Abstract
Aims
We performed a systematic review of the literature to determine whether earlier surgical repair of acute rotator cuff tear (ARCT) leads to superior post-operative clinical outcomes.
Methods
The MEDLINE, Embase, CINAHL, Web of Science, Cochrane Libraries, controlled-trials.com and clinicaltrials.gov databases were searched using the terms: ‘rotator cuff’, or ‘supraspinatus’, or ‘infraspinatus’, or ‘teres minor’, or ‘subscapularis’ AND ‘surgery’ or ‘repair’. This gave a total of 15 833 articles. After deletion of duplicates and the review of abstracts and full texts by two independent assessors, 15 studies reporting time to surgery for ARCT repair were included. Studies were grouped based on time to surgery < 3 months (group A, seven studies), or > 3 months (group B, eight studies). Weighted means were calculated and compared using Student’s t-test.
Results
Group B had a significantly higher pre-operative Constant score (CS) (p < 0.001), range of movement in external rotation (p = 0.003) and abduction (p < 0.001) compared with group A. Both groups showed clinical improvement with surgical repair; group A had a significantly improved Constant score, University of California, Los Angeles (UCLA) shoulder score, abduction and elevation post-operatively (all p < 0.001). Group B had significantly improved Constant score (p < 0.001) and external rotation (p < 0.001) post-operatively. The mean Constant score improved by 33.5 for group A and by 27.5 for group B.
Conclusion
These findings should be interpreted with caution due to limitations and bias inherent to case-series. We suggest a trend that earlier time to surgery may be linked to better Constant score, and active range of movement in abduction and elevation. Additional prospective studies are required.
Article focus
To perform a systematic review of the literature to determine whether earlier surgical repair of acute rotator cuff tear (ARCT) leads to superior post-operative clinical outcomes
Key messages
This systematic review demonstrates that clinical outcomes vary depending on delayed time to surgery for ARCT repair
We observe a trend that earlier time to surgery may be linked to better Constant score, and active range of movement in abduction and elevation
Strengths and limitations
This is the first systematic review on time to surgery for acute rotator cuff tear
Findings should be interpreted with caution due to limitations and bias inherent to case-series included in this review
Introduction
Acute rotator cuff tears (ARCTs) occur in previously asymptomatic patients, who identify a traumatic incident leading to a sudden onset of symptoms such as severe pain, immediate loss of strength and functional impairment of the shoulder.1 ARCTs account for 8% of patients who present with symptomatic rotator cuffs,2 and correct and early clinical diagnosis is often difficult.3,4
Few studies have reported on the timing of surgery and functional outcomes for ARCT repair. Swedish national guidelines state that acute full-thickness traumatic tears should be repaired within three weeks.5 However, there is conflicting evidence in support of this statement. In 1968, Heikel6 observed the trend that patients with repairs performed within 15 to 60 days post-injury had better clinical outcomes than patients who received their operation longer than six months after injury. In 1983, Basset and Cofield2 demonstrated that operations performed within three weeks of injury had consistently better clinical outcomes. However, more recent reports have suggested that a surgical delay of three to four months post-injury does not affect clinical outcome.1,7
To date, there is no systematic review summarising the findings on the timing of operation for ARCTs. The objective of this study is to systematically review the literature in order to determine whether a delay in either open or arthroscopic repair of ARCTs influences the clinical outcome post-operatively. The key question is whether a shorter time to surgical repair of ARCTs leads to improved clinical outcomes. We hypothesised that earlier surgical intervention will correlate with improved post-operative shoulder function measures including Constant score,8 University of California, Los Angeles (UCLA) shoulder score9 and range of movement.
Materials and Methods
Design
Systematic review and meta-analysis was performed using a priori protocol.
Literature search
The electronic databases MEDLINE, Embase, CINAHL, Cochrane Library, Web of Science, controlled-trials.com and clinicaltrials.gov were independently searched by two reviewers (SB and IM). The terms ‘rotator cuff’, or ‘supraspinatus’, or ‘infraspinatus’, or ‘teres minor’, or ‘subscapularis’ AND ‘surgery’, or ‘repair’ were used as keywords. In databases with a hierarchal structure, search terms were mapped to subject headings and exploded to include specific subheadings. In order to capture all relevant articles, limits were not applied. The literature search involved studies from 1980 to Jan 2012. A health research methodology trained librarian was consulted to ensure the validity of the search. The inclusion and exclusion criteria for study selection are shown in Table I.
