Abstract
Objectives
To report the five-year results of a randomised controlled trial examining the effectiveness of arthroscopic acromioplasty in the treatment of stage II shoulder impingement syndrome.
Methods
A total of 140 patients were randomly divided into two groups: 1) supervised exercise programme (n = 70, exercise group); and 2) arthroscopic acromioplasty followed by a similar exercise programme (n = 70, combined treatment group).
Results
The main outcome measure was self-reported pain as measured on a visual analogue scale. At the five-year assessment a total of 109 patients were examined (52 in the exercise group and 57 in the combined treatment group). There was a significant decrease in mean self-reported pain on the VAS between baseline and the five-year follow-up in both the exercise group (from 6.5 (1 to 10) to 2.2 (0 to 8); p < 0.001) and the combined treatment group (from 6.4 (2 to 10) to 1.9 (0 to 8); p < 0.001). The same trend was seen in the secondary outcome measures (disability, working ability, pain at night, Shoulder Disability Questionnaire and reported painful days). An intention-to-treat analysis showed statistically significant improvements in both groups at five years compared with baseline. Further, improvement continued between the two- and five-year timepoints. No statistically significant differences were found in the patient-centred primary and secondary parameters between the two treatment groups.
Conclusions
Differences in the patient-centred primary and secondary parameters between the two treatment groups were not statistically significant, suggesting that acromioplasty is not cost-effective. Structured exercise treatment seems to be the treatment of choice for shoulder impingement syndrome.
Article focus
The effectiveness of acromioplasty in shoulder impingement syndrome
Key messages
Structured exercise treatment is the treatment of choice for shoulder impingement syndrome
Strengths and limitations of this study
A randomised controlled trial
Results may in part reflect the natural course of shoulder impingement syndrome
Introduction
Shoulder pain is a common complaint, sometimes described as the second most common musculoskeletal disorder after low back pain.1-4 Impingement is often cited as the leading cause of pain in the shoulder,5 which was initially thought to arise from the mechanical friction of the tendon under the acromion.6 However, further studies and treatment trials have not been able to demonstrate a pure mechanical aetiology for this syndrome,7,8 and therefore current treatment options remain controversial.9-16
Impingement of the shoulder has a severe and long-lasting effect on the patient, with costs of treatment and absence from work causing economic consequences.
The syndrome is traditionally divided into three stages: Stage I, oedema and haemorrhage; Stage II, fibrosis and tendinitis; and Stage III, tears of the rotator cuff, biceps ruptures and bone changes.17 The condition usually begins gradually and then over time becomes continuous.18 Its diagnosis is based on clinical examination, which makes its nature somewhat imprecise. The first mode of treatment is non-operative, involving rest, subacromial corticosteroid injections,19 oral non-steroidal anti-inflammatory drugs20 and physiotherapy.9,20-23 Although surgical treatment has not been conclusively shown to be superior to conservative treatment,13-16,24 arthroscopic acromioplasty is still a popular procedure with a rising incidence over the last decade.25,26
Clear indications for different modes of treatment based on randomised clinical trials have not yet been defined. It seems that the expectations of both the surgeons and the patients and the availability of the arthroscopic technology affect the demand.
We designed a randomised clinical trial to investigate the eventual additional effect of arthroscopic decompression with acromioplasty on a supervised exercise program.24 We now report the five-year results.
Patients and Methods
The study design was a prospective, controlled and randomised trial. Patients were recruited from the area of Kanta-Häme Health Care District (population 165 000) between June 2001 and July 2004. The full exclusion and inclusion criteria are provided in Table I. The eligibility of the patients was examined at baseline by a physician (a specialist in rehabilitation or orthopaedics). Impingement was tested with Neer’s method17 by assessing whether lidocain injected into the subacromial space relieved the pain. All patients had a plain radiograph and MRI of the symptomatic shoulder.27 The risks and benefits of both treatments were discussed and the patients were also given written information. Included patients were asked to sign a written consent in which they voluntarily agreed to comply with the randomised treatment protocol and follow-up visits, with the right to withdraw at any time without giving reason for it.
Table I
Inclusion and exclusion criteria (NSAIDs, non-steroidal anti-inflammatory drugs)
| Criteria |
|---|
| Inclusion criteria |
| Clinical symptoms of shoulder impingement syndrome |
| A positive Neer’s test |
| Symptom duration of at least three months |
| Attempts to treat with: rest, NSAIDs, subacromial corticosteroid injections and regular physiotherapy |
| Age between 18 and 60 years |
| No previous operations on shoulder region |
| Willingness and capacity to comply with the treatment protocol and follow-up visits |
| Exclusion criteria |
| Osteoarthritis |
| Signs of glenohumeral instability |
| A penetrating rupture of the rotator cuff |
| Cervical radicular syndrome |
| Adhesive capsulitis |
| Neuropathy of the shoulder region |
A total of 140 patients (52 men and 88 women) with a mean age of 47.1 years (23 to 60) were recruited to the study, which was approved by the Ethics Committee of the Hospital District. Patients were randomly assigned to the treatment groups using computer-generated numbers sealed in envelopes prepared by an independent statistician not otherwise involved with the study.
