Abstract
Objectives
Because posterior cruciate ligament (PCL) resection makes flexion gaps wider in total knee replacement (TKR), preserving or sacrificing a PCL affects the gap equivalence; however, there are no criteria for the PCL resection that consider gap situations of each knee. This study aims to investigate gap characteristics of knees and to consider the criteria for PCL resection.
Methods
The extension and flexion gaps were measured, first with the PCL preserved and subsequently with the PCL removed (in cases in which posterior substitute components were selected). The PCL preservation or sacrifice was solely determined by the gap measurement results, without considering other functions of the PCL such as ‘roll back.’
Results
Wide variations were observed in the extension and flexion gaps. The flexion gaps were significantly larger than the extension gaps. Cases with 18 mm or more flexion gap and with larger flexion than extension gap were implanted with cruciate retaining component. A posterior substitute component was implanted with the other cases.
Conclusions
In order to make adequate gaps, it is important to decide whether to preserve the PCL based on the intra-operative gap measurements made with the PCL intact.
Cite this article: Bone Joint Res 2014;3:95–100.
Article focus
The methodology to make equal gaps in knee extension and flexion has not been established in total knee replacement.
Because PCL resection makes flexion gaps wider, preserving or sacrificing a PCL affects the gap equivalence.
There are no criteria for PCL resection that consider gap situations of each knee.
Key messages
Both extension and flexion gaps showed too wide a variation to predict before operations.
Flexion gaps were bigger than extension gaps in almost all cases and the difference between the two gaps also showed wide variation.
PCL resection in all cases may cause severe gap imbalance between knee extension and flexion.
Strengths and limitations
Intra-operative gap measurement with PCL preservation is important to understand the characteristics of each knee.
This is the first report criteria concerning PCL preservation or sacrifice which considers gap situations in each knee.
Limitation: measurement method reliability and validity are unknown.
Introduction
Total knee replacement (TKR) is widely available, and there are two main types of component design: posterior cruciate ligament (PCL) preserving or substitute. Both cruciate retaining (CR) and posterior substitute (PS) components have been reported to have good clinical results.1-5The difference between CR and PS components regarding PCL function usually concerns posterior roll back during knee bending.6,7 The CR component was expected to produce the roll back as a remaining PCL function; however, some fluoroscopic movement analysis studies revealed paradoxical anterior movement in CR TKR,8,9 while the PS component drives the constant roll back function through the post/cam mechanism.6 Some authors have reported that when the PCL, a strong stabiliser of the knee joint, is resected in an anterior cruciate ligament (ACL-) deficient knee during TKR surgery, the flexion gap becomes wider than the extension gap on average.10,11
Although adequate gap control in knee extension and flexion is important in both CR and PS TKR and sacrificing or sparing PCL influences the equality of the extension and flexion gap, there is no criteria for preserving or sacrificing PCL that consider the gap situations of each knee.
In this study, the PCL was considered only as the stabiliser between the femur and the tibia, and component selection (CR or PS) was determined only by intra-operative gap measurement, without considering other functions of the PCL such as ‘roll back’. The extension and flexion gaps were measured intra-operatively, first with the PCL intact in all cases. In cases in which the flexion gap was considered too small to set the components, the PCL was removed and the gaps were measured to estimate the degree to which they were increased by resection.
Materials and Methods
Between August 2008 and September 2010, 82 patients (65 female, 17 male) with osteoarthritis of the knee (102Â knees; 81 female, 21 male), operated on by a single surgeon (RK) using a Scorpio NRG (Stryker, Kalamazoo, Michigan) and a tension device system with a 30 lbs distraction force, were enrolled in this study. Seven knees were excluded because of lack of intra-operative measurement data. Mean age at operation was 73 years (56 to 91). To assess the influence of pre-operative flexion contracture concerning the extension-flexion gap imbalance, materials were divided into two groups. Cases with pre-operative flexion contracture < 20° and ≥ 20° were placed in groups A and B, respectively, as according to Berend, Lombardi and Adams,12 division at 20° of flexion contracture is important.
At the beginning of the surgery, the extension gap was created with a standard 8 mm femoral distal cut and a 10Â mm tibial cut. To measure the flexion gap easily with the PCL intact before the final femoral cut, it was necessary to create a small temporary gap in flexion. For this purpose, a pre-cut of the femoral posterior condyle was performed with a 4-in-1 femoral cutting guide, which was 4 mm longer in the anterior-posterior dimension than the measured size; therefore, a pre-cutting line was 4Â mm posterior compared with a cutting line for the measured resection technique (Fig. 1). With this technique, the flexion gap created was 4 mm smaller than the flexion gap typically produced by the measured resection technique, and it was easy to remove even large posterior osteophytes through the small flexion gap made by the pre-cut. After removal of all osteophytes, the patella was reduced, and the gaps were measured by an offset knee balancer with a distraction force of 30 lbs. (Fig. 2). The extension gap was measured with the lower limb in a straight position on the operating table. The flexion gap was measured with the thigh held by the surgeon’s hand with resting pressure to prevent lifting of the lower leg.