Table I
Inclusion and exclusion criteria
| Criteria | |
|---|---|
| inclusion criteria | Randomised controlled trials, cohort studies, case series |
| Prospective and retrospective studies | |
| Male or female patients of any age receiving surgical repair for acute rotator cuff tear (RCT) | |
| Open, mini-open, or arthroscopic repair | |
| Reporting data on time to surgery from onset of symptoms | |
| Tears repaired ≤ 7 months | |
| All tear sizes | |
| Supraspinatus, infraspinatus, subscapularis, or teres minor tendon tears | |
| One or more torn tendons | |
| Exclusion criteria | Literature reviews, case studies, commentaries, grey literature |
| Non-English language | |
| Cadavers or animal studies | |
| Non-operative treatments | |
| Chronic RCTs, or studies with heterogeneous patient populations (both acute and chronic tears) |
Article selection
The process of article selection involved multiple stages by two independent reviewers (SB and IM). Titles and abstracts were first scanned for relevance, after which the full text of selected articles was accessed and reviewed for eligibility criteria. Disagreements in article selection at each stage were resolved by discussion. A third assessor (IW) was consulted for consensus when necessary. The references of the included studies and recent review articles were scanned for possible missed articles.
Data extraction
The included studies were assessed by two reviewers (SB and IM) to extract the study design, sample size, participant age, type of surgery, tear size, number of tendons torn, time to surgery, length of follow-up, post-operative complications, outcome and range of movement measures. Disagreements were resolved with consensus. Articles with missing data regarding time to surgery were eliminated. When raw data was presented in the articles, the values for the aforementioned variables were directly calculated from the raw data.
Quality assessment of the included studies
The Methodological Index for NOn-Randomized Studies (MINORS) scale was used to appraise the quality of the included studies,10 and was assessed independently by two reviewers (SB and IM). The MINORS scale includes a 12-item checklist assessing study variables such as study aim, data collection and endpoint measurements, with each item scored between 0 and 2 points. Eight items assess the quality of non-comparative studies and an additional four items assess the quality of comparative studies, giving maximum scores of 16 and 24, respectively.
Outcomes measures
The Constant score is a commonly used measure for assessing outcomes in treatment of shoulder disease, and includes a pain score, functional assessment, range of movement, and strength measures.8 The UCLA shoulder scoring scale includes measures of pain, function, range of movement and patient satisfaction.9 Range of movement is measured with a goniometer, and reported in degrees from the neutral position.
Statistical analysis
The data was verified by each of the two assessors and a quality assessment was performed on the included studies. Level of agreement between the independent assessors was calculated using Kappa statistics for each study selection process. Kappa statistics with 95% confidence intervals were reported. Mean and standard deviation (sd) of quality assessment scores were reported and level of agreement between the reviewers are calculated using intraclass correlation coefficient (ICC).
For subsequent analysis, studies were grouped based on wait time to surgery of a mean of < 3 months (group A), or > 3 months (group B). Mean and sd of quality assessment scores were reported for each group. Results from the 15 studies were analysed by calculating the weighted mean and weighted sd for patient age, wait time to surgery, follow-up, and pre- and post-operative external rotation, abduction, elevation, Constant score and UCLA score for both groups. Weighted means were compared using Student’s t-test and p-value of < 0.05 was considered for statistical significance.
Scatter plots for wait time to surgery and improvement in Constant score (the difference between pre- and post-operative scores) was plotted for studies with sufficient Constant score data. Minitab v16.0 (Minitab, State College, Pennsylvania) was used for statistical analysis.
Results
Literature search
The literature search identified 5183 articles from EMBASE, 3372 articles from MEDLINE, 1708 articles from CINAHL, 3232 articles from Web of Science, 15 articles from Cochrane Libraries, 115 papers studies from controlled-trials.com and 93 studies from clinicaltrials.gov.
The search strategy schematic is outlined in Figure 1. By combining the results from all databases, the search strategy yielded a total of 15 833 articles. After deleting duplicate studies, 8653 papers remained. Elimination by title reduced the article pool to 1172 studies and abstract review narrowed it further to 161 articles. Full-text review yielded a total of 15 articles that reported time to surgery data associated with acute rotator cuff repair (Fig. 1).1,2,6,7,11-21 The eliminated articles comprised duplicates, case reports, letters to editors, commentaries and studies with no quantitative wait time to surgery data (Table I, Fig. 1).
