Abstract
Objectives
Metal-on-metal hip resurfacing (MOMHR) is available as an alternative option for younger, more active patients. There are failure modes that are unique to MOMHR, which include loosening of the femoral head and fractures of the femoral neck. Previous studies have speculated that changes in the vascularity of the femoral head may contribute to these failure modes. This study compares the survivorship between the standard posterior approach (SPA) and modified posterior approach (MPA) in MOMHR.
Methods
A retrospective clinical outcomes study was performed examining 351 hips (279 male, 72 female) replaced with Birmingham Hip Resurfacing (BHR, Smith and Nephew, Memphis, Tennessee) in 313 patients with a pre-operative diagnosis of osteoarthritis. The mean follow-up period for the SPA group was 2.8 years (0.1 to 6.1) and for the MPA, 2.2 years (0.03 to 5.2); this difference in follow-up period was statistically significant (p < 0.01). Survival analysis was completed using the Kaplan–Meier method.
Results
At four years, the Kaplan–Meier survival curve for the SPA was 97.2% and 99.4% for the MPA; this was statistically significant (log-rank; p = 0.036). There were eight failures in the SPA and two in the MPA. There was a 3.5% incidence of femoral head collapse or loosening in the SPA and 0.4% in the MPA, which represented a significant difference (p = 0.041). There was a 1.7% incidence of fractures of the femoral neck in the SPA and none in the MPA (p = 0.108).
Conclusion
This study found a significant difference in survivorship at four years between the SPA and the MPA (p = 0.036). The clinical outcomes of this study suggest that preserving the vascularity of the femoral neck by using the MPA results in fewer vascular-related failures in MOMHRs.
Cite this article: Bone Joint Res 2014;3:150–4
Article focus
Does the modified posterior approach result in better survivorship when compared with the standard posterior approach in metal-on-metal hip resurfacing?
Key messages
Our study demonstrated a statistically significant survivorship with the modified posterior approach compared with the standard posterior approach in metal-on-metal hip resurfacing.
This may be due to preserved vascularity of the femoral head, and thus, fewer vascular-related femoral failures.
Strengths and limitations
