Abstract
The COVID-19 virus is a tremendous burden for the Italian health system. The regionally-based Italian National Health System has been reorganized. Hospitals' biggest challenge was to create new intensive care unit (ICU) beds, as the existing system was insufficient to meet new demand, especially in the most affected areas. Our institution in the Milan metropolitan area of Lombardy, the epicentre of the infection, was selected as one of the three regional hub for major trauma, serving a population of more than three million people. The aims were the increase the ICU beds and the rationalization of human and structural resources available for treating COVID-19 patients. In our hub hospital, the reorganization aimed to reduce the risk of infection and to obtained resources, in terms of beds and healthcare personnel to be use in the COVID-19 emergency. Non-urgent outpatient orthopaedic activity and elective surgery was also suspended. A training programme for healthcare personnel started immediately. Orthopaedic and radiological pathways dedicated to COVID-19 patients, or with possible infection, have been established. In our orthopaedic department, we passed from 70 to 26 beds. Our goal is to treat trauma surgery's patient in the “golden 72 hours” in order to reduce the overall hospital length of stay. We applied an objective priority system to manage the flow of surgical procedures in the emergency room based on clinical outcomes and guidelines. Organizing the present to face the emergency is a challenge, but in the global plan of changes in hospital management one must also think about the near future. We reported the Milan metropolitan area orthopaedic surgery management during the COVID-19 pandemic. Our decisions are not based on scientific evidence; therefore, the decision on how reorganize hospitals will likely remain in the hands of individual countries.
Introduction
The COVID-19 virus was first identified in December 2019 in Hubei region of China,1 and it soon spread exponentially in the city of Wuhan. Within a few months, the outbreak was global, and soon becoming a pandemic.2,3 Due to the predominantly pulmonary symptoms, with a possible rapid evolution to severe acute respiratory syndrome (SARS), and therefore to the need for hospitalization in intensive care, many health systems in the world got into trouble with enormous pressure to manage patients, and are on the verge of collapse. The first cases in Italy were confirmed on 30 January 2020 by the Spallanzani Institute of Rome.4 In the last month, the Italian national health system was stressed by the outbreak of the COVID-19 pandemic. The Milan metropolitan area in Lombardy was the epicentre of the infection, with the first positive patient in the region recorded on 20 February 2020. The Italian government declared a state of emergency, and a surveillance network on the new coronavirus was activated under the coordination of the ministerial taskforce.
On 8 March 2020, the Lombardy region implemented its emergency measures for the closure of non-core or strategic production activities, and the regional health system was reorganized.5,6 On 11 March 2020, the World Health Organization (WHO) declared the ‘pandemic state’, calling on global governments to take ‘urgent and aggressive action’ to delay and mitigate the peak of infection.2 As of 7 April 2020, 135,586 total cases have been identified since the first isolated case, made up of 94,067 people testing positive for the COVID-19, 17,127 patients who died, and 24,392 patients who recovered; in all, 755,445 tests were performed. Overall, Lombardy was the region affected first and with the highest number of cases (38%). (Figure 1). Nowadays, the Italian national healthsystem, is facing the battle of a huge unbalance between the clinical needs of the population and the overall availability of resources overstretched by the demands of COVID-19 caseloads.7 Hospitals' biggest challenge was to create new intensive care unit (ICU) beds, as the existing system was insufficient to meet the new demand, especially in the most affected areas. Before the COVID-19 pandemic, ICU beds in Italy were slightly over 5,000, with Lombardy having less than 800. By April 2020, the maximum number of patients admitted to intensive care throughout Italy was 4,068, of whom 1,381 were in Lombardy. Following the sharp increase in the number of people infected requiring hospital admission and intensive care treatment, in order to contain the epidemic, on 1 April 2020 a new ministerial decree extended all measures until 13 April.
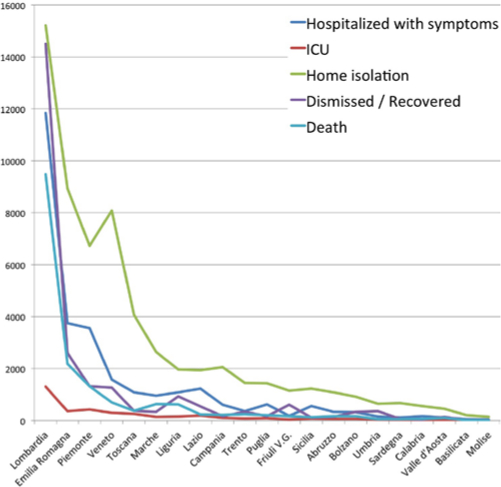
Fig. 1
Graphical Representation of the nCov-19 infection in the Italian Regions, at April the seventh 2020.
