Abstract
Aims
To compare time dependent functional improvement for patients with medial, respectively lateral knee osteoarthritis (OA) after treatment with opening wedge osteotomy relieving the pressure on the osteoarthritic part of the knee.
Methods
In all, 49 patients (52 knees) with a mean age of 47 years (31 to 64) underwent high tibial osteotomies (HTO), and 24 patients with a mean age of 48 years (31 to 62) low femoral osteotomies (LFO) with opening wedge technique due to medial, respectively lateral knee OA with malalignment. All osteotomies were stabilized with a Puddu plate and bone grafting performed in the same time period (2000 to 2008). The patients were evaluated by the Knee Injury and Osteoarthritis Outcome Score (KOOS) pre-operatively and at six months, and at one, two, five, and ten years postoperatively. The knee OA was graded according to the Ahlbäck and Kellgren-Lawrence radiological scoring systems.
Results
The mean angular corrections were 8.0° (4° to 12°) for the HTO and 9.6° (4° to 20°) for the LFO. Both the pre-operative KOOS and the osteoarthritic gradings were similar for the two patient groups. The five subscores of KOOS increased significantly during the postoperative period (p < 0.001 to 0.029) levelling out after one year in both groups. The KOOS subscore symptoms was significantly higher for patients with HTO than those with LFO at all follow-up times, for sport and recreation in the period one to five years, and for pain and quality of life at two to five years (p < 0.001 to 0.009). Eight HTOs (15%) and five LFOs (21%) were converted to total knee arthroplasty after mean 6.7 years (2.0 to 9.8) and 5.4 years (4.0 to 8.0) respectively. The ten-year osteotomy survival rates were 88% for the HTO and 79% for the LFO (p = 0.745).
Conclusion
Patients with unicompartmental knee OA improved after a corrective opening wedge osteotomy, but four of the five subscores of KOOS were significantly higher for those with medial than those with lateral OA in most of the ten-year follow-up period.
Cite this article: Bone Joint Open 2020;1-7:346–354.
Introduction
The medial compartment of the knee is more congruent than the lateral compartment as the medial tibial plateau is concave and the medial femoral condyle is convex, whereas the lateral tibial plateau and the lateral femoral condyle both are convex. The lateral meniscus is therefore more important for the congruency of the lateral knee compartment than the medial meniscus is for the congruency of the medial compartment.1 Both menisci act as stress absorbers in the knee, and the medial meniscus is especially important in this respect as most of the load to the knee pass through the medial compartment during the stance phase when the leg is adducted.1,2 The absence of a meniscus leads to stress concentration and progressive deterioration of the joint surfaces with increasing varus if the medial compartment is affected,3 and increasing valgus if the lateral compartment is affected.3,4
The symptoms may be relieved if the affected compartment is unloaded by a corrective osteotomy shifting the load to the healthy compartment of the knee,1,4 and destroyed hyaline cartilage may later be replaced by fibrocartilage.5-7 A corrective osteotomy may be performed either as a closing wedge or opening wedge osteotomy on tibia or femur.6,8-11 In the late 1990s, Puddu10 simplified the surgical technique for opening wedge osteotomy by introducing a spacer plate securing the planned correction.
Two previous prospective studies of opening wedge osteotomies with Puddu plates from our group suggested a better outcome of high tibial osteotomy (HTO) for medial knee osteoarthritis (OA),12 than low femoral osteotomy (LFO) for lateral knee OA.13 The purpose of the present study was to compare the two patient groups more closely with a longer follow-up time (ten years) to explore any differences in time dependent functional outcome of HTO for medial knee OA compared to LFO for lateral knee OA.
Methods
In all, 49 consecutive patients with medial and 24 with lateral knee OA were treated with HTO, respectively LFO with opening wedge technique in the period 2000 to 2008. Three patients with medial knee OA had bilateral surgery at different timepoints, including 52 HTOs in the study. The demographic data of the two patient groups were similar (Table I). The OA was mainly due to open medial, respectively lateral meniscal resection performed 20 to 30 years previously before the arthroscopic era, or to several successive arthroscopic meniscal resections.12,13 Inclusion criteria were severe pain in an osteoarthritic knee with varus, respectively valgus malalignment which had not responded to conservative treatment, and where knee arthroplasty was not the first treatment of choice because of relatively young age.
Table I.
Demographic data of patients with high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Patients | HTO (n = 49) | LFO (n = 24) |
|---|---|---|
| Female, n (%) | 19 (39) | 11 (46) |
| Male, n (%) | 30 (61) | 13 (54) |
| Age (yrs), mean (95% confidence interval; range) | 47 (44.8 to 49.2; 31 to 64) | 48 (40.3 to 55.7; 31 to 62) |
| BMI, mean (95% confidence interval; range) | 27.4 (23.4 to 27.5; 20.5 to 37.9) | 26.2 (25.8 to 27.8; 22.0 to 31.7) |
-
BMI, body mass index
Clinical examination
This included knee range of motion (ROM) measured with a goniometer, and body weight and height for calculation of body mass index (BMI). The patients also filled in a questionnaire for calculation of the Knee Injury and Osteoarthritic Outcome Score (KOOS).14 KOOS has five subscales: pain, other symptoms, activities of daily living (ADL), sport and recreational function, and knee-related quality of life (QoL). A score from 0 to 100 is calculated for each subscale, with 100 representing the best result. A score improvement of 10 is supposed to have clinical relevance.15
Radiology
Radiological evaluations were made on weight-bearing radiographs with straight knees and on lateral knee radiographs. The radiographs were scored according to both the Ahlbäck classification criteria16 and the Kellgren-Lawrence grading scale.17 Tthe tibiofemoral anatomical axis angle was also recorded. The angular correction for the HTO was calculated on standing (full leg length) hip, knee and ankle (HKA) radiographs according to Dugdale et al,18 aiming for the mechanical axis to pass just lateral to the intercondylar eminence corresponding to 62% of the width of the tibial plateau, measured from the medial tibial side, and through the middle of the knee for the LFO.4
Osteotomy failure
Failure was defined as conversion of the osteotomy to total knee arthroplasty (TKA). Data from TKA converted patients were only included in the study until TKA surgery.
Surgical technique
The patients were operated on a traction table with slight flexion of the knee to ease fluoroscopic guidance during the operation and secure rotational control of the leg. The osteotomy was performed as described by Puddu.10 The proximal part of the tibia was approached through a medial incision for the HTO. The superficial medial collateral ligament was cut as part of an oblique osteotomy starting from the upper edge of pes anserinus and aiming for the tip of the fibular head. The distal part of the femur was approached through a lateral incision for the LFO, and an oblique supracondylar opening wedge osteotomy with a medial bone hinge was performed.
