Abstract
Objectives
The purpose of this study was to examine the effect of posterior cruciate ligament (PCL) retention, PCL recession, and PCL excision during cruciate-retaining total knee replacement.
Methods
A total of 3018 anatomic graduated component total knee replacements were examined; 1846 of these retained the PCL, 455 PCLs were partially recessed, and in 717 the PCL was completely excised from the back of the tibia.
Results
Clinical scores between PCL groups favored excision for flexion (p < 0.0001), and recession and retention for stairs (p < 0.0001). There was a mild difference in long-term all-cause aseptic survivorship between PCL-retained (96.4% at 15 years) combined with PCL-recessed groups (96.6% at 15 years) when compared with the PCL-excised group (95.0% at 15 years) (p = 0.0411, Wilcoxon; p = 0.0042, log-rank), as well as tibial or femoral loosening, which reported prosthesis survival of 97.8% at 15 years for PCL-retained knees, 98.2% for recessed knees, and 96.4% for excised knees (p = 0.0934, Wilcoxon; p = 0.0202, log-rank).
Conclusions
Despite some trade-off in clinical performance, if the PCL is detached at the time of operation, conversion to a posterior-stabilised prosthesis may not be necessarily required as long as stability in the anteroposterior and coronal planes is achieved.
Article focus
The focus of this study was to examine the various degrees of recession of the posterior cruciate ligament (PCL) (retained, partially-recessed, and excised) on the long-term clinical outcome and survivorship of total knee replacement
Key messages
There was an observable increase in flexion for PCL-excised knees, and an increase in stairs score for -recessed and -retained knees
We observed a mild difference in all-cause aseptic survivorship at 15 years, along with a mild difference in survivorship for aseptic tibial and femoral failure at 15 years favouring PCL-retained and -recessed knees
Increase in the variability of the excised group may partially explain the ambiguity present in the literature; however, the observations of this study do not necessarily justify the change to a posterior-stabilised prosthesis when the PCL is excised
Strengths and limitations
Strengths include a large population and longer follow-up than previously reported in the literature
Limitations include that this is a retrospective observational study and the determination of a direct and exclusive causal relationship between PCL excision and outcome cannot be directly proven, although these findings are important in this debate
Introduction
Total knee replacement (TKR) has provided success rates of > 90%,1-13 with many studies reporting success rates > 95% after ten or more years.1,3,4,6,7,10-12 In order to further improve the procedure, debate has arisen regarding sources of failure in TKR, including examination of the role of the posterior cruciate ligament (PCL). Some studies have demonstrated less consistent success with retention of the PCL,9,14 while other studies have found advantages in proprioception15 and kinematics16-20 when the PCL is retained. Studies examining recession of the PCL have found similarly conflicting results.11,21 Survivorship analyses have examined the success of each method,9,22 but taken collectively, the literature has not been able to recommend one procedure over the others.23 Two studies using a cruciate-retaining prosthesis have shown that the PCL may not play a dominant role if the ligaments overall are balanced.8,21 The first study examined 129 knees with a mean follow-up of 4.8 years (4.7 to 6.0),8 and the second followed 211 knees for a mean of 3.5 years (1.0 to 6.5).21
This study was undertaken to determine whether knees treated with a cruciate-retaining TKR alongside different PCL treatments would produce different outcomes. We hypothesised that sacrificing the PCL in a cruciate-retaining TKR would not result in a different outcome compared with retention of the PCL with regard to survivorship and clinical results.
Patients and Methods
Between April 1987 and December 2007, 10 677 primary TKRs were performed at our center. Of these, 9930 used anatomic graduated components (AGC; Biomet, Warsaw, Indiana), a cruciate-retaining TKR. Of these, 3905 were performed by two surgeons involved in the study (MAR, JBM). A total of 3018 TKRs (2002 patients) were cemented and had complete information regarding the status of the PCL recorded in the database, as well as a minimum follow-up of two years. These 3018 TKRs met the inclusion criteria of the study.
This study group comprised 1144 females (57%) and 858 males (43%), with a mean age at surgery of 69.3 years (sd 9.8; 23 to 93), and a mean body mass index (BMI) of 28.7 kg/m2 (sd 5.3; 16.5 to 53.4). Diagnoses included osteoarthritis in 2916 knees (96.6%), rheumatoid arthritis in 77 knees (2.6%), and osteonecrosis in 25 knees (0.8%).
In 1846 TKRs in 1214 patients (1833 TKRs undertaken by MAR, 13 by JBM), specific recession or release of the PCL was not required, and these procedures comprised the PCL-retained group. The intra-operative management of the PCL was uniformly based on obtaining minimal to no femoral roll-back. If any anterior tibial component lift-off at 90° of flexion was noted, the tight PCL fibers were selectively released from the proximal tibia until lift-off no longer occurred. At this point the PCL was considered to be balanced. The entire PCL was not released in this case. A thicker implant was never necessary, and a loose flexion gap or posterior insufficiency was never accepted intra-operatively. In 455 TKRs in 327 patients (all TKRs undertaken by MAR), the PCL was progressively released off the posterior tibia until the above criteria were met, with these knees comprising the PCL-recessed group. In the remaining 717 TKRs in 461 patients (four TKRs undertaken by MAR and 713 by JBM), the PCL was completely released off the back of the tibia during the approach and not in a stepwise fashion. These knees comprise the PCL-excised group.
The tibial component of the AGC total knee system is a mono-block titanium-backed fixed-bearing component with nearly flat-on-flat geometry. This flat design was used for all three procedure types; no posterior-stabilised designs were used. The two surgeons used the same arthroplasty procedure, beginning with a standard medial parapatellar approach; each TKR differed only in treatment of the PCL (retention, recession or excision). All patients in all categories underwent an identical post-operative course of treatment, with walking initiated within one day post-operatively, and distance walked and range of motion increased on subsequent days.
Patients were evaluated pre-operatively, at six months, and at one, three, five, seven, ten, 12, and 15 years post-operatively using the Knee Society clinical rating system.24 Knee Society knee and function scores; the pain, stairs, and walking subscores; range of motion; anatomic alignmentwith varus < 5° of anatomical valgus, neutral between 5° and 10°, and valgus > 10°; and anteroposterior and mediolateral stability were recorded prospectively. Each exam was performed by the attending surgeon.
The mean follow-up was 7.8 years (sd 4.0, 2 to 21). Table I lists the demographic and pre-operative data between groups.
Statistical analysis
Statistical analysis was performed to determine differences in survivorship, mean knee, function, pain, stairs and walk scores, flexion, and anterolateral posterior stability as defined by the Knee Society knee score post-operatively after primary TKR. Kaplan-Meier survivorship analysis25 over 15 years was performed for each type of arthroplasty with failure defined as re-operation of the femoral or tibial component for any reason except infection. P-values for survival analyses were given by Kaplan-Meier analysis, and Cox regression was not performed due to possible confounding between surgeon and PCL status.
Due to a relatively large number of repeatedly returning patients after the index surgery (a mean of 3.1 post-operative clinical visits per knee), the clinical scores collected between one and ten years post-operatively were analysed by repeated measures linear regression. The authors selected an unstructured covariance structure in the model to allow the correlation of each patient to themselves to vary between each follow-up interval. Significant covariates analysed for each clinical outcome were age, gender, diagnosis, pre-operative BMI, pre-operative clinical score (matching the post-operative clinical score), differences between surgeons, pre-operative varus < -8°, pre-operative valgus > 11° and the variable of interest (status of the PCL).
