Abstract
Femoroacetabular impingement (FAI) causes pain and chondrolabral damage via mechanical overload during movement of the hip. It is caused by many different types of pathoanatomy, including the cam ‘bump’, decreased head–neck offset, acetabular retroversion, global acetabular overcoverage, prominent anterior–inferior iliac spine, slipped capital femoral epiphysis, and the sequelae of childhood Perthes’ disease.
Both evolutionary and developmental factors may cause FAI. Prevalence studies show that anatomic variations that cause FAI are common in the asymptomatic population. Young athletes may be predisposed to FAI because of the stress on the physis during development. Other factors, including the soft tissues, may also influence symptoms and chondrolabral damage.
FAI and the resultant chondrolabral pathology are often treated arthroscopically. Although the results are favourable, morphologies can be complex, patient expectations are high and the surgery is challenging. The long-term outcomes of hip arthroscopy are still forthcoming and it is unknown if treatment of FAI will prevent arthrosis.
Femoroacetabular impingement (FAI) and the general area of hip preservation surgery are currently two of the hottest topics in orthopaedics. The idea that bone-on-bone contact during movement of the hip, or ‘impingement’, causes pain, restricted range of movement, and degeneration of the joint was anecdotally mentioned before Reinhold Ganz’s work describing FAI in 2003.1 In 1936 Smith-Petersen2 described acetabular rim trimming and femoral neck osteoplasty for impingement of the acetabular rim on the femoral head or neck for cases of protrusio, healed slipped capital femoral epiphysis (SCFE) and osteoarthritis. Other authors recognised that impingement could occur secondary to healed SCFE and advocated osteoplasty of the femoral neck to alleviate pain and improve range of movement.3 However, it was Ganz et al4 in 1991 who began to resurrect these ideas, describing FAI occurring secondary to other hip pathology. In the decade that followed, the Bern group described impingement from callus formation or malunion after femoral neck fractures,4,5 impingement following periacetabular osteotomy6-10 and FAI as a cause of chondrolysis after healed SCFE.11,12 The description of a safe technique for surgical dislocation of the hip13 and MRI studies describing the alpha angle and decreased head-neck offset as potential causes of idiopathic impingement14,15 were also published prior to 2003, laying the foundation for this concept and its treatment.
The article published by Ganz et al1 in 2003 is widely cited by other authors as the introduction of the concept of FAI, and is now nearly ten years old. This article was the first conceptual description of FAI, and the first to propose FAI as a primary cause of idiopathic hip arthrosis. These ideas were substantiated by clinical and intra-operative observations made in a series of over 200 patients who underwent surgical hip dislocation for impingement.1 Although the ideal reason to treat FAI is to prevent further chondrolabral damage and future osteoarthrosis, the more immediate goals of treatment are to relieve pain, improve range of movement and allow a return to previous activity.
When considering the mechanical causes of hip pain, it is important to recognise that chondrolabral damage and arthrosis can be caused by static overload, dynamic motion, or both. Static overload of the cartilage and labrum most commonly occurs in the setting of dysplasia,16-18 but more recently has also been proposed as a cause of pain for patients with valgus neck-shaft angles.19 Intra-articular damage occurring as a result of hip motion – dynamic mechanical arthrosis – can be due to impingement or from motion-induced instability, similar to that occuring when impingement on the acetabular rim induces levering of the femoral head.1,20-24
There are two distinct mechanical types of impingement.1 Cam impingement can also be described as an inclusion-type of injury,1,11,12 where a bony deformity at the femoral head–neck junction enters the joint when the hip flexes (Fig. 1).12,25-27 Pincer impingement can also be thought of as an impaction-type of injury1,11,12 and occurs as a result of global or focal acetabular overcoverage, causing the acetabular rim to contact (or impact) the femoral head, metaphysis, or neck when the hip flexes (Fig. 2).25,28 Impaction injury can also occur in the setting of a relatively normal acetabulum with a very large femoral head offset deformity, or a broad or short femoral neck.11,12 Although this particular point is somewhat controversial, symptomatic patients most commonly have features of both cam/inclusion and pincer/impaction injury.29-33 Thinking about FAI in terms of mechanical forms of injury allows for the recognition that variations in anatomy can cause impingement, including the cam ‘bump’,1,14,15,31 lack of head-neck offset,14 increased acetabular depth or protrusio deformity,1,2,22 acetabular retroversion,1,34-38 and, at the extremes of this spectrum, slipped capital femoral epiphysis (SCFE)11,12 and the sequelae of childhood Perthes’ disease.39 This also explains why FAI can occur after a periacetabular osteotomy. Even if the acetabular correction is appropriate, the anterior femoral head in the dysplastic hip is characteristically flat,8,40 with a lack of head-neck offset that results in impingement when the acetabulum is rotated into a more normal position.8 Finally, there is also the most recently recognised cause of pincer/impaction-type impingement: that which occurs when a prominent anterior-inferior iliac spine (AIIS) or sub-spine region impinges on the femoral neck in hip flexion.28
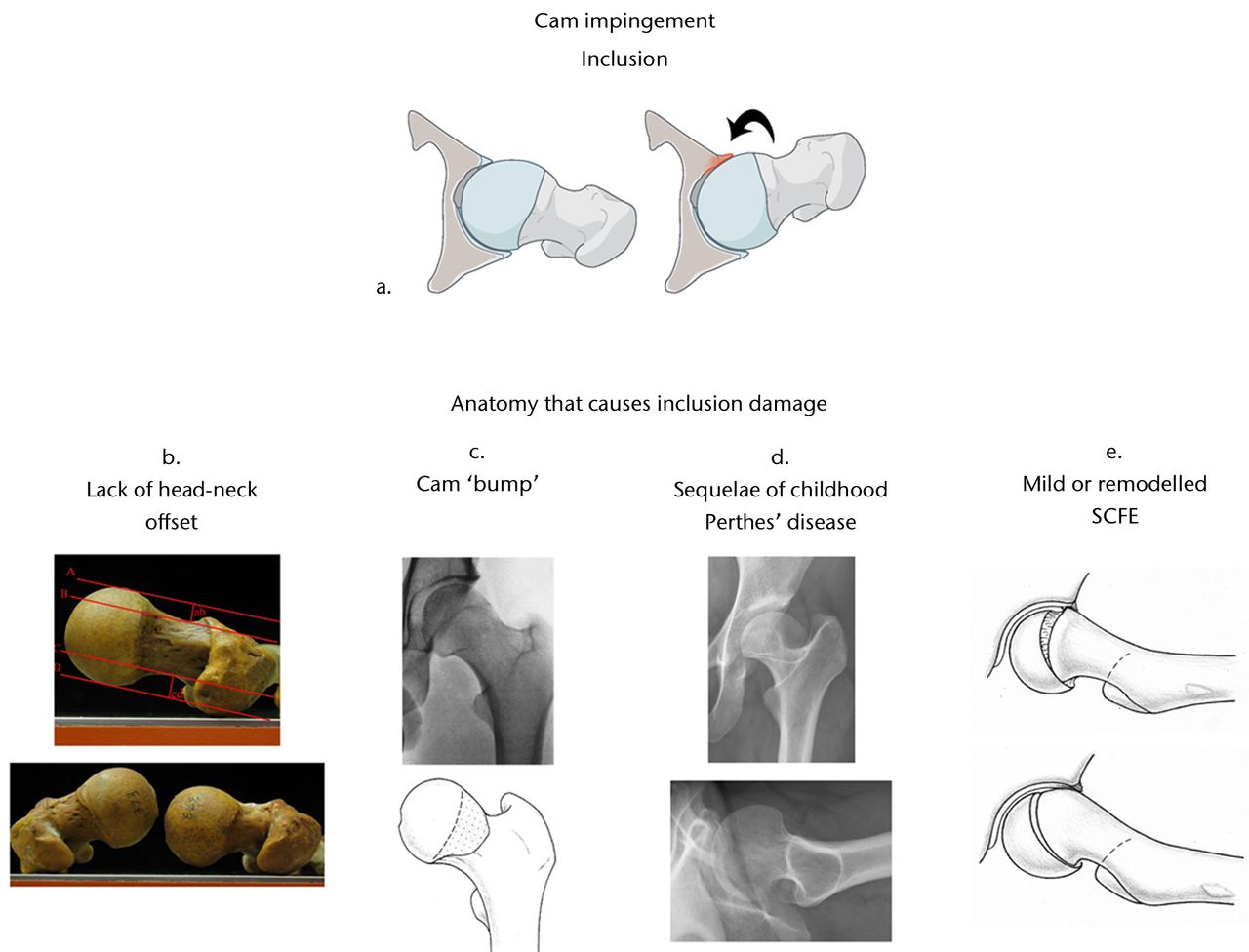
Fig. 1
Cam impingement creates an inclusion-type of injury (a).25 A bony deformity at the femoral head-neck junction enters the acetabulum in hip flexion (curved arrow). This causes delamination of the cartilage and separation at the chondrolabral junction. Many different types of deformities can cause cam impingement, including a lack of femoral head-neck offset (b),26 a cam ‘bump’ (c),27 childhood Perthes’ disease (d) and both mild and remodelled slipped capital femoral epiphysis (SCFE) (e)12 (Reprinted with permission: a) Leunig et al. Femoroacetabular impingement: diagnosis and management, including open surgical technique. Oper Tech Sports Med 2007;15:178–188. b) Toogood et al. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res 2009;467:876–885. c) Siebenrock et al. Abnormal extension of the femoral head as a cause of cam impingement. Clin Orthop Relat Res 2004;418:54–60. e) Leunig et al. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 2000;71:370–375).