Regional health system organization
Medical practice, and in particular orthopaedic practice, were markedly affected by the reorganization of the regional health system needed to face the COVID-19 pandemic. Our regional trauma registry shows 1,800 trauma per year; this means an estimated of five major traumas per day. On the basis of those epidemiological data, three hub hospitals for major trauma were identified, for a population of around ten million. Our institution was selected as the hub for the Milan metropolitan area, thus serving a population of more than three million people.
The aims of this reorganization were to increase the ICU beds and the rationalization of human and structural resources available for treating COVID-19 patients through a redistribution between the regional hubs. Specifically, this means that every major trauma occurring in the Milan metropolitan area and managed by the territorial emergency network has to be taken to our hospital. Furthermore, hub hospitals were requested to organize separate pathways and ‘clean’ areas for non-COVID-19 patients. Forecasting a work overload for hub hospitals, the authorities identified a list of ‘Spoke’ hospitals, i.e. peripheral hospitals that refers to a specific hub, that had to make their medical personnel available for shifts in these hub hospitals. On 15 March 202o, another regional decree identified two additional hub hospitals for minor trauma with high expertise in the field. The aim was to unload the major trauma referring hub from patients that might require ICU or prolonged hospital stay. This new management ensure the treatment of trauma patients fast and with minimal risk of in-hospital contagion.
The healthcare reorganization also interested residents currently enrolled in the orthopedics training programme of the University of Milan, which is the biggest in the country with more than 100 medical doctors assigned. In an attempt to find a balance between resident safety and need for assistance, the activity was reorganized giving each resident either the possibility to stay at home, continue the work in the assigned hospital, or taking shifts in COVID-19 wards. Regarding formal training, such as lectures and seminars, the university began an online lesson platform to reduce interpersonal contact while maintaining the existing scheduled programme.
Hospital reorganization
The principles of our hub hospital organization were to reduce the risk of infection and obtain resources in terms of beds and health personnel (doctor, nurses, etc) to be used in the COVID-19 emergency. Of course, several aspects of the hospital organization were changed. Control checkpoints have been set up at the hospital entrance where body temperature is measured, and an oral questionnaire is asked to all people entering, to find some suspected infection, or contact with COVID-19 patients. Inside the hospital, patients cannot sit next to each other in the waiting rooms and caregivers are not allowed unless strictly necessary.
Non-urgent outpatient orthopaedic activity was suspended, and patients were contacted to cancel the appointment; outpatient activity remained open only for fractures or surgeries follow-up, or orthopaedic oncology. A training programme for doctors, nurses, and healthcare personnel was started immediately with the objective to learn how to dress and undress properly with personal protective equipment (gloves, surgical face masks, goggles, face shield, and gowns, as well as items for specific procedures) and make correct use of them. Surgical procedures on COVID-19 patients or emergency surgeries in patientes without test results, full precautions are usually taken: the number of people in the OR reduced at the necessary minimum; Anesthesiologist, nurses and surgeon dressed properly with protective equipment: triple gloves, FFP2 surgical face masks and goggles or face shield. On the contrary, surgeries on known negative patients are perfromed as usual.8
Health workers who are reassigned to the COVID-19 department needed theoretical and practical training with direct support in the ward to review the medical knowledge necessary to face the new emergency. This is because after years of hyperspecialization, such as orthopaedic, some general medical notions must be resumed and on the other part some notions are characteristic of the anesthesiology specialist field.
At the beginning of each working shift, health personnel must measure body temperature and record it in appropriate forms. Whenever possible, the administrative staff started working from home with remote smart working. Orthopaedic and radiological pathways dedicated to COVID-19 patients, or with possible infection, have been established. This way, negative patients are able to undergo their clinical and therapeutic pathway without mixing with COVID-19 patients. Moreover, to avoid unnecessary contact, patients' relatives are informed about clinical situation by phone. Overall, we also assisted a general reorganization of ICU beds and wards. Currently, in our hospital there are seven ICU with 96 beds; five (76 beds) dedicated to COVID-19 patients. In our orthopaedic department we went from, 70 to 26 beds plus 2 ‘grey’ beds, intended as temporary stations for patients waiting for the test results. The remaining 40 beds are now dedicated to COVID-19 patients.
