Abstract
This review explores recent advances in fixator design and used in contemporary orthopaedic practice including the management of bone loss, complex deformity and severe isolated limb injury.
Introduction
Externally applied methods to stabilise the injured limb have been in use since antiquity. In the modern era, advances in technique and technology have led to the development of the external fixator, with an expansion of potential applications. This review explores recent advances in fixator design and contemporary indications including management of bone loss, complex deformity, severe isolated limb injury and the polytraumatised patient.
In 1938 Hoffmann described a modular external fixator with the ability to reduce fractures and to make postoperative corrections to the alignment of fragments in three planes with the frame in situ.1 This was the prototype mono-lateral adjustable fixator and continues in widespread use in its third incarnation.
In the period following the Second World War, Ilizarov developed a fine wire circular fixator for use in the management of fractures, non-unions and deformity. This device was patented in 1952 and has developed into a highly versatile apparatus which, in common with the monolateral fixator, is widely used today.
Distraction osteogenesis
Ilizarov used the term “regenerate” to describe the bone formed in distraction osteogenesis and investigated the biological and mechanical factors that were fundamentally important for bone formation.2-4 The conclusion of these canine experiments, in association with 40 years of clinical experience, was that osteogenic activity was positively correlated with increased stability of the external fixator, with unstable constructs tending to result in pseudoarthroses. De Bastiani popularised distraction osteogenesis in Europe with the Orthofix monobody external fixator and introduced the term ‘callotasis’.5 The technique involved a tissue preserving osteotomy and after a delay, distraction at 1mm per day. When the target length was achieved, the fixator was dynamised, allowing load sharing between fixator and bone.
Monolateral fixators are stiffer than fine wire circular fixators in axial loading,6 particularly the bulky monobody designs.7 They are less resistant to torsion and bending when forces are applied outside the plane of the monolateral device.8 This produces asymmetrical (anisotropic) loading, which may be detrimental to fracture healing and osteogenesis. Increased stability can be achieved with increased diameter of fixation pin, pin placement at the periphery of each bone segment, decreasing the distance between the rods and the bone, increasing the number of connecting rods, and using multiplanar fixation.
Fine wire circular fixators in general, produce symmetrical (isotropic) loading of regenerate or fracture. They exhibit nonlinear stiffness behaviour under axial loading8,9 with low stiffness at low loads stimulating callus formation, and increased stiffness at higher loads protecting regenerate bone from excessive strain. Stability of the construct is improved by utilising the smallest diameter rings that give adequate soft tissue clearance, avoiding excessive distance between the rings and using two rings per bone segment.
An external fixator that employs elements of both monolateral and circular fixators, is termed “hybrid” .This describes a construct in which one bone segment is fixed to monolateral bars and another to a ring, or where rings are used for all segments, but with a combination of wires and half pins attaching bone to ring.
The use of half pins particularly in the tibial diaphysis, allows bone to ring fixation without transfixion across myofascial compartments. Many centres have adopted this hybrid technique, reporting improved patient tolerance, but it is uncertain whether hybrid constructs maintain the favourable biomechanical properties of the fine wire Ilizarov fixator. In vitro studies have investigated the biomechanics of hybrid fixators10-16 but the multiplicity of possible frame configurations and component variables make it difficult to compare results. Yang et al14,demonstrated that replacement of one fine wire with a 6mm half pin on each ring of a standard 4 ring / 8 wire Ilizarov construct resulted in an approximately one third increase in axial stiffness and corresponding reduction in the inter-fragmentary displacement. The authors concluded that this hybrid construct closely resembled the mechanical environment of a mono-lateral fixator. Lundy et al12,investigated the mechanical properties of four hybrid fixator configurations and demonstrated nonlinear stiffness characteristics similar to a conventional Ilizarov fixator.
Recent advances in fixator design
The Stewart-Gough hexapod fixator (described in detail elsewhere in this issue) has the potential to offer the advantages of the Ilizarov system with some key advances.
Management of residual deformity with a programmable fixator is straightforward, requiring no more than revision of a printed, computer-generated correction algorithm which is given to the patient, and can also be managed through the use of a mobile phone ‘App’.
