Abstract
Aims
This study aims to evaluate a new home medical stretching device called the Self Treatment Assisted Knee (STAK) tool to treat knee arthrofibrosis.
Methods
35 patients post-major knee surgery with arthrofibrosis and mean range of movement (ROM) of 68° were recruited. Both the STAK intervention and control group received standard physiotherapy for eight weeks, with the intervention group additionally using the STAK at home. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and Oxford Knee Scores (OKS) were collected at all timepoints. An acceptability and home exercise questionnaire capturing adherence was recorded after each of the interventions.
Results
Compared to the control group, the STAK intervention group made significant gains in mean ROM (30° versus 8°, p < 0.0005), WOMAC (19 points versus 3, p < 0.0005), and OKS (8 points versus 3, p < 0.0005). The improvements in the STAK group were maintained at long-term follow-up. No patients suffered any complications relating to the STAK, and 96% of patients found the STAK tool ‘perfectly acceptable’.
Conclusion
The STAK tool is effective in increasing ROM and reducing pain and stiffness. Patients find it acceptable and adherence to treatment was high. This study indicates that the STAK tool would be of benefit in clinical practice and may offer a new, cost-effective treatment for arthrofibrosis.
Cite this article: Bone Joint Open 2020;1-8:465–473.
Introduction
Arthrofibrosis leading to poor outcome after total knee arthroplasty (TKA) is a growing problem worldwide.1 Overall, 112,836 knee arthroplasty procedures are performed each year in the UK2 and 700,000 in the USA3 at a total annual cost of around $10.2 billion in the USA.4 Due to obesity and longevity, this is expected to increase six-fold to 672,0005 and 4,200,000 respectively by 2030;6 alongside this, the demand for better outcomes will continue to rise.
Stiffness following TKA is common, occurring in between 5% and 30% of patients.7 It accounts for 28% of hospital readmissions due to surgical complications within 90 days of discharge and 10% of all revisions within five years of initial surgery.8,9 Stiffness is the primary cause of dissatisfaction with approximately 20% of patients being severely dissatisfied following TKA.10 This rate of dissatisfaction is consistently reported across countries.11 Poor medium- to long-term patient outcomes following TKA are consistent between studies with only 50% of patients having a clinically important improvement in pain stiffness and function on the validated patient self-reported outcome measure (Western Ontario and McMaster Universities Osteoarthritis Index score; WOMAC) a year after surgery.12
The process of arthrofibrosis involves abnormal scarring of the joint caused by an exaggerated inflammatory response. It leads to loss of range of movement (ROM), oedema, pain, muscle weakness, and functional disability. Arthrofibrosis limits patients’ ability to perform basic activities of daily living and contributes to chronic diffuse knee pain severely impairing a patient’s quality of life.13 Biomechanical studies show patients require 67° ROM for walking on the flat, 90° to 100° to manage stairs, 95° to stand from a chair, 105° to tie shoelaces, up to 120° to ride a bike, 135° to get out of a bathtub, and kneeling, squatting, and sitting cross-legged require over 150° ROM.14,15 Research shows < 90° ROM leads to significant patient dissatisfaction and ongoing pain from the cause of stiffness.16
Conventional treatment is aggressive physiotherapy, progressing to manipulation under anaesthetic (MUA) or arthroscopic debridement if 90° flexion is not attained within six to 12 weeks post-surgery.17 MUA after primary TKA has been reported in up to 12% of patients and is a costly complication with some degree of risk attached to the procedure.16 MUA can lead to impressive increases in ROM18; however, initial gains may not be maintained19 and further surgery to restore ROM may be required with only 37% of these reporting satisfactory results.20 Patients undergoing MUA also have twice the rate of revision surgery measured at seven to ten years post-primary TKA.21
Standard physiotherapy includes joint mobilizations and passive stretches where force is applied to the joint at its end of range by the physiotherapist to improve ROM.22,23 Although high-grade mobilizations may result in immediate improvements in ROM, these gains have been reported to be only temporary.24
Regular high-intensity or prolonged stretching is required to achieve plastic deformation facilitating collagen fibres to be remodelled lineally in response to the lines of stress, resulting in permanent elongation of the tissue.25
As part of standard physiotherapy, exercise sheets involving active assisted movement (self-applied over pressure using the patients contralateral unaffected limb) plus knee strengthening, stretching and functional exercise are also prescribed for patients to complete at home.22,26 However, home exercises have been found to produce less than 10% of the torque applied by a physiotherapist.27
Home mechanical stretching devices can improve ROM and clinical outcomes by enabling patients to treat themselves daily.28 There are two distinct kinds of stretching devices; high intensity stretch (HIS), displacement-control devices where tissues are placed under a large amount of stress near the end range of the joints movement.29 Low-intensity stretching (LIS) devices use the technique known as creep-loading or load-control. This involves a low load, constant, prolonged force over an extended period, such as between eight and 12 hours. Displacement control devices require much shorter treatment times and provide greater levels of patient acceptability and compliance to treatment.
Studies using displacement control devices have achieved significant ROM increases.30-33 The former two studies achieving the greatest gains in ROM used a patient-actuated serial stretch HIS (PASS) device which was found to apply the greatest force,27,34 require the shortest treatment time of 60 minutes a day and led to a reduced rate of additional surgery.20 Although current devices on the market are a good start for a home solution, current devices on the market either require custom fitting, are cumbersome for home use and come with a significant price tag.
The purpose of this research is to assess the impact of eight weeks treatment at home using the Self Treatment Assisted Knee (STAK) tool, a PASS HIS medical stretching device, on patients’ ROM, pain, stiffness and function (WOMAC and Oxford Knee Score (OKS) at eight weeks and at long-term follow-up. It also seeks information on the acceptability of the device to patients. This study will test the hypothesis that changes in ROM, WOMAC, and OKS will significantly differ from baseline to follow-up after using the STAK tool plus standard physiotherapy for eight weeks compared to the control group receiving standard physiotherapy alone for eight weeks and that the improvements in the STAK Intervention group will be maintained at long-term follow-up.
