Abstract
Aims
With increasing burden of revision hip arthroplasty (THA), one of the major challenges is the management of proximal femoral bone loss associated with previous multiple surgeries. Proximal femoral arthroplasty (PFA) has already been popularized for tumour surgeries. Our aim was to describe the outcome of using PFA in these demanding non-neoplastic cases.
Methods
A retrospective review of 25 patients who underwent PFA for non-neoplastic indications between January 2009 and December 2015 was undertaken. Their clinical and radiological outcome, complication rates, and survival were recorded. All patients had the Stanmore Implant – Modular Endo-prosthetic Tumour System (METS).
Results
At mean follow-up of 5.9 years, there were no periprosthetic fractures. Clearance of infection was achieved in 63.6% of cases. One hip was re-revised to pseudo arthroplasty for deep infection. Instability was noted in eight of the hips (32%), of which seven needed further surgery. Out of these eight hips with instability, five had preoperative infection. Deep infection was noted in five of the hips (20%), of which four were primarily revised for infection. One patient had aseptic loosening of the femoral component and awaits revision surgery. The Kaplan-Meier survivorship free of revision of any component for any reason was 72% (95% confidence interval (CI) 51.3% to 92.7%), and for revisions of only femoral component for any reason was 96% (95% CI 86.3% to 105.7%) at five years.
Conclusion
Dislocation and infection remain the major cause for failure, particularly in patients with pre-existing infection. The use of dual mobility cups, silver-coated implants, and less aggressive postoperative rehabilitation regimens would possibly aid in the reduction of complications. PFA performed in patients with periprosthetic fracture seem to fair better. This study supports the judicious use of PFA in non-oncological revision hip arthroplasties, and that they be performed by experienced revision arthroplasty surgeons.
Cite this article: Bone Jt Open 2022;3(3):229–235.
Take home message
Proximal femoral arthroplasty (PFA) is a sensible option in revision total hip arthroplasty with massive proximal femoral bone loss.
PFA performed in periprosthetic fractures seem to fair better.
Dislocation and infection continues to be common complication particularly in patients with periprosthetic joint infection. Judiciuos use of dual mobility socket favours consideration.
Introduction
The number of hip arthroplasties being performed around the world is on the increase, which is predicted to result in an increased burden of revision total hip arthroplasties (THA) by 137% until the year 2030.1 The rate of revision arthroplasty from the UK National Joint Registry in patients under the age of 55 years is approximately 12% at 15 years.2 Patients aged under 35 years undergoing THA showed implant survival of 95% at five years, 87% at ten years, and 61% at 20 years.3 Patients who have arthroplasty whilst at a very young age are more likely to require multiple revision procedures in their lifetime. The major challenge faced by an arthroplasty surgeon in these revision scenarios is the excessive bone loss. Various factors such as aseptic osteolysis, infection, periprosthetic fractures, stress shielding, and multiple previous surgeries are considered to be responsible for such bone loss.4-11
The surgical options available to tackle this problem include Girdle stone arthroplasty, impaction bone grafting using allografts, structural allograft-prosthesis composite, modular fluted tapered stems, long-stemmed implants, and proximal femoral arthroplasty (PFA).5,7 However, when it comes to the management of massive bone loss, the reconstructive options available are limited to allograft-prosthesis composite and PFA.4 The use of allografts carries concurrent risk of non-union, infection, graft resorption, and fear of disease transmission.12,13 Additionally, the associated significant period of protected weightbearing is a major issue for the frail and the elderly population in whom these surgeries are generally performed.14
On the other hand, PFA, with the advantage of early postoperative weightbearing, absence of union problems, and with no risk of disease transmission, seems to be a better solution for such complex revision scenarios.15 These reasons have already made PFA the choice of treatment in limb salvage surgeries in orthopaedic oncology.16 PFA is also being increasingly used for non-oncological indications associated with bone loss. However, the wide range of complication rates in the form of dislocation, infection, loosening, and failure of the prosthesis raises concerns.17-19 Hence, further studies are warranted to look at the outcomes of PFA in non-neoplastic conditions.
The preliminary aim of the present study is to evaluate the clinical outcome and five-year survivorship in patients undergoing PFA for non-neoplastic indications in complex revision hip surgeries with massive bone loss. The factors that influenced the outcome were also explored.