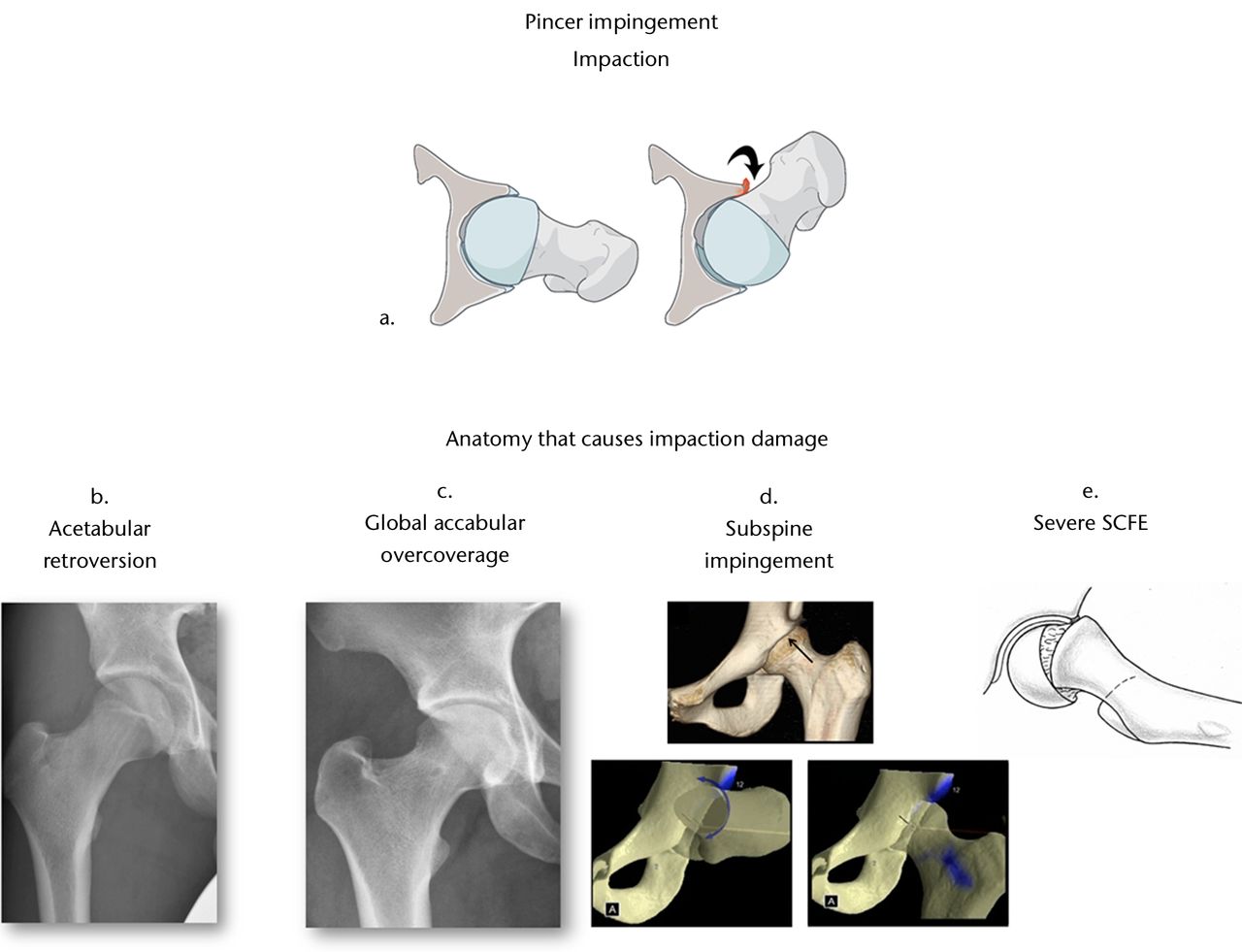
Fig. 2
Pincer impingement causes an impaction injury (a).25 Global or focal acetabular overcoverage causes the rim to contact the femoral head, metaphysis or neck when the hip is flexed (curved arrow). Anatomical deformities that can produce impaction-type injury include acetabular retroversion (b), global acetabular overcoverage (c), a large or prominent subspine (d)28 or severe slipped capital femoral epiphysis (SCFE) (e). (Reprinted with permission: a) Leunig et al. Femoroacetabular impingement: diagnosis and management, including open surgical technique. Oper Tech Sports Med 2007;15:178–188. d) Larson et al. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy 2011;27:1732–1737. e) Leunig et al. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand 2000;71:370–375).
Pathoanatomy
Evolutionary factors
Anthropological studies of the proximal femur give some clues as to the aetiology of the anatomy that causes impingement. In mammals, there are two distinct types of development and resulting shape of the proximal femur. When the femoral capital epiphysis is completely separate from the trochanteric apophysis, the femoral head is rounder and the neck is longer (Fig. 3).41 This is thought to be the result of an evolutionary need for more range of movement at the hip, and is the typical developmental pattern in the human hip.41,42 More commonly, however, the two physes are coalesced, resulting in a hip with a shorter, stouter neck and a smaller range of movement (Fig. 3).41 This type of hip has been called coxa recta, and is seen most commonly in ‘runners’; quadripeds that require a stable hip without a large range of movement (such as horses).43 The counterpart to the coxa recta is the coxa rotunda, which is a hip with a round femoral head, relatively long femoral neck and higher head-neck offset circumferentially. This is seen in animals that are ‘climbers’ or ‘swimmers’; species that need a greater range of movement but bear less weight through the hip (such as chimpanzees or gorillas). After studying the spectrum of mammalian pelvis anatomy, Hogervorst et al43 proposed that evolutionary forces – specifically the increase in the size of the human brain and the biomechanics necessary for upright ambulation – are responsible for the pathoanatomy that results in symptomatic FAI.43 In order to accommodate the increased size of the human brain, ‘obstetric selection’ occurred, resulting in enlargement of the birth canal and anteroposterior deepening of the human female pelvis (Fig. 4).43 The acetabular socket became deeper and closer to the centre of rotation in order to keep the lever arm of body weight at a favourable distance. This requires a rounder head due to the reciprocal development of the femoral head and acetabulum, but also decreases the required abductor force. Hogervorst et al43 also hypothesised that the shape of the human proximal femur evolved to fit the needs of a ‘running ape’: a sturdy hip with more limited range of movement, and some features of the coxa recta hip.43Corresponding to this, a study examining proximal femur morphology associated with cam impingement noted that femurs with the cam ‘bump’ also had shorter and thicker femoral necks than femurs with a normal alpha angle.44
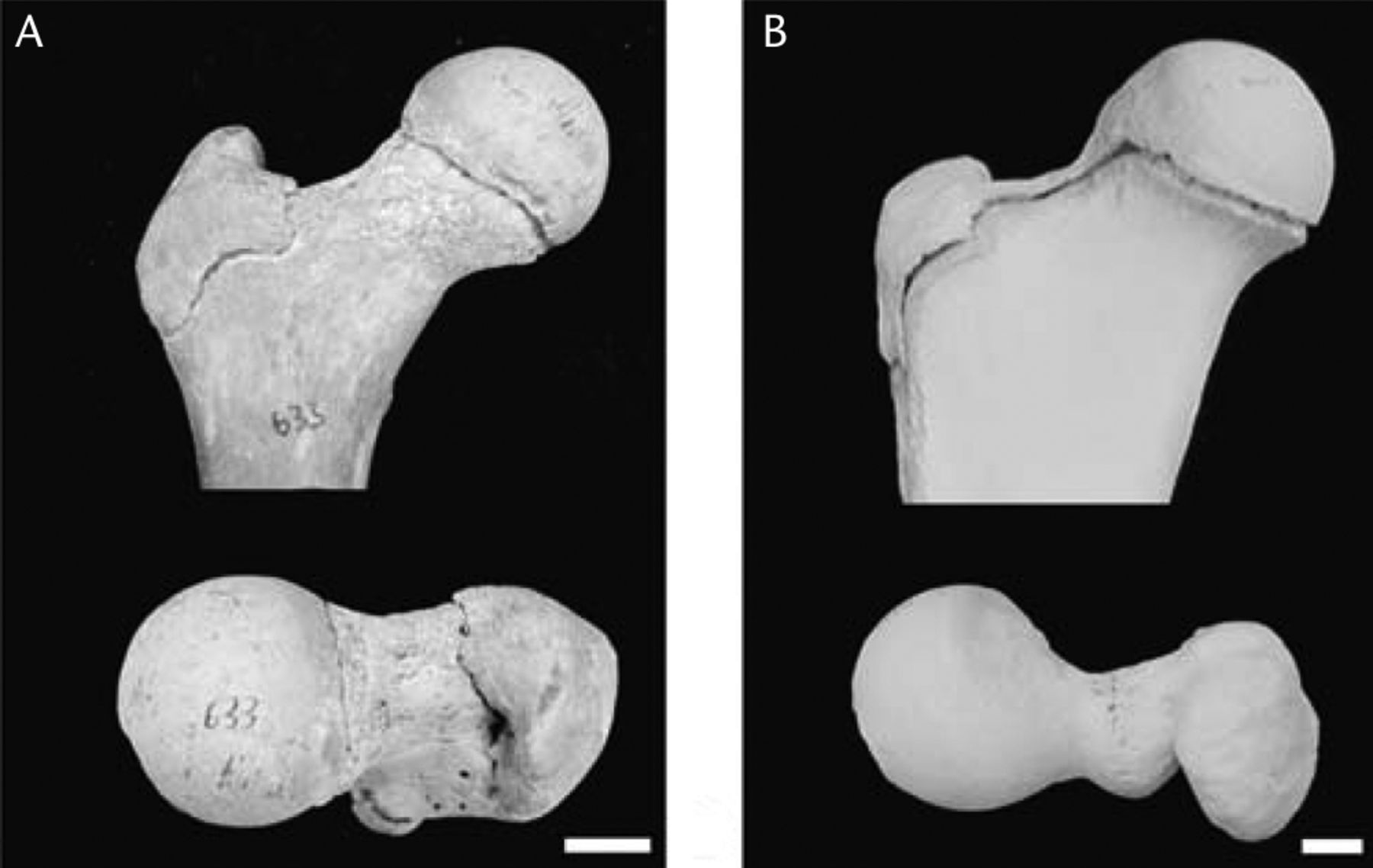
Fig. 3
Examples of separate and coalesced epiphyses during development of the proximal femur. At the end of growth, humans (A) have separation of the femoral capital epiphysis and the trochanteric apophysis, resulting in a rounder femoral head and longer femoral neck. Most quadripedal mammals (B) have coalescence at the proximal femur, resulting in a shorter, stouter femoral neck, which is more stable but with a smaller range of movement. (Reprinted with permission: Serrat et al. Variation in mammalian proximal femoral development: comparative analysis of two distinct ossification patterns. J Anat 2007;210:249–258).
![Fig. 4
Photographs and reconstructions showing
the evolution of the female pelvis, from the chimpanzee to man,
in anteroposterior (AP) (top row) and axial views (bottom row) From
left to right: chimpanzee, Ardipithecus ramidus (4.4
million years ago), Australopithecus afarensis (3.2
million years ago), Australopithecus africanus (2.7
million years ago), Homo erectus (1.5 million years
ago) and Homo sapiens. Scale is approximate. The
birth canal first widened transversely, but from Au. afarensis to H.
sapiens, the AP dimension deepened. (Reprinted with permission: Hogervorst
et al. Human hip impingement morphology: an evolutionary
explanation. J Bone Joint Surg [Br] 2011;93-B:769–776).](/api/asset/2046-3758.110.2000105/2000105-galleyfig4.jpeg)
Fig. 4
Photographs and reconstructions showing the evolution of the female pelvis, from the chimpanzee to man, in anteroposterior (AP) (top row) and axial views (bottom row) From left to right: chimpanzee, Ardipithecus ramidus (4.4 million years ago), Australopithecus afarensis (3.2 million years ago), Australopithecus africanus (2.7 million years ago), Homo erectus (1.5 million years ago) and Homo sapiens. Scale is approximate. The birth canal first widened transversely, but from Au. afarensis to H. sapiens, the AP dimension deepened. (Reprinted with permission: Hogervorst et al. Human hip impingement morphology: an evolutionary explanation. J Bone Joint Surg [Br] 2011;93-B:769–776).
