Abstract
Aims
Evaluate if treating an unstable femoral neck fracture with a locking plate and spring-loaded telescoping screw system would improve construct stability compared to gold standard treatment methods.
Methods
A 31B2 Pauwels’ type III osteotomy with additional posterior wedge was cut into 30 fresh-frozen femur cadavers implanted with either: three cannulated screws in an inverted triangle configuration (CS), a sliding hip screw and anti-rotation screw (SHS), or a locking plate system with spring-loaded telescoping screws (LP). Dynamic cyclic compressive testing representative of walking with increasing weight-bearing was applied until failure was observed. Loss of fracture reduction was recorded using a high-resolution optical motion tracking system.
Results
LP constructs demonstrated the highest mean values for initial stiffness and failure load. LP and SHS constructs survived on mean over 50% more cycles and to loads 450 N higher than CS. During the early stages of cyclic loading, mean varus collapse of the femoral head was 0.5° (SD 0.8°) for LP, 0.7° (SD 0.7°) for SHS, and 1.9° (SD 2.3°) for CS (p = 0.071). At 30,000 cycles (1,050 N) mean femoral neck shortening was 1.8 mm (SD 1.9) for LP, 2.0 mm (SD 0.9) for SHS, and 3.2 mm (SD 2.5) for CS (p = 0.262). Mean leg shortening at construct failure was 4.9 mm (SD 2.7) for LP, 8.9 mm (SD 3.2) for SHS, and 7.0 mm (SD 4.3) for CS (p = 0.046).
Conclusion
Use of the LP system provided similar (hip screw) or better (cannulated screws) biomechanical performance as the current gold standard methods suggesting that the LP system could be a promising alternative for the treatment of unstable fractures of the femoral neck.
Cite this article: Bone Joint Res 2020;9(6):314–321.
Article focus
-
This study evaluated the biomechanical performance of a locking plate system with spring-loaded telescoping screws (LP) in cyclic compressive loading in comparison to two widely accepted gold standard treatment methods for an unstable femoral neck fracture.
-
The locking plate system was hypothesized to demonstrate improved survival and loss of fracture reduction compared to three cannulated screws in an inverted triangle configuration (CS) and a sliding hip screw system with anti-rotation screw (SHS).
Key messages
-
Femoral neck fracture fixation by LP and SHS both showed higher overall stiffness, biomechanical stability, and number of cycles to failure than by CS.
-
Adequate LP systems provide sufficient biomechanical stability and could be a promising alternative for the treatment of unstable fractures of the femoral neck.
Strengths and limitations
-
Primary strengths were the implementation of a physiologically representative test setup and increasing load protocol and clinically relevant outcome parameters.
-
The design of this study does not allow for speculation on the potential effect of the spring mechanism in the LP group on biomechanical stability.
Introduction
Femoral neck fractures typically account for over 50% of hip fractures, the incidence of which is expected to increase to 4.5 million worldwide by 2050.1 These fractures are especially common in patients prone to osteoporosis with low bone mineral density (BMD) but can also occur after high-impact trauma in younger individuals.2,3 The fixation of femoral neck fractures remains challenging, with relevant complication and nonunion rates despite advances in treatment.4,5 Femoral neck fractures are particularly problematic when they are displaced and occur at more vertically oriented angles, presenting a higher likelihood of failure due to instability.6 To date, there is no consensus in the medical community on the most appropriate technique for fixing femoral neck fractures, with the most commonly applied methods being screw fixation, sliding hip screw systems, and hip arthroplasty.3 The gold standard for vertical fractures of the femoral neck is the sliding hip screw (SHS; also when supplemented with an additional cannulated screw), which is sometimes recommended over three cannulated screws in an inverted triangle configuration (CS) mainly due to advantages in biomechanical performance.7-9 More recently, locking plate systems utilizing telescoping screws (LP) have been introduced and show encouraging clinical results.10-12
The aim of this study was to evaluate the biomechanical performance of a locking plate system in cyclic compressive loading in comparison to two widely accepted gold standard treatment methods for an unstable femoral neck fracture. Comparisons were made between CS, SHS, and a LP construct in a worst-case configuration with only two out of three screws implanted. We hypothesized that in an unstable femoral neck fracture the LP construct would demonstrate improved survival and loss of fracture reduction compared to these gold standard treatment methods (Figure 1).