This allows rapid modification to be undertaken during complex deformity correction. Modification of the fixator is confined to replacement of telescopic struts and can be conducted in an out patient setting by an assistant without specialist training. The major advantage is therefore the ease and rapidity of use combined with greater accuracy of correction.17
The hexapod fixator may alter the biomechanical environment at the distraction site and some surgeons have expressed concerns that this may be detrimental to osteogenesis. To date, there has not been a prospective randomised trial comparing the hexapod with the Ilizarov external fixator,(IEF) but two small comparative studies have been published. In a retrospective case-control study of paediatric limb lengthening, Iobst18demonstrated significantly longer lengthening index using the Taylor Spatial Frame (TSF) compared with IEF (1.8 vs 1.3 months/cm, p = 0.01), concluding that the TSF was excellent for complex deformity correction but the IEF was superior for simple paediatric lengthening. Conversely, Kristiansen19 did not demonstrate a significant difference in lengthening index after case selection for comparable lengthening distances, between 9 cases performed with TSF and 23 performed with IEF (2.4 vs 1.8 months/cm respectively, p = 0.17).
Case series describing distraction osteogenesis using TSF alone20-24report lengthening indices between 1.3 and 2.5 months/cm. Direct comparison between TSF and lengthening indices reported in the multiple published series utilising the IEF is impractical due to multiple variables including anatomy of limb segment, patient age, indication for surgery and use of pure or hybrid IEF configuration.
Despite the biomechanical differences, good clinical results continue to be reported for distraction osteogenesis using pure Ilizarov, hybrid25,26and simple monolateral27,28 external fixators.
McFadyen et al29 reported results of the first 100 consecutive cases treated with the TSF system since its introduction into our unit in 1999. The majority were applied to correct non-union and malunion (60) and the tibia was most commonly involved. Union was achieved in 99 cases and complete correction of deformity in all but seven.
Advances in mono-lateral fixator design have led to the introduction of devices which allow correction of complex multi-planar deformities. The original Orthofix monobody external fixator has been refined, with the introduction of swivelling and multiplanar clamps and angulation and rotation templates to facilitate complex deformity correction.
The Multiaixal Correction System (Biomet) is a hybrid monobody fixator which utilises a central component consisting of two perpendicular hinges. In common with the IEF, placement of the hinge directly over the axis of the deformity will result in a pure angular correction, and alternative hinge placement can be used to produce deliberate translational correction or shortening / lengthening. Unintended deformity resulting from incorrect placement of the hinge can be corrected with angulation and translation and the system can be used with rotating rings to correct a rotational deformity. Clarke30 utilised this fixator to correct 58 cases of tibia vara secondary to Blount’s disease and found no significant difference in complication rates compared to the devices previously used in that centre for deformity correction.
Irrespective of the design of the fixator, loosening and infection of the components used to connect the fixator to bone is a major source of morbidity. The introduction of hydroxyapatite- (HA-) coated half pins has improved the characteristics of the bone fixator interface and by bonding to bone have increased extraction torque.31 Prospective randomised trials have shown significantly increased extraction torques and decreased rates of loosening compared to uncoated steel or titanium pins.32-35 One prospective randomised human trial36 reported a 50% reduction in the rate of pin site infection with HA-coated pins (p = 0.009).
Staged management of high energy and multiple injuries
The role of the external fixator in the initial management of isolated high energy limb injury has become firmly established over the past two decades.
Conventional wisdom in the 1950s dictated that operative fixation of severe fractures of the tibial plafond was impossible.37 Subsequently, development of the principles of surgical management of intra-articular fractures by the AO group led to promising results in lower energy injuries.38,39 It became clear that early open reduction and internal fixation (ORIF) of the higher energy fracture patterns through traumatised soft tissues resulted in poor outcomes40-42with deep infection rates as high 30-50%.43,44 This led has led to the acceptance of staged management of these injuries, with initial application of an ankle-spanning external fixator and surgical stabilisation delayed up to three weeks until recovery and an improvement in outcome45-47 and the management of other high energy periarticular fractures has evolved in a similar way.
