Abstract
Objectives
Orthopaedic surgeons use stems in revision knee surgery to obtain stability when metaphyseal bone is missing. No consensus exists regarding stem size or method of fixation. This in vitro study investigated the influence of stem length and method of fixation on the pattern and level of relative motion at the bone–implant interface at a range of functional flexion angles.
Methods
A custom test rig using differential variable reluctance transducers (DVRTs) was developed to record all translational and rotational motions at the bone–implant interface. Composite femurs were used. These were secured to permit variation in flexion angle from 0° to 90°. Cyclic loads were applied through a tibial component based on three peaks corresponding to 0°, 10° and 20° flexion from a normal walking cycle. Three different femoral components were investigated in this study for cementless and cemented interface conditions.
Results
Relative motions were found to increase with flexion angle. Stemmed implants reduced relative motions in comparison to stemless implants for uncemented constructs. Relative motions for cemented implants were reduced to one-third of their equivalent uncemented constructs.
Conclusions
Stems are not necessary for cemented implants when the metaphyseal bone is intact. Short cemented femoral stems confer as much stability as long uncemented stems.
Article focus
This laboratory study aims to determine the optimum implant configuration and method of fixation by measuring relative motion between bone and implant for a range of flexion angles
Key messages
Relative motions were found to increase with flexion in all cases. Testing for relative motions in extension only can provide misleading results
Cemented constructs were found to provide more initial stability than the equivalent uncemented constructs
Cemented short stems provide as much stability as long uncemented stems and are easier to use
Strengths and limitations
This is the first study to attempt to measure relative motions of the femoral component in all six degrees of freedom
This study supplements current knowledge on selection of appropriate stem sizes and fixation methods to aid informed decision making at the time of operation
A limitation of the study is that a relatively small number of cycles were applied. While this has been shown by previous studies to be adequate to describe initial relative motions further work should be conducted to investigate if these trends apply to long-term loosening behaviour of the implants
Introduction
There is a general consensus among orthopaedic surgeons that stemmed tibial and femoral components are required to obtain initial mechanical stability when there is deficient metaphyseal bone.1,2 However, no consensus exists regarding the appropriate selection of stem size, length or method of fixation. Surgeons choose between cemented fixation, cementless fixation and “hybrid” fixation, comprising a cementless stem coupled with a cemented metaphyseal component. One recent review of the current literature of long-term clinical outcomes did not demonstrate sufficient evidence to recommend one method over the other.3