The height of the osteotomy cleft was calculated from the length of the osteotomy cut and the planned correcting angle, and the appropriate spacer plate chosen from a table provided by the plate manufacturer (Arthrex, Naples, Florida, USA). Puddu plates of the first generation were used. The osteotomy cleft was filled with bone from the iliac crest. All patients received antithrombotic prophylaxis with low molecular heparin (Fragmin; Pfizer, New York, USA) for ten days postoperatively. They were allowed partial weightbearing postoperatively (10 kg), and no braces were used. Increasing weightbearing was allowed after six weeks and full weightbearing a few weeks later, depending on the radiological healing of the osteotomy. Healing was defined as three-quarters of the osteotomy filled with new bone, and delayed healing as healing beyond five months postoperatively.
Follow-up
Standing weightbearing radiographs of both knees were obtained at the three months, five- and ten-year follow-ups, but only supine radiographs of the index knee at the six-weeks follow-up. The patients filled in KOOS at the six-month, one-, two-, five- and ten-year follow-ups. Most of the follow-ups were performed by the first author, and no patients were lost to follow-up. The collection of data was approved by the Norwegian Social Science Data Services (project 22075), and the study was performed in accordance with the Helsinki Declaration with informed patient consent.
Statistical analysis
The results are presented as mean with 95% confidence interval (CI) and range. Statistical differences were calculated by fitting separate linear mixed models for each of the KOOS subscores. Missing data were assumed to be missing at random. The chi square test was used for categorical variables, and the two-tailed Fisher exact test when groups with small numbers were involved. The calculations were made with the SPSS software version 22 (IBM, Armonk, New York, USA) and Stata v16 (Stata 2015, College Station, Texas, USA). The level of statistical significance was set to p < 0.05.
Results
The mean angular correction measured from pre- and three-month postoperative radiographs was 8.0° for the HTO and 9.6° for the LFO (Table II). These corrections were later sustained. Overall, 42 of the 52 HTOs (82%) were healed at the three months follow-up, and all except one with osteosynthetic failure at the six-month follow-up. Of the 24 LFOs, 18 (75%) were healed at the three-month follow-up, and all at the six-month follow-up. Radiographs of a HTO and a LFO at the ten-year follow-up are shown in Figure 1a.
Table II.
Angular correction and pre- and postoperative tibiofemoral angles for high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Angles (degree) | HTO (n = 52) | LFO (n = 24) |
|---|---|---|
| Angular correction | 8.0 (7.3 to 8.7) (4 to 12) | 9.6 (7.7 to 11.5) (4 to 20) |
| Pre-operative tibiofemoral angle | 1.1 varus (0.3 to 1.8) (7 varus to 3 valgus) | 11.5 valgus (10.1 to 13.0) (7 to 20) |
| Postoperative tibiofemoral angle | 6.9 valgus(6.4 to 7.5) (3 to 10) | 2.0 valgus (0.5 to 3.4) (3 varus to 7 valgus) |
-
n, number of osteotomies. Mean with CI 95% and range.
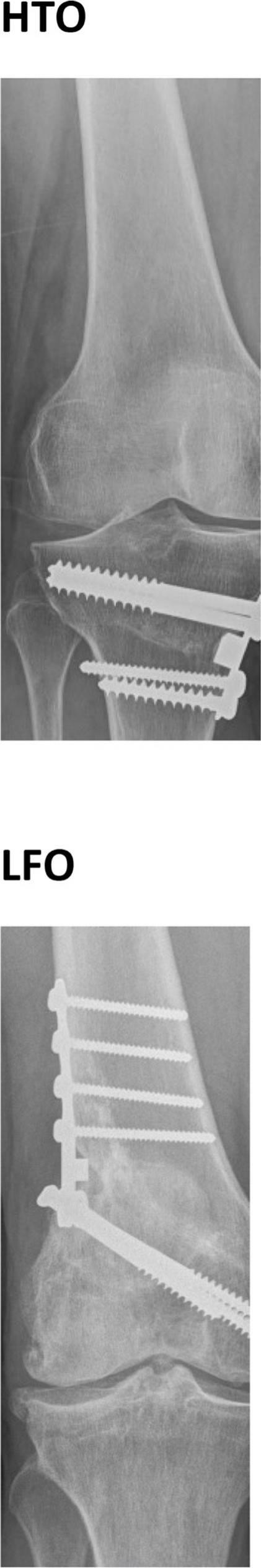
Fig. 1
High tibial osteotomy (HTO) ten years after an angular correction of 8° and low femoral osteotomy (LFO) ten years after an angular correction of 6° (frontal views). Note the open medial, respectively lateral joint spaces. Both patients had a good knee function.
One patient with HTO died in the follow-up period of causes unrelated to the knee surgery.
KOOS
Similar KOOS were recorded pre-operatively for both osteotomy groups. Most of the improvement in KOOS occurred during the first year. At the one-year follow-up the mean KOOS had increased significantly compared to the pre-operative values (p < 0.001 to 0.029), and more than 10 points and clinical relevant for all KOOS subgroups both for patients with HTO and LFO (Figures 2 to 6). Thereafter, the KOOS values plateaued, remaining on that level throughout the ten-year follow-up period for surviving osteotomies. For the KOOS subgroup symptoms the mean scores for those with HTO was 10 points above those with LFO at all follow-up times (p < 0.000 to 0.004) (Figure 2), for the subgroup sport and recreation at one to five years (p < 0.001–= to 0.009) (Figure 3), and for pain and QoL at two to five years (p < 0.003 to 0.008) (Figures 4 and 5). No significant difference between the HTO and LFO groups were observed for the KOOS subgroup ADL (Figure 6).