Elective surgery
Elective orthopaedic surgery has been cancelled. In our hospital, this happened gradually: from 2 March, only non-ICU candidates and patients that did not expect prolonged hospital stay were operated. From 8 March 2020, we had a suppression of all elective surgery. For the patients already hospitalized, a programme of facilitated home discharge was introduced, aiming to avoid any unnecessary days of hospital stay. This approach allowed us to free space for the emergency and to reduce potential exposure to COVID-19 among our patients. Indeed, the 30 beds usually destined for elective orthopaedic patients were reallocated to the hospitalization of COVID-19 patients. Differently, in other countries, as reported by Liang et al in Singapore, day surgical cases that required less than 23 hours of hospital stay have been allowed to continue.9 The rationale of their management was that in this elective surgery, patients can be quickly discharged after the procedure, therefore not overloading health-care resources and with a limited risk of nosocomial COVID-19 infection. Their approach was justified by the previous SARS experience in 2003, after which they developed a systematic outbreak response system and probably favoured by the peculiar geographical condition. However, it would be difficult to apply the same management in countries with larger and less trackable population.
Urgency and emergency surgery
Orthopaedic trauma surgery could not be postponed nor delayed. In addition, patients with a fracture may be at a higher risk of COVID-19 pneumonia.10 The basic principle to follow during the pandemic is to limit as much as possible the hospital stay in order to maximizing the availability of beds to treat upcoming other emergencies, while maintaining an high standard of care for the patients. In this context, the timing of treatment play a crucial role in the good management of patients especially during the current pandemic. Our goal is to treat all patient in the “golden 72 hours” in order to reduce the overall hospital length of stay.
According to our COVID-19 reorganization, two different pathways were set to separate COVID-19 negative and positive trauma patients. Overall, patients admitted to our ER because of trauma are all tested for COVID-19, unless they have a recent (< 7 days) negative test. In case of a major trauma, patients known to be COVID-19-positive, or those without recent negative test, transition in a ‘grey’ area, that comprises the shock room, a CT scan, and nuclear magnetic resonance (NMR), and finally a room with negative pressure to station the patients until the results of the test are available. Patients requiring urgent early surgery are treated as COVID-19 positive until the definitive test results are available. On the other hand, known negative patients are transitioned to the ‘clean’ pathway after completing the diagnostic workup. In case of minor trauma, known positive patients are directly admitted to dedicated trauma COVID-19 beds; known negative patients follow again the clean pathway and are admitted to regular trauma beds; finally patients who are waiting for test results station in ‘grey’ beds up until the results are available, after which the follow either the ‘clean’ or ‘dirty’ pathway (Figure 2). In cases of negative test, a test is repeated during the coures of the hospitalization if the patient develop new respiratory symptoms. Of note, we recorded few cases of in-hospital positivization of patients with previous negative test. In this situation, patients were promptly transferred to the dedicated COVID-19 beds; healthcare personell in contact with those patients was followed up clinically to monitor eventual symptoms onset.
