Abstract
Objectives
There are several reports clarifying successful results following open reduction using Ludloff’s medial approach for congenital (CDH) or developmental dislocation of the hip (DDH). This study aimed to reveal the long-term post-operative course until the period of hip-joint maturity after the conventional surgical treatments.
Methods
A long-term follow-up beyond the age of hip-joint maturity was performed for 115 hips in 103 patients who underwent open reduction using Ludloff’s medial approach in our hospital. The mean age at surgery was 8.5 months (2 to 26) and the mean follow-up was 20.3 years (15 to 28). The radiological condition at full growth of the hip joint was evaluated by Severin’s classification.
Results
All 115 hips successfully attained reduction after surgery; however, 74 hips (64.3%) required corrective surgery at a mean age of 2.6 years (one to six). According to Severin’s classification, 69 hips (60.0%) were classified as group I or II, which were considered to represent acceptable results. A total of 39 hips (33.9%) were group III and the remaining seven hips (6.1%) group IV. As to re-operation, 20 of 21 patients who underwent surgical reduction after 12 months of age required additional corrective surgeries during the growth period as the hip joint tended to subluxate gradually.
Conclusion
Open reduction using Ludloff’s medial approach accomplished successful joint reduction for persistent CDH or DDH, but this surgical treatment was only appropriate before the ambulating stage.
Cite this article: Bone Joint Res 2014;3:1–6.
Article focus
Several reports with mid-term follow-up have clarified successful results following open reduction using Ludloff’s medial approach for congenital (CDH) or developmental dislocation of the hip (DDH)
This study aimed to provide longer follow-up until the age of hip-joint maturity, which is crucial to assess the success of this surgical method
Key messages
All 115 hips successfully attained reduction after surgery
A total of 74 hips (64%) required additional corrective surgery
Patients undergoing surgical reduction after 12 months of age were very likely to require further corrective surgery (incidence of 95%)
Strengths and limitations
This is a long-term follow-up study with a substantial number of patients
This study is based on the experience of a single surgeon
Introduction
The term congenital dislocation of the hip (CDH) has been replaced by developmental dislocation (dysplasia) of the hip (DDH).1,2 In a narrow sense, for CDH the femoral head must be dislocated out of the acetabulum cavity at birth, but such cases are very rare and sometimes difficult to diagnose immediately after birth. In addition, pathological differentiation between CDH and DDH appears to be very difficult, especially if a patient does not have an obvious pre-natal deficit or genetic abnormality.1 The treatment strategy is also similar as the aims of treatment are to obtain normal joint congruity and to encourage ordinal development of the hip joint, regardless of when the dislocation is found. However, there are many controversial points, such as appropriate initial conservative attempts, timing of surgical reduction, ideal surgical approach and necessity of combined surgery.3-7 The reason for such controversy can be attributed to the lack of studies reporting long-term follow-up until full growth of the hip joint is achieved.
The authors have performed open reduction for over 40 years using a medial (known as Ludloff’s8) approach with a small skin incision. As the authors’ surgical strategy is based on the concept that immature joint structures in these patients have the potential to recover a normal growth process after successful reduction,9 open reduction alone is selected as early as possible for patients aged < two years. This study was designed to investigate the rate of further surgery following this treatment and to evaluate radiological results at full growth by a long-term follow-up of more than 15 years. The final aim was to clarify the benefits and limitations of open reduction alone for infantile hip dislocation.
Patients and Methods
A total of 222 hips in 194 patients were treated with open reduction alone via the medial approach between 1967 and 1984 in the authors’ hospital. After excluding those with radiological follow-up < 15 years, a total of 115 hips in 103 patients (involving 12 bilateral cases) were included in this study (52% follow-up rate).