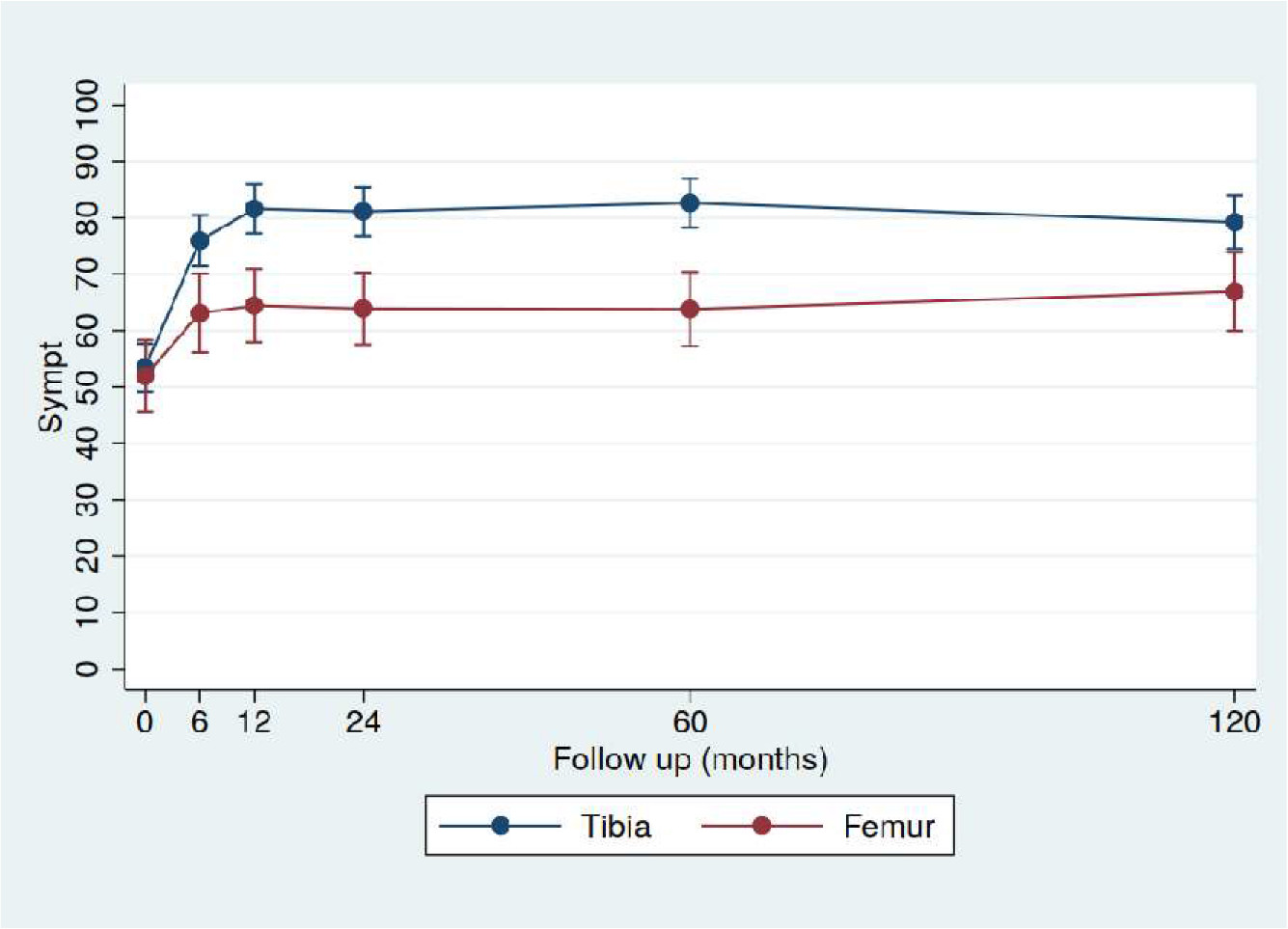
Fig. 2
Improvement of the Knee Injury and Osteoarthritic Outcome (KOOS) subscale Symptoms for high tibial osteotomy (HTO) (n = 52) and low femoral osteotomy (LFO) (n = 24) as a function of time after the operation. Significant higher values for HTO than for LFO were observed for at all follow-up times (p < 0.001 to 0.004). Mean with 95% CI.
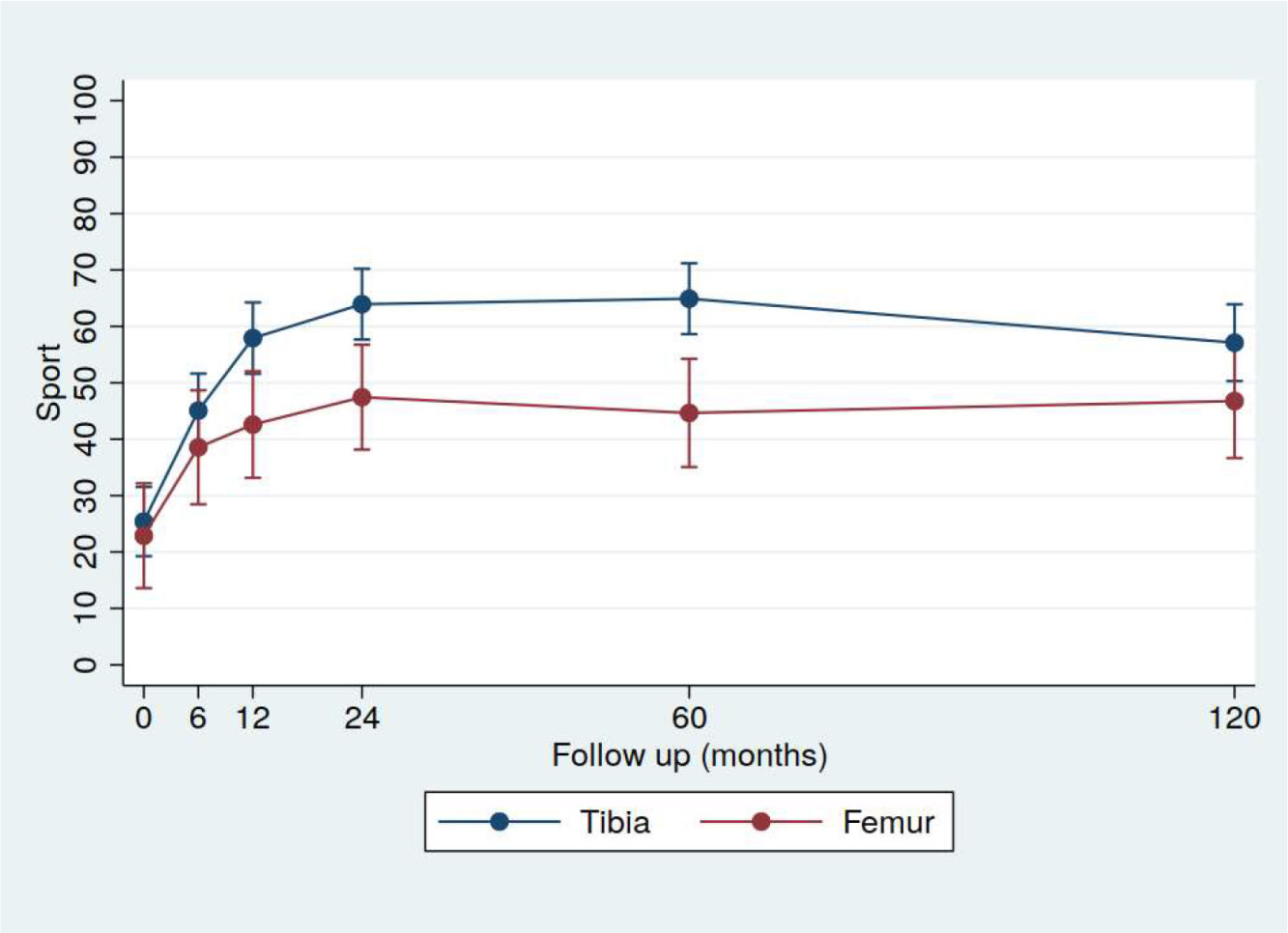
Fig. 3
Improvement of the Knee Injury and Osteoarthritic Outcome (KOOS) subscale sport and recreation for high tibial osteotomy (HTO) (n = 52) and low femoral osteotomy (LFO) (n = 24) as a function of time after the operation. Significant higher values for HTO than for LFO were observed at the follow-up times one to five years (p < 0.001 to 0.009). Mean with 95% CI.
