Abstract
Aims
The aim of this study was to evaluate medium-term outcomes and complications of the S-ROM NOILES Rotating Hinge Knee System (DePuy, USA) in revision total knee arthroplasty (rTKA) at a tertiary unit.
Methods
A retrospective consecutive study of all patients who underwent a rTKA using this implant from January 2005 to December 2018. Outcome measures included reoperations, revision for any cause, complications, and survivorship. Patients and implant survivorship data were identified through both local hospital electronic databases and linked data from the National Joint Registry/NHS Personal Demographic Service. Kaplan-Meier survival analysis was used at ten years.
Results
A total of 89 consecutive patients (89 knees) were included with 47 females (52.8%) and a median age of 74 years (interquartile range 66 to 79). The main indications were aseptic loosening with instability (39.4%; n = 35) and infection (37.1%; n = 33) with the majority of patients managed through two-stage approach. The mean follow-up was 7.4 years (2 to 16). The overall rate of reoperation, for any cause, was 10.1% (n = 9) with a rate of implant revision of 6.7% (n = 6). Only two cases required surgery for patellofemoral complications. Kaplan-Meier implant-survivorship analysis was 93.3% at ten years, using revision for any cause as an endpoint.
Conclusion
This implant achieved high ten-year survivorship with a low complication rate, particularly patellofemoral complications. These can be avoided by ensuring central patella tracking and appropriate tension of the patellofemoral joint in this posterior hinge design.
Cite this article: Bone Jt Open 2022;3(3):205–210.
Take home message
High ten-year survivorship can be expected with rotating-hinge implant with metaphyseal sleeve fixation in revision total knee arthroplasty.
Patellofemoral complications can be avoided by ensuring central patella tracking and appropriate tension of the patellofemoral joint in this posterior hinge design.
Introduction
The indications for a rotating-hinge implant in revision total knee arthroplasty (rTKA) practice are well-established. These include gross multidirectional instability or flexion-extension mismatch, bone loss that compromises ligament attachments, and collateral ligament deficiency, particularly of the medial collateral ligament, among others.1
Early hinged designs only allowed for flexion-extension motion. This high level of constraint led to high failure and complication rates.2-4 Varus-valgus motion and axial rotation were introduced in second-generation designs, reducing the level of prosthetic constraint and subsequently the torque stresses on the implant-cement and implant-bone interfaces.5-7 More contemporary third-generation implants saw the introduction of an improved rotating-hinge mechanism, improved patellofemoral biomechanics, increased component modularity, and improved fixation techniques leading to significant improvements in survivorship and clinical outcomes.8-11
Survivorship ranges from 51% to 92.5% at up to ten-year follow-up with complication rates ranging from 9.2% to 63%, as reported in a systematic review of rotating-hinge implants in rTKA.12 Patellofemoral complications remain high, with patella subluxation reported in 29.6% of cases in a recent contemporary series.13 Patellofemoral instability following a rotating-hinge implant is multifactorial with patient-, surgical-, and implant-related factors. The mobile bearings in contemporary hinges allow rotation with varying degrees of constraint, shapes, and mechanisms in different prostheses, with some having a long rotating tibiofemoral axis, a short and intra-articular one, or with a fixed longitudinal axis.14
The S-ROM NOILES Rotating Hinge Knee System (DePuy, USA) is well-established and widely used. However, high rates of patellofemoral complications have been reported with this prosthesis.15-18 The mobile-bearing insert in this system is congruent with the femoral component with a flat undersurface where rotation occurs at the insert-tibial tray interface. The aim of this study was to evaluate the outcomes of this prosthesis at medium-term follow-up in rTKA at our tertiary unit.
Methods
This was a retrospective consecutive study of all patients who underwent a rTKA using S-ROM implant between January 2005 and December 2018. Local institutional study approval was obtained. Patients were identified using a local prospective database and linkable data obtained from the National Joint Registry (NJR) for rTKA. Surgeries were performed by two authors (BVB, PJJ). We excluded patients that required endoprostheses with distal femoral arthroplasties and patients with periprosthetic fractures.19,20 Demographic, clinical, and surgical data were collected from patients’ electronic health records. All patients underwent routine preoperative anaesthetic assessment and received a spinal anaesthetic with upper thigh sterile tourniquet and perioperative prophylactic antibiotics. Postoperatively, full weightbearing was commenced as tolerated with routine physiotherapy. Follow-up was performed regularly at six weeks and three months, and every 12 months thereafter.