Strengths: the operations were undertaken by one surgeon.
The study used a consecutive data set.
Limitations: the follow-up period is short, however, it is likely that vascular failure would have occured during this period.
There are a small number of failures in both cohorts, making statistical comparison difficult between the two groups.
Introduction
Metal-on-metal hip resurfacing (MOMHR) is available as an alternative option to total hip replacement (THR) for younger, more active patients with end-stage hip osteoarthritis. Favourable outcomes for MOMHR have been reported at mid- and long-term follow-up for appropriate patients.1-3 The larger components of MOMHR provide increased joint stability and range of movement, and studies have shown outcomes comparable with traditional THR in male patients with osteoarthritis.1-3
Because of the nature of proximal femoral bone preservation inherent to the procedure, there are failure modes that are unique to MOMHR, including femoral head collapse or loosening, and fractures of the femoral neck.4-6The reported incidences of femoral head collapse or loosening and fractures of the femoral neck are 3%, and between 0% and 4%, respectively.3,6-11 A traumatic fracture of the femoral neck is the most common cause of early revision4,12,13 and femoral head collapse or aseptic loosening is the second-most common.13 Previous studies have speculated that changes in the vascularity of the femoral head and resulting osteonecrosis, may contribute to these failure modes.14-17 Retrieval studies have shown areas of avascular necrosis (AVN) in cases of fracture of the femoral neck and femoral head loosening, suggesting that AVN may play a role in the aetiology of these failure modes.4,5,16
The main blood supply to the head comes from the deep branch of the medial femoral circumflex artery (MFCA) (Fig. 1) (Fig. 1).18,19 The deep branch of the MFCA runs along the posterosuperior aspect of the femoral neck, where it divides into two or four subsynovial retinacular vessels.18,19 The lateral femoral circumflex artery and foveal artery are not thought to contribute much with regard to the blood supply of the femoral head.19,20
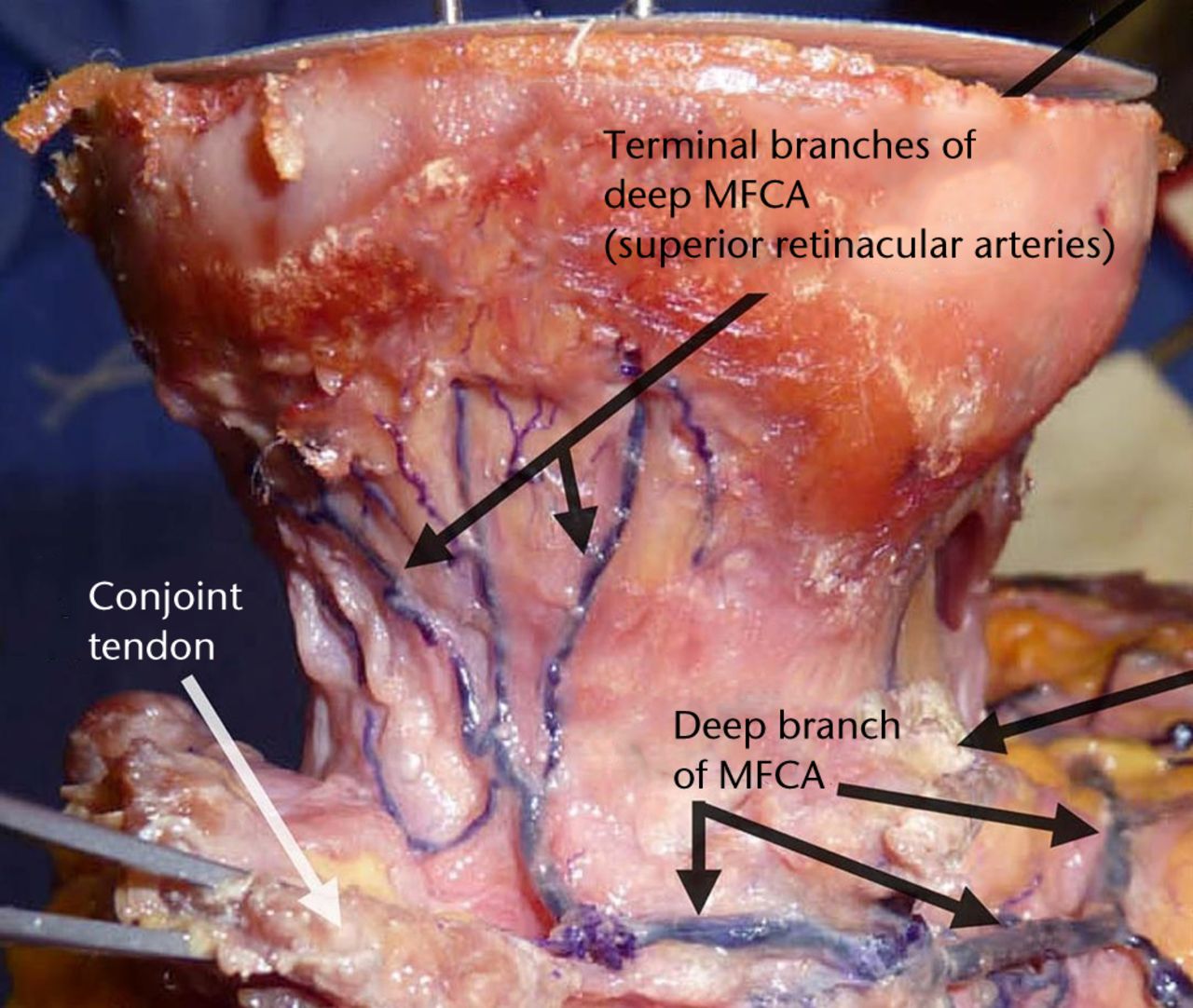
Fig. 1
Photograph showing a femoral head. The main blood supply comes from the deep branch of the medial femoral circumflex artery (MFCA).
