Abstract
Aims
Severe spinal deformity in growing patients often requires surgical management. We describe the incidence of spinal deformity surgery in a National Health Service.
Methods
Descriptive study of prospectively collected data. Clinical data of all patients undergoing surgery for spinal deformity between 2005 and 2018 was collected, compared to the demographics of the national population, and analyzed by underlying aetiology.
Results
Our cohort comprised 2,205 patients; this represents an incidence of 14 per 100,000 individuals among the national population aged between zero and 18 years. There was an increase in mean annual incidence of spinal deformity surgery across the study period from 9.6 (7.2 to 11.7) per 100,000 individuals in 2005 to 2008, to 17.9 (16.1 to 21.5) per 100,000 individuals in 2015 to 2018 (p = 0.001). The most common cause of spinal deformity was idiopathic scoliosis accounting for 56.7% of patients. There was an increase in mean incidence of surgery for adolescent idiopathic scoliosis (AIS) (from 4.4 (3.1 to 5.9) to 9.8 (9.1 to 10.8) per 100,000 individuals; p < 0.001), juvenile idiopathic scoliosis (JIS) (from 0.2 (0.1 to 0.4) to one (0.5 to 1.3) per 100,000 individuals; p = 0.009), syndromic scoliosis (from 0.7 (0.3 to 0.9) to 1.7 (1.2 to 2.4) per 100,000 individuals; p = 0.044), Scheuermann’s kyphosis (SK) (from 0.2 (0 to 0.7) to 1.2 (1.1 to 1.3) per 100,000 individuals; p = 0.001), and scoliosis with intraspinal abnormalities (from 0.04 (0 to 0.08) to 0.6 (0.5 to 0.8) per 100,000 individuals; p = 0.008) across the study period. There was an increase in mean number of posterior spinal fusions performed each year from mean 84.5 (51 to 108) in 2005 to 2008 to 182.5 (170 to 210) in 2015 to 2018 (p < 0.001) and a reduction in mean number of growing rod procedures from 45.5 (18 to 66) in 2005 to 2008 to 16.8 (11 to 24) in 2015 to 2018 (p = 0.046).
Conclusion
The incidence of patients with spinal deformity undergoing surgery increased from 2005 to 2018. This was largely attributable to an increase in surgical patients with adolescent idiopathic scoliosis. Paediatric spinal deformity was increasingly treated by posterior spinal fusion, coinciding with a decrease in the number of growing rod procedures. These results can be used to plan paediatric spinal deformity services but also evaluate preventative strategies and research, including population screening.
Introduction
Paediatric spinal deformity carries a high risk for deterioration primarily during periods of rapid skeletal growth, producing back pain, respiratory compromise, and impacting on self-image. Scoliosis is the most common type and creates a three-dimensional deformity including axial rotation, causing rib cage deformation and waistline asymmetry, as well as sagittal imbalance with often reduced thoracic kyphosis and lumbar lordosis.
Idiopathic scoliosis represents around 80% of all paediatric patients with spinal deformity.1 Depending upon age at onset this can be classified into infantile (< 3 years), juvenile (4 to 9 years), and adolescent (10 to 18 years) which is the most common having a prevalence of approximately 2% to 3% in most populations.2,3 Other types of scoliosis include neuromuscular, congenital, syndromic, and scoliosis associated with congenital cardiac disease or intraspinal anomalies. Spinal deformities affecting primarily the sagittal plane include Scheuermann’s kyphosis (SK) and spondylolisthesis.
Scoliosis can be managed conservatively or operatively. Bracing is used in skeletally-immature patients with progressive curves < 40° either as the only treatment or as a temporizing measure to delay scoliosis surgery for a later age while preserving spinal growth.1 Scoliosis surgery is indicated if the curve progresses over 40° to 50°, nonoperative management has failed, or in the presence of significant symptoms. Surgery usually comprises spinal fusion, which can be performed through an anterior or posterior approach to the spine. The goals of surgical treatment include deformity correction and spinal stabilization in order to alleviate pain, improve cosmesis, ability to perform activities of daily living and personal care, as well as prevent respiratory compromise or neurological impairment. An array of growth-friendly techniques has been developed to address early onset scoliosis when casting/bracing cannot control the deformity.
The prevalence of scoliosis can vary between 1% and 12%.4 This increases with age with females being affected twice as often as males.5 Epidemiological studies from Arabic countries have indicated the aetiology of scoliosis to include 59% idiopathic, 17% congenital, 11% neuromuscular, and 13% as unclassified.6 Limited information exists regarding the incidence of severe scoliosis requiring surgery,7-9 and no previous study has reported on sagittal plane spinal deformities. Our study aims to define the incidence of paediatric spinal deformity surgery according to underlying diagnosis at the Scottish National Spinal Deformity Centre (SNSDC) between 2005 and 2018, and compare to demographics of the general national population. We also report on changes in the incidence of types of surgery and compare the age at surgery and sex for individual diagnosis during the study period.
Methods
The SNSDC was established in 2005 in order to centralize care for all patients with paediatric spinal deformity in Scotland. We reviewed all patients who underwent spinal deformity surgery between 2005 and 2018 including age at surgery, diagnosis and type of deformity, as well as type of operation. We included patients from birth up to the age of 18 years (before their 19th birthday) which corresponds to the inclusion criteria for our service. Aetiology of spinal deformity was grouped into eight categories: idiopathic, neuromuscular, congenital, syndromic scoliosis, scoliosis associated with spinal dysraphism (intraspinal anomalies) or congenital cardiac disease (CCD), SK, and spondylolisthesis. Patients with idiopathic scoliosis were subdivided into infantile, juvenile, and adolescent based on the age when scoliosis was identified. Table I shows the list of underlying diagnosis among patients with neuromuscular or syndromic scoliosis. Patients who underwent surgery for spinal infection, fractures, or tumours (34 patients), as well as patients with adult presentation spinal deformity (after their 19th birthday) who have been treated as part of our adult deformity service, were also excluded from this study.
Table I.
Distribution of patients having surgery for syndromic and neuromuscular spinal deformity according to underlying diagnosis.
