Abstract
Aim
Restarting elective services presents a challenge to restore and improve many of the planned patient care pathways which have been suspended during the response to the COVID-19 pandemic. A significant backlog of planned elective work has built up representing a considerable volume of patient need. We aimed to investigate the health status, quality of life, and the impact of delay for patients whose referrals and treatment for symptomatic joint arthritis had been delayed as a result of the response to COVID-19.
Methods
We interviewed 111 patients referred to our elective outpatient service and whose first appointments had been cancelled as a result of the response to the COVID-19 pandemic.
Results
Patients reported significant impacts on their health status and quality of life. Overall, 79 (71.2%) patients reported a further deterioration in their condition while waiting, with seven (6.3%) evaluating their health status as ‘worse than death’.
Conclusions
Waiting lists are clearly not benign and how to prioritize patients, their level of need, and access to assessment and treatment must be more sophisticated than simply relying on the length of time a patient has been waiting. This paper supports the contention that patients awaiting elective joint arthroplasty report significant impacts on their quality of life and health status. This should be given appropriate weight when patients are prioritized for surgery as part of the recovery of services following the COVID-19 pandemic. Elective surgery should not be seen as optional surgery—patients do not see it in this way.
Introduction
The response to the coronavirus-19 (COVID-19) pandemic required an immediate increase in acute care capacity across the globe for what was expected to be an unprecedented number of critically ill patients. This necessitated a pause for all but the most urgent planned elective care and a focus on immediate acute and critical care only. The effects are global and far-reaching. As we ‘reset and recover’ from a period where all healthcare systems and resources have been redirected to focus on an emerging global pandemic, we must now consider how best to reintroduce elements of planned care. How to prioritize patients is a difficult problem. A fair, equitable, clinical, and risk-based system seems intuitively what we should aim for but as in all healthcare systems, there are competing clinical priorities.
It is logical that patients with life-threatening cancers and other critical illnesses should be given priority, but it is important not to underestimate the burden and significant impact on the quality of life for patients who are awaiting planned surgery and procedures for other reasons. It has been reported that up to one-fifth of patients awaiting joint arthroplasty surgery are in a health state ‘worse than death’.1 This is a powerful statement and particularly relevant when balancing up the risks and benefits of undertaking planned elective surgery in the setting of COVID-19. The limited evidence available suggests that for many patients, the outcomes of surgery may be significantly worse if they develop COVID-19 pneumonia in the perioperative period.2 However, for some patients in a ‘worse than death’ state, the risks may be acceptable.
We undertook a study to evaluate the health status and quality of life for patients scheduled for their first outpatient assessment for major joint arthritis and/or joint arthroplasty surgery and whose appointments had been cancelled or deferred as a result of the response to the COVID-19 pandemic. We hoped that this information would be helpful in establishing patient need and priority as planned elective services are restarted.
Methods
We reviewed all adult patients referred to the elective orthopaedic service and with first appointments that were cancelled or deferred at the height of the COVID-19 pandemic between 18 March and 13 May 2020. The orthopaedic service is based in an urban teaching hospital environment with a well-defined catchment area, taking referrals locally and regionally. The electronic patient record and referral documentation were reviewed for each patient. The patients were then contacted by a trained interviewer and invited to complete the EuroQol five-level five-dimension (EQ-5D-5L) assessment.3 Formal ethical approval was not required for this study as it was undertaken as a clinical audit and service evaluation approved by our institutional board. All patients provided informed consent as to their participation and the publication of results.
The EQ-5D-5L assessment is a tool for assessing health status and quality of life and has been validated for use in a number of conditions including musculoskeletal pathologies.4 It measures five core domains: mobility; self-care; ability to perform usual activities; pain/discomfort; and anxiety/depression. The tool also includes a visual analogue scale (EQ-VAS) which the patient uses to self-rate health status.
The EQ-5D score is converted to an index score out of a maximum of 100. The EQ-VAS is measured on a scale with endpoints labelled ‘the best health you can imagine’ and ‘the worst health you can imagine’ with the result converted to a scale of 0 to 1.0. Higher scores representing better functional status. Negative scores represent a health-status assessment that is ‘worse than death’. In addition to the EQ-5D-5L assessment, each patient was asked to make a subjective assessment as to whether their health status, quality of life, and the symptoms related to their joint arthritis had remained stable, had improved, or had deteriorated since the time of referral for consultation. Patients were asked, "Since you were referred to the outpatient clinic, do you feel that your joint arthritis and the impact it has on your overall health and quality of life has stayed at the same level, got better or got worse?"
