Abstract
Aims
In elderly patients with osteoarthritis and protrusio who require arthroplasty, dislocation of the hip is difficult due to migration of the femoral head. Traditionally, neck osteotomy is performed in situ, so this is not always achieved. Therefore, the purpose of this study is to describe a partial resection of the posterior wall in severe protrusio.
Methods
This is a descriptive observational study, which describes the surgical technique of the partial resection of the posterior wall during hip arthroplasty in patients with severe acetabular protrusio operated on between January 2007 and February 2017.
Results
In all, 49 hip arthroplasties were performed. The average age of patients was 60 years, and idiopathic was the most frequent aetiology of protrusio. All patients were treated with femoral head autograft and no intra- or postoperative complications were reported. No patients required revision surgery.
Conclusion
Partial resection of the posterior wall demonstrated to be a safe surgical technique with 100% survival in a follow-up to ten years in total hip arthroplasty due to severe acetabular protrusio.
Cite this article: Bone Joint Open 2020;1-7:431–437.
Introduction
Acetabular protrusio is a condition in which the femoral head protrudes into the pelvis. It can be primary or secondary due to different pathologies, such as infections, tumours, inflammatory diseases, metabolic diseases, and genetic disorders.1 Therefore, the diagnosis of primary or idiopathic protrusio is reserved for patients in whom a causative factor is not found.
Young patients without severe osteoarthritis (OA) can be managed with femoral or pelvic osteotomies;2 in older patients with OA, the appropriate treatment is the arthroplasty.
Acetabular protrusio is defined using the inner wall of the acetabulum, whether it protrudes medially the ilioischial line more than 3 mm in males or 6 mm in females, or if the centre edge angle of Wiberg is greater than 40°.1,3
In 1978, Sotelo et al4 described a classification of acetabular protrusio. He used the ilioischiatic line as reference in an AP radiograph of the hip, making a measurement of the distance between the acetabular floor and the ilioischiatic line, classifying it as: I) low if the distance is between 1 mm and 5 mm; II) moderate from 6 mm to 15 mm; and III) severe when it is greater than 15 mm.4
Traditionally, the acetabular protrusio has been managed using graft obtained from the femoral head that is placed in the acetabular floor. It is impacted and then the cemented or uncemented acetabular component is implanted;4,5 in some cases, when the rim support is inadequate or the bone stock has poor quality, it is recommended to use an acetabular ring.6 The goal of the bone graft in these patients is to improve the biomechanics of the hip by achieving the restoration of the rotation hip centre. If this is not accomplished, the risk of loosening of the component increases by 24% for each millimetre away from the hip centre of the prosthetic head.7
During total hip arthroplasty (THA), dislocation can be difficult due to the internal protrusio of the femoral head towards the pelvis. Performing forced manoeuvres can cause complications such as femoral fractures, which increases surgical time and therefore delays patient rehabilitation. Traditionally, when a satisfactory dislocation is not achieved, surgeons aim to visualize the femoral neck and perform the osteotomy with the hip reduced, which is known as an in situ osteotomy. The need for in situ osteotomy in hip arthroplasty due to protrusio is reported in the literature as between 8% and 22%.4,8 However, when the protrusio is very severe and the femoral neck is completely covered, visualization of the neck can become difficult. Sometimes the entrapment of the head is worse than expected and the intra-articular adhesions cause stiffness making the dislocation of the hip harder, (Figure 1), which complicates the realization of the in situ osteotomy, making this technique not easy to perform.
To our knowledge, there is no other technique different than the in situ osteotomy described to dislocate the hip in severe protrusio. In these cases, where the acetabular resection of the posterior wall is useful to achieve dislocation of the hip safely and the subsequent acetabular reconstruction. Therefore, the objective of this study is to describe the surgical technique and show the results obtained in ten years of performance.