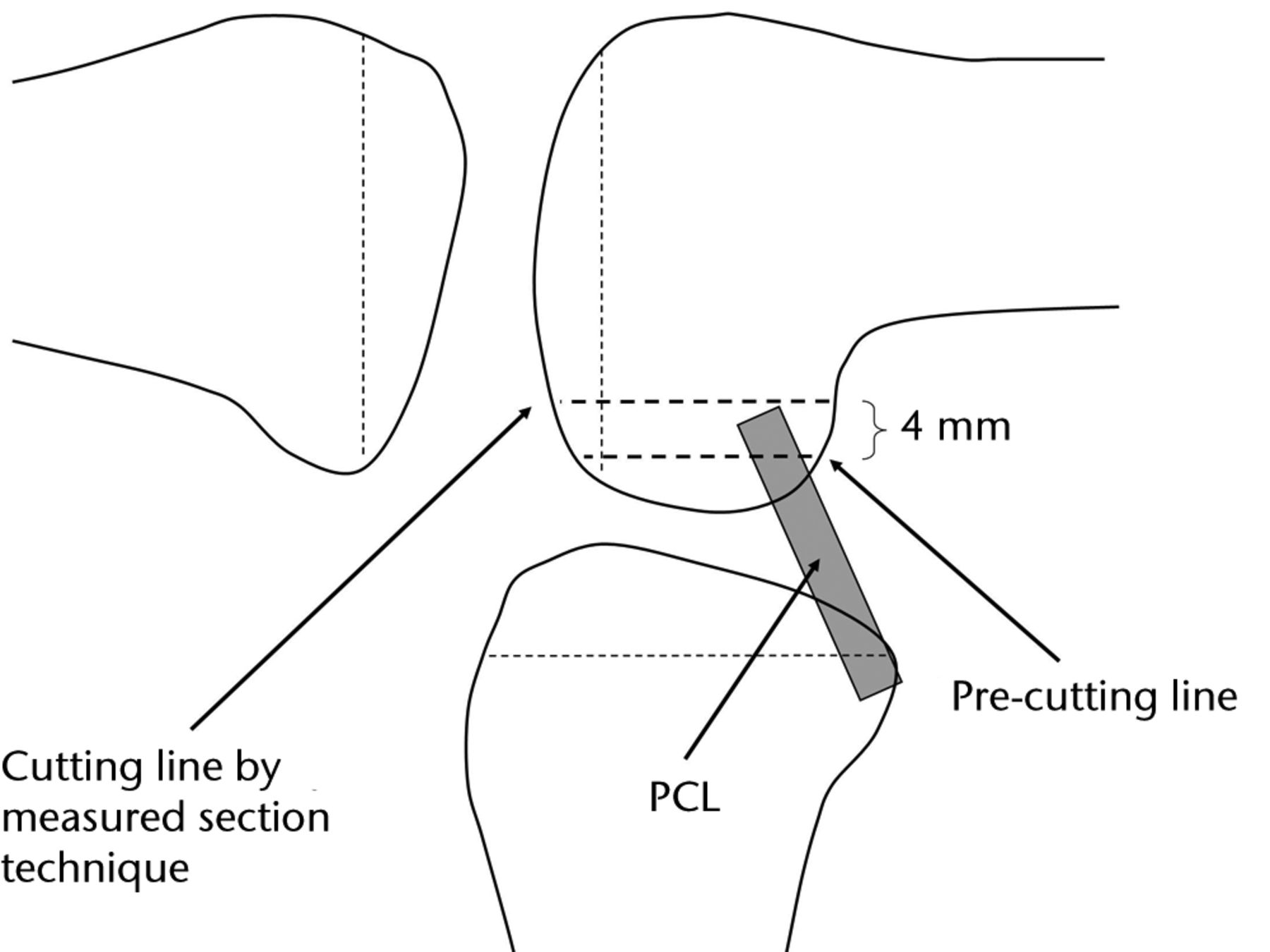
Fig. 1
Diagram showing the pre-cut of the femoral posterior condyle.

Fig. 2
Intra-operative photograph showing measurement of the flexion gap with the patella reduced.
To compare both gaps, the flexion gap was corrected by the length of the pre-cut. This corrected gap, which is a theoretical amount and not the actual final flexion gap, is the same as a flexion gap produced by the measured resection technique. A component type was selected according to the extension and corrected flexion gap. If there was enough space to set the all components on the femur and tibia in flexion with the PCL intact, the CR component was implanted; otherwise, the PCL was resected and the PS component selected. The degree to which PCL resection increased the two gaps was also measured in PS cases. If necessary, soft tissue was released for good ligament balance. An additional distal cut of the femur was considered in cases where the extension gap was too small compared with the flexion gap. At the final step of the surgery, the optimal size of the femoral component for an adequate extension and flexion space was estimated. At this time, if a 4 mm additional bone resection was performed, it became the same surgical procedure as the measured resection technique. A smaller or bigger bone resection than 4 mm could be chosen for an adequate flexion gap as with the gap technique. Specifically, it could be adjusted to up to 4 mm larger than the measured size of the femoral component (Fig. 1).
The Student’s t-test and paired t-test were applied for statistical analysis; a p value of < 0.05 was considered statistically significant and results presented as mean and sd.
Results
After initial bone cutting by a femoral posterior condylar pre-cut with the PCL intact, the extension gap ranged from 9 mm to 24 mm (16.9 mm (sd 2.9)), and the corrected flexion gap by the amount of the pre-cut ranged from 13 mm to 30 mm (20.5 mm (sd 3.2)). There were wide variations in both gaps and neither could be predicted pre-operatively. The flexion gap was larger than the extension gap in almost all of the cases and the difference was significant (p < 0.001, Fig. 3). The difference between the two gaps ranged from -3 mm to 12 mm (3.6 mm (sd 2.7)). It seemed too wide to make equal extension and flexion gaps in every case (Fig. 4a).