In the standard posterior approach, an electrocautery device is used to transect the capsule at the base of the femoral neck, and the soft tissues are stripped off, where they attach to the greater trochanter, potentially disrupting the vascular supply to the femoral head. In the modified posterior approach, however, a sharp knife is used to perform the capsulotomy at the level of the femoral head, thus preserving the soft tissues around the femoral neck. This has the effect of leaving a capsular cuff of tissue on the femoral neck, and retains the retinacular arteries that vascularise the femoral head, thereby preserving blood supply to the femoral head. While studies have shown differences in oxygenation and vascularity between the standard and the modified posterior approaches, the clinical outcomes of these changes have not been shown.14 Therefore, we sought to investigate whether these changes in surgical approach result in better clinical outcomes.
This study examines the survivorship differences between the standard posterior and modified posterior approaches. We hypothesise that the modified posterior approach will preserve the vascularity of the femoral head, which should result in fewer failures in MOMHRs due either to osteonecrosis, or a fracture of the femoral neck.
Materials and Methods
A retrospective clinical outcomes study was performed examining 351 hips (279 male, 72 female) in 313 patients with MOMHR by the senior author (EPS) between June 2006 and June 2008. This study was approved by the Institutional Review Board, and patient consent was obtained. All hips were replaced with Birmingham Hip Resurfacing (BHR) replacement (Smith and Nephew, Memphis, Tennessee).
The senior author modified his approach from the standard posterior to the modified posterior approach in May 2007. The first 50 patients after the technique modification were excluded from analysis as part of an assumed learning curve, as studies have suggested fracture of the femoral neck to be associated with the surgical learning curve.6 The mean follow-up period for the standard posterior group was 2.8 years (0.1 to 6.1) and for the modified posterior it was 2.2 years (0.03 to 5.2); this difference in follow-up period was statistically significant (p < 0.01) as the surgeon (EPS) switched to the modified approach in May 2007. The patient demographics are listed in Table I. To avoid patients with pre-existing vascular issues (such as existing avascular necrosis of the femoral head), patients were limited to those with a pre-operative diagnosis of osteoarthritis.
Table I
Patient demographics (N/A, not applicable)
| Standard posterior | Modified posterior | p-value | |
|---|---|---|---|
| Duration | 11 months (5/6/06 to 3/5/07) | 11 months (24/07/07 to 20/06/08) | N/A |
| No of hips | 115 | 236 | |
| Mean follow-up (years) | 2.8 (0.1 to 6.1) | 2.2 (0.03 to 5.2) | < 0.001* |
| Age (years) | 49.5 | 49.4 | 0.928* |
| Body mass index | 27.3 | 27.5 | 0.647* |
| Gender | 0.171† | ||
| Male | 96 | 183 | - |
| Female | 19 | 53 | - |
| Mean head size (mm) | 48 (42 to 54) | 48 (38 to 58) | 0.977* |
-
* Student’s t-test † Chi Squared test
Statistical analysis
Patient demographic and follow-up data were collected from medical records. Parametric variables were compared using the Student’s t-test and non-parametric variables were compared using the Mann–Whitney U test. A survival analysis was completed using the Kaplan–Meier method, and a log-rank test was used to compare the equality of survival distribution.21 A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 16 (SPSS, Inc., Chicago, Illinois).
Results
The Kaplan–Meier survival curve for the standard posterior approach was 97.2% at four years, and 99.4% at four years for the modified posterior approach (Fig. 2). The log-rank test demonstrated a statistical significance in the difference in survivorship (p = 0.036). There were eight failures in the standard posterior approach and two in the modified posterior approach. The mean time to failure in the standard posterior approach was 36.9 months (0.9 to 73.6) and 27.4 months (9 to 45.8) for the modified posterior approach (p = 0.69). There was a 1.7% (2/115) incidence of femoral neck fractures in the standard posterior group and none in the modified posterior group (p = 0.108, chi-squared). There was a 3.5% (4/115) incidence of femoral head collapse or loosening in the standard posterior group and a 0.4% (1/236) incidence in the modified posterior group; this difference was significant (p = 0.045, chi-squared). The breakdown by failure modes is listed in Table II.