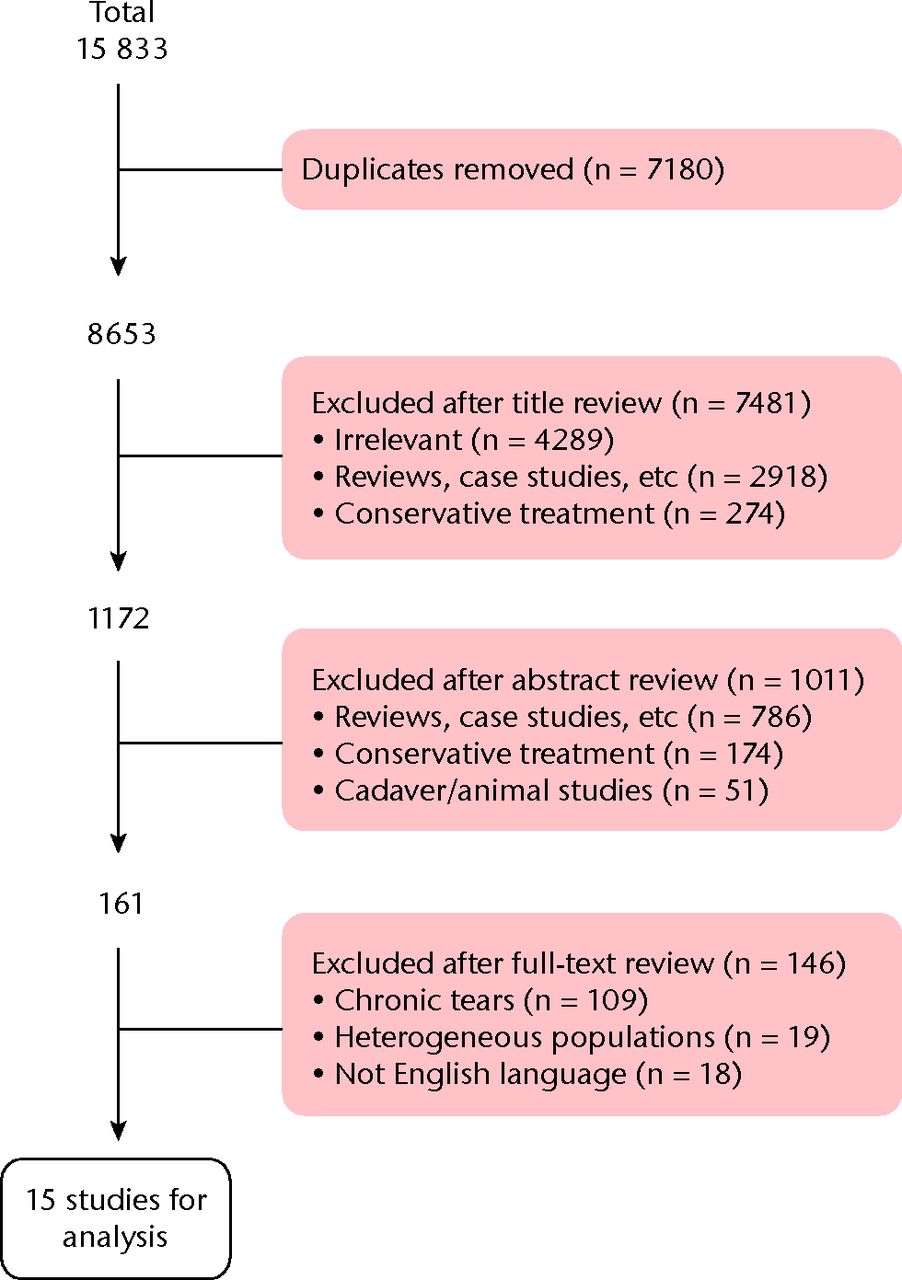
Fig. 1
Flowchart showing the literature search strategy.
Level of agreement
Reviewer agreement data is shown in Table II. Following three rounds of article elimination, both reviewers had selected 15 studies that contributed to the data set. The Kappa statistic for the level of agreement was 0.996 (95% confidence interval (CI) 0.994 to 0.998) after deleting articles by title, and 0.982 (95% CI 0.966 to 0.998) after deleting articles by abstract. As there was perfect agreement on the final step there was no need to calculate the Kappa statistic.
Table II
Agreement data for two independent reviewers
| Papers (n) | ||||
|---|---|---|---|---|
| Review | Reviewer 1 | Reviewer 2 | Consensus | |
| After elimination by title | 1174 | 1179 | 1172 | |
| After elimination by abstract | 158 | 161 | 161 | |
| After elimination by full text | 15 | 15 | 15 | |
Quality of included studies
Only four of the 15 studies were prospective, with the remainder retrospective case series. There were no randomised controlled trials. The level of agreement between the reviewers for quality assessment was 0.980 (95% CI 0.963 to 0.996). The mean MINORS score for all included studies was 10.93 (sd 1.83; 8 to 15). For the non-comparative studies, the mean MINORS score was 10.45 (sd 1.63; 8 to 12). For the comparative studies, the mean MINORS score was 12.25 (sd 1.89; 11 to 15).