Methods
All study participants provided written informed consent. The study methodology utilized a block allocation strategy. 35 participants (15 males, 64 years ± 11 years, 177 cm ± 6 cm, 95 kg ± 14 kg; and 20 females, 64 years ± 7 years, 161 cm ± 6 cm, 80 kg ± 17 kg) with < 80° ROM or that had been prescribed intensive physiotherapy for stiffness by their surgeon were recruited consecutively into two groups. Sample size estimation was done in G*Power software (Heinrich-Heine-Universität Düsseldorf, Germany). Based on a previous study’s32 power calculation to attain 80% power at a level of significance to 0.05 in a two tailed test with mean changes in ROM of 17° and 29.9° and pooled standard deviation (SD) 10° an effect size of 1.2 was produced and a suggested sample size of 24. To be cautious we reduced the anticipated effect size in our study to 0.99 calculating the estimated required sample size to be 34. 20 participants were allocated into the STAK device intervention group and a subsequent 15 allocated to the control group (see Figure 1). The groups were not quite fully balanced in their numbers as two dropouts in the intervention group were back filled (as per protocol), the overall target sample of 34 was attained on recruitment of the 14th participant into the control group.
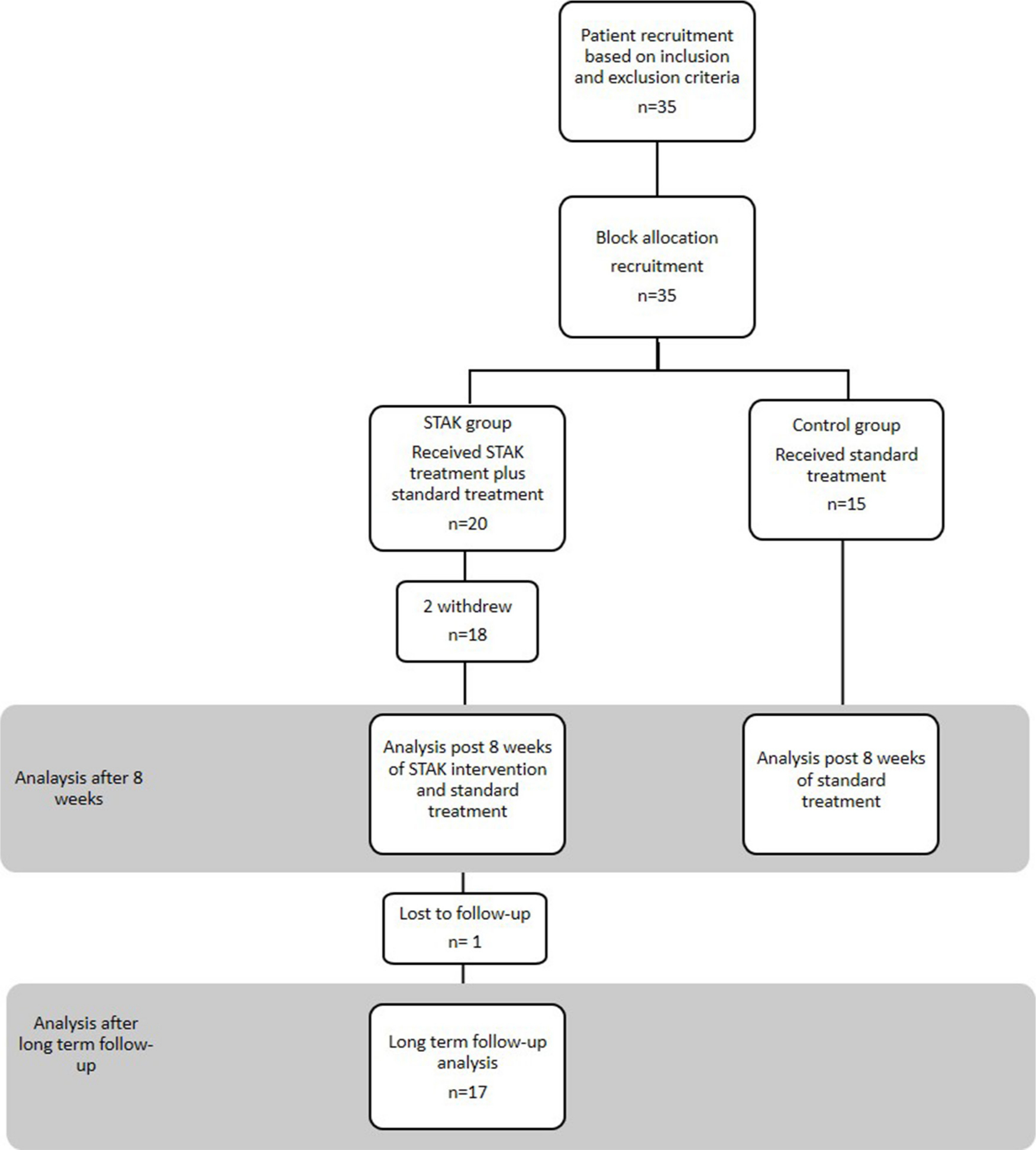
Fig. 1
Flowchart demonstrating patient recruitment, allocation and follow-up.
The intervention group included 16 primary TKA, one unicompartmental knee, one patella fracture; the control group comprised 12 primary TKA, one revision TKA, one knee dislocation, and one patella fracture. All patients were recruited from a caseload of 15 knee surgeons’ at UHL NHS trust. Patients were excluded if they had leaking wounds or infected joints, preoperative flexion < 90°, were post malignancy or the surgeon felt the patient was at risk of postoperative fracture, if they fell outside a weight of 44 kg and 159 kg or were unable to give consent themselves.
