Abstract
Aims
In UK there are around 76,000 hip fractures occur each year 10% to 15% of which are undisplaced intracapsular. There is considerable debate whether internal fixation is the most appropriate treatment for undisplaced fractures in older patients. This study describes cannulated hip screws survivorship analysis for patients aged ≥ 60 years with undisplaced intra-capsular fractures.
Methods
This was a retrospective cohort study of consecutive patients aged ≥ 60 years who had cannulated screws fixation for Garden I and II fractures in a teaching hospital between March 2013 and March 2016. The primary outcome was further same-side hip surgery. Descriptive statistics were used and Kaplan-Meier estimates calculated for implant survival.
Results
A total of 114 operations were performed on 112 patients with a mean age of 80.2 years (SD 8.9). The 30-day and one-year mortality were 1% (n = 1) and 13% (n = 15), respectively. Median follow-up was 6.6 years (interquartile range 6.0 to 7.3). Kaplan-Meier estimates showed a survivorship of 95% at one year and 90% at five years (95% confidence interval 84% to 95%) for cannulated screws. Nine patients underwent further hip surgery: four revision to total hip arthroplasty, one revision to hemiarthroplasty, three removals of screws, and one haematoma washout. Posterior tilt was assessable in 106 patients; subsequent surgery was required in two of the six patients identified with a posterior angle > 20° (p = 0.035 vs angle < 20°). Of the 100 patients with angle < 20°, five-year survivorship was 91%, with seven patients requiring further surgery.
Conclusion
This study of cannulated hip screw fixation for undisplaced fractures in patients aged ≥ 60 years reveals a construct survivorship without further operation of 90% at five years. Cannulated screws can be considered a safe reliable treatment option for Garden I and II fractures. Caution should be taken if posterior tilt angle on lateral view exceeds 20°, due to a higher failure rate and reoperation, and considered for similar management to Garden III and IV injuries.
Cite this article: Bone Jt Open 2022;3(3):182–188.
Take home message
Cannulated hip screws in undisplaced intracapsular neck of femure fractures in patients aged 60 years or older have good outcomes.
Posterior tilt angle in lateral view must be assessed before decision-making to proceed to cannulated screws.
If posterior tilt angle exceeds 20°, the fracture should be considered Garden grade III/IV.
Introduction
In UK, there are annually around 76,000 hip fractures, and undisplaced intracapsular fractures make up 8% of those affecting people aged 60 years or more.1 Treatment options include fixation (with cannulated screws or dynamic hip screws), or replacement of the femoral head with arthroplasty (either hemi or total). There is currently considerable debate as to whether internal fixation is the more appropriate treatment for patients with undisplaced fracture.2,3 Internal fixation has the advantage of a shorter operation, and less blood loss.4 However, it carries the risk of avascular necrosis, malunion, and nonunion, with reported revision rates ranging from 8% to 20%,5-7 and patients converted to arthroplasty following failed internal fixation of femoral neck fractures have poorer outcomes when compared to those treated with primary arthroplasty.8
The authors of the National Institute of Health and Care Excellence (NICE) guideline (CG124, 2017)3 were unable to make a recommendation about management of undisplaced intracapsular hip fractures owing to inadequate evidence. Review of the literature suggested evidence for internal fixation for undisplaced fracture, but none of the studies considered survivorship analysis or long-term mortality and revision rate.3
The primary aim of this study was to describe the survivorship, with a minimum of five years’ follow-up, of patients aged 60 years and over, with cannulated hip screw fixation for undisplaced intracapsular (Garden9 I and II) fractures. A secondary aim was to examine the effect of posterior tilt angle on survivorship.
Methods
A descriptive retrospective observational cohort study was undertaken for a consecutive series of all patients presenting to a large prospectively updated database in our regional trauma centre, between March 2013 and March 2016.
Inclusion criteria were: patients aged ≥ 60 years, Garden classification type I and II on preoperative anteroposterior (AP) view and lateral radiographs or CT, and use of cannulated hip screws. Exclusion criteria included patients with associated ipsilateral fractures (e.g. femoral shaft), and those receiving alternative fixation (e.g. dynamic hip screw), and three patients operated elsewhere and without follow-up after discharge were removed from the analysis. No ethical approval was needed as data were collected retrospectively, and did not involve contacting patients.
Demographic data including age, sex, and American Society of Anesthesiologists (ASA)10 grade were collected (Table I). All preoperative radiographs were reviewed by consultants and orthopaedic residents of over five years’ experience, evaluating intra- and interobserver reliability. Fracture classification was recorded using Garden’s classification on an AP view, and posterior tilt angle (more or less than 20°) was identified from the lateral view using the method described by Palm et al (Figure 1).11
Table I.
Demographic data and radiograph classification.
| Variable | Value, n (%) |
|---|---|
| Total operations, n | 114 |
| Age at operation, yrs | |
| 60 to 69 | 21 (18) |
| 70 to 79 | 25 (22) |
| 80 to 89 | 51 (45) |
| 90+ | 17 (15) |
| Mean age, yrs (SD; range) | 80.2 (9.0; 60 to 98) |
| Sex | |
| Female | 94 (82) |
| Male | 20 (18) |
| ASA grade | |
| 1 | 7 (6) |
| 2 | 63 (56) |
| 3 | 39 (35) |
| 4 | 3 (3) |
| Laterality | |
| Left | 45 (39) |
| Right | 69 (61) |
| Garden classification | |
| 1 | 90 (79) |
| 2 | 24 (21) |
| Posterior tilt angle | 100/114 (87%) |
| < 20° | 100 (94) |
| > 20° | 6 (6) |
| No information | 8 |
| Grade/tilt angle | |
| Garden 1 < 20° | 79 (75) |
| Garden 1 > 20° | 4 (4) |
| Garden 2 < 20° | 21 (20) |
| Garden 2 > 20° | 2 (2) |
-
ASA, American Society of Anesthesiologists; SD, standard deviation.