There were 84 females and 19 males, with a mean age at surgery of 8.5 months (two to 26). They were followed for a mean of 20.3 years (15 to 28). As most patients aged > 12 months had attained joint reduction conservatively, 88 patients (85%) of these surgically treated patients were aged < 12 months. A total of 95 hips in 85 patients had undergone previous treatment, comprising a Pavlik harness in 84 hips, manual reduction in seven and overhead traction in four. Open reduction was indicated for patients with unsuccessful reduction using a Pavlik harness during infancy. We performed arthrography under general anesthesia in all patients who failed to get complete reduction. Most infantile hip joints were able to get reduction by gentle traction force, unless any specific intra-articular intervening structures were found. Joints that could not maintain a reduced position due to intra-articular intervening structures clearly shown by the arthrography, were also candidates for the surgical treatment.10
Surgical procedure and intra-operative findings
A 3 cm to 4 cm skin incision was made along the adductor muscle and the anterior aspect of the joint exposed via the intermuscular approach. The branch of the medial circumferential artery was not ligated. The iliopsoas tendon was dissected when it was so tight that it prevented mobility of the femoral head, which was the case in 51 (49%) of 104 hips with detailed surgical records. Following an incision in the tense anterior capsule, the intra-articular structures were carefully inspected. The thickened ligamentum teres was excised and removed from the acetabular origin in 78% of hips (81 of 104). When the thickened labrum was inverted, it was separated and everted from the articular surface, occurring in 88% of hips (92 of 104). The thickened medial portion of the labrum was occasionally excised in an arc to form a labrum (32% of hips, 33 of 104). A substantial amount of intervening fibrous tissue (known as ‘pulvinar’)11 at the bottom of the acetabulum that prevented centralisation of the femur head was found in 15 of 104 hips (14%). Of these, four joints required gouging of the articular cartilage as the acetabular cavity was found to be shallow even after removal of the pulvinar. Following clean-up, the dislocated femoral head was gently placed into the acetabulum, and stability of the joint was confirmed. In retrospective evaluation of obstacles, thickened ligamentum teres and an inverted labrum were considered major factors interfering with conservative reduction, and both factors coexisted in 75 of 104 hips (72%).
For post-operative immobilisation, a flexion–abduction cast was applied for between two and four weeks post-operatively, followed by a flexion–abduction brace for a further four weeks and finally a Pavlik harness for the following four months.
Radiological evaluation
Final radiological images taken after full growth were evaluated according to the Severin classification (Table I).12 In addition, aseptic necrosis of the femoral head was evaluated according to the system of Kalamchi and MacEwen.13,14 The relationship between age at open reduction and radiological findings was also assessed.
Table I
Severin’s classification15 CE, centre–edge
| Degree | Radiological appearance | CE angle (°) | Age (years) |
|---|---|---|---|
| Ia | Very good | > 19 | 6 to 13 |
| > 25 | > 14 | ||
| Ib | Good | 15 to19 | 6 to 13 |
| 20 to 25 | > 14 | ||
| II | Mild deformity | Same values as degree Ia-Ib | |
| III | Moderate dysplasia without subluxation | < 15 | 6 to 13 |
| < 20 | > 14 | ||
| IVa | Moderate subluxation | ≥ 0 | |
| IVb | Severe subluxation | < 0 | |
| V | Bad articulation with false acetabulum | ||
| VI | Complete re-dislocation |
Results
Following open reduction alone by Ludloff’s approach, 74 hips (64%) required additional corrective surgery during the growth period because the hip joint tended to subluxate gradually. In particular, of the 23 hips that underwent open reduction after 12 months of age, 21 (91%) required corrective surgeries. In contrast, of nine hips treated before the age of four months, only two (22%) needed corrective surgery, which consisted of femoral derotation varus osteotomy (DVO) in 20 hips, a Salter operation16 in 36 hips (combined with DVO in 32) and a Pemberton operation17 in 18 hips (combined with DVO in ten). The mean age at corrective surgery was 2.6 years (one to six), 2.1 years (one to four) and 2.1 years (one to four) for DVO, Salter and Pemberton procedures, respectively. Additional surgery after full growth was required in three hips at a mean age of 23.3 years (19 to 28), comprising rotational acetabular osteotomy in two hips and a Chiari osteotomy18 in one.
Final radiological evaluation was performed at a mean post-operative follow-up of 20.3 years (15 to 28). The hips were classified according to Severin12 as group Ia in 23 (20.0%), group Ib in four (3.5%), group IIa in 22 (19.1%), group IIb in 20 (17.4%), group III in 39 (33.9%) and group IV in seven (6.1%). Severin groups I and II are considered to represent a good result, which was therefore found in 69 hips (60%). However, only 27 hips (23.5%) were classified as group I or II without additional corrective surgery (Fig. 1). There were no hips in Severin group I that were treated with surgical reduction after 18 months of age. Additionally, 21 (91%) of 23 hips in 20 (95%) of the 21 patients aged > 12 months, surgery required correction later (Fig. 2).