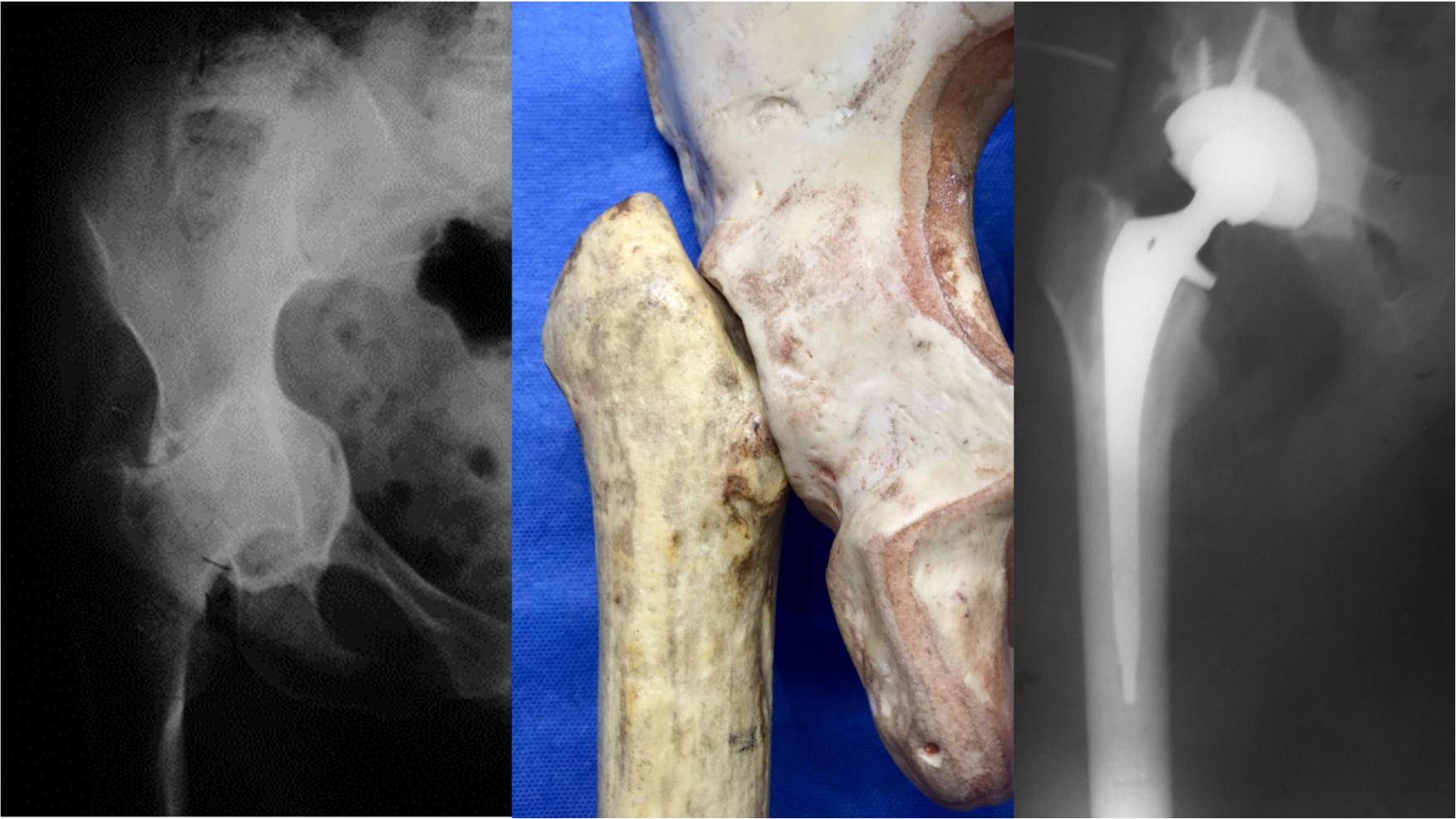
Fig. 1
Severe protrusio; the femoral neck is completely covered and impossible to see.
Methods
This is a case series observational descriptive study, performed in a university hospital, Hospital infantil Universitario de San José. We included all patients who underwent THA due to acetabular protrusion with partial resection of the posterior rim from January 2007 to May 2017. A six-month to ten-year follow-up of the patients was carried out (median 5.5 years, interquartile range 1.4 to 7.6; mean 3.1 years).
All procedures in the study were performed by the same surgeon (HAR) in accordance with the ethical standards of the institutional and national research committee and in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
All patients aged older than 18 years with partial resection of the posterior and a minimum follow-up of six months were included. Patients who underwent THA for any other reason, or patients with incomplete follow-up or records, were excluded.