Methods
This Institutional Review Board-approved study was a retrospective review of consecutive series of multi-surgeon performed PFA for non-neoplastic indications in a tertiary referral centre for arthroplasty. Data was collected from the joint arthroplasty database from January 2009 to December 2015. All patients apart from the ones who died or lost to follow-up were followed up to a minimum of five years. The Stanmore modular, cemented stemmed implants (Stanmore Implants, UK) was used in all patients in this study.
A total of 25 patients underwent PFA for non-neoplastic indications. The indications for PFA are as presented in Figure 1. In all, 11 of the cases (44%) had periprosthetic joint infection (PJI) as the indication for the use PFA. The organisms cultured from these cases with PJI prior to the index PFA included Staphylococcus aureus in five (45.4%), Escherichia coli in three (27.3%), Enterococcus faecalis in two (18.2%), Staphylococcus epidermis in one (9.1%), Streptococcus in one (9.1%), Campylobacter in one (9.1%), Proteus in one (9.1%), and Micrococcus in one (9.1%). The decision for two-stage or single-stage revision for these patients were taken after involving the multidisciplinary team comprising of senior hip surgeons, radiologists, microbiologists, pathologists, and the anaesthetists. Out of the 11 cases with preoperative infection, a two-staged revision using antibiotic loaded cement spacer was performed in ten. Only one patient had undergone single-stage revision as the patient was medically unfit for a two stage procedure. Two PFAs in the PJI group had silver-coated implants (Agluna; Stanmore Implants). None of the patients required any plastic surgeons’ input.
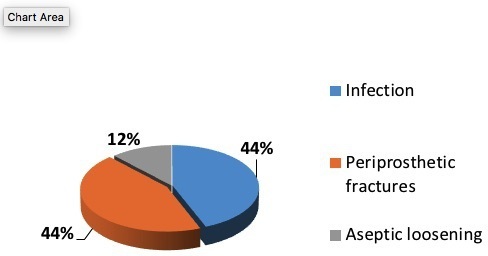
Fig. 1
Pie diagram depicting indications for proximal femoral arthroplasty.
Surgical technique
The surgeries were performed by the senior hip surgeons (AG, NS, MP) at the same institute. With the patient in lateral decubitus position, posterior approach was the default approach. The mean surgical time was found to be 209.2 minutes (135 to 291). A trochanteric slide osteotomy was used when found necessary to preserve the abductors and vastus lateralis. The pre-existing acetabular components were assessed for adequacy of positioning, as well as stability, and were retained in seven cases. Standard surgical techniques were followed for femoral canal preparation. Trial components were used to achieve optimal soft-tissue balance and fine tune the resection level. All PFAs were cemented in place. Care was taken to preserve the cancellous bone for a better cement interdigitation. A cement restrictor was inserted in the distal segment when possible to achieve adequate pressurization and an optimal cement mantle.
The final implant was inserted taking care to achieve direct and firm contact between the hydroxyapatite (HA)-coated collar of the implant and the host bone without any cement inter-positioning. Depending upon the intraoperative stability of the hip joint, a decision was taken by the surgeon with regard to the optional use of constrained acetabular liners. In this series, constrained liner was used in four and dual mobility cups in two cases. The trochanter was reattached in 12 cases using trochanter reattachment plate. Among the rest of the hips without the trochanter, the abductors were reattached using heavy non absorbable sutures to the shoulder of the proximal aspect of the femoral component. There was no preponderance to instability based on the type of trochanter reattachment.
Prophylactic antibiotics were used in all the patients in the form of intravenous teicoplanin and oral ciprofloxacin until final culture reports were available from the intraoperative samples. Appropriate antibiotics were continued only in the presence of a positive culture report and in discussion with our microbiologists. All the patients also received thromboprophylaxis as per the local trust guidelines. Postoperatively, the majority of the patients (64%) were allowed either partial weightbearing or weightbearing as tolerated. The remaining patients were kept on toe touch weightbearing for the initial six weeks, and then progressed to increasing weightbearing. Abduction brace was not used as a standard postoperative precaution in this series.