Advances in understanding the mechanism of systemic inflammatory response in the multiply injured patient48 resulted in the introduction of Damage Control Orthopaedics (DCO) and these polytraumatised patients are now routinely managed with simple mono-lateral external fixators providing rapid, minimally invasive temporary fracture stabilisation and avoiding the “second hit” of more invasive surgery associated with the development of adult respiratory distress syndrome and multi-organ dysfunction in susceptible patients.49
Acute fracture management
In AO/OTA Type C periarticular fractures of the tibial plateau and plafond, modern adjustable external fixators can provide immediate, minimally-invasive and stable fixation of the reconstructed articular block to the diaphyseal segment. It is also possible to carry out adjustments in the post operative period facilitating anatomical restoration of articular angles and prevention of mechanical axis deviation. In a series of 44 AO/OTA Type C fractures (30 of which were C3 fractures, 27 of those highly comminuted), union was achieved in all cases with normal coronal plane alignment in 52% and no cases of condylar angulation greater than 10 degrees.50
In our experience, the hexapod circular fixator is effective in the management of long bone diaphyseal fractures, particularly those of the tibia, which are irreducible closed and where the soft tissues will not permit open reduction. Stable fixation can be achieved with the fracture shortened and translated, reducing the tension in the soft tissues, with gradual fracture reduction in the postoperative period and definitive fixation until union without the need for further surgical intervention. Joint mobilisation can begin immediately, but weightbearing may be difficult until satisfactory alignment of the limb is restored.
Paediatric and adolescent tibial diaphyseal fractures that are associated with a significant soft tissue injury are frequently not appropriate for open reduction and plate fixation, and the presence of open physes precludes the use of an intramedullary device. Monolateral or Conventional circular external are an accepted treatment but fixator adjustment in the postoperative period may be difficult. Al-Sayyad51 reported the use of the TSF in 10 unstable adolescent tibial fractures, 5 of which were open. All fractures united at a mean time of 18 weeks, with no significant rotational, angular or axial deformity. Eidelman52 reported similarly excellent results using the TSF and we reported the results of 10 consecutive high-energy open diaphyseal tibial fractures in children of mean age 11 (range 5-15) managed with the TSF.53 There were no cases of delayed or nonunion, with a mean time to union and frame removal of 16 weeks with minimal residual deformity.
Combining techniques – external fixators with plates and nails
The management of patients with multi-apical deformity is complicated, especially in association with limb-length discrepancy. Patients typically require a protracted period of fixator use following lengthening to allow maturation of regenerate prior to frame removal.
Lengthening in isolation54 and in the presence of deformity55,56 has been managed with a combined approach using circular or mono-lateral external fixators with intra-medullary nails. In a matched-case comparison, femoral lengthening over an intra-medullary nail reduced the external fixator time by almost one half (p< 0.001) and more than doubled the rate of recovery of knee motion, compared to lengthening with the fixator alone.55 Kocaoglu57 reported the results of femoral deformity correction and lengthening over an intra-medullary nail using a mono-lateral external fixator in 28 cases, with a mean length gain of 6 cm and an external fixation index of just 0.5 months/cm.
Although a small early series using this technique in the tibia was associated with a high rate of significant complications,58 more recently published large series support its use59-63 and Guo64 reported the results of a retrospective study of tibial lengthenings using Ilizarov external fixation over a nail (51 cases) compared to Ilizarov external fixation alone (23 cases). The mean lengthening was 7.4cm with no difference in the lengthening or consolidation index. The complication rate in the fixator over nail group was less than half of that observed with fixator alone.
Computer hexapod assisted orthopaedic surgery (CHAOS)
A technique of distal femoral deformity correction using fixator-assisted nailing has been described by Gugenheim.66 A Hex-Fix mono-lateral fixator was used in 12 cases and the IEF in the remaining 2 cases to acutely restore normal distal femoral anatomy, prior to retrograde intra-medullary nailing, with healing of the osteotomy at a mean time of 13 weeks. This technique has also been described for the management of distal femoral peri-prosthetic fractures64 and windswept deformity of the knees.65
Whilst these papers describe an elegant solution for these difficult cases, we have struggled to obtain sufficient stability of the distal fragment, and accuracy of reduction of complex multi-planar deformities with mono-lateral devices and the IEF. This has led to the development of a technique that uses the stability of a ring fixator, and accuracy of reduction provided by the TSF and has provided a straightforward solution for complex deformity.
The pin placement involves antero-medial and antero-lateral half pins in a convergent configuration. This allows passage of a retrograde intra-medullary nail without alteration of the fixator. The proximal ring is secured with 2 half pins inserted proximal to the tip of the nail. This technique is easily modified by rotating the distal ring to allow insertion of a lateral locking plate.
The accuracy of the TSF program allows precise reorientation of the distal fragment allowing anatomical reconstruction. Our initial experience involved eight femoral deformity corrections in 7 patients.66 All deformities were complex oblique plane deformities, often with a rotational component, and ranged from 10 degrees valgus to 35 degrees varus; up to 45 degrees of external rotation; 10 mm of translation and in 1 case, 100 mm of shortening. All patients underwent acute intra-operative deformity correction67 mediated by the TSF prior to definitive internal fixation using either a percutaneous locking plate or locked intra-medullary nail. Deformity correction and restoration of the mechanical axis were achieved in all cases. We have subsequently expanded the use of this technique to allow multilevel femoral osteotomy correction of multiapical deformity(Fig. 1).