Demographic data and disability-values and a structured Shoulder Disability Questionnaire (SDQ)28,29were collected at baseline. The SDQ contains common situations referring to the preceding 24 hours (yes/no/not applicable (i.e. not occurred)). The score is calculated by dividing the number of positive scores to the total number of applicable items subsequently multiplied by 100 (0 no disability, 100 all applicable items positive). All patients had received various types of physiotherapy including massage, heat, transcutaneous nerve stimulation and exercises, but had not been treated by a specialised physician before entering the study.
The control visit assessment, including SDQ-score and the clinical measurements, were performed by an independent, blinded investigator (physiotherapist), not otherwise involved in the study or rehabilitation, at three and six months and at one, two and five years. The health-related quality of life was measured at the five-year visit using the 15D quality of life tool.30
Supervised exercise
Physiotherapeutic training was based on home exercises, for which the patients received individual guidance and general information during an average of seven visits to an independent physiotherapist.
The aim of the supervised exercise treatment was to restore painless, normal mobility of the shoulder complex and to increase the dynamic stability of the glenohumeral joint and the scapula.31 Series of long painless movement with repetition were undertaken with the aim of strengthening the tendons. Patients were instructed to do nine different exercises at least four times a week, with three courses of 30 to 40 repetitions. As the self-assessed ability and strength improved, resistance was increased and repetitions diminished. The progress was evaluated at control visits (mean of seven) and continued until the patient and the therapist considered that the trainee was independently able to maintain the practise level.
Combined treatment: surgery
One independent experienced orthopaedic surgeon performed all the arthroscopic decompressions under regional anaesthesia at Kanta-Häme Central Hospital, Hämeenlinna, Finland. Debridement and decompression were performed with a shaver and/or a vaporisator. Acromioplasty was undertaken with a burr drill (Arthroscope Karl Storz GmbH, Tuttlingen, Germany). A standard posterior portal was used to analyse the structures of the glenohumeral joint and to reach the subacromial space. An anterolateral portal was used to perform debridement and decompression. The range of movement was tested under arthroscopic visualisation to check for any local impingement.
The use of a collar cuff sling was recommended for one week, after which mobilisation was allowed with free active movements, starting with pendular motion. In the rehabilitation period patients in the combined treatment group received similar training instructions from a physiotherapist as were provided for the exercise group with the same kind of follow-up schedule. The training programme was individually planned and progressive. It started progressing once the post-operative pain had started to diminish. Like in the supervised exercise treatment group, the progress was evaluated at the visits to the physiotherapist (mean of six visits).
Follow-up
At five years one trained independent physiotherapist, who had not been involved with the patients before evaluation and who was blinded to the mode of treatment, performed all standardised assessments. Patients were instructed not to indicate their treatment group and they wore a T-shirt to cover eventual operation scars.
Outcome measures
Self-reported shoulder pain, as the primary outcome measure, was assessed on a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (extreme pain). Secondary outcome measures included disability (measured on a VAS from 0 (no disability) to 10 (total disability)), working ability (VAS from 0 (totally unable to work) to 10 (no restriction on work)), pain at night (VAS from 0 (no pain) to 10 (extreme pain)), SDQ score, number of painful days during the previous three months and the proportion of pain-free patients (defined as a VAS for pain ≤ 3). The health related quality of life was measured at the five-year visit using the 15-D tool and compared with the age-adjusted population values.30
Statistical analysis
Power calculations were performed based on the use of self-reported pain (VAS) as the primary outcome measure. Using 1.5 (sd 2.5) as a clinically important change,32 the sample size was estimated to 45 patients per group, if 5% type I (α) and 20% type II (β) errors were allowed. As the standard deviation of the outcome measure was only a rough estimate, a total of 70 patients were included in both groups.
Statistical analyses were performed using IBM SPSS Statistics for Windows v19.0 (IBM Corp., Armonk, New York). Descriptive statistics are presented as percentages, frequencies, and means. The independent samples t-test was used for group comparisons, paired samples t-test for comparisons within groups over time and the chi-squared test for equal proportions of pain-free patients between groups. A p-value < 0.05 was considered to represent statistical significance.