Interventions
In addition to standard physiotherapy, patients in the intervention group also used the STAK tool daily at home for eight weeks. STAK is a non-motorized medical stretching device similar to a patient actuated serial stretch (PASS) that incorporates the principles of stress relaxation, with a series of high-intensity stretches at end range applied for a short duration. The patient has full control over the intensity and duration of the stretch. While seated in a chair, the patient places their foot into the STAK tool which is set to the limit of their current knee flexion ability. The patient then applies force using their body weight and leverage to stretch their knee to the limit of their pain threshold at their end range of movement holding the stretch for as long as they feel able (approximately five minutes). The intense long stretch allows the collagen fibres to achieve plastic deformation, realign and lengthen. Participants were required to stretch for a total of 60 minutes each day.
This stretching protocol is similar to those used effectively by Noyes and Barber-Westin (2010)35 and Davies and Ellenbecker (1999).23 The STAK tool has a motivational scale which provides feedback for patients on their progress in gaining ROM (see Figure 2). Following the intervention periods, both the groups were asked to complete a home exercise questionnaire. This captured adherence to treatment, duration/intensity of stretch (dose). Patients were telephoned once a week to check there were no problems using the device. Patients in both the intervention and control group received standard physiotherapy treatment for the eight week treatment period. Standard physiotherapy treatment included stretching, range of movement and strengthening exercises, gait training and education, a home exercise programme and if required hydrotherapy and land-based classes. The physiotherapist altered the treatment of arthrofibrosis depending on individual patient’s needs. The mean frequency of treatment was one treatment every two weeks.

Fig. 2
Photograph of the STAK showing the scale and adjustable footplate.
Outcomes
Both groups had knee ROM, WOMAC, and OKS recorded before and after the eight-week treatment period and the STAK group was re-measured at long-term follow-up (minimum seven months). The OKS and WOMAC are well validated patient reported outcome measures demonstrating strong validity, reliability and sensitivity to change in TKA populations and patients undergoing lower limb rehabilitation.36,37 A high WOMAC score indicates extreme pain/dysfunction, conversely a low OKS score indicates extreme pain/difficulty. A home exercise questionnaire was completed by patients at the end of the eight-week intervention period to capture their compliance to the treatments and an acceptability questionnaire was administered to quantify their views on the STAK tool’s acceptability.
The primary outcome measure was active ROM which was measured using a 12” universal goniometer in a standardized procedure with the participant seated in a chair. A photographic record and measure were also taken using the Hudl Ubersense smartphone app (Agile Sports Technologies, Lincoln, Nebraska, USA) (see Figure 3). A recent study has found the app to have high levels of concurrent validity and intra-rater reliability demonstrating a mean 0.80° difference in a study comparing 40 knee measurements to the gold standard measuring instrument the electrogoniometer.38 Naylor et al’s (2011)39 evidence based standardized method for identifying bony landmarks was employed, including marking the distal flare of the lateral malleolus, the centre of rotation of the knee and the proximal flare of the greater trochanter. The assessor visually checked the knee joint was in the sagittal plane ensuring a 2D image was photographed. The same physiotherapist (SKA) recorded all ROM measurements for each patient, angles were randomly double checked by a blinded third-party clinician.
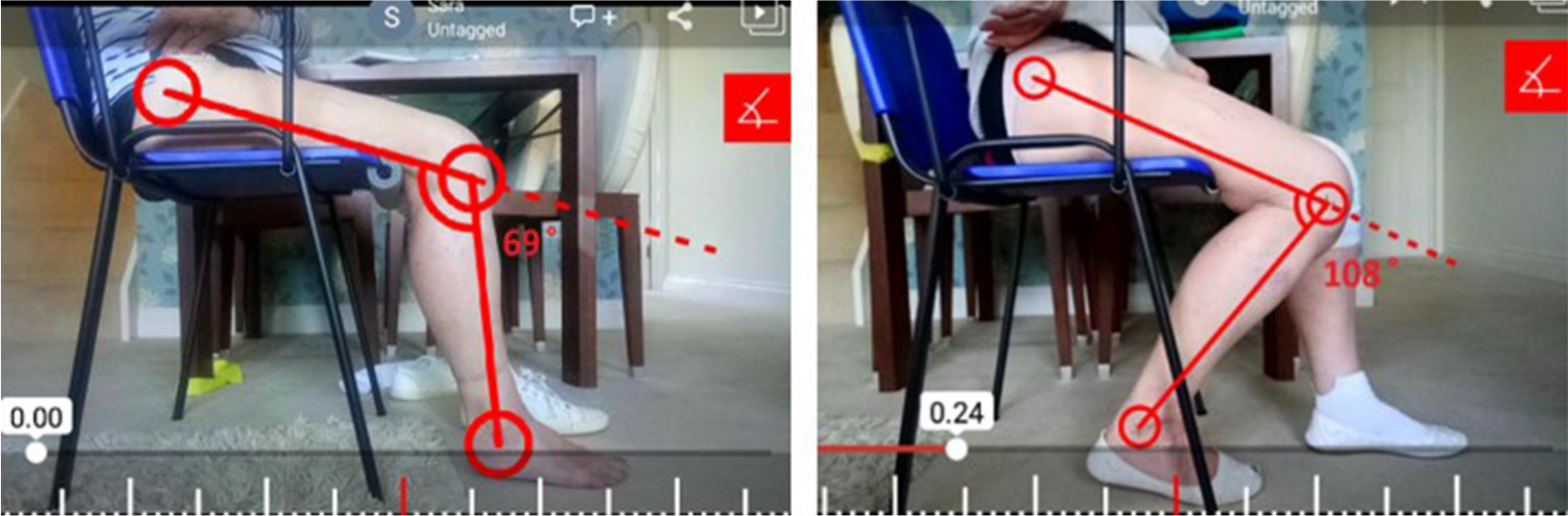
Fig. 3
Patient ROM measured by Hudl Ubersense smartphone app.
After the eight weeks treatment period, patients in the intervention group were asked to rate the acceptability of the STAK. This involved marking responses to three questions (one on a seven-point and two on five-point Likert scales), where one denotes a negative response (completely unacceptable) and seven denotes a positive response (perfectly acceptable).