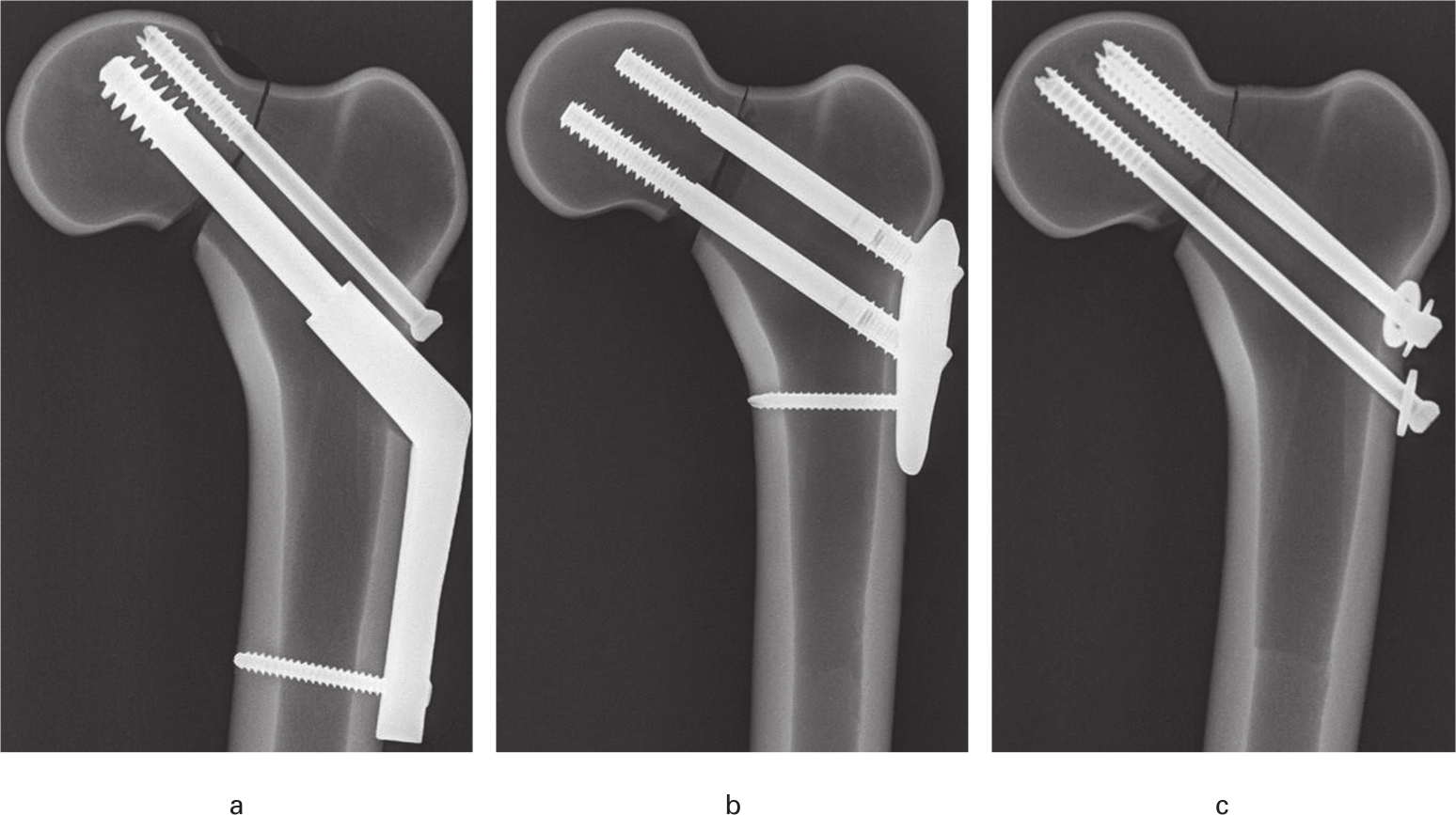
Fig. 1
a) Sliding hip screw and anti-rotation screw (SHS). b) Locking plate with spring-loaded telescoping screw-plate system (LP). c) Three cannulated screws in an inverted triangle configuration (CS). Representative configurations implanted in Sawbones specimens (Malmö, Sweden) for demonstration purposes only.
Methods
A total of 30 fresh-frozen human femora from 15 female donors with a mean age of 62 years (SD 8) and a mean body mass index of 34 kg/m2 (SD 9) were obtained through a commercial body donation programme (Science Care, Phoenix, Arizona, USA) to be used in this study. Only specimens without any signs of previous fracture, deformities, or bone tumours were included. All specimens were scanned by quantitative CT (160 kV, 60 mA, slice thickness 0.75 mm, SOMATOM AS+; Siemens AG, Erlangen, Germany) to assess BMD at the femoral neck and head. Analysis was conducted using clinical medical imaging software (ImpaxEE R20 VII; Agfa HealthCare, Bonn, Germany) and femoral head BMD was calculated using a European Forearm Phantom calibration. Specimens were evenly distributed based on BMD into three groups: LP, CS, and SHS. Distribution was carried out such that two femora from the same specimen were never assigned to the same group. Mean BMD across all specimens was measured to be 233 mg/cm3 (SD 73), with no significant differences between groups (p = 0.980, multivariate analysis of variance (MANOVA)). Mean femoral neck length was found to be 50 mm (SD 3) across all specimens when measured from CT scans as per the methods of Nakamura et al,13 also with no significant differences between groups (p = 0.995, MANOVA).