Demographics and results of the included studies
Seven studies reported a mean time to surgery of < 3 months, with mean times ranging from 0.4 months to 2.8 months. The other eight studies reported a mean time to surgery > 3 months, ranging from 3.7 to 7.2 months. The full details of the studies are provided in the Supplementary Material.
Two studies suggested that surgery within three weeks resulted in better post-operative outcomes.2,11 Basset and Cofield2 reported that repair within three weeks of injury lead to significantly greater active abduction compared with patients treated later than three weeks. However, strength in abduction or external rotation was not significantly different between the two groups. Hantes et al11 demonstrated significantly better Constant scores, UCLA scores and shoulder flexion and abduction in repairs within three weeks of injury (mean 0.4 months), compared with those undertaken later than three weeks (mean 4.4 months). Heikel6 suggested that repairs performed within 60 days produced better results compared with those undertaken after six months, based on subjective complaints, pain, extent and power in active abduction, flexion and rotation.
In contrast, four studies concluded that repair within four to six months does not produce significantly inferior clinical outcomes compared with those attempted earlier.1,7,12,14 Björnsson et al1 suggested no significant difference in Constant-Murley score,8 Disabilities of the Arm Shoulder and Hand (DASH) score,22 or Western Ontario Rotator Cuff (WORC) index23 if repair is performed within three months. Similarly, Kreuz et al12 showed that a three- to four-month delay in surgery still produces an ‘acceptable’ improvement in Constant score (defined as an improvement ≥ 40 points). Peterson and Murphy7 suggested no statistical difference in UCLA score, American Shoulder and Elbow Surgeons (ASES) score24 or active elevation if repair is performed within 16 weeks compared with repairs performed within eight weeks or those between eight and 16 weeks. However, they did note significantly poorer outcomes associated with times to surgery > four months.7 Namdari et al14 found no significant correlation between duration of symptoms outcome measures, including the DASH score, visual analogue scale (VAS) for pain, Simple Shoulder Test (SST) score,25 active forward elevation, active external rotation, passive internal rotation, mean strength, and Short-Form 36.26 However, Warner and Parsons13 reported a significantly lower Constant score when surgery is delayed > six months.
Both Kreuz et al12 and Warner and Parsons13 described an inverse relationship between Constant score and time to repair within six months. Overall, there is no consensus amongst these studies as to when repair of ARCT should be performed for optimal post-operative outcomes.
Analysis of time to surgery and clinical outcomes
Seven studies comprising 209 patients contributed data to group A, while eight studies comprising 162 patients contributed data to group B. There was no significant difference in patient age between the two groups, with each group having a mean age of 56 years (p = 1.00). No significant difference in follow-up time was identified between the two groups (p = 0.280). The mean time to surgery was 1.8 months (sd 1.3) in group A and 4.9 months (sd 3.1) in group B. There is no significant difference in study quality as assessed by mean MINORS score between the two groups (p = 0.327) (Table III).
Table III
Pre- and post-operative outcome analysis by time to surgery (< 3 months (Group A) versus > 3 months (Group B))
| Outcome* | Group A (< 3 months) | Group B (> 3 months) | p-value |
|---|---|---|---|
| Studies (n) | 7 | 8 | |
| Mean (sd) MINORS score | 11.4 (0.5) | 10.5 (2.4) | 0.328 |
| Total patients (n) | 209 | 162 | |
| Mean (sd) age (yrs) | 56.0 (9.0) | 56.0 (6.0) | 1.00 |
| Mean (sd) time to surgery (mths) | 1.8 (1.3) | 4.9 (3.1) | |
| Mean (sd) follow-up (mths) | 49.0 (20.3) | 38.3 (15.3) | 0.280 |
| Mean (sd) Constant score | |||
| Pre-operative | 39.5 (3.8) (one study) | 53.5 (6.2) | < 0.001 |
| Post-operative | 73.0 (16.0) | 81.0 (10.4) | < 0.001 |
| Difference | 33.5 | 27.5 | |
| p-value | < 0.001 | < 0.001 | |
| Mean (sd) UCLA | |||
| Pre-operative | 11.0 (1.7) | - | |
| Post-operative | 31.1 (3.3) | - | |
| p-value | < 0.001 | - | |
| Mean (sd) external rotation (°) | |||
| Pre-operative | 61.0 (8.2) | 68.0 (19.0) | 0.003 |
| Post-operative | 59.7 (6.3) | 77.3 (14.3) | < 0.001 |
| Difference | -1.3 | 9.3 | |
| p-value | 0.253 | < 0.001 | |
| Mean (sd) abduction (°) | |||
| Pre-operative | 41.8 (5.8) | 88.5 (61.0) | < 0.001 |
| Post-operative | 150.5 (15.6) | 102.7 (54.7) | < 0.001 |
| Difference | 108.5 | 14.2 | |
| p-value | < 0.001 | 0.140 | |
| Mean (sd) elevation (°) | |||
| Pre-operative | 76.0 (34.0) | 115.8 | |
| Post-operative | 134.6 (29.1) | 125.7 | |
| Difference | 58.6 | 10 | |
| p-value | < 0.001 | - | |
-
* MINORS, Methodological Index for NOn-Randomized Studies; UCLA, University of California, Los Angeles shoulder score
Constant score
Group B had a significantly better pre-operative Constant score (p < 0.001). Although these groups were different at baseline, their relative improvement and final scores were compared. Group A showed a significant improvement in Constant score from a pre-operative score of 39.5 (sd 3.8) to 73.0 (sd 16.0) post-operatively (p < 0.001). Group B also showed a significant improvement from 53.5 (sd 6.2) pre-operatively to 81.0 (sd 10.4) post-operatively (p < 0.001) (Table III).