Patient evaluation
The patients had routine clinical follow ups at six weeks, three months, six months, one year, and then annually. The clinical and radiological data was obtained retrospectively from the institution’s electronic database, medical records, and picture archiving and communications system (PACS). The mobility status, complication rates, and the subsequent management of these complications were determined from these records. The radiological evaluations were conducted by reviewing the serial anteroposterior and lateral radiographs. Aseptic loosening of the femoral component was defined as circumferential radiolucent line on all views and/or subsidence around the stem.
Statistical analysis
Survival analysis was performed using the Kaplan-Meier method with 95% CIs. The following end points were used to assess survivorship: revision or removal of femoral component for any reason, revision of any component for any reason, and revision of any component for any reason excluding posterior lip augmentation device (PLAD) application. All analysis was performed using SPSS software version 23.0 (SPSS, USA).
Results
A total of 25 proximal femoral arthroplasties were performed in patients with a minimum follow-up of two years. The mean age of the study group was found to be 71.8 years (50 to 89). The mean follow-up was 5.9 years (2.0 to 11.8). The patients had undergone a mean of 2.4 total hip arthroplasties (1 to 5) prior to the index PFA. The summary of the patient’s demographics is depicted in Table I. Six out of the 25 patients died due to reasons unrelated to the surgical procedure. The hips in these six patients survived for a mean of 3.2 years (2.2 to 5.1). Four hips were lost to follow-up. The remaining 15 hips (60%) had a minimum follow-up of five years. All patients had a minimum of type 3B femoral deficiency based on classification of Paprosky.20Figures 2a and 2b demonstrates the radiographs of a representative case from the study sample.
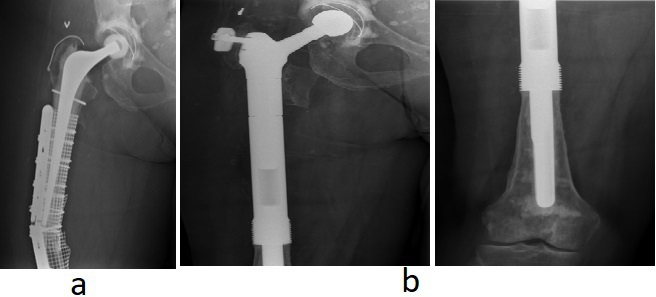
Fig. 2
a) Preoperative radiograph of a failed periprosthetic fracture fixation with profound bone loss. b) Postoperative radiograph at nine years follow-up.
Table I.
Demographics of the study group.
| Variable | Data |
|---|---|
| Total hips, n | 25 |
| Hips with minimum five years follow-up, n (%) | 15 (60) |
| Lost to follow-up, n | 4 |
| Death, n | 6 |
| Mean age, yrs (range) | 71.8 (50 to 89) |
| Left:right, n | 09:16 |
| Male:female, n | 10:15 |
| Mean surgical time, mins (range) | 209.2 (135 to 291) |
A total of 11 cases had a preoperative diagnosis of PJI. Clearance was achieved in seven out of 11 cases, ten of whom had undergone two-stage revisions. Four out of the 11 patients continued to have postoperative infection. Among them, one had a pseudo arthroplasty and the other three went on to having suppressive antibiotic therapy.
A total of 11 patients (44%) had complications. The most common complications were dislocation in eight patients, followed by infection, and one aseptic loosening of the stem at 6.9 years. Figure 3 illustrates the demographics of the pre-existing indication and outcome. All the eight cases (32%) of dislocation occurred within five months from the index procedure. Of the eight patients with dislocation, five underwent a PLAD placement, two had a socket revision with a constrained liner, and one had successful results with manipulation under anaesthesia with an abduction brace for eight weeks. The one with aseptic loosening had subsidence of the femoral component and progressive radiolucency in all zones and awaits revision surgery with a custom made implant. There were no cases of established periprosthetic fractures around the femoral component. The Kaplan-Meier survivorship at five years for revision of femoral stem for any reason was 96% (95% confidence interval (CI) 86.3% to 105.7%), 72% (95% CI 51.3% to 92.7%) for revision of any component for any reason, and 87.7% (95% CI 70.2% to 105.1%) for revision of any component for any reason excluding PLAD application (Figures 4 to 6).