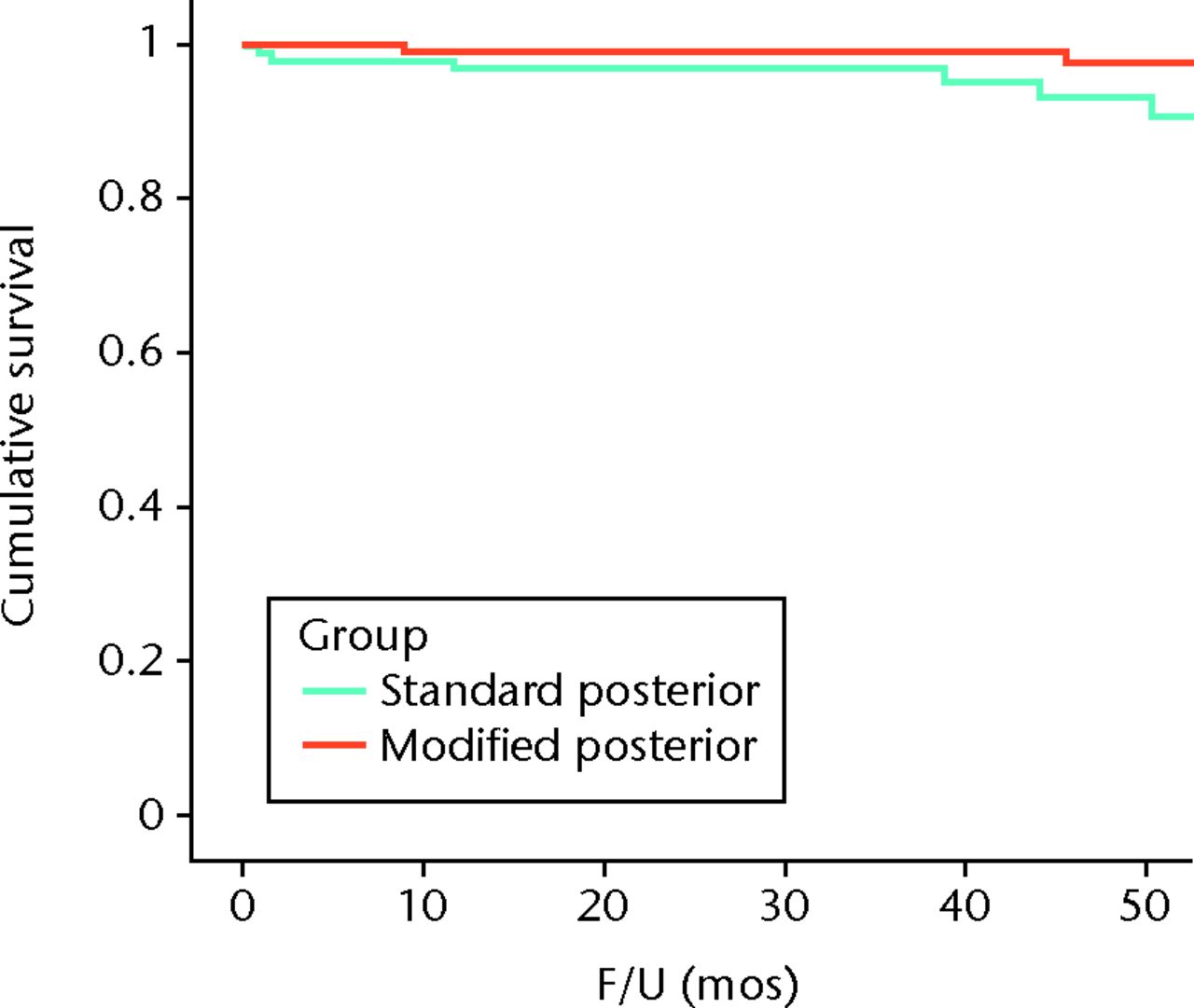
Fig. 2
Graph showing the Kaplan-Meier survivorship curve for the standard posterior and the modified posterior approach.