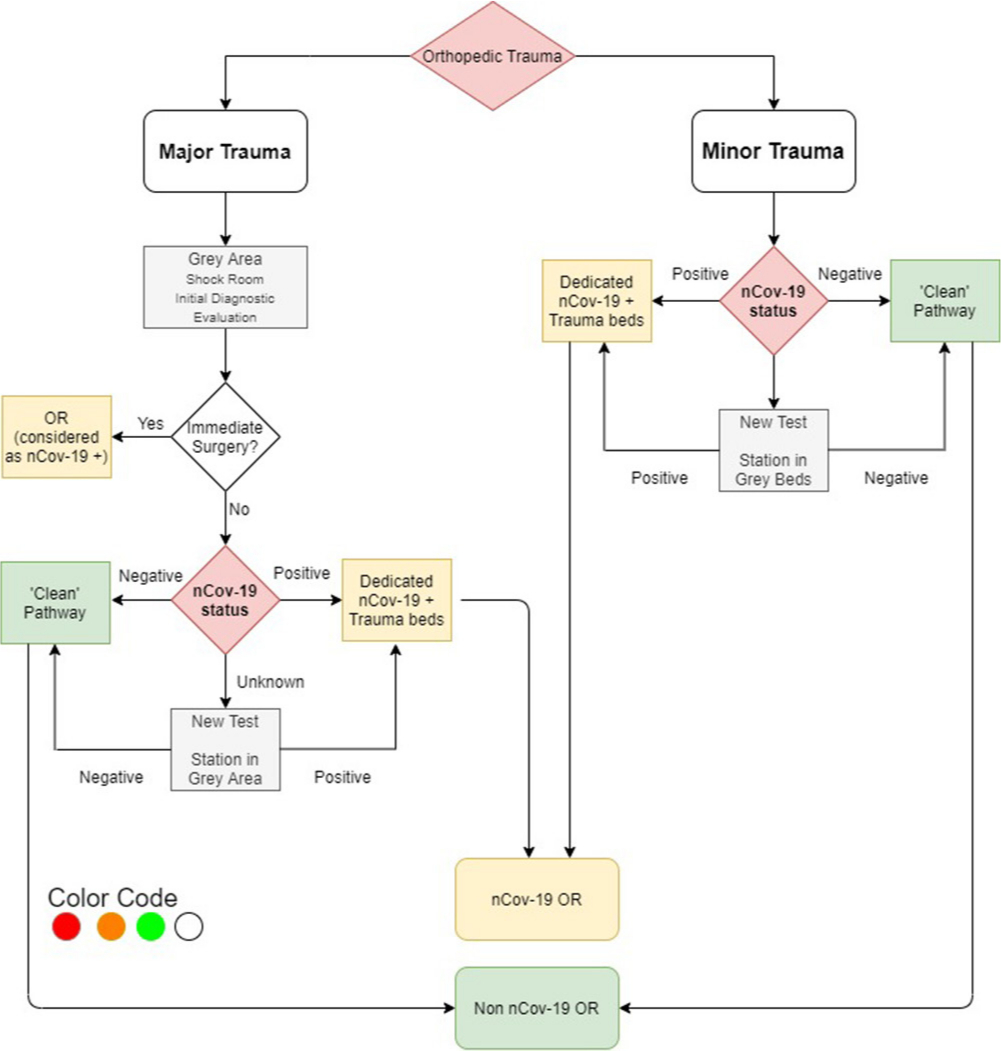
Fig. 2
The flowchart for orthopaedic trauma admission and management. OR, operating room.
Due to the unpredictability with which patients arrive in the emergency room and to the heterogeneity of the injuries presented, urgent and emergency surgery cannot be planned. The priority of the surgical procedures is a crucial point in the organization of the operating room. Moreover, due to the predicted increment in trauma admission after the centralization of the cases, a priority system that regulates the flow in the OR is mandatory. In our hospital, major trauma hub for the Milan Metropolitan area, we applied an objective priority system, based on a color code, to manage the flow of surgical procedures in the emergency room based on clinical outcomes and guidelines.11 This system was maintained and adapted since the regional health system reorganization due to the COVID-19 pandemic. As previously detailed, an orthopaedic trauma surgical team was made available for emergencies 24/7, using a dedicated OR with two nurses and an anesthesiologist. To fit the system, all orthopaedic emergencies have been classified according to the urgency of the condition and assigned to a color code (Table I). Each color is associated with a time, in hours, within which the surgery should be performed. The red color identifies emergencies that need surgery in the shortest possible time; with the orange color surgery is required in one to six hours, with the green one in six to 24 hours and with the white one within 48 hours. The ER consultant orthopaedic specialist use this system of urgencies’ stratification, filling in a form with patient’s health data and hanging it on a blackboard at the entrance to the operating rooms: surgical procedures are scheduled according to the priority given by the color code. Everyone in the operating room can see which emergencies are waiting to surgery and with what priority. It is a simple and transparent system. For all the other orthopaedic trauma not included in the colour code, a dedicated second OR is available five days a week (Monday to Friday) to reach the goal of operating all trauma in less than 72 hours.
Table I.
Orthopaedic emergency conditions defined for the colour code system.
| Diagnosis | Color | Timing |
|---|---|---|
| Hemodynamically unstable pelvic ring fractures | Red | Immediate |
| Long bones fractures with associated vascular lesions | ||
| Compartimental syndrome | ||
| Amputations/subamputaions | ||
| Exposed fractures | Orange | One to six hours |
| Hemodynamically stable, mechanically unstable pelvic ring fractures | ||
| Non-reducible dislocations | ||
| Unstable dislocations of the knee or ankle joint | ||
| Paediatric proximal humeral fractures with vascular compromise (Gartland IV) | ||
| Major trauma with long bone fractures | ||
| Femoral neck fracture in young | ||
| Paediatric proximal humeral fractures without vascular compromise (Gartland II-III) | Green | Six to 24 hours |
| Femoral or tibial dyaphiseal fractures | ||
| Distal femoral fractures | ||
| Proximal tibial fracture with soft tissue compromise | ||
| Distal tibial fracture with soft tissue compromise | ||
| Deep wound with tendineous lesions | ||
| Femoral neck fractures in elderly (> 65 year old) | White | Less than 48 hours |
| Paediatric fractures without vascular lesions |
Conclusion
Organizing in the face of the COVID-19 emergency is a challenge, but in the global plan of hospital management we must also think about the near future. When the surgical and outpatient activity resumes, part of the postponed services will have to be recovered gradually so as not to collapse the national health system with a sudden increase of requests.