Developmental influences
The most common deformity causing cam impingement, the cam ‘bump’, may result from an abnormal extension of the epiphysis onto the anterior or anterosuperior neck.27 Initially, the decreased head–neck offset and the cam deformity were thought to occur following a subclinical SCFE. However, the morphology of the proximal femur and the orientation of the physeal scar after a SCFE is substantially different from that occurring in idiopathic cam-type FAI.27,45 There is also evidence that, as the physis is closing, it extends further distally onto the femoral neck,45 supporting the hypothesis that the deformity is due to extension of the epiphysis. One study looked at the incidence of cam deformity in young male basketball players compared with non-athlete volunteers.46 The study included hips both before and after physeal closure, and specifically excluded control volunteers who participated in more than two hours of any vigorous activity per week. The basketball players with closed physes had larger mean alpha angles and a much higher incidence of cam deformity (89%) than the control population (9%).46 Thus, what remains hypothesised but as yet unproven, is that sports cause increased rotational or other mechanical stresses on the physis that are responsible for a change in the physeal growth or closure pattern, causing the stereotypical cam deformity. Specific patterns of physeal adaptation in response to repetitive sports during growth are well-recognised for the upper extremities. These adaptations can be beneficial; for example, asymmetric humeral and glenoid retroversion allowing baseball pitchers to have increased external rotation in the throwing arm.47,48 Alternatively, the load on the physis can cause significant problems, such as wrist pain and early physeal closure seen in many gymnasts.49 There is also good evidence that the relative position and growth of femoral capital epiphysis and trochanteric apophysis affects the shape and orientation of the proximal femur.50,51 The classic proximal femur shape that occurs as the sequelae of childhood Perthes’ disease is one example of this.50 In another example, bony bar formation between the two physes was observed to produce coxa valga with a horizontal physeal scar.51
Prevalence of FAI
The bony anatomy that causes FAI is quite common, and the prevalence depends on the population being studied (Table I).52-65 In asymptomatic young males recruited for the Swiss military, the overall prevalence of the cam deformity was 24%.58 When recruits with limited internal rotation were selected out of the larger cohort, 50% had a cam deformity visible on MRI.58 A different study of this same cohort found that cam deformities were associated with a two- to threefold relative risk of damage to the labrum and cartilage, depending on the lesion.59 Others have also observed that the cam deformity is quite common, with a prevalence of between 14% and 35% in asymptomatic populations, and occurring more frequently in male compared with female hips.53,54,56 When regarding anatomical variations that contribute to FAI (such as acetabular retroversion or overcoverage), 33% of females and 52% of males were found to have at least one factor predisposing them to FAI.55 There may be some genetic influence to this as well, with an increased incidence of cam and pincer morphology in siblings of patients with FAI, with respective relative risk rates of 2.8 and 2.0, respectively, compared with controls.57 In comparison, there is a much stronger genetic component to hip dysplasia, with the relative risk in first-degree relatives of patients with dysplasia ranging from 3 to 12.66
Table I
Prevalence of femoroacetabular impingement (FAI) in asymptomatic and symptomatic hips and those of athletes (AP, anteroposterior)
| Author/s | Population description | Cohort assessed | Imaging used | Major finding | |||
|---|---|---|---|---|---|---|---|
| Asymptomatic general population | |||||||
| Dudda et al52 | Elderly patients with non-arthritic hips (China and US) | 200 (400 hips) (all F) | Supine AP pelvis x-ray | Cam deformity found in 24% of US women and 7% of Chinese women. Pincer deformity (centre-edge angle > 35°) found in 46% of US women and 22% of Chinese women | |||
| Gosvig et al53 | Population-based (Denmark) | 3620 patients (1332M, 2288F) | Standing AP pelvis x-ray | Pistol grip found in 19.4% of male and 5.2% of female hips, deep socket found in 15.2% of male and 19.4% of female hips. Deformity was not predictive for groin pain but deep socket and pistol grip were risk factors for development of OA (relative risks 2.4 and 2.2, respectively) | |||
| Hack et al54 | Recruited volunteers (Canada) | 200 (400 hips) (89M, 111F) | MRI radial slice | 53% had an alpha angle > 50° at the 1:30 (anterosuperior) position. The mean alpha angle was greater in male hips | |||
| Kang et al55 | Patients having abdominal CT for trauma (New Zealand) | 50 (100 hips) | CT | At least one predisposing factor for FAI was found in 33% of female hips and 52% of male hips | |||
| Laborie et al56 | Population-based (Norway) | 2060 (874M, 1207F) | Standing AP pelvis, frog lateral x-ray | In males: 25% bilateral cam and 22% bilateral pincer. In females: 6% bilateral cam and 10% bilateral pincer | |||
| Pollard et al57 | Siblings of FAI patients vs control patients (UK) | 96 cases (54M, 42F) and 77 controls (39M, 38F) | Supine AP pelvis, cross-table lateral x-ray | Siblings of FAI patients have a risk ratio (RR) of 2.8 of having cam deformity, RR 2.0 of pincer deformity and RR 2.6 of bilateral deformity compared with controls | |||
| Reichenbach et al58 | Military recruits (Switzerland) | 244 (all M) | MRI | Cam deformity in 24%, increasing to 48% in hips with limited internal rotation | |||
| Reichenbach et al59 | Military recruits (Switzerland) | 244 (all M) | MRI | Cam deformity associated with labral lesion (adjusted odds ratio (OR) 2.8), impingement pits (adj. OR 2.9) and cartilage thinning | |||
| Sahin et al60 | Contralateral hip of THR patients compared with age and gender controls (Turkey) | 44 cases (23M, 21F) and 40 controls (21M, 19F) | Supine AP pelvis and cross-table lateral x-ray | All 84 participants: pincer FAI in 26% and cam FAI in 68%. Cam deformity found in 84% of study hips vs 32% of control hips; no significant difference in prevalence of pincer FAI | |||
| Athletes | |||||||
| Gerhardt et al61 | Professional soccer players (US) | 95 (75M, 20F) | AP pelvis, frog lateral x-ray | Cam deformity in 68% of male and 50% of female hips; pincer anatomy in 26.7% of male and 10% of female hips | |||
| Kapron et al62 | Collegiate football players (US) | 67 (134 hips) (all M) | Supine AP pelvis, frog lateral x-ray | 95% with at least one finding of FAI: 72% with an abnormal alpha angle, 61% with crossover sign | |||