Relatively few studies have been conducted on the distal femur.2,4-7 Studies that have focused on the distal femur have often been limited to loading in extension.2,4 Wackerhagen et al5 investigated motion of the femoral component through the use of a custom-built dynamic knee rig, capable of flexion angles between 0° and 90°. Later work by Cristofolini et al6,7 employed a modified simulator of knee wear in order to investigate the long-term loosening behaviour of both cobalt–chromium and ceramic primary knee implants, with loading based on the International Organization for Standardization ISO 14243-1 and ISO 14243-3 testing regimes.8,9 These studies investigated motion of the femoral component along only a few degrees of freedom (typically anteroposterior translation and rotation in the sagittal plane), which were recorded at the bone–implant interface, and the type of implant was limited to primary stemless prostheses.5-7
The aim of this laboratory study was to investigate the influence of stem length on the overall pattern and level of relative motions, at a range of flexion angles, for both cemented and uncemented total knee prostheses.
Materials and Methods
Test rig design
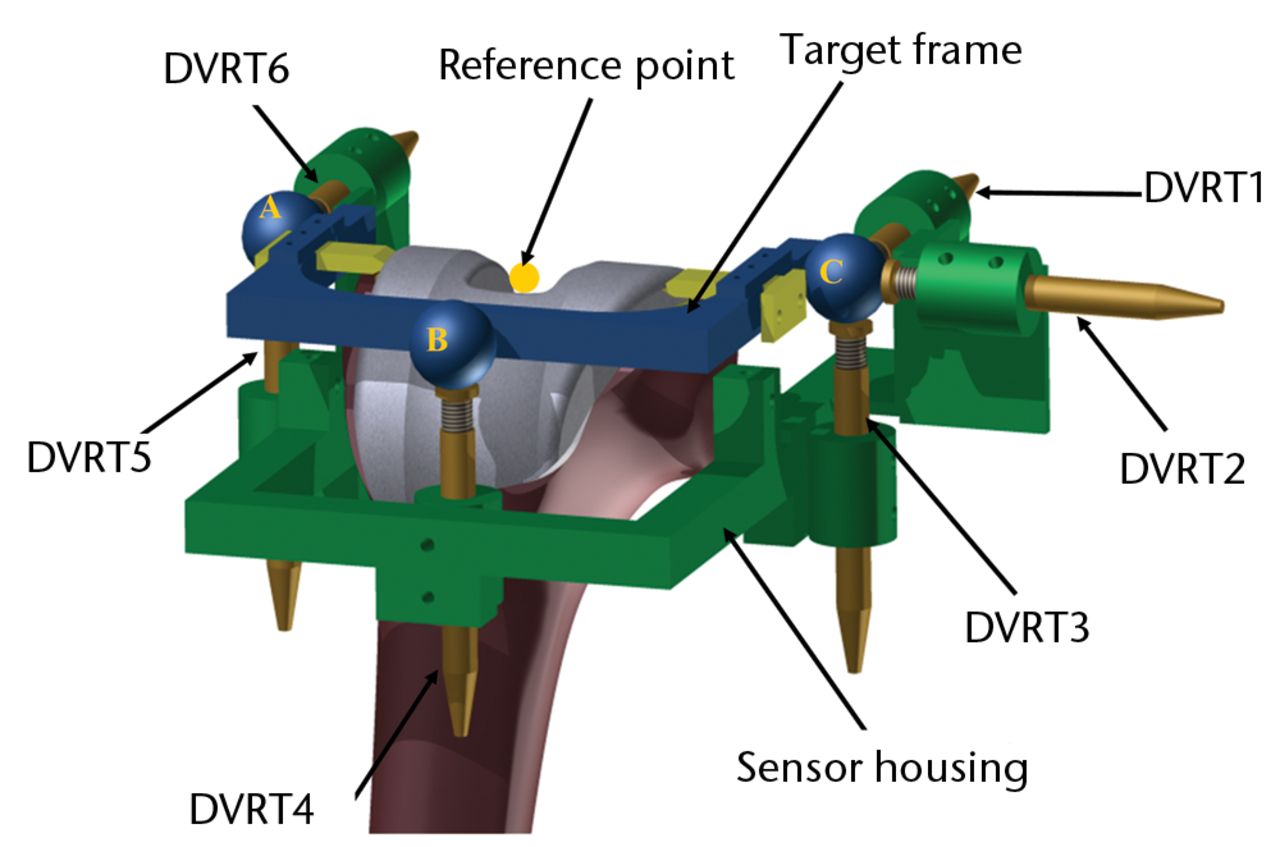
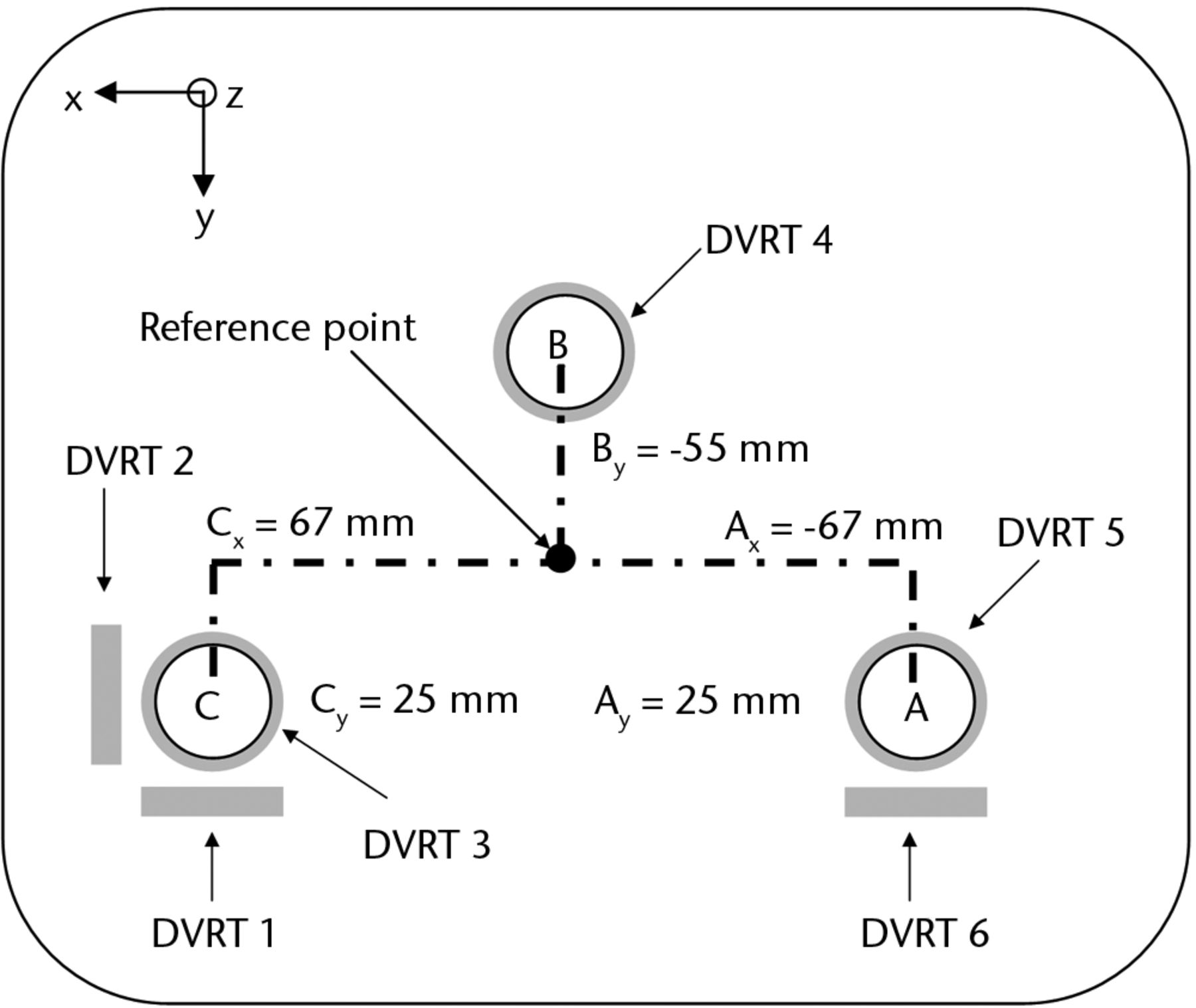
A custom test rig was developed based on concepts similar to those employed by experimental studies on hip implant migration.10,11 It comprises two structures: the sensor housing attached to the bone and the target frame attached to the implant (Fig. 1a). Six differential variable reluctance transducers (DVRTs; Microstrain Inc., Williston, Vermont) were attached to the sensor housing in the following arrangement (Fig. 1): DVRT 3, 4 and 5 were positioned to record displacement in the distal/proximal (z) direction; DVRT 1 and 6 in the anterior/posterior (y) direction; and DVRT 2 in the medial/lateral (x) direction. The target frame consisted of three large spheres attached to a stiff frame; sphere A was offset in the posterior-lateral direction, sphere C in the posteromedial direction and sphere B in the anterior direction relative to the implant reference point, as shown in Figure 1b. These spheres acted as ‘targets’ for each of the DVRT sensors and were attached rigidly to the target frame, which in turn was connected to the implant through two adjustable wedges machined to provide an interference fit between the frame and the tool grooves of the implant. Once the target frame was fixed to the implant, the sensor housing was then positioned as close as possible to the distal surface and secured through the use of three adjustable screws. Fine adjustment of the DVRTs was then carried out to ensure that the flat surface of each sensor was orthogonal to and in direct contact with one of the three target spheres.