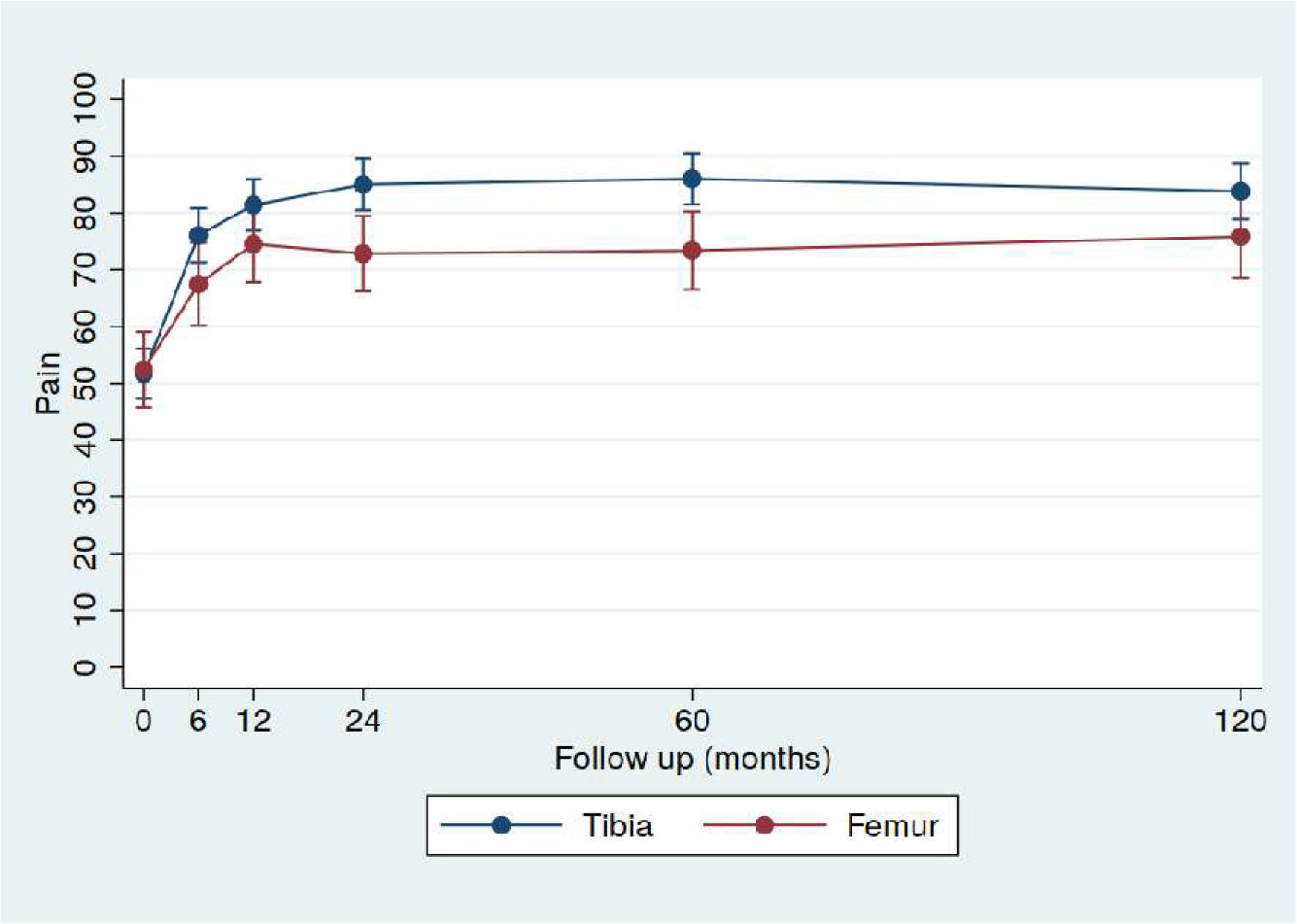
Fig. 4
Improvement of the Knee Injury and Osteoarthritic Outcome (KOOS) subscale pain for high tibial osteotomy (HTO) (n = 52) and low femoral osteotomy (LFO) (n = 24) as a function of time after the operation. Significant higher values for HTO than for LFO were observed at the follow-up times two to five years (p = 0.003). Mean with 95% CI.