Results
The study groups did not differ at baseline in any pre-operative measure (Table II). During the follow-up between two and five years, a total of four patients in the exercise group had undergone acromioplasty and one patient had undergone operation of a rotator cuff rupture. The mean time after randomisation until these five operations were performed was 2.9 years (2.6 to 3.3). Additionally, a total of 12 patients originally allocated to the combined treatment group refused operation; one of whom went on to undergo surgery at a follow-up of 2.6 years. The total number of operated patients in the exercise group was 18. All these patients were invited to and attended the five-year control visit. The follow-up results were analysed using an intention-to-treat approach, but the outcome is also described based on the actual treatment using a per protocol approach.
Table II
Results in the intention-to treat analysis (CI, confidence interval)
| Mean outcome (range)* | Exercise | Combined treatment | Mean difference (99% CI) | p-value† |
|---|---|---|---|---|
| Number of patients | ||||
| At baseline (n = 140) | 70 | 70 | ||
| At two years (n = 134) | 66 | 68 | ||
| At five years (n = 109) | 52 | 57 | ||
| Self-reported pain VAS | ||||
| Baseline | 6.5 (1 to 10) | 6.4 (2 to 10) | -0.1 (-1.01 to 0.77) | 0.73 |
| Two years | 2.9 (0 to 9) | 2.5 (0 to 10) | -0.4 (-1.60 to 0.78) | 0.37 |
| Five years | 2.2 (0 to 8) | 1.9 (0 to 8) | -0.3 (-1.54 to 0.84) | 0.44 |
| Mean change from baseline | ||||
| At two years | -3.7 | -3.9 | -0.2 (-1.61 to 1.14) | 0.65 |
| At five years | -4.1 | -4.7 | -0.6 (-2.13 to 1.01) | 0.35 |
| p-value (baseline vs five-year) | < 0.001‡ | < 0.001‡ | ||
| Disability VAS | ||||
| Baseline | 6.5 (2 to 10) | 6.2 (1 to 10) | -0.3 (-1.13 to 0.75) | 0.23 |
| Two years | 2.6 (0 to 9) | 2.0 (0 to 10) | -0.6 (-1.81 to 0.62) | 0.21 |
| Five years | 1.8 (0 to 9) | 1.5 (0 to 8) | -0.3 (-1.45 to 0.93) | 0.57 |
| Mean change from baseline | ||||
| At two years | -3.8 | -4.2 | -0.4 (-1.76 to 1.00) | 0.47 |
| At five years | -4.4 | -4.8 | -0.4 (-2.07 to 1.16) | 0.46 |
| Working ability VAS | ||||
| Baseline | 5.9 (0 to 9) | 5.7 (0 to 9) | -0.2 (-1.42 to 0.85) | 0.78 |
| Two years | 8.0 (1 to 10) | 8.0 (0 to 10) | 0.0 (-0.82 to 0.85) | 0.96 |
| Five years | 7.5 (2 to 10) | 7.8 (1 to 10) | +0.3 (-0.66 to 1.27) | 0.41 |
| Mean change from baseline | ||||
| At two years | +2.0 | +2.3 | +0.3 (-0.93 to 1.52) | 0.47 |
| At five years | +1.6 | +2.2 | +0.6 (-0.81 to 2.18) | 0.23 |
| Night pain VAS | ||||
| Baseline | 6.4 (0 to 10) | 6.2 (0 to 10) | -0.2 (-1.46 to 0.93) | 0.60 |
| Two years | 2.6 (0 to 9) | 2.0 (0 to 8) | -0.6 (-1.95 to 0.65) | 0.19 |
| Five years | 1.7 (0 to 8) | 1.7 (0 to 9) | 0.0 (-1.19 to 1.25) | 0.95 |
| Mean change from baseline | ||||
| At two years | -3.8 | -4.2 | -0.4 (-2.00 to 1.17) | 0.51 |
| At five years | -4.8 | -4.8 | 0.0 (-1.75 to 1.73) | 0.99 |
| SDQ score | ||||
| Baseline | 82.5 (0 to 100) | 78.1 (0 to 100) | -4.4 (-14.4 to 4.47) | 0.21 |
| Two years | 32.8 (0 to 100) | 24.2 (0 to 100) | -8.6 (-23.34 to 6.10) | 0.13 |
| Five years | 22.2 (0 to 100) | 16.9 (0 to 100) | -5.3 (-19.54 to 8.90) | 0.33 |
| Mean change from baseline | ||||
| At two years | -50.0 | -53.2 | -3.2 (-19.11 to 12.75) | 0.6 |
| At five years | -61.7 | -60.4 | +1.3 (-15.74 to 18.34) | 0.84 |
| Reported painful days in preceding three months (n) | ||||
| Baseline | 73.8 (5 to 90) | 70.1 (0 to 90) | -3.7 (-16.28 to 8.86) | 0.44 |
| Two years | 19.7 (0 to 90) | 13.9 (0 to 90) | -5.8 (-18.16 to 6.52) | 0.22 |