Pre-operative score and patient demographics were analysed by one-way analysis of variance (ANOVA) for continuous variables (age, BMI, alignment and clinical score), and 2 × 2 contingency tables (the chi-square statistic) for categorical variables (gender and diagnosis). Level of significance was set at p = 0.05. All analyses were performed with SAS 9.1 (SAS Institute, Cary, North Carolina).
Results
The all-cause aseptic failure survival at ten years was 97.70% (95% confidence interval (CI) 96.53 to 98.47) for the PCL-retained knees, 96.60% (95% CI 93.33 to 98.28) for the PCL-recessed knees and 96.46% (95% CI 93.88 to 97.96) for the PCL-excised knees (Fig. 1). The all-cause aseptic fail survival at 15 years was 96.36% (95% CI 94.21 to 97.71) for PCL-retained, 96.60% (95% CI 93.33 to 98.28) for PCL-recessed and 94.95% (95% CI 89.98 to 97.49) for PCL-excised knees (Fig. 1). Excised knees were found to have a statistically significant lower survival than the combined retained and recessed groups (p = 0.0411, Wilcoxon; p = 0.0042, log-rank), and the retained and recessed group were not found to be significantly different from each other (p = 0.7020, Wilcoxon; p = 0.9543, log-rank).
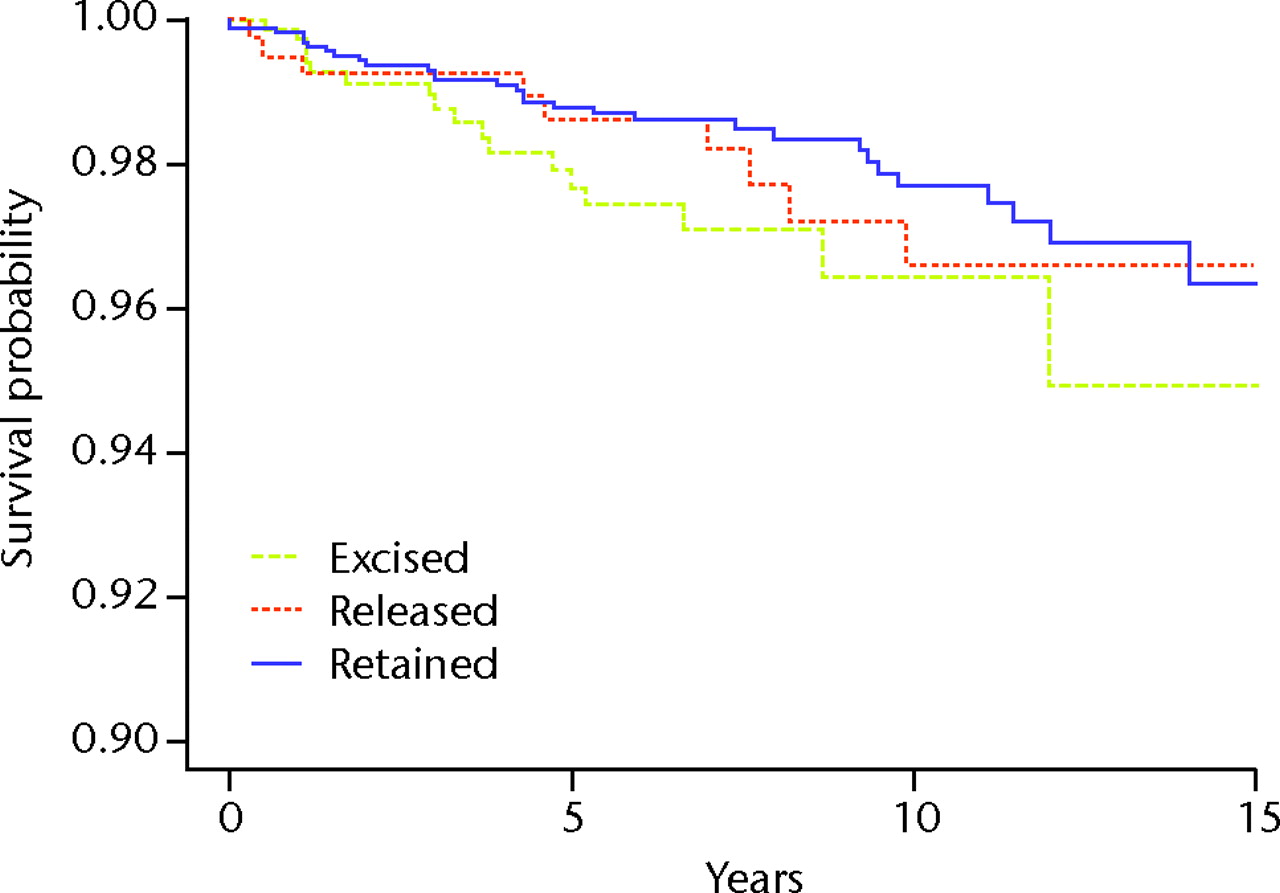
Fig. 1
Kaplan-Meier curve showing the all-cause aseptic survival for total knee replacements with the posterior cruciate ligament retained, partially recessed and excised.
With aseptic femoral loosening (n = 7), failure of the tibial prosthesis (n = 26), and radiolucency failure (n = 3) as endpoints, the survival at ten years was 98.95% (95% CI 98.13 to 99.41) for the PCL-retained knees, 98.16% (95% CI 95.03 to 99.33) for the PCL-recessed knees and 97.94% (95% CI 96.12 to 98.92) for the PCL-excised knees (Fig. 2). The corresponding survival at 15 years was 97.84% (95% CI 95.74 to 98.91) for the PCL-retained, 98.16% (95% CI 95.03 to 99.33) for the PCL-recessed, and 96.41% (95% CI 91.23 to 98.56) for the PCL-excised knees (Fig. 2). Excised knees were found to have a statistically significant lower survival than the combined retained and recessed groups (p = 0.0934, Wilcoxon; p = 0.0202, log-rank), and the retained and recessed group were not found to be significantly different from each other (p = 0.6000, Wilcoxon; p = 0.8330, log-rank).