| Syndromic | Neuromuscular | ||
|---|---|---|---|
| Diagnosis | Number of patients | Diagnosis | Number of patients |
| Chromosome abnormality | 63 | Cerebral palsy | 111 |
| Neurofibromatosis type I | 20 | Uncharacterized congenital myopathy | 63 |
| Marfan’s syndrome | 17 | Duchenne muscular dystrophy | 34 |
| Autistic spectrum disorder | 15 | Spina bifida | 17 |
| Mucopolysaccharidosis | 12 | Friedrich’s ataxia | 11 |
| Prader-Willi syndrome | 10 | Rett’s syndrome | 11 |
| Osteogenesis imperfecta | 8 | Spinal cord injury | 10 |
| Achondroplasia | 4 | Developmental delay | 9 |
| Angelman’s syndrome | 4 | Spinal muscular atrophy | 8 |
| DiGeorge syndrome | 4 | Hereditary motor sensory neuropathy | 7 |
| Down’s syndrome | 4 | Encephalopathy | 3 |
| Coffin-Lowry syndrome | 3 | Neuronal migration disorder | 2 |
| Ehler’s Danlos syndrome | 3 | Congenital muscular dystrophy | 2 |
| Sotos syndrome | 2 | Cerebral ataxia | 1 |
| Tuberous sclerosis | 2 | Facioscapulohumeral dystrophy | 1 |
| Arthrogryposis | 1 | Focal dystonia | 1 |
| Disequilibrium syndrome | 1 | Limb girdle muscular dystrophy | 1 |
| Hypermobility syndrome | 1 | Post-viral neuropathy | 1 |
| Nager syndrome | 1 | Dandy-Walker syndrome | 1 |
| Noonan’s syndrome | 1 | Brain injury | 1 |
| Oculofrontonasal syndrome | 1 | ||
| Primary cilia dyskinesia | 1 | ||
| Smith-Magenis syndrome | 1 | ||
| Moebius syndrome | 1 | ||
| Ohdo syndrome | 1 | ||
| Laurence Moon Bardet Biedl syndrome | 1 | ||
| Pierre-Robin syndrome | 1 | ||
| Brown Vialetto Van Laere syndrome | 1 | ||
The annual incidence was calculated by comparing the patients with spinal deformity requiring surgery to the number of individuals of the same age in the general population who were at risk. Population data for individuals aged zero to18 years for the period 2005 to 2018 was retrieved from the National Records of Scotland database. The total number of individuals at risk summing up the year population (zero to 18 years) for the study period was 15,482,868 (7,919,930 males; 7,562,938 females). This data was compared with that for surgical patients from the SNSDC to determine the incidence of different types of spinal deformity requiring surgery. To detect trends in the mean incidence of surgery for different diagnosis of spinal deformity, the study period was subdivided into periods of three to four years comprising 2005 to 2008, 2009 to 2011, 2012 to 2014, and 2015 to 2018. The incidence of surgery for spinal deformity and type of procedure was analyzed across these four chronological periods.
Type of surgery was stratified into: posterior, anterior or anteroposterior spinal fusion, and growing rod procedures. Growing rod procedures included primary insertions, rod lengthening, and revisions. Patients who underwent serial growing rod treatment appeared in the analysis of incidence for surgery at the time of their primary growing rod insertion only.
Statistical Analysis
Statistical analysis was performed using SPSS v. 23.0.0 (SPSS, Chicago, Illinois, USA). Statistical significance was set at p < 0.05. All continuous dependent variables measured for independent groups were assessed for conformity with a normal distribution using the Shapiro-Wilk Test for normality with p < 0.05 indicating deviation from a normal distribution. Independent samples t-test was used to compare normally distributed continuous dependent variables between different groups of patients undergoing surgery for spinal deformity. One-way analysis of variance (ANOVA) with post-hoc Tukey’s range tests was performed to compare means of normally distributed variables between two or more groups of patients, with differences between each group subsequently examined.
Results
A total of 2,205 patients with spinal deformity had surgery between 2005 and 2018, representing a mean annual incidence in the Scottish population of 14 per 100,000 individuals (7 to 21; Tables II and III). The mean incidence of surgery increased from 9.6 (7.2 to 11.7) in the period 2005 to 2008 to 17.9 (16.1 to 21.4) per 100,000 individuals in 2015 to 2018 (p = 0.001). The annual incidence of spinal deformity surgery increased during the study period for both male (p < 0.001) and female patients (p < 0.001; Figure 1). The incidence of surgery for each type of spinal deformity is shown in Figure 2.
Table II.
Annual incidence of paediatric spinal deformity surgery between 2005 and 2018 at the Scottish National Spinal Deformity Centre.
| Mean annual incidence of surgery for paediatric spinal deformity (per 100,000 individuals) | |||
|---|---|---|---|
| Year | Males | Females | Total |
| 2005 | 5.2 | 9.3 | 7 |
| 2006 | 6.8 | 12.4 | 9 |
| 2007 | 6.5 | 17.2 | 12 |
| 2008 | 6.5 | 13.9 | 10 |
| 2009 | 6.3 | 15.5 | 11 |
| 2010 | 10 | 20.2 | 15 |
| 2011 | 7.4 | 19.2 | 13 |
| 2012 | 10.8 | 21.9 | 16 |
| 2013 | 10.3 | 26.1 | 18 |
| 2014 | 9.3 | 23.8 | 16 |
| 2015 | 13.7 | 29.6 | 21 |
| 2016 | 9.8 | 26.2 | 18 |
| 2017 | 11.1 | 21.4 | 16 |
| 2018 | 10.8 | 21.7 | 16 |
Table III.
Mean incidence per time period group of paediatric spinal deformity surgery between 2005 and 2018 at the Scottish National Spinal Deformity Centre.
| Mean incidence of surgery for paediatric spinal deformity (per 100,000 individuals) | |||
|---|---|---|---|
| Time period | Males | Females | Total |
| 2005 to 2008 | 6.2 | 13.2 | 9.6 |
| 2009 to 2011 | 7.8 | 18.3 | 13 |
| 2012 to 2014 | 10.1 | 23.9 | 17 |
| 2015 to 2018 | 11.4 | 24.7 | 17.9 |
| 2005 to 2018 | 8.9 | 19.9 | 14 |
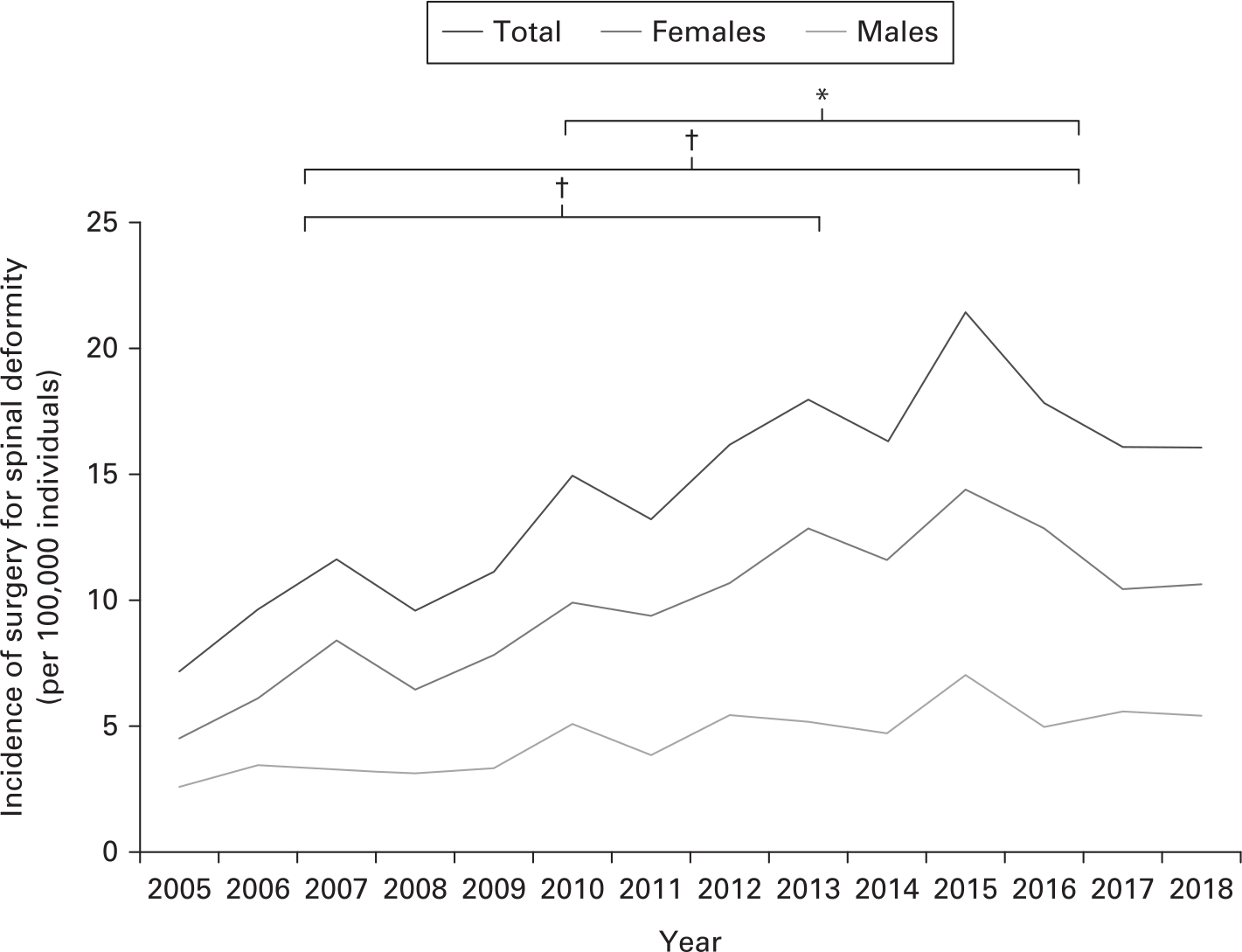
Figure 1
Incidence of surgery for paediatric spinal deformity in the Scottish population between 2005 and 2018 (total group; females; males). Note that the year 2015 recorded the maximum surgical activity for the service. The brackets at the top of the figure represent statistical comparison for the total group between the designated surgical periods of the study (2005 to 2008 compared with 2012 to 2014; 2005 to 2008 compared with 2015 to 2018; 2009 to 2011 compared with 2015 to 2018). *p < 0.05; †p < 0.005.