| Five years | 11.8 (0 to 90) | 12.2 (0 to 90) | +0.4 (-12.52 to 13.32) | 0.94 |
| Mean change from baseline | ||||
| At two years | -53.3 | -55.0 | -1.7 (-19.68 to 16.22) | 0.80 |
| At five years | -59.4 | -60.8 | -1.4 (-20.57 to 17.83) | 0.85 |
| Patients pain-free (%) | ||||
| Baseline | 4% (3 of 70) | 11% (8 of 70) | +7% (-0.197 to 0.055) | 0.21§ |
| Two years | 64% (42 of 66) | 65% (44 of 68) | +1% (-0.224 to 0.203) | 0.89§ |
| Five years | 77% (40 of 52) | 75% (43 of 57) | -2% (-0.219 to 0.195) | 0.86§ |
-
* VAS, visual analogue scale: pain/night pain (0 = no pain, 10 = extreme pain), disability (0 = no disability, 10 = total disability), working ability (0 = totally unable to work, 10 = no restriction on work); SDQ, Shoulder Disability Questionnaire (from 0 to 100, with 0 denoting no functional impairment) † independent samples t-test, unless otherwise stated ‡ paired samples t-test, unless otherwise stated § chi-squared test
The five-year follow-up was attended by 109 (77.9%) of the original 140 patients recruited; 52 patients (74.3%) in the exercise group and 57 (81.4%) in the combined group. A statistically significant decrease in the mean self-reported pain was observed from baseline to the five-year follow-up in both groups: from 6.5 (1 to 10) to 2.2 (0 to 8) in the exercise group and from 6.4 (2 to 10) to 1.9 (0 to 8) in the combined treatment group (both p < 0.001, t-test). There was no difference in self-reported pain between the groups at the five-year follow-up (p = 0.44, independent-samples t-test).
At five years, there was no statistically significant difference between the two groups in terms of self-reported disability (p = 0.57), working ability (p = 0.41), night pain (p = 0.95) or SDQ (p = 0.33, independent-samples t-tests) (Table II). The proportion of pain-free patients at two years was similar in the two groups, with 64% (42 of 66) of the exercise group and 65% (44 of 68) of the combined treatment group pain-free (p = 0.89, chi-squared test). These proportions increased to 77% (40 of 52) of the exercise group and 73% (43 of 57) of the combined treatment group at five years (p = 0.86, chi-squared test) (Table II). Of the 109 patients who attended the five-year follow-up, 39 (36%) reported that they had had similar symptoms or complaints in the contralateral shoulder: 18 (35%) in the exercise group (35%) and 21 (37%) in the combined treatment group.
The 15D quality of life index was analysed in an intention-to-treat setting. Figure 1 displays the mean scores for each parameter for the two groups and also the age-adjusted general population.30 The groups had similar 15D values for total score (p = 0.82) and also by each domain (mobility, p = 0.13; vision, p = 0.91; hearing, p = 0.95; breathing, p = 0.67; sleeping, p = 0.81; eating, p = 0.30; speech, p = 0.95; elimination, p = 0.01; usual activities, p = 0.49; mental function, p = 0.45; discomfort and symptoms, p = 0.81; depression, p = 0.99; distress, p = 0.57; vitality, p = 0.45; and sexual activity, p = 0.61; all independent samples Mann–Whitney U test). In comparison with the age-adjusted general population the exercise treatment group had lower values in the ‘usual activities’ and ‘discomfort’ dimensions (p = 0.040 and p = 0.037, respectively), and the combined treatment group had lower values in the ‘mobility’, ‘sleeping’ and ‘discomfort’ parameters (p < 0.001, p = 0.049 and p = 0.028, respectively; all independent samples Mann–Whitney U test). All these differences exceeded the minimally clinically important difference (MCID) of between 0.02 and 0.0333(Fig. 1).