Table II
Failures
| Standard posterior | Modified posterior | |
|---|---|---|
| Femoral loosening | 4 | 1 |
| Metal sensitivity | 0 | 1 |
| Fracture of the femoral neck | 2 | 0 |
| Wear | 2 | 0 |
| Total | 8 | 2 |
Clinical scores in both groups were significantly improved at the time of last follow-up examination (p < 0.001 in both groups, Student’s t-test). Post-operative Harris hip scores improved from a mean of 60 (38 to 83) in the standard posterior group and 63 (41 to 83) in the modified posterior group to 98 (80 to 100) in the standard posterior group and 97 (68 to 100) in the modified posterior group at last follow-up. There was no significant difference between the two cohorts (p = 0.386, Student’s t-test). No patient in either cohort experienced deep venous thrombosis, dislocation, nerve injury, or infection.
Discussion
This study found the modified posterior approach to have a significantly better (p = 0.036, log-rank test) survivorship compared with the standard posterior approach at four years. There were six osteonecrosis-related failures in the standard posterior approach and one in the modified posterior approach, which may be a result of preserved vascularity in the modified posterior approach; this is speculation based on previous studies in the literature that show that femoral neck fractures and loosening are likely a result of osteonecrosis and loss of blood supply to the femoral head.14,16,22,23Since retrieval studies were not done on the failures, we cannot be certain of their aetiology. However, we can infer that, based on previous studies, our fracture of the femoral neck and loosening were likely secondary to osteonecrosis from disrupted femoral head blood supply.
Steffen et al14 found the modified posterior approach to preserve more oxygen compared with the standard posterior approach. Disrupted vascularity to the femoral neck may be an important pathophysiological process that leads to avascular necrosis, and eventual fracture of the femoral neck and loosening of the femoral component. If vascular supply to the femoral head is compromised, AVN can occur; bone can resorb at the interface of viable and dead bone, which can weaken the femoral neck to the point that it fractures.14 Steffen et al22 found fractures after hip resurfacing to be significantly associated (p < 0.001) with a greater proportion of empty osteocyte lacunae within trabecular bone, compared with osteoarthritic controls, thus establishing a relationship between fractures and AVN. Furthermore, Steffen et al22 suggest that it is unlikely that the fracture led to AVN, as most of the blood supply to the femoral head is extraosseous (in order for a fracture to cause AVN, the fracture would need to progress slowly which interrupts the intraosseous supply to the femoral head).22 Little et al16 histologically investigated 13 retrieved components (eight of which were fractures of the femoral neck and one of which was femoral loosening), and found changes “indicative of established osteonecrosis”16 in all but one case. Their study suggests that since none of these patients had osteonecrotic bone removed at the time of implantation, the necrotic changes found on the explanted femoral components happened after the resurfacing procedure.16
While Campbell et al4 have suggested that the thermal injury after the polymerisation of cement may be the process that leads to osteonecrosis (and thus osteonecrosis-related failures), Little et al16 argue that their study found areas of necrosis to be present both at the cement-bone interface, and remote sites. Furthermore, if cement polymerisation was the main cause of osteonecrosis and its resulting failure, we would have expected to see an equal incidence of osteonecrosis-related failures in both groups. This suggests that other factors, in addition to cement polymerisation, must play a role in the aetiology of osteonecrosis-related failures in MOMHRs.
Early femoral loosening has been attributed to pathological changes of the femoral bone, including osteonecrosis and pseudoarthrosis.23 Zustin et al23 identified four different morphological patterns of loosening: pseudoarthrosis (median in situ time of 16 weeks), collapsed osteonecrosis (median in situ time of 79 weeks), cement-socket debonding (median in situ time of 89 weeks) and bone-cement loosening (median in situ time of 175 weeks). However, the aetiology of femoral loosening is not as clear, and several different aetiologies, such as hypersensitivity reaction and inadequate cement fixation,11 have been suggested to play a role.