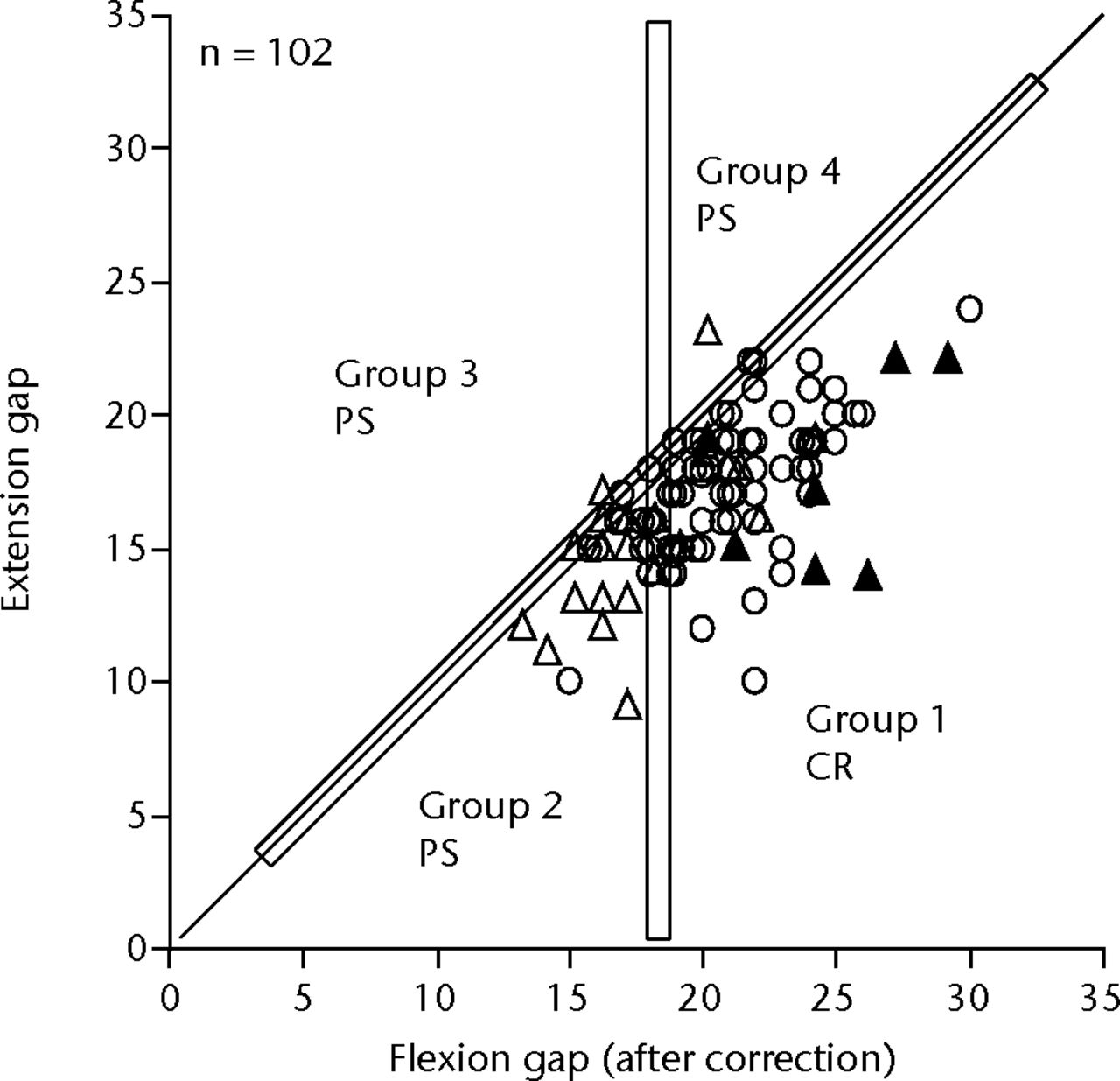
Fig. 3
Graph showing measurement results of the gaps after pre-cut of the femoral posterior condyle with the posterior cruciate ligament (PCL) preserved. The mean extension gap was 16.9 mm (sd 2.9) and the corrected flexion gap by the amount of the pre-cut was 20.5 mm (sd 3.2). The flexion gap was significantly larger than the extension gap (p < 0.001). The range of both gaps were too wide to know pre-operatively in each case. Cases with 18Â mm or more (minimum space to set the component) flexion gap and larger flexion gap than extension gap (Group 1) were implanted with a CR component, except for cases with PCL insufficiency. A PS component was implanted with the other cases (Group 2, 3 and 4). ○, implanted with CR component; ▵▴, implanted with PS component; ▴, PS implanted due to PCL insufficiency.
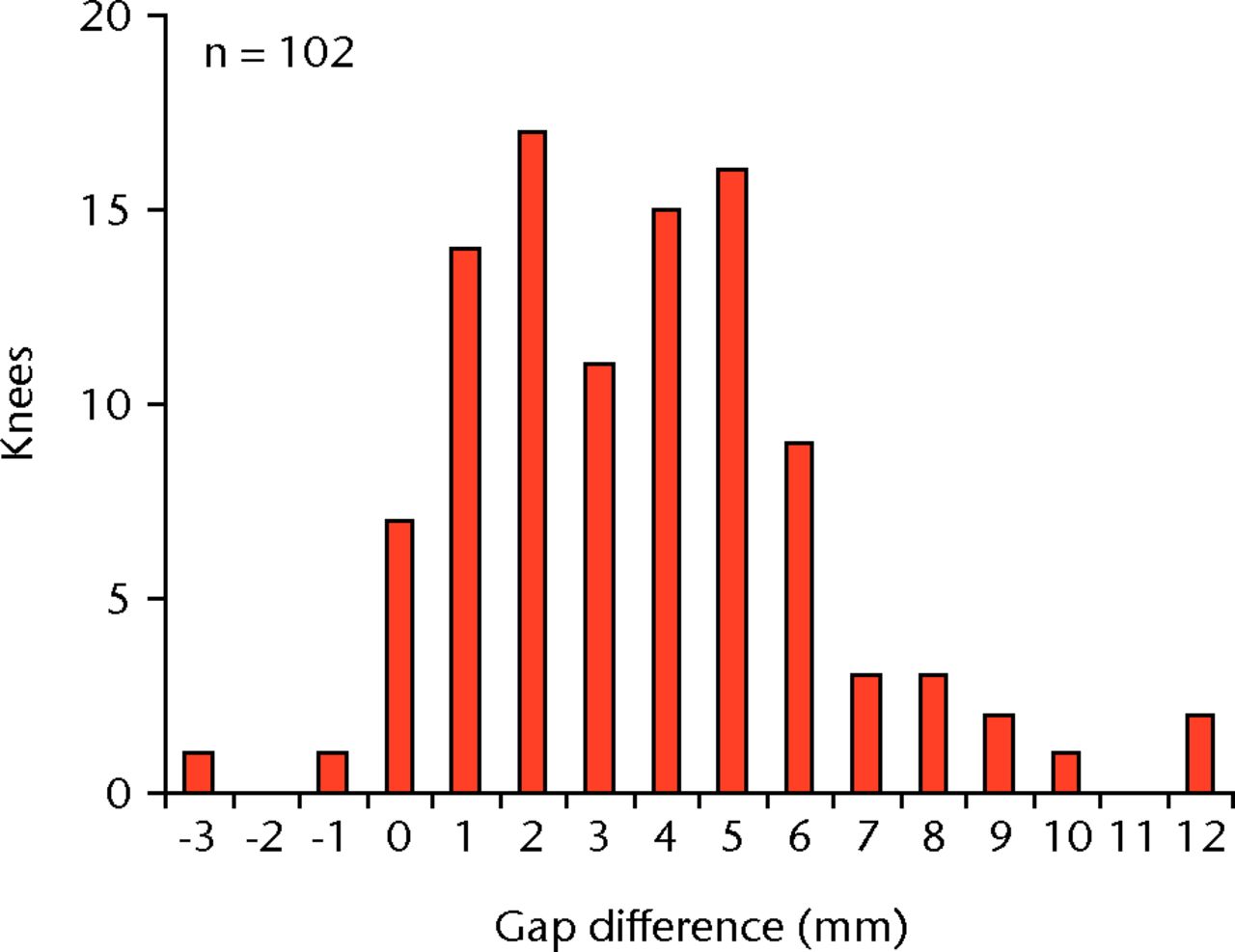
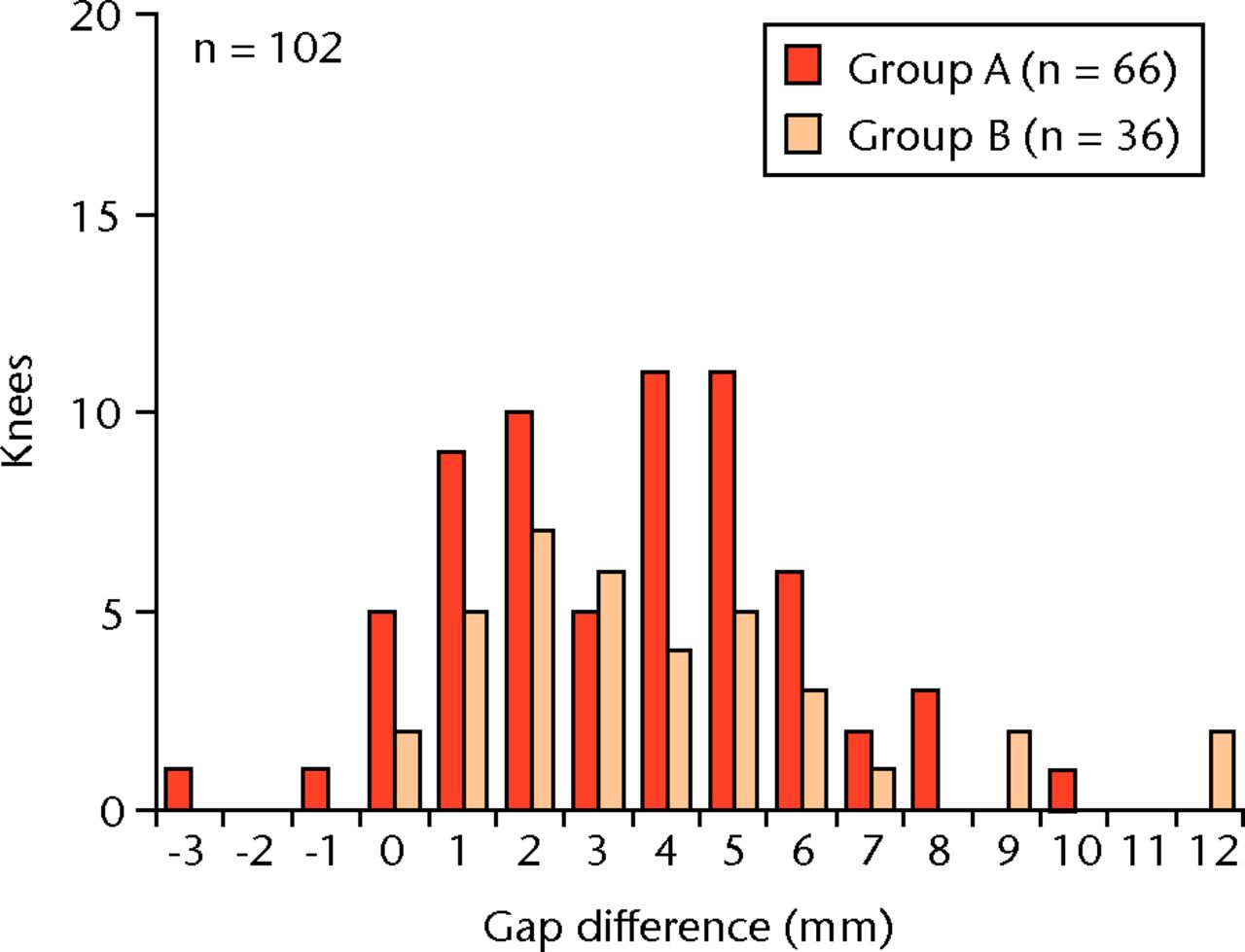
Figs. 4a - 4b
Figure 4a – Graph showing gap difference between the extension gap and the corrected flexion gap. The mean of the difference was 3.6 mm (sd 2.7) and the variation of the difference was wide. Figure 4b – Graph showing gap difference by group. Group A: pre-operative flexion contracture < 20°. Group B: flexion contracture ≥ 20°. The mean differences between extension and corrected flexion gaps were 3.4 mm (sd 2.5) in group A and 3.9 mm (sd 3.0) in group B, (p = 0.42). Additionally, if groups A and B are divided at flexion contracture of 15°, 25° and 30°, the p-values are 0.39, 0.38 and 0.20 respectively.
The extension and corrected flexion gaps were 17.2Â mm (sd 3.0) and 20.6 mm (sd 3.2) in group A and 16.3 mm (sd 2.8) and 20.2 mm (sd 3.3) in group B, respectively. The difference of the mean extension gap between the two groups was only 0.9 mm, which was not significantly different, and there was no significant difference in flexion gap between both groups (Fig. 5).