Statistical analysis
The software package used for statistical analysis was SPSS v. 21.0 (IBM, Armonk, New York, USA). Results are reported as means, including SDs, or as medians with interquartile ranges where appropriate. Non-parametric data was analyzed using Mann-Whitney U tests to compare differences in continuous variables between groups (sex, deterioration status, referral complaint). The Spearman r was calculated to assess relationships between linear variables. Associations between nominal categorical variables were determined using chi-squared tests or Fisher's exact tests where n < 5. A value of p < 0.05 was considered significant.
Results
In total, 210 eligible patients were identified from the outpatient referrals scheduled over this period. Demographic data (age and sex), the subject of the referral, date of referral from primary care, and date of the first scheduled orthopaedic appointment were recorded. Five (2.4%) patients were excluded because the full patient record and referral information were not accessible. One (0.5%) patient had already undergone surgery privately, 78 (36.7%) patients could not be contacted, and seven (3.3%) patients were unable to participate because of difficulties with language. Two (1%) patients reported that their condition had resolved. Six (3%) patients declined to participate. 111 (52.9%) patients agreed to participate and formed the study group (Table I). Demographics and referral diagnoses were compared for non-responders and the study group and were found to be similar.
Table I.
Numbers of referrals deferred considered by referral complaint/symptomatic joint.
| Symptomatic joint | n (%) |
|---|---|
| Hip | 58 (52.3) |
| Knee | 5 (4.5) |
| Spine | 1 (0.9) |
| Foot/ankle | 31 (27.9) |
| Shoulder | 13 (11.7) |
| Elbow | 3 (2.7) |
The mean age of the 111 patients taking part in the study was 59.2 years old (SD 14.7) and 63 (56.8%) of the patients were women. In total, 79 (71.2%) patients reported that their health and quality of life had deteriorated since the time of their initial referral from primary care. The mean EQ-5D and EQ-VAS scores for these patients are reported in Table II. Patients awaiting assessment for symptomatic hip joint arthritis had poorer scores (Figure 1a and b).
Table II.
Descriptive statistics for sex and self-reported deterioration in health since referral. Patients who self-reported deterioration in health had statistically significant lower mean EuroQol five-dimension assessment (EQ-5D) and EuroQol visual analogue scale (EQ-VAS) scores.
| Variable | n (%) | Mean EQ-5D score (SD) | p-value* | Mean EQ-VAS score (SD) | p-value* |
|---|---|---|---|---|---|
| Sex | 0.662 | 0.948 | |||
| Male | 63 (56.8) | 0.513 (0.311) | 62.0 (18.1) | ||
| Female | 48 (43.2) | 0.484 (0.285) | 63.8 (23.0) | ||
| Self-reported deterioration in health status | < 0.001 | 0.007 | |||
| Yes | 79 (71.2) | 0.420 (0.285) | 59.6 (21.6) | ||
| No | 32 (28.8) | 0.682 (0.216) | 70.6 (17.5) | ||
-
*
Mann-Whitney U test.