An assessment of the medical records and completion of the data collection format was carried out in patients who met the inclusion criteria; the information was complemented with phone calls to patients.
Description of surgical technique
Radiological pre-surgical planning was performed with templates in the acetabulum to determine the true centre of rotation of the hip, taking as reference the tear drop.
A posterolateral approach was performed in all cases. On occasion, the protrusio has not only a medial displacement of the femoral head, but also a proximal migration of the femur, making it necessary to carry out a proximal incision to avoid being too high in the approach. External rotators and capsule are identified and repaired for later re-insertion into the greater trochanter. Special care should be taken with the sciatic nerve that is often closer to the greater trochanter due to the protrusion of the femoral head.
The acetabular labrum is completely resected and a meticulous dissection of the posterior wall of the acetabulum is performed with a Cobb dissector to be able to visualize the entire wall (Figure 2). Once the posterior wall is identified, a 3 mm or 4 mm resection of the posterior acetabular rim is performed with an osteotome according to each case (Figure 3). Dislocation of the femoral head is performed with the described technique with a gentle circumduction prior to dislocation, which allows dislocation of the femoral head in all cases. Without performing the cut of the femoral neck, the smaller acetabular reamers can be used to scarify directly on the femoral head and take the necessary graft to place in the acetabular floor. Finally, the femoral neck cut is made, as described in previously published literature9 (Figure 4).
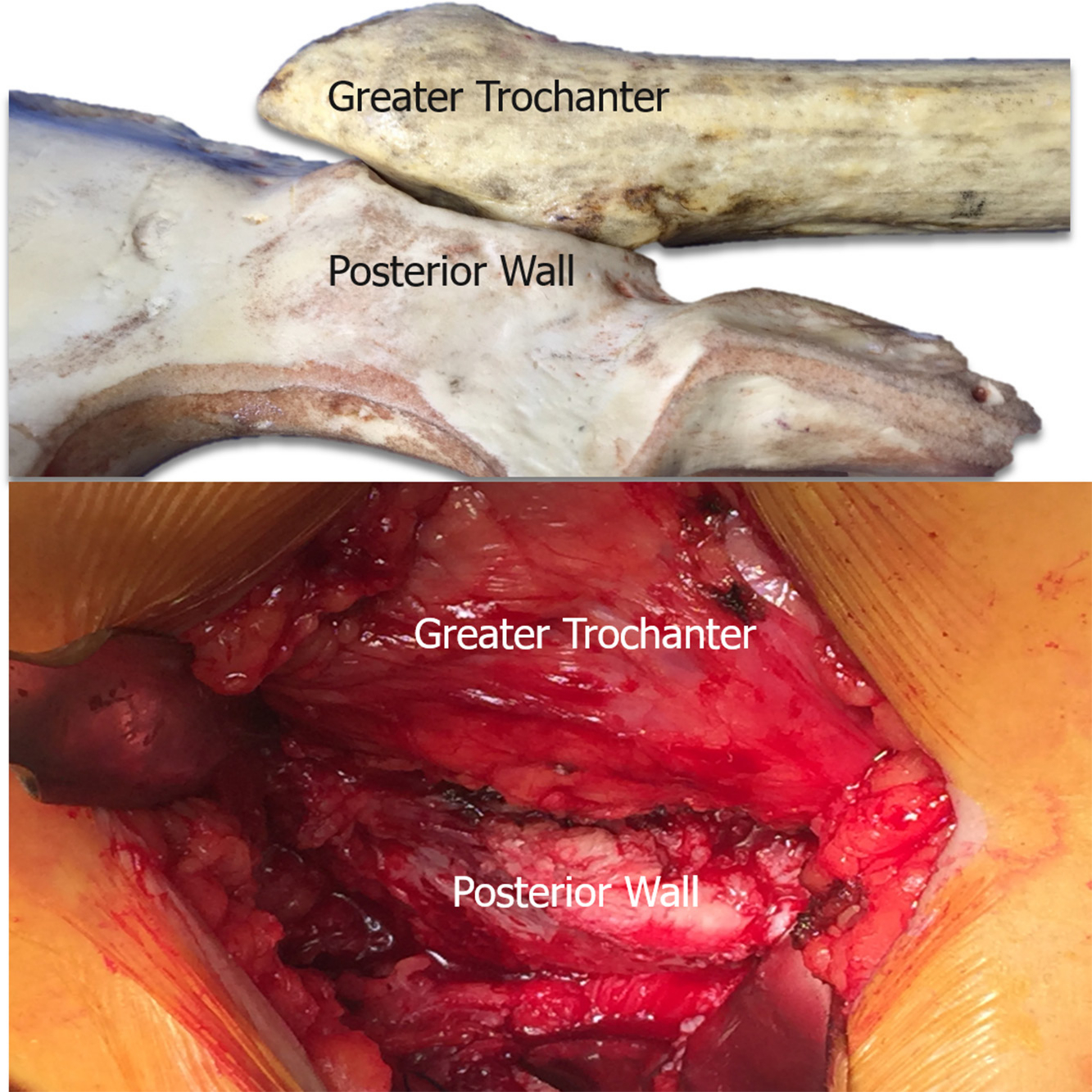
Fig. 2
Posterior wall exposed during arthroplasty and femoral neck completely covered by the posterior wall.