Femur preparation protocol
This study used fourth-generation composite femurs (Sawbones; Pacific Research Laboratories, Vashon, Washington). This human bone analogue has been widely used to assess stability of stemmed femoral components used in total hip replacement.12-14 A number of studies have shown the composite femur to be a suitable substitute that replicates the strength and material properties of bone adequately while permitting higher levels of repeatability than their biological equivalent for smaller sample sizes due to the standardised nature of their geometry.15 Three different femoral components were investigated in this study; a posterior-stabilising (PS), a total-stabilising (TS) implant with short stem (12 mm × 50 mm) and a TS implant with long offset stem (19 mm × 150 mm stem with 4 mm lateral offset), all from the Triathlon series (Stryker, Newbury, United Kingdom) (Fig. 2). Due to the design of the implant system used in this study and geometry of the composite bone, a 4 mm lateral offset was necessary to allow the long-stemmed implant to be implanted into the femoral canal, as is often the case clinically.16,17
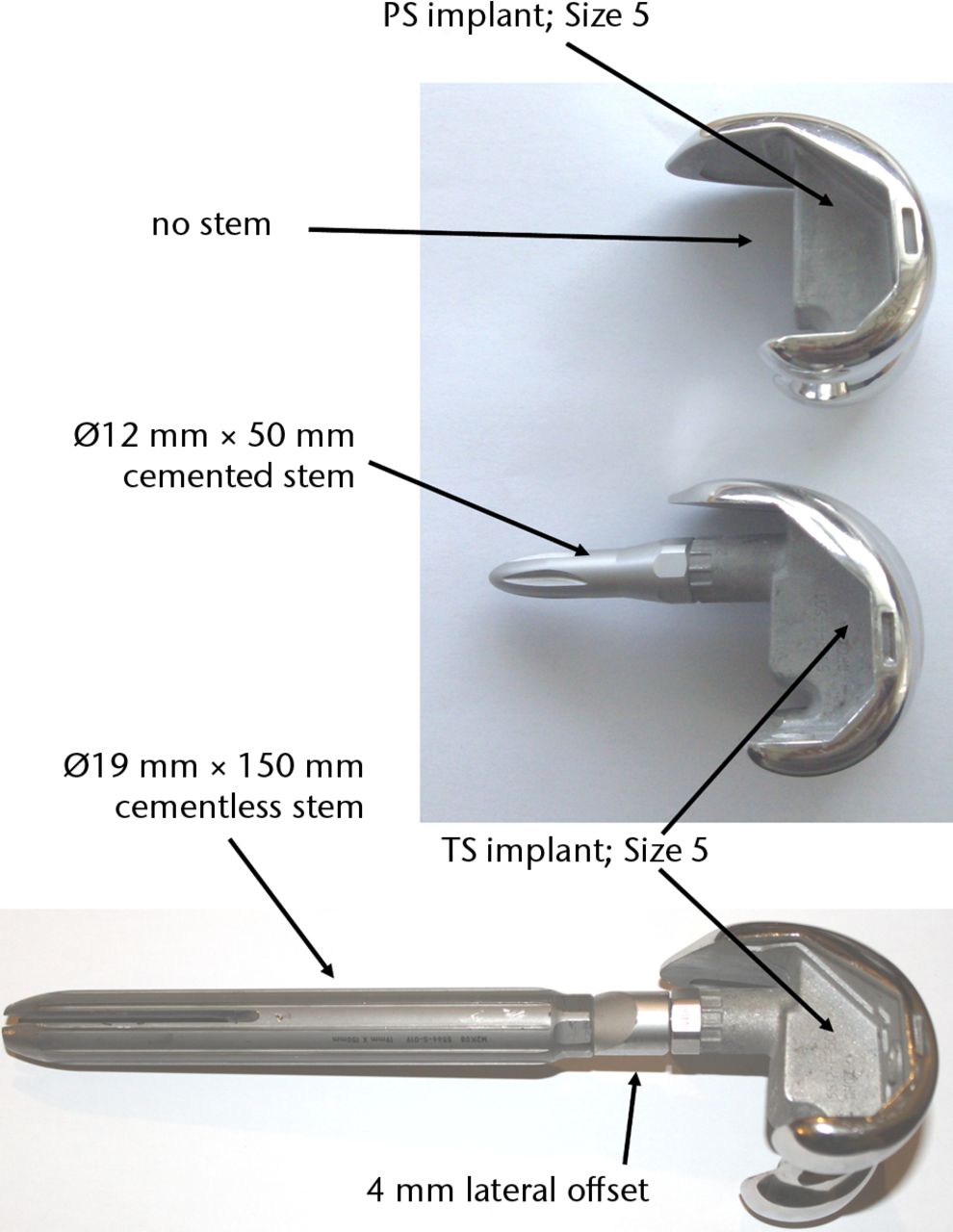
Fig. 2
Photographs of the implants investigated, showing a posterior-stabilised (PS) implant (top row), a total-stabilised (TS) implant with short stem (middle row) and a TS implant with long offset stem (bottom row).
Tests were divided into two main groups as listed in Table I. The first group consisted of all components implanted into the femur without cement. In the second group (cemented) PS implants were cemented at the metaphysis. TS short stemmed implants were cemented both distally and up past the stem to the cement restrictor (Hardinge; DePuy, Leeds, United Kingdom). Long-stemmed TS implants employed a “hybrid” cementing technique, with cement on the metaphysis only. All femoral component implantation and cementing was carried out by a qualified and experienced orthopaedic surgeon (HG) in accordance with each implant’s surgical protocol using the appropriate cutting guides and instrumentation (Triathlon TS, System 5; Stryker). The cement was mixed in a standardised manner using a Mixevac (Stryker) in a constant temperature fume-cupboard. A timer was used to ensure cementing and component impaction was performed with the cement at the same viscosity for all samples.
Table I
Outline of experimental test groups
| Group 1 | Group 2 | |
|---|---|---|
| Posterior-stabilised implant | Uncemented | Cemented |
| Total-stabilised short-stem | Uncemented | Cemented (pressurised) |
| Total-stabilised long offset stem | Uncemented | Hybrid cemented (implant cemented distally, stem remains uncemented) |
Experimental loading protocol
The bone was secured in a custom holder, which permitted variation in bone orientation from 0° to 90°. However, we were unable to carry out tests at angles ≥ 30° flexion (as is discussed later). Once fixed at the desired angle, a cyclical load was applied through a matching tibial component using a Zwick–Roell testing machine (Zwick, Ulm, Germany). Loading was based on three peaks of 728.5 N, 1186 N and 1643 N corresponding to 0°, 10° and 20° flexion during the stance phase of gait from a normal walking cycle for an assumed body weight of 775 N.18 During the test the load was applied at a constant rate of 42 N/s up to the maximum indicated for each step, the maximum load was applied for 10 seconds after which it was reduced back to a reference load of 20 N (to maintain contact) for a further 10 seconds. Each test consisted of 40 cycles at each of the three flexion angles investigated. Previous studies have shown that a stabilised value of relative motions of uncemented implants can be determined within relatively few cycles of load application.19
Data acquisition was carried out using a National Instruments DAQpad-6070E and virtual instrumentation software LabView 7.0 (both National Instruments, Austin, Texas). For each test the signal was logged at a rate of 10 samples per second. This signal was then converted from voltage to microns using each individual DVRT sensors’ calibration curves and filtered using a third-order Butterworth filter to reduce noise. This gave a displacement curve for each sensor that varied over time corresponding to the loading and unloading of the femoral component. A custom program was developed in LabView that extracted the amplitude of each sensor’s displacement curve at one-cycle intervals over the entire 40 cycles of load application; this gave the values of inducible displacement due to loading for each sensor over the test period.