Fig. 1
Computerised hexapod Assisted Orthopaedic Surgery (CHAOS) for femoral deformity correction.
Bone transport
Bone transport is a technique in which a segment of bone is gradually moved from the site of an osteotomy to the end of a segmental defect, usually under the control of an external fixator. Bone forms in the gap by distraction osteogenesis and the technique can predictably bridge skeletal defects between 5 and 10 cm.
The technique has been described for the management of acute high energy open fractures with bone loss,68 chronic post traumatic intercalary defects,69,70 atrophic and infected non-unions,71-73 and for reconstruction after excision of benign and malignant bone tumours.73,74 The technique can be performed using a mono-lateral or circular fixator and relies on stable fixation and precise alignment of the donor and recipient bone segments. This may present major technical difficulties in long segmental transport, where, by definition, the segment will transport in a straight line, but due to the natural bowing of the femur and, to a lesser extent, the tibia, the transporting segment fails to dock. Repeated reorientation of the fixator, and occasionally an open procedure to realign the segments, may be necessary. This can be avoided if very accurate application of the initial IEF can be achieved, but the use of a hexapod circular fixator facilitates ongoing correction of alignment during the transport without fixator reconfiguration. The fixator is constructed using a three ring system, one pair lengthening, and the second shortening to allow gradual displacement of the transporting segment. Fixation of this segment with half pins provides stability and prevents “yawing” that is associated with a fine wire construct which can results in shearing of the regenerate, delayed bone formation and an extended treatment time. Residual programming permits very accurate apposition of the bone segments and obiviates the need for an open docking procedure in the majority of cases(Fig. 2).
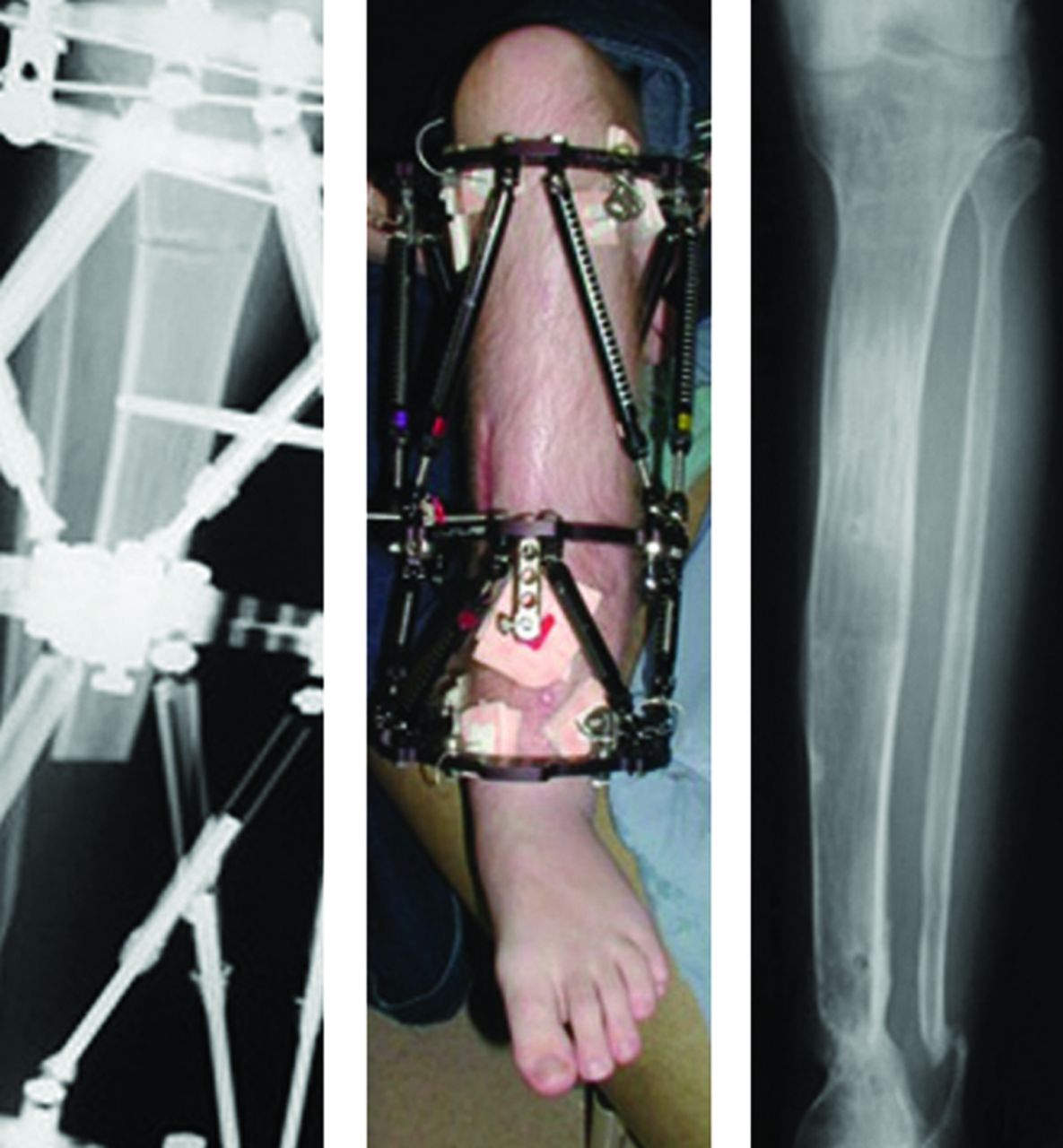
Fig. 2
Bone transport following infection.
Conclusion
External fixation devices have been in use for over 2000 years, but in their modern incarnation have become extremely versatile. Traditionally regarded as devices for the temporary stabilisation of fractures prior to definitive fixation, the experimental and clinical work of Ilizarov and his successors has resulted in a significant expansion of the indications. External fixators are employed in contemporary practice in definitive management of complex trauma, correction of complex deformity and limb salvage by bone transport. The hexapod ring fixator has built upon the strengths of the original IEF, increasing its versatility and ease of use in these complex cases.
1 Hoffmann R . “Rotules à os” pour la “réduction dirigée”, non sanglante, des fractures (“ostéotaxis”). Helv Med Acta1938;5:844–850. Google Scholar
2 Ilizarov GA . The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res1989;238:249–281.PubMed Google Scholar
3 Ilizarov GA . The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res1989;239:263–285.PubMed Google Scholar
4 Ilizarov GA . Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res1990;250:8–26.PubMed Google Scholar