UCLA shoulder score
There was insufficient data for reporting UCLA scores in group B. However, there was a significant improvement in the mean UCLA score in group A from 11.0 (sd 1.7) pre-operatively to 31.1 (sd 3.3) post-operatively (p < 0.001) (Table III).
Range of movement
ROM measures for external rotation, abduction and elevation were analysed. Group B had a significantly greater mean pre-operative external rotation (p = 0.003) and abduction (p < 0.001) when compared with group A. The external rotation in group B improved significantly from pre-operative values (p < 0.001), whereas the mean external rotation in group A actually worsened by a mean of 1.3° (Table III). This suggests that external rotation may not be greatly improved by earlier ARCT repair.
On the other hand, there was significant mean improvement in post-operative abduction for group A (108.5°; p < 0.001) but not in group B (14.2°; p = 0.140) (Table III). However, this trend may be driven by the lower pre-operative ROM values in group A, probably as a result of the early inflammatory stages of the injury that limit mobility. Interestingly, group A had a higher mean post-operative abduction (150.5° (sd 15.6) vs 102.7 (sd 54.7)).
Group A showed significant improvement in elevation after surgical repair (p < 0.001). Group A demonstrated a mean improvement in elevation of 58.6° post-operatively, while group B only improved by 10° (Table III). Group A had a higher mean post-operative elevation (134.6° vs 125.7°).
Relationship between time to surgery and Constant score
By plotting time to surgery and the difference in pre- and post-operative Constant score, we can show a trend suggesting that earlier time to surgery is related to greater improvement in Constant score (Fig. 2). This graph is based on results from four studies that measured the Constant score in a similar way,4,9,12,14 and should therefore be interpreted with caution. There was insufficient data for other clinical outcome measurements to be analysed by scatter plot.