Relative motion evaluation
Coordinate transformation theory for small angles10 was then applied to allow the displacements (u, v, w) and rotations (θx, θy, θz) of the femoral component relative to the bone to be determined for a fixed reference point (Fig. 1). If Uc, Vc and Wc are the displacements measured by DVRT 2, DVRT 1 and DVRT 3, respectively; Va and Wa are the displacements measured by DVRT 6 and DVRT 5, respectively; and Wb is the displacement measured by DVRT 4; then the equations can be represented as given in Figure 3.
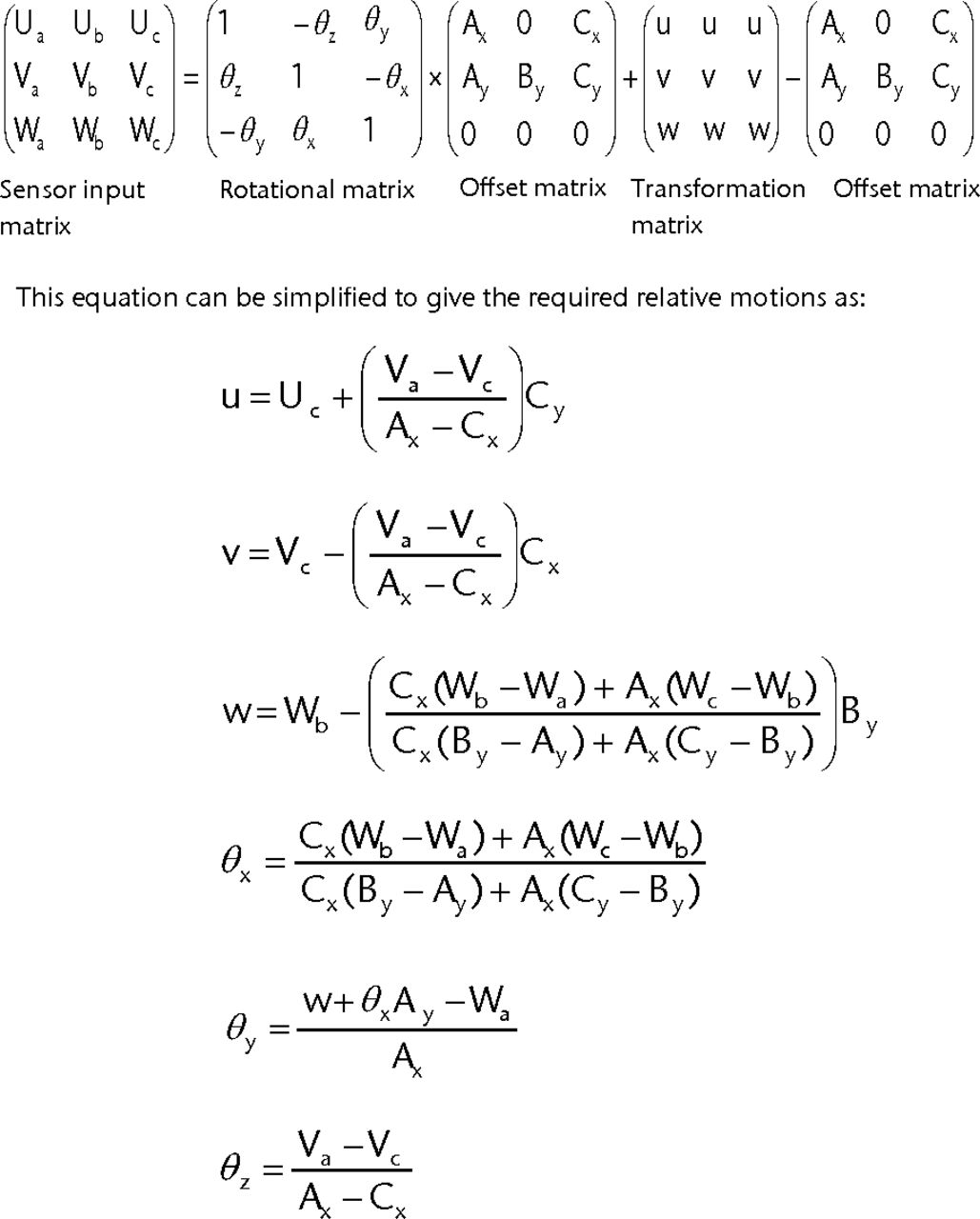
Fig. 3
Equations used to determine the relative motion of the implant reference point based on individual sensor displacements.
The terms Ax, Ay, By, Cx and Cy represent the distance each target sphere is offset from the reference point, as shown in Figure 1b.
Results
Mean translational and rotational relative motions are shown in Figure 4. Numerical values along with standard deviation (sd) are presented in Tables II and III.