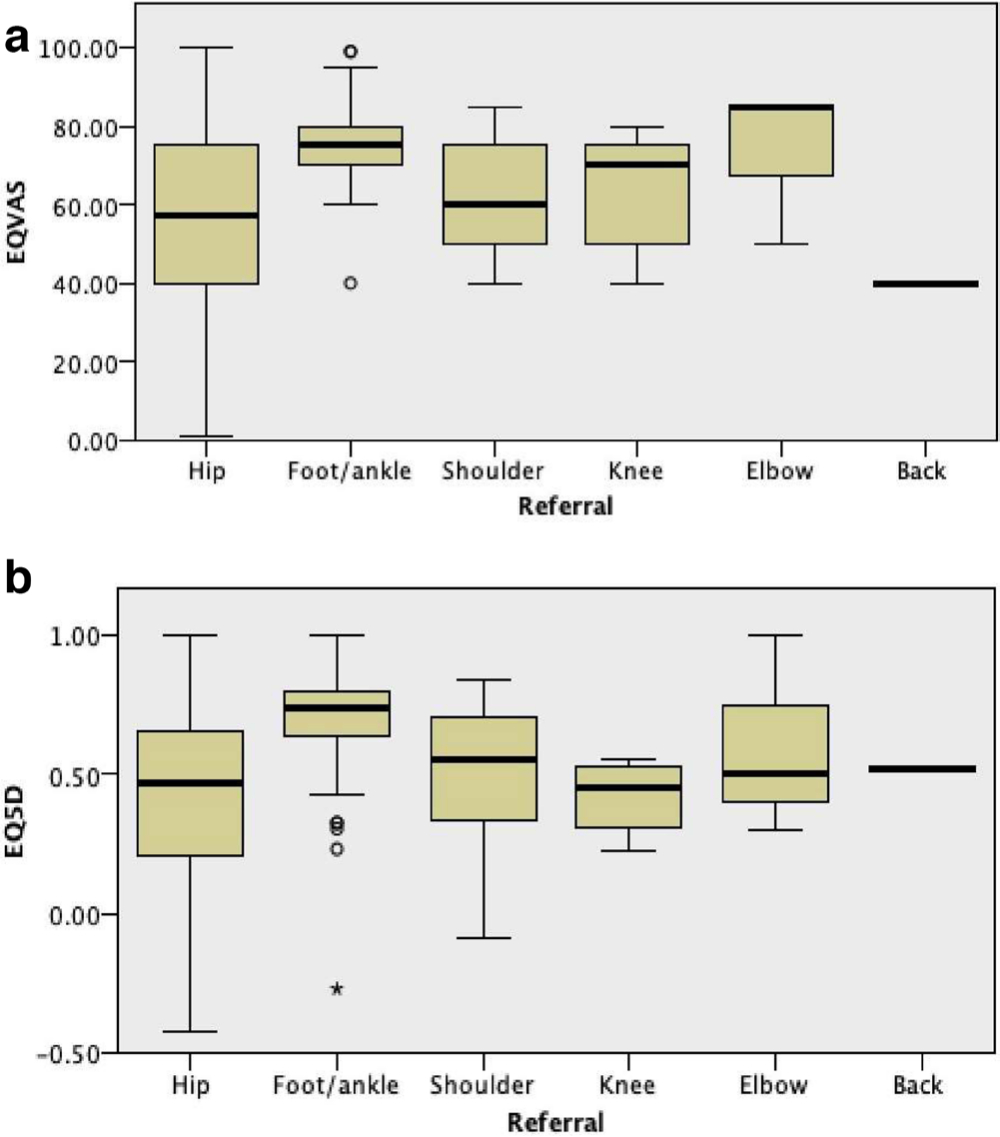
Fig. 1
a) EuroQol visual analogue scale (EQ-VAS) scores represented by referral complaint/symptomatic joint. b) EuroQol five-dimension assessment (EQ-5D) scores represented by referral complaint/symptomatic joint.
Those patients who reported deterioration in their symptoms and quality of life had objectively poorer EQ-5D index scores and EQ-VAS scores. Patient self-reported health status and quality of life rated on a visual analogue scale (VAS) correlated with the EQ-5D-5L score.
Discussion
This study shows that, while not suffering from immediately life-threatening conditions, patients with symptomatic joint arthritis awaiting delayed assessment and treatment as a result of COVID-19 report markedly negative impacts on their health status and quality of life. These impacts may not be as prominent or obvious as for some other pathologies but this does not make them insignificant.
As healthcare systems adapt and recover, plans to restore some of the nonemergent healthcare services are being developed and patients are being prioritized based on an assessment of the urgency of their proposed treatment, the potential harm from further delay ,and the risk of undertaking the treatment in the context of COVID-19. Our study shows that this assessment is complex and the impact of non-fatal but symptomatic joint arthritis on health status and quality of life should not be underestimated.