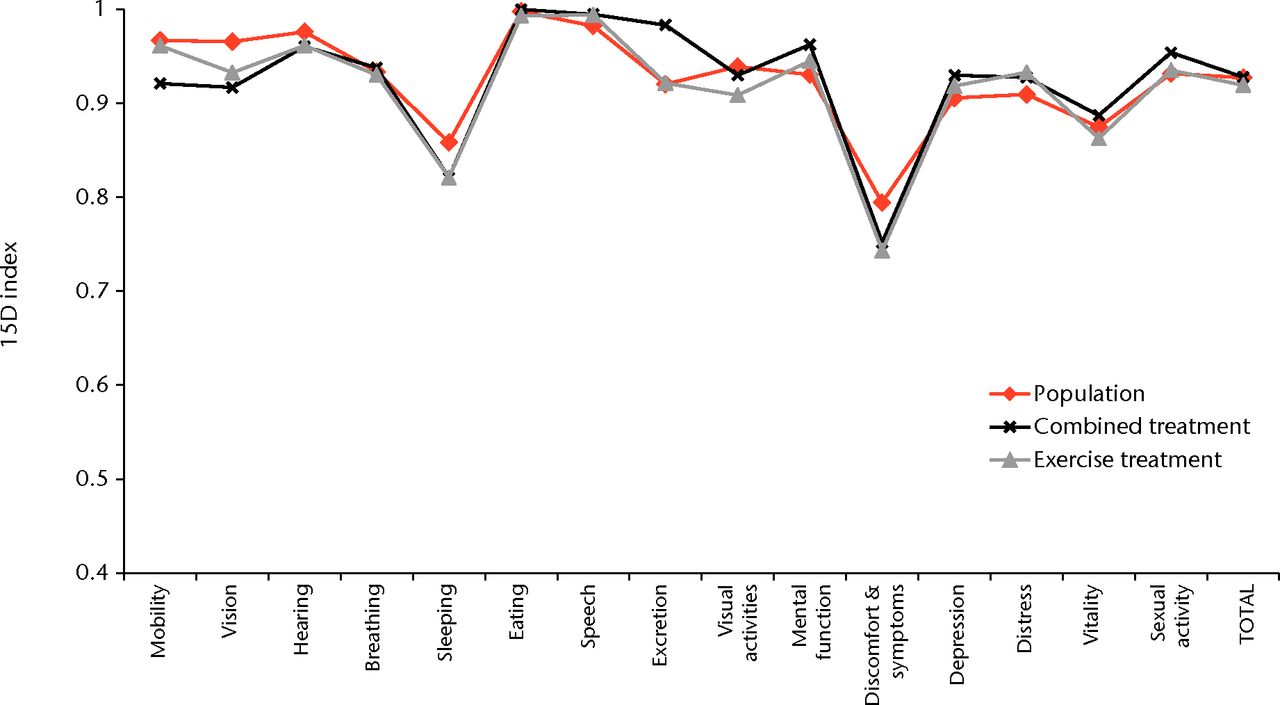
Fig. 1
Graph showing the 15D Quality of Life index in the combined and exercise treatment groups and in comparison with age-adjusted standard population at five years.
Of the whole group, 16 patients were retired at five years (one already at enrolment). In the combined treatment group five were retired, one due to old age and four on a disability/unemployment pension unrelated to shoulder symptoms. In the exercise group 11 patients were retired, three due to old age and eight were on a disability/unemployment pension, two of which were due to shoulder-related reasons. Two additional patients were part-time retired, one due to shoulder-related reasons (exercise group).
Seven patients in each group reported that changes had been made in their working arrangements due to shoulder-related reasons.
Discussion
The current study suggests that treatment with arthroscopic decompression combined with structured exercise treatment did not provide better results at five years compared with structured exercise alone, when assessed by self-reported pain. The same pattern was seen in the secondary outcome measures of disability, pain at night, SDQ score, number of painful days and the proportion of pain-free patients.
The improvements seen in both groups at the two-year follow-up continued to the five-year follow-up, resulting in highly significant improvements compared with the baseline values. However, there were no statistically significant differences between the groups. These five-year results indicate that arthroscopic decompression does not have any additional effect on conservative structured exercise. Furthermore, based on the current results, arthroscopic decompression does not have any prophylactic effect from a five-year perspective because the non-decompressed conservatively treated patients did as well as those who underwent operative release of the impingement.
Some parameters of the 15D quality of life index were slightly worse in patients treated for shoulder impingement than in the age-adjusted general population, but there were no differences between the treatment groups in these health-related quality of life parameters.
There have been randomised controlled trials comparing conservative and operative treatment of shoulder impingement syndrome13,14 and others have investigated the effect of the treatment on disability and working capacity.15,16 In these earlier studies, failure to respond to regular physiotherapy and other conservative treatment was used as an inclusion criterion. In contrast, the present study aimed to examine whether operative treatment provided any additional value to a conservative structured exercise treatment. At all follow-up visits the patients were evaluated by a blinded, independent assessor, thus minimising any bias. Selection and drop-out biases were minor as all eligible consecutive 140 patients volunteered to the study and the drop-out rate even at five years was relatively small (six of 140 at two years and 31 of 140 at five years).