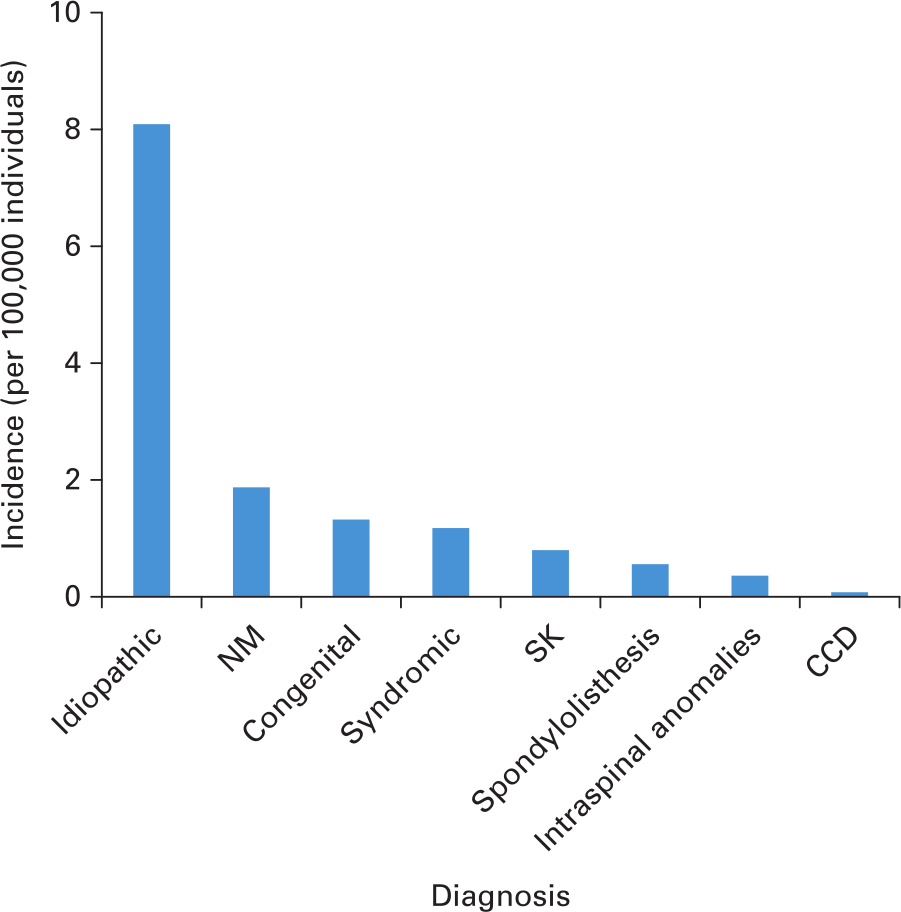
Figure 2
Incidence of surgery for paediatric spinal deformity of different aetiology between 2005 and 2018. CCD, scoliosis associated with congenital cardiac disease; NM, neuromuscular; SK, Scheuermann’s kyphosis.
The number of patients undergoing surgery each year increased over the 14 year period from 81 in 2005 to 175 in 2018 (p < 0.001) with a mean of 158 (81 to 235) patients across the study period and a maximum surgical activity of 235 patients in 2015 (Figure 3). There was an increase in the mean number of surgeries per year, from 142.3 (90 to 178) performed in the 2005 to 2008 period, to 205.5 (183 to 243) in 2015 to 2018 (p = 0.03; Table IV). There was no difference in the mean number of surgeries performed between the later periods of the study (2009 to 2011, 2012 to 2014, and 2015 to 2018; p = 0.572). The number of patients undergoing surgery for each type of spinal deformity is shown in Figure 3.
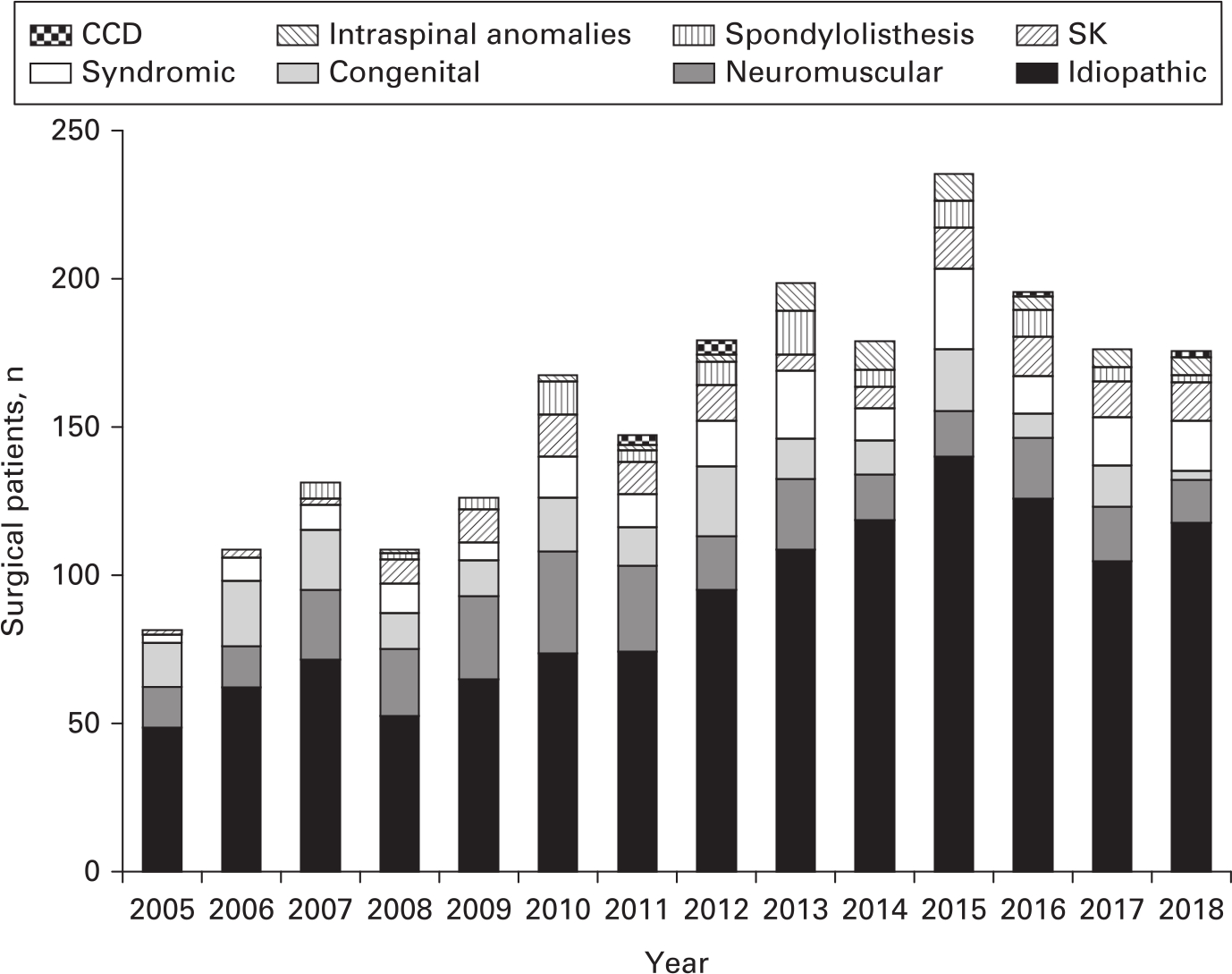
Figure 3
Number of patients undergoing surgery for spinal deformity of different aetiology between 2005 and 2018. CCD, scoliosis associated with congenital cardiac disease; SK, Scheuermann’s kyphosis.