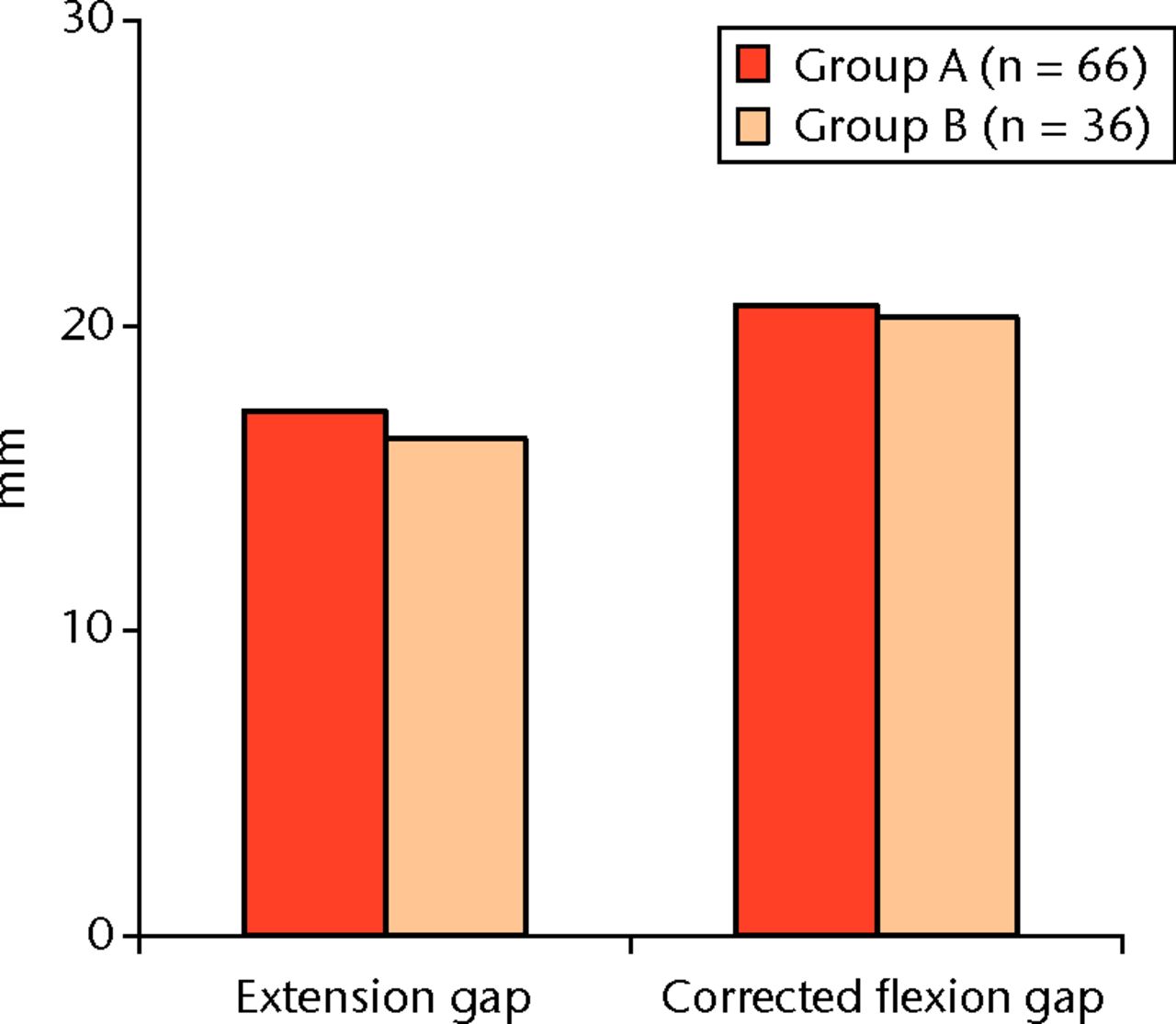
Fig. 5
Graph showing gaps and flexion contracture. The mean extension and corrected flexion gaps were 17.2 mm (sd 3.0) and 20.6 mm (sd 3.2) in group A and 16.3 mm (sd 2.8) and 20.2 mm (sd 3.3) in group B, respectively. There were no significant differences between the two groups.
The difference between the extension and flexion gap is the most important factor to make equal-sized extension-flexion gaps; this difference was also assessed in both groups. The mean differences between the extension and corrected flexion gap were 3.4 mm (sd 2.5) in group A and 3.9 mm (sd 3.0) in group B, which was not statistically significant. The variation of extension-flexion gap difference was very wide in both groups; however, cases of excessive gap difference (> 8 mm) were more common in group B (Fig. 4b).
Based on the measured gaps, the CR component was selected for use in 73 knees, and PS was used in only 29 knees. In the cases in which the PS was selected, the gap increase following PCL resection ranged from 0 mm to 3 mm (0.6 mm (sd 0.9)) in extension and from 0 mm to 7 mm (2.7 mm (sd 2.0)) in flexion, and the difference between the increases in both gaps was significant (p <  0.001). The gap increase in extension was 0 mm or 1 mm in almost all of the cases. Meanwhile, the variation of the flexion gap increase was too wide to predict before PCL resection (Fig. 6).
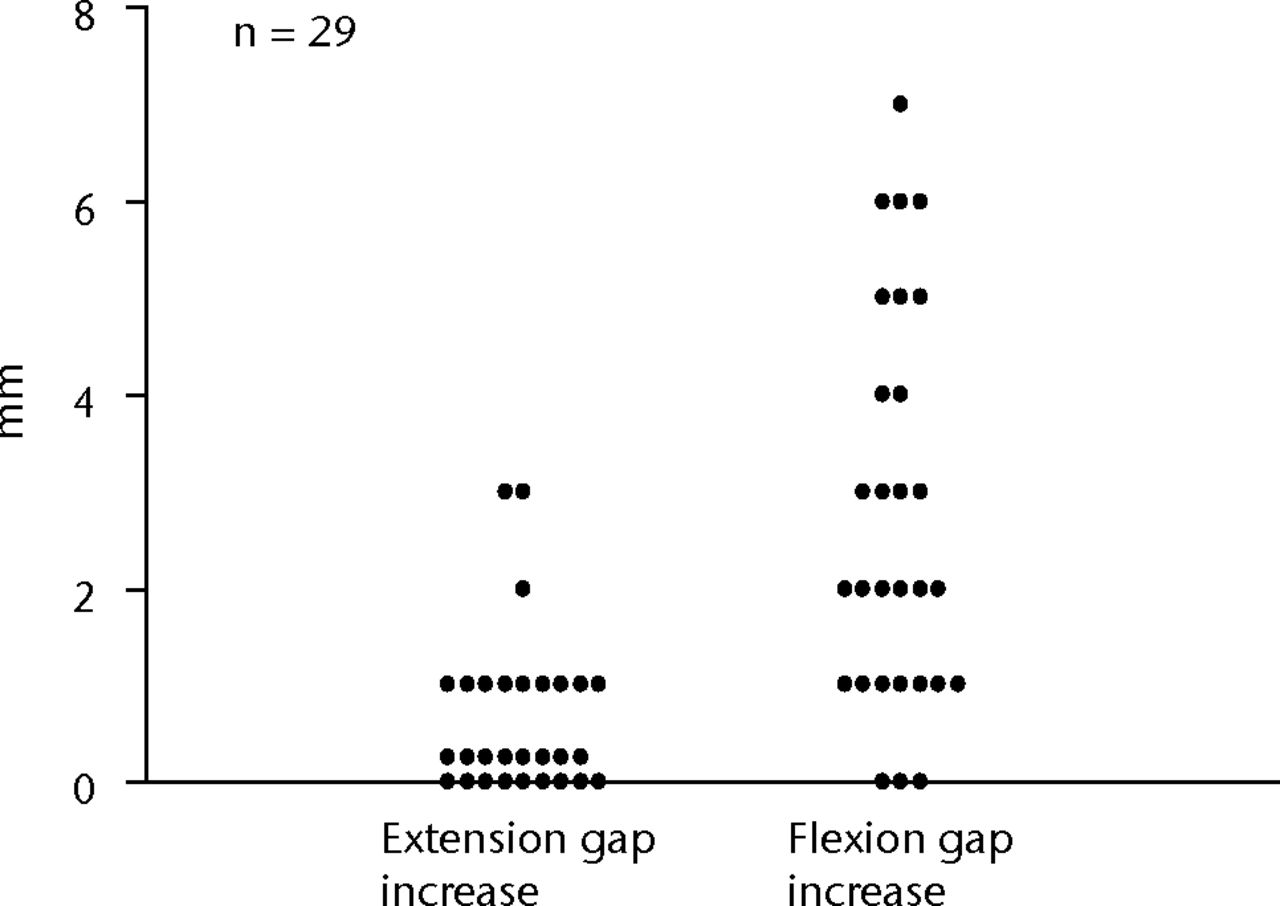
Fig. 6
Graph showing gap increase after posterior cruciate ligament (PCL) resection. The flexion gap increase was significantly larger than extension, and the variation of the flexion gap increase was wide. The gap increases following PCL resection were 0.6 mm (sd 0.9) in extension and 2.7 mm (sd 2.0) in flexion, and the difference between the increases of both gaps was significant (p < 0.001).