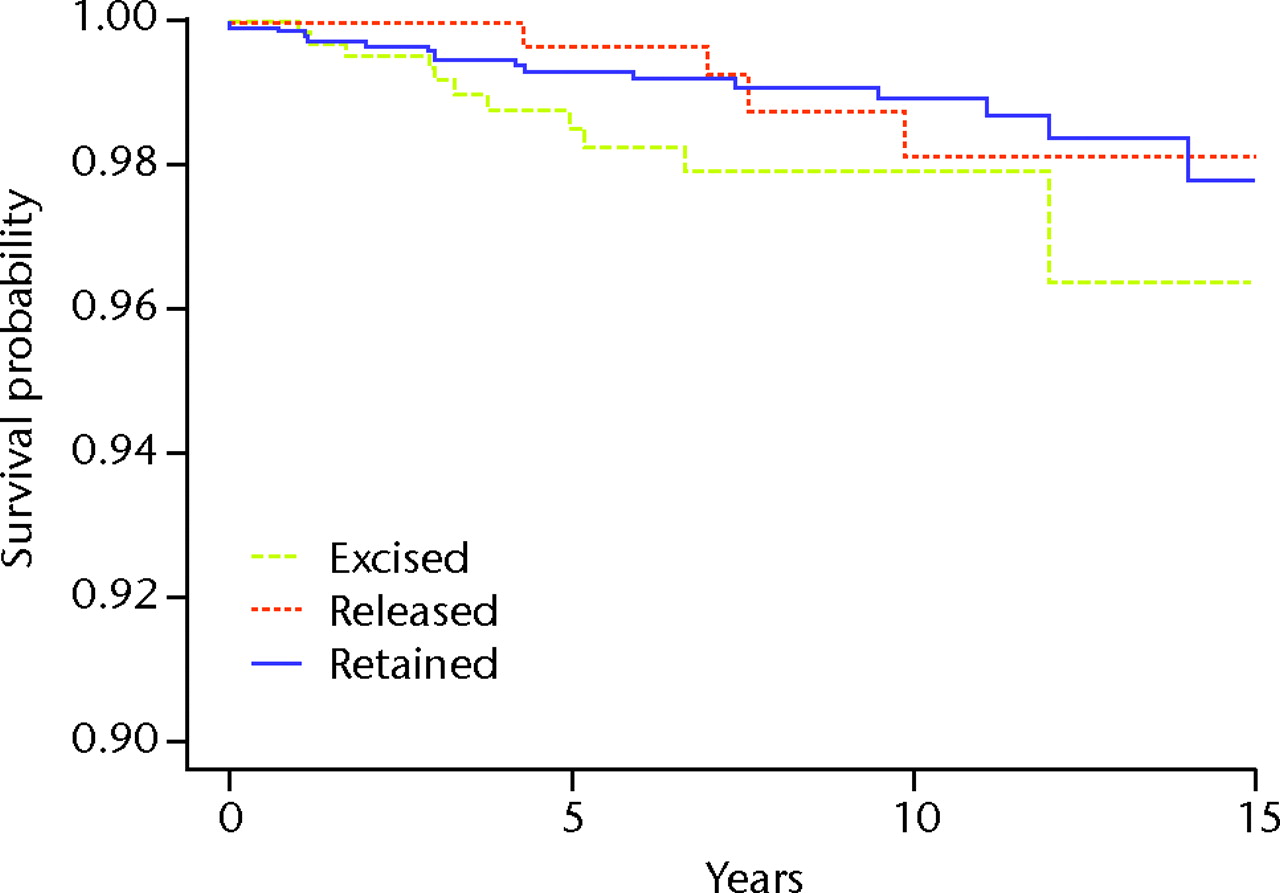
Fig. 2
Kaplan-Meier curve showing the survival of total knee replacements with the posterior cruciate ligament retained, released and excised, with aseptic femoral or tibial revision as the endpoints.
Failure rates of the additional all-cause failure mechanisms (infection in ten, trauma in seven, polyethylene wear in two, tibial fracture in one and patellar fracture in one) are described in Table II. The seven knees revised after trauma included a tibial collapse after a reported twisted knee in one, one loose tibia with polyethylene wear after stepping in a hole, a PCL tear exhibiting a 2 cm anterior-posterior instability after a motor vehicle accident, one patella found at the end of the endochondral notch after twisting the knee concurrent with a patient-reported “snap,” one medial tibial collapse after a fall, a loose femur and patella after a fall, and a clinical presentation of decreased flexion after being kicked by a cow.