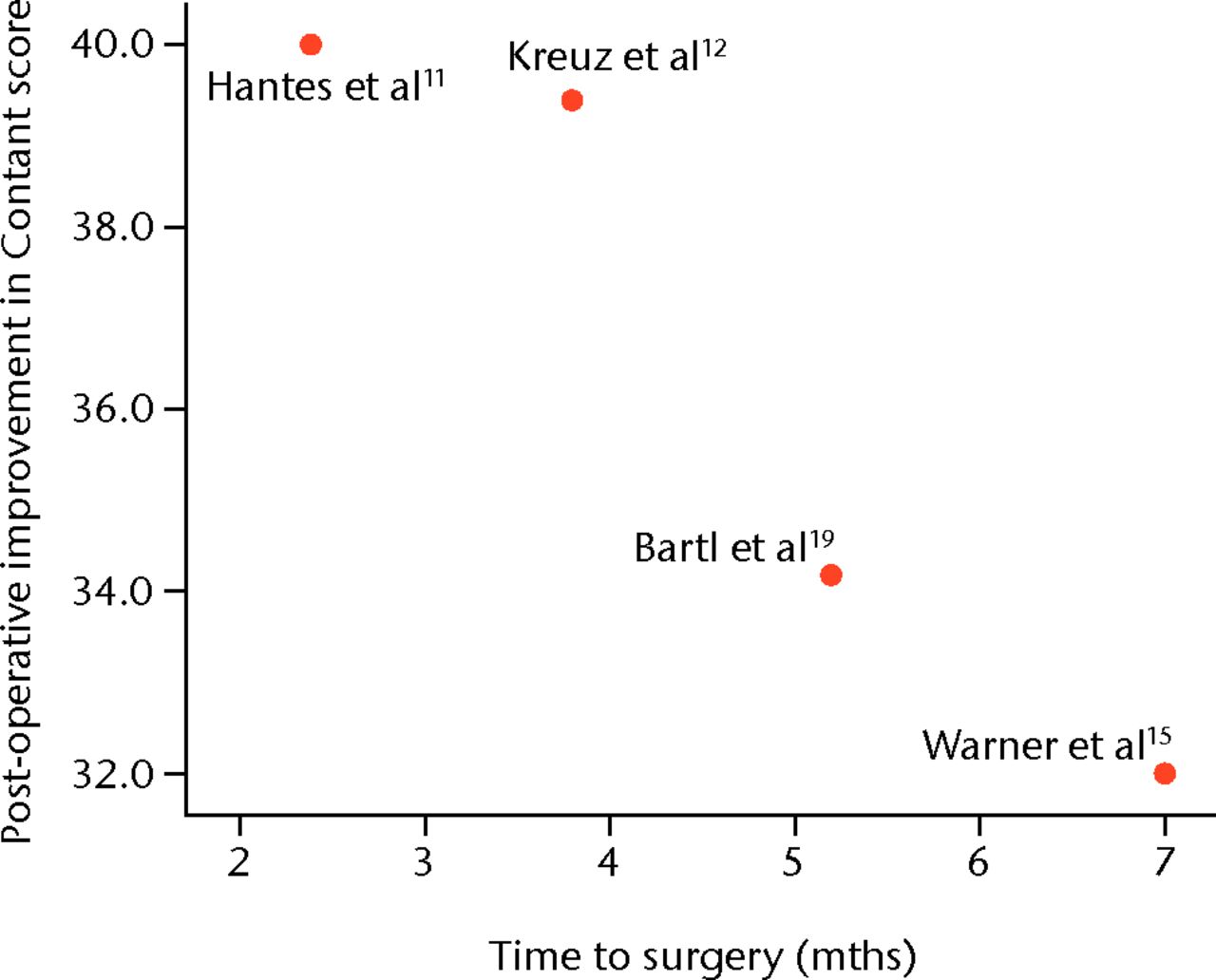
Fig. 2
Scatter plot showing a trend between mean post-operative improvement in Constant score and mean time to surgery as reported in four studies.11,12,15,19
Discussion
The timing of operation for patients with acute rotator cuff tear is controversial. This systematic review compiles time to surgery data for ARCT repair, across 15 retrospective and prospective studies. The aim was to evaluate whether early repair of ARCTs results in superior post-operative shoulder function in terms of Constant score, UCLA shoulder score and range of movement of the shoulder. In order to minimise bias, two reviewers performed the search strategy, study selection and data collection process independently. Another strength of this review is that we have used the most optimal method of analysis to account for the heterogeneity inherent to case-series.
We have found that repairs undertaken after a mean post-injury time of < three months (group A) and those undertaken later than three months after injury (group B) both demonstrated clinical improvement with surgical repair. Group A had significantly improved Constant and UCLA scores, abduction, and elevation post-repair (all p < 0.001), while group B had significantly improved Constant score and external rotation post-operatively (both p < 0.001) (Table III). The early-repair group demonstrated a mean improvement of 108.5° in abduction and 58.6° in elevation, whereas group B improved only by means of 14.2° in abduction and 10° in elevation (Table III). However, it should be noted that these differences were largely driven by low ROM in group A patients, as a result of the more restrictive early stage of an ARCT. Finally, we observed a trend that while earlier time to surgery leads to greater improvements in Constant score, the post-operative scores were higher in the group with the later repairs (group B) (81.0 vs 73.0) (Fig. 2).
