Abstract
Objective
In ex vivo hip fracture studies femoral pairs are split to create two comparable test groups. When more than two groups are required, or if paired femurs cannot be obtained, group allocation according to bone mineral density (BMD) is sometimes performed. In this statistical experiment we explore how this affects experimental results and sample size considerations.
Methods
In a hip fracture experiment, nine pairs of human cadaver femurs were tested in a paired study design. The femurs were then re-matched according to BMD, creating two new test groups. Intra-pair variance and paired correlations in fixation stability were calculated. A hypothetical power analysis was then performed to explore the required sample size for the two types of group allocation.
Results
The standard deviation (sd) of the mean paired difference in fixation stability increased from 2 mm in donor pairs to 5 mm in BMD-matched pairs. Intra-pair correlation was 0.953 (Pearson’s r) in donor pairs and non-significant at -0.134 (Pearson’s r) in BMD-matched pairs. Required sample size to achieve a statistical power of 0.8 increased from ten pairs using donor pairs to 54 pairs using BMD-matched pairs.
Conclusion
BMD cannot be used to create comparable test groups unless sample size is increased substantially and paired statistics are no longer valid.
Cite this article: Bone Joint Res 2014;3:317–20.
Article focus
Using human cadaver femurs is regarded as the gold standard in ex vivo hip fracture fixation studies
When pairs of femurs from the same donor cannot be achieved, pairing according to bone mineral density (BMD) is sometimes performed
The aim of this study was to evaluate the statistical consequences of pairing cadaver femurs according to BMD in ex vivo hip fracture fixation experiments when compared with donor pairs
Key messages
Compared with donor pairs, the intra-pair variance in BMD-matched pairs increased considerably and the intra-pair correlation was not significant
The required sample size to achieve a statistical power of 0.8 increased from ten pairs using donor pairs to 54 pairs using BMD-matched pairs
Paired statistics are no longer valid when the femurs are matched according to BMD
Strengths and limitations
Strengths: the test setup was designed to recreate the clinical situation and not to test the extremes
This statistical experiment clearly shows the importance of creating comparable test groups in ex vivo biomechanical experiments that traditionally include a limited number of specimens
Limitation: the study only evaluates pairing according to BMD and donor and not other possible methods of pairing femurs
Introduction
Paired designs are chosen in comparative experiments in order to minimise the effects of femur variation and thereby create comparable test groups. The sample variance is crucial in comparative statistics as increased variance within a given sample decreases statistical power. Consequently, restricting variability within pairs used in comparative studies reduces the required sample size, which is most welcomed amongst researchers working with limited resources such as cadaver bones.
The femoral size, neck–shaft angle, neck and head version and other geometrical factors show great variation between individuals.1 In addition, the relative distribution of cortical and trabecular bone and bone porosity change with ageing.2,3 All of these factors influence the biomechanical properties of human femurs and have the potential to affect the outcomes in experimental hip fracture studies. Using a paired study design, left and right femurs from the same donor can be randomly assigned to one of two modes of treatment.4-8 If paired femurs from the same donor cannot be obtained, or when more than two groups are to be compared, pairing the femurs according to bone mineral density (BMD) seems to be the method of choice.9-11
In a previous study we compared implant A (three screws in an inverted triangle configuration locked in a lateral support plate) and implant B (three screws in an inverted triangle configuration) when used for fixation of fractures of the femoral neck.12 The femurs were paired by donors with the implants randomly allocated to the left or right femur. The main finding was that implant A slightly but significantly improved the stability of the construct. We present here a re-analysis of the obtained data following splitting of the donor pairs with subsequent new pairing according to BMD. The statistical effects were evaluated to see if this mode of matching could produce statistical strength equal to that of donor pairs.