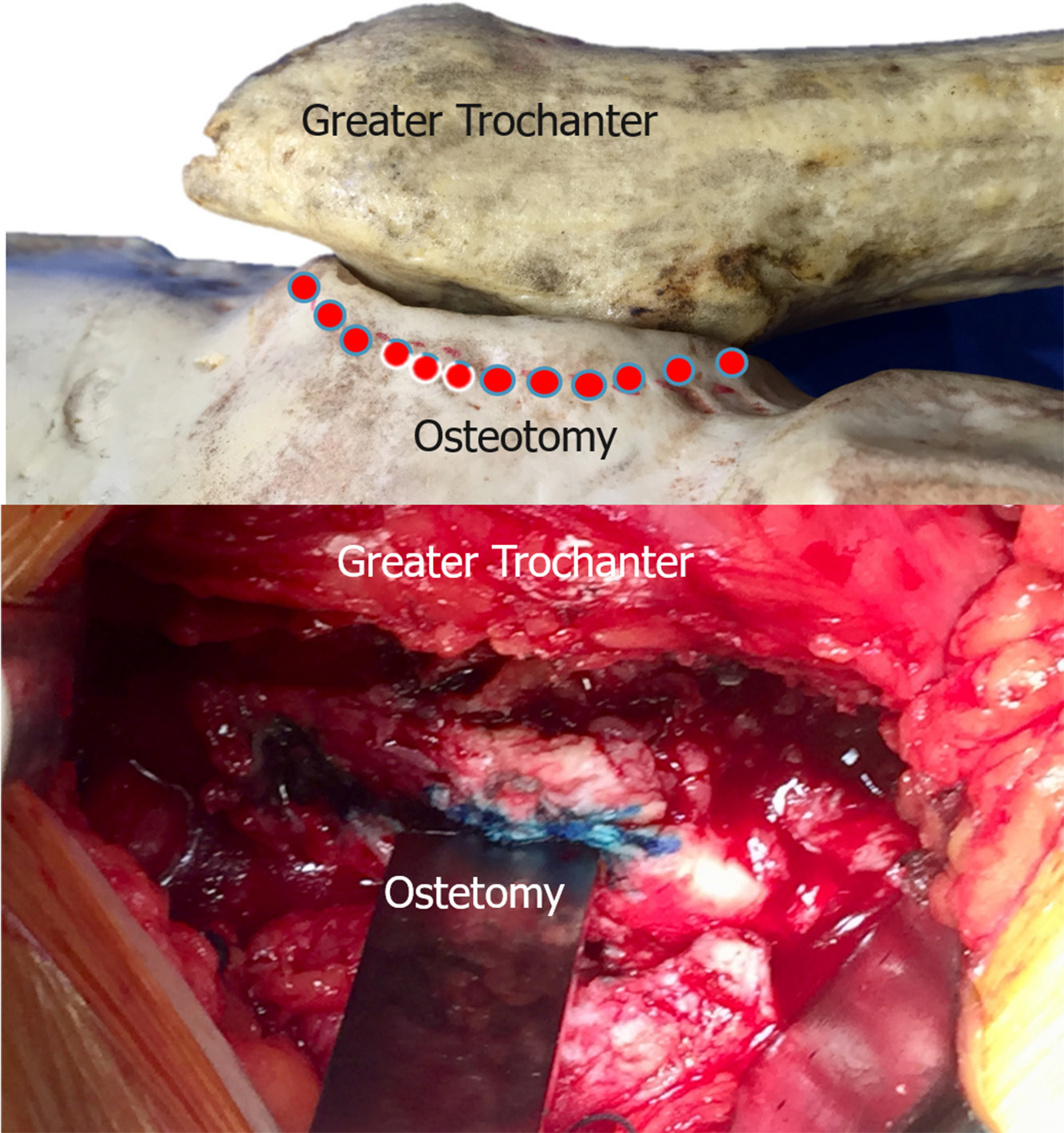
Fig. 3
3 mm or 4 mm osteotomy of the posterior acetabular rim is performed with an osteotome initiating acetabuloplasty of the posterior wall.