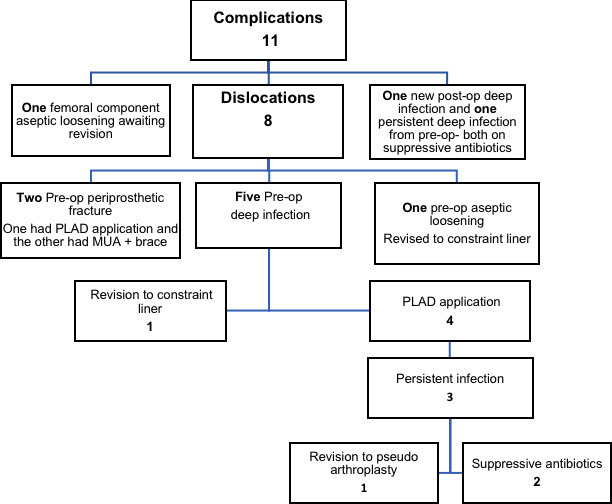
Fig. 3
Flow chart depicting complications and their management.
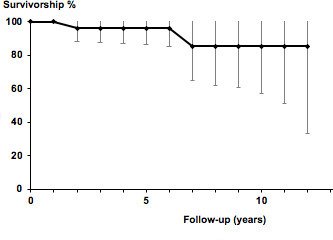
Fig. 4
Graphical representation of Kaplan-Meier curve for revision of femoral component only for any reason.
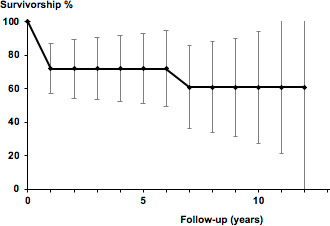
Fig. 5
Graphical representation of Kaplan-Meier curve for revision of any component for any reason.
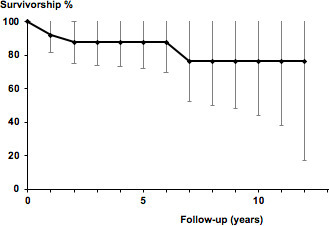
Fig. 6
Graphical representation of Kaplan-Meier curve for revision of any femoral or acetabular component for any reason, excluding application of posterior lip augmentation device.
Discussion
Management of massive bone loss in a revision hip scenario remains a challenge, which is going to be only augmented with the predicted future increase in the number of complex revision case load.1 In reality, the options for reconstruction are either to proceed with allograft-prosthesis composite or perform a PFA. PFA, with its inherent advantage of early postoperative weightbearing, lack of concerns of disease transmission and union, seems to make it the preferred mode of treatment for such complex revisions. The use of PFA in non-neoplastic conditions are rare and are mainly used to treat very complex proximal femoral fractures with bone loss. In these challenging cases, it is not uncommon to consult experienced revision arthroplasty surgeons. The modular PFA implant provides the surgeon with flexibility during the surgical procedure to reconstruct a wide range of skeletal defects. It also allows for intraoperative judgement of leg-length adjustment, trochanteric reattachment to increase the stability of the hip, and is technically less demanding in comparison to an allograft-prosthesis composite. Additionally, it negates the expense and the loss of time for manufacturing a custom-made implant. Despite all these advantages and the assuring results from previously published data,4-11,17-19 PFA still continues to be procedure with broad array of complications making it a procedure reserved as a last resort. The common complications associated with PFA are dislocation and/or infection. There is almost a 25% chance of reoperation.17
Modular PFAs when used for neoplastic indications, and have a five-year survivorship between 75% to 90%.21-23 Parvizi et al5 reported a 73% survival rate at five years in non-neoplastic indications. In our series of patients with Paprosky type 3B and four bone loss reconstructed with PFAs, the rate of survival free of femoral component revision at five years was 96%. This is dissimilar to rates reported by Grammatopoulos et al,18 who had a survivorship of endoprosthetic arthroplasty (EPR) of 87% with revision as an end point. In our series, the survival rate free of any component revision for any reason was 72%. If the patients having a PLAD was not included in the revision category, our overall survivorship at five years was 88%, similar to the rate reported by Grammatopoulos et al.18
The overall complication rate in this study was 44% (11 patients). Aseptic loosening was rare, but dislocation occurred in eight patients (32%). The overall reoperation rate at five years was 36% (nine patients), of which only two involved revision of the femoral component. Our overall complication results compare marginally higher to the recent systematic review available by Korim et al,17 which included 14 studies with a total of 356 PFAs with a mean follow-up of 3.8 years. They reported a reoperation rate of around 24% (0% to 40%) for any reason, and a dislocation rate of 15.7% (0% to 40%). Parvizi et al5 described a number of factors to improve the stability, including the use of modular components, porous coated proximal surface to aid re-attachment of soft-tissues, and constrained liners. Our dislocation rate was high at 32%. However, five out of these (63%) had pre-existing infection. Despite achieving proper implant positioning with respect to the version of the femoral component and the version and inclination of the acetabular component,these hips may still be unstable, due to the significant soft-tissue deficiency left from the previous multiple surgeries. In our series, the mean size of head was 32 mm, and a 28 mm head was used in eight cases. Gramamatopoulos et al18 reported very low dislocation in their series, which was attributed to their practice of