Materials and Methods
For a detailed description of the experimental setup we refer to a previously published paper.12 After receiving approval from the Regional Committee for Medical and Health Research Ethics, 18 fresh-frozen femurs from nine donors underwent Dual Energy X-Ray Absorptiometry (DXA) to obtain femoral neck BMD (Lunar iDXA, GE Healthcare, Madison, Wisconsin). Standardised subcapital fractures of the femoral neck were fixed using implant A or implant B and the femurs were tested in a hip simulator. The femurs completed 10 000 cycles of subject-specific axial load and torque based on the weight of the donor (joint resultant force 2.5 × bodyweight; sd 0.2). Three-dimensional migrations of the femoral head fragments were captured by an optical motion tracker system (Polaris Spectra, NDI, Ontario, Canada). Femoral head fragment migration described the stability of the fracture fixation. In group A, femoral pairs were matched according to donor. In group B, each femur was paired to the femur with the closest match in BMD other than its biological counterpart. For example, in donor pair 1, the two femurs had BMDs of 0.839 g/cm2 and 0.928 g/cm2, respectively. The femur allocated to implant group A was then matched to the femur in implant group B with a BMD of 0.887 g/cm2, which was the closest match.
Statistical analysis
All calculations were performed using IBM SPSS Statistics (version 20; SPSS Inc., Chicago, Illinois) and IBM SPSS Sample Power (version 3; IBM Corp., Armonk, New York). Normality of data was assessed by the Shapiro–Wilk test, and parametric and non-parametric statistics were performed accordingly. Level of significance was set to 0.05 for all tests. Levene’s