5 De Bastiani G , AldegheriR, Renzi-BrivioL, TrivellaG. Limb lengthening by callus distraction (callotasis). J Pediatr Orthop1987;7:129–134.CrossrefPubMed Google Scholar
6 Fleming B , PaleyD, KristiansenT, PopeM. A biomechanical analysis of the Ilizarov external fixator. Clin Orthop Relat Res1989;241:95–105.PubMed Google Scholar
7 Paley D , FlemingB, CatagniM, KristiansenT, PopeM. Mechanical evaluation of external fixators used in limb lengthening. Clin Orthop Relat Res1990;250:50–57.PubMed Google Scholar
8 Gasser B , BomanB, WyderD, SchneiderE. Stiffness characteristics of the circular Ilizarov device as opposed to conventional external fixators. J Biomech Eng1990;112:15–21.CrossrefPubMed Google Scholar
9 Podolsky A , ChaoEY. Mechanical performance of Ilizarov circular external fixators in comparison with other external fixators. Clin Orthop Relat Res1993;293:61–70.PubMed Google Scholar
10 Calhoun JH , LiF, LedbetterBR, GillCA. Biomechanics of the Ilizarov fixator for fracture fixation. Clin Orthop Relat Res1992;280:15–22.PubMed Google Scholar
11 Calhoun JH , LiF, BaufordWL, et al.Rigidity of half-pins for the Ilizarov external fixator. Bull Hosp Jt Dis1992;52:21–26.PubMed Google Scholar
12 Lundy DW , AlbertMJ, HuttonWC. Biomechanical comparison of hybrid external fixators. J Orthop Trauma1998;12:496–503.CrossrefPubMed Google Scholar
13 Pugh KJ , WolinskyPR, DawsonJM, StahlmanGC. The biomechanics of hybrid external fixation. J Orthop Trauma1999;13:20–26.CrossrefPubMed Google Scholar
14 Yang L , NayagamS, SalehM. Stiffness characteristics and inter-fragmentary displacements with different hybrid external fixators. Clin Biomech (Bristol, Avon)2003;18:166–172.CrossrefPubMed Google Scholar
15 Yilmaz E , BelhanO, KarakurtL, ArslanN, SerinE. Mechanical performance of hybrid Ilizarov external fixator in comparison with Ilizarov circular external fixator. Clin Biomech (Bristol, Avon)2003;18:518–522.CrossrefPubMed Google Scholar
16 Voor M , AntociV, KamB, RobertsC. Hybrid external fixation of proximal tibia fractures: biomechanical analysis of four commercial systems. Orthopedics2007;30:1033–1038.CrossrefPubMed Google Scholar
17 Manner HM , HueblM, RadlerC, et al.Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop2007;1:55–61.CrossrefPubMed Google Scholar
18 Iobst C . Limb lengthening combined with deformity correction in children with the Taylor Spatial Frame. J Pediatr Orthop B2010;19:529–534.CrossrefPubMed Google Scholar
19 Kristiansen LP , SteenH, ReikeråsO. No difference in tibial lengthening index by use of Taylor spatial frame or Ilizarov external fixator. Acta Orthop2006;77:772–777. Google Scholar
20 Sala F , ThabetAM, CastelliF, et al.Bone transport for postinfectious segmental tibial bone defects with a combined ilizarov/taylor spatial frame technique. J Orthop Trauma2011;25:162–168.CrossrefPubMed Google Scholar
21 Blondel B , LaunayF, GlardY, et al.Limb lengthening and deformity correction in children using hexapodal external fixation: preliminary results for 36 cases. Orthop Traumatol Surg Res2009;95:425–430.CrossrefPubMed Google Scholar
22 Gessmann J, Seybold D, Baecker H, Muhr G, Graf M. [Correction of supramalleolar deformities with the Taylor spatial frame]. Z Orthop Unfall 2009;147:314-320. Google Scholar