We were unable to detect significant differences between PCL groups for Knee Society knee score (p = 0.3533; Fig. 3), function score (p = 0.4535; Fig. 4), pain score (p = 0.9217; Fig. 5), walking score (p = 0.7195; Fig. 6) or anteroposterior stability (p = 0.9899; Fig. 7). Flexion and stairs scores reported significant differences (both with p < 0.001; Figs 8 and 9), with flexion favouring the PCL-excision group with a mean flexion of 119.2° (sd 10.7; 40° to 150°) for the excised group compared with 112.2° (sd 11.3; 30° to 150°) for the combined PCL retention and recession group, and stairs favouring PCL retention and recession with overall mean stairs score of 40.6 (sd 9.7; 0 to 50) for the combined retention and recession groups compared with 38.8 (sd 11.1; 0 to 50) for the excised group. Comparisons for each clinical measure are shown in Table III.
Table III
Differences in mean Knee Society24 scores between knees with excision of the posterior cruciate ligament (PCL) and those with retention/recession of the PCL
| Mean (sd) outcome score | PCL-retention/ recession | PCL-excision | p-value* |
|---|---|---|---|
| Knee score | 88.8 (9.0) | 89.7 (10.3) | 0.3533 |
| Pain | 45.1 (7.1) | 45.3 (8.2) | 0.9217 |
| Flexion | 112.2 (11.3) | 119.2 (10.7) | < 0.0001 |