Table II
Mean translational and rotational relative motions for uncemented cases
| Mean (sd) motion | |||
|---|---|---|---|
| Relative motion | Posterior-stabilised | Total-stabilised (short) | Total-stabilised (long) |
| u (µm) | |||
| Flexion 0° | 16 (0.71) | 16 (0.45) | 3 (0.57) |
| Flexion 10° | 34 (1.07) | 35 (0.59) | 4 (0.46) |
| Flexion 20° | 48 (4.85) | 49 (1.13) | 7 (0.76) |
| θx (°) | |||
| Flexion 0° | 38.34E-03 (2.69E-03) | -59.22E-03 (3.12E-03) | 6.29E-03 (0.63E-03) |
| Flexion 10° | 56.52E-03 (1.79E-03) | 3.88E-03 (1.59E-03) | 11.53E-03 (0.45E-03) |
| Flexion 20° | 84.15E-03 (24.33E-03) | 22.90E-03 (8.77E-03) | 20.19E-03 (0.99E-03) |
| v (µm) | |||
| Flexion 0° | 36 (1.04) | 6 (0.57) | 16 (0.88) |
| Flexion 10° | 53 (0.79) | 17 (1.04) | 9 (0.73) |
| Flexion 20° | 44 (10.73) | 38 (1.62) | 16 (0.22) |
| θy (°) | |||
| Flexion 0° | -52.07E-03 (1.65E-03) | 19.44E-03 (0.82E-03) | -14.86E-03 (0.79E-03) |
| Flexion 10° | -7.40E-03 (2.41E-03) | 47.03E-03 (1.37E-03) | 10.82E-03 (0.30E-03) |
| Flexion 20° | 0.47E-03 (25.57E-03) | 56.46E-03 (0.98E-03) | 8.12E-03 (0.59E-03) |
| w (µm) | |||
| Flexion 0° | 65 (1.34) | 67 (1.69) | 28 (1.13) |
| Flexion 10° | 110 (1.53) | 103 (2.06) | 39 (0.37) |
| Flexion 20° | 145 (24.60) | 134 (4.46) | 54 (0.68) |
| θz (°) | |||
| Flexion 0° | -11.83E-03 (0.61E-03) | -3.56E-03 (0.25E-03) | 1.28E-03 (0.49E-03) |
| Flexion 10° | -1.83E-03 (1.65E-03) | 3.44E-03 (0.45E-03) | 3.57E-03 (0.42E-03) |
| Flexion 20° | -15.06E-03 (12.12E-03) | -9.54E-03 (2.58E-03) | 0.17E-03 (0.61E-03) |
Table III
Mean translational and rotational relative motions for cemented cases
| Mean (sd) motion | |||
|---|---|---|---|
| Relative motion | Posterior-stabilised | Total-stabilised (short) | Total-stabilised (long) |
| u (µm) | |||
| Flexion 0° | 12 (1.14) | 4 (1.42) | 8 (4.07) |
| Flexion 10° | 26 (0.71) | 4 (1.35) | -0.13 (0.65) |
| Flexion 20° | 32 (0.75) | 6 (1.47) | 0.40 (0.83) |
| θx (°) | |||
| Flexion 0° | 6.25E-03 (0.92E-03) | -11.44E-03 (0.67E-03) | 5.36E-03 (1.30E-03) |
| Flexion 10° | 21.79E-03 (0.67E-03) | 5.27E-03 (0.63E-03) | 10.53E-03 (0.62E-03) |
| Flexion 20° | 39.83E-03 (0.70E-03) | 17.79E-03 (0.57E-03) | 9.04E-03 (0.40E-03) |
| v (µm) | |||
| Flexion 0° | 5 (0.24) | 3 (0.37) | 7 (0.94) |
| Flexion 10° | 14 (0.24) | 6 (0.60) | 9 (0.19) |
| Flexion 20° | 17 (0.56) | 11 (0.97) | 13 (1.54) |
| θy (°) | |||
| Flexion 0° | 13.20E-03 (0.38E-03) | 5.08E-03 (0.65E-03) | 8.44E-03 (0.29E-03) |
| Flexion 10° | 7.11E-03 (0.35E-03) | 16.67E-03 (0.36E-03) | 12.97E-03 (0.40E-03) |
| Flexion 20° | 18.15E-03 (0.25E-03) | 27.25E-03 (0.63E-03) | 11.77E-03 (0.24E-03) |
| w (µm) | |||
| Flexion 0° | 26 (0.67) | 13 (0.41) | 12 (0.47) |
| Flexion 10° | 30 (0.28) | 26 (0.30) | 14 (0.26) |
| Flexion 20° | 45 (0.49) | 30 (0.33) | 15 (0.25) |
| θz (°) | |||
| Flexion 0° | -1.59E-03 (0.25E-03) | -0.35E-03 (0.38E-03) | -2.93E-03 (0.67E-03) |
| Flexion 10° | 3.46E-03 (0.27E-03) | -0.68E-03 (0.49E-03) | -6.48E-03 (0.15E-03) |
| Flexion 20° | 4.44E-03 (0.30E-03) | -1.45E-03 (0.77E-03) | -7.88E-03 (1.33E-03) |
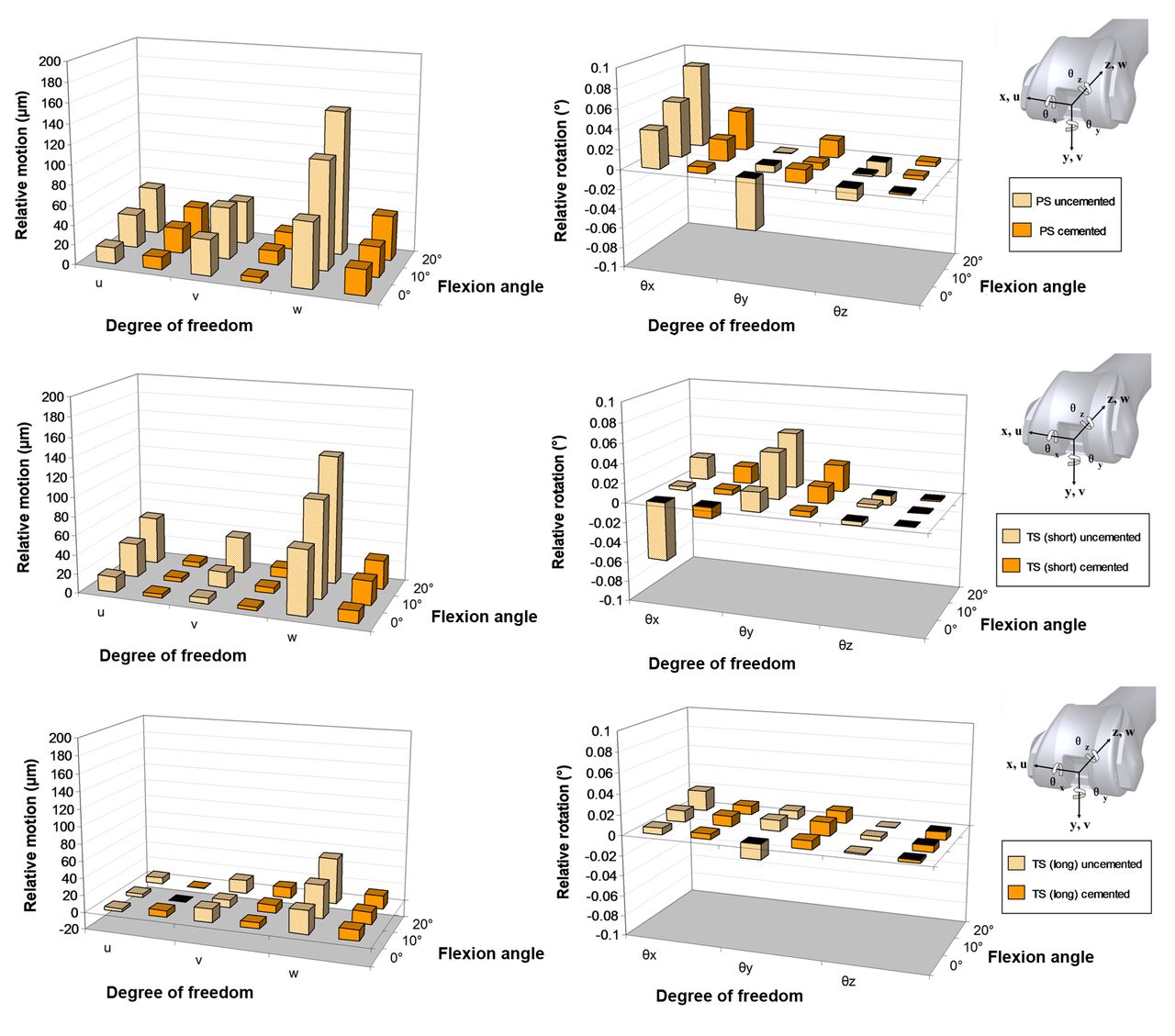
Fig. 4
Diagrams showing the comparison of translational (first column) and rotational (second column) relative motions for: a posterior-stabilised (PS) implanted femur (top row), a total-stabilised (TS) implanted femur with a short stem (middle row) and a TS implanted femur with a long offset stem (bottom row) for both cemented and uncemented cases. Where u, v and w are relative translational motions in the directions of x, y and z, respectively, and θx, θy and θz are relative rotations about the axes of x, y and z, respectively.
All translational relative motions generally increase with flexion angle (Fig. 4; left column). The largest motions occurred in the z direction (distal/proximal) for all three flexion angles of loading. It can be seen that the addition of a short stem (Fig. 4; middle row) for both cemented and uncemented cases leads to a reduction in translational motions compared with PS implants with no stem (Fig. 4; top row). The cemented short stem led to smaller relative motions in comparison with the cemented PS implants with no stem. The TS implant with long stem (Fig. 4; bottom row) shows significantly reduced motions in comparison with both of the other two implants. The translational relative motions reduce with cementing, as expected, in almost all cases.