Fig. 4
Autograft intake directly reaming from the femoral head after dislocation and before making the femoral osteotomy.
Once the acetabulum is exposed, small acetabular reamers are not used to look for the acetabular floor; instead, the last three reamers that would be used are three sizes smaller than the compoent calculated on the preoperative planning; this gives the circumferential shape of the component to the acetabulum to obtain a peripheral support to it.
The autograft taken from the femoral head is placed in the acetabular floor, and the graft is compressed with an acetabular reamer in reverse. The trial component is then placed evaluating the position, if satisfactory the definitive component is placed obtaining an adequate peripheral support. In all cases, screws in the acetabular component are used (Figure 5). Cemented stems were used in patients with a Dorr type C geometry, rheumatoid arthritis (RA), and in poor bone stock.
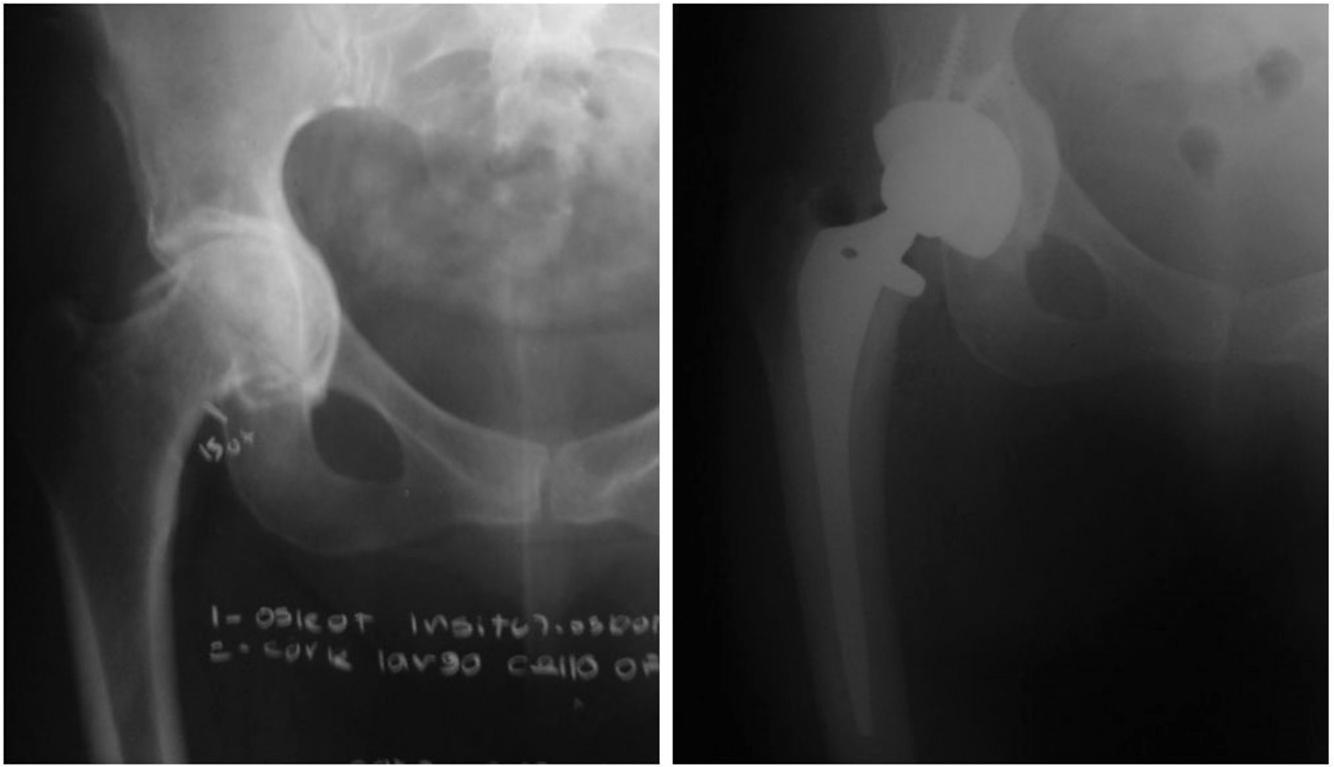
Fig. 5
Preoperative and postoperative x-rays.