Statistical analysis
Variables with the potential to effect results were limited as both groups comprised similar participants in terms of age, sex, body mass index, pre-treatment ROM, OKS, and WOMAC scores. The STAK intervention group and standard physiotherapy control groups’ ROM, OKS and WOMAC score data were normally distributed. The pre- to post-treatment and post STAK treatment to long-term follow-up ROM, OKS, and WOMAC were analyzed using a paired t-test. The difference in the change in the intervention and control group was analyzed using an independent t-test. Pearson’s product-moment correlation coefficients were calculated to determine the relationship between knee ROM and the OKS and WOMAC scores. Variables were also assessed by age, sex and length of time from onset of stiffness to treatment to determine whether any of these factors were associated with change in range of movement. All statistical analyses were performed with the SPSS 25.0 (IBM, Armonk, New York, USA). Patient scores of acceptability and likelihood of recommendation are described using appropriate summary statistics. The home exercise questionnaires provide information regarding adherence including frequency and intensity of STAK and home stretching exercises completed.
Results
Participant demographics, baseline measures of ROM, OKS, WOMAC score and time from surgery to entering the study were compared at baseline and no statistically significant differences between the groups were identified (see Table I). All TKAs had been performed to manage osteoarthritis. Patients were recruited at a mean of 26 weeks post-surgery in the intervention and following a mean of 20 weeks in the control group. In all, 20 patients received the STAK intervention at home in addition to standard physiotherapy and 15 patients received the control intervention receiving physiotherapy alone.
Table I.
Comparison of patient age, BMI, and length of time from surgery to entering the study (mean ± SD) between knee stretching device and control group.
| Variables | STAK group, mean ± SD (range) | Control group, mean ± SD (range) | p-value |
|---|---|---|---|
| Age (years) | 62 ± 8 (49 to 79) | 67 ± 8 (54 to 81) | 0.067* |
| BMI (kg/m2) | 31 ± 7 (23 to 53) | 30 ± 5 (23 to 39) | 0.331* |
| Sex (female:male) | 11:9 | 9:6 | 0.771† |
| Time from surgery to entering study (weeks) | 26 ± 20 (8 to 67) | 20 ± 22 (6 to 87) | 0.358* |
| Baseline | |||
| ROM (°) | 66 ± 9 | 71 ± 11 | 0.132* |
| OKS | 20 ± 9 (6 to 40) | 20 ± 7 (9 to 30) | 0.985* |
| WOMAC | 54 ± 14 (26 to 70) | 51 ± 13 (29 to 73) | 0.488* |
-
STAK, Self Treatment Assisted Knee; SD, standard deviation; BMI, body mass index; ROM, range of movement; OKS, Oxford Knee Score; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
-
*
Independent samples t-test.
-
†
Chi-squared.
There were two withdrawals from the STAK intervention group during the eight-week treatment period due to family commitments and illness (unrelated to the intervention). One patient was not contactable at long-term follow-up (see Figure 1).
The STAK intervention group made significant gains in ROM (mean 30°) compared to control group (8°) (p < 0.0005). The STAK made significant improvements in WOMAC (19 points) versus controls (3 points) (p < 0.0005) (see Figure 4). This was also supported by significant improvements in OKS (8 points) versus controls (3 points) p < 0.0005). (See Table II for details including SD, range, p-values).
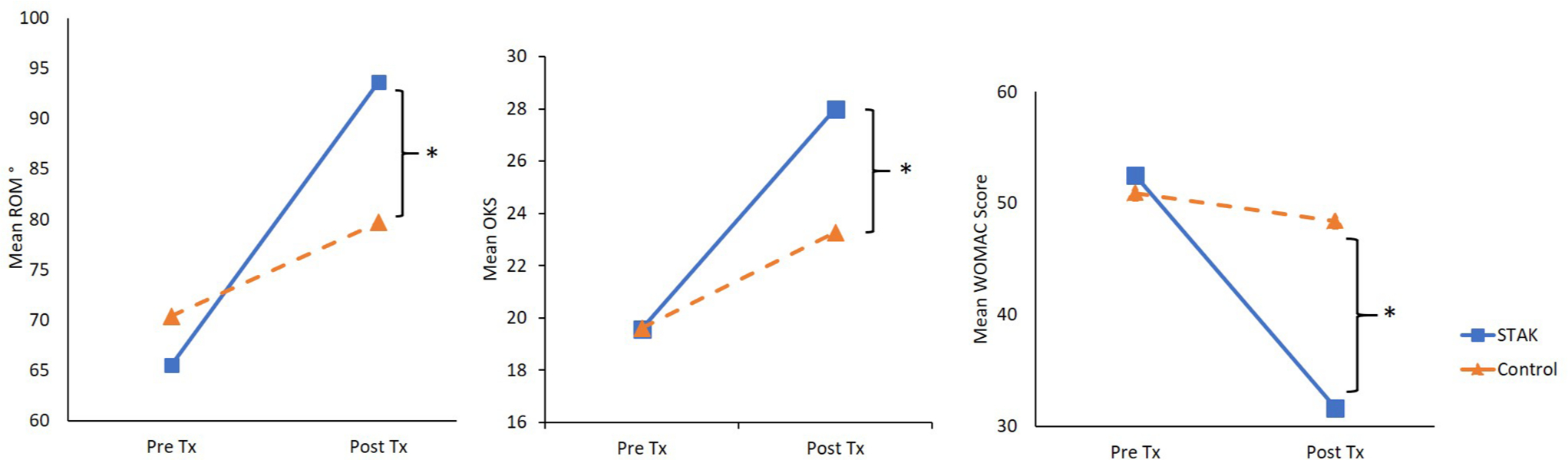
Fig. 4
Mean ROM, OKS, and WOMAC before and after eight-week treatment period (Tx) - STAK versus standard treatment. A high WOMAC score indicates extreme pain/dysfunction, a low OKS score indicates extreme pain/difficulty *The STAK group demonstrated a significantly larger mean improvement in ROM, WOMAC, and OKS (p < 0.0005).