Selection of CR or PS is related to the amount of the flexion gap and the size of the femoral component, regardless of the pre-operative contracture or posterior osteophytes. Using a CR component, in the case of a small flexion gap a smaller femoral component is sufficient to create an appropriate flexion space, but it leads to undesirable reduction of a posterior condylar offset. In large flexion gap cases when the PS component is selected, the size of a femoral component needs to be larger, but there might be some limitations concerning medial-lateral over-size. Our results indicate a wide range of both gaps and a difficulty to know the gaps in each case pre-operatively. We used the CR component if there was enough space to set the components in flexion with the PCL intact; otherwise, the PS component was implanted. This concept developed a criteria in order to make the decision as to whether or not to preserve the PCL: cases with 18Â mm (minimum space to set the component) or more flexion gap and larger flexion gap than extension gap were suitable for a CR component; any other cases were suitable for a PS component (Fig. 3). As a result of using these criteria, in our cases, most knees were implanted with the adequate femoral component size relative to the measured size of the femur in those implanted with either CR or PS components (Fig. 7).
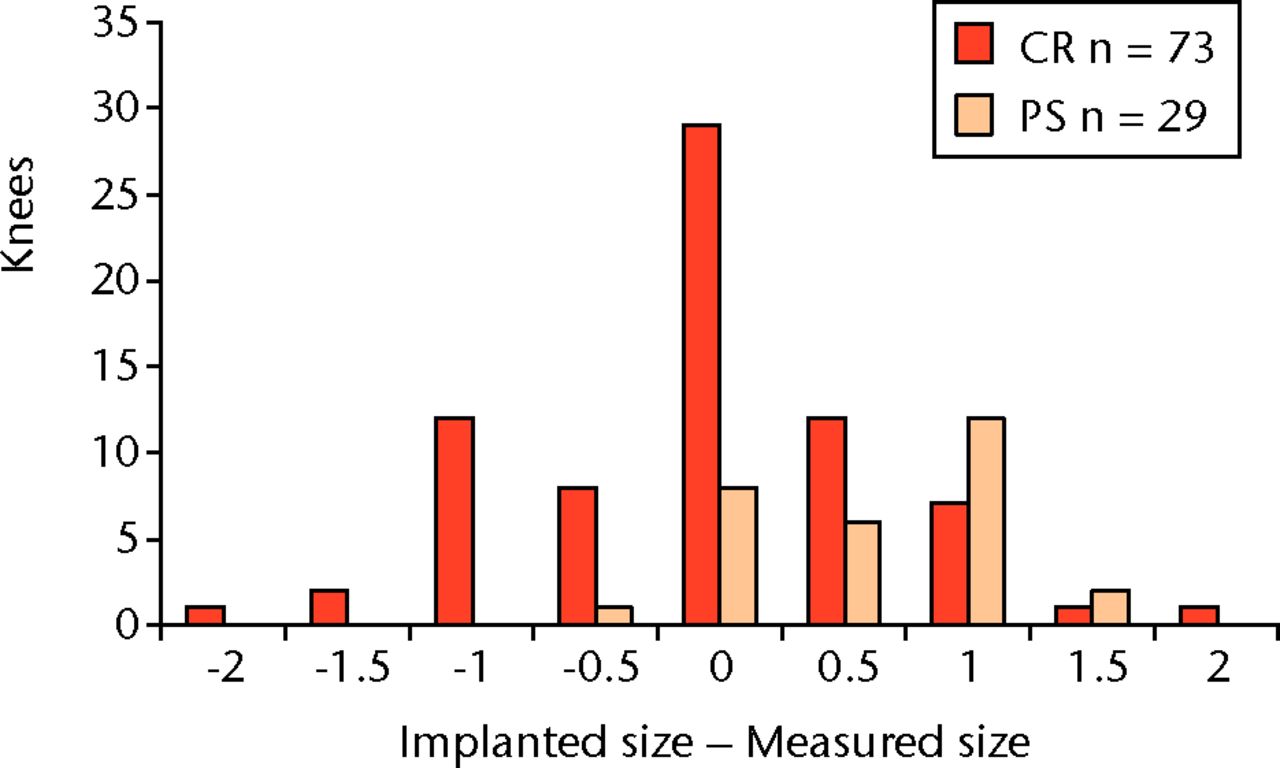
Fig. 7
Graph showing the difference between implanted and measured sizes of the femoral component. Most cases were implanted with ± 1 size compared with the measured size of the femur (CR, cruciate retaining; PS posterior substitute).