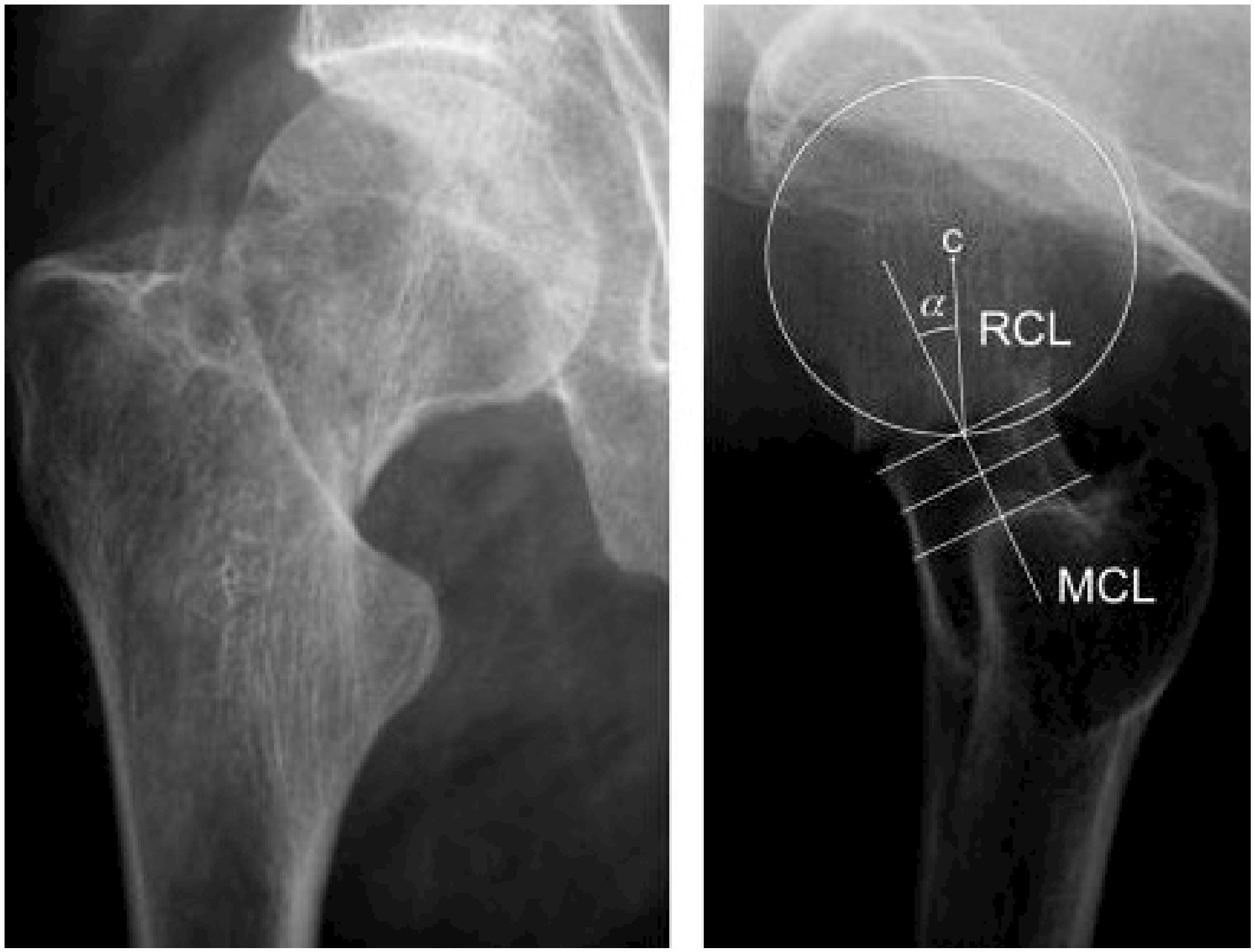
Fig. 1
The posterior tilt is measured as the angle (α) between the mid-column line (MCL) and the radius column line (RCL), which is drawn from the centre (c) of the caput circle to the crossing of the caput circle and the MCL.11
The primary outcome was further same-side hip surgery (either revision, removal, or washout). The secondary outcome was mortality.
Statistical analysis
Data were analyzed by operation rather than by patient. The primary outcome was displayed as Kaplan-Meier estimates (censored at death). Survival was calculated using Kaplan-Meier methodology, and 95% confidence intervals (CIs) derived using the log-log transformation. Associations between groups (Garden classification, posterior tilt angle) were compared using Fisher’s exact tests, and outcomes by group analyzed using log-rank methods. All analyses were undertaken using SAS v. 9.4 (USA). Follow-up is complete to 31 March 2021. The statistical significance threshold used was p < 0.05.
Results
A total of 1,542 patients with hip fractures received surgery between March 2013 and March 2016. Of these, 1,415 (91.7%) were aged 60 or over; 791 (55.9%) had intracapsular fractures, and of these cases, cannulated screw fixation was performed for 128 (16.8%).