| Silvis et al63 | Professional and collegiate hockey players (US) | 39 (all M) | MRI | 36% incidence of common adductor dysfunction, 56% with acetabular labral tears, 39% prevalence of cam deformity | |||
| Symptomatic patients | |||||||
| Ochoa et al64 | Active military with hip symptoms (US) | 157 patients (79M, 78F) | Combination of AP pelvis or AP hip and lateral hip | Total of 135 patients (87%) with at least one finding of FAI. Not all patients had complete radiographs, but of those with complete films, 65% had combined impingement, 17% had pure cam and 18% had pure pincer | |||
| Dolan et al65 | Patients (< 55 yrs) with symptomatic labral tears (US) | 135 patients with symptomatic labral tears (78M, 57F) | CT | 90% of symptomatic hips with at least one bony abnormality; 76% prevalence of cam FAI, 43% acetabular retroversion, 55% combination of deformity | |||
Table II
Prognosis of femoroacetabular impingement (FAI)
| Author/s | Population | Number of cases | Imaging used | Level of evidence | Major finding | ||||
|---|---|---|---|---|---|---|---|---|---|
| Allen et al67 | Patients < 55 yrs with symptomatic cam FAI (Canada) | 113 (82M, 31F) | AP pelvis and lateral x-ray | Prognostic, III | 88 patients with bilateral cam, but only 23 of these with bilateral symptoms | ||||
| Audenaert et al68 | Patients < 65 yrs undergoing THR (Belgium) | 121 | AP pelvis and cross-table lateral x-ray | Prognostic, IV | Low correlation of radiological and activity variables with age at THR. Patients with primarily cam impingement were younger at THR than patients with primarily pincer impingement | ||||
| Bardakos and Villar69 | Patients < 55 yrs with idiopathic OA with 10 years of radiological follow-up (UK) | 43 hips (43 patients) (35M, 8F) | Supine AP pelvis x-ray | Prognostic, III | 28 of 43 showed radiological progression of OA | ||||
| Clohisy et al70 | Patients < 50 yrs undergoing THR (US) | 604 (710 hips), (314M, 290F), 118 with FAI | AP pelvis and cross-table lateral x-ray | Prognostic, IV | High prevalence of FAI in patients previously diagnosed with “unknown causes of OA” (118 of 121), 70 FAI patients with radiographs at more than one timpoint all with bilateral findings, 73% progression of disease over time | ||||
| Hartofilakidis71 | Contralateral hip of patients < 65 yrs treated for unilateral hip disease (Greece) | 96 with FAI (31M, 65F) | AP pelvis x-ray | Prognostic, IV | 17.7% progression of OA over 10 years, presence of “idiopathic OA” on contralateral side was the only predictor of progression |
Lending further support to the hypothesis that stress on the developing physis causes FAI pathomorphology, the prevalence of FAI pathoanatomy appears to be more common in athletes. Pelvic radiographs of a cohort of American football players revealed that 61% had a crossover sign (evidence of acetabular retroversion or focal overcoverage) and 91% had at least some lack of femoral head-neck offset.62 In asymptomatic professional soccer players, 72% of males and 50% of females had at least one radiological abnormality predisposing them to FAI.61 MRIs of asymptomatic professional and collegiate hockey players revealed a 39% incidence of increased alpha angle and a 77% prevalence of hip or groin abnormalities, including labral tears, osteochondral lesions, or irregularities at the common adductor-rectus femoris tendon insertions.63
Although FAI-type morphology is common, the prognosis and identification of those patients who ultimately develop arthrosis is unclear (Table II).67-71 There is indirect evidence of the connection between FAI and hip arthrosis. Several studies have found an increased prevalence of hip arthrosis and total hip replacement in athletic patients compared with non-athletic controls.72-77 In 1971 Murray and Duncan78 found that athletes had higher rates of head-tilt deformity, which they interpreted as subclinical epiphysiolysis78; in the era of FAI the same morphology would likely be interpreted as a cam deformity. They also proposed that the subclinical SCFE was the causative factor of the increased rates of hip arthrosis seen in athletic patients.78 In other studies, elite athletes, dancers and those with high activity levels have at least twice the risk of hip arthrosis compared with controls.72-77 In general, the rates of radiological progression of arthrosis for patients with FAI morphology range from 18% to 73%.70,71 The evidence is limited, however, as these studies are Level III or IV evidence, and based on plain radiographs. In patients who do have hip pain or symptomatic labral tears, FAI morphology is very common, with a prevalence of around 90%.64,65
Intra-articular patterns of damage
The intra-articular pattern of chondrolabral damage is specific for each particular type of impingement. The most frequent site of a cam deformity is between 1 and 3 o’clock on the femoral neck, but can extend from 12 o’clock (directly superior) to the ligament of Weitbrecht at 6 o’clock.21,31,54,79 Cam or inclusion-type impingement causes shear and delamination injury to the cartilage.1,20,24 The labrum tears at the chondrolabral junction, but usually remains attached to the acetabular rim (Fig. 5).1,20 Pincer or impaction-type impingement causes a crush or bruising injury to the labrum, with less cartilage damage. Cartilage damage that does occur typically has a linear wear pattern (Fig. 6).20,24 The impact to the acetabular rim causes microfractures, with resultant bone apposition at the rim and labral ossification.23,24 Frequently the impaction causes levering of the femoral head, with a contre-coup injury to the posterior cartilage, opposite to the site of impingement.1,20,21 Patients with acetabular protrusio will also have medial cartilage thinning.22 Patients with subspine (AIIS) impingement have focal synovitis and labral ecchymosis inferior to the AIIS and localised bony build-up at the anterior acetabular rim or calcific deposits within the rectus insertion.28
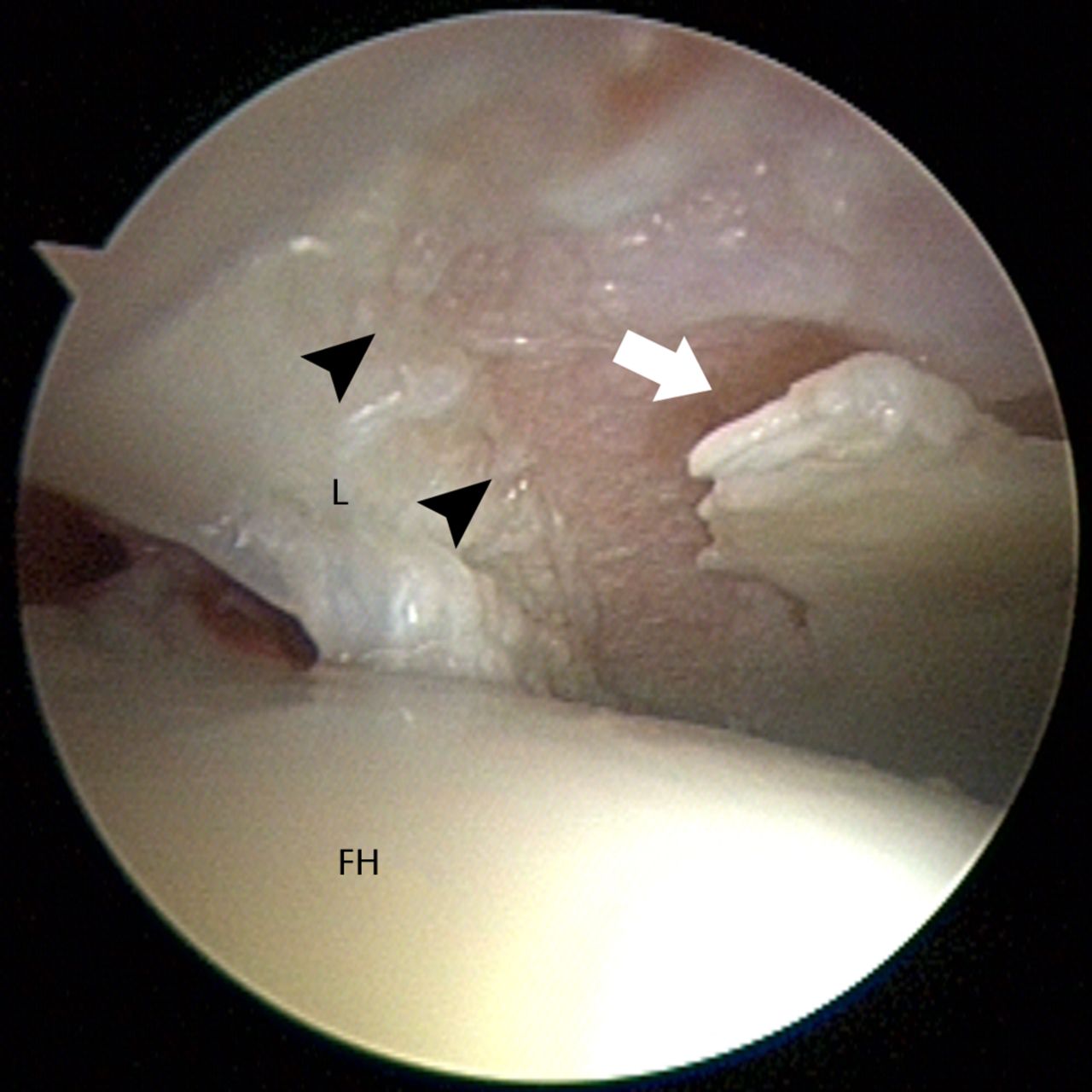
Fig. 5
Arthroscopic image showing chondrolabral damage occurring as a result of cam impingement. The deformity at the head–neck junction causes a shearing, delamination injury to the cartilage (white arrow) with tearing at the chondrolabral junction (black arrowheads) (L, labrum; FH, femoral head).
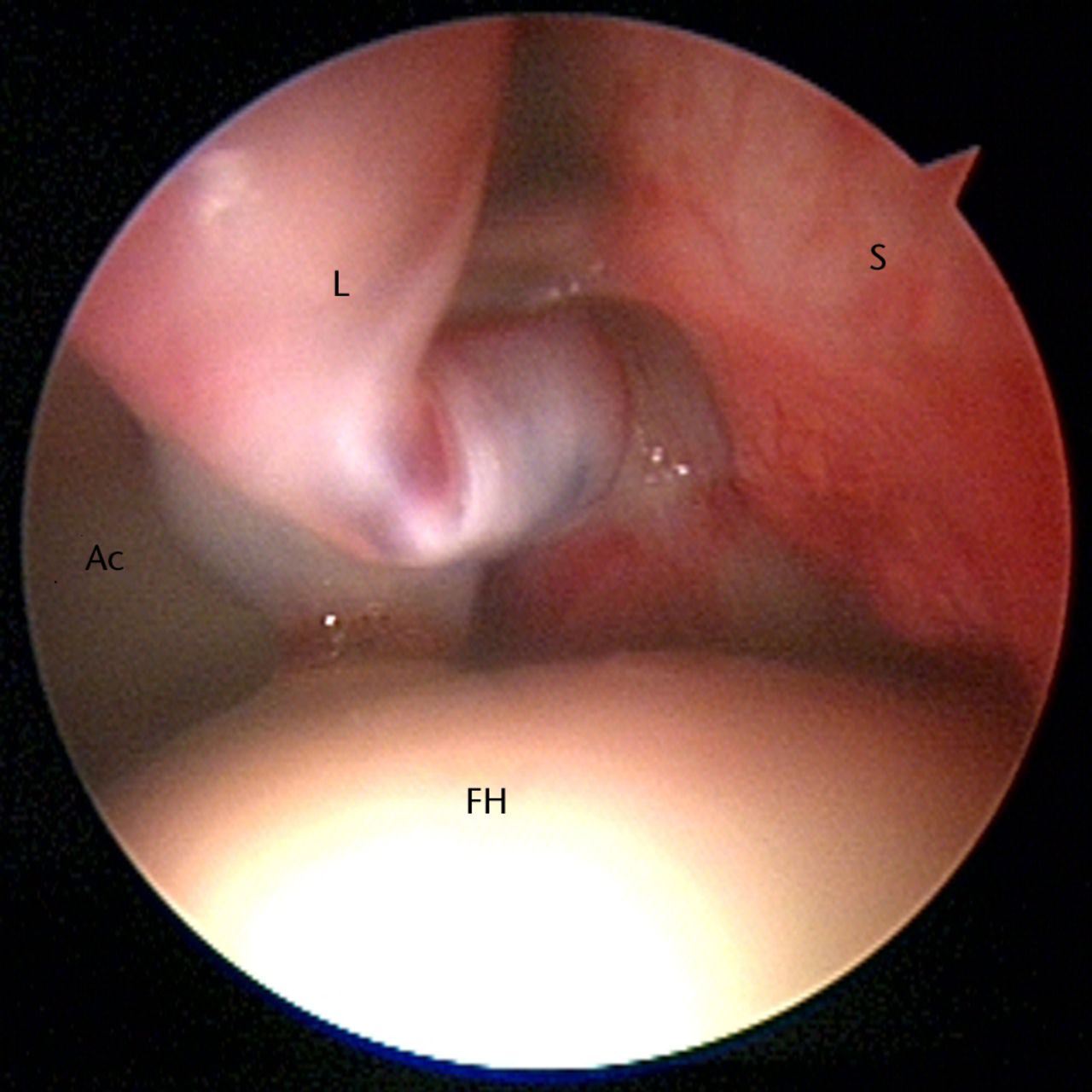
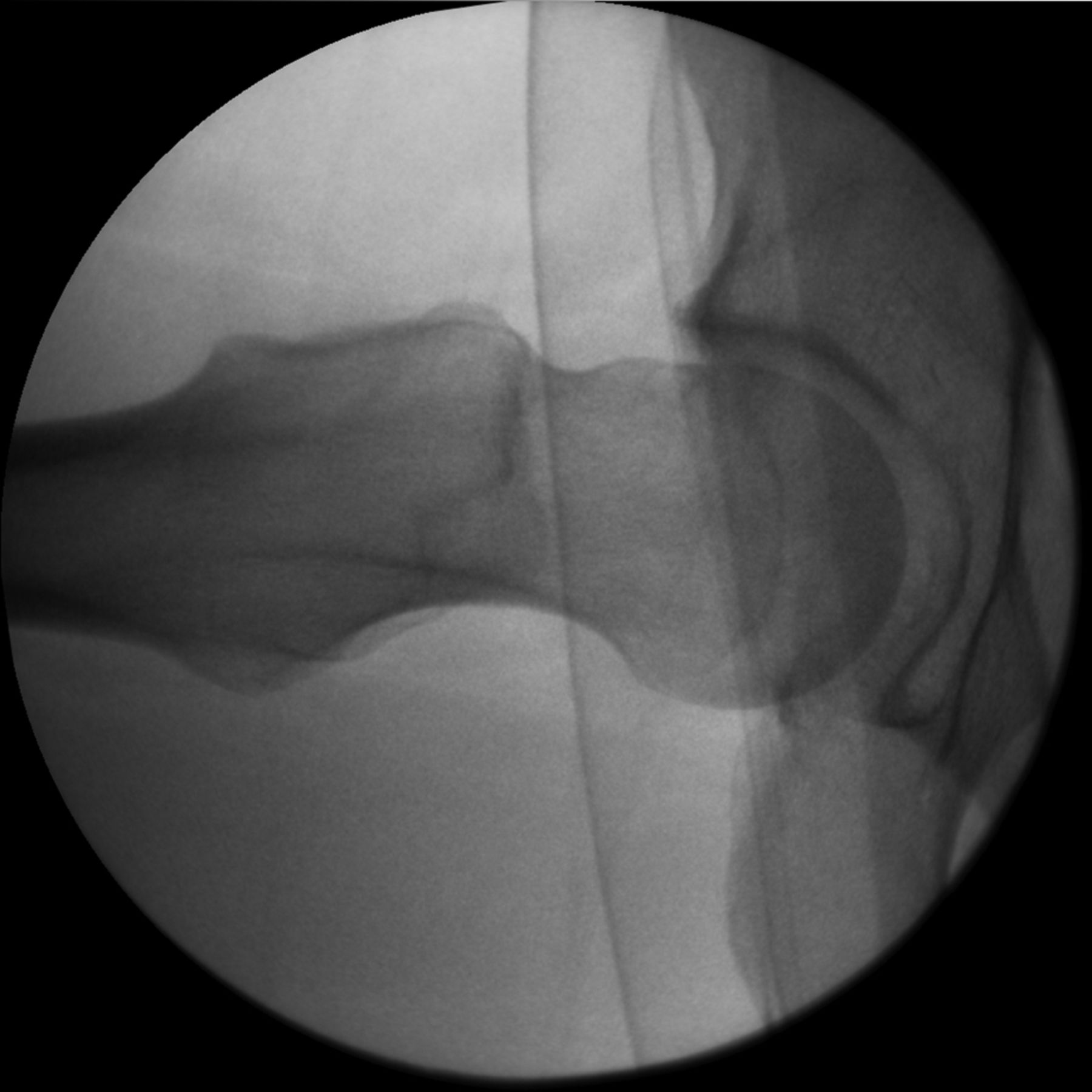
Fig. 6
Arthroscopic image showing chondrolabral damage occurring as a result of pincer impingement. The labrum (L) is bruised and hypertrophied, with adjacent synovitis (S). Cartilage damage occurs on the femoral side in a linear wear pattern (FH, femoral head; Ac, acetabulum).