As the study was conducted in an ordinary provincial hospital setting, not in a highly specialised shoulder centre, the external validity is relatively good. All operations were performed by one experienced orthopaedic surgeon and without any significant surgical complications. Although it concerns patients’ health and their decision, in reality patients do not always follow the given guidance. The similarity of the groups at baseline confirms a successful randomisation. Therefore, the adherence to the treatment was probably rather similar in both study groups.
The diagnosis of the impingement syndrome requires a thorough patient history and a careful clinical examination to exclude other conditions that may mimic impingement. All patients were examined also with MRI at baseline, in order to exclude conditions such as penetrating ruptures of the rotator cuff.
The age limits for inclusion were set at 18 and 60 years in conformity with previous studies.13-16 In patients aged < 18 years, glenohumeral instability is the leading cause of shoulder problems.34 However, our study included only four patients aged < 30 years. The frequency of rotator cuff tears is higher in patients aged > 60 years,35-37 hence their exclusion from our study.
Luyckx et al38 described 166 patients who underwent arthroscopic subacromial decompression, and reported a mean time between operation and full activity of 11.1 weeks (with a minimum of one week). In the present study, patients in the combined treatment group reported a mean of 28.1 days leave of absence due to shoulder-related reasons at the month follow-up visit and additional 4.6 days between the three- and six-month follow-up visits due to surgical procedure (Table III). The use of sick leave was minimal between the two- and five-year follow-up visits. Values were slightly higher in the exercise group, probably due to shifts in the group and operations performed between the two- and five-year visits. The difference in the total number of sick leave days was not statistically significant between the study groups (p = 0.11), but still almost double in the combined treatment group, which raises the overall health care costs.
Table III
Leave of absence from work due to shoulder-related symptoms during the three months preceding the control visit, except at five years when the year preceding the visit was used
| Mean absence from work (days) (range) | |||
|---|---|---|---|
| Control point | Exercise | Combined treatment | p-value* |
| 3 months | 5.3 (0 to 60) | 28.1 (0 to 90) | < 0.001 |
| 6 months | 2.4 (0 to 65) | 4.6 (0 to 90) | 0.45 |
| 12 months | 4.2 (0 to 58) | 4.4 (0 to 90) | 0.94 |
| 2 years | 3.8 (0 to 65) | 0.1 (0 to 4) | 0.03 |
| 5 years | 3.2 (0 to 110) | 0.4 (0 to 10) | 0.22 |
| Total | 16.5 | 31.2 | 0.11 |
-
* t-test
Use of descriptive data in an ad hoc per protocol analysis (43 patients in the exercise group and 43 patients in the combined treatment group) produced only slightly better results (Table IV) than the intention-to-treat analysis (Table II). There were no statistically significant differences between the groups in the per protocol analysis.
Table IV
Results in the per protocol analysis at five years (SDQ, Shoulder Disability Questionnaire)
| Mean outcome | Full exercise treatment group (n = 43) | Full combined treatment group (n = 43) |
|---|---|---|
| Self-reported pain | ||
| 2 years | 2.5 | 2.4 |
| 5 years | 1.8 | 1.6 |
| Disability | ||
| 2 years | 2.1 | 2.0 |
| 5 years | 1.3 | 1.2 |
| Working ability | ||
| 2 years | 8.5 | 8.0 |
| 5 years | 8.0 | 7.8 |
| Night pain | ||
| 2 years | 2.1 | 2.1 |
| 5 years | 1.2 | 1.3 |
| SDQ score | ||
| 2 years | 26.9 | 22.1 |
| 5 years | 16.7 | 12.0 |
| Painful days | ||
| 2 years | 13.6 | 13.9 |
| 5 years | 8.3 | 7.8 |
The reasons for the rising incidence of arthroscopic acromioplasty are complex. This trend may be driven by patient, surgeon, technology, society and/or employer related reasons. At present, expenses and best evidence must also be taken into consideration. Based on our two-year results we concluded that acromioplasty is not cost-effective.24 Structured exercise treatment should be the treatment of choice for shoulder impingement syndrome. Operative treatment should be offered with discernment. In 2010 the Finnish National Institute for Health and Welfare reported that the combined incidence of open and arthroscopic acromioplasties was 91.6/100 000 in Finland.39 In the New York area the incidence was 101.9/100 000 in 2006 and has risen vastly in the previous decade.25 The indications for arthroscopic acromioplasty should also be thoroughly discussed. We believe that the natural course of the disease should be better defined to improve the judgement of different treatment options.
The indications for arthroscopic acromioplasty in the treatment of shoulder impingement syndrome should be reconsidered. Based on our results, it seems that the mere presence of an uncomplicated shoulder impingement syndrome is not an indication for arthroscopic acromioplasty per se, as conservative treatment with a structured exercise program provides as good results at five years at a lower cost.