Implant
The S-ROM Rotating Hinge Knee System is a third-generation modular mobile-bearing prosthesis that has evolved from the original NOILES prosthesis. Fixation is enhanced by the addition of modular titanium metaphyseal sleeves (cemented or cementless), which can be added as part of the construct through a Morse taper junction.18 In this condylar design, the components are made of highly polished cobalt-chromium with a highly congruent mobile-bearing polyethylene. The femoral component is linked via a yoke and axle assembly hinge mechanism. The undersurface of the polyethylene insert is flat and articulates with the flat surface of the tibial tray with no inherent resistance to rotation at this interface (Figure 1). In our practice, we routinely use cementless metaphyseal sleeves on the tibial side and, in selected patients, on the femoral side.21
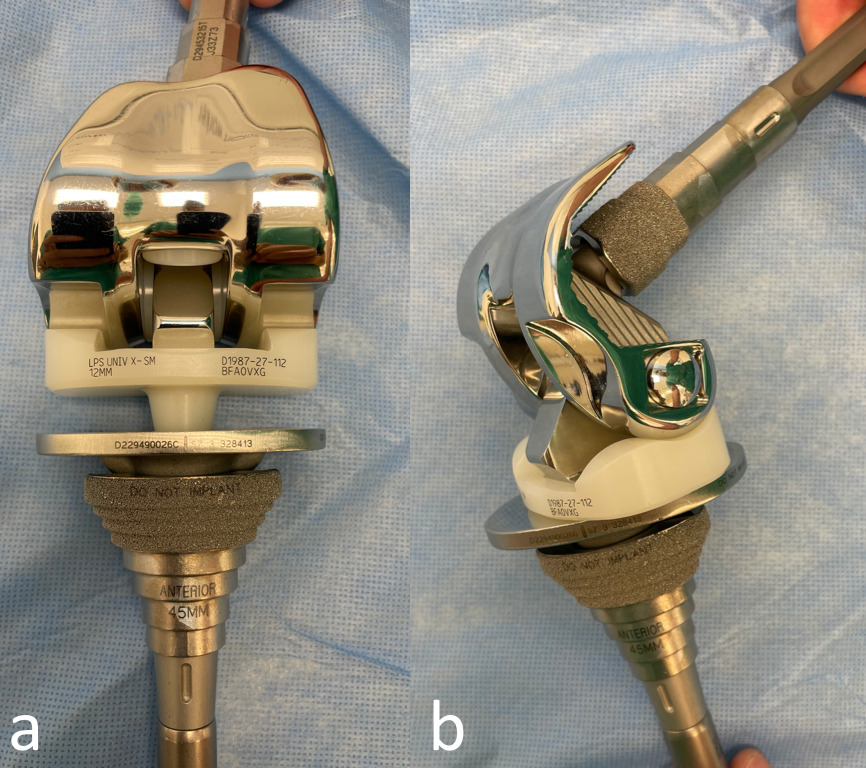
Fig. 1
Photographs of the S-ROM prosthesis. a) The polyethylene insert is congruent with the femoral component with a flat-on-flat articulation with the tibial tray. b) Note that there is no inherent resistance to rotation at the insert-tibial tray interface.
Operating technique
Using the pre-existing midline incision, whenever possible with appropriate proximal and distal extensions, knees were approached through a standard medial parapatellar arthrotomy with subluxation of the patella following complete synovectomy. Components were then removed in the standard fashion with minimal bone loss. The tibia was prepared and the canal was reamed to accept an appropriately sized stem with press-fit metaphyseal sleeve. Attention was then turned to the femur, and the canal was similarly prepared using a press-fit cementless stem with femoral metaphyseal sleeve. We posteriorized the sleeve to ensure central stem position in the femoral canal. A trial was then assembled and articulated with the tibial component. The joint line level was restored in flexion and extension and checked using a combination of anatomical markers, soft-tissue tension (particularly extensor apparatus), and length measurements, including patellofemoral articulation.22 We routinely resurfaced the native patella in revision cases. However, if the patella had been resurfaced at time of primary surgery and was tracking well with minimal wear, it was left in situ and selectively revised in cases of button wear to mitigate risk of patellar fracture or fragmentation. Once satisfactory trial positioning was obtained, definitive implants were assembled to match the trials. For surface cementing, Palacos R + G (Hereaus Medical, Germany) was used. Additional antibiotics can be added to the cement as required.23 Routine closure was then performed in layers over a drain, which was removed in 24 hours. Full weightbearing was commenced as tolerated with routine physiotherapy.