test, based on mean or ranks,13 tested equality of variance. Pearson’s correlation coefficients14 of femoral head fragment migrations within pairs were calculated. A related samples t-test tested the null hypothesis that construct stability using implant A and implant B was equal. Obtained data from these calculations were then used in a hypothetical power analysis to explore the effect of different grouping on required sample size when considering 2 mm difference in femoral head fragment migration to be of potential clinical relevance.
Results
Intra-pair differences of BMD
The mean (95% confidence interval (CI)) difference in BMD of donor pairs was 0.068 g/cm2 (0.045 to 0.091) and 0.079 g/cm2 (0.050 to 0.111) of BMD-matched pairs. The difference in variance was not statistically different in the two groups (p = 0.420).
Stability of the femoral head fragment
The mean paired difference in head fragment migration using implant A and implant B was 1.6 mm. The sd (mm) increased from 2.0 to 5.0 when paired according to BMD (p = 0.118).
The correlation of femoral head fragment migrations within pairs was highly significant when using donor pairs (Pearson’s r 0.953, p < 0.000). This correlation was lost in BMD-matched pairs (Pearson’s r -0.134, p = 0.730) (Fig. 1) (Fig. 1).
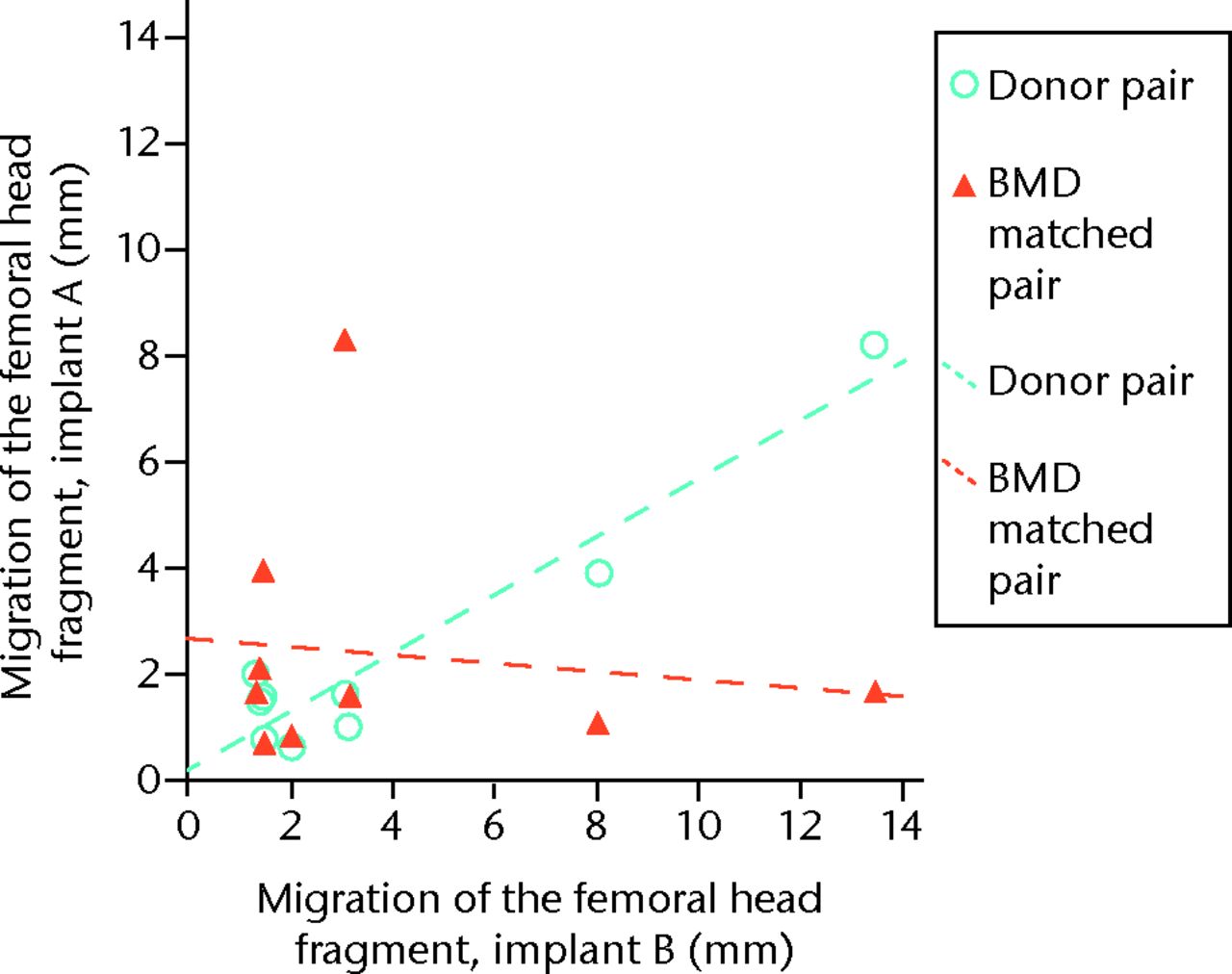
Fig. 1
Graph showing intra-pair correlations of femoral head fragment migrations.
Using donor pairs, the difference of 1.6 mm in femoral head fragment migration between implant group A and group B reached statistical significance (95% CI 0.1 to 3.1, p = 0.040). In BMD-matched pairs this difference was not significant (95 % CI -2.27 to 5.47, p= 0.368) (Fig. 2) (Fig. 2).