Table IV.
Type of spinal deformity surgery performed in Scotland between 2005 and 2018. Statistical analyses were performed by one-way analysis of variance (ANOVA) with post-hoc Tukey’s range tests.
| Surgical procedures; n = (mean procedures per year) | ||||||
|---|---|---|---|---|---|---|
| Surgical procedure | 2005 to 2008 | 2009 to 2011 | 2012 to 2014 | 2015 to 2018 | Total | p-value (2005 to 2008 vs 2015 to 2018) |
| Growing rods (insertion or lengthening) | 182 (45.5) | 166 (55.3) | 104 (34.7) | 67 (16.8) | 519 (37.1) | 0.046* |
| Posterior spinal fusion | 338 (84.5) | 373 (124.3) | 475 (158.3) | 730 (182.5) | 1916 (136.9) | < 0.001* |
| Anterior spinal fusion | 18 (4.5) | 7 (2.3) | 26 (8.7) | 13 (3.3) | 64 (4.6) | 0.819 |
| Anterior and posterior spinal fusion | 31 (7.8) | 29 (9.7) | 30 (10) | 12 (3) | 102 (7.3) | 0.345 |
| Total | 569 (142.3) | 575 (191.7) | 635 (211.7) | 822 (205.5) | 2601 (185.8) | 0.034* |
-
*
Statistically significant.
Surgery was most commonly performed in patients diagnosed with idiopathic scoliosis, accounting for mean 89 patients (48 to 139) per year. The number of patients undergoing surgery for idiopathic scoliosis over the 14 year period was 1,250, representing 56.7% of all operations (Table V). The mean incidence of patients with idiopathic scoliosis undergoing surgery increased between 2005 to 2008 and 2015 to 2018 (5.2 to 11.1 per 100,000 individuals, p = 0.001; Table VI). The number of patients undergoing surgery for each type of idiopathic scoliosis is shown in Figure 4. There was no significant difference in the incidence of surgery for infantile idiopathic scoliosis (IIS) across the study period (p = 0.695). The mean age at surgery for patients with IIS was significantly lower than for all other diagnoses (IIS: 8.6 years, other diagnoses: 14.4 years; p < 0.001, Table V). The incidence of surgery for juvenile idiopathic scoliosis (JIS) significantly increased across the study period between 2005 to 2008 and 2015 to 2018 (0.2 (0.1 to 0.4) to 0.9 (0.5 to 1.3) per 100,000 individuals, p = 0.009; Table VI). The incidence of surgery for adolescent idiopathic scoliosis (AIS) also increased from 4.4 (3.1 to 5.9) per 100,000 individuals in 2005 to 2008, to 9.8 (9.1 to 10.8) per 100,000 individuals in 2015 to 2018 (p < 0.001; Figure 5).
Table V.
Number and proportion of patients undergoing surgery for spinal deformity of different aetiology in the Scottish National Spinal Deformity Centre between 2005 and 2018 including male to female distribution.
| Aetiology of scoliosis | Number of surgical patients | Percentage of total surgical patients (%) | Mean age at surgery, yrs (range) | Sex, M:F n, (M:F ratio) |
|---|---|---|---|---|
| Total | 2,205 | 100 | 14.2 (1 to 18.9) | 684:1,521 (1:2.2) |
| Idiopathic | 1,250 | 56.7 | N/A | N/A |
| AIS | 1,124 | 51.0 | 15.4 (11 to 18) | 175:949 (1:5.4) |
| JIS | 65 | 2.9 | 12.4 (5 to 17) | 17:48 (1:2.8) |
| IIS | 61 | 2.8 | 8.7 (1 to 17) | 34:27 (1.2:1) |
| Neuromuscular | 297 | 13.5 | 13 (2 to 18) | 141:135 (1:1) |
| Congenital | 207 | 9.4 | 11 (1 to 18.8) | 99:101 (1:1) |
| Syndromic | 183 | 8.3 | 13.6 (2 to 17.8) | 90:86 (1:1) |
| Scheuermann’s kyphosis | 121 | 5.5 | 17 (12 to 18.9) | 76:45 (1.7:1) |
| Spondylolisthesis | 83 | 3.7 | 14.1 (5 to 14) | 30:47 (1:1.6) |
| Scoliosis with intraspinal anomalies | 53 | 2.4 | 13.6 (5 to 18.7) | 14:39 (1:2.8) |
| Scoliosis with congenital cardiac disease | 11 | 0.5 | 16.1 (14 to 17) | 8:3 (2.7:1) |
-
AIS, adolescent idiopathic scoliosis; IIS, infantile idiopathic scoliosis; JIS, juvenile idiopathic scoliosis; N/A, not applicable.
Table VI.
Incidence of surgery for spinal deformity according to underlying aetiology in the Scottish National Spinal Deformity Centre between 2005 and between , 2018. Statistical analyses were performed by one-way analysis of variance (ANOVA) with post-hoc Tukey’s range tests.
| Number of surgical patients (mean annual incidence per 100,000 individuals) | |||||
|---|---|---|---|---|---|
| Aetiology | 2005 to 2008 | 2009 to 2011 | 2012 to 2014 | 2015 to 2018 | p-value (2005 to 2008 vs 2015 to 2018) |
| Idiopathic | 233 (5.2) | 211 (6.3) | 321 (9.7) | 485 (11.1) | 0.001* |
| AIS | 196 (4.4) | 195 (5.8) | 306 (9.3) | 427 (9.8) | < 0.001* |
| JIS | 10 (0.2) | 9 (0.3) | 3 (0.1) | 43 (1.0) | 0.009* |
| IIS | 26 (0.6) | 8 (0.2) | 12 (0.4) | 16 (0.4) | 0.695 |
| Neuromuscular | 75 (1.7) | 93 (2.8) | 58 (1.8) | 71 (1.6) | 0.998 |
| Congenital | 69 (1.5) | 43 (1.3) | 49 (1.5) | 46 (1.1) | 0.599 |
| Syndromic | 30 (0.7) | 31 (0.9) | 49 (1.5) | 73 (1.7) | 0.044* |
| Scheuermann’s kyphosis | 9 (0.2) | 36 (1.1) | 24 (0.6) | 52 (1.2) | 0.001* |
| Spondylolisthesis | 10 (0.2) | 19 (0.6) | 29 (0.9) | 25 (0.6) | 0.470 |
| Scoliosis with intraspinal abnormalities | 2 (0.04) | 4 (0.1) | 20 (0.6) | 27 (0.6) | 0.008* |
| Scoliosis with congenital cardiac disease | 0 (0) | 3 (0.1) | 6 (0.2) | 2 (0.04) | 0.958 |
-
*
Statistically significant.