Outcome measures
Clinical outcomes includng surgical complications, reoperations, revision for any cause, loosening, and mortality data were collected. Revision was defined as removal or exchange of any component; debridement, antibiotics and implant retention (DAIR) was also considered a revision procedure. Death was identified through both local hospital electronic databases and linked data from the NJR/NHS Personal Demographic Service.
Statistical analysis
The values of all parameters are presented as number and percentage. Power calculation for sample size was calculated using average reported rate of complications (22%).1,12,14 A minimum of 63 knees were required to detect a statistically significant difference (power: 0.8, α = 0.05). Kaplan-Meier survival curves were used for survivorship analysis. Statistical analyses were performed using SPSS 16.0 software (SPSS, USA).
Results
There were 89 consecutive patients (89 knees) during the study period and were all included in the analysis. These included 47 female (52.8%) and 42 male patients (47.25%) with median age of 74 years (interquartile range (IQR) 66 to 79) and median BMI of 30 kg/m2 (IQR 28 to 33; Table I). The main indications were aseptic loosening with instability (39.4%; n = 35) and infection (37.1%; n = 33), with the majority of patients managed through two-stage approach (Table I).
Table I.
Baseline characteristics and indication for surgery.
| Characteristic | Total |
|---|---|
| Patients/knees, n | 89/89 |
| Median age, yrs (IQR) | 74 (66 to 79) |
| Female, n (%) | |
| Median BMI, kg/m2 (IQR) | 30 (28 to 33) |
| ASA grade, n (%) | |
| I | 3 (3.4) |
| II | 49 (55.0) |
| III | 36 (40.4) |
| IV | 1 (1.2) |
| Indication | |
| Aseptic loosening with ligamentous instability, n (%) | 35 (39.4) |
| Instability (incompetent MCL), n (%) | 15 (16.8) |
| Subluxation/dislocation (posterior capsular failure), n (%) | 3 (3.4) |
| Stiffness, n (%) | 1 (1.1) |
| Implant fracture, n (%) | 1 (1.1) |
| Malalignment, n (%) | 1 (1.1) |
| Infection, n (%) | 33 (37.1) |
| Two-stage | 31 (34.8) |
| Single-stage | 2 (2.2) |
-
ASA, American society of Anesthesiologists; IQR, interquartile range; MCL, medical collateral ligament.
The mean follow-up was 7.4 years (2 to 16). The overall rate of reoperation for any cause was 10.1% (n = 9) with rate of implant revision of 6.7% (n = 6; Table II and Table III). There were three reoperations (two infection, one patella instability) and six component revisions: three infections, one extensor mechanism failure, one instability, and one aseptic loosening (Table III).
Table II.
Complications, reoperations, and ten-year implant survivorship results.
| Outcome | Total |
|---|---|
| Patients/knees, n | 89 |
| Mean follow-up, yrs (range) | 7.4 (2 to 16) |
| Reoperation, n (%) | |
| Any cause | 9 (10.1) |
| Component revision | 6 (6.7) |
| Ten-year implant-survivorship, % | 93.3 |
Table III.
Reoperation for any cause.