After exclusion of people with displaced fractures (Garden III and IV), the final analysis included 114 cannulated screw operations; 14% (114/791) of all operations for intracapsular fracture, and 8% (114/1415) of all hip fracture operations in people aged 60 years or over (Figure 2). All patients received three cannulated screws (size 7.3 mm) in an inverted triangle distribution.
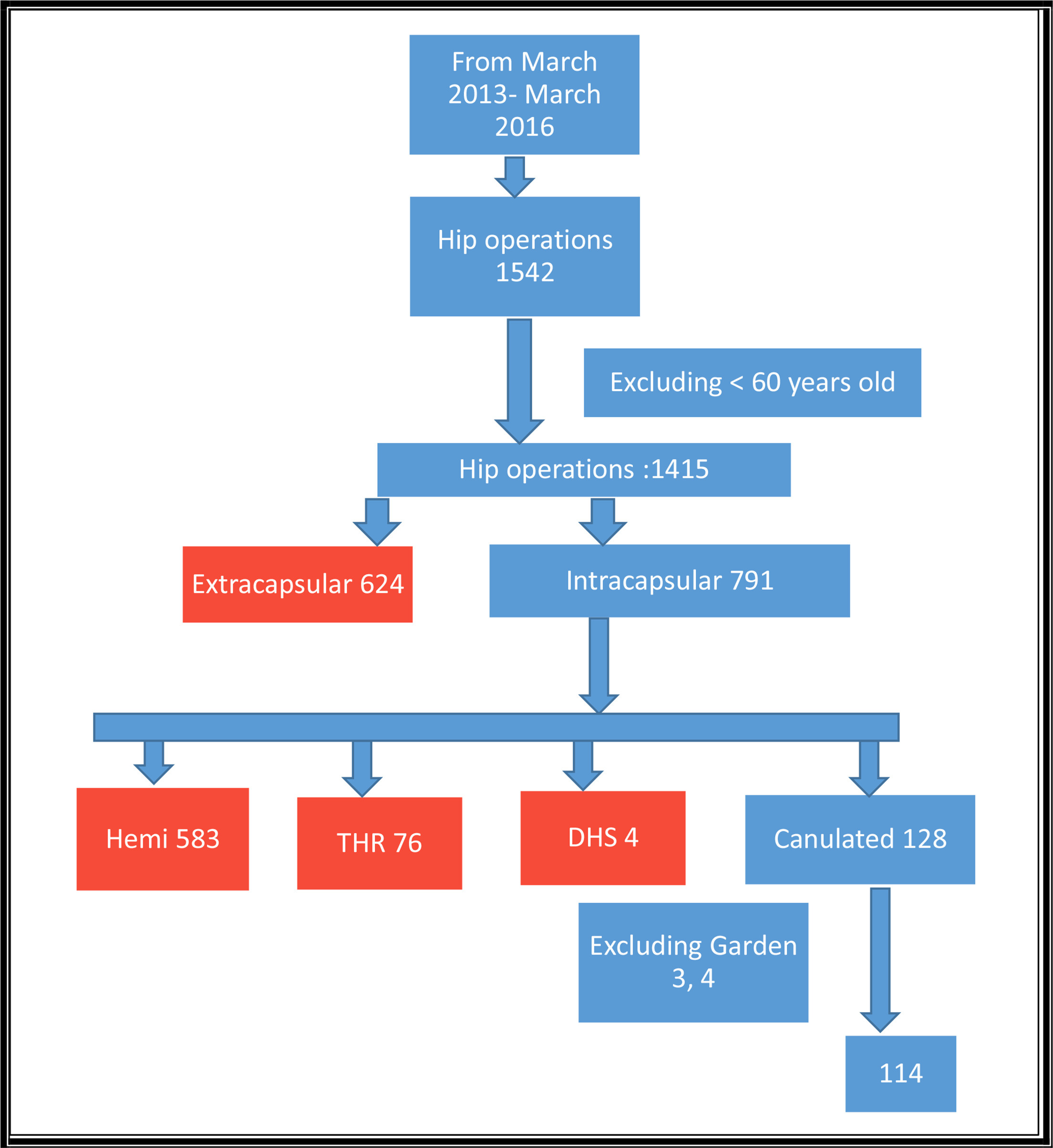
Fig. 2
Flowchart of hip operations and exclusions. DHS, dynamic hip screw; hemi, hemiarthroplasty; THR, total hip replacement.
These 114 operations were undertaken in 112 patients (two patients had both sides fixed on separate admissions). The patients’ mean age was 80.2 years (60 to 98; SD 8.9) and 94 (82%) were females.
No cases had a vertical fracture configuration (Pauwel angle > 50°). Patient demographic data and details of the fracture are given in Table I. Reviewers agreed that all included fractures were undisplaced (Garden I and II) on AP view radiographs.
In eight cases, the lateral view could not be assessed; seven appeared as Garden I on AP view and one appeared as Garden II. Out of the 106 cases where the lateral view could be assessed, six had a posterior tilt angle > 20°. Four of these six cases were considered Garden I on AP view (4/83 (5%) Garden I fractures). The remaining two were in Garden II group: (2/23 (8%) Garden II fractures). There was no significant association between Garden classification and posterior angle (p = 0.609, Fisher’s exact test).
To ensure the reliability of the assessment of Garden classification and posterior tilt, the fractures were each assessed by two observers (JB, SW), and by the same observer two months apart (Table II). Interoperator agreement with respect to Garden classification was 91% (104/114) and intraoperator agreement 89% (101/114).