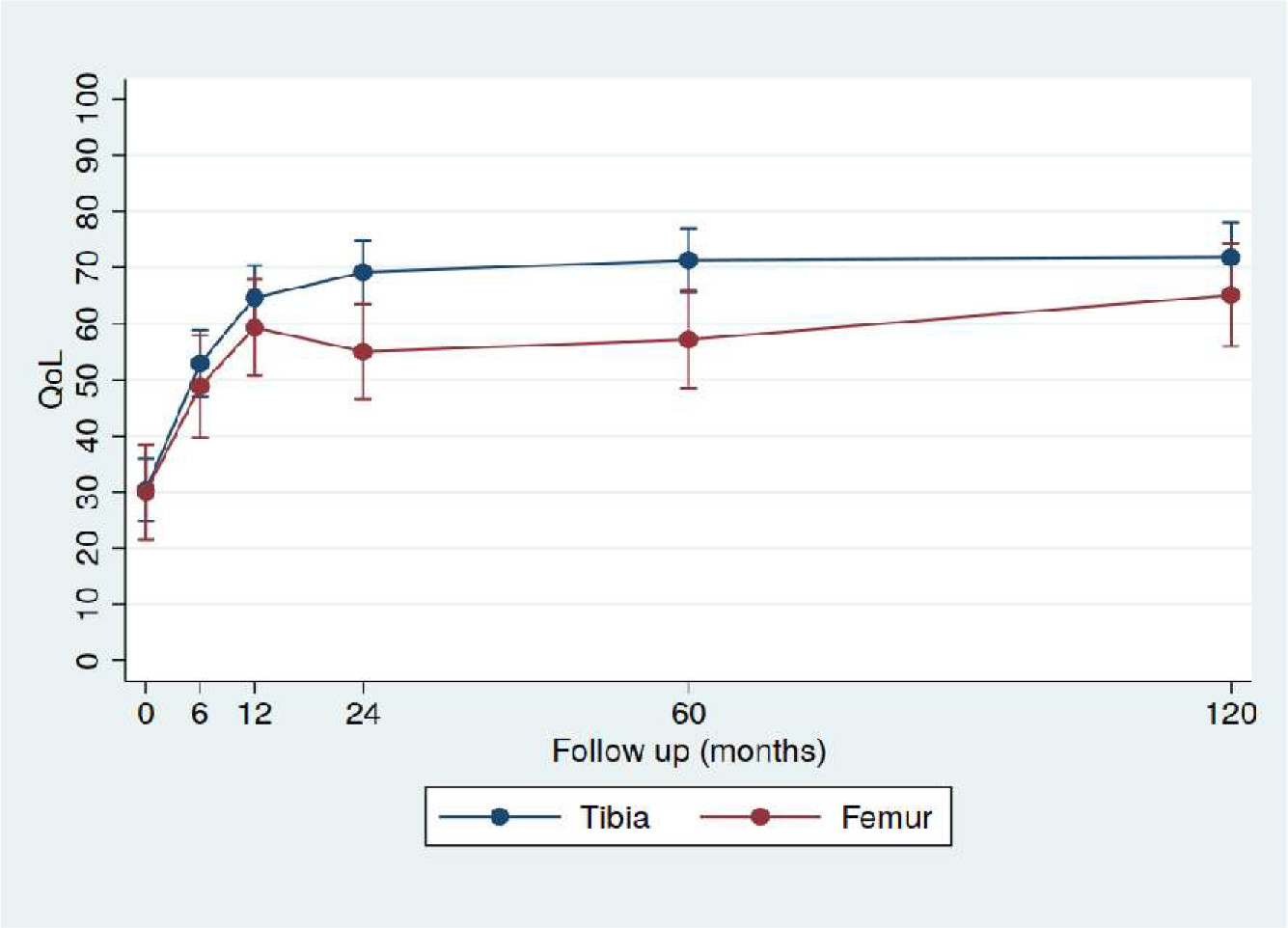
Fig. 5
Improvement of the Knee Injury and Osteoarthritic Outcome (KOOS) subscale quality of life (QoL) for high tibial osteotomy (HTO) (n = 52) and low femoral osteotomy (LFO) (n = 24) as a function of time after the operation. Significant higher values for HTO than for LFO were observed at the follow-up times two to five years (p = 0.007 to 0.008). Mean with 95% CI.
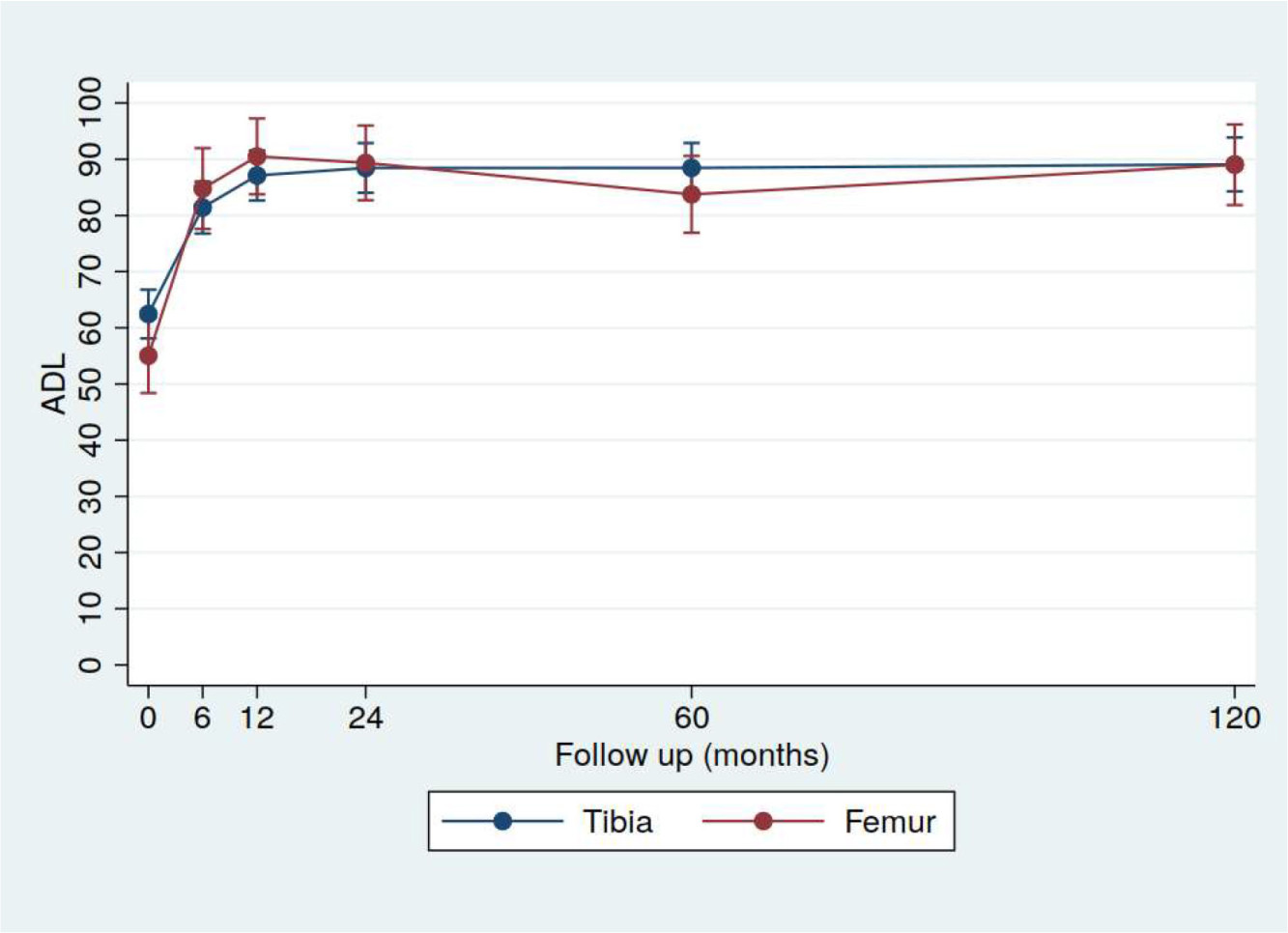
Fig. 6
Improvement of the Knee Injury and Osteoarthritic Outcome (KOOS) subscale activity of daily living (ADL) for high tibial osteotomy (HTO) (n = 52) and low femoral osteotomy (LFO) (n = 24) as a function of time after the operation. No significant differences were observed between the groups. Mean with 95% CI.
