arthroplasties. Huduk et al30 investigated a population of patients with hip and knee OA who had elected not to have an arthroplasty. Patients who do not proceed to joint arthroplasty tend to view OA as an inevitable part of ageing, see others as worse off than themselves, and wait for the doctor to recommend it. These findings are consistent with findings from our review, especially with the samples of patients who were at an earlier stage in their treatment course. This aspect is key in understanding the high rate of patients who are unwilling to consider knee arthroplasty.9
Elwyn and Miron-Shatz31 suggested that the decision making process can be split into deliberation and decision making. This would suggest that the deliberation process occurs until the decision to have surgery is reached (what Clark et al32 refer to as the “Decision Making Threshold”). Included studies demonstrated that patients experience decisional conflict, however, it is unclear if this conflict causes a degree of stress during the deliberation stage, or if this is resolved once the threshold is reached. It is also unclear if patients would be willing to move back into the deliberation phase if their symptoms improved. The relationship between the decision making threshold and the movement from deliberation to decision making is currently poorly understood, and should be a focus for further research.
In 2007 O’Neill et al11 conducted a qualitative metasynthesis of decision making in joint arthroplasty. This study concluded that social and cultural categories shape patients’ expectations of treatment options. Coping strategies and life context determined the short- and longer-term outcomes of joint arthroplasty. Interestingly, the strongest theme identified was trust in the health professional. This is broadly consistent with the findings of this review, however, one paper reports a notable exception.26
In 2012 Jayadev7 conducted a review on patient decision aids. This included evidence from a Cochrane review that concluded that decision aids improved patient knowledge, resulted in less decisional conflict, less indecision, and greater concordance between patient values and chosen options. However, it also commented on the varying quality of decision aids, finding that the content regarding different treatment options was commonly lacking. Compounding this, our review would suggest that there are various concerns that patients have over and above the different treatment options (e.g. the “relationship with the clinician”). Using the findings from this review, there is the potential to tailor the information in decision aids to address patients’ major concerns.
This review is prone to various weaknesses. The indexing of qualitative work from electronic databases is not as well developed as that of quantitative studies.21 There are currently no registers of qualitative work and studies that commonly use descriptive or imaginative titles, making identification through standard search techniques problematic.19,21 To address this, a broad based approach, searching for only the subject and topic terms was used.19 This results in a large number of irrelevant studies, and, with an estimated 23% of studies not having indexed abstracts, results in a large number of full text articles being screened.19 Furthermore, we conducted a comprehensive bibliographic search of all full text articles retrieved, including those excluded from the review. This approach is consistent with that used by the Evidence for Policy and Practice Information Centre.19
The definition of a qualitative study is problematic, with experienced qualitative researchers disagreeing over what constitutes qualitative.19 We addressed this by having strict criteria – practically this was achieved by only including research that, in the authors’ opinion, was unequivocally qualitative in nature. Studies examining knee arthroplasty decision making with other conditions (e.g. hip arthroplasty or back pain) were excluded.11,33,34 These studies may have contained useful information, but were excluded on the basis that the themes may not have been relevant to knee arthroplasty decision making.
No synthesis of the data took place, although common themes have been highlighted. This is a controversial subject in itself, as is providing a narrative review of qualitative research.18,19,21 Our aim was to provide an overview of what is known about how patients make decisions, and to let the reader interpret the themes expressed from each paper.
Various weaknesses were present in the studies included within this review. Some samples of patients were homogeneous within certain characteristics (e.g. black African Americans).23 Additionally, the stage of the decision making process has not been addressed, with each included study focusing on one stage of the pathway of care. The stage of decision making is likely to be key to understanding the decision making process, and therefore these studies lack an essential dimension. We found it interesting that positive findings were reported throughout all studies and only one study mentioned a negative result.26 It is unclear if authors did not report negative findings, or did not make any attempts to investigate certain factors that could affect decision making. This could be thought of as a reporting bias. To what degree this influenced the result is unclear.
An additional aspect, that has became relevant recently is that of providing a personalised prediction of outcome for patients considering knee arthroplasty and which has been identified as a research priority by the National Institute for Health and Clinical Excellence (NICE).35 Currently there are several investigations into the development of such a tool.36-39 It is unclear how such a tool would affect decision making.
The strengths of this study are the systematic method of identifying studies, the accurate reporting of themes from individual papers, and the process of cross-validating the themes that were extracted from the papers.
We identified 17 individual themes across seven studies that covered all stages of the decision making journey, from developing symptoms through to recovery after knee arthroplasty. Ten themes were repeated across studies, with fear, pain, coping mechanisms, expectations of surgery, and the relationship with the clinician seen most frequently.
