Abstract
Aims
The Oswestry-Bristol Classification (OBC) was recently described as an MRI-based classification tool for the femoral trochlear. The authors demonstrated better inter- and intraobserver agreement compared to the Dejour classification. As the OBC could potentially provide a very useful MRI-based grading system for trochlear dysplasia, it was the aim to determine the inter- and intraobserver reliability of the classification system from the perspective of the non-founder.
Methods
Two orthopaedic surgeons independently assessed 50 MRI scans for trochlear dysplasia and classified each according to the OBC. Both observers repeated the assessments after six weeks. The inter- and intraobserver agreement was determined using Cohen’s kappa statistic and S-statistic nominal and linear weights.
Results
The OBC with grading into four different trochlear forms showed excellent inter- and intraobserver agreement with a mean kappa of 0.78.
Conclusion
The OBC is a simple MRI-based classification system with high inter- and intraobserver reliability. It could present a useful tool for grading the severity of trochlear dysplasia in daily practice.
Cite this article: Bone Joint Open 2020;1-7:355–358.
Take home message
The Oswestry-Bristol Classification (OBC) is an easy to use grading system for trochlear dysplasia with excellent inter- and intraobserver reliability.
Introduction
In patients with patellofemoral instability, dysplasia of the femoral trochlea is common, as trochlear dysplasia is the most important risk factor for recurrent patella dislocation.1-4 Therefore, besides analyzing all other passive and active stabilizers of the patellofemoral joint, it is important to assess the form of the femoral trochlea during the individual workup of the pathomorphological causes of patella instability.
For grading of trochlear dysplasia, Dejour et al5 introduced a three-grade classification system in 1990. It was subsequently modified in 1998 to four grades in order to improve the inter- and intraobserver agreement.6,7 Still, the Dejour classification system, which was based on radiographs and CT, demonstrated an inconsistent inter- and intraobserver agreement throughout the literature over the years, especially when MRI was used.8-13
In 2020, Sharma et al14 published a new classification system for trochlear dysplasia: the Oswestry-Bristol Classification (OBC). This MRI-based, four-grade system is depicted in figure 1.
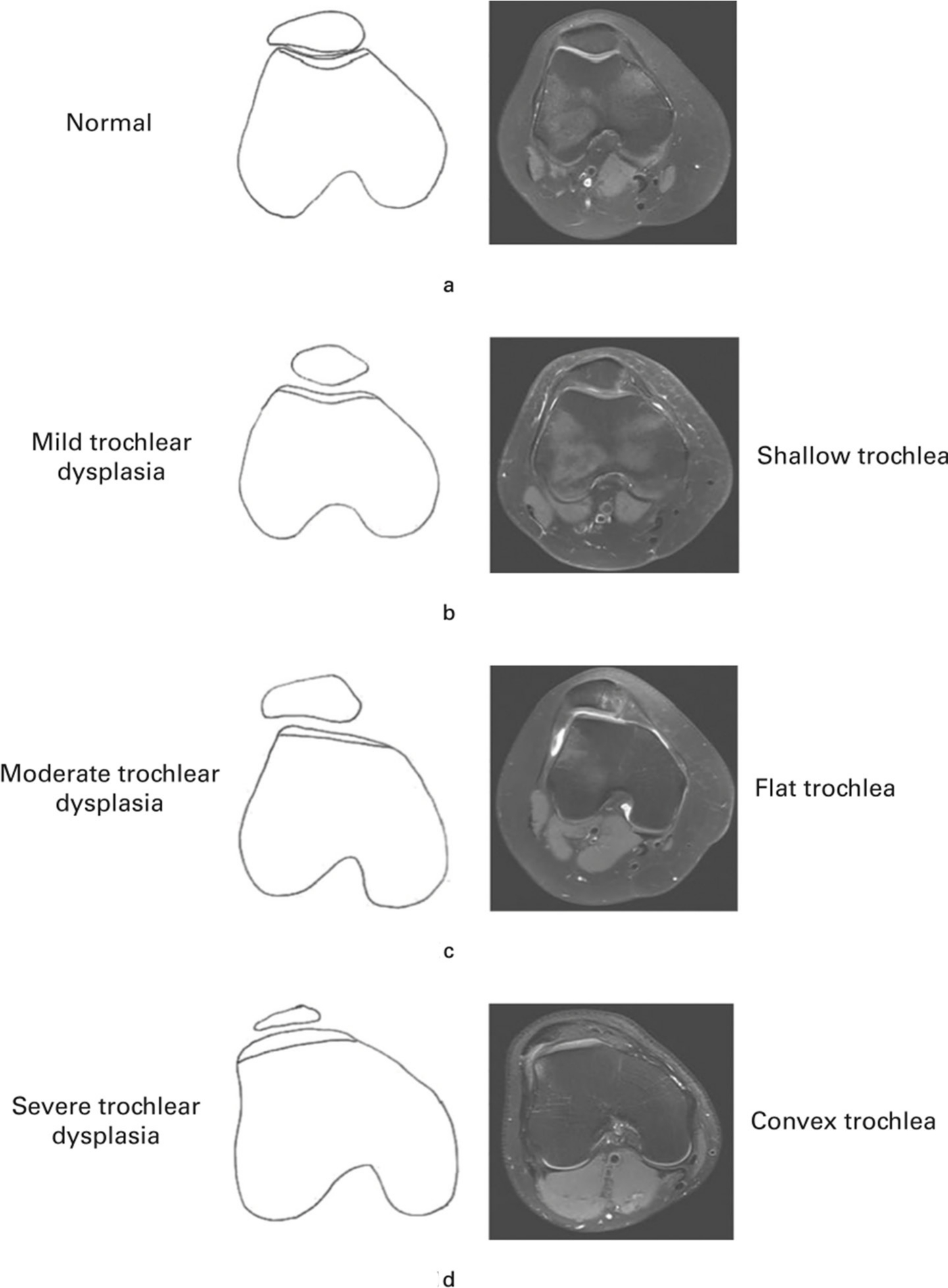
Fig. 1
The Oswestry-Bristol Classification (OBC). Drawings and MRI (reprinted14).