Discussion
TKR implant designs and materials have improved in recent decades. However, the selection criteria for use of the CR or PS component, one of the most fundamental factors in TKR, remains obscure. Both components have been widely used, with good clinical results,1-5 but there has been limited discussion regarding their faults.13-19 Although some surgeons may assert that using the PS component with the gap technique is useful for creating proper gaps during extension and flexion,16-19 there are simple limitations. It is not always easy to remove large posterior osteophytes with the gap technique, which may have some influence on the gaps unless femoral posterior condyles are resected. If the posterior osteophytes are removed after both the extension and flexion gaps are made, these gap amounts will change.20,21
We found that flexion gaps were larger than extension gaps in most of the cases, and the PCL resection made flexion gaps wider (up to 7 mm). The gap technique can control the flexion gap by adjusting the size of the femoral component, but there might be some limitations concerning medial-lateral over-size. A large femoral component, relative to the measured size, leads to an undesirable medial-lateral overhang of the femoral component. Meanwhile, our results indicate that the combination of the measured resection technique and the use of a PS component, introduces the possibility of an overly large flexion gap (Figs 3, 4a, 6). Following the measured resection of the femur, it is difficult to change the gaps, even if the acquired gaps were inadequate.
On the other hand, the CR component also has some faults. In cases of small flexion gaps due to a tight PCL, it is necessary to diminish the femoral component size with a CR component. This leads to a small femoral posterior offset, which can limit knee flexion. Although, some surgeons may say that it is useful to partially release the PCL in cases of a small flexion gap in CR TKR, there is a limitation. Our results demonstrated that the widening of the flexion gap after PCL resection is variable, and some cases showed minimal increase of flexion gaps, even with complete PCL resection (Fig. 6).
The reasons why flexion gaps are larger than extension gaps in PCL-maintained knees are multifactorial and ambiguous. One of the reasons is probably related to relative PCL loosening because of ACL deficiency. Christen et al22 and Heesterbeek et al23 reported that PCL orientation with the knee at 90° was elevated by tension between the femur and tibia in ACL-deficient knees. The elevated PCL orientation may cause a flexion gap increase with the appropriate distraction force between the femur and tibia.
Another reason for the bigger flexion gap, compared with the extension gap, involves pre-operative flexion contracture, which was generally considered a decreasing factor of extension gaps.12,24-26 Although pre-operative flexion contracture is reported to influence extension gaps, we found the mean difference of the extension gaps between groups A and B was only about 1Â mm and there was no significant difference (Fig. 5). In this study, a 30 lbs distraction force was applied to measure the gaps, however, it might not have been enough to reveal the difference. The actual reason as to why there was no significance is still unclear.
From a viewpoint of gap difference between the flexion and extension, a gap difference of 5 mm or more was often seen in both groups A and B; however, extremely difficult cases with > 8 mm difference were more common in group B and there was no case with a larger extension gap than that of the flexion gap in group B (Fig. 4b). The pre-operative flexion contracture could have had some influence on the gap situation in our cases, despite the lack of significant difference in extension gaps between the two groups. Although each factor of PCL orientation and flexion contracture may have small influences on the gaps, the combined effects may become significant.
The importance of equal extension and flexion gaps in TKR has been discussed; however, how this goal is achieved remains unclear. Insall27 described PCL management in TKR:
It must also be accepted that not all arthritic knees are suitable for PCL-retaining designs, and there must be more objective methods for deciding when the PCL is too tight or so loose as to be rendered nonfunctional. When the PCL is not fulfilling its purpose within acceptable and defined limits, a PCL release may be performed or, alternatively, a posterior stabilized design adopted. Many newer knee systems allow an intraoperative switch from PCL retention to PCL substitution, and in my view this is the way of the future. 27
To create adequate extension and flexion gaps, intra-operative gap measurement in each knee and proper component choice are important. As he described, from a view point of gap adjustment, it seems that some knees are not suitable for a PCL-retaining component and some are not suitable for a PCL-substitute component and it is difficult to decide pre-operatively which to use for an adequate gap. Our results support his assertion by numerical data (Fig. 3). The technique in this report is only aimed at achieving perfect gap control in TKR. For this purpose, PCL function as a roll-back producer was neglected, and the intra-operative gap measurement in PCL preservation was performed to investigate the individual gap characteristics of each knee. Component type was decided intra-operatively by the measured gaps, without any preconceptions.
Our results indicate that the selection of the PS component in all cases would have resulted in much larger flexion gaps in many cases. An adequate extension and flexion gap can be attained to a limited extent, of course, by using a larger femoral component to make the flexion gap smaller and by performing an additional resection of the distal femur to make the extension gaps bigger, but this technique is limited.
Conversely, the use of a CR component in the case of a small flexion gap requires a femoral component smaller than the measured size to optimise the flexion gap, compared with the extension gap. This, however, leads to a smaller posterior condylar offset, which is inappropriate for good knee flexion. Considering the gap amounts and the adequate size of the femoral component, the criteria for PCL preservation or sacrifice can be discussed. To attain an adequately sized femoral component in cases where the extension gap is larger than the flexion gap, it is necessary to create an adequate flexion gap by cutting the PCL (groups 3 and 4, Fig. 3). In the cases in which the flexion gap is small, it also becomes necessary to cut the PCL and create a sufficient flexion gap (groups 2 and 3, Fig. 3). This is complicated in group 2 (Fig. 3), and an additional cut of the proximal tibia should be considered first. If the flexion gap is still not large enough, PCL resection should be considered. To achieve the appropriate size for the femoral component and adequate extension and flexion gaps, PCL resection and additional cutting of the distal femur and proximal tibia should be considered. Selection of the PS component leads to safer control of the extension and flexion gaps in groups 2, 3, and 4. Meanwhile, selection of the CR component only leads to better results in group 1, but the number of cases is not small (Fig. 3). Given the wide variations in the extension and flexion gaps, the difference between the two gaps and the flexion gap increase after PCL resection, it would be difficult to only use one component (CR or PS) in every case. To attain a femoral component of an adequate size that provides appropriate gaps, better results are achieved by deciding which component to use (CR or PS) based on intra-operative gap measurement.