Understanding all facets that may affect patient decision making when considering knee arthroplasty is essential to the shared decision making process. This work can act as a framework for understanding common concerns of patients considering knee arthroplasty and aid clinicians in delivering patient-centred care. Other methods of delivering information to patients (e.g. patient decision aids) should address these factors. However, how best to integrate these findings into information delivery systems for patients is an area that requires greater understanding.
By facilitating the patient–doctor interaction, a sound understanding of patient decision making has the potential to address increasing financial pressures, variation in uptake, and improved satisfaction from surgery and the decision making process itself.
1 No authors listed. Clinical Surgical Practice Issues 2012. British Orthopaedic Association. http://www.boa.ac.uk/PP/Pages/clin-issues.aspx (date last accessed 16 July 2015). Google Scholar
2 Gonzalez Saenz de Tejada M , EscobarA, BilbaoA, et al.A prospective study of the association of patient expectations with changes in health-related quality of life outcomes, following total joint replacement. BMC Musculoskelet Disord2014;15:248.CrossrefPubMed Google Scholar
3 No authors listed. National Joint Registry 2015. http://www.njrcentre.org.uk/njrcentre/default.aspx (date last accessed 16 July 2015). Google Scholar
4 No authors listed. The Autumn Statement: NHS Funding. The King’s Fund. http://www.kingsfund.org.uk/publications/articles/autumn-statement (date last accessed 16 July 2015). Google Scholar
5 Culliford D , MaskellJ, JudgeA, et al.Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage2015;23:594–600.CrossrefPubMed Google Scholar
6 Stacey D , BennettCL, BarryMJ, et al.Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev2011;10:CD–001431.CrossrefPubMed Google Scholar
7 Jayadev C , KhanT, CoulterA, BeardDJ, PriceAJ. Patient decision aids in knee replacement surgery. Knee2012;19:746–750.CrossrefPubMed Google Scholar
8 No authors listed. Atlas of Variation 2010. RightCare. http://www.rightcare.nhs.uk/index.php/programme/ (date last accessed 16 July 2015). Google Scholar
9 Hawker GA , WrightJG, BadleyEM, CoytePC. Perceptions of, and willingness to consider, total joint arthroplasty in a population-based cohort of individuals with disabling hip and knee arthritis. Arthritis Rheum2004;51:635–641.CrossrefPubMed Google Scholar
10 Borkhoff C . Disparities in access and in quality of care in rheumatology. [abstract]. Ann Rheum Dis2013;71:10. Google Scholar
11 O’Neill T , JinksC, OngBN. Decision-making regarding total knee replacement surgery: a qualitative meta-synthesis. BMC Health Serv Res2007;7:52.CrossrefPubMed Google Scholar
12 Bourne RB , ChesworthB, DavisA, MahomedN, CharronK. Comparing patient outcomes after THA and TKA: is there a difference?Clin Orthop Relat Res2010;468:542–546.CrossrefPubMed Google Scholar
13 Bachmeier CJ , MarchLM, CrossMJ, et al.A comparison of outcomes in osteoarthritis patients undergoing total hip and knee replacement surgery. Osteoarthritis Cartilage2001;9:137–146.CrossrefPubMed Google Scholar
14 Ibrahim SA , SiminoffLA, BurantCJ, KwohCK. Differences in expectations of outcome mediate African American/white patient differences in “willingness” to consider joint replacement. Arthritis Rheum2002;46:2429–2435. Google Scholar
15 Grotle M , HagenKB, NatvigB, DahlFA, KvienTK. Obesity and osteoarthritis in knee, hip and/or hand: an epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet Disord2008;9:132.CrossrefPubMed Google Scholar
16 Jokela M , HintsanenM, HakulinenC, et al.Association of personality with the development and persistence of obesity: a meta-analysis based on individual-participant data. Obes Rev2013;14:315–323.CrossrefPubMed Google Scholar
17 Sandelowski M , BarrosoJ, VoilsCI. Using qualitative metasummary to synthesize qualitative and quantitative descriptive findings. Res Nurs Health2007;30:99–111.CrossrefPubMed Google Scholar
18 Pantoja T. Sythesis methods in Systematic reviews of Health Policy and Systems Research. In: Note Af HB, ed. Alliance for HPSR Alliance for HPSR; 2011.http://www.who.int/alliance-hpsr/projects/alliancehpsr_briefingnotesynthesismethodschile.pdf (date last accessed 24 August 2015). Google Scholar
19 No authors listed. Centre for Reviews and Dissemination: Incorporating qualitative evidence in or alongside effectiveness reviews. https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf (date last accessed 24 August 2015). Google Scholar
20 Dixon-Woods M , SuttonA, ShawR, et al.Appraising qualitative research for inclusion in systematic reviews: a quantitative and qualitative comparison of three methods. J Health Serv Res Policy2007;12:42–47.CrossrefPubMed Google Scholar