Table II.
Range of movement, OKS, and WOMAC before and after treatment with STAK compared to standard treatment control group.
| STAK group | Control group | |||||
|---|---|---|---|---|---|---|
| Variable | Preoperative, mean ± SD |
Postoperative, mean ± SD |
Change, mean ± SD |
Preopeative, mean ± SD |
Postoperative, mean ± SD |
Change, mean ± SD |
| ROM° Goniometer | 65° ± 9°(44 to 75) | 95° ± 9° (78 to 110) | 30°* (12 to 50) p < 0.0005 | 71° ± 11° (49 to 93) | 79° ± 14° (42 to 93) | 8* (-7 to 36) p = 0.004 |
| ROM° app | 65° ± 9° (44 to 75) | 96° ± 9° (81 to 111) | 31°* (12 to 50) p < 0.0005 | 71° ± 11° (49 to 93) | 79° ± 14° (43 to 96) | 8°* (-7 to 37) p = 0.004 |
| WOMAC | 52 ± 16° (26 to 70) | 33 ± 18 (29 to 68) | 19* (4 to 49) p < 0.0005 | 51 ± 13 (29 to 73) | 48 ± 15 (21 to 72) | 3* (-23 to 19) p = 0.390 |
| OKS | 20 ± 9°(6 to 40) | 28 ± 10 (6 to 44) | 8* (0 to 20) p < 0.01 | 20 ± 7 (9 to 30) | 23 ± 9 (11 to 37) | 3* (-6 to 17) p = 0.051 |
-
*
p < 0.0005; STAK group mean change significantly greater than control group change.
-
STAK, Self Treatment Assisted Knee; SD, standard deviation; ROM, range of movement; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index; OKS, Oxford Knee Score.
Reliability of the results is strengthened by very strong positive correlation between the measurements taken with the Hudl App and universal goniometer with a correlation co-efficient of r = 0.991; p = 0.0005. (Correlation is significant at p < 0.01 level). Two patients in the STAK intervention group had previously failed to improve ROM after both extensive physiotherapy and MUA with ROM of only 44° and 73°, but following use of the STAK for eight weeks they achieved 94° and 103° with changes of 50° and 29° respectively (see Figure 5).

Fig. 5
Patient who achieved increase of 50° ROM using the STAK after failed manipulation under anaesthetic.
Discussion
Long-term follow-up
Patients in the STAK intervention group maintained their ROM, WOMAC, and OKS at long-term follow-up (mean 10.5 months, (7 to 15); mean 16 months post-surgery (10 to 24). ROM fell by mean 2° to 93° (p = 0.644), WOMAC improved by mean 2 points to 31 points (p = 0.410). OKS also improved by 2 points to a mean score of 30 (p = 0.291). One patient who achieved 94° following the STAK treatment may have later regressed her ROM as her surgeon felt MUA was still necessary. At long-term follow-up (ten months post starting the STAK treatment (one-year post-TKA) she had 98°.
Adherence and dose
Analysis of home exercise questionnaires showed participants from both groups adhered to their intervention, although adherence was higher in the STAK intervention group with patients using the STAK for an average three times a day at a ‘very intense’ level of stretch for average 13 mintes per session for seven days a week. While the control completed the home exercises on average twice a day at a ‘moderate intensity’ level of stretch for 14 minutes per session for 4.8 days a week. This adds up to a much lower total end range time (TERT) dose in the control standard physiotherapy group.
Acceptability
Acceptability of the STAK tool intervention was high with a mean score of 6.8 out of a possible 7 and 96% acceptability for the question, ‘how acceptable did you find the STAK tool?’, 98% of patients were ‘extremely likely’ to ‘recommend the STAK to a friend’, and 93% of patients felt the STAK was wholly responsible for their change in knee ROM. No adverse events relating to either of the interventions were reported.
Discussion
The purpose of this initial trial was to compare the effectiveness of home use of the STAK (PASS HIS device) and standard physiotherapy compared to standard physiotherapy treatment alone in a sample of patients with severe arthrofibrosis, and to assess the long-term outcomes following the STAK intervention. The hypothesis was accepted as the HIS STAK intervention achieved significantly greater improvements in ROM (p < 0.0005) and patient reported outcome measures (WOMAC (p < 0.0005), OKS (p < 0.0005) and maintained these at long-term follow-up (mean 10.5 months from starting the STAK intervention).
The ROM scores correlate closely with the WOMAC (r = -4.17; p = 0.008) and OKS (r = −3.333; p = 0.016) and it is likely that the mean increase in ROM of 30° in the intervention group resulted in reduced pain and stiffness and improved function measured in WOMAC and OKS scores (mean improvement 19 and 8 points respectively). Poor flexion ROM is the primary reason for poor satisfaction following TKA26 and symptoms of stiffness are associated with lower function.40 In clinical practice if 90° ROM is not attained an MUA is often performed.41 66% of patients in the STAK intervention group achieved ROM over 90° (mean increase 30°). Patients in our study had very poor ROM (mean 65°) with 69% of the sample starting with 70° ROM or less. Seven patients had undergone MUA without significant improvement with ROM below 78°. Further MUA or revision knee arthroplasty surgery may have been required, however the two patients who used the STAK increased their ROM by 50° and 29° in eight weeks. This eliminated the need for a further MUA and the associated risks and complications (fracture wound dehiscence, patella ligament avulsions, hemarthrosis, and pulmonary embolism)28,32 as well as making considerable cost savings to the NHS. MUAs are expensive requiring an overnight stay in hospital costing £4,30042, revision surgery costs approximately £30,01143 and 20% to 25% do not result in lasting gains in ROM.44
The intervention group using the STAK tool improved their OKS score by 8 points, and the control group by only 3 points. An improvement of over 4.3 is regarded as a clinically relevant improvement after TKA.45 The control group is below this threshold whereas the STAK group exceedes this which in this group of patients with extreme arthrofibrosis is exceptional. All patients stated that they would have liked use of the STAK on discharge from hospital and considered it would have prevented development of their arthrofibrosis.