Conclusions
The additional effect of acromioplasty on top of structured exercise is not significant in the treatment of shoulder impingement syndrome when evaluated at two and five years. Approximately 75% of patients recover well and the rest continue to have discomfort despite the treatment. The effects of the arthroscopic acromioplasty may have been overestimated due to regression to the mean and the natural long-term course of the shoulder impingement syndrome.
The authors would like to thank A-M. Lampela, Physiotherapist, for assistance in examining the patients and Professor H. Sintonen for providing the 15D age-adjusted general population data for comparison.
1 Pope DP , CroftPR, PritchardCM, SilmanAJ. Prevalence of shoulder pain in the community: the influence of case definition. Ann Rheum Dis1997;56:308–312.CrossrefPubMed Google Scholar
2 Urwin M , SymmonsD, AllisonT, et al.Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis1998;57:649–655.CrossrefPubMed Google Scholar
3 Mäkelä M , HeliövaaraM, SainioP, et al.Shoulder joint impairment among Finns aged 30 years or over: prevalence, risk factors and co-morbidity. Rheumatology (Oxford)1999;38:656–662.CrossrefPubMed Google Scholar
4 Picavet HS , SchoutenJS. Musculoskeletal pain in the Netherlands: prevalences, consequences and risk groups, the DMC(3)-study. Pain2003;102:167–178.CrossrefPubMed Google Scholar
5 van der Windt DA , KoesBW, de JongBA, BouterLM. Shoulder disorders in general practice: incidence, patient characteristics, and management. Ann Rheum Dis1995;54:959–964.CrossrefPubMed Google Scholar
6 Neer CS 2nd . Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg [Am]1972;54-A:41–50.PubMed Google Scholar
7 Soyer J , VazS, PriesP, ClaracJP. The relationship between clinical outcomes and the amount of arthroscopic acromial resection. Arthroscopy2003;19:34–39.CrossrefPubMed Google Scholar
8 Henkus HE , de WittePB, NelissenRG, BrandR, van ArkelER. Bursectomy compared with acromioplasty in the management of subacromial impingement syndrome: a prospective randomised study. J Bone Joint Surg [Br]2009;91-B:504–510.CrossrefPubMed Google Scholar
9 Morrison DS , FrogameniAD, WoodworthP. Non-operative treatment of subacromial impingement syndrome. J Bone Joint Surg [Am]1997;79-A:732–737.CrossrefPubMed Google Scholar
10 Lindh M , NorlinR. Arthroscopic subacromial decompression versus open acromioplasty: a two-year follow-up study. Clin Orthop Relat Res1993;290:174–176. Google Scholar
11 Spangehl MJ , HawkinsRH, McCormackRG, LoomerRL. Arthroscopic versus open acromioplasty: a prospective, randomized, blinded study. J Shoulder Elbow Surg2002;11:101–107.CrossrefPubMed Google Scholar
12 Husby T , HaugstvedtJR, BrandtM, HolmI, SteenH. Open versus arthroscopic subacromial decompression: a prospective, randomized study of 34 patients followed for 8 years. Acta Orthop Scand2003;74:408–414.CrossrefPubMed Google Scholar
13 Brox JI , GjengedalE, UppheimG, et al.Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg1999;8:102–111.CrossrefPubMed Google Scholar
14 Brox JI , StaffPH, LjunggrenAE, BrevikJI. Arthroscopic surgery compared with supervised exercises in patients with rotator cuff disease (stage II impingement syndrome). BMJ1993;307:899–903.CrossrefPubMed Google Scholar
15 Haahr JP , AndersenJH. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4-8-years’ follow-up in a prospective, randomized study. Scand J Rheumatol2006;35:224–228. Google Scholar
16 Haahr JP , ØstergaardS, DalsgaardJ, et al.Exercises versus arthroscopic decompression in patients with subacromial impingement: a randomised, controlled study in 90 cases with a one year follow up. Ann Rheum Dis2005;64:760–764.CrossrefPubMed Google Scholar
17 Neer CS 2nd . Impingement lesions. Clin Orthop Relat Res1983;173:70–77. Google Scholar
18 van der Windt DA , KoesBW, BoekeAJ, et al.Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract1996;46:519–523.PubMed Google Scholar
19 Buchbinder R , GreenS, YoudJM. Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev2003;1:CD004016.CrossrefPubMed Google Scholar
20 van der Heijden GJ . Shoulder disorders: a state-of-the-art review. Baillieres Best Pract Res Clin Rheumatol1999;13:287–309.CrossrefPubMed Google Scholar
21 Green S , BuchbinderR, HetrickS. Physiotherapy interventions for shoulder pain. Cochrane Database Syst Rev2003;2:CD004258.CrossrefPubMed Google Scholar
22 Ludewig PM , BorstadJD. Effects of a home exercise programme on shoulder pain and functional status in construction workers. Occup Environ Med2003;60:841–849.CrossrefPubMed Google Scholar