23 Marangoz S , FeldmanDS, SalaDA, HymanJE, VitaleMG. Femoral deformity correction in children and young adults using Taylor Spatial Frame. Clin Orthop Relat Res2008;466:3018–3024.CrossrefPubMed Google Scholar
24 Sluga M , PfeifferM, KotzR, NehrerS. Lower limb deformities in children: two-stage correction using the Taylor spatial frame. J Pediatr Orthop B2003;12:123–128.CrossrefPubMed Google Scholar
25 Nakase T , KitanoM, KawaiH, et al.Distraction osteogenesis for correction of three-dimensional deformities with shortening of lower limbs by Taylor Spatial Frame. Arch Orthop Trauma Surg2009;129:1197–1201.CrossrefPubMed Google Scholar
26 Ganger R , RadlerC, SpeignerB, GrillF. Correction of post-traumatic lower limb deformities using the Taylor Spatial Frame. Int Orthop2010;34:723–730.CrossrefPubMed Google Scholar
27 Aldegheri R , Renzi-BrivioL, AgostiniS. The callotasis method of limb lengthening. Clin Orthop Relat Res1989;241:137–145.PubMed Google Scholar
28 Lavini F , Dall’OcaC, BartolozziP. Bone transport and compression-distraction in the treatment of bone loss of the lower limbs. Injury2010;41:1191–1195.CrossrefPubMed Google Scholar
29 McFadyen I, Atkins R. The Taylor Spatial Frame in trauma and limb reconstruction surgery: report of 100 cases. J Bone Joint Surg [Br] 2006;88-B(suppl 1):158. Google Scholar
30 Clarke SE , McCarthyJJ, DavidsonRS. Treatment of Blount disease: a comparison between the multiaxial correction system and other external fixators. J Pediatr Orthop2009;29:103–109.CrossrefPubMed Google Scholar
31 Placzek R , RufferM, DeuretzbacherG, HeijensE, MeissAL. The fixation strength of hydroxyapatite-coated Schanz screws and standard stainless steel Schanz screws in lower extremity lengthening: a comparison based on a new torque value index: the fixation index. Arch Orthop Trauma Surg2006;126:369–373. Google Scholar
32 Magyar G , Toksvig-LarsenS, MoroniA. Hydroxyapatite coating of threaded pins enhances fixation. J Bone Joint Surg [Br]1997;79-B:487–489.CrossrefPubMed Google Scholar
33 Pommer A , MuhrG, DávidA. Hydroxyapatite-coated Schanz pins in external fixators used for distraction osteogenesis: a randomized, controlled trial. J Bone Joint Surg [Am]2002;84-A:1162–1166. Google Scholar
34 Caja VL , PizăG, NavarroA. Hydroxyapatite coating of external fixation pins to decrease axial deformity during tibial lengthening for short stature. J Bone Joint Surg [Am]2003;85-A:1527–1531.CrossrefPubMed Google Scholar
35 Pizà G , CajaVL, González-ViejoMA, NavarroA. Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-track infection in leg lengthening for short stature. J Bone Joint Surg [Br]2004;86-B:892–897.CrossrefPubMed Google Scholar
36 Moroni A , HeikkilaJ, MagyarG, Toksvig-LarsenS, GianniniS. Fixation strength and pin tract infection of hydroxyapatite-coated tapered pins. Clin Orthop Relat Res2001;(388):209–217.CrossrefPubMed Google Scholar
37 Jergesen F . Open reduction of fractures and dislocations of the ankle. Am J Surg1959;98:136–151.CrossrefPubMed Google Scholar
38 Ruedi T , AllgowerM. Fractures of the lower end of the tibia into the ankle joint. Injury1969;1:92–99.CrossrefPubMed Google Scholar
39 Heim U, Näser M. [Operative treatment of distal tibial fractures. Technique of osteosynthesis and results in 128 patients (author’s transl)]. Arch Orthop Unfallchir 1976;86:341-356. Google Scholar