Table II.
Inter- and intraobserver reliability of posterior angle and Garden classification.
| Initial assessment | n | Interoperator | Intraoperator |
|---|---|---|---|
| n (%) | n (%) | ||
| Posterior angle | |||
| < 20° | 100 | 100 (100) | 100 (100) |
| > 20° | 6 | 5 (83.30) | 4 (66.70) |
| Garden grade | |||
| 1 | 90 | 84 (93.30) | 83 (92.20) |
| 2 | 24 | 20 (83.30) | 18 (75.00) |
There were 15 cases (13%) which were not scored consistently on all three assessments. When considering posterior angle, all 100 cases initially identified as having posterior angle < 20° were confirmed as such. However, only four of the six cases initially identified as having posterior angle > 20° were confirmed on both reassessments. Two factors were considered at a re-rating by the same assessor as having posterior angle < 20°, and one of these was also assessed as having posterior angle < 20° by a different assessor (SW).
Revision rate
Patients were followed up for a minimum of five years. Median follow-up of the 111 remaining procedures was 6.6 years (interquartile range (IQR) 6 to 7); a total of 472.1 person-years of follow-up. Nine reoperations were performed. One haematoma washout was needed nine days after the original operation. One revision to hemiarthroplasty was required at three months; it was not clear whether the revision resulted from nonunion or a new fracture following a fall. It has been considered here as a failure of the original operation. Three patients required removal of screws at eight, 22, and 33 months (all for protruding screws). Four patients had revision to total hip arthroplasty (THA) at five, seven, 23, and 32 months postoperatively: three for avascular necrosis, one for protruding screws.
Survivorship analysis
Survivorship was calculated using a Kaplan-Meier approach, censoring patients at the end of follow-up, loss to follow-up, or death. One-year survivorship was 95%. Five-year survivorship was 90% (95% CI 83% to 95%) (Figure 3).
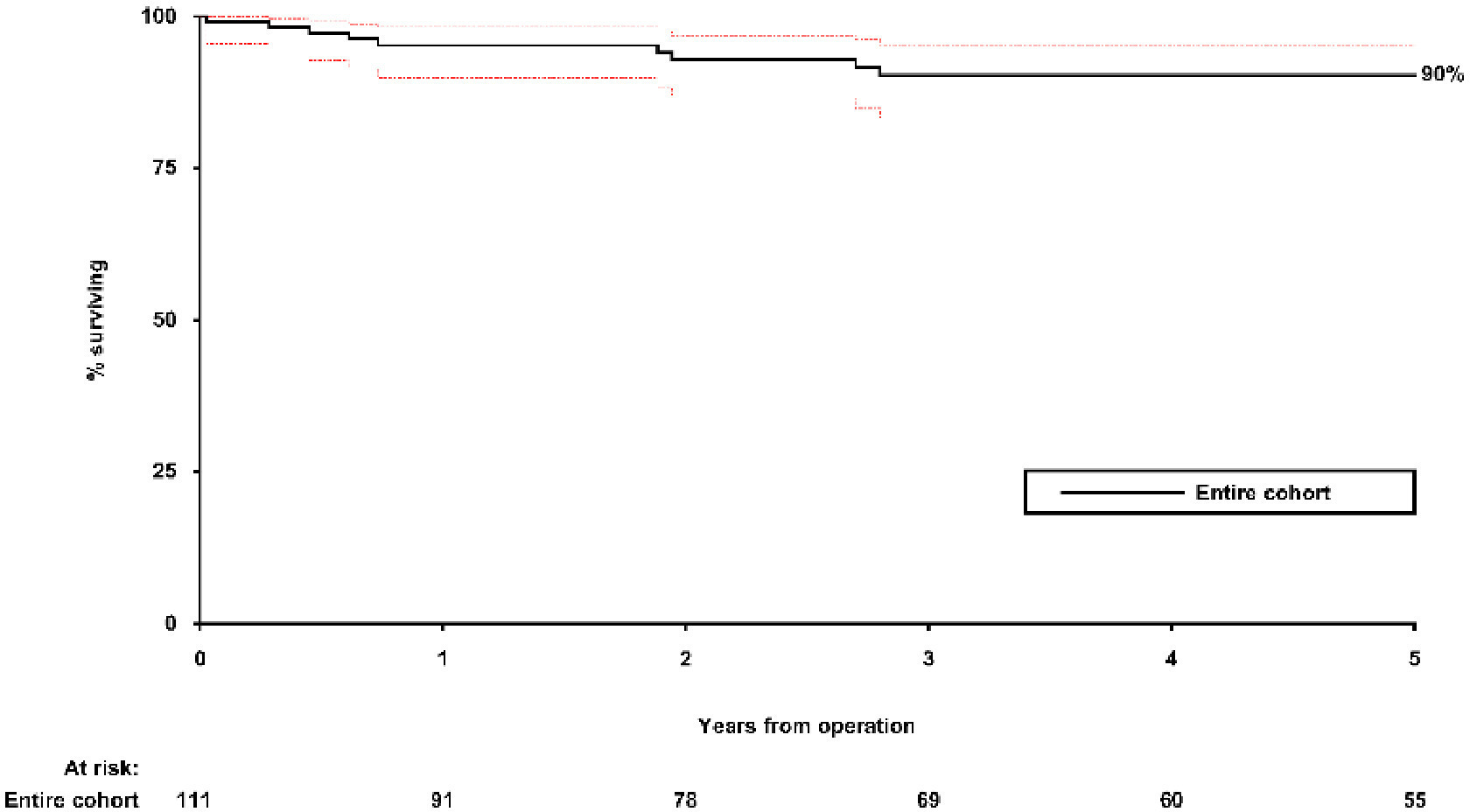
Fig. 3
Survivorship of original operation using Kaplan-Meier curve censoring at death.