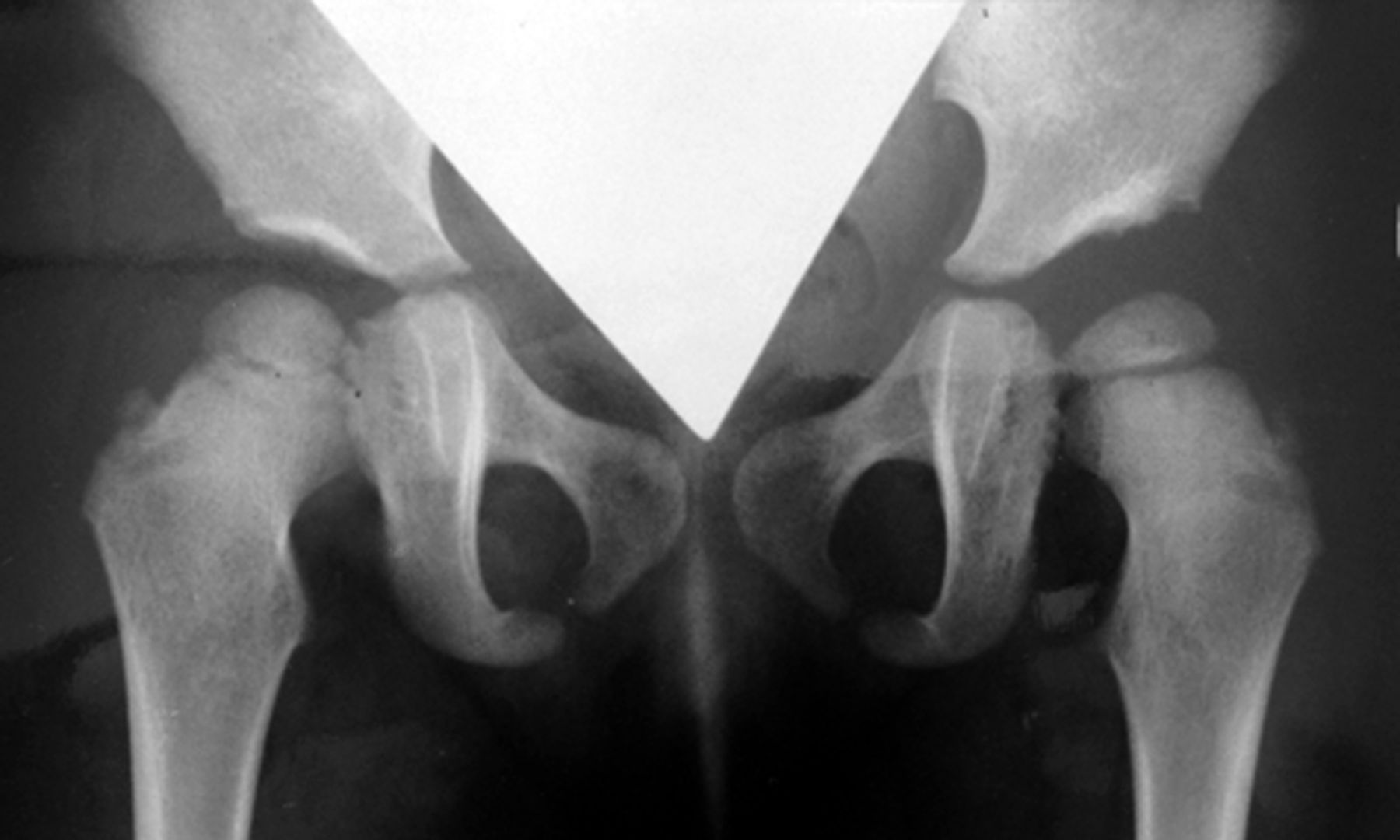

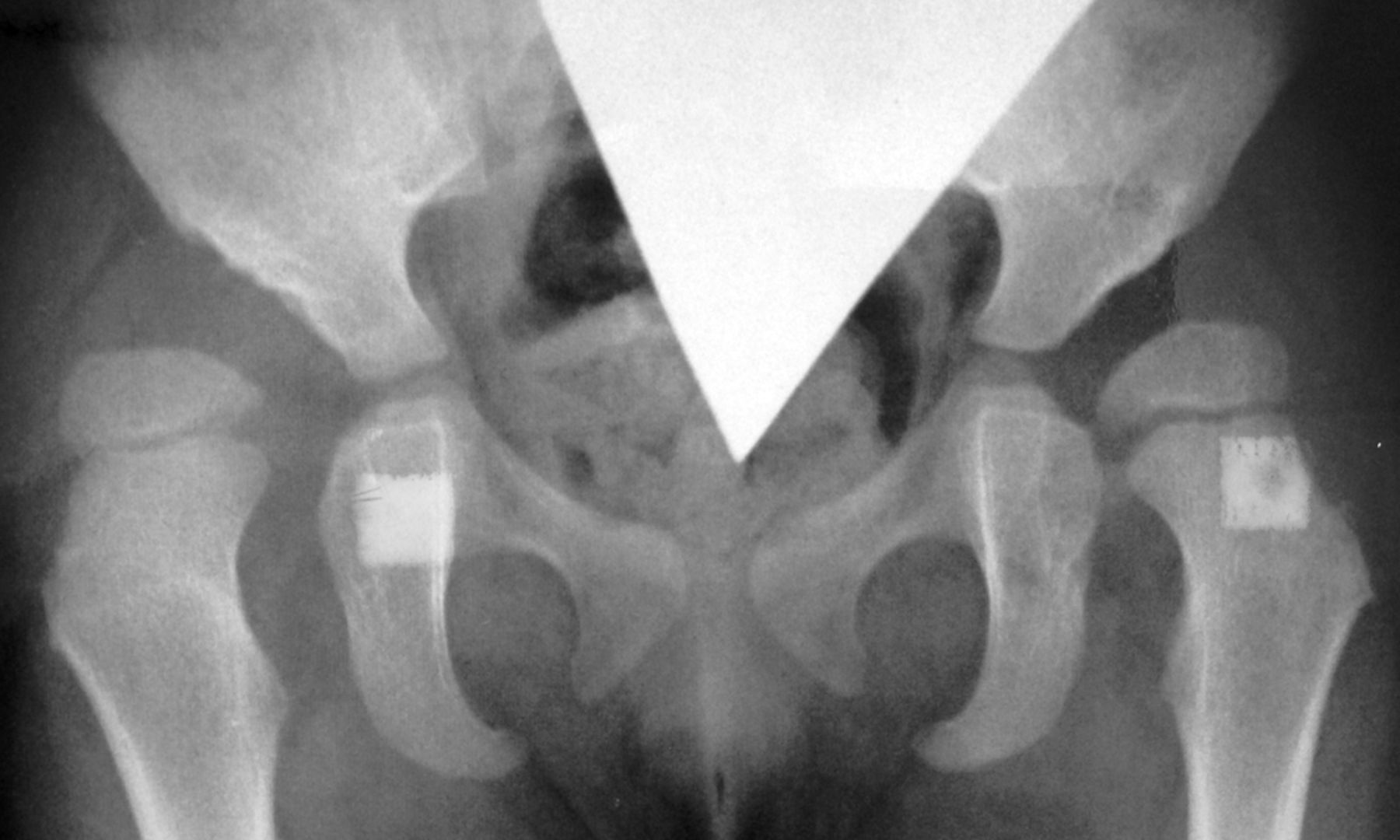
Figs. 1a - 1d
Anteroposterior radiographs showing a female patient aged nine months at Ludloff open reduction, a) pre-operatively, b) Severin group Ia of the left hip joint at two years post-operatively, c) at ten years of age, and d) Severin Ia with 26° of CE angle at 26 years of age. This patient did not show subluxation or any aseptic necrosis at any time points and therefore did not need any additional operations.
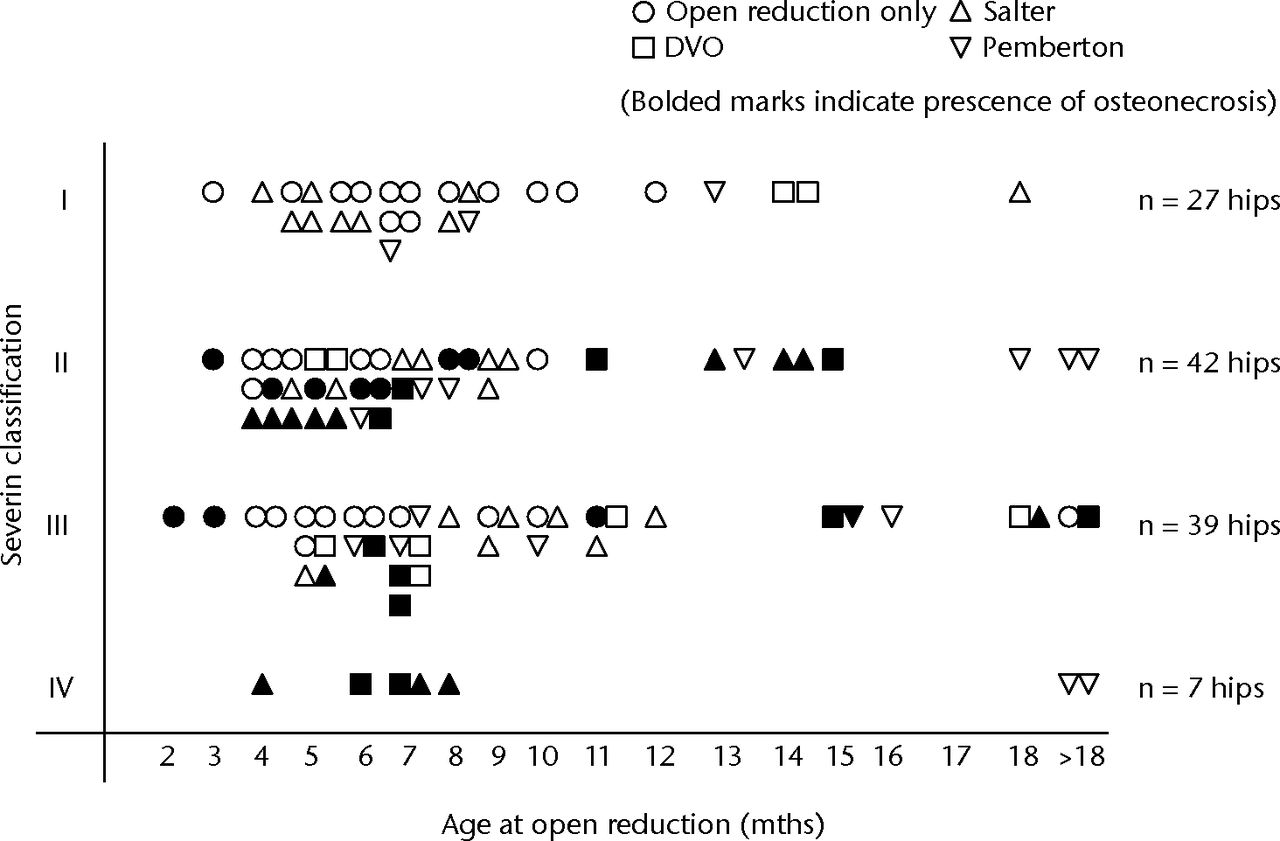
Fig. 2
Diagram showing each hip by age at open reduction, Severin classification and presence of aseptic necrosis of the femoral head.
A total of 35 hips (30.4%) showed signs of aseptic necrosis of the femoral head at final follow-up. These were classified according to Kalamchi and MacEwen13,14 as type I in three hips, type II in 18, type III in nine and type IV in five. Hips in patients who underwent surgical reduction aged ≤ three months had a higher incidence of aseptic necrosis (three of four hips, 75%) compared with those in patients aged > 18 months at surgery (two of 10 hips, 20%) (Fig. 2). Severe aseptic necrosis was often noted in patients with a long period of prior conservative treatments at previous hospitals or clinics.