The trends with respect to relative rotations are considerably more complex (Fig. 4; right column). The largest relative rotations are found to occur with the uncemented PS implant. For long-stem cases the relative rotations can be seen to be extremely small in comparison with both of the other two implants. Cementing is found to reduce relative rotations. The component of relative rotations found to be the smallest in general was rotation in the transverse plane (θz).
Discussion
We measured relative motion along all six degrees of freedom for femoral components. However, previous studies on femoral component relative motion can provide cross validation where components of motion measured in the current study are similar to those recorded by previous studies. The mean inducible displacements in the direction of the long axis of the femur as reported by Cristofolini et al6 are comparable with those recorded by DVRTs 3, 4 and 5 in this study. Furthermore, the range of inducible relative motion found in this study for both cemented (0 µm to 45 µm) and uncemented (4 µm to 145 µm) are similar to the range of relative motions reported previously by Wackerhagen et al5 (14 µm to 250 µm) and Cristofolini et al6 (9 µm to 130 µm).
The overall magnitude of relative motions for each of the uncemented and cemented implant cases were plotted in a single figure (Fig. 5). This shows an overall increasing trend of motion with flexion angle for all implants tested. It can also be seen that the addition of a stem serves to reduce the levels of femoral component relative motion, with the long offset stem exhibiting the lowest relative motion. The difference in implants is particularly noticeable in flexion.
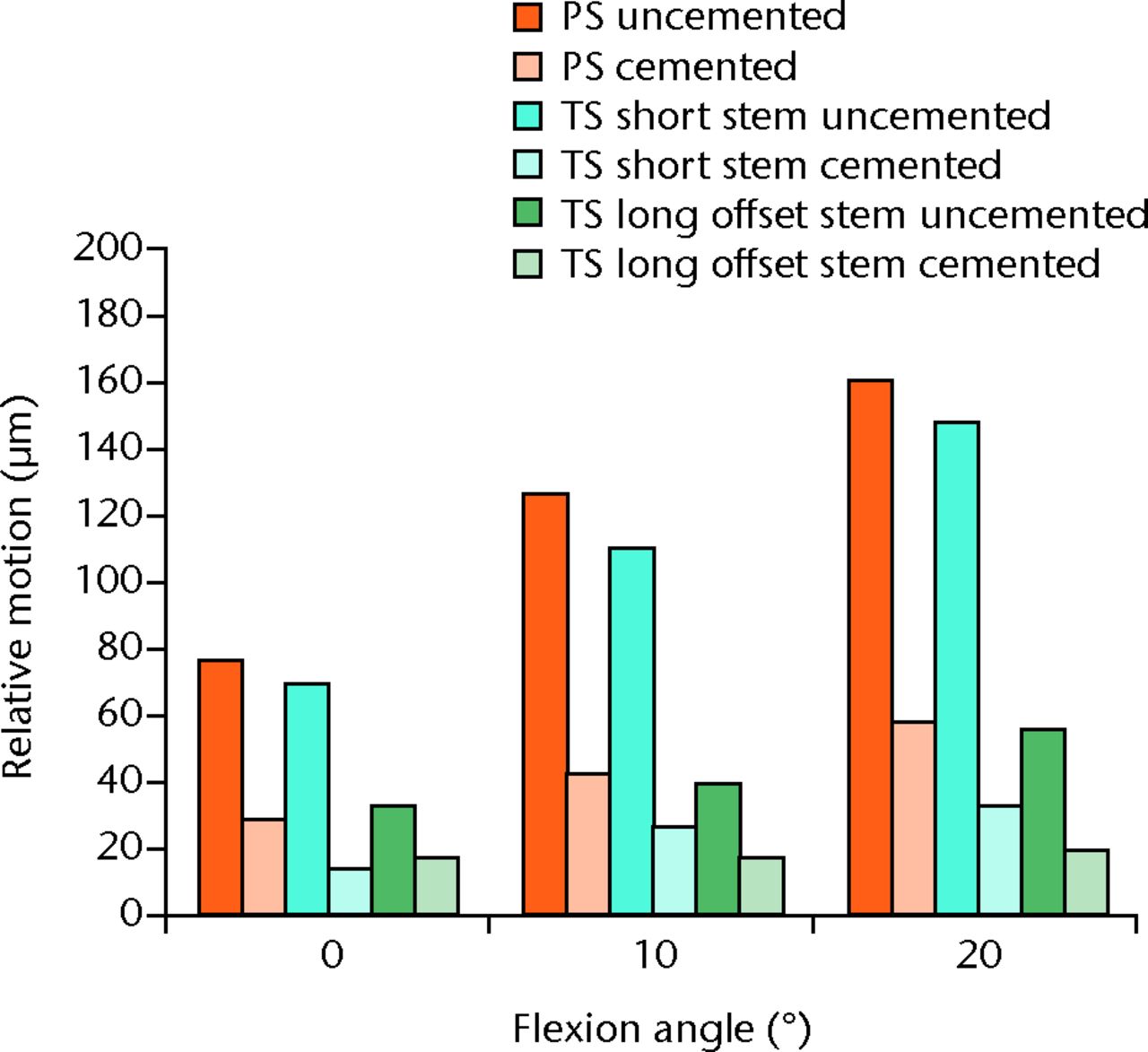
Fig. 5
Bar chart showing the overall magnitude of relative motions for the three flexion angles investigated for cemented and uncemented implants (PS, posterior-stabilised; TS, total-stabilised)..
Once cemented, relative motions were found to reduce to approximately one-third of their uncemented levels; these findings are within the range reported by a previous cemented study on cadaveric bone.5 It can also be observed from Figure 5 that PS implants, once cemented, exhibit similar levels of relative motion to uncemented TS implants with long offset stem. TS implants with a short cemented stem were found to have comparable relative motions to the hybrid cemented long stemmed implants. Again as with the uncemented tests the long offset stem was seen to result in the lowest relative motion.
Previous biomechanical studies have been performed to analyse primary stability and shear forces for the various fixation techniques using both cadaveric simulation and finite element analysis.20-22 These studies have largely been performed upon the tibia and tibial components. Unlike the tibia, the contact area and direction of loading across the distal femur changes significantly with flexion and extension of the knee during the gait cycle. In the present study it was observed that micromotion increased with increasing flexion angle for all components and fixation methods. This highlights the complexity of the distal femur, and that simulation or analysis in the anatomical position of extension does not accurately reflect the conditions for the majority of gait cycle and may lead to an overestimation of component stability.