All specimens were stored at -20°C before preparation and testing and allowed to thaw overnight before implantation. The fracture model was an OTA/AO 31B2 osteotomy14 with a calcar wedge and smaller posterior wedge positioned cranial dorsal of the femoral neck, further classified as a Pauwels type III fracture at an angle of 70° to the horizontal,15 reproducibly implemented using a custom sawing guide. The CONQUEST FN 1-hole locking plate system with locking screws that employ a dedicated spring mechanism for fracture site compression was implanted for the LP group, utilizing only the calcar and anterosuperior screw holes, as well as a 4.5 mm shaft screw. Although implanting three spring-loaded screws is the standard surgical technique, inserting only two screws is FDA-approved due to anatomical constraints and limitations or in the case of small stature patients. The CS group was implanted with three 7.0 mm cannulated screws in the inverted triangle configuration and washers corresponding to each screw. The SHS group comprised a 130° 2-slot 60 mm sliding hip screw and an additional 6.5 mm cannulated screw implanted superiorly, often referred to as the ‘anti-rotation’ screw. Implantation of the sliding hip screw without ‘anti-rotation’ screw is a widely accepted treatment method; however, we chose to implant the construct with the additional ‘anti-rotation’ screw to embody one of the strongest options currently available for such fractures.
The orthopaedic equipment for all groups had the same manufacturer (Smith & Nephew, Cordova, Tennessee, USA). All implantations were conducted under radiograph control according to the manufacturer’s guidelines per respective fixation technique by a fellowship-trained orthopaedic surgeon. Specimens were cut to a length of 25 cm, measured from the most superior point of the femur, and embedded distally in 5 cm of a three-component casting resin (RenCast FC53A/B + Filler DT082; Gößl + Pfaff, Karlskron/Brautlach, Germany). Samples were embedded such that the femoral head was vertically aligned with the femoral condyles with the femoral shaft inclined by 7°.
For biomechanical testing each specimen was mounted at 10° adduction and 11° extension (Figure 2), representing the physiological direction of the maximum applied hip forces during gait.16 The femoral head was seated into a customary inverted hemispherical chamber attached to a multidirectional bearing plate fixed to the load cell on the actuator of an electrodynamic testing machine (E3000; Instron, High Wycombe, UK). The embedding protocol ensured that the distal portion of each specimen was fully constrained within the test apparatus throughout testing. After preloading each specimen to 50 N, three quasistatic ramp loads of 10 mm per minute to 500 N were conducted to determine initial axial construct stiffness, calculated from the linear portion of the load-deformation curve. Specimens were then cyclically loaded to failure at 2 Hz frequency. Cyclic sinusoidal compressive loading with a tapered sine waveform began with the initial 500 N upper load and stepwise increasing upper loads by 50 N every 2500 cycles. The lower load limit was always 50 N. Failure was defined as construct breakage, reaching a vertical actuator limit of 15 mm, or a maximum applied load of 3,000 N, whichever occurred first.
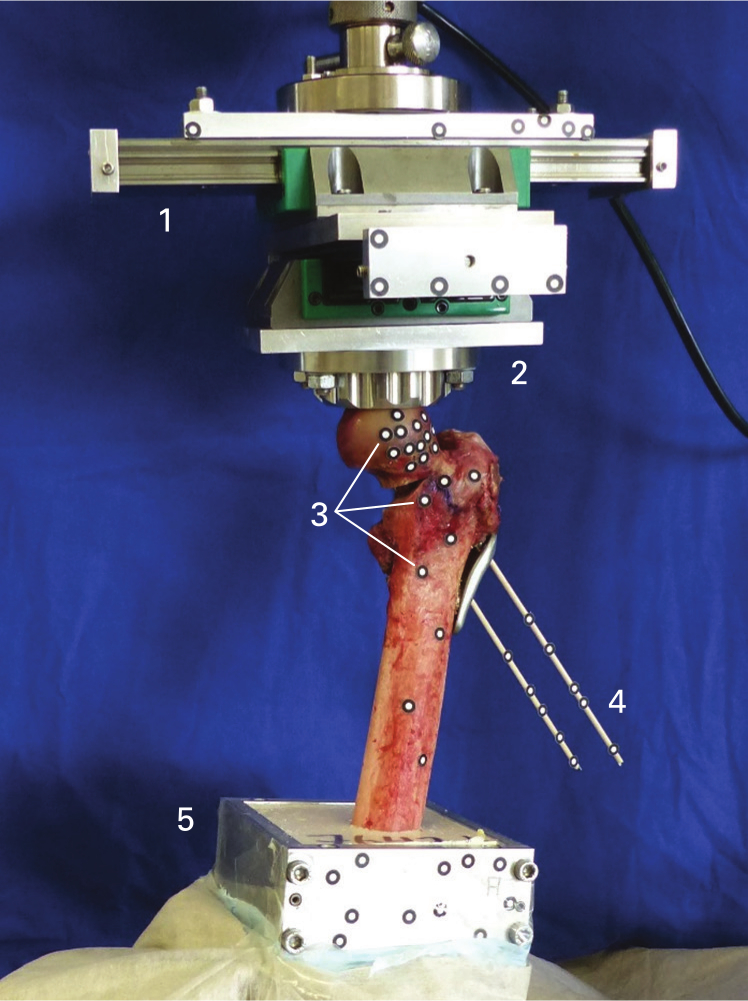
Fig. 2
Biomechanical test setup with multidirectional bearing plate (1), inverted hemispherical chamber (2), reference markers for movement analysis (3), adaptors for definition of the neck axis (4), and rigid embedding (5).