It is also important to recognise the intra-articular pathology associated with instability. Static instability, which typically occurs in the setting of dysplasia, is associated with labral hypertrophy and ganglia.80,81 In contrast to the ‘outside-in’ damage that occurs with inclusion-type impingement, there is an inside-out avulsion of the labrum due to the lateral shear force of the subluxing femoral head. Often this piece of labrum has an attached piece of cartilage.16 Dynamic instability, or instability associated with motion and levering, can also cause the labrum to hypertrophy and develop ganglia. As mentioned earlier, instability that results from levering causes the posterior contre-coup injury to the cartilage. The extreme example of this is an anterior labral tear associated with a posterior subluxation or dislocation event (Fig. 7).82
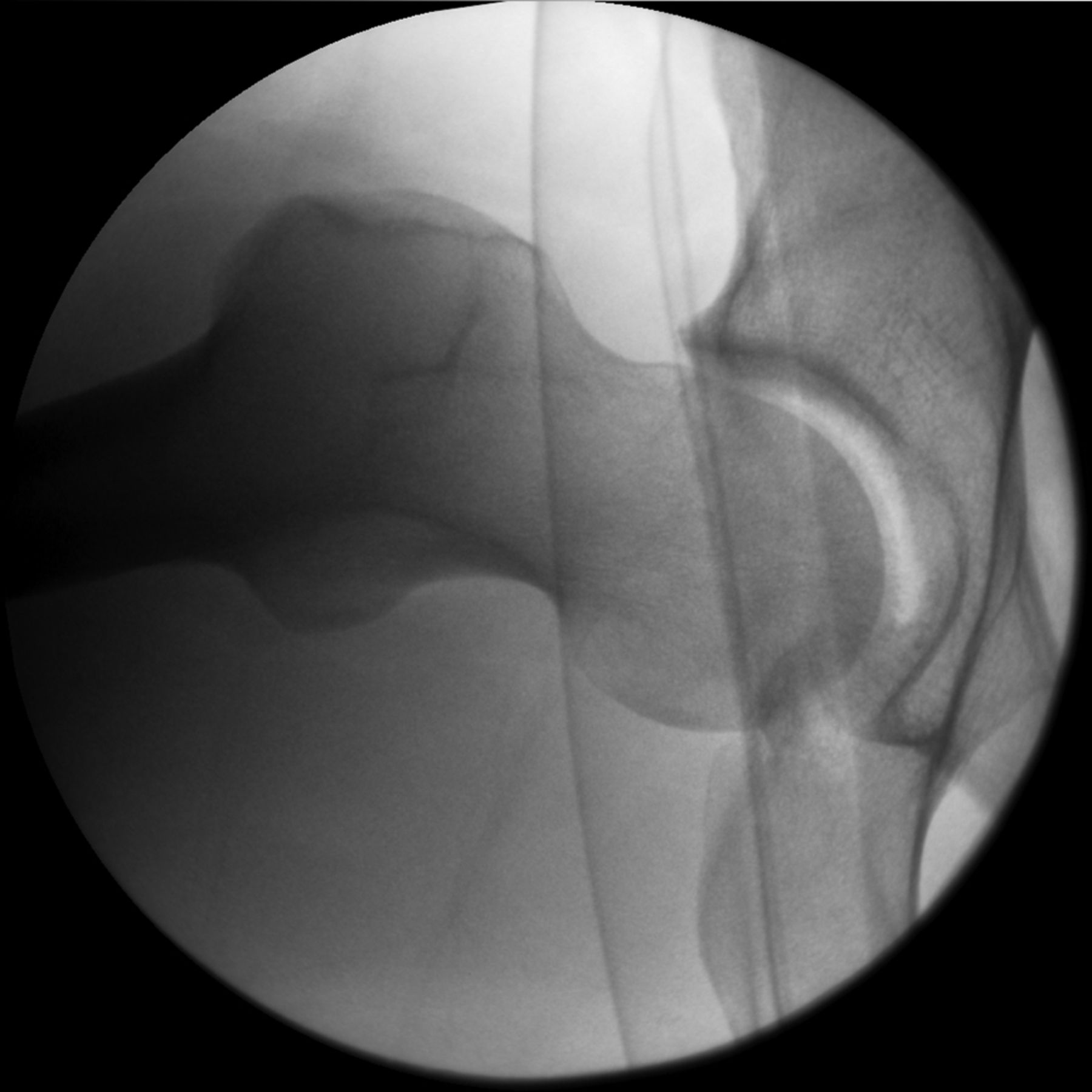
Figs. 7a - 7b
Fluoroscopic images showing dynamic instability due to impingement. The patient has a large anterior cam deformity, seen here on a lateral view with the leg in flexion (a). As the leg is flexed further, the deformity contacts the rim and causes levering of the head (b).
Exacerbating and mitigating factors
There are clear gender differences in FAI, some of which may actually be a consequence of gender differences in soft-tissue laxity. For example, it is well-recognised that women with symptomatic cam impingement have smaller deformities than men.14,61,83 A motion-analysis study of professional ballet dancers revealed that the repetitive motion of dance and relative soft-tissue laxity allowed the dancers to place their hips in impinging positions, despite not having any anatomic predisposition towards FAI.84 Similarly, because females typically have more soft-tissue laxity than males, they may become symptomatic or have impingement with more subtle deformities than males. The combination of soft-tissue laxity and a predisposition towards acetabular overcoverage also makes females more prone to dynamic instability and levering, with contre-coup cartilage injury.1,11,22,85 Looking at bony anatomy and the mechanical types of FAI, the prototypical patient with cam impingement is a young athletic male,1,21 whereas pincer impingement is more common in women.1,21,29 Further complicating the mechanical situation, symptomatic dysplasia is also more common in females86,87 and can co-exist with acetabular retroversion as well as with FAI.1,37,38,88 One study also found that women presented with worse pre-operative scores for pain and function than men.89 Post-operatively, however, there was no difference in outcomes between men and women, implying that the women had a more marked improvement than the men.89
There is increasing recognition that femoral version can exacerbate or mitigate the severity of FAI (Fig. 8).85,90 Specifically, femoral retroversion may exacerbate the effect of a cam deformity and is associated with decreased internal rotation and osteoarthrosis.83,88 Femoral retroversion was also recognised to be part of the pattern of malunion in post-traumatic FAI.5 An early radiological study of FAI found less femoral anteversion (i.e., retroversion) in a cohort of patients with cam-predominant FAI compared with a control group,14 but a more recent study did not observe a difference in femoral version between FAI patients and a control group.90 The proposed mechanism is that, in the retroverted femur, the femoral head is relatively rotated into the acetabulum, which decreases the clearance for flexion or flexion and internal rotation.14,85,90 Conversely, increased femoral anteversion may mitigate the effect of an anterior cam deformity, but is known to place increased stress on the psoas tendon.91 Patients with increased femoral anteversion who undergo psoas tenotomy are known to have worse results post-operatively, and it is thought that the psoas tendon is a dynamic anterior stabiliser in these patients.91 There has been one study that observed an association between increased femoral anteversion and pincer-type FAI morphology,90 but on the whole the relationship between femoral and acetabular version is unclear, as both positive and negative or inverse relationships between the two have been observed.88,92
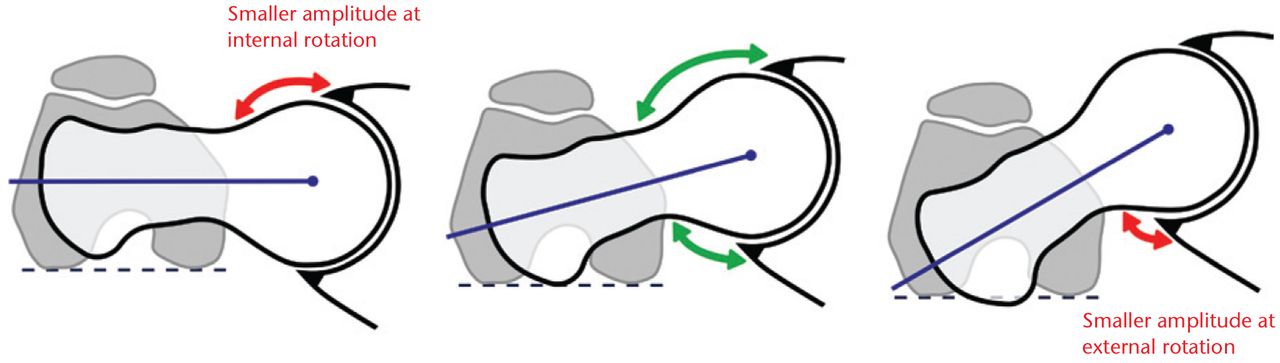
Fig. 8
Diagrams showing the proposed mechanism of the effect of femoral version. In the retroverted femur (left), the femoral head is already relatively rotated into the acetabulum, which decreases the clearance of any head-neck abnormality in flexion and exacerbates cam impingement. In an opposite manner, femoral anteversion (right) may mitigate the effect of an anterior cam deformity but could result in more impact on the posterior rim in external rotation. (Reprinted with permission: Sutter et al. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology 2012;263:475–483).