The OBC could potentially provide a very useful grading system for trochlear dysplasia. It was the purpose of this study to firstly validate the inter- and intraobserver agreement of the classification system by non-founding authors.
Methods
From our database, we retrospectively identified 50 knee MRI scans, which were performed in different patients who presented due to patellofemoral symptoms of pain or instability. These patients did not have any history of knee surgery altering the form of the femoral trochlea prior to MRI.
Two orthopaedic surgeons (Orthopaedic Sports Medicine Fellow (SSA)/Fellowship-trained Senior Consultant (CK)) independently graded the axial T2-weighted MRI slices according to OBC, in normal trochlea, mild trochlear dysplasia (shallow trochlea), moderate (flat trochlea), or severe (convex trochlea) trochlear dysplasia. Both observers repeated the assessments after six weeks. For the second phase, the order of MRI scans was randomized to eliminate any bias from the first reading.
We determined the interobserver agreement using Cohen’s kappa statistic.15 A kappa value greater than 0.75 represents excellent agreement beyond chance, whereas values below 0.40 represent poor agreement.16 We also determined the S-statistic to verify the kappa value.17
For determining the intraobserver agreement, we calculated the mean kappa of both observers.18 All statistical analyses were performed using the software R, Vienna, Austria.
Results
According to the ratings of both orthopaedic surgeons using the OBC, 6% (n = 3) of all trochleae were classified as normal, 56% (n = 28) as mild dysplastic, 22% (n = 11) as moderate dysplastic, and 16% (n = 8) as severe dysplastic.
We determined the interobserver agreement, kappa-statistic and S-statistic values separately for each set of observations (Table I). In the first round of observations, the agreement was 90% and in the second round it was 96%. Also, the intraobserver agreement was excellent with a kappa-value of 77% for the first observer and a kappa-value of 79% for the second observer.
Table I.
Interobserver agreement, kappa-statistic, and S-statistic values for the first and second round of observations.
| Round of assessment | Observed agreement | Expected agreement | Kappa (95% CI) | S-statistic (nominal) (95% CI) | S-statistic (linear weights) (95% CI) |
|---|---|---|---|---|---|
| 1 | 90.0% | 86.96% | 0.69 | 1.480 | 1.960 |
| 2 | 96.0% | 89.04% | 0.77 | 1.645 | 1.645 |
-
CI, confidence interval.
Discussion
This study represents the first inter- and intraobserver agreement validation of the MRI based OBC for trochlear dysplasia by non-founders. We demonstrated excellent intra- and interobserver reliability of the classification tool.
In specialized orthopaedic departments, patients with patellofemoral instability symptoms present regularly. Besides history and thorough clinical evaluation, radiograph examination and MRI of the knee represent part of the standard workup.
The originally CT-based Dejour Classification for trochlear dysplasia is known to be the standard grading system for the form of the trochlear. This classification system showed inconsistent intra- and interobserver reliability in several studies, whereas the first classification of Henri Dejour, published in 1990 (three grades), demonstrated lower agreements than the second classification by David Dejour, published in 1998 (four grades).8-13 An advantage of the OBC over the Dejour classification besides its simplicity is that it can reliably be used with standard T2-weighted axial MRI slides of the knee. Furthermore, it simplifies the classification to relevant categories.