The number of revisions was relatively small, but we performed an exploratory analysis by Garden classification and posterior angle. While survivorship was lower in Garden II than Garden I fractures (75% vs 94%, Figure 4b) the difference was not significant (hazard ratio (HR) 5.05 (95% CI 0.96 to 26.51); HR 5.05 (95% CI 0.96 to 26.51); p = 0.084, log-rank test (Figure 4a)).
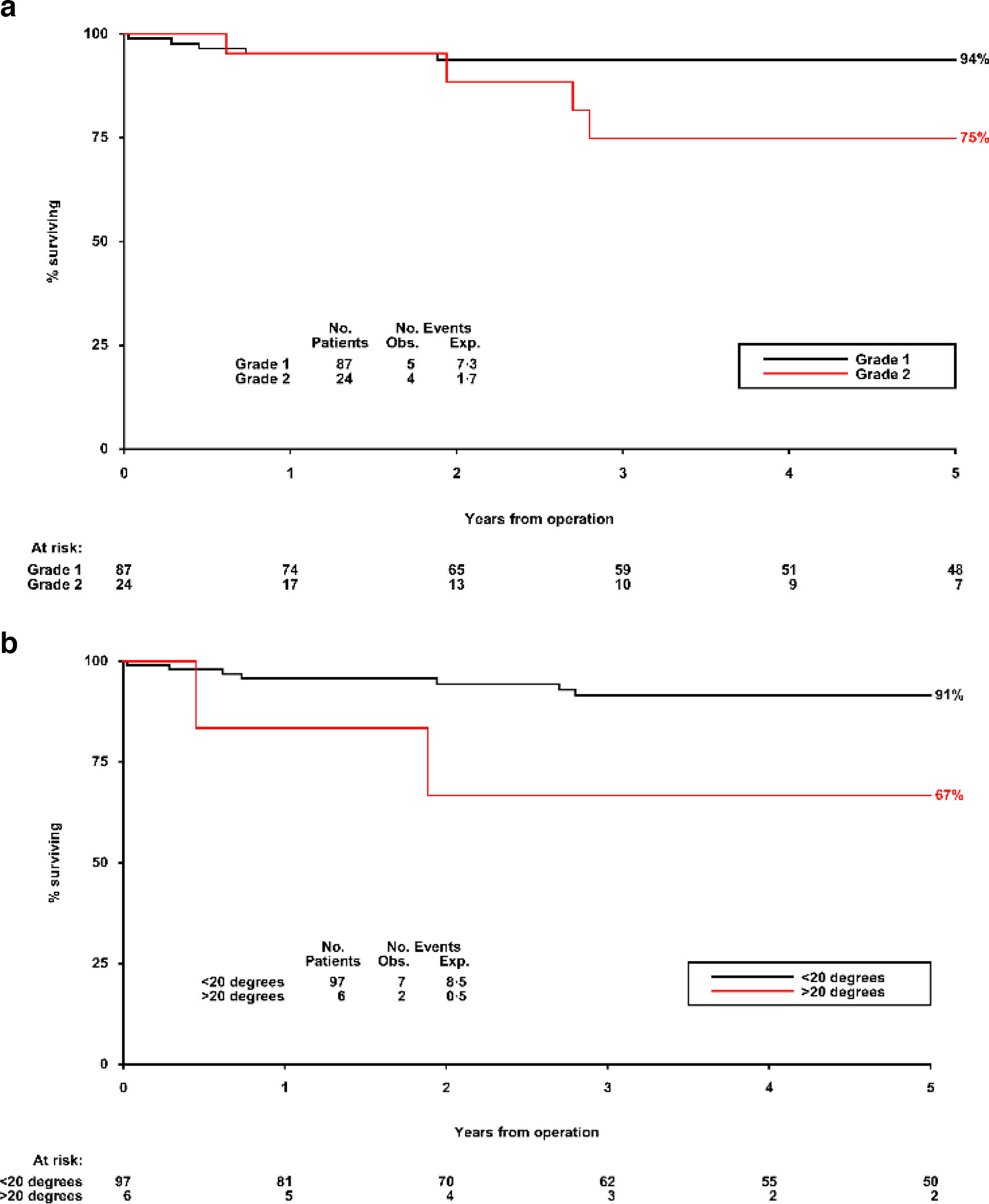
Fig. 4
Kaplan-Meier survivorship censored at death by a) Garden classification. Kaplan-Meier survivorship censored at death by b) posterior angle.
There were two revisions among the six cases with posterior angle > 20°, compared to seven among the 100 patients with posterior angle < 20°; five-year survivorship 67% versus 91%; HR 20.1 (CI 1.23 to 328.4); p = 0.035, log-rank test (Figure 4b).
Mortality
A total of 47 patients died during the follow-up period; no deaths were recorded after revision. The 30-day and one-year mortality were 1% (n = 1, ASA grade 4) and 13% (n = 15), respectively. Five-year survival was 58% (95% CI 49% to 67%) (Figure 5). While survival in men was worse than in women (40% vs 62%; HR 1.39 (95% CI 1.07 to 5.38); p = 0.035, log-rank test), neither Garden classification nor angle were significantly associated with mortality.