During all tests a 3D high-resolution motion tracking system (ARAMIS 5 M; GOM, Braunschweig, Germany) was used to record displacement of the femoral head fragment with respect to the shaft fragment, identified by groups of reference markers affixed to each specimen. The system took photos every 500 cycles at both the fully loaded and 50 N levels and conducted analysis based on data obtained in these photos. Marker displacement analysis was aided with the construction of two different coordinate systems based on the axes of the femoral neck and shaft, as defined in the corresponding software programme (GOM Correlate Professional 2018; GOM). Failure mode, location, reference marker displacement, and construct stiffness were recorded and each sample was photographed.
Parameters of interest were varus collapse, femoral neck shortening, and rotation of the femoral head. Varus collapse was defined as rotation of the femoral head in the frontal plane about the sagittal axes. Femoral head rotation was calculated about the axis of the femoral neck in both the posterior and anterior directions, and femoral neck shortening as lateral displacement along the femoral neck axis. Leg shortening in the form of inferior dislocation of the femoral head with respect to the shaft was analyzed to provide an indication of expected leg length discrepancy. Leg shortening can be understood to occur as a result of neck shortening and varus collapse combined. All outcome parameters were calculated in terms of movement of the femoral head relative to the femoral shaft. To ensure that values were representative of permanent (plastic) deformation during loading, measurements were only taken at the minimum compressive load (50 N) to provide an indication of non-recoverable deviations from the initial state of the system.
Permanent deformation was analyzed at three instances: initially (after a 500 N static ramp and before cyclic loading), after 30,000 cycles (representative of three to four weeks of healing time),17 and at the final recorded point before failure was observed in each specimen. Values calculated at 30,000 cycles excluded all samples that had failed before this point (two SHS and three each of CS and LP groups). Comparison was chosen to be conducted at this number of cycles because it represents a later point in cyclic loading before a large portion of CS samples exhibited failure shortly thereafter. The maximum force applied at 30,000 cycles was 1,050 N, which is the load typically expected at the femoral head for the tested population (mean 91 kg (SD 28)) during walking under partial weight-bearing (50%).16
Quasistatic measurement data were normally distributed according to a Shapiro-Wilk test (p = 0.109). Independent variables were treatment method (LP, CS, SHS) and dependent variables included neck shortening, varus collapse, femoral head rotation, leg shortening, initial stiffness, and cycles to failure. Testing for significant differences between groups was performed using MANOVA with Bonferroni correction and femoral head BMD as a covariate. Movement values were reported prior to testing, after 30,000 cycles and at failure. Kaplan-Meier survival analysis was performed in terms of the number of cycles to failure. All statistical testing was carried out using SPSS Software (IBM SPSS Statistics v19; IBM, Armonk, New York, USA). Statistical significance was set at p < 0.05.
Results
Construct stiffness values during the initial quasistatic ramps varied widely, ranging from 157 N/mm to 1,396 N/mm (Table I). The maximum number of cycles survived during loading also varied; one LP specimen reached the maximum applied load of 3,000 N without any obvious sign of failure while one CS specimen failed already after 500 N static loading before cyclic testing began (Table I). Based on mean values, LP and SHS specimens survived over 50% longer than CS specimens, with no significant differences between groups observed (p = 0.347; Kaplan-Meier survival; Figure 3). The predominant failure mode observed was reaching of the defined 15 mm limit, occurring in the form of varus collapse and femoral neck shortening (Figure 4). Three specimens (SHS and two LP) failed by a fracture at the femoral shaft. In terms of hardware failure, the calcar screw of one of the LP specimens was discovered as having broken at the distal screw thread. There was no significant correlation found between maximum applied load and femoral neck length (p = 0.187, R2 = 0.064; Pearson r ).
Table I.
Initial stiffness, number of cycles, and maximum load to failure for three groups: sliding hip screw with anti-rotation screw; locking plate system with spring-loaded telescoping screws; and three cannulated screws in an inverted triangle configuration.
| Group | Mean initial stiffness, N/mm (SD) | Mean cycles to failure, n (SD) | Mean load at failure, N (SD) |
|---|---|---|---|
| SHS | 535 (172) | 65,974 (33,670) | 1,790 (674) |
| LP | 805 (414) | 66,933 (43,726) | 1,815 (873) |
| CS | 625 (351) | 43,775 (36,289) | 1,355 (720) |
-
CS, three cannulated screws in an inverted triangle configuration; LP, locking plate system with spring-loaded telescoping screws; SHS, sliding hip screw with anti-rotation screw.