Coxa magna, which the authors define as a treated femoral head with transverse diameter > 110% of the contralateral side on a plain radiograph, was encountered in 23 hips (20%) at final follow-up (when the transverse diameter was obviously enlarged compared with a normal hip at same age, the authors also considered the hip as Coxa magna in bilateral cases). Of these, five joints showed obvious osteo-arthritic changes both on the femoral head and the acetabulum (Fig. 3).



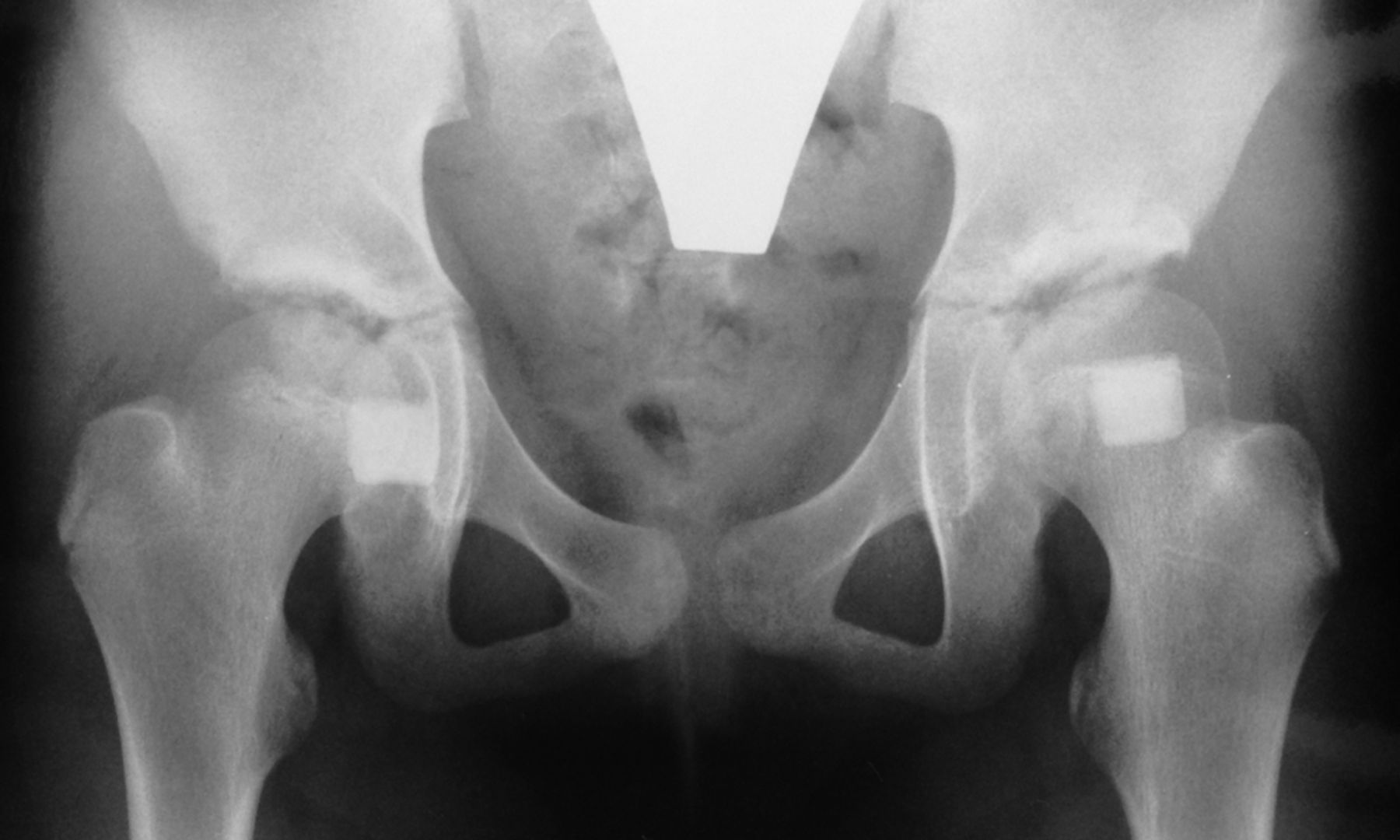
Figs. 3a - 3d
Anteroposterior radiographs of a female patient who underwent bilateral Ludloff open reduction aged 5 months; a) at 1.6 years post-operatively, showing advanced subluxation of the femoral head and residual acetabular dysplasia; b) two months after bilateral Salter and femoral derotation varus osteotomies;c) after recurrence of coxa valga without aseptic necrosis at nine years of age and d) Severin group IIa of both hips at 28 years of age.
Discussion