In revision knee replacement, stems transfer load from the metaphysis to the diaphysis. The use of longer stems increases surgical complexity and raises the concern of metaphyseal stress-shielding and resultant fractures in the long-term. Stem size, offset adaptors, stress shielding and the presence of either cement or bony on-growth can also complicate further revision surgery. Beckmann et al3 recently published a review of the literature on revision knee replacement fixation. It was indicated that the majority of recent research has dealt with the comparison of hybrid and cemented fixation, reporting comparable rates of loosening and clinical outcomes for both methods.3 Fewer studies were available for cementless fixation. Overall the authors of the review could not make a final statement recommending one form of fixation over the other, based on clinical outcome studies in the current literature.
The present study suggests that in uncemented reconstructions, stemmed implants perform better than stemless implants, with the long offset stem seen to provide the greatest resistance to relative motion. However, once cemented, all implants with and without stems had comparable levels of relative motion. These findings indicate that the use of stems provides no obvious advantage for cemented implants unless there is a need to bypass a condylar defect. For the implants used in this study (PS or TS design) the central box housing can be regarded as a short stem in engineering terms. In situations where stems are necessary, metaphyseal defects requiring augments, these findings support the use of a short cemented stem, which has been shown in this study to provide comparable results to long offset stems (cemented and uncemented). Recent finite element studies also support the use of short stems due to their more favourable pattern of stress distally in comparison with long stems, which leads to less severe instances of stress shielding over time.23 Another key practical factor is the relative ease of insertion when using short stems. In comparison, fitting of a long stem can be complicated by the natural AP bow in the femur, variations in the valgus angle, distal metaphyseal anatomical variants and other conditions that may affect the geometry of the shaft.
There are a number of limitations in our study. We only investigated three flexion angles in a walking gait cycle (0°, 10° and 20°). Depending on the activity, higher flexion angles are present during gait, and following the observed trends one would expect even greater relative motions at higher flexion angles, such as those occurring during stair climbing or rising from a chair. The current test rig was designed to allow flexion angles from 0° to 90° to be investigated. In practice, due to the large bending moment introduced at higher flexion angles (≥ 30°) and the absence of ligaments or muscles to redistribute the load and protect the bone, the results became heavily influenced by deformation, in one instance leading the test specimen to fracture in the bone holder. This study does not measure the true levels of motion at the interface; it instead measures motion of the implant relative to the point of fixation of the DVRT rig to the bone. While every effort was taken to minimise the distance of the attachment site to the bone-implant interface, it must be accepted that experimental values measured will therefore include other aspects, such as deformation of the bone. This combined motion deformation may result in experimental values overestimating the level of motion at the interface. This has been a common issue in other studies of this nature.6,7,11,13 Relatively few loading cycles (n = 40) were carried out during each test. While a small number of cycles have been shown to be adequate for determining the loosening behaviour of uncemented components,19 cemented components have been seen to fail only after millions of cycles. Due to the comparative nature of this work (cemented versus uncemented) we believe that the behaviour observed in these short-term findings is a good predictor of possible long-term results, although further testing for a greater number of cycles may be necessary to verify if the short-term behaviour observed in the current study applies to long-term scenarios.