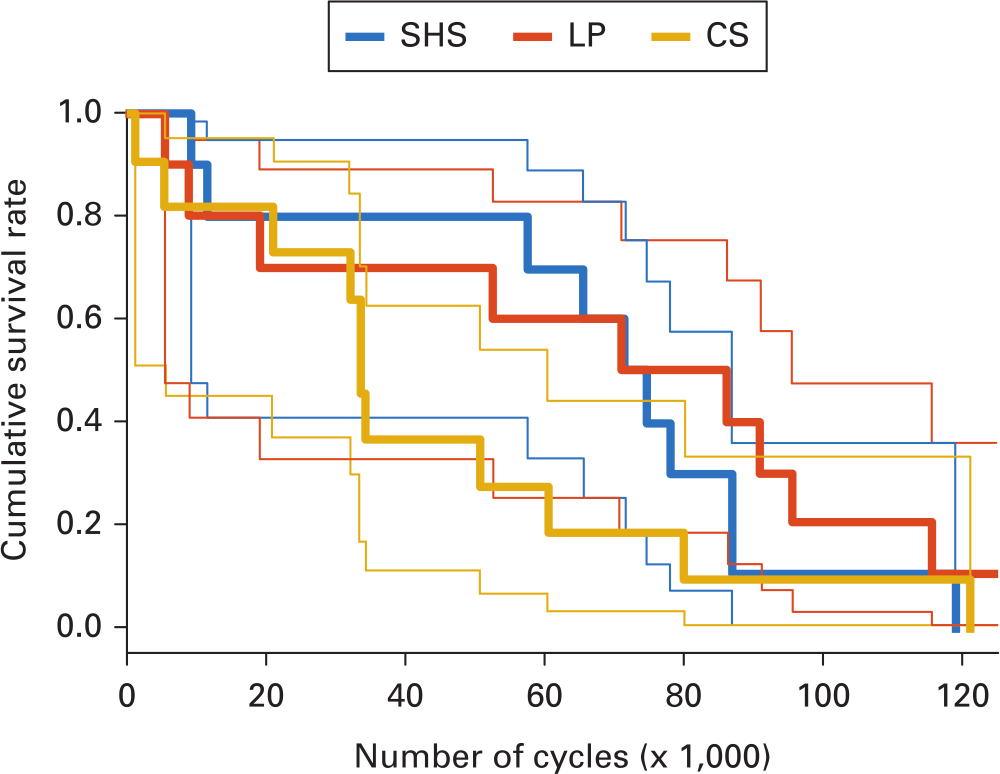
Fig. 3
Cumulative rate of survival for all three groups (n = 10 each) in terms of number of cycles until failure criteria were reached. CS, three cannulated screws in an inverted triangle configuration; LP, locking plate system with spring-loaded telescoping screws; SHS, sliding hip screw with anti-rotation screw. 95% standard error bands for each group are depicted by the thinner lines corresponding to each respective colour.
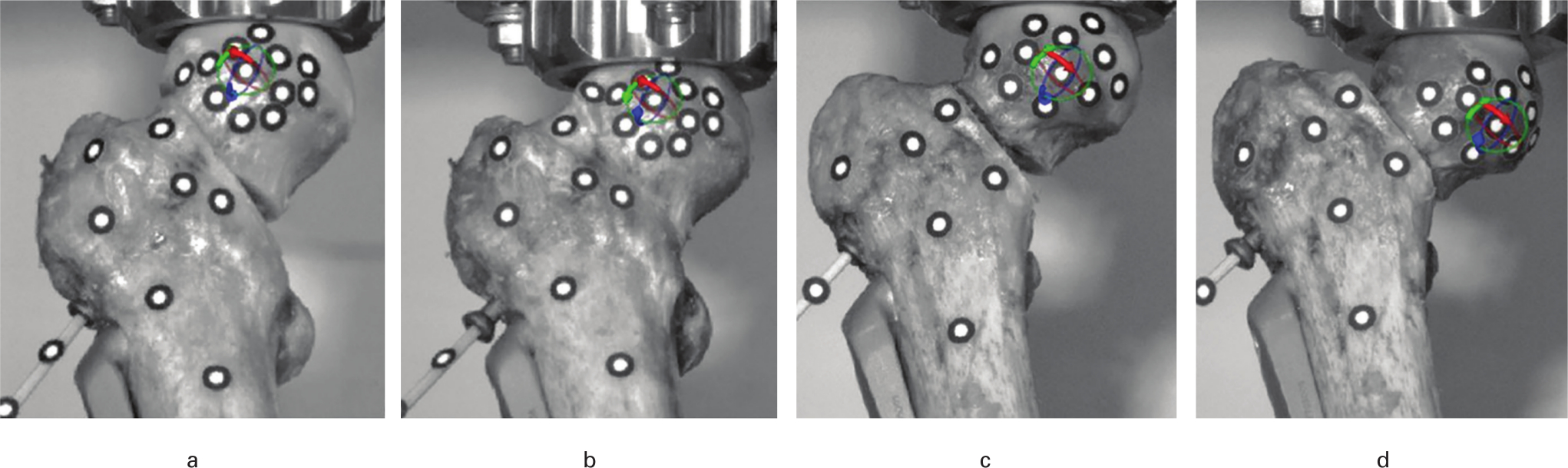
Fig. 4
Specimens before (A and B) and after cyclic testing exhibiting neck shortening (C: 78,000 cycles and 2,000 N) and varus collapse (D: 57,000 cycles and 1,600 N).