The 13 patients who later had their osteotomy converted to TKA had lower pre-operative KOOS values, but they too improved significantly after the osteotomy (data not shown).
Radiological evaluation
The pre-operative Ahlbäck and Kellgren-Lawrence gradings were similar for knees with HTO and LFO (Tables III and IV). Higher osteoarthritic gradings were observed five and ten years postoperatively, but without significant differences between knees with HTO and LFO.
Table III.
Ahlbäck1 radiological osteoarthritic grading of high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Time | HTO (n = 52) | LFO (n = 24) |
|---|---|---|
| Grades 0 to 1/2 to 3 | Grades 0 to 1/2 to 3 | |
| Pre-operatively | 39/13 | 16/8 |
| 5 years postoperatively | 34/16 | 13/8 |
| 10 years postoperatively | 27/14 | 11/8 |
-
n = number of osteotomies. No significant difference between HTO and LFO (pre-operatively (p = 0.631), five years postoperatively (p = 0.825), and ten years postoperatively (p = 0.759)).
Table IV.
Kellgren-Lawrence14 radiological osteoarthritisc grading of high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Time | HTO (n = 52) | LFO (n = 24) |
|---|---|---|
| Grades 1 to 2/3 to 4 | Grades 1 to 2/3 to 4 | |
| Pre-operatively | 30/22 | 11/13 |
| Five years postoperatively | 16/34* | 6/17 |
| Ten years postoperatively | 9/32** | 5/14 |
-
*Significant different from pre-operative gradings p = 0.016, **p < 0.001 from pre-operative grading. No significant difference between HTO and LFO (pre-operatively (p = 0.474), five-year postoperatively (p = 0.831), and ten-year postoperatively (p = 0.749)).
-
n, number of osteotomies
Range of motion
The pre-operative ROM was mean 132° (CI 130 to 135, range 85 to 140) for patients with HTO and 126° (CI 121 to 132, range 105 to 140) for patients with LFO. Three months postoperatively the mean ROMs were reduced by mean 6°, respectively 12°, but the pre-operative ROM was regained at the six-month follow-up in both groups, and later remained at the pre-operative level.
Complications
Seven complications were observed both after HTO (13%) and LFO (29%) (Table V), but only two HTOs (4%) and one LFO (4%) needed an early reoperation. The only osteosynthetic failure was due to fatigue fracture of two screws in a HTO, and occurred in an obese patient three months postoperatively. The patient was reoperated with a Tomofix plate (Synthes, Stratec Medical, Oberdorf, Switzerland) with autologous bone grafting, and the osteotomy healed. The other reoperation after HTO was a wound revision after prolonged secretion with negative cultures, and the osteotomy healed at the three-month follow-up. The re-operation after LFO was arthroscopic removal of intraarticular adhesions that caused reduced knee flexion at the three-month follow-up. The pre-operative ROM was regained.
Table V.
Postoperative complications after high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Complication type | HTO (n = 52) | LFO (n = 24) |
|---|---|---|
| Wound infection | 2 | 0 |
| Prolonged wound secretion | 1 | 0 |
| Hinge fracture | 0 | 2 |
| Reduced flexion | 0 | 2 |
| Delayed healing | 1 | 3 |
| Deep venous thrombosis | 2 | 0 |
| Osteosynthetic failure | 1 | 0 |
-
n, number of osteotomies.
Survival
In all, eight HTOs (15%) and five LFOs (21%) were converted to TKA (p = 0.534) at a mean 6.7 years (CI 3.9 to 9.5, range 2.0 to 9.8), respectively 5.4 years (CI 3.4 to 7.4, range 4.0 to 8.0) postoperatively. The knees converted to TKA had pre-operative osteoarthritic scores in the upper range and lower pre-operative KOOS than surviving osteotomies. The survival of the osteotomies were similar with a ten-year survival of 84% for HTO and 79% for LFO (Table VI). The angular correction was similar for the patients who ended up with TKA and those where the osteotomy survived.
Table VI.
Survival of high tibial osteotomy (HTO) and low femoral osteotomy (LFO).
| Time | HTO (n = 52) | LFO (n = 24) |
|---|---|---|
| 2 years postoperatively | 100% | 100% |
| 5 years postoperatively | 94% | 88% |
| 10 years postoperatively | 84% | 79% |
-
No significant difference between HTO and LFO (five years postoperatively (p = 0.372), and ten years postoperatively (p = 0.745).
The osteotomy plate was removed in 12 of the 44 survived HTOs (27%) and in seven of the 17 survived LFOs (41%) without significant difference (p = 0.457).
Body mass index
The pre-operative BMI of the patients with HTO and LFO was similar (Table I). No significant difference in BMI was observed between the patients with a survived osteotomy and those where the osteotomy was converted to TKA (Table I).
Discussion
This study revealed that opening wedge HTO for medial knee OA had a better functional outcome than opening wedge LFO for lateral knee OA, even though the age of the patients, the pre-operative KOOS, the degree of pre-operative OA and the BMI were similar in both patient groups. KOOS increased far beyond pre-operative values in both groups, and the increase gained one year postoperatively was sustained throughout the ten-year follow-up for surviving osteotomies (Figures 2 to 6). About one of five had their osteotomy converted to TKA after about six years in both groups.
The better outcome of the HTO was most evident in the KOOS subgroups symptoms and sport and recreation with scores 10 points or more beyond those of the LFO group and therefore clinical relevant15 throughout most of the ten-year period (Figures 2 and 3). At the ten-year follow-up the functional difference between the two groups was only significant in the subgroup Symptoms (Figure 2). The KOOS subgroup symptoms also disclosed a higher difference than the other KOOS subgroups when two patient groups with light knee OA and similar age as in the present study were compared.19 It is a clinical experience that corrective osteotomy for medial knee OA has a better outcome than corrective osteotomy for lateral knee OA, but to our knowledge this has not been shown in a comparative follow-up study previously.