This study demonstrates that the STAK HIS device significantly improves patients’ ROM, pain stiffness, and function even in the most severe arthrofibrosis patients when intensive standard physiotherapy and possibly even MUA has failed. Improvements in ROM compare favourably over research using the JAS knee device (Joint Active Systems, Effingham, Illinois, USA) (median 19° flexion33 and mean 24° flexion30 and also in comparison with published increases in ROM following MUA (mean 26.5°, 0° to 80°).46 The current study supports other research finding HIS home mechanical therapy devices work more effectively than physiotherapy alone.20,31,32,47 Stretching theory supports this as HIS devices apply forces to the joint that are similar to those applied by physiotherapists, whereas force generated by home exercises is much lower.27 Applying too low a force (home exercises), or applying force for too short of a period of time (biweekly physiotherapy session) produces elastic deformation that does not correspond with a lasting change in ROM.23,29,48 Research involving 60,000 patients with knee arthrofibrosis found HIS PASS devices had a lower risk of hospital readmissions compared to low intensity stretch (LIS) devices20 and groups receiving standard physiotherapy were 71% more likely to require revision surgery compared with the HIS device users.20
The STAK enables the patient to use their own body weight and leverage to generate the HIS and have finely adjustable control over their stretch. The short duration stretch is better tolerated and limits damage to the tissue as the patient actuates the device to the limit of their pain threshold.31 This together with the motivational scale providing feedback on progress enables and empowers patients to take control of their rehabilitation increasing self-efficacy. This is supported by the high adherence rates captured by the home exercise and acceptability questionnaires. Research in the joint arthroplasty field has found higher levels of postoperative self-efficacy lead to better longer term outcomes49 and enhance adherence to home exercises.50 This current study indicates the STAK programme achieves this and maintains these improvements at long term follow-up (mean 10.5 months (7 to 15), which made patients a mean 16 months post-surgery (10 to 24).
Limitations
The study did not formerly randomize the sample. The first 20 patients were allocated to the intervention group and the next available 15 to the control. Although a traditional randomization procedure was not conducted analysis reveals no significant difference in patient demographics or baseline characteristics including ROM, OKS, and WOMAC scores between the groups (see Table II). Physiotherapists carrying out standard treatment were blinded to the research, but it is possible patients may have communicated to their physiotherapist that they were using the STAK at home while receiving standard treatment. Patients received an average of four physiotherapy appointments during the eight weeks. Improvements in all the STAK group outcome measures were maintained at long term follow-up; however, no long-term follow-up measures were taken from the control group. A future study comparing long-term follow-up data including a control group would enable long-term comparisons to be made.
Conclusion
Patients undertaking the STAK home treatment programme and standard physiotherapy demonstrated significantly greater gains in ROM, WOMAC, and OKS than the control group receiving standard physiotherapy alone. The improvements were also maintained at long term follow-up. Adherence to the STAK programme and acceptability of the device were high and no complications occurred as a result of its use.
The results suggest that the STAK programme enables knee arthrofibrosis patients to perform high intensity self-stretching effectively at home with exceptional patient adherence levels. Incorporation of the STAK into clinical practice would significantly improve patient’s outcomes, satisfaction and result in considerable cost savings on physiotherapy and further surgery.
References
1. Cheuy VA , Foran JRH , Paxton RJ , et al. Arthrofibrosis associated with total knee arthroplasty . J Arthroplasty . 2017 ; 32 ( 8 ): 2604 – 2611 . Crossref PubMed Google Scholar
2. National Joint Registry 15th Annual Report 2018 – HQIP [Internet] . [cited 2019 Mar 25]. Available from . https://www.hqip.org.uk/resource/national-joint-registry-15th-annual-report-2018/#.XJjLTvn7SUk (date last accessed 09 July 2020 ). Google Scholar
3. Rissman CM , Keeney BJ , Ercolano EM , Koenig KM . Predictors of facility discharge, range of motion, and patient-reported physical function improvement after primary total knee arthroplasty: a prospective cohort analysis . J Arthroplasty . 2016 ; 31 ( 1 ): 36 – 41 . Jan 1 . Crossref PubMed Google Scholar
4. Ferket BS , Feldman Z , Zhou J , et al. Impact of total knee replacement practice: cost effectiveness analysis of data from the osteoarthritis initiative . BMJ . 2017 ; 356 : j1131 Crossref PubMed Google Scholar
5. Culliford D , Maskell J , Judge A , et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research Datalink . Osteoarthritis Cartilage . 2015 ; 23 ( 4 ): 594 – 600 . Crossref PubMed Google Scholar
6. Kurtz S , Ong K , Lau E , Mowat F , Halpern M . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030 . J Bone Joint Surg Am . 2007 ; 89 ( 4 ): 780 – 785 . Crossref PubMed Google Scholar