Beaulé et al24 found that femoral reaming decreased blood flow by 70% in nine out of ten hips using the Ganz trochanteric flip approach,24,25 likely due to disrupted nutrient retinacular vessels, which predominantly penetrate the bone in the anterosuperior and posterosuperior quadrants of the femoral neck.26,27 These findings support the importance of preserving the extraosseous blood supply to the femoral neck. Furthermore, notching of the femoral neck is associated with femoral loosening,28 but removal of up to 30% of the anterolateral femoral neck does not alter the load-bearing capacity of the proximal femur, also suggesting that vascularity plays an important role.15,26 Beaulé et al’s29 review on the vascularity of the arthritic femoral head and resurfacing concludes that “it is clear” osteonecrosis causes early failure, either as an acute fracture of the femoral neck, or as femoral loosening at least three years following operation.23,29 However, it is highly likely that both failures from fractures of the femoral neck and femoral loosening are multifactorial. We believe that preservation of the retinacular blood supply should be an important goal of exposing the hip via a posterior approach, in order to maintain the perfusion, or blood supply, of the femoral head. To this end, we have adopted a modified posterior approach that avoids the use of cautery along the femoral neck; furthermore, a cuff of capsule is left attached to the femoral neck to avoid disruption of this retinacular ring of vessels. We believe that the improved survivorship of the modified posterior group is a clear indication that the perfusion is preserved, and thus reduces the number of vascular-related failures.
A limitation of this study was the short follow-up period and the small number of failures, which made it difficult to analyse the incidence of vascular versus non-vascular related failures statistically. However, fractures of the femoral neck occur early on following operation, at a mean time of 15.4 weeks (0 to 56)10 and our study encompasses that time period. It is likely that the observed outcome is the result of multiple factors, one of which appears to be the preserved vascularity from the modified posterior approach. We can make this assumption with confidence because the two groups are statistically similar; the only variable that is different between the groups is the surgical approach. The clinical outcomes of this study suggest that preserving the vascularity of the femoral neck by using the modified posterior approach results in fewer vascular-related failures in MOMHR.
1 Amstutz HC , Le DuffMJ. Eleven years of experience with metal-on-metal hybrid hip resurfacing: a review of 1000 conserve plus. J Arthroplasty2008;23(6 Suppl 1):36–43.CrossrefPubMed Google Scholar
2 Murray DW , GrammatopoulosG, PanditH, et al.The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg [Br]2012;94-B:1180–1186.CrossrefPubMed Google Scholar
3 Treacy RB , McBrydeCW, PynsentPB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg [Br]2005;87-B:167–170.CrossrefPubMed Google Scholar
4 Campbell P , BeauléPE, EbramzadehE, et al.The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop Relat Res2006;453:35–46.CrossrefPubMed Google Scholar
5 Morlock MM , BishopN, ZustinJ, et al.Modes of implant failure after hip resurfacing: morphological and wear analysis of 267 retrieval specimens. J Bone Joint Surg [Am]2008;90-A(Suppl)3:89–95.CrossrefPubMed Google Scholar
6 Marker DR , SeylerTM, JinnahRH, et al.Femoral neck fractures after metal-on-metal total hip resurfacing: a prospective cohort study. J Arthroplasty2007;22(7 Suppl 3):66–71.CrossrefPubMed Google Scholar
7 Amstutz HC , BeauléPE, DoreyFJ, et al.Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg [Am]2004;86-A:28–39.PubMed Google Scholar
8 Beaulé PE , AmstutzHC, Le DuffM, DoreyF. Surface arthroplasty for osteonecrosis of the hip: hemiresurfacing versus metal-on-metal hybrid resurfacing. J Arthroplasty2004;19(8 Suppl 3):54–58.CrossrefPubMed Google Scholar
9 Daniel J , PynsentPB, McMinnDJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg [Br]2004;86-B:177–184.CrossrefPubMed Google Scholar