Results for varus collapse and femoral neck shortening can be seen in Figures 5 and 6, respectively. The LP group exhibited the lowest amount of leg shortening at all points of analysis. At 30,000 cycles mean leg shortening was 3.4 mm for SHS (95% confidence interval (CI) 1.2 to 5.2), 2.0 mm for LP (95% CI 0.2 to 4.5), and 5.6 mm for CS (95% CI 3.4 to 7.6), with no statistically significant differences found (p = 0.104, MANOVA; n = 22). Values increased up until construct failure, with LP constructs showing a mean value significantly lower than SHS at failure when adjusted for number of cycles (p = 0.046, MANOVA). Mean leg shortening values at failure were 4.9 mm for LP (95% CI 2.8 to 7.3), 8.9 mm for SHS (95% CI 6.8 to 11.3), and 7.0 mm for CS (95% CI 4.4 to 9.0; p = 0.049, MANOVA; n = 30).
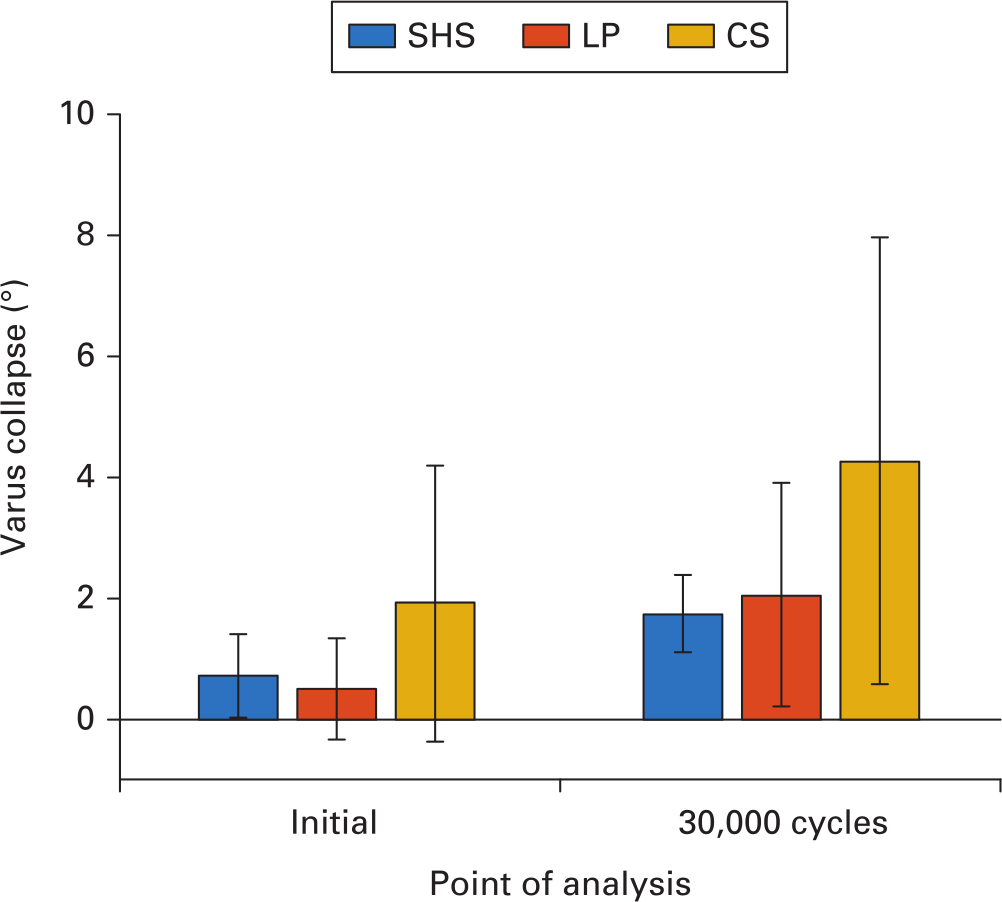
Fig. 5
Plastic deformation of the femoral head in the form of varus collapse initially (pre-cyclic loading) and after 30,000 cycles for the three study groups: sliding hip screw and anti-rotation screw (SHS); locking plate with spring-loaded telescoping screws (LP); and three cannulated screws in an inverted triangle configuration (CS).