-
AIS, adolescent idiopathic scoliosis; IIS, infantile idiopathic scoliosis; JIS, juvenile idiopathic scoliosis.
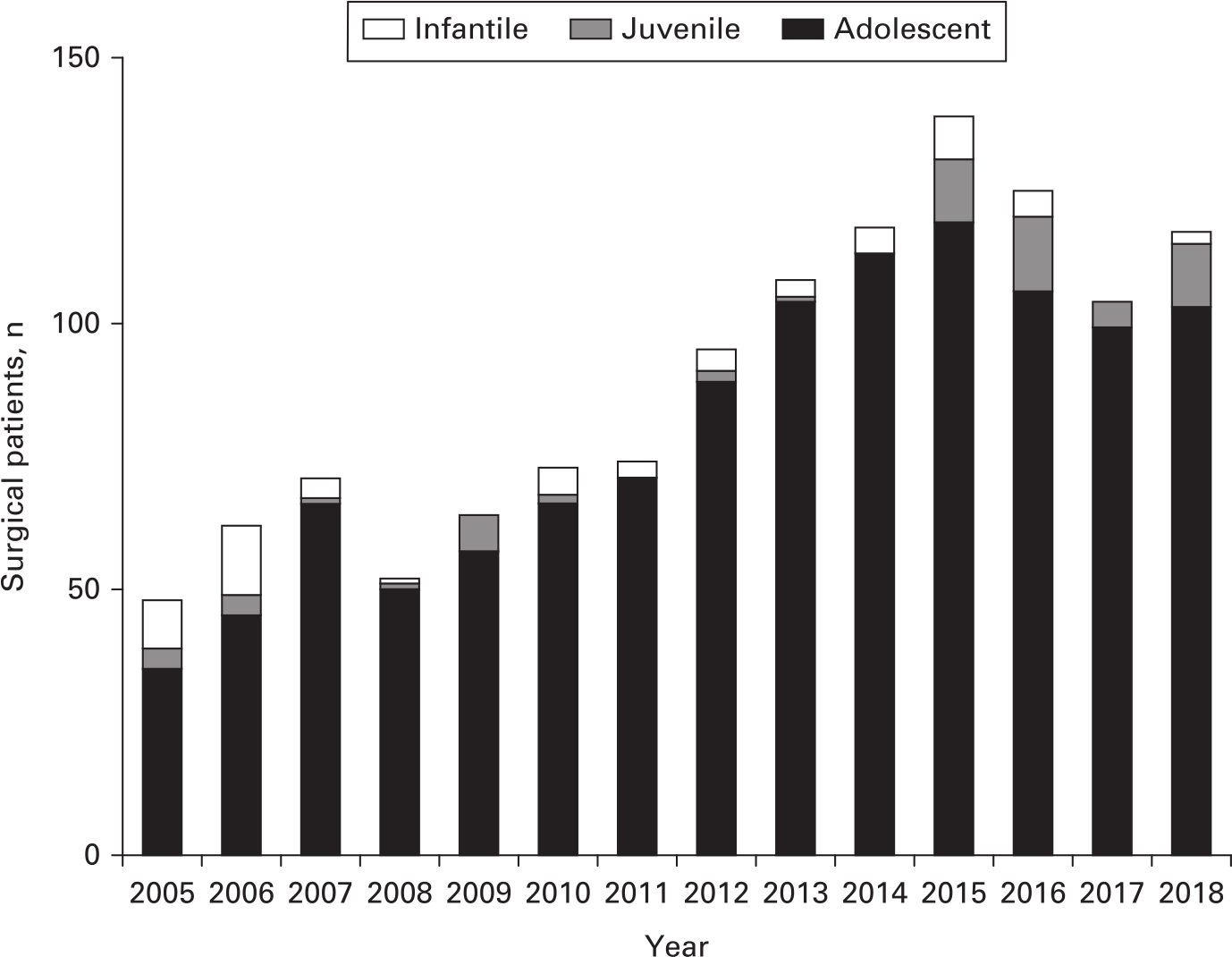
Figure 4
Number of patients with idiopathic scoliosis undergoing surgery between 2005 and 2018.
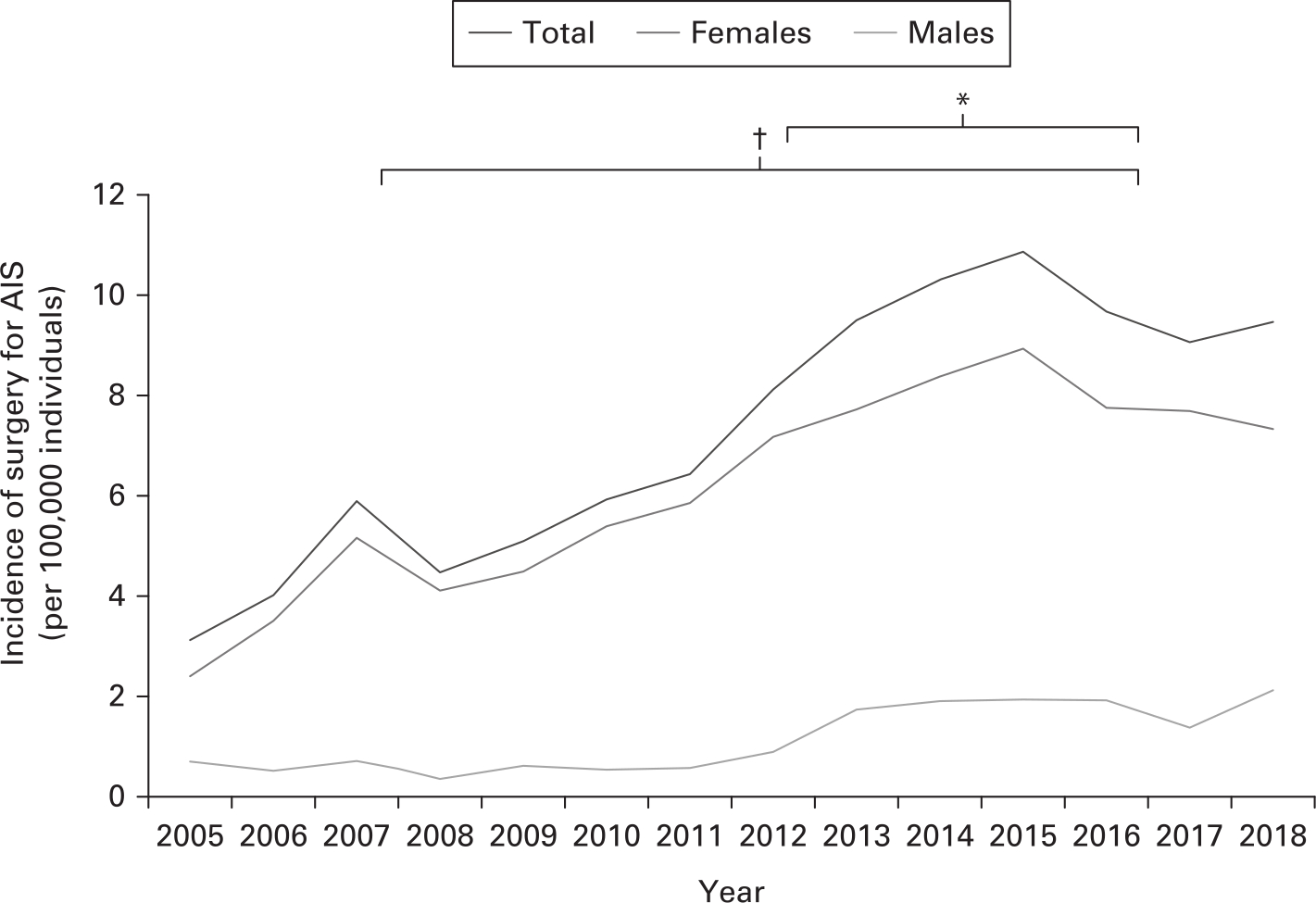
Figure 5
Incidence of surgery for AIS in the Scottish population between 2005 and 2018 (total group; females; males). The brackets at the top of the figure represent statistical comparison for the total group between the designated surgical periods of the study (2005 to 2008 compared with 2015 to 2018; 2012 to 2014 compared with 2015 to 2018). *p < 0.005; †p < 0.05. AIS, adolescent idiopathic scoliosis.