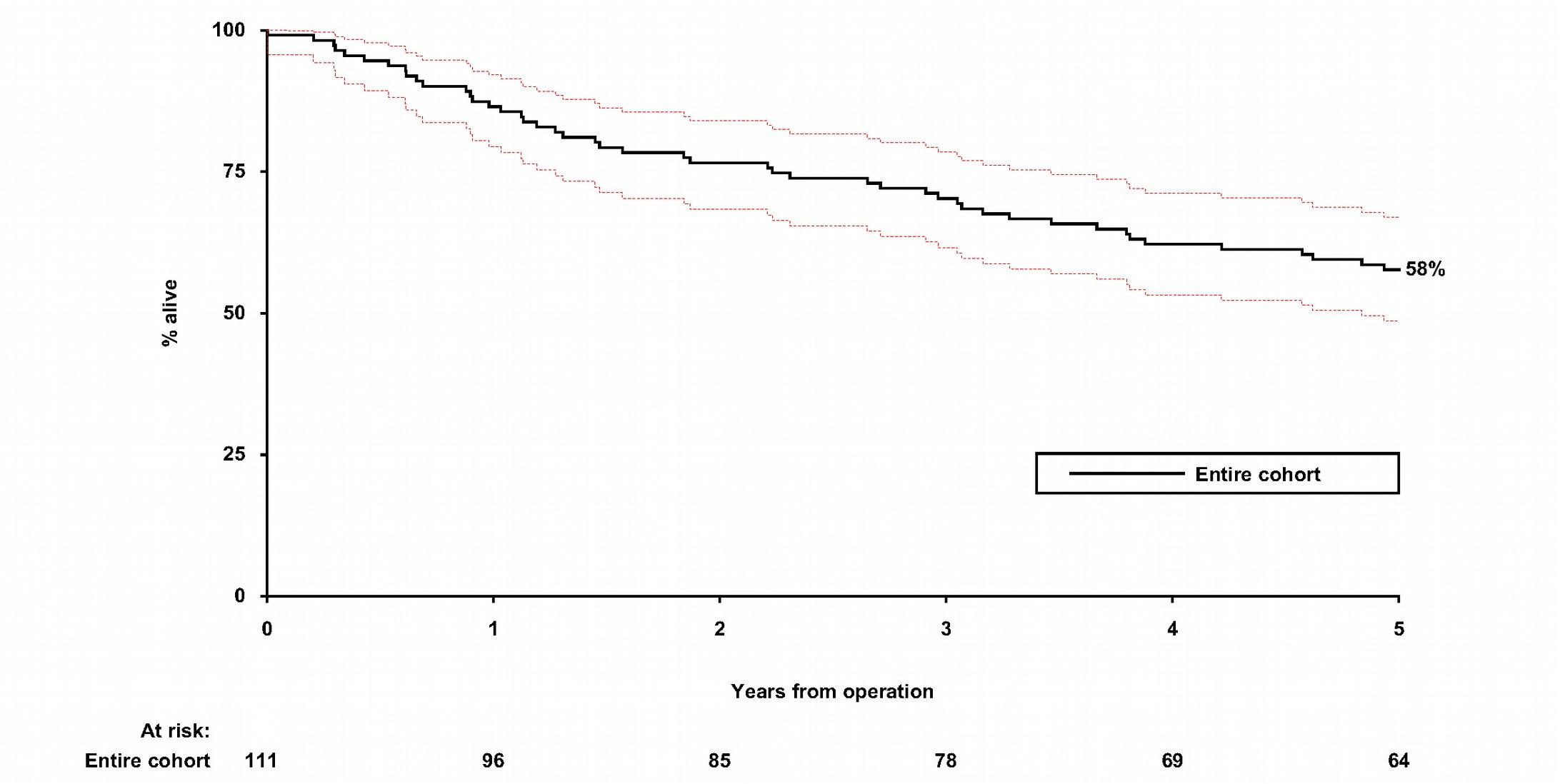
Fig. 5
Kaplan-Meier analysis of overall survival.
Discussion
The authors of the NICE guideline (CG124, 2017) felt there was insufficient evidence as to which method (fixation or arthroplasty) was the most appropriate for undisplaced intracapsular hip fractures, and NICE’s recommendation was that a randomized controlled trial (RCT) was needed.3 Our cohort study will help estimate failure rates in clinical practice, and provides information that will help inform the design and power calculations for such a trial.
Over a minimum of five years’ follow-up, we have shown that fixation using three cannulated screws has a good survivorship with a low complication rate. For Garden I and II fractures, survivorship is 95% and 90% at one year and five years, respectively. Of nine reoperations, only four were revision arthroplasties and only three were for avascular necrosis (AVN). Mortality at one year was 13% (n = 15/112).
We have shown that posterior tilt angle is a prognostic factor for reoperation; if fractures with posterior angle > 20° are excluded, survivorship improves to 91% at five years. This argues that surgeons should use lateral view radiographs to confirm that a fracture is truly undisplaced. If the posterior angle tilt is more than 20°, the fracture is considered Garden III/IV and alternative treatment should be considered.
Traditionally, the Garden classification has been used to classify AP views of intracapsular fracture neck of femur, but there has been no clear method of angle measurement on lateral view,9 though the classification mentioned the importance of intraoperative fracture reduction both in AP and lateral views.