10 Shimmin AJ , BackD. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg [Br]2005;87-B:463–464.CrossrefPubMed Google Scholar
11 Amstutz HC , Le DuffMJ, CampbellPA, DoreyFJ. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing. Results of 600 Conserve Plus with a 3 to 9 year follow-up. J Arthroplasty2007;22:481–489.CrossrefPubMed Google Scholar
12 Steffen RT , FoguetPR, KriklerSJ, et al.Femoral neck fractures after hip resurfacing. J Arthroplasty2009;24:614–619.CrossrefPubMed Google Scholar
13 Steffen RT , PanditHP, PalanJ, et al.The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg [Br]2008;90-B:436–441.CrossrefPubMed Google Scholar
14 Steffen RT , De SmetKA, MurrayDW, GillHS. A modified posterior approach preserves femoral head oxgenation during hip resurfacing. J Arthroplasty2011;26:404–408.CrossrefPubMed Google Scholar
15 Beaulé PE , CampbellPA, HokeR, DoreyF. Notching of the femoral neck during resurfacing arthroplasty of the hip: a vascular study. J Bone Joint Surg [Br]2006;88-B:35–39.CrossrefPubMed Google Scholar
16 Little CP , RuizAL, HardingIJ, et al.Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg [Br]2005;87-B:320–323.CrossrefPubMed Google Scholar
17 Steffen RT , SmithSR, UrbanJP, et al.The effect of hip resurfacing on oxygen concentration in the femoral head. J Bone Joint Surg [Br]2005;87-B:1468–1474.CrossrefPubMed Google Scholar
18 Gautier E , GanzK, KrügelN, GillT, GanzR. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg [Br]2000;82-B:679–683.PubMed Google Scholar
19 Sevitt S , ThompsonRG. The distribution and anastomoses of arteries supplying the head and neck of the femur. J Bone Joint Surg [Br]1965;47-B:560–573.PubMed Google Scholar
20 Judet J , JudetR, LagrangeJ, DunoyerJ. A study of the arterial vascularisation of the femoral neck in the adult. J Bone Joint Surg [Am]1955;37-A:663–680. Google Scholar
21 Dorey F , AmstutzHC. Survivorship analysis in the evaluation of joint replacement. J Arthroplasty1986;1: 63-69.CrossrefPubMed Google Scholar
22 Steffen RT , AthanasouNA, GillHS, MurrayDW. Avascular necrosis associated with fracture of the femoral neck after hip resurfacing: histological assessment of femoral bone from retrieval specimens. J Bone Joint Surg [Br]2010;92-B:787–793.CrossrefPubMed Google Scholar
23 Zustin J , HahnM, MorlockMM, et al.Femoral component loosening after hip resurfacing arthroplasty. Skeletal Radiol2010;39:747–756.CrossrefPubMed Google Scholar
24 Beaulé PE , CampbellP, ShimP. Femoral head blood flow during hip resurfacing. Clin Orthop Relat Res2007;456:148–152.CrossrefPubMed Google Scholar
25 Ganz R , GillTJ, GautierE, et al.Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg [Br]2001;83-B:1119–1124.CrossrefPubMed Google Scholar
26 Lavigne M , KalhorM, BeckM, GanzR, LeunigM. Distribution of vascular foramina around the femoral head and neck junction: relevance for conservative intracapsular procedures of the hip. Orthop Clin North Am2005;36:171–176.CrossrefPubMed Google Scholar
27 Amanatullah DF , CheungY, Di CesarePE. Hip resurfacing arthroplasty: a review of the evidence for surgical technique, outcome, and complications. Orthop Clin North Am2010;41:263–272.CrossrefPubMed Google Scholar
28 de Waal Malefijt MC , HuiskesR. A clinical, radiological and biomechanical study of the TARA hip prosthesis. Arch Orthop Trauma Surg1993;112:220–225.CrossrefPubMed Google Scholar
29 Beaulé PE , CampbellP, LuZ, et al.Vascularity of the arthritic femoral head and hip resurfacing. J Bone Joint Surg [Am]2006;88-A(Suppl4):85–96.CrossrefPubMed Google Scholar
Funding statement:
This study was supported by the Hospital for Special Surgery and a grant from Smith & Nephew.
Author contributions:
K. Takamura: Data collection, Data analysis, Writing the paper
P. Maher: Data collection, Writing the paper
T. Nath: Data collection, Writing the paper
E. P. Su: Data collection, Performed surgeries, Writing the paper, Original idea for the study
ICMJE Conflict of Interest:
E. P Su receives research support from Smith & Nephew, Knee Creations, Inc., and is a paid consultant for Smith & Nephew.
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