The second most common type of spinal deformity needing surgery was neuromuscular scoliosis comprising 297 patients (13.5% of all operations) and accounting for mean 21 patients (14 to 35) per year. There was no significant difference in the incidence of surgery for neuromuscular scoliosis across the study period (p = 0.998). Congenital scoliosis was the third most common type of spinal deformity with 207 patients across the study period (9.4% of all operations), representing a mean 15 patients (three to 24) per year. The mean age at surgery for patients with congenital scoliosis was significantly lower than for all other diagnoses (congenital: 11 years, other diagnoses: 14.6 years; p < 0.001, Table V). All other types of spinal deformity accounted for a total of 451 surgeries (20.4% of all operations) during the 14 year period (Tables V and VI). There was no significant change in the incidence of surgery for congenital scoliosis (p = 0.559), spondylolisthesis (p = 0.470), or scoliosis associated with congenital cardiac abnormalities (p = 0.958) across the study period. There was a significant increase in the mean annual incidence of surgery for syndromic scoliosis from 0.7 (0.3 to 0.9) in 2005 to 2008 to 1.7 (1.2 to 2.5) per 100,000 individuals in 2015 to 2018 (p = 0.044), SK from 0.2 (0 to 0.7) in 2005 to 2008 to 1.2 (1.1 to 1.3) per 100,000 individuals in 2015 to 2018 (p = 0.001), and scoliosis with intraspinal abnormalities from 0.04 (0 to 0.09) in 2005 to 2008 to 0.6 (0.5 to 0.8) per 100,000 individuals in 2015 to 2018 (p = 0.008; Table VI).
A total of 2,601 procedures were performed during the study period (2005 to 2018). The discrepancy between the number of patients (2,205) and the number of surgeries (2,601) accounts for the repeat procedures within the growing rod group (Table IV). There was significant reduction in the mean number of growing rod procedures from 45.5 (18 to 66) in 2005 to 2008 to 16.8 (11 to 24) in 2015 to 2018 (p = 0.046). There was also significant increase in the mean number of posterior spinal fusions from 84.5 (51 to 108) in 2005 to 2008, to 182.5 (170 to 210) in 2015 to 2018 (p < 0.001; Table IV). There was no significant difference in the number of anterior or combined anteroposterior spinal fusions performed across the 14 year study period. The types of surgical procedures performed each year are shown in Figure 6.
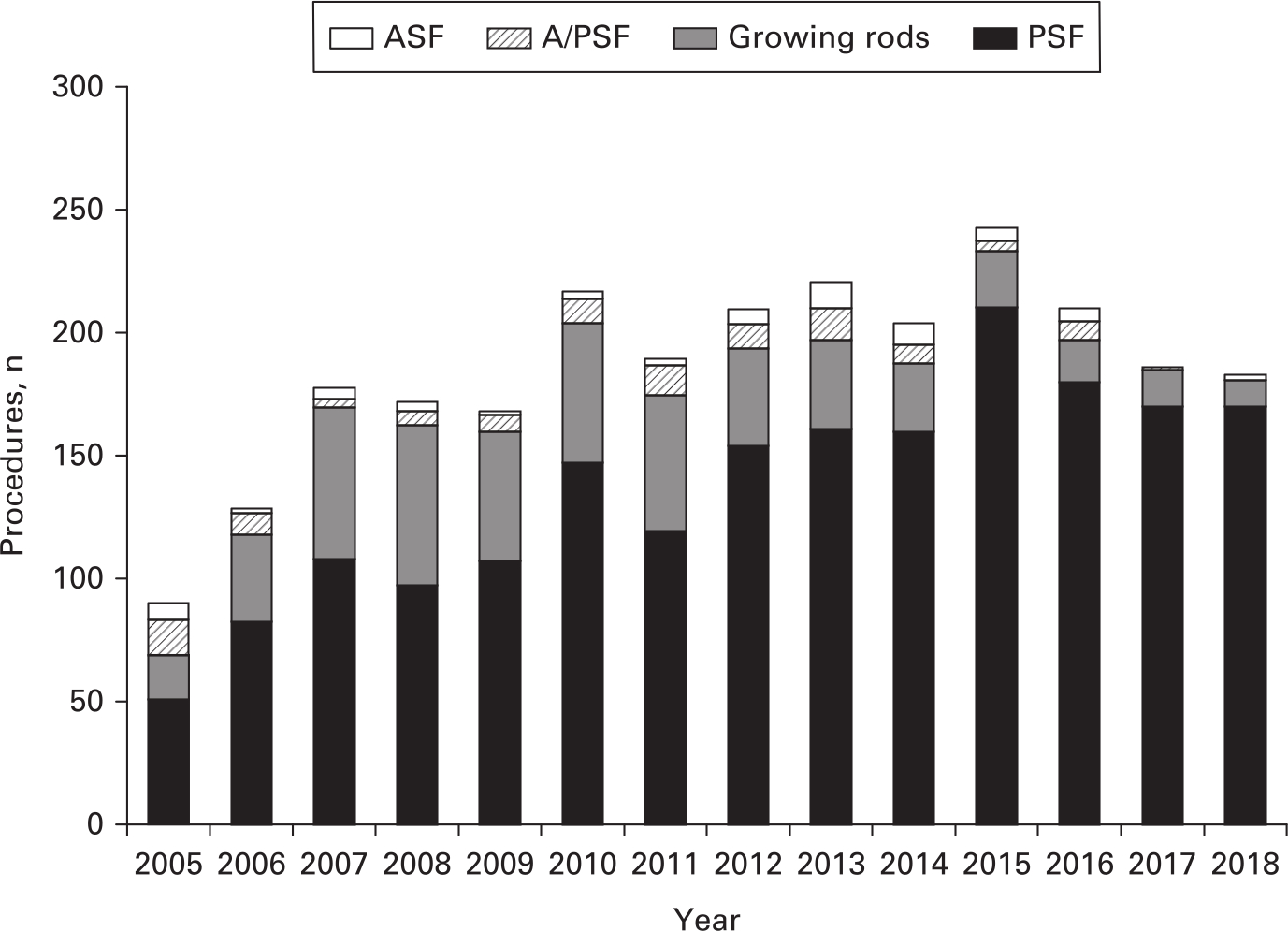
Figure 6
Types and number of surgical procedures performed for paediatric spinal deformity between 2005 and 2018. ASF, anterior spinal fusion; A/PSF: combined anteroposterior spinal fusion; PSF, posterior spinal fusion.