The effect of posterior tilt angle in lateral view on reoperation rate has been highlighted in the last 20 years.12,13 In 2009, Palm et al11 introduced a new method for measurement of posterior tilt angle in lateral view, which later led to a new classification where an undisplaced fracture neck of femur is Garden I or II on AP view, and less than 20° posterior tilt on lateral view.14 This classification was supported by a study which found increased reoperation rates to 19% (8/43) with posterior angle > 20°, as compared to 11% (14/127) in the 10° to 20° category and 6% (9/152) in the < 10° category (p = 0.03).15
In 2019, secondary analysis of the Fracture fixation in the operative management of hip fractures (FAITH) trial found that of 555 patients in the study sample, 67 (12.1%) had posterior tilt 20° or more, and 488 (87.9%) had posterior tilt < 20°. At two years’ follow-up, patients with posterior tilt ≥ 20° had a significantly higher risk of subsequent arthroplasty in contrast to those with posterior tilt < 20°: 22.4% (15 of 67) compared with 11.9% (58 of 488); (p = 0.008).16 Our study was consistent with this, with a reoperation rate 33% (2/6) in tilt angle > 20° versus 7% (7/100) for angle < 20° (p = 0.035, log-rank test).
In 2016, Kang et al17 performed a retrospective cohort study of hip fractures management in an elderly population in South Korea. The study included 81 cases that underwent internal fixation for undisplaced fracture. The rate of AVN was 7.4% and that of nonunion was 4.9%, leading to a 36-month reoperation rate of 6.1%. The complication rate was higher than the figures we found: AVN was 2.6% (3/114) and nonunion 0.8% (1/114). Their study noted that reoperation rate is correlated with the degree of anatomical reduction during operation, but they used Garden classification without measuring posterior tilt angle.
Two RCTs have been reported. In China in 2016, a RCT compared cannulated screws with hemiarthroplasty for undisplaced intracapsular hip fractures in older patients.18 With five-year follow-up, they reported a reoperation rate of hemiarthroplasty group (5.41%, 2/37) that was significantly lower than that for their internal fixation arm (21.4%, 9/41) (p = 0.001). The study was, however, small with 78 patients, and further studies questioned the findings and found no statistically significant difference in reoperation rates between the two groups. Thus, the totality of the evidence remains inconclusive.19
A second RCT in Norway in 2019 compared cannulated screws and hemiarthroplasty for undisplaced intracapsular hip fractures in older people, with two years of follow up.6 This was larger, with 111 patients randomized to screw fixation and 108 to hemiarthroplasty. At two years, there was no significant difference in hip function between the groups. The reoperation rate with screw fixation was 20% compared with 5% in those undergoing hemiarthroplasty. However, internal fixation was with two cannulated screws instead of our three inverted triangle screws, and there was no assessment of posterior tilt angle.
There are currently two ongoing randomized trials looking at internal fixation versus hemiarthroplasty. In Denmark, the SENSE trial started on February 2020.20 It will recruit a total of 330 patients, and will classify fractures with posterior tilt > 20° as displaced, and they will therefore be excluded. The internal fixation will include two or three cannulated screws or dynamic hip screws.1
The Fix or Replace Undisplaced Intracapsular fractures Trial of Interventions (FRUITI) Trial started in the UK in March 2021 and will include a minimum of 878 patients.21 It will look at functional outcome within the first year, as well as long-term outcome with follow-up to five years. Approaches to fixation include sliding hip screw and cannulated screws, and treatment option to be decided by the operating surgeon, without clarification regarding posterior tilt angle.21
This single-centre review of cannulated hip screw fixation for undisplaced fractures of the hip in patients aged 60 reveals a construct survivorship without further operation of 90% at five years. Cannulated screws can be considered a safe reliable option for treatment of Garden I and II fractures for this age group. Caution should, however, be taken if the posterior tilt angle on lateral view exceeds 20° with the potential for a higher rate of fixation failure and reoperation, and these fractures considered more appropriately as Garden III to IV injuries.
This is a single-centre study with retrospective data collection. The main weakness of our study arises from one of its main findings: despite collecting three years of data for all patient presenting to a large teaching hospital, we were only able to identify a small number of failures. This will pose a real challenge to those running or considering future RCTs of this unresolved question. With so few such cases, it was not appropriate to try and relate failure to patient factors such as prior mobility or residence. The nine reoperations we found in this five-year follow-up study need to be viewed in the context of a total number of deaths that was over five times higher, and it is clear that patient factors must always be considered alongside the details of fracture classification. However, the finding regarding posterior angle was striking, though this was not an a priori hypothesis, and as such it requires prospective validation in other large datasets.