21 Barnett-Page E , ThomasJ. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol2009;9:59.CrossrefPubMed Google Scholar
22 Walsh D , DowneS. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs2005;50:204–211.CrossrefPubMed Google Scholar
23 Figaro MK , RussoPW, AllegranteJP. Preferences for arthritis care among urban African Americans: “I don’t want to be cut”. Health Psychol2004;23:324–329. Google Scholar
24 Suarez-Almazor ME , RichardsonM, KrollTL, SharfBF. A qualitative analysis of decision-making for total knee replacement in patients with osteoarthritis. J Clin Rheumatol2010;16:158–163.CrossrefPubMed Google Scholar
25 Chang HJ , MehtaPS, RosenbergA, ScrimshawSC. Concerns of patients actively contemplating total knee replacement: differences by race and gender. Arthritis Rheum2004;51:117–123.CrossrefPubMed Google Scholar
26 Al-Taiar A , Al-SabahR, ElsalawyE, ShehabD, Al-MahmoudS. Attitudes to knee osteoarthritis and total knee replacement in Arab women: a qualitative study. BMC Res Notes2013;6:406.CrossrefPubMed Google Scholar
27 Toye FM , BarlowJ, WrightC, LambSE. Personal meanings in the construction of need for total knee replacement surgery. Soc Sci Med2006;63:43–53.CrossrefPubMed Google Scholar
28 Woolhead GM , DonovanJL, ChardJA, DieppePA. Who should have priority for a knee joint replacement?Rheumatology (Oxford)2002;41:390–394.CrossrefPubMed Google Scholar
29 Marcinkowski K , WongVG, DignamD. Getting back to the future: a grounded theory study of the patient perspective of total knee joint arthroplasty. Orthop Nurs2005;24:202–209.CrossrefPubMed Google Scholar
30 Hudak PL , ClarkJP, HawkerGA, et al.“You’re perfect for the procedure! Why don’t you want it?” Elderly arthritis patients’ unwillingness to consider total joint arthroplasty surgery: a qualitative study. Med Decis Making2002;22:272–278. Google Scholar
31 Elwyn G , Miron-ShatzT. Deliberation before determination: the definition and evaluation of good decision making. Health Expect2010;13:139–147.CrossrefPubMed Google Scholar
32 Clark JP , HudakPL, HawkerGA, et al.The moving target: a qualitative study of elderly patients’ decision-making regarding total joint replacement surgery. J Bone Joint Surg [Am]2004;86-A:1366–1374. Google Scholar
33 Dosanjh S , MattaJM, BhandariM. , Anterior THA Research Collaborative. The final straw: a qualitative study to explore patient decisions to undergo total hip arthroplasty. Arch Orthop Trauma Surg2009;129:719–727. Google Scholar
34 Katz JN , LyonsN, WolffLS, et al.Medical decision-making among Hispanics and non-Hispanic Whites with chronic back and knee pain: a qualitative study. BMC Musculoskelet Disord2011;12:78.CrossrefPubMed Google Scholar
35 No authors listed. Osteoathritis: Care and management in adults. National Institute for Health and Care Excellence. http://www.nice.org.uk/Guidance/CG177 (date last accessed 16 July 2015). Google Scholar
36 Baker PN , DeehanDJ, LeesD, et al.The effect of surgical factors on early patient-reported outcome measures (PROMS) following total knee replacement. J Bone Joint Surg [Br]2012;94-B:1058–1066.CrossrefPubMed Google Scholar
37 Judge A , ArdenNK, CooperC, et al.Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford)2012;51:1804–1813.CrossrefPubMed Google Scholar
38 No authors listed. Targeted rehabilitation to improve outcome after knee replacement (TRIO). Arthritis Research U.K. http://www.arthritisresearchuk.org/research/grant-tracker-items/2012/targeted-rehabilitation-to-improve-outcome-after-knee-replacement-trio.aspx (date last accessed 16 July 2015). Google Scholar
39 Barlow T , DunbarM, SprowsonA, ParsonsN, GriffinD. Development of an outcome prediction tool for patients considering a total knee replacement--the Knee Outcome Prediction Study (KOPS). BMC Musculoskelet Disord2014;15:451.CrossrefPubMed Google Scholar
Funding statement:
A research grant from Arthritis Research UK for a series of studies examining patient decision making and the development of an outcome prediction tool has been received in relation to this study.
D Griffin has received expenses from Stryker UK which is not related to this article.
Author contributions:
T. Barlow: Design, data collection, data analysis, writing the paper
D. Griffin: Writing the paper
D. Barlow: Data collection, data analysis, drafting paper
A. Realpe: Design, data analysis, drafting paper
ICMJE Conflict of Interest:
None declared
©2015 Griffin et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
Supplementary material. A table showing themes is available alongside the online version of this article at www.bjr.boneandjoint.org.uk