Revision surgery among the whole study cohort between 2005 and 2018 was performed in 65 patients for removal or exchange of instrumentation (2.9%), 35 patients for nonunion (1.5%), 24 patients who had wound debridement due to infection (1.1%), and 19 patients with add-on deformity to extend the fusion (0.8%). This data excludes patients with growing rod procedures who occasionally needed exchange of instrumentation due to failure or to allow additional length for rod extension.
Discussion
The SNSDC is the only service where treatment can be provided for patients with spinal deformity in Scotland. Surgical data from this service, therefore, provides an accurate representation of children and adolescents with spinal deformity who require surgery nationwide and can inform trends in the incidence of these conditions in a predominantly Caucasian population. There has been no previous epidemiological study reporting the incidence of paediatric spinal deformity surgery from a single national centre. Over the 14 year study period (2005 to 2018) the mean population incidence of spinal deformity surgery was 14 per 100,000 individuals and there was a gradual increase from 9.6 in the period 2005 to 2008 to 17.9 per 100,000 individuals in 2015 to 2018.
The calculations reported in our study cannot be compared against epidemiological data on the generic incidence of scoliosis as we have only included patients with severe deformities requiring surgery and excluded all patients treated conservatively or those kept under monitoring. Results from a national school screening programme in Greece (1975 to 1999) reported the incidence of scoliosis as 2.9% with only 0.19% of these patients requiring surgery. The study population was limited to five- to 15-year-olds attending screening for idiopathic scoliosis.2 Other studies including larger age ranges not limited to surgical patients have reported lower scoliosis incidence: China 1.04%, Japan 1.75%, and Saudi Arabia (curves > 20°) 0.3%.4,10 A recent multicentre review of the Swedish National Patient Register identified an annual incidence of surgery for scoliosis of 9.1 per 100,000 individuals;7 in their analysis the authors have included all types of scoliosis but no SK or spondylolisthesis, which were calculated in our study.
Our data review recorded a gradual increase in the incidence of spinal deformity surgery through the 14 year study period which was consistent for both female and male patients. The mean incidence of surgery doubled from 2005 to 2008 (9.6 per 100,000 individuals) to 2015 to 2018 (17.9 per 100,000 individuals; Tables II and III, Figure 1). The increase in this incidence is likely to reflect a combination of better awareness of this group of conditions by the local referring clinicians, development of referral criteria, and more effective surgical techniques to manage the range and severity of deformities with improved patient outcomes. A similar increase in the annual incidence of scoliosis surgery from 5.1 to 9.8 per 100,000 individuals was recorded in the Swedish National Patient Register study.7 There was no difference in the mean incidence of surgery between the last two periods of our analysis (2012 to 2014 and 2015 to 2018) which may indicate well-established patient pathways from initial referral to treatment in our service.
The incidence of surgery for AIS increased across the study period from 4.4 to 9.8 per 100,000 individuals between 2005 to 2008 and 2015 to 2018 (p < 0.001). There was also an increase in the mean annual incidence of surgically treated AIS between 2009 to 2011 and 2012 to 2014 (p = 0.006) but not between 2012 to 2014 and 2015 to 2018 (p = 0.897; Table VI, Figure 5). This indicates that the incidence of surgery for AIS increased from the establishment of the service to the period from 2012 to 2014, but then remained stable in the later years of the study. This supports the development of comprehensive referral pathways for patients with idiopathic scoliosis. AIS has been estimated at 2% to 3% prevalence in ten- to 16-year-olds but more severe curves (> 40°) have a lower prevalence of 0.1% with mean reported incidence for surgery of seven per 100,000 individuals.3 AIS has been consistently identified as the most common deformity requiring surgery: in a Chinese study idiopathic scoliosis comprised 67.7% of all patients;4 an American study reported the incidence of surgery for AIS as 5.8 in 1997 and 7.4 per 100,000 individuals in 2012.8 These figures are similar to our series and to those of the Swedish Register.7 The predominance of AIS within different types of spinal deformity in children and adolescents among the surgical groups may prompt a reconsideration of the scope, efficacy, and cost-effectiveness of national screening programmes as a means to improve population education, as well as achieve an early diagnosis and treatment.11
There was a statistically significant increase in surgical incidence of JIS between 2012 to 2014 and 2015 to 2018 from 0.2 to one per 100,000 individuals (Table VI). In contrast, the rate of surgery for JIS was stable in the earlier periods of the study. This increase may be due to the earlier and improved detection of children with idiopathic scoliosis as education of primary care practitioners and referral pathways have improved. The overall incidence of surgical treatment for IIS was unchanged during the study period (Table VI).
Indications for surgery in neuromuscular scoliosis are not standardized. In a retrospective study of patients undergoing spinal deformity surgery, 2.5% had neuromuscular conditions.9 In our study, neuromuscular scoliosis accounted for 13.5% of all surgical patients, which is similar to reports from the Saudi Arabian screening programme (11%).6 We identified the mean incidence of surgery for neuromuscular scoliosis as two per 100,000 individuals, which remained stable across the study period (Table VI). Surgical decision-making in neuromuscular scoliosis depends on the underlying neurological/myopathic condition and medical comorbidities, as well as the carer’s expectations.
There is limited information on the incidence of congenital scoliosis requiring surgical treatment. Our study has identified the annual incidence of surgery for congenital scoliosis for the 14 year period as 1.4 per 100,000 individuals. Congenital scoliosis can account for 80% of scoliosis in infants and in a screening study in Saudi Arabia, 17% of paediatric patients with spinal deformity were diagnosed with congenital scoliosis.6 Congenital scoliosis accounted for 18.1% of surgically treated patients in a Chinese cohort.4 In our study, congenital scoliosis comprised 9.4% of all surgical patients. In contrast to AIS, the incidence of surgery for congenital scoliosis remained stable between 2005 and 2018 (Table VI). With improved understanding of the incidence and natural history of congenital scoliosis, early prophylactic surgery can be performed to prevent severe deformity resulting in neurological and cardiopulmonary complications.
The incidence of surgery for syndromic scoliosis increased across the study period from 0.7 in 2005 to 2008 to 1.7 per 100,000 individuals in 2015 to 2018 (Table VI). This increase is likely due to improved surgical techniques and medical management for many of these complex conditions. A good example is mucopolysaccharidoses where enzyme replacement therapy and bone marrow transplantation have led to increased survival of patients to adulthood with development of progressive spinal deformity requiring surgery.12,13
The incidence of surgery for SK increased from 0.2 per 100,000 individuals in 2005 to 2008 to 1.2 per 100,000 individuals in 2015 to 2018 (Table VI). Surgery for SK in the form of posterior instrumented fusion has provided, in our experience, consistent results and improved patient outcomes that may explain the increased incidence of procedures in later periods of our study.