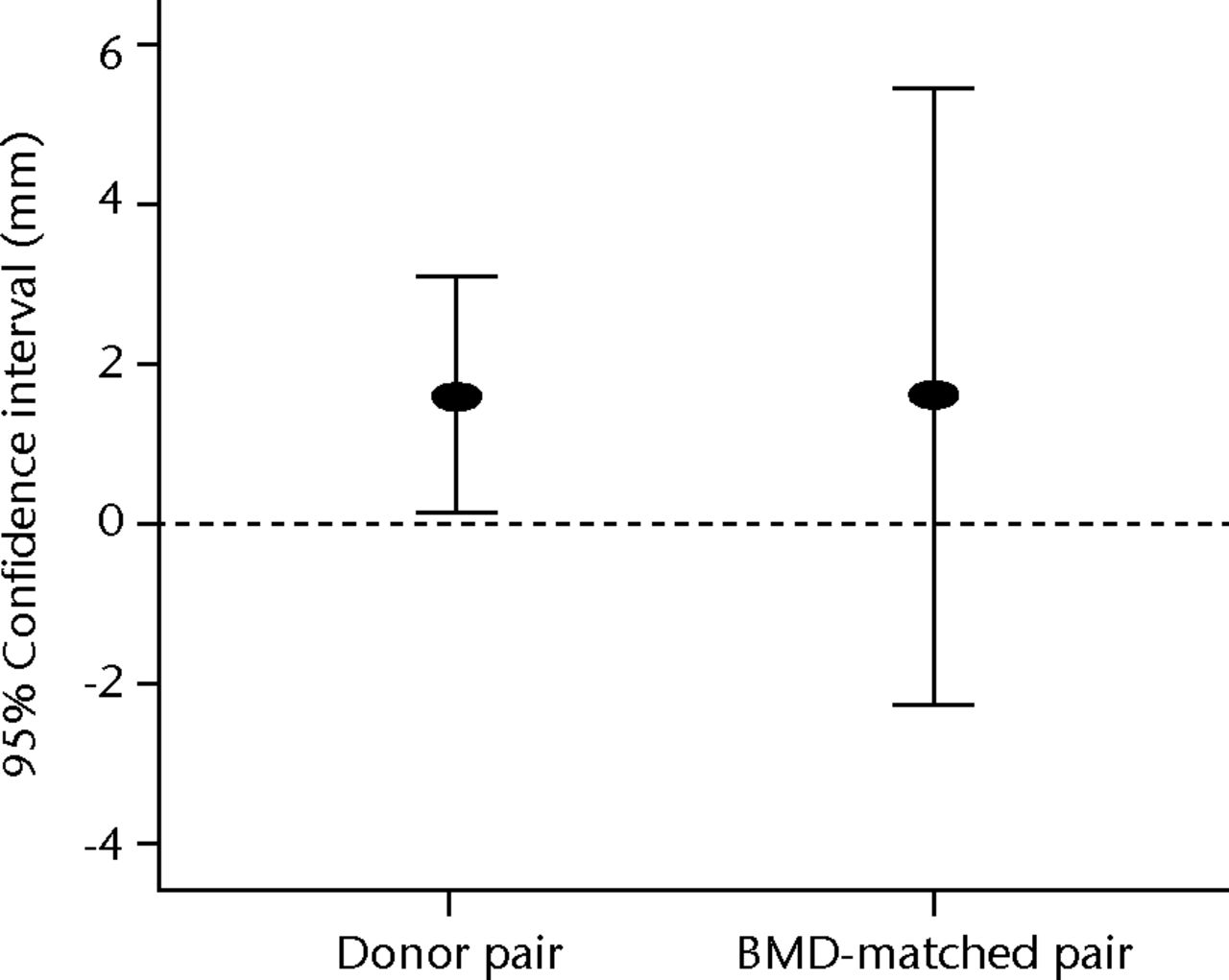
Fig. 2
Graph showing the slightly statistically significant difference between the two implant groups using donor pairs, which is lost in BMD-matched pairs due to increased variance.
The sds of the difference in femoral head fragment migration in donor pairs and in BMD-matched pairs were used to calculate the hypothetical sample size required to test a difference in migration of 2 mm. To obtain statistical power of 80%, ten pairs were needed when using donor pairs and 54 pairs were needed when using BMD-matched pairs (Fig. 3).