Limitations
The chief limitation of this study was the measurement method. In this study, 30 lbs of tension was applied as a distracting force between the femur and tibia. However, it is still unknown how much force is appropriate for gap measurement. Additionally, the influence of gravity on the flexion gap measurement has not yet been discussed. We believe it is better to measure the flexion gap when at least some effort has been made to avoid the influence of the thigh weight. Therefore, we measured the flexion gap with the thigh held by the surgeon’s hand to prevent lifting of the lower leg. However, the accuracy of this method is not verified.
1 Colizza WA , InsallJN, ScuderiGR. The posterior stabilized total knee prosthesis: assessment of polyethylene damage and osteolysis after a 10 year minimum follow-up. J Bone Joint Surg [Am]1995;77-A:1713–1720. Google Scholar
2 Migakaka KC , RanawatC, MullajiA. 10 to 20 years follow-up of total knee arthroplasty for valgus deformities. Clin Orthop Relat Res1997;345:29–37. Google Scholar
3 Ritter MA , HerbstSA, KeatingEM, FarisPM, MedingJB. Long-term survival analysis of a posterior cruciate-retaining total condylar total knee arthroplasty. Clin Orthop Relat Res1994;309:136–145.PubMed Google Scholar
4 Tanzer M , SmithK, BurnettS. Posterior-stabilized versus cruciate-retaining total knee arthroplasty. Balancing the gap. J Arthroplasty2002;17:813–819. Google Scholar
5 Rand JA , TrousdaleRT, IlstrupDM, HarmsenWS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg [Am]2003;85-A:259–265.CrossrefPubMed Google Scholar
6 Mahoney OM , NoblePC, RhoadsDD, AlexanderJW, TullosHS. Posterior cruciate function following total knee arthroplast: a biomechanical study. J Arthroplasty1994;9:569–578. Google Scholar
7 Most E , ZayontzS, LiG, et al.Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop Relat Res2003;410:101–113.CrossrefPubMed Google Scholar
8 Banks SA , MarkovichGD, HodgeWA. In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplasty1997;12:297–304.CrossrefPubMed Google Scholar
9 Stiehl JB , KomistekRD, DennisDA, PaxsonRD, HoffWA. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg [Br]1995;77-B:884–889.PubMed Google Scholar
10 Kadoya Y , KobayashiA, KomatsuT, NakagawaS, YamanoY. Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res2001;391:210–217.CrossrefPubMed Google Scholar
11 Yagishita K , MunetaT, IkedaH. Step-by-step measurements of soft tissue balancing during total knee arthroplasty for patients with varus knees. J Arthroplasty2003;18:313–320.CrossrefPubMed Google Scholar
12 Berend K , LombardiAV Jr, AdamsJ. Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Clin Orthop Relat Res2006;452:83–87.CrossrefPubMed Google Scholar
13 Townley CO . The anatomic total knee resurfacing arthroplasty. Clin Orthop Relat Res1985;192:82–96.PubMed Google Scholar
14 Hungerford DS , KrackowKA. Total joint arthroplasty of the knee. Clin Orthop Relat Res1985;192:23–33. Google Scholar
15 Hanada H , WhitesideLA, SteigerJ, DyerP, NaitoM. Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop Relat Res2007;462:137–142.CrossrefPubMed Google Scholar
16 Insall JN , BibazziR, SoudryM, MestrinerLA. Total knee arthroplasty. Clin Orthop Relat Res1985;192:13–22.CrossrefPubMed Google Scholar
17 Insall JN . Presidential address to The Knee Society: choices and compromises in total knee arthroplasty. Clin Orthop Relat Res1988;226:43–48. Google Scholar
18 Dennis DA. Measured resection: An outdated technique in total knee arthroplasty. Orthopedics 2008;31:940, 943-4. Google Scholar
19 Dennis DA , KomistekRD, KimRH, SharmaA. Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res2010;468:102–107.CrossrefPubMed Google Scholar
20 Sugama R , KadoyaY, KobayashiA, TakaokaK. Preparation of the flexion gap affects the extension gap in total knee arthroplasty. J Arthroplasty2005;20:602–607.CrossrefPubMed Google Scholar
21 Baldini A , ScuderiGR, AgliettiP, ChalnickD, InsallJN. Flexion-extension gap changes during total knee arthroplasty: effect of posterior cruciate ligament and posterior osteophytes removal. J Knee Surg2004;17:69–72.CrossrefPubMed Google Scholar
22 Christen B , HeesterbeekP, WymengaA, WehrliU. Posterior cruciate ligament balancing in total knee replacement: the quantitative relationship between tightness of the flexion gap and tibial translation. J Bone Joint Surg [Br]2007;89-B:1046–1050.CrossrefPubMed Google Scholar
23 Heesterbeek P , KeijsersN, JacobsW, VerdonschotN, WymengaA. Posterior cruciate ligament recruitment affects antero-posterior translation during flexion gap distraction in total knee replacement, An intraoperative study involving 50 patients. Acta Orthop2010;81:471–477. Google Scholar
24 Ritter M , LutgringJ, DavisK, et al.The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty2007;22:1092–1096.CrossrefPubMed Google Scholar
25 Griffin F , InsallJ, ScuderiG. Accuracy of soft tissue balancing in total knee arthroplasty. J Arthroplasty2000;15:970–973.CrossrefPubMed Google Scholar
26 Scuderi G , KochharT. Management of flexion contracture in total knee arthroplasty. J Arthroplasty2007;22(4 Suppl 1):20–24.CrossrefPubMed Google Scholar
27 Insall JN. Surgery of the knee. Vol. 2. Second ed. New York: Churchill-Livingstone, 1993:754. Google Scholar
Funding statement:
None declared
Author contributions:
R. Kaneyama: Writing the paper, Data management and collection, Study design
M. Otsuka: Adviser for study design, Preliminary study co-worker.
H. Shiratsuchi: Adviser for study design, Writing the paper, Data management, Surgical assistance.
K. Oinuma: Adviser for study design, Writing the paper, Data management, Surgical assistance.
Y. Miura: Data collection, Surgical assistance
T. Tamaki: Data collection, Surgical assistance.
ICMJE Conflict of Interest:
None declared
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