The incidence of spondylolisthesis among children and adolescents is 8.7%.14 Most patients will not require surgery, which may explain the relatively low incidence recorded in our study (0.6 per 100,000 individuals for the whole study period). The incidence of surgically treated spondylolisthesis was stable across the study period (Table VI). There was significant increase in the incidence of surgery for scoliosis associated with spinal dysraphism. The low incidence of scoliosis associated with congenital cardiac disease without congenital vertebral anomalies likely explains why no significant changes were identified between 2005 and 2018.
The increase in mean number of surgical procedures each year from 2005 to 2018 probably reflects the improvement in referral pathways for paediatric patients with spinal deformity across Scotland (Table IV). The increase in posterior-only instrumented spinal fusion when compared to anterior or anteroposterior surgery is due to improved results that can be achieved with modern instrumentation techniques, as well as the ability for early detection and treatment of severe deformities as robust referral criteria were developed (Table IV, Figure 6). The reduction in growing rod procedures from 2005 to 2018 reflects our trend to manage early onset scoliosis with casting and bracing until spinal growth and thoracic development permits definitive spinal fusion in order to avoid repetitive surgery.
This study has strengths and limitations. Data collection from a single national centre permits an as complete as possible capture of children and adolescents with spinal deformity requiring surgery in the Scottish population. This study has not analyzed patients managed nonoperatively and, therefore, does not include patients with mild or moderate deformities who we kept under monitoring or treated with bracing. However, the number of patients with severe deformity who were not captured in this study should be limited but cannot be fully excluded. We elected to include all patients who underwent surgery for spinal deformity and not only those with scoliosis, as did previous studies, in order to report the incidence of surgery across all diagnoses that are seen in a typical paediatric spinal practice. The results of our study are most applicable to primarily Caucasian populations, as there are ethnic variations in the incidence of scoliosis. Syndromic and neuromuscular surgical groups included in this study encompass a variety of underlying diagnoses with different clinical expression, surgical considerations, and prognosis. This often makes comparison between reported series difficult.
Defining the incidence of surgery for paediatric spinal deformity has significant implications for healthcare resource management and directing research into the treatment of associated conditions. We recorded an increase in the annual incidence of surgery for paediatric spine deformity between 2005 and 2012 but the mean incidence was stable in the later periods of our study (2012 to 2014; 2015 to 2018). This indicates that it may take regional and national services a number of years to establish robust referral pathways for children with spinal deformity requiring surgery. In AIS and SK specifically, which have demonstrated the highest rate of increase in the early and middle periods of this study, increased medical support may be required to allow early diagnosis and timely referrals to treatment.
This study is the first to report the incidence of surgery for paediatric spine deformity from a single national treatment centre. This incidence doubled between the first (2005 to 2008) and last periods (2015 to 2018) of our study. The most common cause of spinal deformity requiring surgery was AIS. As our service developed there was a gradual increase in the total number of surgical procedures performed. Paediatric spinal deformity was increasingly treated by posterior spinal fusion, coinciding with a reduced utilization of growing rod procedures.
References
1. Sud A , Tsirikos AI . Current concepts and controversies on adolescent idiopathic scoliosis: Part I . Indian J Orthop . 2013 ; 47 ( 2 ): 117 - 128 . Crossref PubMed Google Scholar
2. Grivas TB , Koukos K , Koukou UI , Maziotou C , Polyzois BD . The incidence of idiopathic scoliosis in Greece-analysis of domestic school screening programs . Stud Health Technol Inform . 2002 ; 91 : 71 - 75 . Google Scholar
3. Altaf F , Gibson A , Dannawi Z , Noordeen H . Adolescent idiopathic scoliosis . BMJ . 2013 ; 346 : f2508 . Crossref PubMed Google Scholar
4. Liu SL , Huang DS . Scoliosis in China. A general review . Clin Orthop Relat Res . 1996 ; 323 : 113 - 118 . PubMed Google Scholar
5. Konieczny MR , Senyurt H , Krauspe R . Epidemiology of adolescent idiopathic scoliosis . J Child Orthop . 2013 ; 7 ( 1 ): 3 - 9 . Crossref PubMed Google Scholar
6. Al-Arjani AM , Al-Sebai MW , Al-Khawashki HM , Saadeddin MF . Epidemiological patterns of scoliosis in a spinal center in Saudi Arabia . Saudi Med J . 2000 ; 21 ( 6 ): 554 - 557 . PubMed Google Scholar
7. von Heideken J , Iversen MD , Gerdhem P . Rapidly increasing incidence in scoliosis surgery over 14 years in a nationwide sample . Eur Spine J . 2018 ; 27 ( 2 ): 286 - 292 . Google Scholar
8. Vigneswaran HT , Grabel ZJ , Eberson CP , Palumbo MA , Daniels AH . Surgical treatment of adolescent idiopathic scoliosis in the United States from 1997 to 2012: an analysis of 20,346 patients . J Neurosurg Pediatr . 2015 ; 16 ( 3 ): 322 - 328 . Crossref PubMed Google Scholar
9. Barsdorf AI , Sproule DM , Kaufmann P . Scoliosis surgery in children with neuromuscular disease: findings from the US national inpatient sample, 1997 to 2003 . Arch Neurol . 2010 ; 67 ( 2 ): 231 - 235 . Crossref PubMed Google Scholar
10. No authors listed . Committee UNS. Screening for adolescent idiopathic scoliosis: version 3. UK NSC External Review , 2011 . Available at. legacyscreening.phe.org.uk › policydb_download (date last accessed (Date last accessed 11 February 2020) . Google Scholar
11. Fong DY , Cheung KM , Wong YW , et al. A population-based cohort study of 394,401 children followed for 10 years exhibits sustained effectiveness of scoliosis screening . Spine J . 2015 ; 15 ( 5 ): 825 - 833 . Crossref PubMed Google Scholar
12. Roberts SB , Tsirikos AI . Thoracolumbar kyphoscoliosis with unilateral subluxation of the spine and postoperative lumbar spondylolisthesis in Hunter syndrome . J Neurosurg Spine . 2016 ; 24 ( 3 ): 402 - 406 . Crossref PubMed Google Scholar
13. Roberts SB , Dryden R , Tsirikos AI . Thoracolumbar kyphosis in patients with mucopolysaccharidoses: clinical outcomes and predictive radiographic factors for progression of deformity . Bone Joint J . 2016 ; 98-B ( 2 ): 229 - 237 . Crossref PubMed Google Scholar
14. Tsirikos AI , Garrido EG . Spondylolysis and spondylolisthesis in children and adolescents . J Bone Joint Surg Br . 2010 ; 92-B ( 6 ): 751 - 759 . Crossref PubMed Google Scholar
Author contributions
A. I. Tsirikos: Analyzed the data, Drafted the manuscript, Revised the manuscript.
S. B. Roberts: Analyzed the data, Drafted the manuscript, Revised the manuscript.
E. Bhatti: Collected the data, Analyzed the data.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
No grants or external funding was received by the authors to support research and preparation of this manuscript. No payments or other benefits nor any commitment or agreement to provide such benefits were received from a commercial entity. Neither payment or direction, nor agreement for payment or direction, of any benefits to any research fund, foundation, educational institution or other charitable or non-profit organization with which the authors are affiliated or associated were received from any commercial entity.
Ethical review statement
Institutional approval received.
©2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