| Anteroposterior stability | 10.0 (0.3) | 10.0 (0.0) | 0.9899 |
| Function score | 80.0 (19.1) | 77.3 (21.1) | 0.4535 |
| Stairs | 40.6 (9.7) | 38.8 (11.1) | < 0.0001 |
| Walk | 41.0 (10.2) | 40.3 (12.7) | 0.7195 |
-
* repeated measures linear regression
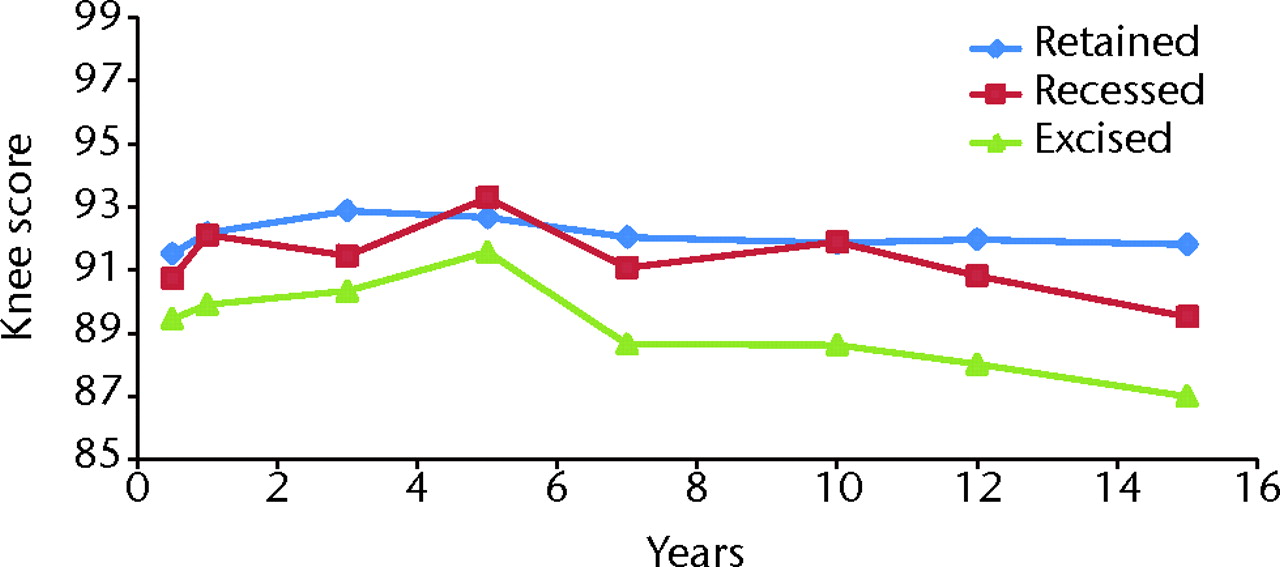
Fig. 3
Graph showing the mean Knee Society knee scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
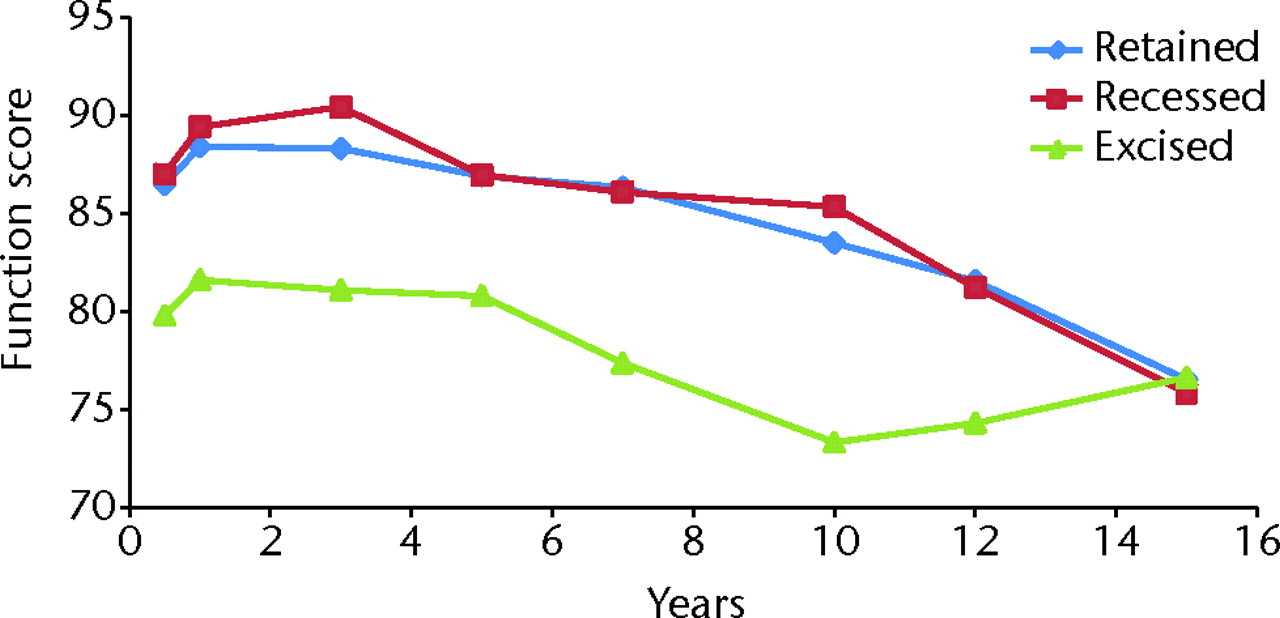
Fig. 4
Graph showing the mean Knee Society function scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
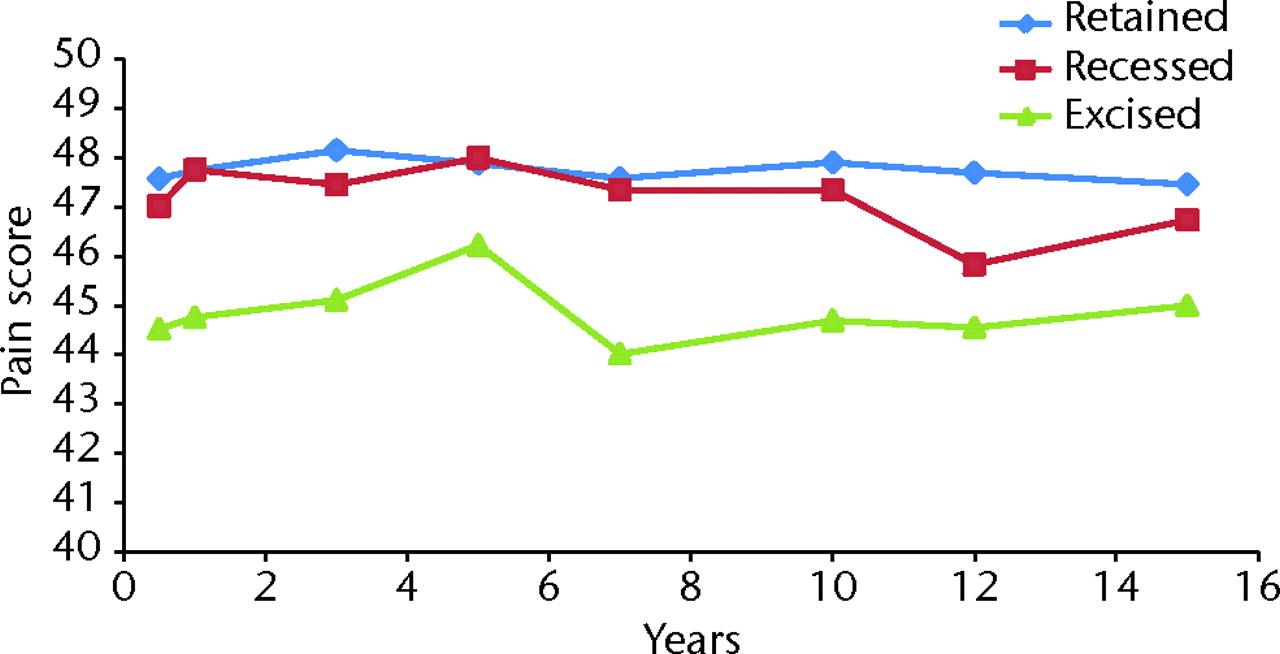
Fig. 5
Graph showing the mean Knee Society pain scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
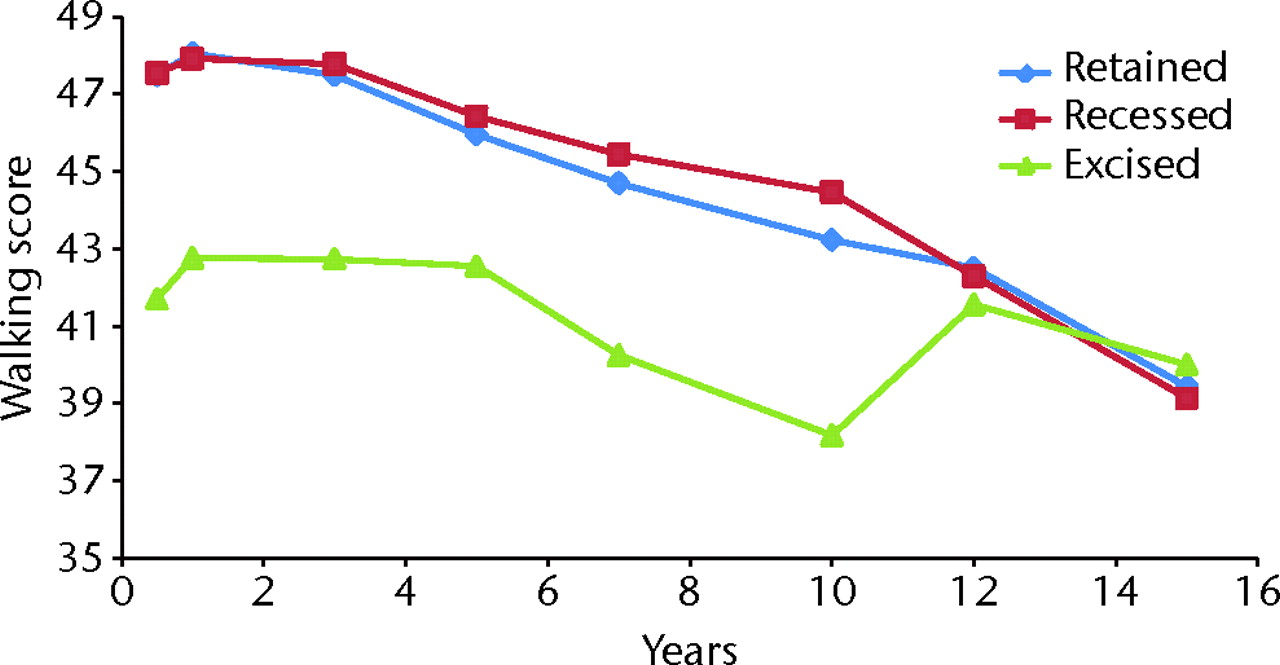
Fig. 6
Graph showing the mean Knee Society walking scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
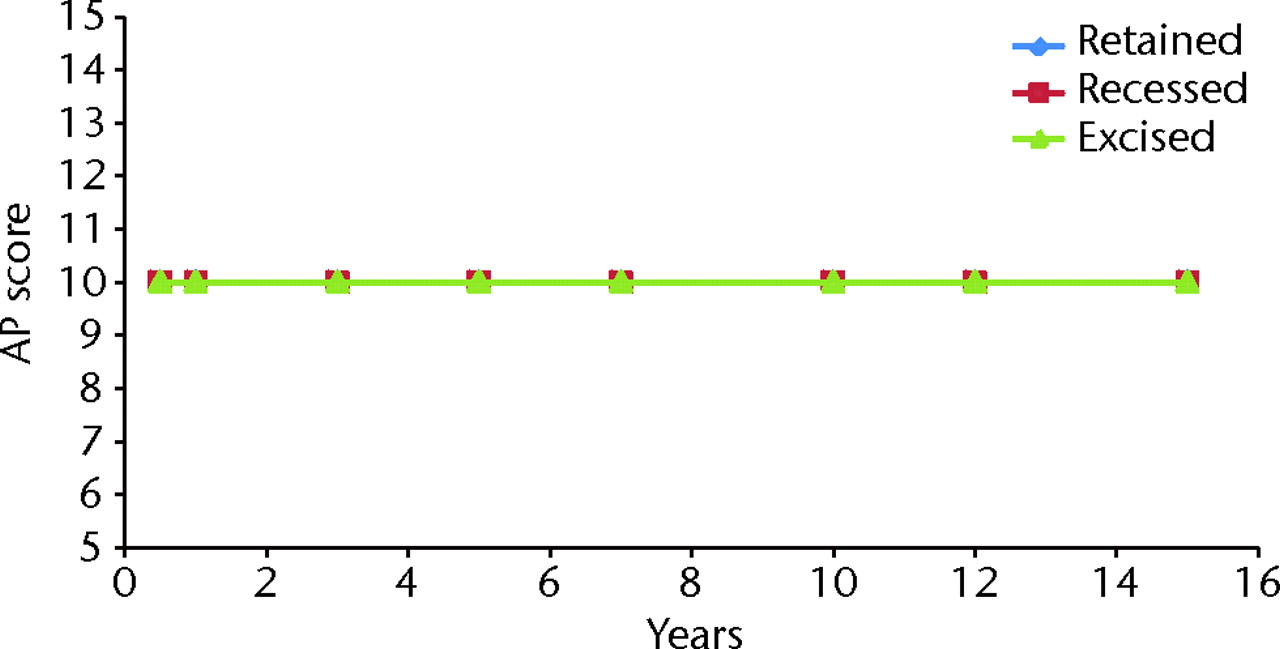
Fig. 7
Graph showing the mean Knee Society anteroposterior (AP) scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
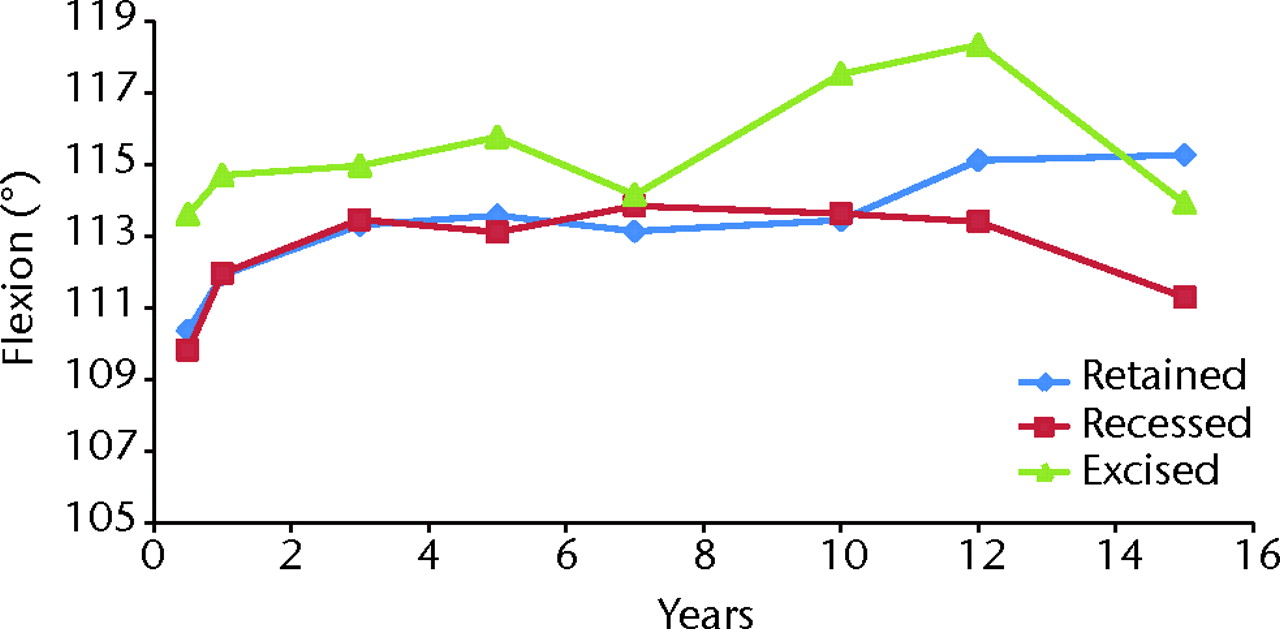
Fig. 8
Graph showing the mean flexion for the groups with retention, recession and excision of the posterior cruciate ligament.