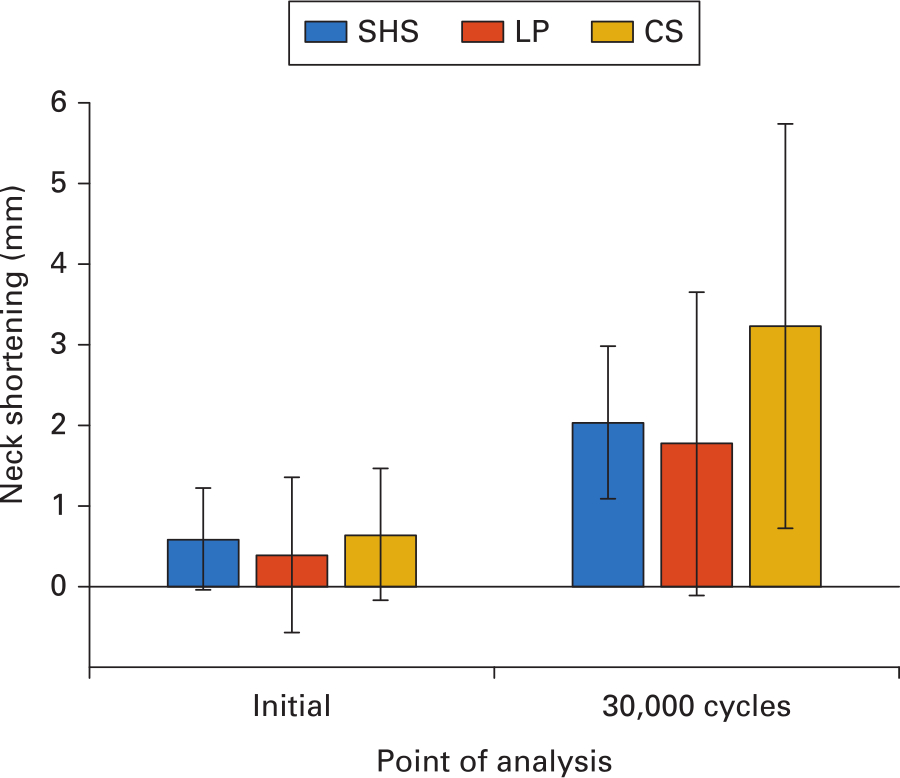
Fig. 6
Plastic deformation in the form of femoral neck shortening initially (pre-cyclic loading) and after 30,000 cycles for the three study groups: sliding hip screw and anti-rotation screw (SHS); locking plate with spring-loaded telescoping screws (LP); and three cannulated screws in an inverted triangle configuration (CS).
The direction of the rotation of the femoral head around the femoral neck axis was not consistent, with most specimens rotating posteriorly and approximately one-third in the anterior direction. Thus, only absolute values are presented for this parameter. The LP constructs showed the lowest amount of rotation initially with a mean value of 0.8° (95% CI -0.6° to 2.3°), compared to 2.1° observed for CS constructs (95% CI 0.7° to 3.5°; p = 0.395, MANOVA; n = 30). The mean amount of femoral head rotation at 30,000 cycles was 2.0° for LP (95% CI 0.3° to 4.0°), 3.1° for SHS (95% CI 1.3° to 4.8°), and 5.0° for CS (95% CI 3.1° to 6.8°; p = 0.107, MANOVA; n = 22). At failure, femoral head rotation was 5.8° for LP (95% CI 1.6° to 9.7°), 7.8° for SHS (95% CI 3.7° to 11.7°), and 9.5° for CS (95% CI 5.6° to 13.8°; p = 0.368, MANOVA; n = 30).
Discussion
The primary aim of this study was to evaluate the biomechanical performance of a locked plating system for the fixation of unstable femoral neck fractures and compare it to the gold standard fixation methods of cannulated screws and a sliding hip screw system with anti-rotation screw. Both the LP and SHS constructs demonstrated superiority over CS constructs in terms of the mean number of cycles to failure, initial axial stiffness, and loss of fracture reduction during loading. The LP system demonstrated similar mechanical performance to a sliding hip screw construct with anti-rotation screw.
LP was found to exhibit the highest stability in initial loading across all recorded variables. This trend could also be observed in values recorded at 30,000 cycles, except for varus collapse, of which SHS demonstrated a slightly lower mean value by 0.3°. Relative fragment displacements in the early stages of loading were relatively low, which may bring into question their clinical relevance. However, data recorded at these stages together with the initial stiffness values should still be taken into consideration when assessing implant performance, as such low-loading scenarios represent situations common to early postoperative recovery under reduced weight-bearing. While smaller relative displacement and higher construct stiffness are likely to promote fracture healing in the femoral neck, large displacements due to reduced construct stiffness may initiate healing disturbances.18
The CS construct exhibited the most varus collapse at all three analyzed timepoints, demonstrating room for improvement in the stabilization of such a fracture under typically expected loads. Furthermore, the high femoral neck rotation values observed in the CS group at failure could affect functional outcomes if observed clinically, as malalignment of the two fracture fragments would reduce the likelihood of proper healing.19 This outcome is substantiated by high failure rates of CS constructs reported clinically.20
The results of this study correspond with those of similarly carried out biomechanical studies showing better performance of SHS than CS for this type of fracture.21-23 Furthermore, our results for neck shortening24 and varus collapse25 at construct failure are comparable to those published in clinical studies. The consistent improved performance of LP in terms of leg shortening is also worth considering; clinically, leg length discrepancy is commonly observed after internal fixation of femoral neck fractures and increased prevalence is associated with consequences such as pain, limping, impaired mobility, and a higher fall risk.26,27
Although statistically significant differences were unable to be demonstrated for most outcome parameters, a trend for higher biomechanical stability was observed in the LP group at the first two reported timepoints. Because successful initiation of fracture healing requires proper reduction and stabilization of the fracture, it may be that the mechanical environment of the injury in the initial stages after surgery is one of the most important factors with regard to achieving successful patient outcomes. The higher load and larger number of cycles to failure demonstrated by LP and SHS also offer benefits in terms of clinical outcomes, as cut-out and screw penetration are frequent failure mechanisms, especially in osteoporotic bone.28
The biomechanical benefits of locked plating for fixation of the femoral neck have been suggested in other studies, specifically in more vertical fractures.29-31 The design of this study unfortunately does not allow for inference on the potential benefits of the spring mechanism of the tested LP construct specifically. The results presented are only indicative of overall performance differences between this technology and other gold standard methods.