| Pt | Age (yrs), sex | BMI, kg/m2 | ASA grade | Indication | Time to reoperation, yrs | Cause | Component revision | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 | 77, M | 31 | III | Second stage; PJI | 0.5 | PJI, DAIR | No | 1.4 yrs, death |
| 2 | 81, F | 32 | III | Second stage; PJI | 0.6 | PJI, DAIR | No | 9.5 yrs, no further surgery |
| 3 | 78, M | 27 | II | Second stage; PJI | 2.8 | PFJ instability, no component revision | No | 6.6 yrs, no further surgery |
| 4 | 81, M | 30 | II | Second stage; PJI | 3.0 | PJI, extensor mechanism failure | Yes | Implant-arthrodesis |
| 5 | 50, F | 30 | III | Aseptic loosening, instability (Ehlers-Danlos) | 5.0 | Instability, revised with change of poly, then revised to fixed hinge SMILES | Yes | 5.5 yrs, no further surgery |
| 6 | 70, M | 29 | II | Second stage; PJI | 8.7 | PJI, two-stage DFR | Yes | 4.7 yrs, no further surgery |
| 7 | 63 M | 32 | II | Repeat two-stage for presumed PJI | 1.5 | Repeat two-stage DFR | Yes | 2.6 yrs, no further surgery |
| 8 | 75, F | 32 | II | Aseptic loosening, instability | 2.2 | PJI, two-stage DFR | Yes | 10.9 yrs, no further surgery |
| 9 | 80, M | 27 | II | Aseptic loosening, instability | 6.2 | Aseptic loosening femur, revised to DFR | Yes | 5.3 yrs, death |
-
DAIR, debridement, antibiotics and implant retention; DFR, distal femoral arthroplasty; PFJ, patellofemoral joint; PJI, periprosthetic joint infection; SMILES, Stanmore Modular Individualised Lower Extremity System.
Patellofemoral-specific complications
As above, there were one reoperation for patellar instability and one revision with extensor mechanism failure for an overall 2.25% rate of patellofemoral complications requiring surgery.
Survivorship analysis
At ten years, 30 patients had died, leaving a patient survivorship of 70.9%. Kaplan-Meier implant-survivorship analysis, using revision for any cause as an endpoint, showed a 93.3% survival rate at ten years with mean implant survivorship of 9.5 years (95% confidence interval (CI) 9.1 to 9.9) (Figures 2 to 4).
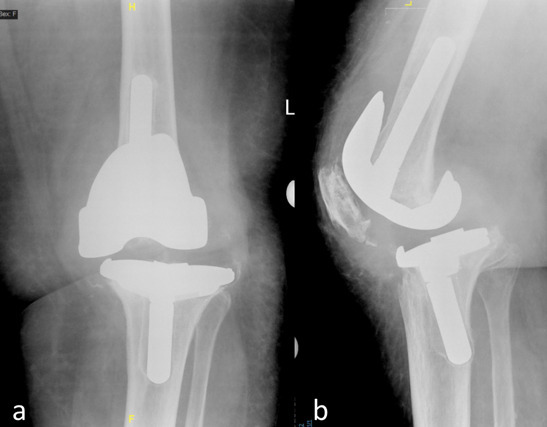
Fig. 2
a) Preoperative anteroposterior and b) lateral radiographs of left knee in an 81-year-old female patient with aseptic loosening and instability.

Fig. 3
Immediate a) anteroposterior and b) lateral radiographs in the same 81-year-old female patient, and c) and d) at seven-year follow-up using S-ROM mobile rotating-hinge with cementless metaphyseal sleeves on both femoral and tibial sides with satisfactory clinical outcomes.
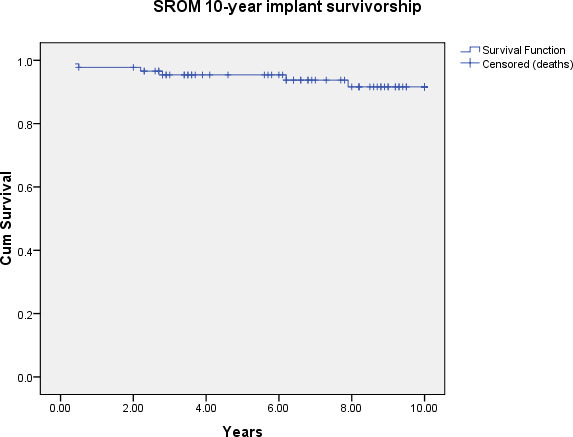
Fig. 4
Kaplan-Meier survival analysis using any cause revision as an endpoint at ten years.
Discussion
In this consecutive series, we present our experience using S-ROM hinge knee implant in rTKA. We report ten-year implant survivorship of 93.3% and approximately 10% complication rate over the entire 17-year study period in this challenging group of patients.