The effect of femoral neck-shaft angle is even less clear. A varus femur may be associated with symptomatic protrusio and pincer-type FAI,22 and varus malunion was also part of the pattern of post-traumatic FAI.5 A valgus femur can cause static acetabular overload19 and, in rare cases, can cause atypical patterns of impingement such as those occurring after valgus SCFE or valgus malunion of the femoral neck.4 On the whole, however, the mechanical effects of neck–shaft angle, femoral neck length, and femoral offset on FAI are unknown.
The athlete with asymptomatic FAI but limited hip motion may be at risk for additional soft-tissue injury or groin strain when trying to compensate for inadequate rotation.82 This may be especially common for sports requiring axial loading and rotation of the acetabulum over the femur. The ‘sports hip’ triad of labral tears, adductor strains, and rectus strain has been described in a cohort of American football players and provides some evidence for this.82 Other investigators have noted an association of athletic pubalgia and osteitis pubis with decreased hip range of movement.93 There is biomechanical evidence of increased movement at the pubic symphysis in the setting of a cam deformity,94 also providing some confirmation of the hypothesis that osteitis pubis is a compensatory injury secondary to decreased hip range of motion in FAI.
Arthroscopic management of FAI
A review article published on hip arthroscopy in 2003,95 the same year as Ganz et al’s description of FAI,1 lists the following indications for hip arthroscopy: labral tears, capsular laxity, chondral injury, ligamentum teres injuries, snapping hip, loose bodies and osteoarthritis. Although this review describes cheilectomy of the femoral neck for early osteophytes,95 the first arthroscopic technique specifically for management of FAI was published in 2005.96 As the understanding of FAI has improved, arthroscopic treatment of FAI and associated labral tears has also evolved. With minor (and sometimes major) variations in technique, arthroscopic management of FAI is similar to open management and involves resecting the impinging bone on the femoral neck, acetabular rim, or subspine region and addressing the associated chondrolabral pathology with either debridement or refixation.28,97-104
Presently, there are seven systematic review articles examining the outcomes of treatment for FAI, all of which were published between 2008 and 2011.105-111 Although each examines a slightly different question, many of the conclusions are similar. Nonetheless, this collective assessment of the available evidence is useful and makes several important points:
1. The level of the published evidence for arthroscopic management of FAI is relatively low. By far, the majority of studies constitute Level IV evidence, describing the outcomes in retrospective cohorts of patients.105-110
2. However, in comparison to other indications for hip arthroscopy, management of FAI had the best grade of recommendation (B), meaning that there was fair evidence to support the use of hip arthroscopy for treating FAI.108
3. Overall, most patients show improvement after surgery, with good to excellent outcomes in 68% to 96% of patients at two years post-operatively.105,106,110
4. There is an observed ceiling effect to the outcomes scores. Many studies are published with outcomes scores that are not validated for, or responsive to, the hip arthroscopy population.111 Furthermore, non-blinded observers assessed many of the outcome measures, which is a potential source of bias in the evaluation.111
Several systematic reviews have compared open and arthroscopic management of FAI. When early open series were included in the analysis, there was a higher rate of conversion to arthroplasty with open management.107,110 However, when the analysis included only the later series with more selective indications for surgery, conversion rates between arthroscopic and open management were similar. Correspondingly, the rates of good to excellent outcomes are comparable between open and arthroscopic techniques,105,107,110 although reported complications may be slightly less with arthroscopy.109,110 It is important to keep in mind that all of these reports were from high-volume surgeons and that complications will occur more frequently in the hands of less-experienced surgeons. The speed and rate of return to play was initially touted to be faster with arthroscopy,109,110 although this conclusion is debatable due to cultural differences in rehabilitation protocol and incentives for early return to sport. Finally, no direct comparison of return-to-play rates or time to return has been made in an otherwise homogeneous population.109,110 Since these systematic reviews were published, four other studies describing return-to-play in elite athletes have been published, which may have narrowed the gap in time to return, especially as the rehabilitation after arthroscopy may take longer than that initially published.102-104,112
Lessons learned in a decade of treating FAI
The past ten years of treating impingement though both arthroscopic and open techniques have produced important advances in the management of FAI. These advancements have served to refine the surgical indications, improved management of labral tears and helped to minimise complications. Treatment of FAI is, however, a ‘triple threat’: correct diagnosis of the impingement pathoanatomy can be difficult, the surgery itself is technically difficult, and the patients are typically young and active, with high expectations for their post-operative function. One study that assessed six-month post-operative outcomes found that, although patients demonstrated significant improvement in pain and function, “feeling better” (improvement) did not equate with “feeling good” (acceptability of the current status).89 Furthermore, for patients to consider their current state acceptable, the six-month outcome scores had to be 80% to 95% of the best achievable score for the given scale.89
A better understanding of the biomechanics of impingement, instability, and dysplasia facilitated the realisation that most labral tears are actually secondary to an underlying bony abnormality.65,113 Thus, if the patient undergoes labral repair without addressing the underlying impingement or dysplasia, the repair is likely to fail.97,98,114,115 This concept was reinforced by the clinical experience treating patients with recurrent labral tears and hip pain following arthroscopic labral repair, but who had inadequate treatment of their impingement or dysplasia.97,98,114,115 Although the initial observations of the pathology associated with instability and impingement were made via open surgery, observations made during arthroscopy have helped to clarify these mechanisms and the subsequent damage. In particular, arthroscopists have validated the concept that the intra-articular location and pattern of damage correlates with the particular type of impingement or instability,1,20,23,24,28,81 Although the pre-operative clinical and radiological evaluation should guide the plan for addressing the pathoanatomy causing FAI, the intra-operative appearance of the joint and associated damage should be used as confirmatory evidence guiding treatment.
The early failures, complications, and poor outcomes that occurred despite performing a technically good surgery are also important to note. As the short and mid-term results of hip arthroscopy and the treatment of FAI were published, it became evident that chondral damage is the biggest predictor of outcome after surgery for FAI.107,116-118 As a result of this early experience, most authors now consider Tönnis grade 2 or greater arthrosis on pre-operative radiographs a contraindication to surgical management. Heterotopic ossification can be a frequent complication after both open or arthroscopic femoral neck osteoplasty.99,100,119,120 This can be decreased or prevented entirely by giving non-steroidal anti-inflammatories post-operatively.100,120,121 Even prior to the introduction of the arthroscopic technique for managing FAI, it was recognised that traction-related complications are frequent in hip arthroscopy.117,122-127 Thus, inherent to the arthroscopic management of FAI is the importance of being efficient when addressing central compartment pathology and under traction.
Summary and conclusions
The field of preservation of the hip is currently the focus of intense interest, both within the orthopaedic community and among the general public. Correspondingly, this concentrated attention has produced tremendous advancements and change over the past decade. Some types of impingement pathoanatomy can now be treated with predictably good outcomes, for example, those patients with large cam deformities and minimal chondral damage. However, some mechanical hip pain is not yet fully understood. In particular, the intertwined effect of hyperlaxity and gender on both impingement and instability is only now being recognised. Similarly, the importance of femoral version to the mechanics of impingement is currently being worked out. Although femoral retroversion may exacerbate existing cam impingement, further biomechanical confirmation of this effect is necessary. The normal correlation between the acetabular and femoral version is unknown, as is whether a ‘mismatch’ in version can cause pincer impingement or instability.88,92 Finally, the potential contribution of extra-articular impingement and/or secondary instability to hip pain and pathology is beginning to be discussed among leaders in the field, but also remains unexamined. Valuable information about the pathoanatomy and biomechanics of impingement has been produced over the past decade. As a result, the treatment of FAI can relieve symptoms and help return patients to sports and activity. The latter has however be carefully balanced with the intra-articular damage; for some hips, return to sports might be ill-advised, and should not be considered as a measure for treatment success. It remains to be seen, however, if mid and long-term outcomes can be maintained and, ultimately, if this treatment will prevent hip arthrosis.