In total, 79 (71.2%) participants reported that their health had further deteriorated since the time of referral, and seven (8.9%) patients were assessed to be in a functional state ‘worse than death’. This is a remarkable state of poor health and one that may not be easily detected by established clinical prioritization and harm assessment tools based on waiting time and the relative acuity of the relevant pathology. It would be incorrect to attribute this deterioration in health status solely to progression of arthritis and delay in treatment, and just how much of the deterioration is related to progression of arthritis is difficult to establish. An initial functional or health status score from the time of referral would have been helpful in quantifying the absolute level of deterioration in function for the patient. Otherwise, patients may be subject to recall and other biases. Nevertheless, patient reported deterioration in function and overall health status is an important finding as more and more patients wait for assessment and treatment and this delay in treatment has consequences.
Comparing the health status and quality of life scores for the patients awaiting assessment with those reported for patients with common chronic conditions, the mean EQ-5D scores for patients with symptomatic joint arthritis awaiting assessment were worse than those reported for patients with heart failure, diabetes, and chronic obstructive pulmonary disease.4–6 Assessing harm and priority is not necessarily straightforward. In our study, patients were able to reliably self-report deterioration in their health status and quality of life.
An obvious limitation of our study is the fact that we were unable to contact a large number of patients scheduled for assessment in this period. This was despite multiple attempts over an extended period. The methods of contact and review open to us were somewhat limited in view of the social mobility restrictions in place as a result of the pandemic.
A ‘worse than death’ state based on functional scoring does not necessarily mean that a patient would rather be dead, but it is a patient-based assessment of their health status and the impact of their comorbidities and pathologies. This potentially could have relevance for the level of associated risk that patients and clinicians are prepared to accept with elective surgery in the setting of COVID-19.
It is obvious that some form of prioritization is needed to restart elective services and surgery safely and based on need. It is important that this is done in such a way that patients with hidden pathology, health deficits, and poor quality of life are not disadvantaged. Patients with symptomatic joint arthritis are often hidden by the statistics and their needs are not necessarily obvious. Our study shows what many have already come to realise, waiting lists are not benign, and elective surgery does not necessarily mean optional surgery, certainly not for patients who find themselves in a state ‘worse-than-death’. Systems to prioritize patients for planned assessments, procedures, and surgery must be more sophisticated than simply depending on the waiting time and nature of the underlying pathology. The impact of symptomatic joint arthritis on quality of life and health status should not be underestimated when consideration is given to setting clinical priorities.
References
1. Scott CEH , MacDonald DJ , Howie CR . 'Worse than death' and waiting for a joint arthroplasty . Bone Joint J . 2019 ; 101-B ( 8 ): 941 – 950 . Crossref PubMed Google Scholar
2. COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study . Lancet . 2020 ; 396 ( 10243 ): 27 – 38 . Crossref PubMed Google Scholar
3. Janssen MF , Pickard AS , Golicki D , et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study . Qual Life Res . 2013 ; 22 ( 7 ): 1717 – 1727 . Crossref PubMed Google Scholar
4. Gallagher AM , Lucas R , Cowie MR . Assessing health-related quality of life in heart failure patients attending an outpatient clinic: a pragmatic approach . ESC Heart Fail . 2019 ; 6 ( 1 ): 3 – 9 . Crossref PubMed Google Scholar
5. Pickard AS , Wilke C , Jung E , et al. Use of a preference-based measure of health (EQ-5D) in COPD and asthma . Respir Med . 2008 ; 102 ( 4 ): 519 – 536 . Crossref PubMed Google Scholar
6. Nauck MA , Buse JB , Mann JFE , et al. Health-related quality of life in people with type 2 diabetes participating in the leader trial . Diabetes Obes Metab . 2019 ; 21 ( 3 ): 525 – 532 . Crossref PubMed Google Scholar
Author contributions
J. A. Morris: Designed the study, Co-ordinated the project, Wrote and edited the manuscript.
J. Super: Recruited and surveyed the patients, Analyzed and presented the data, Edited the manuscript.
D. Huntley: Recruited and surveyed the patients, Edited the manuscript.
T. Ashdown: Recruited and surveyed the patients, Edited the manuscript.
W. Harland: Recruited and surveyed the patients, Edited the manuscript.
R. Anakwe: Supervised the study, Recruited and surveyed the patients, Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Follow R. Anakwe @VirtualFracClin
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