Several scooring systems are used to evaluate the results after knee surgery. The KOOS system was developed by Roos et al14 and published in 1998. We found KOOS suitable for this study, and this is supported by the study of Tanner et al,20 who compared the different knee evaluation systems and found KOOS and the International Knee Documentation Committee (IKDC) Standard Evaluation Form to be the best quality of life instruments ensuring that the point of view of the patients was considered.
The pre-operative Ahlbäck16 and Kellgren-Lawrence17 radiological classifications were similar for HTO and LFO (Tables III and IV). The patients had pain and significant reduced activity pre-operatively, and the osteotomy was performed to prevent or delay TKA in this middle- aged group of patients. At the final follow-up, 16% of the HTOs and 21% of the LFOs were converted to TKA, but this difference was not significant (p = 0.534). Neither did the five- and ten-year osteotomy survival for the two groups of patients disclose any significant differences (Table VI). The osteotomy survival rate for the HTOs was similar to those reported by Yoon et al21 and Jin et al,22 but higher than reported by Keenan et al.23 The survival rate for the LFOs agrees with those reported by Kim et al.24
The lateral compartment of the knee is less congruent than the medial compartment with a smaller articular contact area, and hence, higher contact stresses if the forces are similar to those in the medial compartment. A corollary of this morphology is that the lateral meniscectomy has a major effect on the contact stresses than does a medial one.1 We think this may be a possible explanation for the better functional results of HTO compared to LFO since the pre-operative age, BMI and degree of OA were similar in the two groups, but a dismorfic lateral femoral condyle may also play an important role in this respect. Since most of the load passes through the medial compartment during walking, OA is most common on the medial side despite the better morphological adaptation.1 Because of the increased load in the medial knee compartment in normal knees, the mechanical axis in the knees with medial OA was overcorrected to pass just lateral to the middle of the knee.18 In the knees with lateral OA the mechanical axis was only brought back to normal through the middle of the knee to prevent overloading of the medial compartment.1,4
Both the Ahlbäck and Kellgren Lawrence radiological classification systems for OA are in common use. In the Ahlbäck classification,16 great importance is attatched to obliteriation of the joint space and any bone loss, whereas the Kellgren-Lawrence system17 also consider the presence of osteophytes in addition to narrowing of the joint. Different descriptions of the Kellgren-Lawrence criteria for knee OA have been published, but we used the original description.25 The osteoarthritic grading increased at the five- and ten-year follow-ups without significant differences between knees with HTO and LFO (Tables III and IV). In contrast, the increased KOOS scoring at the one-year follow-up was sustained throughout the study (Figures 2 to 6). The 13 knees with osteotomies that later were converted to TKA were more osteoarthritic and had lower KOOS pre-operatively than the surviving osteotomies, but also these patients reported significantly increased KOOS the first years after the osteotomy.
Obesity has been reported to influence the results after osteotomies negatively.26-28 The mean BMI in the present study was 26 to 27, normal and similar in the two groups, and few patients were obese (Table I).
All osteotomies healed in this study, including the HTO with osteosynthetic failure where the osteotomy healed after re-operation. The successful healing was probably due to autologous bone grafting of the osteotomy cleft.29 Slower healing times have been reported by Jacobi et al,30 who stabilized the osteotomy with the stiffer Tomofix plate without bone grafting. This plate is larger than the Puddu plate giving more local soft tissue irritation, and often has to be removed after consolidation of the osteotomy.11,30 Less than half of the Puddu plates in the present study were removed from survived osteotomies. The Tomofix plate gives, however, a more stable osteotomy than the Puddu plate allowing earlier weightbearing.31
The strength of this study is the prospective design with repetitive KOOS recordings enabling functional evaluation of the patients over time, that no patient was lost, and the long follow-up period. The weakness is that 15 out of 312 (4.8%) KOOS recordings for patients with HTO and six out of 144 (4.2%) for patients with LFO are missing, mostly from the six-month follow-up. This is partly compensated for by using mixed model statistics which account for missing values. Another weakness is the missing of postoperative HKA radiographs since the study started before such radiographs were available at our hospital. The pre-operative HKA radiographs of the first included patients were therefore taken at another hospital making it inconvenient for the patients to visit two hospitals for postoperative follow-ups. A later HTO study with pre- and postoperative HKA radiographs at our hospital disclosed an undercorrection of about 3° related to the planned correction with Dugdale’s method,18 using the same opening wedge technique for HTO as in the present study.32
Conclusion
Opening wedge HTO for medial knee OA gave better functional outcome in the ten-year period than opening wedge LFO for lateral knee OA. The knee function after HTO and LFO improved gradually during the first year, and this improvement sustained ten years after the operation for most of the patients. About one in five patients had their osteotomy converted to TKA after ten years.