In Table II, we summarize the OBC and add aspects, which we consider as important. This overview should facilitate future usage of the classification system as much as possible.
Table II.
Expanded characteristics of the MRI-based Oswestry-Bristol Classification (OBC) for trochlear dysplasia.
| OBC Type | Form of trochlea | Severity of trochlear dysplasia | Cartilaginous sulcus angle | Lateral Trochlear Inclination (LTI) | Indication for Trochleoplasty? |
|---|---|---|---|---|---|
| 0 | Normal | No trochlear dysplasia | Normal ( < 145°) | ≥ 11° | No |
| 1 | Shallow | Mild | Elevated ( ≥ 145°) | < 11° | No |
| 2 | Flat | Moderate | 180° | 0° | Seldom needed |
| 3 | Convex | Severe | > 180° | < 0° | Consider trochleoplasty |
-
MRI, Magnetic Resonance Imaging.
We find differentiation between normal (Type 0) and shallow (Type 1) trochleae the single most difficult aspect in the application of the OBC. Potentially, the sulcus angle might be helpful to differentiate between a normal form of the trochlea and a mild trochlear dysplasia. But the normal sulcus angle differs widely in healthy knees.19 The so-called “Oblique Trochlear View (OTV)” means special and modified axial MRI slides of the knee for evaluation of the femoral trochlea. The OTV displays a more uniform sulcus angle and depth along the trochlea.20 But this requires a modified MRI or software, which is not available on regular daily basis as patients normally present with a standard MRI of their symptomatic knee. Additionally, there are gender-related differences in the sulcus angle: females have a significantly greater sulcus angle than males.21 Thus, the sulcus angle is not a perfect differentiator between a normal (Type 0) and shallow (Type 1) trochlea, although a recently published review and meta-analysis found a cartilaginous sulcus angle of at least 143° in patients with patellofemoral instability.22 Nevertheless, deciding if a certain individual trochlear form is normal (Type 0) or mildly dysplastic (Type 1) remains partially subjective. Differentiation between greater degrees of trochlea dysplasia according to the OBC seems to be more reproducible.
Carrillon et al23 described the Lateral Trochlear Inclination (LTI). This is an angle measured on axial MRI between the posterior condylar line and the lateral trochlear facet. The authors demonstrated an LTI of 11° or higher in stable patellofemoral joints and an LTI < 11° in patellofemoral instability.
As there are many aspects involved in patellofemoral instability, a treatment algorithm cannot be developed from a classification for trochlear dysplasia alone. But we like to mention that patella height correlates with trochlear dysplasia: a higher positioned patella is associated with a more dysplastic trochlea.24 We hypothesize that a severely dysplastic trochlea is responsible for a patella alta and leads to shortening of the quadriceps muscle. This is important for planning of surgical treatment, as a distalization of the tibial tuberosity alone seems to be unsuccessful in severe trochlear dysplasia with a convex trochlea form.
In conclusion, the Oswestry-Bristol Classification (OBC) as an MRI based grading system for trochlear dysplasia showed excellent intra- and interobserver agreement. Therefore and because of its simplicity in usage, the OBC seems to be a very good system for classifying trochlear dysplasia in daily practice.
References
1. Dejour H , Walch G , Nove-Josserand L , Guier C . Factors of Patellar instability: an anatomic radiographic study . Knee Surg Sports Traumatol Arthrosc . 1994 ; 2 ( 1 ): 19 – 26 . Crossref PubMed Google Scholar
2. Farahmand F , Senavongse W , Amis AA . Quantitative study of the quadriceps muscles and trochlear groove geometry related to instability of the patellofemoral joint . J Orthop Res . 1998 ; 16 ( 1 ): 136 – 143 . Crossref PubMed Google Scholar
3. Farahmand F , Tahmasbi MN , Amis AA . Lateral force-displacement behaviour of the human patella and its variation with knee flexion--a biomechanical study in vitro . J Biomech . 1998 ; 31 ( 12 ): 1147 – 1152 . Crossref PubMed Google Scholar
4. Redziniak DE , Diduch DR , Mihalko WM , et al. Patellar instability . J Bone Joint Surg Am . 2009 ; 91 ( 9 ): 2264 – 2275 . Crossref PubMed Google Scholar
5. Dejour H , Walch G , Neyret P , Adeleine P . La dysplasie de la trochlée fémorale [Dysplasia of the femoral trochlea] . Rev Chir Orthop Reparatrice Appar Mot . 1990 ; 76 ( 1 ): 45 – 54 . Google Scholar