Results
All patients were classified as a severe protrusion in the classification of Sotelo and Galarza.4 Overall, 49 hip arthroplasties were performed in 44 patients, all performed by the same surgeon (HAR) with a slight predominance to the left laterality (n = 27). Patients were made up of 34 females and ten males, with an average age of 60 years (37 to 88).
The most common diagnosis was idiopathic in 63% of patients followed by RA. Table I describes the demographic characteristics of the study population. Hybrid fixation was used in 56% of patients (n = 27), uncemented in 40% (n = 20), and cemented in 4% (two hips). The average surgical time was 115 minutes (60 to 240). The average bleeding was 453 cc (300 cc to 100 cc). In all patients, autograft of the femoral head was used to fill the defect.
Table 1.
Demographic characteristics.
| Sample characteristics | Patients (n = 49) |
| Sex, n (%) | |
| Female | 34 (69.3) |
| Male | 10 (20.4) |
| Age, yrs (SD) | 60 (± 4.7) |
| Laterality, n (%) | |
| Left | 27 (57.1) |
| Right | 25 (52.9) |
| Preoperative diagnostic, n (%) | |
| Idiopathic | 28 (63) |
| Reumatoid arthritis | 10 (22) |
| Coxa vara | 2 (4.5) |
| Other | 2 (4.5) |
| Fixation, n (%) | |
| Hybrid | 27 (56) |
| Non-cemented | 20 (40.5) |
| Cemented | 2 (4.5) |
No patient presented intra- or postoperative complications, and until the end of follow-up no patients required arthroplasty revision.
Discussion
THA in some pathologies such as acetabular protrusion requires bone grafting, not only to recover bone mass, but to also allow lateralization of the component, improving the biomechanics of the hip and recover the centre of rotation.
The difficulty in safely accomplishing the dislocation of the hip in these patients due to the medial migration of the femoral head, and the fact that forced manoeuvres are performed during the dislocation, has led to the need of new alternatives to obtain a new technique to carry out the dislocation. Traditionally, the technique described for these cases is the in situ osteotomy, which is reported in the literature as necessary in between 8% and 22% of cases.4,8 But it is worth pointing out that this technique may be uncomfortable, not only due to the narrow work area, but it also leaves the head inside the acetabulum, which forces the surgeon to remove it with a corkscrew or by cutting it into pieces, what can cause the head to be lost as graft. To our knowledge, there is no other surgical technique for the management of hip dislocation in acetabular severe protrusion pathology.
The first protrusion arthroplasty techniques used grafts and cemented components with adequate results. Ranawat et al10 published details of 35 hip arthroplasties performed with graft and cemented components in patients with RA with a follow-up of 12 years; survival of the component was 90% in this time period. Rossemberg et al11 also published similar results, with 36 arthroplasties and an average of seven years follow-up using graft in the floor and cemented components in patients with RA. The study also reports a patient with loosening of the component in this time period. The largest study was carried out by Garcia et al12 with 168 hips. Graft and cemented components where used in patients with mild to severe protrusio using the Sotelo classification; a follow-up of 20 years was carried out, with a survival rate of 79% in mild cases and 63% in severe cases.