DDH has been widely accepted and has replaced CDH, because the term DDH reflects the findings that dislocations of the hip in infants are commonly first found at several months of age, not at birth. As many previous studies have reported, CDH/DDH depends on complex interactions between the pre-natal deficit and the post-natal environment. The authors speculate that most hip dislocations in infants originate from occult dysplasia caused by morphogenetic errors, infection, the intra-uterine environment or chromosomal or genetic abnormality. In fact, most infants who develop hip dislocation show several signs of joint laxity or subluxation at birth, or within one month of age. In order to detect occult dysplasia or joint instability at birth, great attention is necessary even if a sonographic examination shows normal morphology. As dysplasia of the hip is considered to be a multifactorial condition, pathological differentiation between CDH and DDH is very difficult. Therefore, the treatment strategy must be very similar among clinicians as the aims of treatment are to obtain normal joint congruity as soon as possible and to encourage ordinal development of the hip joint, regardless of the pathogenesis or the timing of joint dislocation.
A Pavlik harness should be attempted for early dysplasia or dislocation of the hip, as many clinical reports recommend. Our institution treated 927 infants (1129 hips) with the Pavlik harness alone between 1961 and 1988. As a result, 1016 hips (90%) achieved closed reduction. Aseptic necrosis is a well-known complication of the Pavlik harness due to repetitive contact between the femoral head and the posterior margin of the acetabulum.19 The current study shows a rate of aseptic necrosis as high as 30% before full growth in hips, treated with the Pavlik harness and followed by open reduction. The extent to which the harness was responsible for the necrosis is unknown in this study, as all patients underwent subsequent surgical intervention. It was speculated that persistent use of a Pavlik harness on dislocated or subluxated hip joints might increase the risk of aseptic necrosis rather than surgical invasion. Once a patient shows substantial swelling around the hip joint or cries excessively during harness use, the femoral head position should be confirmed by plain radiography and/or ultrasound scan. Once poor congruency of the hip joint is noticed, the harness should be removed immediately and surgical treatment considered without delay.