primarily using MDM heads in cases where stability was a concern as it significantly increases the jump distance. In cases where a dual mobility was not possible, a large head of 36 mm was used. In very severe cases of instability, constrained liners can be considered, but there is always the concern of increasing shearing forces leading to weakening of the acetabular-bone interface, leading to early failure. The importance of adequate rest to the soft-tissue in the immediate postoperative period, protection to the soft-tissue in the form of bracing, and protected weightbearing could be considered to improve stability. Parvizi et al5 recommended the use of postoperative bracing to limit the risk of dislocation. Perhaps, more judicious use of dual mobility cups, along with potentially exploring modified rehabilitation protocols, could have resulted in a lower rate of dislocation in this present series. More recently, we have now changed our practice to routine use of a dual mobility cup in these cases.
The majority of the patients in this study (22 patients (88%)) could be split equally into those having either infection or a periprosthetic fracture preoperatively as an indication to have a PFA. These hips have had previous multiple operations. The eradication of infection was achieved in seven out of 11 of the patients (64%), which is comparable to the clearance rate of 56% to 92% reported in the review by Korim et al.17 A total of five patients (20%) had PJI at mean follow-up of five years, out of which four had pre-existing infection. This is similar to the rate of infection (0% to 33%) reported in the systematic review on PFA.17 Silver-coated implants (Agluna) have shown favourable results in reducing the infection rate.24,25 Only two patients had received silver-coated implants in this study. Further exploration of this new advance may help to promote the eradication rate of infection.
Where PFA was used in periprosthetic fractures (11 patients (44%)), none of them went on to have postoperative infections. Two of these 11 patients (18.2%) had postoperative dislocation and only one of them had to undergo reoperation for application of PLAD (reoperation rate of 9.2%). Mclean et al26 in their homogeneous study group of 20 PFAs in periprosthetic fractures had a 15% dislocation and a 10% infection rate. Our results compare similar to theirs with regards tothe dislocation rates. Klein et al10 reported a 30% reoperation rate in a similar group of patients. In this present series, there was no infection in this cohort of patients, and lower reoperation rates therefore compared better than the available literature.
Consequently, there is no one single answer for limiting complication, but a multidisciplinary team approach within a specialist unit and surgery performed by experienced surgeons would be ideal. We also would recommend these complex PFA cases be recorded as a separate subset on hip revision proforma towards the National Joint Registry (NJR) data capture. This can then be audited by the 'Getting It Right First Time' (GIRFT), which will help identify changes that will help improve care and patient outcome.
This study has its own limitations. First, it is a retrospective study accompanied with all its related shortcomings. Second, our sample size was only 25 hips due to the infrequent nature of these procedures and its heterogenous indication for the procedure. Additionally, the mean follow-up was only 5.9 years, making it a short-term follow-up study. Lastly, no functional scores were used to quantify the functional outcome after the procedure.
In conclusion, our study supports the fact that PFA is still a viable option for complex revisions with significant bone loss even with pre-existing infection or failed osteosynthesis. Dislocation and infection remain the major cause for failure particularly in patients with PJI. Surgery performed by experienced revision hip surgeons familiar with the use of dual mobility cups, use of silver-coated implants, and less aggressive postoperative rehabilitation regimens would possibly aid in reduction of complications. PFA performed in patients with periprosthetic fracture seem to fair better. Our study supports the use of PFA with caution as a limb salvage option in non-oncological revision hip arthroplasties when other surgical options are not feasible.