7. Sculco PK . The stiff knee: causes and cures . Orthop Proc . 2018 ; 99-B ( 5 ): 2049 . Crossref PubMed Google Scholar
8. Schairer WW , Vail TP , Bozic KJ . What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res . 2014 ; 472 ( 1 ): 181 – 187 . Crossref PubMed Google Scholar
9. Schroer WC , Berend KR , Lombardi AV , et al. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011 . J Arthroplasty . 2013 ; 28 ( 8 Suppl ): 116 – 119 . Crossref PubMed Google Scholar
10. Gunaratne R , Pratt DN , Banda J , et al. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature . J Arthroplasty . 2017 ; 32 ( 12 ): 3854 – 3860 . Crossref PubMed Google Scholar
11. Dunbar MJ , Richardson G , Robertsson O . I can’t get no satisfaction after my total knee replacement . Bone Joint J . 2013 ; 95-B ( 11_Supple_A ): 148 – 152 . Google Scholar
12. Hawker GA , Badley EM , Borkhoff CM , et al. Which patients are most likely to benefit from total joint arthroplasty? Arthritis Rheum . 2013 ; 65 ( 5 ): 1243 – 1252 . Crossref PubMed Google Scholar
13. Saini P , Trikha V . Manipulation under anesthesia for post traumatic stiff knee-pearls, pitfalls and risk factors for failure . Injury . 2016 ; 47 ( 10 ): 2315 – 2319 . Crossref PubMed Google Scholar
14. Laubenthal KN , Smidt GL , Kettelkamp DB . A quantitative analysis of knee motion during activities of daily living . Phys Ther . 1972 ; 52 ( 1 ): 34 – 43 . Crossref PubMed Google Scholar
15. Rowe PJ , Myles CM , Walker C , Nutton R . Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture . 2000 ; 12 ( 2 ): 143 – 155 . Crossref PubMed Google Scholar
16. Donaldson JR , Tudor F , Gollish J . Revision surgery for the stiff total knee arthroplasty . Bone Joint J . 2016 ; 98-B ( 5 ): 622 – 627 . Crossref PubMed Google Scholar
17. Baum KS , Luo TD , Comadoll S , et al. Alternative technique for knee manipulation under anesthesia . Arthroplast Today . 2018 ; 4 ( 4 ): 452 – 453 . Crossref PubMed Google Scholar
18. Esler CNA , Lock K , Harper WM , Gregg PJ . Manipulation of total knee replacements . J Bone Joint Surg Br . 1999 ; 81-B ( 1 ): 27 – 29 . Crossref PubMed Google Scholar
19. Yercan HS , Sugun TS , Bussiere C , et al. Stiffness after total knee arthroplasty: prevalence, management and outcomes . Knee . 2006 ; 13 ( 2 ): 111 – 117 . Crossref PubMed Google Scholar
20. Stephenson JJ , Quimbo RA , Gu T . Knee-attributable medical costs and risk of re-surgery among patients utilizing non-surgical treatment options for knee arthrofibrosis in a managed care population . Curr Med Res Opin . 2010 ; 26 ( 5 ): 1109 – 1118 . Crossref PubMed Google Scholar
21. Thorsteinsson H , Hedström M , Robertsson O , Lundin N , W-Dahl A . Manipulation under anesthesia after primary knee arthroplasty in Sweden: incidence, patient characteristics and risk of revision . Acta Orthop . 2019 ; 90 ( 5 ): 484 – 488 . Crossref PubMed Google Scholar
22. Xu J , Zhang J , Wang X-Q , et al. Effect of joint mobilization techniques for primary total knee arthroplasty: study protocol for a randomized controlled trial . Medicine . 2017 ; 96 ( 49 ): e8827 Crossref PubMed Google Scholar
23. Davies G , Ellenbecker T . Focused exercise aids shoulder hypomobility . Biomechanics . 1999 ; 6 : 77 – 81 . Google Scholar
24. McClure PW , Flowers KR . Treatment of limited shoulder motion using an elevation splint . Phys Ther . 1992 ; 72 ( 1 ): 57 – 62 . Crossref PubMed Google Scholar
25. Ulrich SD , Bonutti PM , Seyler TM , et al. Restoring range of motion via stress relaxation and static progressive stretch in posttraumatic elbow contractures . J Shoulder Elb Surg . 2010 ; 19 ( 2 ): 196 – 201 . Crossref PubMed Google Scholar
26. Ebert JR , Munsie C , Joss B . Guidelines for the early restoration of active knee flexion after total knee arthroplasty: implications for rehabilitation and early intervention . Arch Phys Med Rehabil . 2014 ; 95 ( 6 ): 1135 – 1140 . Crossref PubMed Google Scholar
27. Uhl TL , Jacobs CA . Torque measures of common therapies for the treatment of flexion contractures . J Arthroplasty . 2011 ; 26 ( 2 ): 328 – 334 . Crossref PubMed Google Scholar
28. Witvrouw E , Bellemans J , Victor J . Manipulation under anaesthesia versus low stretch device in poor range of motion after TKA . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 12 ): 2751 – 2758 . Crossref PubMed Google Scholar
29. McElroy MJ , Johnson AJ , Zywiel MG , Mont MA . Devices for the prevention and treatment of knee stiffness after total knee arthroplasty . Expert Rev Med Devices . 2011 ; 8 ( 1 ): 57 – 65 . Crossref PubMed Google Scholar
30. Bonutti PM , McGrath MS , Ulrich SD , et al. Static progressive stretch for the treatment of knee stiffness . Knee . 2008 ; 15 ( 4 ): 272 – 276 . Crossref PubMed Google Scholar
31. Branch TP , Karsch RE , Mills TJ , Palmer MT . Mechanical therapy for loss of knee flexion . Am J Orthop . 2003 ; 32 ( 4 ): 195 – 200 . PubMed Google Scholar
32. Papotto BA , Mills T . Treatment of severe flexion deficits following total knee arthroplasty: a randomized clinical trial . Orthop Nurs . 2012 ; 31 ( 1 ): 29 – 34 . Crossref PubMed Google Scholar
33. Bonutti PM , Marulanda GA , McGrath MS , Mont MA , Zywiel MG . Static progressive stretch improves range of motion in arthrofibrosis following total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc . 2010 ; 18 ( 2 ): 194 – 199 . Crossref PubMed Google Scholar
34. Uhl TL , Jacobs CA . Torque measures of common therapies for the treatment of loss of knee flexion . Sports Health . 2012 ; 4 ( 2 ): 101 – 106 . Crossref PubMed Google Scholar