Conclusions
Testing interface motion in extension only can provide misleading results; future laboratory testing should be carried out in flexion. Cemented constructs provide more initial stability than equivalent uncemented constructs, and cemented short stems provide as much stability as long uncemented stems.
Support from the Lothian University Hospitals NHS Trust Brown and Ireland Estates Fund and The University of Edinburgh is gratefully acknowledged. The authors would also like to acknowledge Stryker UK for providing the implants and surgical instruments used in this study, although they had no part in the conception, analysis or reporting of results.
1 Whittaker JP , DharmarajanR, TomsAD. The management of bone loss in revision total knee replacement. J Bone Joint Surg [Br]2008;90-B:981–987.CrossrefPubMed Google Scholar
2 van Loon CJ , KyriazopoulosA, VerdonschotN, et al.The role of femoral stem extension in total knee arthroplasty. Clin Orthop Relat Res2000;378:282–289.CrossrefPubMed Google Scholar
3 Beckmann J , LüringC, SpringorumR, et al.Fixation of revision TKA: a review of the literature. Knee Surg Sports Traumatol Arthrosc2011;19:872–879.CrossrefPubMed Google Scholar
4 Completo A , FonsecaF, SimõesJA. Experimental validation of intact and implanted distal femur finite element models. J Biomechanics2007;40:2467–2476.CrossrefPubMed Google Scholar
5 Wackerhagen A , BodemF, HopfC. The effect of cement fixation on initial micromotion of the femoral component in condylar knee replacement. Int Orthop1992;16:25–28.CrossrefPubMed Google Scholar
6 Cristofolini L , AffatatoS, EraniP, et al.Long-term implant-bone fixation of the femoral component in total knee replacement. Proc Inst Mech Eng H 2008;222:319–331.CrossrefPubMed Google Scholar
7 Cristofolini L , AffatatoS, EraniP, TiganiD, VicecontiM. Implant fixation in knee replacement: preliminary in vitro comparison of ceramic and metal cemented femoral components. Knee2009;16:101–108.CrossrefPubMed Google Scholar
8 International Organization for Standardization (ISO). ISO 14243-1, 2009. Implants for surgery: wear of total knee-joint prostheses: Part 1: loading and displacement parameters for wear-testing machines with load control and corresponding environmental conditions for test. http://www.iso.org (date last accessed 25 September 2012). Google Scholar
9 International Organization for Standardization (ISO). ISO 14243-3, 2004. Implants for surgery: wear of total knee-joint prostheses: Part 3: loading and displacement parameters for wear-testing machines with displacement control and corresponding environmental conditions for test. http://www.iso.org (date last accessed 25 September 2012). Google Scholar
10 Maher SA , PrendergastPJ. Discriminating the loosening behaviour of cemented hip prosthesis using measurements of migration and inducible displacement. J Biomech2002;35:257–265. Google Scholar
11 Berzins A , SumnerDR, AndriacchiTP, GalanteJO. Stem curvature and load angle influence the initial relative bone-implant motion of cementless femoral stems. J Orthop Res1993;11:758–769.CrossrefPubMed Google Scholar
12 Cristofolini L , TeutonicoAS, MontiL, CappelloA, ToniA. Comparative in vitro study on the long term performance of cemented hip stems: validation of a protocol to discriminate between “good” and “bad” stem designs. J Biomech2003;36:1603–1615. Google Scholar
13 Britton JR , PrendergastPJ. Preclinical testing of femoral hip components: an experimental investigation with four prostheses. J Biomech Eng2005;127:872–880.CrossrefPubMed Google Scholar
14 Cristofolini L , SaponaraTA, SavigniP, EraniP, VicecontiM. Pre-clinical assessment of the long-term endurance of cemented hip stems: Part 1: effect of daily activities: a comparison of two load histories. Proc Inst Mech Eng H2007;221:569–584. Google Scholar
15 Cristofolini L , VicecontiM, CappelloA, ToniA. Mechanical validation of whole bone composite femur models. J Biomech1996;29:525–535.CrossrefPubMed Google Scholar
16 Fehring TK. Use of stems in revision total knee arthroplasty. In: Bono JV, Scott, RD, eds. Revision total knee arthroplasty. New York: Springer, 2005:137–144. Google Scholar
17 Brilhault JM , RiesMD. Influence of offset stem couplers in femoral revision knee arthroplasty: a radiographic study. Knee2012;19:112–115.CrossrefPubMed Google Scholar
18 Bergmann G, ed. Charite – Universitaetsmedizin Berlin (2008). Orthoload. http:// www.orthoload.com (date last accessed 10 January 2010). Google Scholar
19 Schneider E , KinastC, EulenbergerJ, et al.A comparative study of the initial stability of cementless hip prostheses. Clin Orthop Relat Res1989;248:200–209.PubMed Google Scholar
20 Jazrawi LM , BaiB, KummerFJ, HiebertR, StuchinSA. The effect of stem modularity and mode of fixation on tibial component stability in revision total knee arthroplasty. J Arthroplasty2001;16:759–767.CrossrefPubMed Google Scholar
21 Completo A , FonsecaF, SimõesJA. Strain shielding in proximal tibia of stemmed knee prosthesis: experimental study. J Biomech2008;41:560–566.CrossrefPubMed Google Scholar
22 Completo A , RegoA, FonsecaF, et al.Biomechanical evaluation of proximal tibia behaviour with the use of femoral stems in revision TKA: an in vitro and finite element analysis. Clin Biomech (Bristol, Avon)2010;25:159–165.CrossrefPubMed Google Scholar
23 van Lenthe GH , WillemsMM, VerdonschotN, de Waal MalefijtMC, HuiskesR. Stemmed femoral knee prostheses: effects of prosthetic design and fixation on bone loss. Acta Orthop Scand2002;73:630–637.CrossrefPubMed Google Scholar
Funding statement:
Funding was received from the Lothian University Hospitals NHS Trust Brown and Ireland Estates Fund and The University of Edinburgh. Stryker UK provided the implants and surgical instruments, although they had no part in the conception, analysis or reporting of results
Author contributions:
N. Conlisk: Writing the manuscript, Main author, Study design, Data collection and analysis
P. Pankaj: Writing the manuscript, Study design, Support and guidance during study
H. Gray: Writing the manuscript, Preparation and implantation of femora
C. R. Howie: Writing the manuscript, Study design, Support and guidance during study
ICMJE Conflict of Interest:
None declared
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.