References
1. No authors listed . Annual Report 2017. Royal College of Physicians . https://www.nhfd.co.uk/2017report ( date last accessed 16 February 2022 ). Google Scholar
2. Willett S , Alderson P , McFarlane E , Langford P . Surveillance report - Hip fracture (2011), NICE guideline CG124 . December 2015 . https://www.nice.org.uk/guidance/cg124/evidence/surveillance-review-decision-december-2015-pdf-2190593773 ( date last accessed 17 February 2022 ). Google Scholar
3. No authors listed . Hip Fracture: management. National Institute for Health and Care Excellence . 2017 . https://www.nice.org.uk/Guidance/CG124 ( date last accessed 16 February 2022 ). Google Scholar
4. Parker MJ , Gurusamy KS , Cochrane Bone, Joint and Muscle Trauma Group . Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults . Cochrane Database Syst Rev . 2006 ; 2011 ( 4 ): CD001708 . Crossref PubMed Google Scholar
5. Conn KS , Parker MJ . Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients . Clin Orthop Relat Res . 2004 ; 2004 ( 421 ): 249 – 254 . PubMed Google Scholar
6. Dolatowski FC , Frihagen F , Bartels S , et al. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: a multicenter randomized controlled trial . J Bone Joint Surg Am . 2019 ; 101-A ( 2 ): 136 – 144 . Crossref PubMed Google Scholar
7. Sikand M , Wenn R , Moran CG . Mortality following surgery for undisplaced intracapsular hip fractures . Injury . 2004 ; 35 ( 10 ): 1015 – 1019 . Crossref PubMed Google Scholar
8. Richards JT , Overmann AL , O’Hara NN , D’Alleyrand JC , Slobogean GP . Internal fixation versus arthroplasty for the treatment of nondisplaced femoral neck fractures in the elderly: A systematic review and meta-analysis . J Orthop Trauma . 2020 ; 34 ( 1 ): 42 – 48 . Crossref PubMed Google Scholar
9. Garden R . Low-angle fixation in fractures of the femoral neck . J Bone Joint Surg Br . 1961 ; 43-B ( 4 ): 647 – 663 . Google Scholar
10. Saklad M . Grading of patients for surgical procedures . Anesthesiol . 1941 ; 2 ( 5 ): 281 – 284 . Google Scholar
11. Palm H , Gosvig K , Krasheninnikoff M , Jacobsen S , Gebuhr P . A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year . Acta Orthop . 2009 ; 80 ( 3 ): 303 – 307 . Crossref PubMed Google Scholar
12. Conn KS , Parker MJ . Undisplaced intracapsular hip fractures: results of internal fixation in 375 patients . Clin Orthop Relat Res . 2004 ; 421 : 249 – 254 . PubMed Google Scholar
13. Bjørgul K , Reikerås O . Outcome of undisplaced and moderately displaced femoral neck fractures . Acta Orthop . 2007 ; 78 ( 4 ): 498 – 504 . Crossref PubMed Google Scholar
14. Palm H , Posner E , Ahler-Toftehøj H-U , et al. High reliability of an algorithm for choice of implants in hip fracture patients . Int Orthop . 2013 ; 37 ( 6 ): 1121 – 1126 . Crossref PubMed Google Scholar
15. Dolatowski FC , Adampour M , Frihagen F , Stavem K , Erik Utvåg S , Hoelsbrekken SE . Preoperative posterior tilt of at least 20° increased the risk of fixation failure in Garden-I and -II femoral neck fractures . Acta Orthop . 2016 ; 87 ( 3 ): 252 – 256 . Crossref PubMed Google Scholar
16. Okike K , Udogwu UN , Isaac M , et al. Not all Garden-I and II femoral neck fractures in the elderly should be fixed: effect of posterior tilt on rates of subsequent arthroplasty . J Bone Joint Surg Am . 2019 ; 101-A ( 20 ): 1852 – 1859 . Crossref PubMed Google Scholar
17. Kang JS , Jeon YS , Ahn CH , Roh TH . Osteosynthesis versus endoprosthesis for the treatment of femoral neck fracture in Asian elderly patients . BMC Musculoskelet Disord . 2016 ; 17 : 264 . Crossref PubMed Google Scholar
18. Lu Q , Tang G , Zhao X , Guo S , Cai B , Li Q , et al. Hemiarthroplasty versus internal fixation in super-aged patients with undisplaced femoral neck fractures: a 5-year follow-up of randomized controlled trial . Arch Orthop Trauma Surg . 2017 ; 137 ( 1 ): 27 – 35 . Crossref PubMed Google Scholar
19. Dolatowski FC , Randsborg PH , Utvåg SE , Jakobsen RB . Comment on the article: Hemiarthroplasty versus internal fixation in super-aged patients with undisplaced femoral neck fractures: a 5-year follow-up of randomized controlled trial . Arch Orthop Trauma Surg . 2017 ; 137 ( 9 ): 1269 – 1270 . Crossref PubMed Google Scholar
20. Viberg B , Kold S , Brink O , et al. Is arthroplasty better than internal fixation for undisplaced femoral neck fracture? A national pragmatic RCT: the SENSE trial . BMJ Open . 2020 ; 10 : 10 . Crossref PubMed Google Scholar
21. Xavier G , Rafael P-V , Susan D , Antony J , David K . World Hip Trauma Evaluation - FRUITI: Fix or Replace Undisplaced Intracapsular fractures Trial of Interventions . National Institute for Health Research . https://fundingawards.nihr.ac.uk/award/NIHR128399 ( date last accessed 17 February 2022 ). Google Scholar
Author contributions
J. Boktor: Conceptualization, Formal analysis, Methodology, Writing – original draft.
A. Badurudeen: Investigation.
M. Rijab Agha: Investigation.
P. M. Lewis: Writing – original draft.
G. Roberts: Conceptualization, Writing – original draft.
R. Hills: Formal analysis, Writing – original draft.
A. Johansen: Writing – original draft.
S. White: Writing – original draft.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
A. Johansen is the Clinical Lead for the national clinical audit the National Hip Fracture Database (NHFD), managed by the Royal College of Physicians (UK).
Acknowledgements
Mr Declan O’Doherty for his help to understand and plan survivorship analysis.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