40 Kellam JF , WaddellJP. Fractures of the distal tibial metaphysis with intra-articular extension--the distal tibial explosion fracture. J Trauma1979;19:593–601.CrossrefPubMed Google Scholar
41 Bourne RB , RorabeckCH, MacnabJ. Intra-articular fractures of the distal tibia: the pilon fracture. J Trauma1983;23:591–596.CrossrefPubMed Google Scholar
42 Ovadia DN , BealsRK. Fractures of the tibial plafond. J Bone Joint Surg [Am]1986;68-A:543–551. Google Scholar
43 Teeny SM , WissDA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res1993;292:108–117.PubMed Google Scholar
44 Dillin L , SlabaughP. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma1986;26:1116–1119.CrossrefPubMed Google Scholar
45 Helfet DL , KovalK, PappasJ, SandersRW, DiPasqualeT. Intraarticular “pilon” fracture of the tibia. Clin Orthop Relat Res1994;298:221–228. Google Scholar
46 Sirkin M , SandersR, DiPasqualeT, HerscoviciD. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma1999;13:78–84.CrossrefPubMed Google Scholar
47 Patterson MJ , ColeJD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma1999;13:85–91.CrossrefPubMed Google Scholar
48 Giannoudis PV . Current concepts of the inflammatory response after major trauma: an update. Injury2003;34:397–404.CrossrefPubMed Google Scholar
49 Giannoudis PV, Giannoudi M, Stavlas P. Damage control orthopaedics: lessons learned. Injury 2009;40 (suppl4): S47-S52. Google Scholar
50 Morgan B, McFadyen I, Livingstone JA, Jackson M, Atkins RM. Outcome in patients with complex fractures of the tibial plateau treated with minimally invasive internal fixation and circular frame external fixation. J Bone Joint Surg [Br] 2012 vol. 94-B no. SUPP IV 148. Google Scholar
51 Al-Sayyad MJ . Taylor Spatial Frame in the treatment of pediatric and adolescent tibial shaft fractures. J Pediatr Orthop2006;26:164–170.CrossrefPubMed Google Scholar
52 Eidelman M , KatzmanA. Treatment of complex tibial fractures in children with the taylor spatial frame. Orthopedics2008;31:992.PubMed Google Scholar
53 Monsell FP , HowellsNR, LawniczakD, JeffcoteB, MitchellSR. High-energy open tibial fractures in children: treatment with a programmable circular external fixator. J Bone Joint Surg [Br]2012;94-B:989–993.CrossrefPubMed Google Scholar
54 Paley D , HerzenbergJE, ParemainG, BhaveA. Femoral lengthening over an intramedullary nail. A matched-case comparison with Ilizarov femoral lengthening. J Bone Joint Surg [Am]1997;79-A:1464–1480.CrossrefPubMed Google Scholar
55 Kocaoglu M , EralpL, RashidHU, SenC, BilselK. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg [Am]2006;88-A:2137–2145.CrossrefPubMed Google Scholar
56 Kristiansen LP , SteenH. Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator. Major complications and slow consolidation in 9 lengthenings. Acta Orthop Scand1999;70:271–274.CrossrefPubMed Google Scholar
57 Kocaoglu M , EralpL, BilenFE, BalciHI. Fixator-assisted acute femoral deformity correction and consecutive lengthening over an intramedullary nail. J Bone Joint Surg [Am]2009;91-A:152–159.CrossrefPubMed Google Scholar
58 Eralp L , KocaogluM, YusofNM, BulbulM. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg [Am]2007;89-A:2218–2224.CrossrefPubMed Google Scholar
59 Park HW , YangKH, LeeKS, et al.Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg [Am]2008;90-A:1970–1978.CrossrefPubMed Google Scholar