We reported the Milan metropolitan area orthopaedic surgery management during the COVID-19 pandemic. Indeed, our decisions are not based on scientific evidence and expert opinions, but only on the urgent need to free beds for COVID-19 patients and to limit the in-hospital spread of the virus. Again, our experience may not be sufficient to guide policy changes in other national health systems. Therefore, the decision on how reorganize hospitals will likely remain in the hands of individual countries.
References
1. Zhu N , Zhang D , Wang W , et al. A novel coronavirus from patients with pneumonia in China, 2019 . N Engl J Med . 2020 ; 382 ( 8 ): 727 – 733 . Crossref PubMed Google Scholar
2. Coronavirus disease (COVID-19) Pandemic [Internet] . Available from: . https://www.who.int/emergencies/diseases/novel-coronavirus-2019 Google Scholar
3. Callaway E . Time to use the p-word? coronavirus enters dangerous new phase . Nature . 2020 ; 104 : 579 . Crossref PubMed Google Scholar
4. Spiteri G , Fielding J , Diercke M , et al. First cases of coronavirus disease 2019 (COVID-19) in the who European region, 24 January to 21 February 2020 . Euro Surveill . 2020 ; 25 ( 9 . Crossref PubMed Google Scholar
5. DELIBERAZIONE N° XI / 2906 - Regione Lombardia [Internet] . [cited 2020 Mar 31]. Available from: https://www.regione.lombardia.it/wps/wcm/connect/5e0deec4-caca-409c-825b-25f781d8756c/DGR+2906+8+marzo+2020.pdf?MOD=AJPERES&CACHEID=ROOTWORKSPACE-5e0deec4-caca-409c-825b-25f781d8756c-n2.vCsc Google Scholar
6. Corsini A , Bisciotti GN , Eirale C , Volpi P . Football cannot restart soon during the COVID-19 emergency! A critical perspective from the Italian experience and a call for action. British journal of sports medicine . England . 2020 . Google Scholar
7. Remuzzi A , Remuzzi G . COVID-19 and Italy: what next? Lancet . 2020 ; 395 ( 10231 ): 1225. Crossref PubMed Google Scholar
8. Rational use of personal protective equipment for coronavirus disease (NCOV-19) and considerations during severe shortages [Internet] . Available from: https://www.who.int/publications-detail/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(nCov-19)-and-considerations-during-severe-shortages Google Scholar
9. Chang Liang Z , Wang W , Murphy D , Po Hui JH . Novel Coronavirus and Orthopaedic Surgery: Early Experiences from Singapore. JBJS [Internet]. 9000;Latest Art. Available from: . https://journals.lww.com/jbjsjournal/Fulltext/latest/Novel_Coronavirus_and_Orthopaedic_Surgery__Early.99807.aspx Google Scholar
10. Mi B , Chen L , Xiong Y , et al. Characteristics and early prognosis of COVID-19 infection in fracture patients . J Bone Joint Surg Am . 2020 : 1 . Crossref PubMed Google Scholar
11. Leppäniemi A , Jousela I . A traffic-light coding system to organize emergency surgery across surgical disciplines . Br J Surg . 2014 ; 101 ( 1 ): e134 – e140 . Crossref PubMed Google Scholar
Author contributions
P. D. Giorgi: Designed the Study. Wrote the paper
E. Gallazzi: Designed the Study. Wrote the paper
P. Capitani: Wrote the paper
G. A. D’Aliberti: Edited the paper
F. Bove: Edited the paper
O. Chiara: Edited the paper
G. Peretti: Edited the paper
G. R. Schirò: Designed the Study. Wrote the paper
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors wish to thank Dario Capitani MD, Head of Orthopedics and Traumatology Unit at ASST Grande Ospedale Metropolitano Niguarda, for his effort in response co-ordination during the emergency.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited. Standard