Currently, the most common technique is the application of compressed autograft in the acetabular floor and uncemented components. In this series, 49 hips with autograft and non-cemented components were presented with a follow-up of six months to ten years with 100% survival. Similar studies, such as that of Mullaji et al,13 reported details of 30 hips with graft and uncemented components with an average follow-up of 4.2 years, and 90% of good to excellent results without revisions at the end of follow-up.14
This results are similar to the ones reported by Zuh et al;15 the difference is the average follow-up in this case was 4.5 years and without revisions at the end of the follow-up. The study with the largest number of patients (n = 65) is that of Baghdadi et al,8 with an average follow-up of 15 years and a survival rate of 70% (85% for the acetabulum and 83% for the femur).
Our series is comparable with the results reported in the literature so far. However, there are some limitations. As a retrospective study, in which the data used for analysis is taken from the medical records, it may have selection bias as only patients with this pathology are included without a control group. There may also be information loss that is not documented in the medical record.
The study also has several strengths. The sample is quite homogeneous in terms of diagnosis. All procedures were performed by the same surgeon, which reduces the variability of the technique or experience. Autograft was used in all patients with a standardized technique, and the most frequently used component was uncemented (47 uncemented vs 2 cemented), which makes a similar sample in terms of technique and materials.
The technique proved to be safe, since no patient presented intra-operative complications, such as acetabular or femoral fracture. Nor were there complications during the acetabular reconstruction.
However, a question arose during the development of this technique; how much posterior rim can be resected in an acetabular resection? This is difficult question to answer, but based on studies of hips with pincer femoroacetabular impingement, where this issue has been studied, it was found that it is also unclear how much can be resected. There is a report that tries to explain this issue, but it was only able to describe a decrease of 1° to 2° of anterior and lateral coverage in the Wiberg angle for each resected millimetre.16
However, it is important to note that this type of resection is anterior and lateral in native hips. Therefore, they are not comparable when trying to extrapolate these data to a resection of the posterior wall and more in a pathological hip due to acetabular protrusion that is going to be taken to a prosthetic reconstruction.
We resected between 3 mm and 4 mm of the posterior margin of the acetabulum and this size resection is not big . We sustain this appreciation based on two measurements : 1 ) the acetabular ridge above the ischial spine measures 48 mm in males and 41 mm in females; and 2) at the level of the ischial spine, the size of the ream is 40 mm in males and 35 mm in females.17 Those sizes in a patient with protrusio seems to be bigger, so in the worst case scenario there are still a minimum of 36 mm remaining. In our experience, this resection was enough to be able to dislocate all the hips without complication and without compromising the posterior wall in any case, nor leaving it insufficient to support the component.
We wish to share this surgical technique as an option for the dislocation in a patient with severe acetabular protrusion. Additional studies are required with other surgeons to evaluate the reproducibility of the technique.
Conclusion
Partial resection of the posterior rim demonstrated to be a safe technique. There were no intra- or postoperative complications in long-term monitoring. A 100% survival rate was also seen at ten-year follow-up in THA due to severe acetabular protrusio. Partial resection of the posterior rim can be a useful and safe tool replacing the in situ osteotomy.