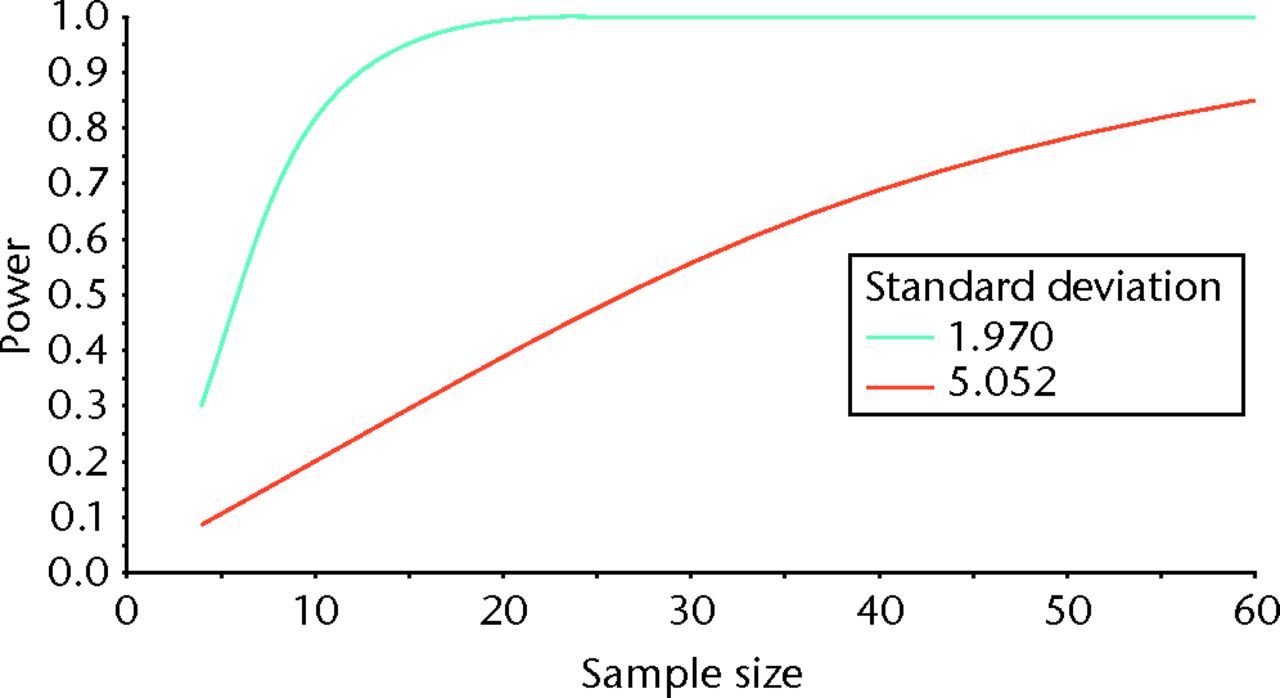
Fig. 3
Graph showing sample size estimation for BMD-matched pairs (orange line) and donor pairs (green line).
Discussion
Re-pairing donor pairs according to BMD did not change the within-group variance in BMD. Consequently, the observed differences within and between donor pairs and BMD-matched pairs cannot be explained by an initial difference in BMD.
The sample size in this experiment was small but reflects the number of femurs often used in biomechanical hip fracture experiments, regardless of the mode of matching. This is reflected by all of the comparative studies cited here. However, the results from this statistical experiment are rather unambiguous: after operating the fractures of the femoral neck with implant A or implant B and testing the constructs for fixation stability, the related sample correlation was 0.953 when using donor pairs. This correlation was -0.134 and non-significant in the BMD-matched pairs. Consequently, paired statistics can no longer be used and statistics for independent samples must be performed instead. When adding that the sd increased from 2 mm to 5 mm following re-pairing, the results showed that a fivefold increase in sample size was needed to compensate for this when seeking a statistical power of 80%. Ignoring this when setting up hip fracture experiments increases the risk of missing an existing effect (type II error).
The mechanical property of the human femur is not only determined by its microstructure such as bone mineral content. Femoral size, neck length, neck diameter, neck–shaft angle and anteversion angle must also be considered important factors in providing stable bone-implant constructs. Matching the pairs according to BMD alone does not take into account these factors as two anthropometrically different femurs might have similar BMDs.