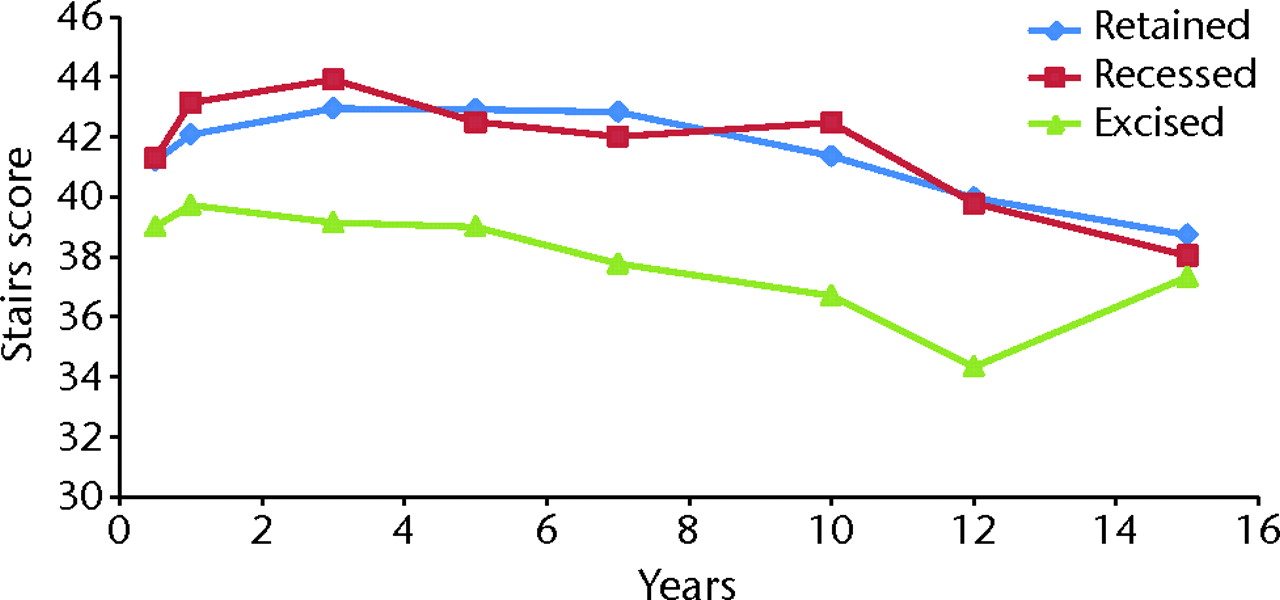
Fig. 9
Graph showing the mean Knee Society stairs scores24 for the groups with retention, recession and excision of the posterior cruciate ligament.
The observed numerical differences in the PCL-excised group for clinical scores were found to be multifactorial, primarily caused by the effects of 1) age (older patients scored lower for function score (p < 0.0001), higher for flexion (p = 0.0495), lower for stairs score (p < 0.0001) and lower for walking score (p < 0.0001)), 2) gender (males scored higher for function score, higher for flexion, higher for stairs and walking scores (all p < 0.0001)), 3) surgeon differences (flexion (p < 0.0001) and walk score (p = 0.0007)), 4) diagnosis of rheumatoid arthritis (lower than osteoarthritis for function score (p = 0.0003), lower for stairs score (p = 0.0201) and lower for walk score (p < 0.0001)), 5) diagnosis of osteonecrosis (lower than osteoarthritis for pain score (p = 0.0168)), 6) pre-operative BMI (higher BMI scored lower for function (p < 0.0001), better (higher) for pain score (p = 0.0006), lower for flexion (p = 0.0094), lower for stairs score (p = 0.0447) and lower for walk score (p < 0.0001)), 7) a pre-operative clinical score positively correlated with post-operative clinical outcome (function score (p < 0.0001), flexion (p < 0.0001), stairs (p ≤ 0.0007) and walking scores (p = 0.0015)), and 8) pre-operative valgus deformity > 11° (lower for knee score (p = 0.0217), lower for function score (p = 0.0001), lower for walk (p = 0.0150), higher for flexion (p < 0.0001) and lower for stairs (p < 0.0001)).
There was an increase in the variability of clinical outcome between PCL groups indicating a somewhat wider dispersion for the excised group about the mean in clinical outcome scores. The observed differences were +49% variance for knee score (p < 0.0001), +140% variance for function score (p < 0.0001), -23% variance for flexion (p =0.0026), +56% variance for pain score (p ≤ 0.0001), +12% variance for stairs (p = 0.0302), +96% variance for walk score (p < 0.0001) and +0% for anteroposterior stability (p = 1.000).
Discussion
The fate of the posterior cruciate ligament in TKR has remained unclear since the first TKR designs. Some have argued that the PCL should be retained, either partially or completely, because it aids knee joint proprioception15 and results in a closer approximation of normal knee kinematics.16,18-20 Others have not found an increase in proprioception with preservation of the PCL,26,27 possibly as a result of marked degenerative changes in the PCL of osteoarthritic patients.28 Some studies have found that TKRs that sacrifice the PCL, such as posterior-stabilised prostheses, provide more natural kinematics with appropriate posterior femoral translation.29 Clinical results also have not definitively supported either preserving or removing the PCL, as studies have demonstrated similar clinical outcome scores for retention and excision of the PCL.8,13,21,30,31
We were unable to find any differences in the clinical outcome of retention or recession of the PCL in AGC TKR. Flexion (in favour of PCL excision) and stairs subscore (in favour of PCL retention and recession) were found to be influenced by the presence or absence of the PCL, and some differences were found both in the all-cause and femorotibial failure rates between knees with and without the PCL. We are continuing to study if those differences were a consequence of excision or some other factor related to knees requiring excision.
For the clinical data, we used repeated measures multiple linear regression on data up to ten years both to control the loss of late follow-up that we did encounter, and because data up to ten years after surgery is sufficiently stable to prove reliable.32 This statistical method also accounted for the demographic and pre-operative differences between the PCL groups (Table I), decreasing the chance that such differences could influence the results.