References
1. Kurtz S , Ong K , Lau E , Mowat F , Halpern M . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030 . J Bone Joint Surg Am . 2007 ; 89-A ( 4 ): 780 – 785 . Crossref PubMed Google Scholar
2. Howard P , Brittain R , Lawrence S , et al. National Joint Registry 17th annual report . 2020 . https://www.njrcentre.org.uk/njrcentre/default.aspx ( date last accessed 11 February 2022 ). Google Scholar
3. Swarup I , Lee Y-Y , Chiu Y-F , Sutherland R , Shields M , Figgie MP . Implant survival and patient-reported outcomes after total hip arthroplasty in young patients . J Arthroplasty . 2018 ; 33 ( 9 ): 2893 – 2898 . Crossref PubMed Google Scholar
4. Parvizi J , Sim FH . Proximal femoral replacements with megaprostheses . Clin Orthop Relat Res . 2004 ; 420 : 169 – 175 . Crossref PubMed Google Scholar
5. Parvizi J , Tarity TD , Slenker N , et al. Proximal femoral replacement in patients with non-neoplastic conditions . J Bone Joint Surg Am . 2007 ; 89-A ( 5 ): 1036 – 1043 . Crossref PubMed Google Scholar
6. Rasouli MR , Porat MD , Hozack WJ , Parvizi J . Proximal femoral replacement and allograft prosthesis composite in the treatment of periprosthetic fractures with significant proximal bone loss . Orthop Surg . 2012 ; 4 ( 4 ): 203 – 210 . Crossref PubMed Google Scholar
7. Al-Taki MM , Masri BA , Duncan CP , Garbuz DS . Quality of life following proximal femoral replacement using a modular system in revision THA . Clin Orthop Relat Res . 2011 ; 469 ( 2 ): 470 – 475 . Crossref PubMed Google Scholar
8. Springer BD , Berry DJ , Lewallen DG . Treatment of periprosthetic femoral fractures following total hip arthroplasty with femoral component revision . J Bone Joint Surg Am . 2003 ; 85-A ( 11 ): 2156 – 2162 . Crossref PubMed Google Scholar
9. Friesecke C , Plutat J , Block A . Revision arthroplasty with use of a total femur prosthesis . J Bone Joint Surg Am . 2005 ; 87-A ( 12 ): 2693 – 2701 . Crossref PubMed Google Scholar
10. Klein GR , Parvizi J , Rapuri V , et al. Proximal femoral replacement for the treatment of periprosthetic fractures . J Bone Joint Surg Am . 2005 ; 87-A ( 8 ): 1777 – 1781 . Crossref PubMed Google Scholar
11. Gebert C , Wessling M , Götze C , Gosheger G , Hardes J . The modular universal tumour and revision system (MUTARS®) in endoprosthetic revision surgery . Int Orthop . 2010 ; 34 ( 8 ): 1261 – 1265 . Crossref PubMed Google Scholar
12. Thompson RC , Pickvance EA , Garry D . Fractures in large-segment allografts . J Bone Joint Surg Am . 1993 ; 75 ( 11 ): 1663 – 1673 . Crossref PubMed Google Scholar
13. Zehr RJ , Enneking WF , Scarborough MT . Allograft_Prosthesis_Composite_Versus.26.pdf . Clin Orthop Relat Res . 1996 ; 322 : 207 – 223 . Crossref Google Scholar
14. Haddad FS , Masri BA , Garbuz DS , Duncan CP . Femoral bone loss in total hip arthroplasty: classification and preoperative planning . Instr Course Lect . 2000 ; 49 : 83 – 96 . https://pubmed.ncbi.nlm.nih.gov/10829164/ ( date last accessed 11 February 2022 ). PubMed Google Scholar
15. Dobbs HS , Scales JT , Wilson JN , Kemp HB , Burrows HJ , Sneath RS . Endoprosthetic replacement of the proximal femur and acetabulum. A survival analysis . J Bone Joint Surg Br . 1981 ; 63-B ( 2 ): 219 – 224 . Crossref PubMed Google Scholar
16. Horowitz SM , Glasser DB , Lane JM , Healey JH . Prosthetic and extremity survivorship after limb salvage for sarcoma how long do the reconstructions last? Clin Orthop Relat Res . 1993 ; NA ( 293 ): 280 . Crossref PubMed Google Scholar