References
1. Amis AA . Biomechanics of high tibial osteotomy . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 1 ): 197 – 205 . Crossref PubMed Google Scholar
2. Shelburne KB , Torry MR , Pandy MG , Muscle PMG . Muscle, ligament, and joint-contact forces at the knee during walking . Med Sci Sports Exerc . 2005 ; 37 ( 11 ): 1948 – 1956 . Crossref PubMed Google Scholar
3. Maquet P . The treatment of choice in osteoarthritis of the knee . Clin Orthop . 1985 ; 192 : 108 – 112 . PubMed Google Scholar
4. Puddu G , Cipolla M , Cerullo G , Franco V , Giannì E . Which osteotomy for a valgus knee? Int Orthop . 2010 ; 34 ( 2 ): 239 – 247 . Google Scholar
5. Fujisawa Y , Masuhara K , Shiomi S . The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints . Orthop Clin North Am . 1979 ; 10 ( 3 ): 585 – 608 . PubMed Google Scholar
6. Haviv B , Bronak S , Thein R , Thein R . The results of corrective osteotomy for valgus arthritic knees . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 1 ): 49 – 56 . Crossref PubMed Google Scholar
7. Jung W-H , Takeuchi R , Chun C-W , et al. Second-Look arthroscopic assessment of cartilage regeneration after medial opening-wedge high tibial osteotomy . Arthroscopy . 2014 ; 30 ( 1 ): 72 – 79 . Crossref PubMed Google Scholar
8. Coventry MB . Osteotomy about the knee for degenerative and rheumatoid arthritis . J Bone Joint Surg Am . 1973 ; 55 ( 1 ): 23 – 48 . PubMed Google Scholar
9. Coventry MB . Proximal tibial varus osteotomy for osteoarthritis of the lateral compartment of the knee . J Bone Joint Surg Am . 1987 ; 69 ( 1 ): 32 – 38 . PubMed Google Scholar
10. Puddu G , Franco V , Cipolla M , Cerullo G , Gianni E . Opening wedge osteotomy: proximal tibia and distal femur. In: Jackson RW, ed . Reconstructive knee surgery . Philadelphia : Lippincott, Williams and Wilkins , 2002 : 375 – 390 . Google Scholar
11. Staubli AE , Simoni CD , Babst R , Lobenhoffer P . TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia – early results in 92 cases . Injury . 2003 ; 34 ( Suppl 2 ): 55 – 62 . Google Scholar
12. Ekeland A , Nerhus TK , Dimmen S , Heir S . Good functional results following high tibial opening-wedge osteotomy of knees with medial arthritis. A prospective study with a mean of 8.3 years of follow-up . Knee . 2017 ; 24 ( 2 ): 380 – 389 . Google Scholar
13. Ekeland A , Nerhus TK , Dimmen S , Heir S . Good functional results of distal femoral opening-wedge osteotomy of knees with lateral osteoarthritis . Knee Surg Sports Traumatol Arthrosc . 2016 ; 24 ( 5 ): 1702 – 1709 . Crossref PubMed Google Scholar
14. Roos EM , Roos HP , Lohmander LS , Ekdahl C , Beynnon BD . Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a Self-Administered Outcome Measure . J Orthop Sports Phys Ther . 1998 ; 28 ( 2 ): 88 – 96 . Google Scholar
15. Roos EM , Lohmander LS . The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis . Health Qual Life Outcomes . 2003 ; 1 : 64 . Crossref PubMed Google Scholar
16. Ahlbäck S . Osteoarthrosis of the knee. A radiographic investigation . Acta Radiol Diagn . 1968 ; 7 ( Suppl 277 ): 7 – 72 . PubMed Google Scholar
17. Kellgren JH , Lawrence JS . Radiological assessment of Osteo-Arthrosis . Ann Rheum Dis . 1957 ; 16 ( 4 ): 494 – 502 . Crossref PubMed Google Scholar
18. Dugdale TW , Noyes FR , Styer D . Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length . Clin Orthop . 1992 ; 274 : 248 – 264 . PubMed Google Scholar
19. Kise NJ , Risberg MA , Stensrud S , et al. Excercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up . BMJ . 2016 ; 354 : i3740 . Google Scholar
20. Tanner SM , Dainty KN , Marx RG , Kirkley A . Knee-specific quality-of-life instruments: which ones measure symptoms and disabilities most important to patients? Am J Sports Med . 2007 ; 35 ( 9 ): 1450 – 1458 . Crossref PubMed Google Scholar
21. Yoon JR , S-N K , Jung K-Y , et al. Risk of revision following total knee arthroplasty or high tibial osteotomy: a nationwide propensity-score-matched study . J Bone Joint Surg Am . 2019 ; 101 ( 9 ): 771 – 778 . Crossref PubMed Google Scholar
22. Jin C , Song E-K , Santoso A , et al. Survival and risk factor analysis of medial open wedge high tibial osteotomy for unicompartment knee osteoarthritis . Arthroscopy . 2020 ; 36 ( 2 ): 535 – 543 . Crossref PubMed Google Scholar
23. Keenan OJF , Clement ND , Nutton R , Keating JF . Older age and female gender are independent predictors of early conversion to total knee arthroplasty after high tibial osteotomy . Knee . 2019 ; 26 ( 1 ): 207 – 212 . Crossref PubMed Google Scholar
24. Kim YC , Yang J-H , Kim HJ , et al. Distal femoral varus osteotomy for valgus arthritis of the knees: systematic review of open versus closed wedge osteotomy . Knee Surg Relat Res . 2018 ; 30 ( 1 ): 3 – 16 . Crossref PubMed Google Scholar
25. Schiphof D , Boers M , Bierma-Zeinstra SMA . Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis . Ann Rheum Dis . 2008 ; 67 ( 7 ): 1034 – 1036 . Crossref PubMed Google Scholar
26. Brinkman J-M , Lobenhoffer P , Agneskirchner JD , et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies . J of Bone Joint Surg Br . 2008 ; 90 ( 12 ): 1548 – 1557 . Crossref PubMed Google Scholar
27. Hui C , Salmon LJ , Kok A , et al. Long-Term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee . Am J Sports Med . 2011 ; 39 ( 1 ): 64 – 70 . Crossref PubMed Google Scholar
28. Morales LA , Navalon LA , Ribot P , Valle JA . Treatment of osteoarthritis of the knee with valgus deformity by means of varus osteotomy . Acta Orthop Belg . 2000 ; 66 ( 3 ): 272 – 278 . PubMed Google Scholar
29. Jung W-H , Takeuchi R , Kim D-H , Nag R . Faster Union rate and better clinical outcomes using autologous bone graft after medial opening wedge high tibial osteotomy . Knee Surg Sports Traumatol Arthrosc . 2019 ; 28 ( 5 ): 1380 – 1387 . Crossref PubMed Google Scholar
30. Jacobi M , Wahl P , Bouaicha S , Jakob RP , Gautier E . Distal femoral varus osteotomy: problems associated with the lateral open-wedge technique . Arch Orthop Trauma Surg . 2011 ; 131 ( 6 ): 725 – 728 . Crossref PubMed Google Scholar
31. Floerkemeier S , Staubli AE , Schroeter S , Goldhahn S , Lobenhoffer P . Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 1 ): 170 – 180 . Crossref PubMed Google Scholar
32. Nerhus TK , Ekeland A , Solberg G , et al. Radiological outcomes in a randomized trial comparing opening wedge and closing wedge techniques of high tibial osteotomy . Knee Surg Sports Traumatol Arthrosc . 2017 ; 25 ( 3 ): 910 – 917 . Crossref PubMed Google Scholar
Author contributions
A. Ekeland: Designed the study, Collected, analyzed, and interpreted the data, Wrote and edited the manuscript.
T. K. Nerhus: Designed the study, Analyzed and interpreted the data, Edited the manuscript.
S. Dimmen: Analyzed and interpreted the data, Edited the manuscript.
S. Heir: Analyzed and interpreted the data, Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors thank Jonas Ranstam BSc PhD, CStat CSci, Lund University, Sweden, for valuable statistical help.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