In their recent series, Panesar et al15 reported their outcomes of 99 rTKAs using S-ROM implant (68% aseptic aetiology and 32% infection) at a mean seven years’ follow-up. They reported a 26% complication rate, particularly with patellofemoral disorders, and a 19% revision rate. In our experience, patellofemoral complications with rotating-hinge implants are multifactorial with tibiofemoral rotation, quads tension, position of the hinge mechanism (posterior vs central) with the resulting stress on the soft-tissue envelope anteriorly, and trochlea groove design all playing a role in patellofemoral complications. In the S-ROM design, the flat undersurface of the insert articulates with the flat metal surface of the tibial tray with no inherent resistance to rotation. From a fixation point of view, this complete rotational freedom is advantageous in protecting the fixation interface. However, if the patella starts to track slightly more laterally, the tibial tubercle will externally rotate through the extensor mechanism and the patella drifts more laterally, leading to subluxation and dislocation.
Furthermore, the S-ROM implant is a posterior hinge. If the patellofemoral joint is overstuffed, this leads to excessive tension on the extensor mechanism and the patella not tracking centrally will lead to patella escape or extensor mechanism failure. These potential complications can be avoided by ensuring patella central tracking and appropriate patellofemoral joint tension.
Our recommendations are: restoring the joint line and to avoid overstuffing the patellofemoral joint; b) during trialling stage, ensure that the patella is central in rest extension (adjustments to component rotation helps to optimize this position), and c) ensure that the quads and extensor mechanism have adequate tension by performing gravity flexion. If it is too tight at this stage despite restoring joint line with adequate rotation and central position, the next step is to downsize the femoral component to detension the extensor mechanism.
We have reported high survivorship at ten years, in keeping with contemporary literature. In their recent biomechanical study comparing stresses of constrained condylar knee (CCK) with rotating-hinge implants, Andreani et al24 reported interesting findings where rotating-hinge implant induced high stress compared to the CCK, especially in the region close to tip of the stem. However, higher stresses in the proximal tibia were seen with CCK implant due to the post-cam system, leading to higher implant micromotions due to greater torsional constraint. This was also evident in the dramatic reduction in rates of aseptic loosening with a rotating-hinge compared to a fixed-hinge implant, where those high stresses were dissipated by the rotating-hinge mechanism.11,25 This has led to improved survivorship of contemporary rotating-hinge implants and have become more widely used in complex rTKA practice.
Most published series on contemporary rotating-hinge implants in rTKA have only reported short- to medium-term outcomes (Supplementary Table i).10,26-30 Our study has medium-term follow-up with low complication and revision rates for any cause. However, this study is limited by the retrospective nature of its design and the lack of clinical scores. Finally, although the practice of rTKA in different healthcare systems is variable, this study has a relatively large sample size for this complex group of patients and high internal validity as our data were collected uniformly for all patients and surgical/mortality data was collected nationally, making these findings generalizable. Further, our unit is a specialist tertiary centre with a multidisciplinary team approach ensuring standardization of care.
The S-ROM rotating hinge knee has a high ten-year survivorship and a low complication rate in rTKA. Potential patellofemoral complications can be avoided by ensuring central tracking and appropriate tension of the patellofemoral joint in this posterior hinge design.