6. Dejour D , Reynaud P , Lecoultre B . Douleurs et instabilité rotulienne, Essai de classification . Med Hyg . 11998 ; 56 ( 2217 ): 1466 – 1471 . Google Scholar
7. DeJour D , Saggin P . The sulcus deepening trochleoplasty—the Lyon’s procedure . Int Orthop . 2010 ; 34 ( 2 ): 311 – 316 . Google Scholar
8. Rémy F , Chantelot C , Fontaine C , et al. Inter- and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia . Surg Radiol Anat . 1998 ; 20 ( 4 ): 285 – 289 . Crossref PubMed Google Scholar
9. Lippacher S , Dejour D , Elsharkawi M , et al. Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images . Am J Sports Med . 2012 ; 40 ( 4 ): 837 – 843 . Crossref PubMed Google Scholar
10. Nelitz M , Lippacher S , Reichel H , Dornacher D . Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia . Knee Surg Sports Traumatol Arthrosc . 2014 ; 22 ( 1 ): 120 – 127 . Crossref PubMed Google Scholar
11. Nelitz M , Lippacher S . Arthroscopic evaluation of trochlear dysplasia as an aid in decision making for the treatment of patellofemoral instability . Knee Surg Sports Traumatol Arthrosc . 2014 ; 22 ( 11 ): 2788 – 2794 . Crossref PubMed Google Scholar
12. Stepanovich M , Bomar JD , Pennock AT . Are the current classifications and radiographic measurements for trochlear dysplasia appropriate in the skeletally immature patient? Orthop J Sports Med . 2016 ; 4 ( 10 ): 232596711666949 . Crossref PubMed Google Scholar
13. Mousinho RSMS , Ribeiro JNA , Pedrosa FKS , et al. Evaluation of the reproducibility of the Dejour classification for femoropatellar instability . Rev Bras Ortop . 2019 ; 54 ( 2 ): 171 – 177 . Crossref PubMed Google Scholar
14. Sharma N , Brown A , Bouras T , et al. The Oswestry-Bristol classification: a new classification system for trochlear dysplasia . Bone Joint J . 2020 ; 102-B ( 1 ): 102 – 107 . Google Scholar
15. Shoukri MM . Measures of interobserver agreement and reliability . Boca Raton, Florida, USA : CRC Press , 2004 . Google Scholar
16. Fleiss JL , Levin B , Paik MC . Statistical methods for rates and proportions. Hoboken , ed . Third . New Jersey : John Wiley & Sons , 2003 . Google Scholar
17. Marasini D , Quatto P , Ripamonti E . Assessing the inter-rater agreement for ordinal data through weighted indexes . Stat Methods Med Res . 2016 ; 25 ( 6 ): 2611 – 2633 . Crossref PubMed Google Scholar
18. Light RJ . Measures of response agreement for qualitative data: some generalizations and alternatives . Psychol Bull . 1971 ; 76 ( 5 ): 365 – 377 . Google Scholar
19. Hochreiter B , Hess S , Moser L , et al. Healthy knees have a highly variable patellofemoral alignment: a systematic review . Knee Surg Sports Traumatol Arthrosc . 2020 ; 28 ( 2 ): 398 – 406 . Crossref PubMed Google Scholar
20. Ambra LF , Galvão PHSAF , Mameri ES , Farr J , Gomoll AH . Femoral trochlear geometry in patients with trochlear dysplasia using MRI oblique trochlear view . J Knee Surg . 2019 . Epub ahead of print . Crossref PubMed Google Scholar
21. Koh Y-G , Nam J-H , Chung H-S , et al. Gender-Related morphological differences in sulcus angle and condylar height for the femoral trochlea using magnetic resonance imaging . Knee Surg Sports Traumatol Arthrosc . 2019 ; 27 ( 11 ): 3560 – 3566 . Crossref PubMed Google Scholar
22. SHS T , Chng KSJ , Lim BY , et al. The difference between cartilaginous and bony sulcus angles for patients with or without patellofemoral instability: a systematic review and meta-analysis . J Knee Surg . 2020 . Epub ahead of print . Crossref PubMed Google Scholar
23. Carrillon Y , Abidi H , Dejour D , et al. Patellar instability: assessment on Mr images by measuring the lateral trochlear Inclination—Initial experience . Radiology . 2000 ; 216 ( 2 ): 582 – 585 . Google Scholar
24. Ferlic PW , Runer A , Dammerer D , et al. Patella Height Correlates With Trochlear Dysplasia: A Computed Tomography Image Analysis . Arthroscopy . 2018 ; 34 ( 6 ): 1921 – 1928 . Google Scholar
Author contributions
C. Konrads: Planned the study, Collected and analyzed the data, Wrote the manuscript.
C. Gonser: Carried out the statistic work-up, Revised and approved the manuscript.
S. S. Ahmad: Collected the data, Revised and approved the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
This publication was supported by the German Research Foundation (DFG) and the University of Tübingen in the funding programme Open Access Publishing.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