Regarding the surgical method for CDH or DDH, numerous studies described results of open reduction using Ludloff’s medial approach3-5,20-22; however, only a few reports have demonstrated long-term results to full growth of the hip joints.6,7 Since 1967, the authors’ institution has aggressively performed open reduction on infants. This study evaluated the long-term results for 115 fully grown hips and revealed that 60% were classified into group I or II of Severin’s classification, which were considered successful maturation of the hip joints. One of the significant advantages of Ludloff’s medial approach is that intra-articular interfering factors can be directly removed with a minimally invasive approach, particularly for an infant. Mau et al21 reported that the major interfering factor in reduction was not the labrum or ligamentum teres, but the tension on the anterior joint capsule, which could be easily dissected through Ludloff’s approach. In addition, this approach allows bilateral surgery in the same supine position, which is considered safer for infants under general anaesthesia. An inconspicuous surgical scar seems to be cosmetically favourable,22 particularly for female patients.
On the other hand, Koizumi et al7 suggests that Ludloff’s approach allows only limited exposure and thus cannot deal with extra-articular factors such as adhesion of the posterior aspect of the joint capsule to the ilium, torsion of the joint capsule, or contracture of short rotator muscles, which might prevent ideal centralisation of the head even after successful reduction. We consider that the main factor interfering with head reduction is intra-articular tissue23; therefore other factors, particularly those on the posterior aspects of the hip joint, may gradually diminish after open reduction and mobilisation after cast removal. However, the authors suggest that insufficient centralisation of the femoral head may induce subluxation in early childhood, which commonly requires additional corrective surgery for acquiring better congruency in the majority of these hip joints, as shown in this study; thus according to the authors, the purpose of second stage osteotomy is to acquire better congruency of the hip joint. As superior transition of the femoral head may progress even after achieving reduction in patients who have already started to ambulate, appropriate candidates for open reduction through the medial approach alone would be infants before the ambulating stage.24
The incidence of aseptic necrosis was 30% in our study, which was relatively low compared with the rates of 42%, 41% and 35.5% reported by Koizumi et al,7 Morcuende et al22 and Sosna and Rejholec,25 respectively. Mankey, Arntz and Staheli26 and Mau et al21 suggested that the incidence of aseptic necrosis was not caused by surgical treatment, but instead by improper conservative treatments prior to surgery. In this study, most cases were referred from other hospitals or clinics after unsuccessful conservative treatments for several months, and many already had substantial damage to the femoral head before surgical intervention. Also, long-term immobilisation in an uncentralised position may cause an ossification disorder at the outer edge of the acetabulum, which may induce acetabulum dysplasia later, thereby influencing the final outcome.15 It has been suggested that a hip spica cast in the flexion–abduction position may increase the risk of aseptic necrosis.27,28 We used a spica cast in this position for between two and four weeks post-operatively. Because continuous high pressure on the femoral head is the main cause of aseptic necrosis, sufficient removal of fibrous tissue (pulvinar) in the acetabulum is crucial at surgery. In addition, three of four patients who underwent surgical reduction aged ≤ three months developed necrosis and coxa magna in this study. Gentle surgical maneouvres are also important to prevent additional damage to the femoral head, particularly for extremely immature hip joints. Such radiological changes usually appear after ten years of age,5 so careful follow-up is crucial to evaluate the development of the treated hip joint to full growth.
Conclusions
More than half of the patients who underwent open reduction with Ludloff’s medical approach required additional corrective surgery; in particular patients aged > 12 months at reduction. Early diagnosis and gentle surgical reduction at an appropriate age (before the ambulating stage) is important to obtain good joint congruity and encourage ideal maturity of the joint. This long-term follow-up study provides useful information regarding the treatment strategy for CDH (DDH).