Table I
Demographics and mean [sd] (range) pre-operative clinical scores for the posterior cruciate ligament (PCL)-retained, -recessed and -excised groups
| p-values (1-way ANOVA, least squares means test) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| PCL-retained (n = 1846) | PCL-recessed (n = 455) | PCL-excised (n = 717) | PCL-retained vs PCL-recessed | PCL-retained vs PCL-excised | PCL-recessed vs PCL-excised | ||||
| Age (yrs) | 71.0 [9.2] (23 to 93) | 70.0 [9.3] (39 to 89) | 65.9 [10.2] (28 to 91) | 0.0269 | < 0.0001 | < 0.0001 | |||
| Body mass index (kg/m2) | 27.1 [3.4] (18 to 49) | 26.6 [3.1] (19 to 37) | 33.1 [6.5] (17 to 53) | 0.6792 | < 0.0001 | < 0.0001 | |||
| Female (%) | 57.6% | 57.9% | 53.8% | 0.1149 | 0.0558 | 0.9073 | |||
| Follow-up (yrs) | 8.0 [4.6] (2 to 23.2) | 7.8 [4.0] (2.0 to 18.1) | 5.8 [3.0] (2.0 to 14.8) | < 0.0001 | < 0.0001 | < 0.0001 | |||
| Knee score | 33.8 [13.9] (2 to 95) | 34.7 [13.9] (3 to 81) | 38.7 [10.6] (10 to 77) | 0.0846 | < 0.0001 | 0.0002 | |||
| Pain score | 4.4 [10.0] (0 to 50) | 6.8 [10.5] (0 to 50) | 9.0 [8.4] (0 to 50) | < 0.0001 | < 0.0001 | 0.0006 | |||
| Flexion (°) | 113.7 [12.7] (30 to 150) | 112.7 [13.5] (40 to 140) | 106.0 [12.0] (45 to 135) | 0.2275 | < 0.0001 | < 0.0001 | |||
| Alignment (°) | 0.1 [8.5] (-22 to 35) | -0.3 [8.9] (-22 to 30) | 0.0 [2.9] (-15 to 20) | 0.4568 | 0.8836 | 0.6585 | |||
| Function score | 45.9 [11.6] (0 to 100) | 45.3 [13.2] (0 to 100) | 47.6 [15.6] (0 to 100) | 0.4816 | 0.0045 | 0.0073 | |||
| Walking score | 19.8 [6.8] (0 to 50) | 20.1 [7.8] (0 to 50) | 21.2 [9.2] (0 to 50) | 0.4879 | 0.0004 | 0.0436 | |||
| Stairs score | 29.5 [5.0] (0 to 50) | 28.7 [5.9] (0 to 50) | 29.2 [7.8] (0 to 50) | 0.0111 | 0.2556 | 0.1784 | |||
Table II
Details of failures in the knees with retention, recession and excision of the posterior cruciate ligament
| Mode of failure (n, %) | PCL-retained (n = 1846) | PCL-recessed (n = 455) | PCL-excised (n = 717) |
|---|---|---|---|
| Instability | 8 (0.4) | 3 (0.7) | 4 (0.6) |
| Tibial collapse | 7 (0.4) | 0 (0) | 4 (0.6) |
| Loose tibial component | 0 (0) | 0 (0) | 1 (0.1) |
| Femur | 1 (0.1) | 2 (0.4) | 4 (0.6) |
| Radiolucency | 2 (0.1) | 1 (0.2) | 0 (0) |
| Polyethylene wear | 2 (0.1) | 0 (0) | 0 (0) |
| Patellar failure | 3 (0.2) | 0 (0) | 0 (0) |
| Tibial bone fracture | 0 (0) | 1 (0.2) | 0 (0) |
| Infection | 4 (0.2) | 2 (0.4) | 4 (0.6) |
| Trauma | 4 (0.2) | 1 (0.2) | 2 (0.3) |
| Total failed (n, %) | 31 (1.7) | 10 (2.2) | 19 (2.6) |
Kinematic analyses have examined the motion paths and weight loads of various TKR designs, including those that retain and excise the PCL.17,18,24,33-37 One study found no difference between PCL retention and excision with regards to the position and movement of the lateral and medial femoral condyles on the tibial component.18 Another study found PCL-retained TKR to be more efficient due to decreased muscle activity.17 Other analyses have found paradoxical anterior femoral translation on the tibia in PCL-retained arthroplasties.35-37 One analysis of axial rotation during stair-stepping found a wide range of internal rotation patterns in PCL-retained knees33; however, all knees selected for the study provided excellent clinical results, suggesting that “a range of knee motion patterns are well accommodated by patients”.33 The present study did not examine the kinematics aspect of the PCL debate; however, we report PCL-retained and PCL-recessed TKRs with noticeably greater stair-stepping outcomes compared with arthroplasties that excise the PCL. This implies that the PCL may be necessary for obtaining optimum function after TKR, regardless of the internal rotation patterns of knees with a retained or recessed PCL. Additionally, the PCL-excised knees exhibited increased flexion, indicating the possibility that the kinematics of the excised knee may be somewhat different than that of the retained or recessed knee.
The literature has not yet exposed one treatment of the PCL as the best method in TKR. A systematic review23 of the literature found eight randomised controlled trials.8,21,26,30,34,38-40 Of these, three studies8,21,30 examined the results of the same implant with and without the PCL, two of the groups included in our study. A best-evidence synthesis found no differences in the Hospital for Special Surgery score,41 range of motion or patient satisfaction between PCL-retained and PCL-excised TKR. The wider meta-analysis of the data from all eight studies demonstrated no significant difference in range of motion between PCL retention and PCL excision with use of the same prosthesis. This was the only conclusion the meta-analysis could produce because of the methodological inconsistencies between the eight studies; also, it could not conclude anything about PCL recession because it was not studied separately. Our study agrees with the meta-analysis in that there is no significant difference in objective knee score, using the Knee Society score instead of the Hospital for Special Surgery score.
The limitations of this study include retrospective analysis of prospectively-gathered data without a radiological review. There is no way for us to determine whether the state of the PCL directly caused higher or lower scores; however, our finding of the lack of differences between groups with PCL retention, recession, and excision remains important to the debate over its preservation. We excluded patients from our study who did not have an AGC implant or complete data required for analysis, and who were not treated by one of the two surgeons involved with the study, which may introduce a slight selection bias into our results. However, given the high number of joints that remained in the study, the data provided should prove valuable.
One could express concern that by 15 years we had lost a significant amount of patients over the study period. However, that conclusion requires an assumption that all surgeries were performed within a short time period, which is not the case in this study. We examined patients with surgeries that occurred between 1987 and 2007, so knees that had an operation in the latter part of the study period were not lost to follow-up; they simply would not reach the longer follow-up levels that knees which underwent earlier procedures could.
Knees with PCL retention or recession with an AGC prosthesis had improved stairs subscores compared with those with excision of the PCL, whereas greater motion was attained in knees with PCL excision. Post-operative pain was not found to be different among PCL groups. Although difficult to quantify here, the effect of surgeon appeared to weigh heavily on the effect of PCL status, more so than previously thought. If the PCL is detached at the time of operation, conversion to a posterior-stabilised prosthesis may not necessarily be needed as long as anteroposterior and coronal plane stability is achieved.