23 Michener LA , WalsworthMK, BurnetEN. Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review. J Hand Ther2004;17:152–164.CrossrefPubMed Google Scholar
24 Ketola S , LehtinenJ, ArnalaI, et al.Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg [Br]2009;91-B:1326–1334.CrossrefPubMed Google Scholar
25 Vitale MA , AronsRR, HurwitzS, AhmadCS, LevineWN. The rising incidence of acromioplasty. J Bone Joint Surg [Am]2010;92-A:1842–1850.CrossrefPubMed Google Scholar
26 Yu E , CilA, HarmsenWS, SchleckC, SperlingJW, CofieldRH. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: an epidemiologic study. Arthroscopy2010;26(Suppl):S142–S147.CrossrefPubMed Google Scholar
27 Moeller TB, Reif E. MRI parameters and positioning. Stuttgart: Thieme, 2003. Google Scholar
28 van der Windt DA , van der HeijdenGJ, de WinterAF, et al.The responsiveness of the Shoulder Disability Questionnaire. Ann Rheum Dis1998;57:82–87.CrossrefPubMed Google Scholar
29 van der Heijden GJ , LeffersP, BouterLM. Shoulder disability questionnaire design and responsiveness of a functional status measure. J Clin Epidemiol2000;53:29–38.CrossrefPubMed Google Scholar
30 Sintonen H . The 15D instrument of health-related quality of life: properties and applications. Ann Med2001;33:328–336.CrossrefPubMed Google Scholar
31 Bøhmer AS , StaffPH, BroxJI. Supervised exercises in relation to rotator cuff disease (impingement syndrome stages II and III): a treatment regimen and its rationale. Physiother Theory Pract1998;14:93–105. Google Scholar
32 Gallagher EJ , LiebmanM, BijurPE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med2001;38:633–638.CrossrefPubMed Google Scholar
33 Sintonen H . Outcome measurement in acid-related diseases. Pharmaco Economics1994;5(Suppl 3):17–26. Google Scholar
34 Chang WK . Shoulder impingement syndrome. Phys Med Rehabil Clin N Am2004;15:493–510.CrossrefPubMed Google Scholar
35 Yamaguchi K , TetroAM, BlamO, et al.Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg2001;10:199–203.CrossrefPubMed Google Scholar
36 Nove-Josserand L, Walch G, Adeleine P, Courpron P. Effect of age on the natural history of the shoulder: a clinical and radiological study in the elderly. Rev Chir Orthop Reparatrice Appar Mot 2005;91:508–514 (in French). Google Scholar
37 Moosmayer S , SmithHJ. Diagnostic ultrasound of the shoulder: a method for experts only?: results from an orthopedic surgeon with relative inexpensive compared to operative findings. Acta Orthop2005;76:503–508. Google Scholar
38 Luyckx L , LuyckxT, DonceelP, DebeerP. Return to work after arthroscopic subacromial decompression. Acta Orthop Belg2011;77:737–742.PubMed Google Scholar
39 Finnish National Institute of Health and Welfare. Statistics and registers. www.thl.fi/statistics (date last accessed 28 June 2013). Google Scholar
Funding statement:
None declared
Author contributions:
S. Ketola: Planning of the study (overall planning), Substantive intellectual contribution, Seeking permits from the ethical committee, Seeking permits from the hospitals, Recruitment of the patients, Organisation of the study, Collection and organisation of the data, Statistical analysis, Literature review, Writing the draft, Critical commenting and improvement of the manuscript
J. Lehtinen: Recruitment of the patients, Organisation of the study, Thesis supervision, Clinical analysis of the data, Literature review, Writing the draft, Critical commenting and improvement of the manuscript
T. Rousi: Planning of the study (overall and especially physiotherapeutic aspects), Seeking permits from the ethical committee, Seeking permits from the hospitals, Clinical analysis of the data, Critical commenting and improvement of the manuscript
M. Nissinen: Planning of the study, Recruitment of the patients, Seeking permits from the hospitals, Critical commenting and improvement of the manuscript
H. Huhtala: Statistical analysis, Critical commenting and improvement of the manuscript
Y. T. Konttinen: Substantive intellectual contribution, Clinical analysis of the data, Critical commenting and improvement of the manuscript
I. Arnala: Planning of the study (overall and especially operative aspects), Seeking permits from the hospitals, Organisation of the study, Thesis supervision, Clinical analysis of the data, Critical commenting and improvement of the manuscript
ICMJE Conflict of Interest:
None declared
©2013 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