60 Kristiansen LP , SteenH. Lengthening of the tibia over an intramedullary nail, using the Izamov external fixator. Major complications and slow consultations in 9 lengthenings. Acta Orthop Scand1999;70:271–274. Google Scholar
61 Eralp L , KocaogluM, YusofNM, BulbulM. Distal tibial reconstruction with use of a circular external fixator and an intramedullary nail. The combined technique. J Bone Joint Surg [Am]2007;89-A:2218–2224.CrossrefPubMed Google Scholar
62 Park HW , YangKH, LeeKS, et al.Tibial lengthening over an intramedullary nail with use of the Ilizarov external fixator for idiopathic short stature. J Bone Joint Surg [Am]2008;90-A:1970–1978.CrossrefPubMed Google Scholar
63 Kim SJ , MandarA, SongSH, SongHR. Pitfalls of lengthening over an intramedullary nail in tibia: a consecutive case series. Arch Orthop Trauma Surg2012;132:185–191.CrossrefPubMed Google Scholar
64 Guo Q , ZhangT, ZhengY, et al.Tibial lengthening over an intramedullary nail in patients with short stature or leg-length discrepancy: a comparative study. Int Orthop2012;36:179–184.CrossrefPubMed Google Scholar
65 Sun XT , EaswarTR, Manesh S et al. Complications and outcome of tibial lengthening using the Ilizarov method with or without a supplementary intramedullary nail: a case-matched comparative study. J Bone Joint Surg [Br]2011;93-B:782–787.CrossrefPubMed Google Scholar
66 Gugenheim JJ , BrinkerMR. Bone realignment with use of temporary external fixation for distal femoral valgus and varus deformities. J Bone Joint Surg [Am]2003;85-A:1229–1237.CrossrefPubMed Google Scholar
67 Kendoff DO, Fragomen AT, Pearle AD, Citak M, Rozbruch SR. Computer navigation and fixator-assisted femoral osteotomy for correction of malunion after periprosthetic femur fracture. J Arthroplasty 2010;25:333.e13-333.e19. Google Scholar
68 Eralp L , KocaogluM, CakmakM, OzdenVE. A correction of windswept deformity by fixator assisted nailing. A report of two cases. J Bone Joint Surg [Br]2004;86-B:1065–1068.CrossrefPubMed Google Scholar
69 Rogers MJ , McFadyenI, LivingstoneJA, et al.Computer hexapod assisted orthopaedic surgery (CHAOS) in the correction of long bone fracture and deformity. J Orthop Trauma2007;21:337–342.CrossrefPubMed Google Scholar
70 Sen C , KocaogluM, EralpL, GulsenM, CinarM. Bifocal compression-distraction in the acute treatment of grade III open tibia fractures with bone and soft-tissue loss: a report of 24 cases. J Orthop Trauma2004;18:150–157.CrossrefPubMed Google Scholar
71 Green SA , JacksonJM, WallDM, MarinowH, IshkanianJ. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res1992;280:136–142.PubMed Google Scholar
72 Sen C , ErlapL, Gunes T et al. An alternative method for the treatment of nonunion of the tibia with bone loss. J Bone Joint Surg [Br]2006;88-B:783–789.CrossrefPubMed Google Scholar
73 Tsuchiya H , TomitaK, MinematsuK, et al.Limb salvage using distraction osteogenesis. A classification of the technique. J Bone Joint Surg [Br]1997;79-B:403–411.CrossrefPubMed Google Scholar
74 Tsuchiya H , Abdel-WanisME, SakurakichiK, YamashiroT, TomitaK. Osteosarcoma around the knee. Intraepiphyseal excision and biological reconstruction with distraction osteogenesis. J Bone Joint Surg [Br]2002;84-B:1162–1166.CrossrefPubMed Google Scholar