References
1. Rodríguez-Merchán EC . Total knee arthroplasty using hinge joints: Indications and results . EFORT Open Rev . 2019 ; 4 ( 4 ): 121 – 132 . Crossref PubMed Google Scholar
2. Jones EC , Insall JN , Inglis AE , Ranawat CS . GUEPAR knee arthroplasty results and late complications . Clin Orthop Relat Res . 1979 ; 140 : 145 – 152 . PubMed Google Scholar
3. Jones GB . Total knee replacement-the Walldius hinge . Clin Orthop Relat Res . 1973 ; 94 : 50 – 57 . Crossref PubMed Google Scholar
4. Lettin AW , Deliss LJ , Blackburne JS , Scales JT . The Stanmore hinged knee arthroplasty . J Bone Joint Surg Br . 1978 ; 60-B ( 3 ): 327 – 332 . Crossref PubMed Google Scholar
5. Murray DG , Wilde AH , Werner F , Foster D . Herbert total knee prosthesis: combined laboratory and clinical assessment . J Bone Joint Surg Am . 1977 ; 59-A ( 8 ): 1026 – 1032 . PubMed Google Scholar
6. Shaw JA , Balcom W , Greer RB . Total knee arthroplasty using the kinematic rotating hinge prosthesis . Orthopedics . 1989 ; 12 ( 5 ): 647 – 654 . Crossref PubMed Google Scholar
7. Walker PS , Emerson R , Potter T , Scott R , Thomas WH , Turner RH . The kinematic rotating hinge: biomechanics and clinical application . Orthop Clin North Am . 1982 ; 13 ( 1 ): 187 – 199 . Crossref PubMed Google Scholar
8. Jones RE , Barrack RL , Skedros J . Modular, mobile-bearing hinge total knee arthroplasty . Clin Orthop Relat Res . 2001 ; 392 : 306 – 314 . Crossref PubMed Google Scholar
9. Barrack RL . Evolution of the rotating hinge for complex total knee arthroplasty Clin Orthop Relat Res . 2001 ; 392 : 292 – 299 . Crossref PubMed Google Scholar
10. Cottino U , Abdel MP , Perry KI , Mara KC , Lewallen DG , Hanssen AD . Long-term results after total knee arthroplasty with contemporary rotating-hinge prostheses . J Bone Joint Surg Am . 2017 ; 99-A ( 4 ): 324 – 330 . Crossref PubMed Google Scholar
11. Myers GJC , Abudu AT , Carter SR , Tillman RM , Grimer RJ . Endoprosthetic replacement of the distal femur for bone tumours: long-term results . J Bone Joint Surg Br . 2007 ; 89-B ( 4 ): 521 – 526 . Crossref PubMed Google Scholar
12. Kouk S , Rathod PA , Maheshwari AV , Deshmukh AJ . Rotating hinge prosthesis for complex revision total knee arthroplasty: a review of the literature . J Clin Orthop Trauma . 2018 ; 9 ( 1 ): 29 – 33 . Crossref PubMed Google Scholar
13. Hintze J von , Niemeläinen M , Sintonen H , Nieminen J , Eskelinen A . Good mid-term outcome of the rotating hinge knee in primary total knee arthroplasty - results of a single center cohort of 106 knees with a median follow-up of 6.3 years . Knee . 2021 ; 28 : 273 – 281 . Crossref PubMed Google Scholar
14. Pasquier G , Ehlinger M , Mainard D . The role of rotating hinge implants in revision total knee arthroplasty . EFORT Open Rev . 2019 ; 4 ( 6 ): 269 – 278 . Crossref PubMed Google Scholar
15. Panesar K , Al-Mouazzen L , Nessa L , Jonas SC , Agarwal S , Morgan-Jones R . Revision total knee arthroplasty using an uncemented metaphyseal sleeve, rotating hinge prosthesis: a case series of 99 patients . J Arthroplasty . 2021 ; 36 ( 6 ): 2121 – 2125 . Crossref PubMed Google Scholar
16. Deehan DJ , Gangadharan R , Malviya A , Sutherland A , Holland JP . Anterior knee symptoms after s-rom hinge implantation . Bull Hosp Jt Dis . 2014 ; 72 ( 2 ): 167 – 172 . ( date last accessed 26 August 2014 ). PubMed Google Scholar
17. Jones RE . Total knee arthroplasty with modular rotating-platform hinge . Orthopedics . 2006 ; 29 ( 9 Suppl ): S80 - 2 . PubMed Google Scholar
18. Jones RE , Skedros JG , Chan AJ , Beauchamp DH , Harkins PC . Total knee arthroplasty using the S-ROM mobile-bearing hinge prosthesis . J Arthroplasty . 2001 ; 16 ( 3 ): 279 – 287 . Crossref PubMed Google Scholar
19. Matar HE , Bloch BV , James PJ . Outcomes of salvage endoprostheses in revision total knee arthroplasty for infection and aseptic loosening: experience of a specialist centre . Knee . 2021 ; 29 : 547 – 556 . Crossref PubMed Google Scholar