1 Ali MS , MangaleshkarSR. Uncemented rotating-platform total knee arthroplasty: a 4-year to 12-year follow-up. J Arthroplasty2006;21:80–84.CrossrefPubMed Google Scholar
2 Archibeck MJ , BergerRA, BardenRM, et al.Posterior cruciate ligament-retaining total knee arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg [Am]2001;83-A:1231–1236.CrossrefPubMed Google Scholar
3 Dixon MC , BrownRR, ParschD, ScottRD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament: a study of patients followed for a minimum of fifteen years. J Bone Joint Surg [Am]2005;87-A:598–603. Google Scholar
4 Faris PM , KeatingEM, FarrisA, MedingJB, RitterMA. Hybrid total knee arthroplasty: 13-year survivorship of AGC total knee systems with average 7 years followup. Clin Orthop Relat Res2008;466:1204–1209.CrossrefPubMed Google Scholar
5 Gill GS , JoshiAB. Long-term results of retention of the posterior cruciate ligament in total knee replacement in rheumatoid arthritis. J Bone Joint Surg [Br]2001;83-B:510–512.CrossrefPubMed Google Scholar
6 Lachiewicz PF , SoileauES. Ten-year survival and clinical results of constrained components in primary total knee arthroplasty. J Arthroplasty2006;21:803–808.CrossrefPubMed Google Scholar
7 Meding JB , KeatingEM, RitterMA, FarisPM, BerendME. Long-term followup of posterior-cruciate-retaining TKR in patients with rheumatoid arthritis. Clin Orthop Relat Res2004;428:146–152.CrossrefPubMed Google Scholar
8 Misra AN , HussainMR, FiddianNJ, NewtonG. The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg [Br]2003;85-B:389–392.CrossrefPubMed Google Scholar
9 Rand JA , TrousdaleRT, IlstrupDM, HarmsenWS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg [Am]2003;85-A:259–265.CrossrefPubMed Google Scholar
10 Ritter MA , BerendME, MedingJB, et al.Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop Relat Res2001;388:51–57.CrossrefPubMed Google Scholar
11 Sathappan SS , WassermanB, JaffeWL, et al.Midterm results of primary total knee arthroplasty using a dished polyethylene insert with a recessed or resected posterior cruciate ligament. J Arthroplasty2006;21:1012–1016.CrossrefPubMed Google Scholar
12 Schai PA , ScottRD, ThornhillTS. Total knee arthroplasty with posterior cruciate retention in patients with rheumatoid arthritis. Clin Orthop Relat Res1999;367:96–106.PubMed Google Scholar
13 Tang WM , ChiuKY, NgTP, YauWP. Posterior cruciate ligament-substituting total knee arthroplasty in young rheumatoid patients with advanced knee involvement. J Arthroplasty2004;19:49–55.CrossrefPubMed Google Scholar
14 Laskin RS , O'FlynnHM. The Insall Award. Total knee replacement with posterior cruciate ligament retention in rheumatoid arthritis: problems and complications. Clin Orthop Relat Res1997;345:24–28. Google Scholar
15 Warren PJ , OlanlokunTK, CobbAG, BentleyG. Proprioception after knee arthroplasty: the influence of prosthetic design. Clin Orthop Relat Res1993;297:182–187. Google Scholar
16 Bertin KC , KomistekRD, DennisDA, et al.In vivo determination of posterior femoral rollback for subjects having a NexGen posterior cruciate retaining total knee arthroplasty. J Arthroplasty2002;17:1040–1048. Google Scholar
17 Dorr LD , OchsnerJL, GronleyJ, PerryJ. Functional comparison of posterior cruciate retained versus cruciate-sacrificed total knee arthroplasty. Clin Orthop Relat Res1988;236:36–43. Google Scholar
18 Komistek RD , MahfouzMR, BertinKC, RosenbergA, KennedyW. In vivo determination of total knee arthroplasty kinematics: a multicenter analysis of an asymmetrical posterior cruciate retaining total knee arthroplasty. J Arthroplasty2008;23:41–50.CrossrefPubMed Google Scholar
19 Li G , ZayontzS, MostE, et al.Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty2001;16(Suppl 1):150–156.CrossrefPubMed Google Scholar
20 Most E , ZayontzS, LiG, et al.Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop Relat Res2003;410:101–113.CrossrefPubMed Google Scholar
21 Straw R , KulkarniS, AttfieldS, WiltonTJ. Posterior cruciate ligament at total knee replacement: essential, beneficial, or a hindrance?J Bone Joint Surg [Br]2003;85-B:671–674. Google Scholar
22 Buechel FF Sr . Long-term followup after mobile-bearing total knee replacement. Clin Orthop Relat Res2002;404:40–50.CrossrefPubMed Google Scholar
23 Jacobs WC , ClementDJ, WymengaAB. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop2005;76:757–768.CrossrefPubMed Google Scholar
24 Insall JN , DorrLD, ScottRD, ScottWN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res1989;248:13–14.PubMed Google Scholar
25 Kaplan EL , MeierP. Nonparametric estimation from incomplete observations. J Am Stat Assoc1958;53:457–481. Google Scholar
26 Swanik CB , LephartSM, RubashHE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg [Am]2004;86-A:328–334.CrossrefPubMed Google Scholar
27 Simmons S , LephartS, RubashH, BorsaP, BarrackRL. Proprioception following total knee arthroplasty with and without the posterior cruciate ligament. J Arthroplasty1996;11:763–768.CrossrefPubMed Google Scholar
28 Kleinbart FA , BrykE, EvangelistaJ, ScottWN, VigoritaVJ. Histologic comparison of posterior cruciate ligaments from arthritic and age-matched knee specimens. J Arthroplasty1996;11:726–731.CrossrefPubMed Google Scholar
29 Sharma A , KomistekRD, ScuderiGR, CatesHE Jr. High-flexion TKA designs: what are their in vivo contact mechanics?Clin Orthop Relat Res2007;464:117–126.CrossrefPubMed Google Scholar
30 Shoji H , WolfA, PackardS, YoshinoS. Cruciate retained and excised total knee arthroplasty: a comparative study in patients with bilateral total knee arthroplasty. Clin Orthop Relat Res1994;305:218–222. Google Scholar
31 Pereira DS , JaffeFF, OrtigueraC. Posterior cruciate ligament-sparing versus posterior cruciate ligament-sacrificing arthroplasty: functional results using the same prosthesis. J Arthroplasty1998;12:138–144. Google Scholar
32 Ritter MA , ThongAE, DavisKE, et al.Long-term deterioration of joint evaluation scores. J Bone Joint Surg [Br]2004;86-B:438–442.CrossrefPubMed Google Scholar
33 Banks SA , HodgeWA. Implant design affects knee arthroplasty kinematics during stair stepping. Clin Orthop Relat Res2004;426:187–193. Google Scholar
34 Clark CR , RorabeckCH, MacDonaldS, et al.Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res2001;392:208–212.CrossrefPubMed Google Scholar
35 Komistek RD , ScottRD, DennisDA, et al.In vivo comparison of femorotibial contact positions for press-fit posterior stabilized and posterior cruciate-retaining total knee arthroplasties. J Arthroplasty2002;17:209–216.CrossrefPubMed Google Scholar
36 Victor J , BanksS, BellemansJ. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg [Br]2005;87-B:646–655.CrossrefPubMed Google Scholar
37 Yoshiya S , MatsuiN, KomistekRD, et al.In vivo kinematic comparison of posterior cruciate-retaining and posterior stabilized total knee arthroplasties under passive and weight-bearing conditions. J Arthroplasty2005;20:777–783.CrossrefPubMed Google Scholar
38 Catani F , LeardiniA, EnsiniA, et al.The stability of the cemented tibial component of total knee arthroplasty: posterior cruciate retaining versus posterior-stabilized design. J Arthroplasty2004;19:775–782. Google Scholar
39 Maruyama S , YoshiyaS, MatsuiN, KurodaR, KurosakaM. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty2004;19:349–353.CrossrefPubMed Google Scholar
40 Tanzer M , SmithK, BurnettS. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty2002;17:813–819.CrossrefPubMed Google Scholar
41 Insall JN , RanawatCS, AgliettiP, ShineJ. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg [Am]1976;58-A:754–765.CrossrefPubMed Google Scholar
Funding statement:
None declared
Author contributions:
M. A. Ritter: Research leader, Lead surgeon, Writing the paper, Shaped research message
K. E. Davis: Data analysis, Writing the paper
J. B. Meding: Surgeon, Writing the paper
A. Farris: Writing the paper, Patient research
ICMJE Conflict of Interest:
None declared
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