35. Noyes F , Barber-Westin S . Prevention and treatment of knee arthrofibrosis . Knee Disord Surgery, Rehabil Clin outcomes . 2010 ; 1 : 1053 – 1095 . Google Scholar
36. Murray DW , Fitzpatrick R , Rogers K . The use of the Oxford hip and knee scores . Journal of Bone and Joint Surgery . 2007 ; 89 ( 8 ): 1010 – 1014 . Google Scholar
37. Angst F , Aeschlimann A , Stucki G . Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities . Arthritis Rheum . 2001 ; 45 ( 4 ): 384 – 391 . Crossref PubMed Google Scholar
38. Aspinall S , Sparks T , King A , Price M , Godsiff S . A mobile APP to replace the Goniometer? A pilot study focusing on the measurement of knee range of movement . JSS . 2019 ; 7 ( 3 ): 71 – 80 . Google Scholar
39. Naylor JM , Ko V , Adie S , et al. Validity and reliability of using photography for measuring knee range of motion: a methodological study . BMC Musculoskelet Disord . 2011 ; 12 : 77 . Crossref PubMed Google Scholar
40. Beard DJ , Harris K , Dawson J , et al. Meaningful changes for the Oxford hip and knee scores after joint replacement surgery . J Clin Epidemiol . 2015 ; 68 ( 1 ): 73 – 79 . Crossref PubMed Google Scholar
41. Baum KS , Luo TD , Comadoll S , et al. Alternative technique for knee manipulation under anesthesia . Arthroplast Today . 2018 ; 4 ( 4 ): 452 – 453 . Crossref PubMed Google Scholar
41. Department of Health . Reference costs 2017-18 . 2018 . https://improvement.nhs.uk/resources/reference-costs/ (date last accessed 15 July 2020 ). Google Scholar
43. Kallala RF , Vanhegan IS , Ibrahim MS , Sarmah S , Haddad FS . Financial analysis of revision knee surgery based on NHS tariffs and hospital costs: does it pay to provide a revision service? Bone Joint J . 2015 ; 97-B ( 2 ): 197 – 201 . Crossref PubMed Google Scholar
44. Christensen CP , Crawford JJ , Olin MD , Vail TP . Revision of the stiff total knee arthroplasty . J Arthroplasty . 2002 ; 17 ( 4 ): 409 – 415 . Crossref PubMed Google Scholar
45. Clement ND , MacDonald D , Simpson A . The minimal clinically important difference in the Oxford knee score and short form 12 score after total knee arthroplasty . Knee Surg Sports Traumatol Arthrosc . 2014 ; 22 ( 8 ): 1933 – 1939 . Crossref PubMed Google Scholar
46. Ipach I , Schäfer R , Lahrmann J , Kluba T . Stiffness after knee arthrotomy: evaluation of prevalence and results after manipulation under anaesthesia . Orthop Traumatol Surg Res . 2011 ; 97 ( 3 ): 292 – 296 . Crossref PubMed Google Scholar
47. Dempsey AL , Branch TP , Mills T , Karsch RM . High-Intensity mechanical therapy for loss of knee extension for worker’s compensation and non-compensation patients . Sports Med Arthrosc Rehabil Ther Technol . 2010 ; 2 : 26 . Google Scholar
48. Jacobs CA , Sciascia AD . Factors that influence the efficacy of stretching programs for patients with hypomobility . Sports Health . 2011 ; 3 ( 6 ): 520 – 523 . Crossref PubMed Google Scholar
49. Westby MD , Backman CL . Patient and health professional views on rehabilitation practices and outcomes following total hip and knee arthroplasty for osteoarthritis:a focus group study . BMC Health Serv Res . 2010 ; 10 : 119 . Crossref PubMed Google Scholar
50. Artz N , Dixon S , Wylde V , et al. Comparison of group-based outpatient physiotherapy with usual care after total knee replacement: a feasibility study for a randomized controlled trial . Clin Rehabil . 2017 ; 31 ( 4 ): 487 – 499 . Crossref PubMed Google Scholar
Author contributions
S. K. Aspinall: Principal investigator, Carried out statistical analysis, Wrote the paper.
P. C. Wheeler: Wrote the paper.
S. P. Godsiff: Wrote the paper, Gatekeeper for patients in the study, Chief investigator.
S. M. Hignett: Wrote the paper.
D. T. P. Fong: Wrote the paper.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
S. K. Aspinall reports patents (planned, pending or issued) for Self Treatment Assisted Knee (STAK) being patented in the UK, with international patents pending, which are not related to this article. S. M. Hignett reports employment by Loughborough University and consultancy from Loughborough University Enterprise, both of which are unrelated to this article.
Acknowledgements
The authors would like to thank Tim Diggle and the Leicester Hospital’s Charity for kindly supporting this study. A special thanks to the Medical Physics Team at UHL NHS Trust for manufacturing the STAK tools for the study.
Ethical review statement
Ethical approval for the controlled trial was obtained from the South Birmingham Research Ethics Committee and University Hospitals of Leicester NHS Trust were the study sponsor. The trial protocol was registered with the Clinical Trials Registry (CTR number: NCT04019847).
Follow S. K. Aspinall @Sara_Aspinall
Follow P. C. Wheeler @patrickwheeler7
Follow S. M. Hignett @HUMANFIIT
Follow D. T. P. Fong @dtpfong
Animation
Patient: ID: 05 Demonstrating her progress after using the STAK: https://youtu.be/swUNRIZ3nHM
Patient: ID: 13 Discussing her experience of using the STAK tool: https://youtu.be/DVuPLf84qME
Mr Aujla (Orthopaedic Knee Surgeon) outlining the potential of the STAK Tool to treat the stiff knee: https://youtu.be/krwsS6ZrCXE
Professor Ashford (Orthopaedic Knee Surgeon) describes how the STAK is effective in enabling patients to quickly regain function following knee replacement https://youtu.be/aCuRl2hfRZg
Mr Elsorafy (Orthopaedic Knee Surgeon) describes his patient’s progress using the STAK Tool https://youtu.be/0a4XjBfPZnw
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