20. Matar HE , Bloch BV , James PJ . Distal femoral replacements for acute comminuted periprosthetic knee fractures: satisfactory clinical outcomes at medium-term follow-up . Arthroplast Today . 2021 ; 7 : 37 – 42 . Crossref PubMed Google Scholar
21. Bloch BV , Shannak OA , Palan J , Phillips JRA , James PJ . Metaphyseal sleeves in revision total knee arthroplasty provide reliable fixation and excellent medium to long-term implant survivorship . J Arthroplasty . 2020 ; 35 ( 2 ): 495 – 499 . Crossref PubMed Google Scholar
22. Hirschmann MT , Becker R . The Unhappy Total Knee Replacement . Hirschmann MT , Becker R . Cham : Springer International Publishing , 2015 : 631 – 638 . Crossref Google Scholar
23. Frew NM , Cannon T , Nichol T , Smith TJ , Stockley I . Comparison of the elution properties of commercially available gentamicin and bone cement containing vancomycin with “home-made” preparations . Bone Joint J . 2017 ; 99-B ( 1 ): 73 – 77 . Crossref Google Scholar
24. Andreani L , Pianigiani S , Bori E , Lisanti M , Innocenti B . Analysis of biomechanical differences between condylar constrained knee and rotating hinged implants: a numerical study . J Arthroplasty . 2020 ; 35 ( 1 ): 278 – 284 . Crossref PubMed Google Scholar
25. Ogura K , Fujiwara T , Morris CD , Boland PJ , Healey JH . Long-term competing risks for overall and cause-specific failure of rotating-hinge distal femoral arthroplasty for tumour reconstruction . Bone Joint J . 2021 ; 103-B ( 8 ): 1405 – 1413 . Crossref PubMed Google Scholar
26. Baier C , Lüring C , Schaumburger J , et al. Assessing patient-oriented results after revision total knee arthroplasty . J Orthop Sci . 2013 ; 18 ( 6 ): 955 – 961 . Crossref PubMed Google Scholar
27. Farid YR , Thakral R , Finn HA . Intermediate-term results of 142 single-design, rotating-hinge implants: frequent complications may not preclude salvage of severely affected knees . J Arthroplasty . 2015 ; 30 ( 12 ): 2173 – 2180 . Crossref Google Scholar
28. Hossain F , Patel S , Haddad FS . Midterm assessment of causes and results of revision total knee arthroplasty . Clin Orthop Relat Res . 2010 ; 468 ( 5 ): 1221 – 1228 . Crossref PubMed Google Scholar
29. Joshi N , Navarro-Quilis A . Is there a place for rotating-hinge arthroplasty in knee revision surgery for aseptic loosening? J Arthroplasty . 2008 ; 23 ( 8 ): 1204 – 1211 . Crossref PubMed Google Scholar
30. Smith TH , Gad BV , Klika AK , Styron JF , Joyce TA , Barsoum WK . Comparison of mechanical and nonmechanical failure rates associated with rotating hinged total knee arthroplasty in nontumor patients . J Arthroplasty . 2013 ; 28 ( 1 ): 62 – 67 . Crossref PubMed Google Scholar
31. Giurea A , Neuhaus H-J , Miehlke R , et al. Early results of a new rotating hinge knee implant . Biomed Res Int . 2014 ; 2014 : 948520 . Crossref PubMed Google Scholar
32. Wignadasan W , Chang JS , Kayani B , Kontoghiorghe C , Haddad FS . Long-term results of revision total knee arthroplasty using a rotating hinge implant . Knee . 2021 ; 28 : 72 – 80 . Crossref PubMed Google Scholar
Author contributions
H. E. Matar: Conceptualization, Methodology, Project administration, Data curation, Formal analysis, Writing – original draft.
B. V. Bloch: Conceptualization, Methodology, Writing – review & editing.
P. J. James: Conceptualization, Methodology, Supervision, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research. Open access fees was provided by the Harlow Wood Reserach Fund, a local research charity managed by Nottingham University Hospitals NHS Trust.
Ethical review statement
Local study approval was obtained.
Open access funding
Open access fees was provided by the Harlow Wood Research Fund, a local research charity managed by Nottingham University Hospitals NHS Trust.
Follow B. V. Bloch @Bloch_Ortho
Follow Nottingham Hip & Knee @NottsHipKnee
Supplementary material
Summary of published studies on contemporary rotating-hinge implants in revision knee arthroplasty.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