1 Yamamuro T . CDH or DDH?J Orthop surg (Hong Kong)2005;13:111–112. Google Scholar
2 Storer SK , SkaggsDL. Developmental dysplasia of the hip. Am Fam Physician2006;74:1310–1316.CrossrefPubMed Google Scholar
3 Fabry G . Open reduction by the Ludloff approach to congenital dislocation of the hip under the age of two. Acta Orthop Belg1990;56:233–235.PubMed Google Scholar
4 O’Hara JN , BernardAA, DwyerNS. Early results of medial approach open reduction in congenital dislocation of the hip: use before walking age. J Pediatr Orthop1988;8:288–294.CrossrefPubMed Google Scholar
5 Scapinelli R , OrtolaniM. Open reduction (Ludloff approach) of congenital dislocation of the hip before the age of two years. Isr J Med Sci1980;16:276–280.PubMed Google Scholar
6 Matsushita T , MiyakeY, AkazawaH, EguchiS, TakahashiY. Open reduction for congenital dislocation of the hip: comparison of the long-term results of the wide exposure method and Ludloff’s method. J Orthop Sci1999;4:333–341. Google Scholar
7 Koizumi W , MoriyaH, TuchiyaK, et al.Ludloff’s medial approach for open reduction of congenital dislocation of the hip: a 20-year follow-up. J Bone Joint Surg [Br]1996;78-B:924–929. Google Scholar
8 Ludloff K . The open reduction of the congenital hip dislocation by an anterior incision. J Bone Joint Surg [Am]1913;2-A:438–454. Google Scholar
9 Lalonde FD , FrickSL, WengerDR. Surgical correction of residual hip dysplasia in two pediatric age-groups. J Bone Joint Surg [Am]2002;84-A:1148–1156.CrossrefPubMed Google Scholar
10 Yamada K. Indication of open reduction for congenital dislocation of the hip. Seikeigeka 1979;30:320–4 (in Japanese). Google Scholar
11 Walker JM . Morphological variants in the human fetal hip joint: their significance in congenital hip disease. J Bone Joint Surg[Am]1980;62-A:1073–1082. Google Scholar
12 Severin E . Contribution to the knowledge of congenital dislocation of the hip joints: late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand Suppl1941;84:1–142. Google Scholar
13 Kalamchi A , MacEwenGD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg [Am]1980;62-A:876–888.PubMed Google Scholar
14 Kalamchi A , SchmidtTL, MacEwenGD. Congenital dislocation of the hip: open reduction by the medial approach. Clin Orthop Relat Res1982;169:127–132. Google Scholar
15 Shapiro F. Pediatric orthopedic deformities: basic science, diagnosis, and treatment. San Diego: Academic Press, 2001:153-262. Google Scholar
16 Salter RB . The classic: innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip by Robert B. Salter, J. Bone Joint Surg. (Brit) 43B:3:518, 1961. Clin Orthop Relat Res1978;137:2–14. Google Scholar
17 Pemberton PA . Pericapsular osteotomy of the ilium for the treatment of congenitally dislocated hips. Clin Orthop Relat Res1974;98:41–54.CrossrefPubMed Google Scholar
18 Chiari K . Medial displacement osteotomy of the pelvisClin Orthop. Relat Res1974;98:55–71. Google Scholar
19 Suzuki S , KashiwagiN, KasaharaY, SetoY, FutamiT. Avascular necrosis and the Pavlik harness. The incidence of avascular necrosis in three types of congenital dislocation of the hip as classified by ultrasound. J Bone Joint Surg [Br]1996;78-B:631–635.PubMed Google Scholar
20 Castillo R , ShermanFC. Medial adductor open reduction for congenital dislocation of the hip. J Pediatr Orthop1990;10:335–340.CrossrefPubMed Google Scholar
21 Mau H , DörrWM, HenkelL, LutscheJ. Open reduction of congenital dislocation of the hip by Ludloff’s method. J Bone Joint Surg [Am]1971;53-A:1281–1288. Google Scholar
22 Morcuende JA , MeyerMD, DoranLA, WeinsteinSL. Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. J Bone Joint Surg [Am]1997;79-A:810–1723.PubMed Google Scholar
23 Weinstein G , PonsetiIV. Congenital dislocation of the hip. J Bone Joint Surg [Am]1979;61-A:119–124.PubMed Google Scholar
24 Gabuzda GM , RenshawTS. Reduction of congenital dislocation of the hip. J Bone Joint Surg [Am]1992;74-A:624–631. Google Scholar
25 Sosna A , RejholecM. Ludloff’s open reduction of the hip: long-term results. J Pediat Orthop1992;12:603–606. Google Scholar
26 Mankey MG , ArntzCT, StaheliLT. Open reduction through a medial approach for congenital dislocation of the hip: a critical review of the Ludloff approach in sixty-six hips. J Bone Joint Surg [Am]1993;75-A:1334–1345. Google Scholar
27 Campbell P , TarlowSD. Lateral tethering of the proximal femoral physis complicating the treatment of congenital hip dysplasia. J Pediatr Orthop1990;10:6–8.PubMed Google Scholar
28 Schoenecker PL , BitzDM, WhitesideLA. The acute effect of position of immobilization on capital femoral epiphyseal blood flow: a quantitative study using the hydrogen washout technique. J Bone Joint Surg [Am]1978;60-A:899–904. Google Scholar
Funding statement:
None declared
Author contributions:
K. Yamada: Performed surgeries, Data collection
H. Mihara: Data collection, Writing the paper
H. Fujii: Data analysis
M. Hachiya: Assisted surgeries, Data collection
ICMJE Conflict of Interest:
None declared
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