1 Ganz R , ParviziJ, BeckM, et al.Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res2003;417:112–120.CrossrefPubMed Google Scholar
2 Smith-Petersen MN . The classic: Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. 1936. Clin Orthop Relat Res2009;467:608–615.CrossrefPubMed Google Scholar
3 Herndon CH , HeymanCH, BellDM. Treatment of slipped capital femoral epiphysis by epiphyseodesis and osteoplasty of the femoral neck: a report of further experiences. J Bone Joint Surg [Am]1963;45-A:999–1012. Google Scholar
4 Ganz R, Bamert P, Hausner P, Isler B, Vrevc F. Cervico-acetabular impingement after femoral neck fracture. Unfallchirurg 1991;94:172–175 (in German). Google Scholar
5 Eijer H , MyersSR, GanzR. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma2001;15:475–481.CrossrefPubMed Google Scholar
6 Leunig M, Ganz R. The Bernese method of periacetabular osteotomy. Orthopäde 1998;27:743–750 (in German). Google Scholar
7 Hussell JG , RodriguezJA, GanzR. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res1999;363:81–92.PubMed Google Scholar
8 Myers SR , EijerH, GanzR. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res1999;363:93–99.PubMed Google Scholar
9 Leunig M , SiebenrockKA, GanzR. Rationale of periacetabular osteotomy and background work. Instr Course Lect2001;50:229–283.PubMed Google Scholar
10 Siebenrock KA , LeunigM, GanzR. Periacetabular osteotomy: the Bernese experience. Instr Course Lect2001;50:239–245.PubMed Google Scholar
11 Rab GT . The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop1999;19:419–424.CrossrefPubMed Google Scholar
12 Leunig M , CasillasMM, HamletM, et al.Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand2000;71:370–375.CrossrefPubMed Google Scholar
13 Ganz R , GillTJ, GautierE, et al.Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg [Br]2001;83-B:1119–1124. Google Scholar
14 Ito K , MinkaMA, LeunigM, WerlenS, GanzR. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg [Br]2001;83-B:171–176.CrossrefPubMed Google Scholar
15 Nötzli HP , WyssTF, StoecklinCH, et al.The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg [Br]2002;84-B:556–560.CrossrefPubMed Google Scholar
16 Klaue K , DurninCW, GanzR. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg [Br]1991;73-B:423–429. Google Scholar
17 Hipp JA , SuganoN, MillisMB, MurphySB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res1999;364:134–143.CrossrefPubMed Google Scholar
18 Zhao X , ChosaE, TotoribeK, DengG. Effect of periacetabular osteotomy for acetabular dysplasia clarified by three-dimensional finite element analysis. J Orthop Sci2010;15:632–640.CrossrefPubMed Google Scholar
19 Birnbaum K , PandorfT. Finite element model of the proximal femur under consideration of the hip centralizing forces of the iliotibial tract. Clin Biomech (Bristol, Avon)2011;26:58–64.CrossrefPubMed Google Scholar
20 Beck M , KalhorM, LeunigM, GanzR. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg [Br]2005;87-B:1012–1018.CrossrefPubMed Google Scholar
21 Pfirrmann CWA , MengiardiB, DoraC, et al.Cam and pincer femoroacetabular impingement: characteristic MR arthrogram findings in 50 patients. Radiology2006;240:778–785. Google Scholar
22 Leunig M , NhoSJ, TurchettoL, GanzR. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res2009;467:2241–2250.CrossrefPubMed Google Scholar
23 Corten K , GanzR, ChosaE, LeunigM. Bone apposition of the acetabular rim in deep hips: a distinct finding of global pincer impingement. J Bone Joint Surg [Am]2011;93-A(Suppl 2):10–16.CrossrefPubMed Google Scholar
24 Kohl S , HosalkarHS, Mainil-VarletP, et al.Histology of damaged acetabular cartilage in symptomatic femoroacetabular impingement: an observational analysis. Hip Int2011;21:154–162.CrossrefPubMed Google Scholar
25 Leunig M , RobertsonWJ, GanzR. Femoroacetabular impingement: diagnosis and management, including open surgical technique. Oper Tech Sports Med2007;15:178–188. Google Scholar
26 Toogood PA , SkalakA, CoopermanDR. Proximal femoral anatomy in the normal human population. Clin Orthop Relat Res2009;467:876–885.CrossrefPubMed Google Scholar
27 Siebenrock KA , WahabKH, WerlenS, et al.Abnormal extension of the femoral head as a cause of cam impingement. Clin Orthop Relat Res2004;418:54–60. Google Scholar
28 Larson CM , KellyBT, StoneRM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy2011;27:1732–1737.CrossrefPubMed Google Scholar
29 Sink EL , GrallaJ, RybaA, DaytonM. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop2008;28:806–811.CrossrefPubMed Google Scholar
30 Anderson LA , PetersCL, ParkBB, et al.Acetabular cartilage delamination in femoroacetabular impingement: risk factors and magnetic resonance imaging diagnosis. J Bone Joint Surg [Am]2009;91-A:305–313. Google Scholar
31 Dudda M , AlbersC, MamischTC, WerlenS, BeckM. Do normal radiographs exclude asphericity of the femoral head-neck junction?Clin Orthop Relat Res2009;467:651–659.CrossrefPubMed Google Scholar
32 Cobb J , LogishettyK, DavdaK, IranpourF. Cam and pincer impingement are distinct, not mixed: the acetabular pathomorphology of femoroacetabular impingement. Clin Orthop Relat Res2010;468:2143–2151. Google Scholar
33 Beck M . Letter to the editor: Cam and pincer impingement are distinct, not mixed: the acetabular pathomorphology of femoroacetabular impingement. Clin Orthop Relat Res2011;469:1207. Google Scholar
34 Reynolds D , LucasJ, KlaueK. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg [Br]1999;81-B:281–288. Google Scholar
35 Siebenrock KA , SchoenigerR, GanzR. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg [Am]2003;85-A:278–286. Google Scholar
36 Jamali AA , MladenovK, MeyerDC, et al.Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res2007;25:758–765. Google Scholar
37 Fujii M , NakashimaY, YamamotoT, et al.Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg [Am]2010;92-A:895–903.CrossrefPubMed Google Scholar
38 Paliobeis CP , VillarRN. The prevalence of dysplasia in femoroacetabular impingement. Hip Int2011;21:141–145.CrossrefPubMed Google Scholar
39 Eijer H , PodeszwaDA, GanzR, LeunigM. Evaluation and treatment of young adults with femoroacetabular impingement secondary to Perthes’ disease. Hip Int2006;16:273–280. Google Scholar
40 Steppacher SD , TannastM, WerlenS, SiebenrockKA. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res2008;466:782–790.CrossrefPubMed Google Scholar
41 Serrat MA , RenoPL, McCollumMA, MeindlRS, LovejoyCO. Variation in mammalian proximal femoral development: comparative analysis of two distinct ossification patterns. J Anat2007;210:249–258.CrossrefPubMed Google Scholar
42 Osborne D , EffmannE, BrodaK, HarrelsonJ. The development of the upper end of the femur, with special reference to its internal architecture. Radiology1980;137:71–76.CrossrefPubMed Google Scholar
43 Hogervorst T , BoumaH, de BoerSF, de VosJ. Human hip impingement morphology: an evolutionary explanation. J Bone Joint Surg [Br]2011;93-B:769–776.CrossrefPubMed Google Scholar
44 Ellis AR , NoblePC, SchroderSJ, ThompsonMT, StocksGW. The cam impinging femur has multiple morphologic abnormalities. J Arthroplasty2011;26(Suppl):59–65.CrossrefPubMed Google Scholar
45 Kienle KP, Keck J, Werlen S, et al. Femoral morphology and epiphyseal growth plate changes of the hip during maturation: MR assessments in a 1-year follow-up on a cross-sectional asymptomatic cohort in the age range of 9-17 years. Skeletal Radiol 2012: Epub. Google Scholar
46 Siebenrock KA , FernerF, NoblePC, et al.The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. C. lin Orthop Relat Res2011;469:3229–3240. Google Scholar
47 Crockett HC , GrossLB, WilkKE, et al.Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med2002;30:20–26.CrossrefPubMed Google Scholar
48 Mair SD , UhlTL, RobbeRG, BrindleKA. Physeal changes and range-of-motion differences in the dominant shoulders of skeletally immature baseball players. J Shoulder Elbow Surg2004;13:487–491.CrossrefPubMed Google Scholar
49 DiFiori JP , CaineDJ, MalinaMR. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med2006;34:840–849.CrossrefPubMed Google Scholar
50 Gage RJ , CaryJM. The effects of trochanteric epiphyseodesis on growth of the proximal end of the femur following necrosis of the capital femoral epiphysis. J Bone Joint Surg [Am]1980;62-A:785–794.PubMed Google Scholar
51 Struijs PAA , OostraRJ, van RijnRR, BesselaarPP. Abnormal growth of the proximal femur due to apophyseal-epiphyseal coalescence resuiting in coxa valga: a report of two cases in adolescents. Acta Orthop2011;82:507–509. Google Scholar
52 Dudda M , KimYJ, ZhangY, et al.Morphologic differences between the hips of Chinese women and white women. Arthritis Rheum2011;63:2992–2999.CrossrefPubMed Google Scholar
53 Gosvig KK , JacobsenS, Sonne-HolmS, PalmH, TroelsenA. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis. J Bone Joint Surg [Am]2010;92-A:1162–1169.CrossrefPubMed Google Scholar
54 Hack K , DiPrimioG, RakhraK, BeauléPE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg [Am]2010;92-A:2436–2444.CrossrefPubMed Google Scholar
55 Kang ACL , GoodingAJ, CoatesMH, et al.Computed tomography assessment of hip joints in asymptomatic individuals in relation to femoroacetabular impingment. Am J Sports Med2010;38:1160–1165. Google Scholar
56 Laborie LB , LehmannTG, EngesæterIØ, et al.Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology2011;260:494–502.CrossrefPubMed Google Scholar
57 Pollard TC , VillarRN, NortonMR, et al.Genetic influences in the aetiology of femoroacetabular impingement: a sibling study. J Bone Joint Surg [Br]2010;92-B:209–216.CrossrefPubMed Google Scholar
58 Reichenbach S , JüniP, WerlenS, et al.Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken)2010;62:1319–1327.CrossrefPubMed Google Scholar
59 Reichenbach S , LeunigM, WerlenS, et al.Association between cam-type deformities and magnetic resonance imaging-detected structural hip damage; a cross-sectional study in young men. :. Arthritis Rheum2011;63:4023–4030. Google Scholar
60 Sahin N , AticiT, ÖztürkA, et al.Prevalence of femoroacetabular impingement in asymptomatic contralateral hips in patients with unilateral idiopathic osteoarthritis. J Int Med Res2011;39:790–797.CrossrefPubMed Google Scholar
61 Gerhardt MB , RomeroAA, SilversHJ, et al.The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med2012;40:584–588.CrossrefPubMed Google Scholar
62 Kapron AL , AndersonAE, AokiSK, et al.Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg [Am]2011;93-A:111.CrossrefPubMed Google Scholar
63 Silvis ML , MosherTJ, SmetanaBS, et al.High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med2011;39:715–721.CrossrefPubMed Google Scholar
64 Ochoa LM , DawsonL, PatzkowskiJC, HsuJR. Radiographic prevalence of femoroacetabular impingement in a young population with hip complaints is high. Clin Orthop Relat Res2010;468:2710–2714.CrossrefPubMed Google Scholar
65 Dolan MM , HeyworthBE, BediA, DukeG, KellyBT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res2011;469:831–838.CrossrefPubMed Google Scholar