17. Korim MT , Esler CNA , Ashford RU . Systematic review of proximal femoral arthroplasty for non-neoplastic conditions . J Arthroplasty . 2014 ; 29 ( 11 ): 2117 – 2121 . Crossref PubMed Google Scholar
18. Grammatopoulos G , Alvand A , Martin H , Whitwell D , Taylor A , Gibbons CLMH . Five-year outcome of proximal femoral endoprosthetic arthroplasty for non-tumour indications . Bone Joint J . 2016 ; 98-B ( 11 ): 1463 – 1470 . Crossref PubMed Google Scholar
19. Viste A , Perry KI , Taunton MJ , Hanssen AD , Abdel MP . Proximal femoral replacement in contemporary revision total hip arthroplasty for severe femoral bone loss: a review of outcomes . Bone Joint J . 2017 ; 99-B ( 3 ): 325 – 329 . Crossref PubMed Google Scholar
20. Della Valle CJ , Paprosky WG . Classification and an algorithmic approach to the reconstruction of femoral deficiency in revision total hip arthroplasty . J Bone Joint Surg Am . 2003 ; 85-A : 1 – 6 . Crossref PubMed Google Scholar
21. Chandrasekar CR , Grimer RJ , Carter SR , Tillman RM , Abudu A , Buckley L . Modular endoprosthetic replacement for tumours of the proximal femur . J Bone Joint Surg Br . 2009 ; 91-B ( 1 ): 108 – 112 . Crossref PubMed Google Scholar
22. Gosheger G , Gebert C , Ahrens H , Streitbuerger A , Winkelmann W , Hardes J . Endoprosthetic reconstruction in 250 patients with sarcoma . Clin Orthop Relat Res . 2006 ; 450 ( 450 ): 164 – 171 . Crossref PubMed Google Scholar
23. Menendez LR , Ahlmann ER , Kermani C , Gotha H . Endoprosthetic reconstruction for neoplasms of the proximal femur . Clin Orthop Relat Res . 2006 ; 450 : 46 – 51 . Crossref PubMed Google Scholar
24. Wafa H , Grimer RJ , Reddy K , et al. Retrospective evaluation of the incidence of early periprosthetic infection with silver-treated endoprostheses in high-risk patients: case-control study . Bone Joint J . 2015 ; 97-B ( 2 ): 252 – 257 . Crossref PubMed Google Scholar
25. Hardes J , von Eiff C , Streitbuerger A , et al. Reduction of periprosthetic infection with silver-coated megaprostheses in patients with bone sarcoma . J Surg Oncol . 2010 ; 101 ( 5 ): 389 – 395 . Crossref PubMed Google Scholar
26. McLean AL , Patton JT , Moran M . Femoral replacement for salvage of periprosthetic fracture around a total hip replacement . Injury . 2012 ; 43 ( 7 ): 1166 – 1169 . Crossref PubMed Google Scholar
Author contributions
K. Syam: Formal analysis, Resources, Visualization, Writing - original draft.
P. N. Unnikrishnan: Supervision, Validation, Writing - review and editing.
L. Naveen: Data curation, Resources, Visualization.
W. Wilson-Theaker: Data curation, Methodology.
A. Gambhir: Methodology, Supervision, Writing - review and editing.
N. Shah: Conceptualization, Supervision, Validation, Writing - review and editing.
M. Porter: Conceptualization, Supervision, Writing - review and editing.
Funding statement
The author(s) received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
The authors confirm that they have no disclosures to declare.
Acknowledgements
We thank A. Saraogi (former International Training Fellow at Wrightington Hospital, Wigan, UK) for his help in the visualization of the study.
Open access funding
The authors report that they received open access funding for this manuscript from Wrightington Hospital, Wigan, UK (order no. 10000360751).
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