In conclusion, pairing femurs according to BMD does not appear to be a good alternative to donor-matched pairs as the intra-pair variances increase. When more than two methods are to be compared, or if paired femurs from the same donor cannot be obtained, the sample size must be increased substantially to provide valid results.
1 Toogood PA , SkalakA, CoopermanDR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res2009;467:876–885.CrossrefPubMed Google Scholar
2 Mayhew PM , ThomasCD, ClementJG, et al.Relation between age, femoral neck cortical stability, and hip fracture risk. Lancet2005;366:129–135.CrossrefPubMed Google Scholar
3 Zebaze RM , Ghasem-ZadehA, BohteA, et al.Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet2010;375:1729–1736.CrossrefPubMed Google Scholar
4 Windolf M , BraunsteinV, DutoitC, SchwiegerK. Is a helical shaped implant a superior alternative to the Dynamic Hip Screw for unstable femoral neck fractures? A biomechanical investigation. Clin Biomech (Bristol, Avon)2009;24:59–64.CrossrefPubMed Google Scholar
5 Brandt E , VerdonschotN, van VugtA, van KampenA. Biomechanical analysis of the percutaneous compression plate and sliding hip screw in intracapsular hip fractures: experimental assessment using synthetic and cadaver bones. Injury2006;37:979–983.CrossrefPubMed Google Scholar
6 Röderer G , MollS, GebhardF, ClaesL, KrischakG. Side plate fixation vs. intramedullary nailing in an unstable medial femoral neck fracture model: a comparative biomechanical study. Clin Biomech (Bristol, Avon)2011;26:141–146.CrossrefPubMed Google Scholar
7 Krischak GD , AugatP, BeckA, et al.Biomechanical comparison of two side plate fixation techniques in an unstable intertrochanteric osteotomy model: sliding hip screw and percutaneous compression plate. Clin Biomech (Bristol, Avon)2007;22:1112–1118.CrossrefPubMed Google Scholar
8 von der Linden P , GisepA, BonerV, et al.Biomechanical evaluation of a new augmentation method for enhanced screw fixation in osteoporotic proximal femoral fractures. J Orthop Res2006;24:2230–2237.CrossrefPubMed Google Scholar
9 Rupprecht M , GrossterlindenL, RueckerAH, et al.A comparative biomechanical analysis of fixation devices for unstable femoral neck fractures: the Intertan versus cannulated screws or a dynamic hip screw. J Trauma2011;71:625–634. Google Scholar
10 Aminian A , GaoF, FedoriwWW, et al.Vertically oriented femoral neck fractures: mechanical analysis of four fixation techniques. J Orthop Trauma2007;21:544–548.CrossrefPubMed Google Scholar
11 Rupprecht M , GrossterlindenL, SellenschlohK, et al.Internal fixation of femoral neck fractures with posterior comminution: a biomechanical comparison of DHS® and Intertan nail.®. Int Orthop2011;35:1695–1701. Google Scholar
12 Basso T , KlaksvikJ, FossOA. The effect of interlocking parallel screws in subcapital femoral-neck fracture fixation: a cadaver study. Clin Biomech (Bristol, Avon)2014;29:213–217.CrossrefPubMed Google Scholar
13 Nordstokke DW , ZumboBD. A new nonparametric levene test for equal variances. Psicológica2010;31:401–430. Google Scholar
14 Rosner B Fundamentals of Biostatistics . 7th Ed, Boston, Massachusetts: Brooks/Cole, 2011. Google Scholar
Funding statement:
The study was funded by the Orthopaedics Department at St. Olavs Hospital.
Author contributions:
T. Basso: Data collection, Data analysis, Writing the first draft of the paper, Co-ordinating revisions.
J. Klaksvik: Data collection, Data analysis, Revision of the manuscript.
O. A. Foss: Data collection, Data analysis, Revision of the manuscript.
ICMJE Conflict of Interest:
None declared
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