References
1. McBride MT , Muldoon MP , Santore RF , Trousdale RT , Wenger DR . Protrusio acetabuli: diagnosis and treatment . J Am Acad Orthop Surg . 2001 ; 9 ( 2 ): 79 – 88 . Crossref PubMed Google Scholar
2. Leunig M , Nho SJ , Turchetto L , Ganz R . Protrusio acetabuli: New insights and experience with joint preservation . In: Clinical Orthopaedics and Related Research . 467 , 2009 : 2241 – 2250 . Google Scholar
3. Hooper JC , Jones EW . Primary protrusion of the acetabulum . J Bone Joint Surg Br . 1971 ; 53 ( 1 ): 23 – 29 . Crossref PubMed Google Scholar
4. Sotelo-Garza A , Charnley J . The results of Charnley arthroplasty of hip performed for protrusio acetabuli . Clin Orthop Relat Res . 1978 ; 8 ( 132 ): 12 – 18 . PubMed Google Scholar
5. Ries MD . Total hip arthroplasty in acetabular protrusio . Orthopedics . 2009 ; 32 ( 9 ): 666 – 668 . Crossref PubMed Google Scholar
6. Hansen E , Ries MD . Revision total hip arthroplasty for large medial (protrusio) defects with a rim-fit cementless acetabular component . J Arthroplasty . 2006 ; 21 ( 1 ): 72 – 79 . Crossref PubMed Google Scholar
7. Baghdadi YMK , Larson AN , Sierra RJ . Restoration of the hip center during THA performed for protrusio acetabuli is associated with better implant survival . Clin Orthop Relat Res . 2013 ; 471 ( 10 ): 3251 – 3259 . Crossref PubMed Google Scholar
8. Baghdadi YMK , Larson AN , Sierra RJ . Long-Term results of the uncemented acetabular component in a primary total hip arthroplasty performed for protrusio acetabuli: a fifteen year median follow-up . Int Orthop . 2015 ; 39 ( 5 ): 839 – 845 . Crossref PubMed Google Scholar
9. Rodríguez HA , Rodríguez AR . Reemplazo total de cadera en la protrusión acetabular . Nota técnica. Rev Colomb Ortop y Traumatol . 2015 ; 28 ( 4 ): 154 – 157 . Google Scholar
10. Ranawat CS , Dorr LD , Inglis AE . Total hip arthroplasty in protrusio acetabuli of rheumatoid arthritis arthroplasty of rheumatoid arthritis . J bone Jt Surg Am Vol . 1980 ; 62 ( 7 ): 1059 – 1065 . Google Scholar
11. Rosemberg W Schreurs W , Slooff TJJH . Impacted morsellized bone grafting and cemented primary total hip arthroplasty for acetabular protrusion in patients with rheumatoid arthritis . Acta Orthop Scand . 2000 ; 71 ( 2 ): 143 – 146 . Crossref PubMed Google Scholar
12. Garcia-Cimbrelo E , Diaz-Martin A , Madero R , Munera L . Loosening of the cup after low-friction arthroplasty in patients with acetabular protrusion. The importance of the position of the cup . J Bone Joint Surg Br . 2000 ; 82 ( 1 ): 108 – 115 . Crossref PubMed Google Scholar
13. Mullaji AB , Shetty GM . Acetabular protrusio: surgical technique of dealing with a problem in depth . Bone Joint J . 2013 ; 95-B ( 11 Suppl A ): 37 – 40 . Crossref PubMed Google Scholar
14. Mullaji AB , Marawar SV . Primary total hip arthroplasty in protrusio acetabuli using impacted morsellized bone grafting and cementless CUPS: a medium-term radiographic review . J Arthroplasty . 2007 ; 22 ( 8 ): 1143 – 1149 . Crossref PubMed Google Scholar
15. Zuh S-G , Zazgyva A , Gergely I , Pop TS . Acetabuloplasty with bone grafting in uncemented hip replacement for protrusion . Int Orthop . 2015 ; 39 ( 9 ): 1757 – 1763 . Crossref PubMed Google Scholar
16. Pun SY , Hingsammer A , Millis MB , Kim Y-J . Is increased acetabular cartilage or fossa size associated with pincer femoroacetabular impingement? Clin Orthop Relat Res . 2017 ; 475 ( 4 ): 1013 – 1023 . Crossref PubMed Google Scholar
17. Krebs V , Incavo SJ , Shields WH . The anatomy of the acetabulum: what is normal? Clin Orthop Relat Res . 2009 ; 467 ( 4 ): 868 – 875 . Crossref PubMed Google Scholar
Author contributions
H. A. Rodriguez: Operated on all patients, Wrote and edited the manuscript.
F. Viña: Edited the manuscript.
M. A. Muskus: Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
The authors have no financial or competing interests to disclose.
Ethical review statement
The authors declare that no experiments were performed on humans or animals for this study, no patient data appear in this article, and no conflicts of interest to declare. The present study was evaluated and approved by the hospital research and ethics committee.
Follow H. A. Rodriguez @hugortopedista
Follow M. A. Muskus @MeyMuskus
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