Warner et al13 suggested that fatty degeneration and muscle atrophy seen with delayed surgery is related to lower post-operative Constant scores. However, our data indicate that a delay to surgery leads to higher post-operative Constant scores. It has also been shown that repair under tension due to tendon retraction, as well as tissue friability and inelasticity, may contribute to lower Constant scores and inferior cuff healing.1,15,27 It may not be necessary to perform surgical repair before the onset of tendon changes to preserve muscle function,16 and even decrease re-tear rates.11,27
Reasons for delay to surgery include delayed help seeking, delayed referral or consultation, surgical wait times, initial conservative treatment, and missed diagnosis. Deutsch et al4 reported that the correct diagnosis of ARCT can be delayed by between four and 24 months. Proper history and physical examination, and identification of typical traumatic injury patterns can help improve early and correct diagnosis.3,28
Interestingly, the threshold of progression from an acute tear to a subacute tear to chronic cuff degeneration is not well-defined.17 Basset and Cofield2 suggested that an acute tear approaches a chronic state by three months, while Warner and Parsons13 described fatty degeneration as significantly greater after six months. It is also possible that acute tears do not exist without some previous tendon degeneration,1 and occur along areas of early degenerative change. This makes the concept of purely ‘acute’ tears more ambiguous.2 Furthermore, the clinical distinction between acute tear, acute tear on chronic tear, or acute symptoms of a chronic tear, is a challenge even with imaging modalities such as radiographs, dynamic sonography, MRI, and arthroscopy.3,17 This could explain why the majority of studies on rotator cuff repair report on a mixed population of patients with both acute and chronic tears, with few studies reporting specifically on ARCT populations.
An important limitation of our study is that it does not account for the role of conservative treatments for ARCTs. Furthermore, we are summarising data from studies with heterogeneous patient populations with variable configurations and number of tendons torn, size and mechanism of tear, prior symptoms from previous chronic or acute shoulder/arm injuries, prior surgery or failed repair, degree of tendon retraction and baseline degeneration, severity of pain and disability, and patient activity level. There was also heterogeneity in the number of patients, surgical approaches, differences in surgical skill, post-operative management, follow-up time, and post-operative complications. Additionally, not all studies on surgical repair indicate whether patients received rotator cuff repair alone or in conjunction with additional procedures. Differences in the number of surgeons and evaluators of post-operative outcomes is likely to have contributed to inter-study variation. Some studies also did not use standardised scales for assessment of pain or patient satisfaction, making compilation and analysis of the data more difficult.
Another limitation of our study is reporting bias. The underreporting of time to surgery in the literature contributed to the lack of data and was a likely source of error. Some studies, particularly with those of > three months wait time, did not report standard deviation for mean outcome scores. This limited the possibility of more powerful correlation analysis and comparison of means. Another limitation is the inclusion of articles in the English language only.
It is difficult to assess in our current analysis whether there is an identifiable therapeutic window or optimal time within which surgical repair leads to ‘acceptable’ or ‘superior’ clinical outcomes. However, there is no clear consensus as to what is an acceptable level of post-operative shoulder function for patients after surgical repair of ARCT based on age and time of follow-up. Advocating for a specific time for surgical repair is meaningless until this has been established, and investigators can clearly describe their patients in terms of the duration of symptoms, age, the surgical technique used, the consecutiveness of their series, and evaluation of shoulder function by independent assessors at a specified follow-up time. Patient satisfaction, longevity of outcomes, cost and recovery time should be further studied so that the risk–benefit profile of early ARCT repair can be fully understood.
Conclusions
This systematic review demonstrates that clinical outcomes vary depending on delayed time to surgery for ARCT repair. There is a trend suggesting that earlier time to surgery may be linked to better Constant scores and range of movement. The findings of this study should be interpreted with caution as a result of the limitations inherent to the case series included in this review. Additional well-designed comparative studies are needed to further evaluate the relationship between time to surgery and shoulder function outcomes.
Despite these limitations, this is the first systematic review on time to surgery for acute rotator cuff tear.