66 Stevenson DA , MineauG, KerberRA, et al.Familial predisposition to developmental dysplasia of the hip. J Pediatr Orthop2009;29:463–466.CrossrefPubMed Google Scholar
67 Allen D , BeauléPE, RamadanO, DoucetteS. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J Bone Joint Surg [Br]2009;91-B:589–594.CrossrefPubMed Google Scholar
68 Audenaert EA , PeetersI, VanOnsemS, PattynC. Can we predict the natural course of femoroacetabular impingement?Acta Orthop Belg2011;77:188–196.PubMed Google Scholar
69 Bardakos NV , VillarRN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg [Br]2009;91-B:162–169.CrossrefPubMed Google Scholar
70 Clohisy JC , DobsonMA, RobisonJF, et al.Radiographic structural abnormalities associated with premature, natural hip-joint failure. J Bone Joint Surg [Am]2011;93-A(Suppl 2):3–9.CrossrefPubMed Google Scholar
71 Hartofilakidis G , BardakosNV, BabisGC, GeorgiadesG. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J Bone Joint Surg [Br]2011;93-B:580–586.CrossrefPubMed Google Scholar
72 Andersson S , NilssonB, HessellT, et al.Degenerative joint disease in ballet dancers. Clin Orthop Relat Res1989;236:233–236.PubMed Google Scholar
73 Lindberg H , RoosH, GärdsellP. Prevalence of coxarthrosis in former soccer players: 286 players compared with matched controls. Acta Orthop Scand1993;64:165–167. Google Scholar
74 Vingard E , AlfredssonL, GoldieI, HogstedtC. Sports and osteoarthritis of the hip: an epidemiologic study. Am J Sports Med1993;21:195–200. Google Scholar
75 Vingard E , AlfredssonL, MalchauH. Osteoarthrosis of the hip in women and its relationship to physical load from sports activities. Am J Sports Med1998;26:78–82.CrossrefPubMed Google Scholar
76 L’Hermette M , PolleG, Tourny-CholletC, DujardinF. Hip passive range of motion and frequency of radiographic hip osteoarthritis in former elite handball players. Br J Sports Med2006;40:45–49.CrossrefPubMed Google Scholar
77 Tveit M , RosengrenBE, NilssonJA, KarlssonMK. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med2012;40:527–533.CrossrefPubMed Google Scholar
78 Murray RO , DuncanC. Athletic activity in adolescence as an etiological factor in degenerative hip disease. J Bone Joint Surg [Br]1971;53-B:406–419.PubMed Google Scholar
79 Rakhra KS , SheikhAM, AllenD, BeauléPE. Comparision of MRI alpha angle measurement planes in femoroacetabular impingement. Clin Orthop Relat Res2009;467:660–665. Google Scholar
80 Leunig M , PodeszwaD, BeckM, WerlenS, GanzR. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res2004;418:74–80.CrossrefPubMed Google Scholar
81 Ross JR , ZaltzI, NeppleJJ, SchoeneckerPL, ClohisyJC. Arthroscopic disease classification and interventions as an adjunct in the treatment of acetabular dysplasia. Am J Sports Med2011;39(Suppl):72S–78S.CrossrefPubMed Google Scholar
82 Feeley BT , PowellJW, MullerMS, et al.Hip injuries and labral tears in the National Football League. Am J Sports Med2008;36:2187–2195.CrossrefPubMed Google Scholar
83 Nakahara I , TakaoM, SakaiT, et al.Gender differences in 3D morphology and bony impingement of human hips. J Orthop Res2011;29:333–339.CrossrefPubMed Google Scholar
84 Charbonnier C , KoloFC, DuthonVB, et al.Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med2011;39:557–566.CrossrefPubMed Google Scholar
85 Bedi A , DolanM, LeunigM, KellyBT. Static and dynamic mechanical causes of hip pain. Arthroscopy2011;27:235–251.CrossrefPubMed Google Scholar
86 Jacobsen S , Sonne-HolmS. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. Rheumatology2005;44:211–218.CrossrefPubMed Google Scholar
87 Clohisy JC , SchutzAL, St JohnL, SchoeneckerPL, WrightRW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res2009;467:2041–2052.CrossrefPubMed Google Scholar
88 Tönnis D , HeineckeA. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg [Am]1999;81-A:1747–1770.CrossrefPubMed Google Scholar
89 Impellizzeri FM , MannionAF, NaalFD, HerscheO, LeunigM. The early outcome of surgical treatment for femoroacetabular impingement: success depends on how you measure it. Osteoarthritis Cartilage2012;20:638–645.CrossrefPubMed Google Scholar
90 Sutter R , DietrichTJ, ZinggPO, PfirrmannCWA. Femoral antetorsion: comparing asymptomatic volunteers and patients with femoroacetabular impingement. Radiology2012;263:475–483.CrossrefPubMed Google Scholar
91 Fabricant PD , BediA, De La TorreK, KellyBT. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy2012;28:965–971.CrossrefPubMed Google Scholar
92 Buller LT , RosneckJ, MonacoFM, et al.Relationship between proximal femoral and acetabular alignment in normal hip joints using 3-dimensional computed tomography. Am J Sports Med2012;40:367–375.CrossrefPubMed Google Scholar
93 Verrall GM , SlavotinekJP, BarnesPG, et al.Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport2007;10:463–466.CrossrefPubMed Google Scholar
94 Birmingham PM , KellyBT, JacobsR, McGradyL, WangM. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med2012;40:1113–1118.CrossrefPubMed Google Scholar
95 Kelly BT , WilliamsRJ, PhilipponMJ. Hip arthroscopy: Current indications, treatment options, and management issues. Am J Sports Med2003;31:1020–1037.CrossrefPubMed Google Scholar
96 Sampson TG . Arthroscopic treatment of femoroacetabular impingement. Tech Orthop2005;20:56–62.CrossrefPubMed Google Scholar
97 Heyworth BE , ShindleMK, VoosJE, RudzkiJR, KellyBT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy2007;23:1295–1302.CrossrefPubMed Google Scholar
98 Philippon MJ , SchenkerML, BriggsKK, et al.Revision hip arthroscopy. Am J Sports Med2007;35:1918–1921.CrossrefPubMed Google Scholar
99 Byrd JW , JonesKS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res2009;467:739–746.CrossrefPubMed Google Scholar
100 Larson CM , GiveansMR. Arthroscopic debridement versus refixation of the labrum associated with femoroacetabular impingement. Arthroscopy2009;25:369–376. Google Scholar
101 Leunig M , HorowitzK, MannerH, GanzR. In situ pinning with arthroscopic osteoplasty for mild SCFE: a preliminary technical report. Clin Orthop Relat Res2010;468:3160–3167.CrossrefPubMed Google Scholar
102 Singh PJ , O’DonnellJM. The outcome of hip arthroscopy in Australian football league players: a review of 27 hips. Arthroscopy2010;26:743–749.CrossrefPubMed Google Scholar
103 Byrd JW , JonesKS. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med2011;39(Suppl):7S–13S.CrossrefPubMed Google Scholar
104 Nho SJ , MagennisEM, SinghCK, KellyBT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med2011;39(Suppl):14S–19S.CrossrefPubMed Google Scholar
105 Bedi A , ChenN, RobertsonW, KellyBT. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy2008;24:1135–1145.CrossrefPubMed Google Scholar
106 Clohisy JC , St JohnLC, SchutzAL. Surgical treatment of femoroacetabular impingement: a systematic review of the literature. Clin Orthop Relat Res2010;468:555–564.CrossrefPubMed Google Scholar
107 Ng VY , AroraN, BestTM, PanX, EllisTJ. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med2010;38:2337–2345.CrossrefPubMed Google Scholar
108 Stevens MS , LeGayDA, GlazebrookMA, AmiraultD. The evidence for hip arthroscopy: grading the current indications. Arthroscopy2010;26:1370–1383.CrossrefPubMed Google Scholar
109 Botser IB , SmithTW, NasserR, DombBG. Open surgical dislocation versus arthroscopy for femoroacetabular impingement: a comparison of clinical outcomes. Arthroscopy2011;27:270–278.CrossrefPubMed Google Scholar
110 Matsuda DK , CarlisleJC, ArthursSC, WierksCH, PhilipponMJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy2011;27:252–269.CrossrefPubMed Google Scholar
111 Kemp JL , CollinsNJ, MakdissiM, et al.Hip arthroscopy for intra-articular pathology: a systematic review of outcomes with and without femoral osteoplasty. Br J Sports Med2011;46:632–643.CrossrefPubMed Google Scholar
112 Naal FD , MiozzariHH, WyssTF, NötzliHP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med2011;39:544–550.CrossrefPubMed Google Scholar
113 Wenger DE , KendellKR, MinerMR, TrousdaleRT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res2004;426:145–150.CrossrefPubMed Google Scholar
114 Parvizi J , BicanO, BenderB, et al.Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty2009;24(Suppl):110–113.CrossrefPubMed Google Scholar
115 Kain MS , NovaisEN, VallimC, MillisMB, KimYJ. Periacetabular osteotomy after failed hip arthroscopy for labral tears in patients with acetabular dysplasia. J Bone Joint Surg [Am]2011;93-A(Suppl 2):57–61.CrossrefPubMed Google Scholar
116 Byrd JW , JonesKS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy2009;25:365–368.CrossrefPubMed Google Scholar
117 Streich NA , GotterbarmT, BariéA, SchmittH. Prognostic value of chondral defects on the outcome of arthroscopic treatment of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc2009;17:1257–1263. Google Scholar
118 McCarthy JC , JarrettBT, OjeifoO, LeeJA, BragdonCR. What factors influence long-term survivorship after hip arthroscopy?Clin Orthop Relat Res2011;469:362–371.CrossrefPubMed Google Scholar
119 Sink EL , BeauléPE, SucatoD, et al.Multicenter study of complications following surgical dislocation of the hip. J Bone Joint Surg [Am]2011;93-A:1132–1136.CrossrefPubMed Google Scholar
120 Bedi A , ZbedaRM, BuenoVF, et al.The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med2012;40:854–863.CrossrefPubMed Google Scholar
121 Randelli F , PierannunziiL, BanciL, et al.Heterotopic ossifications after arthroscopic management of femoroacetabular impingement: the role of NSAID prophylaxis. J Orthop Traumatol2010;11:245–250.CrossrefPubMed Google Scholar
122 Funke EL , MunzingerU. Complications in hip arthroscopy. Arthroscopy1996;12:156–159. Google Scholar
123 Griffin DR , VillarRN. Complications of arthroscopy of the hip. J Bone Joint Surg [Br]1999;81-B:604–606. Google Scholar
124 Clarke MT , AroraA, VillarRN. Hip arthroscopy: complications in 1054 cases. Clin Orthop Relat Res2003;406:84–88.CrossrefPubMed Google Scholar
125 Burnett RS , Della RoccaGJ, PratherH, et al.Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg [Am]2006;88-A:1448–1457.CrossrefPubMed Google Scholar
126 Souza BGS , DaniWS, HondaEK, et al.Do complications in hip arthroscopy change with experience?Arthroscopy2010;26:1053–1057.CrossrefPubMed Google Scholar
127 Nwachukwu BU , McFeelyED, NasreddineAY, et al.Complications of hip arthroscopy in children and adolescents. J Pediatr Orthop2011;31:227–231.CrossrefPubMed Google Scholar
Funding statement:
This work received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author contributions:
L. M. Tibor: Contributed to paper concept, Wrote manuscript draft and revisions
M. Leunig: Developed paper concept, Assisted with manuscript revisions
ICMJE Conflict of Interest:
Dr. Leunig has the following potential conflicts of interest: consultant for Smith & Nephew; stock options in Pivot Medical. No payment or benefit of any kind was received related to this work.
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