1 Björnsson HC , NorlinR, JohanssonK, AdolfssonLE. The influence of age, delay of repair, and tendon involvement in acute rotator cuff tears: structural and clinical outcomes after repair of 42 shoulders. Acta Orthop2011;82:187–192. Google Scholar
2 Bassett RW , CofieldRH. Acute tears of the rotator cuff: the timing of surgical repair. Clin Orthop Relat Res1983;175:18–24. Google Scholar
3 Sørensen AK , BakK, KrarupAL, et al.Acute rotator cuff tear: do we miss the early diagnosis?: a prospective study showing a high incidence of rotator cuff tears after shoulder trauma. J Shoulder Elbow Surg2007;16:174–180. Google Scholar
4 Deutsch A , AltchekDW, VeltriDM, PotterHG, WarrenRF. Traumatic tears of the subscapularis tendon: clinical diagnosis, magnetic resonance imaging findings, and operative treatment. Am J Sports Med1997;25:13–22. Google Scholar
5 Swedish National Musculoskeletal Competence Centre. National indications for shoulder surgery, 2006. Google Scholar
6 Heikel HV . Rupture of the rotator cuff of the shoulder: experiences of surgical treatment. Acta Orthop Scand1968;39:477–492. Google Scholar
7 Petersen SA , MurphyTP. The timing of rotator cuff repair for the restoration of function. J Shoulder Elbow Surg2011;1:62–68.CrossrefPubMed Google Scholar
8 Constant CR , MurleyAH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res1987;214:160–164.PubMed Google Scholar
9 Amstutz HC , Sew HoyAL, ClarkeIC. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res1981;155:7–20.PubMed Google Scholar
10 Slim K , NiniE, ForestierD, et al.Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg2003;73:712–716.CrossrefPubMed Google Scholar
11 Hantes ME , KaridakisGK, VlychouM, et al.A comparison of early versus delayed repair of traumatic rotator cuff tears. Knee Surg Sports Traumatol Arthrosc2011;19:1766–1770.CrossrefPubMed Google Scholar
12 Kreuz PC , RemigerA, ErggeletC, et al.Isolated and combined tears of the subscapularis tendon. Am J Sports Med2005;33:1831–1837.CrossrefPubMed Google Scholar
13 Warner JJ , ParsonsIM. Latissimus dorsi tendon transfer: a comparative analysis of primary and salvage reconstruction of massive, irreparable rotator cuff tears. J Shoulder Elbow Surg2011;10:514–521.CrossrefPubMed Google Scholar
14 Namdari S , HennRF, GreenA. Traumatic anterosuperior rotator cuff tears: the outcome of open surgical repair. J Bone Joint Surg [Am]2008;90-A:1906–1913.CrossrefPubMed Google Scholar
15 Warner JJ , HigginsL, ParsonsIM, DowdyP. Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elbow Surg2001;10:37–46.CrossrefPubMed Google Scholar
16 Ide J , TokiyoshiA, HiroseJ, MizutaH. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg [Am]2007;89-A:2378–2388.CrossrefPubMed Google Scholar
17 Lähteenmäki HE , VirolainenP, HiltunenA, HeikkiläJ, NelimarkkaOI. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elbow Surg2006;15:148–153.CrossrefPubMed Google Scholar
18 Van Riet RP , O’LearyST, HooperA, BellSN. Rotator cuff strength following open subscapularis tendon repair. Acta Orthop Belg2008;74:173–179.PubMed Google Scholar
19 Bartl C , SenftlM, EichhornS, et al.Combined tears of the subscapularis and supraspinatus tendon: clinical outcome, rotator cuff strength and structural integrity following open repair. Arch Orthop Trauma Surg2012;132:41–50.CrossrefPubMed Google Scholar
20 Mansat P , FrankleMA, CofieldRH. Tears in the subscapularis tendon: descriptive analysis and results of surgical repair. Joint Bone Spine2003;70:342–347.CrossrefPubMed Google Scholar
21 Frank JB , ElAttracheNS, DinesJS, et al.Repair site integrity after arthroscopic transosseous-equivalent suturebridge rotator cuff repair. Am J Sports Med2008;36:1496–1503. Google Scholar
22 Gummesson C , AtroshiI, EkdahlC. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord2003;4:11.CrossrefPubMed Google Scholar
23 Kirkley A , AlvarezC, GriffinS. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med2003;13:84–92.CrossrefPubMed Google Scholar
24 Michener LA , McClurePW, SennettBJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg2002;11:587–594.CrossrefPubMed Google Scholar
25 Lippit SB, Harryman DT, Matsen FA III. A practical tool for evaluating function: the simple shoulder test. In: Matsen FA 3rd, Fu FH, Hawkins RJ, eds. The shoulder: a balance of mobility and stability. Rosemont: American Academy of Orthopaedic Surgeons, 1993:501–518. Google Scholar
26 Ware JE Jr, Snow KK, Kosinski M, Gandek B. SF-36 health survey: manual and interpretation guide. Boston: The Health Institute, New England Medical Center, 1993. Google Scholar
27 Gerber C , FuchsB, HodlerJ. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg [Am]2000;82-A:505–515.CrossrefPubMed Google Scholar
28 Kreuz PC , RemigerA, LahmA, HergetG, GächterA. Comparison of total and partial traumatic tears of the subscapularis tendon. J Bone Joint Surg [Br]2005;87-B:348–351.CrossrefPubMed Google Scholar
Funding statement:
None declared
Author contributions:
I. Mukovozov: Design, Data collection, Data analysis, Writing the paper
S. Byun: Design, Data collection, Data analysis, Writing the paper
F. Farrokhyar: Design, Data analysis, Writing the paper
I. Wong: Design, Data analysis, Writing the paper
ICMJE Conflict of Interest:
None declared
©2013 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
Supplementary material. A table providing in-depth details on each of the 15 studies included in this review is available alongside this article on our website www.bjr.boneandjoint.org.uk