This study has a number of strengths, as well as limitations. With regard to biomechanical testing, a primary strength of this study was the implementation of a physiologically representative test setup and realistic increasing load protocol. Furthermore, the fracture model applied in this study included an additional posterior wedge to represent supplementary posterior comminution, which has been shown to decrease fixation strength and diminish the rate of fracture healing.32,33 Our calculation of parameters such as varus collapse is similar to methods carried out in another similar biomechanical study.34
The implants used in this study were chosen with clinical relevance and realistic usage in mind. The CS system has demonstrated clinical35 and biomechanical36 pertinence as an approach for treating femoral neck fractures, alongside the additional use of washers for further stabilization.37 The SHS system has been shown to improve biomechanical stability38 and is considered to be the ‘best-case’ construct among gold standard fixation methods.39 Only two out of three possible locking screws were implanted in the LP to simulate a ‘worst-case’ scenario, taking into account the smaller femoral neck sizes typically seen in the tested population of elderly osteoporotic women. Although other novel devices have been more recently introduced to treat these types of fractures,40 we designed our study with the intention of comparing against the most popular options available.
Many of the limitations of this study are inherent to all biomechanical studies carried out on cadaver specimens. Forces due to muscles and other soft tissues were not considered in our loading protocol. Although all implantations were carried out by a single surgeon (SH) in a repeatable manner, it is likely that minor deviations in implant position within an expected range occurred, possibly due to variations in specimen anatomy. Specimen groups were allocated using BMD values as opposed to other methods such as matched pairs analysis, or the size of the femoral shaft and neck. Differences in specimen size may have had an impact on the resultant moments across the neck fracture site during loading. The boundary conditions of the test setup implemented in this study may have over-constrained the distal end of the femur; however, we felt that such a setup was necessary to maintain construct stability over the prolonged cyclic loading period. Finally, although all specimens were thoroughly hydrated with sodium chloride spray during preparation and upon starting tests, they were not continuously conditioned during the test periods, which could have had an effect on the bone material properties.
In conclusion, the LP group demonstrated the least loss of fracture reduction in early stages of loading, as well as significantly less leg shortening at construct failure. LP and SHS both showed higher overall stiffness, biomechanical stability, and number of cycles to failure than the CS specimens. Due to greater loss of fracture reduction as well as lower stiffness and likelihood of survival, cannulated screws should be used with caution for the treatment of unstable vertical femoral neck fractures, such as those with extensive posterior comminution. Our findings suggest that a locking plate system provides sufficient biomechanical stability for unstable femoral neck fractures and could be a promising alternative to a hip screw system, even when implemented as a ‘worst-case’ configuration with only two screws. The applicability of these results with regard to real patient outcomes should be further investigated in clinical studies.
References
1. Gullberg B , Johnell O , Kanis JA . World-Wide projections for hip fracture . Osteoporos Int . 1997 ; 7 ( 5 ): 407 – 413 . Crossref PubMed Google Scholar
2. Gnudi S , Sitta E , Pignotti E . Prediction of incident hip fracture by femoral neck bone mineral density and neck–shaft angle: a 5-year longitudinal study in post-menopausal females . Br J Radiol . 2012 ; 85 ( 1016 ): e467 – e473 . Google Scholar
3. Augat P , Bliven E , Hackl S . Biomechanics of femoral neck fractures and implications for fixation . J Orthop Trauma . 2019 ; 33 ( Suppl 1 ): S27 – S32 . Crossref PubMed Google Scholar
4. Broderick JM , Bruce-Brand R , Stanley E , Mulhall KJ . Osteoporotic hip fractures: the burden of fixation failure . ScientificWorldJournal . 2013 ; 2013 ( 425 ): 515197. Crossref PubMed Google Scholar
5. Damany DS , Parker MJ , Chojnowski A . Complications after intracapsular hip fractures in young adults. A meta-analysis of 18 published studies involving 564 fractures . Injury . 2005 ; 36 ( 1 ): 131 – 141 . Crossref PubMed Google Scholar
6. Liporace F , Gaines R , Collinge C , Haidukewych GJ . Results of internal fixation of Pauwels type-3 vertical femoral neck fractures . J Bone Joint Surg Am . 2008 ; 90 ( 8 ): 1654 – 1659 . PubMed Google Scholar
7. Bhandari MD . Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH) Investigators. Fracture fixation in the operative management of hip fractures (FAITH): an international, multicentre, randomised controlled trial . Lancet . 2017 ; 389 ( 10078 ): 1519 – 1527 . Google Scholar
8. Florschutz AV , Langford JR , Haidukewych GJ , Koval KJ . Femoral neck fractures: current management . J Orthop Trauma . 2015 ; 29 ( 3 ): 121 – 129 . Crossref PubMed Google Scholar
9. JX M , Kuang MJ , Xing F , et al. Sliding hip screw versus cannulated cancellous screws for fixation of femoral neck fracture in adults: a systematic review . Int J Surg . 2018 ; 52 : 89 – 97 . Crossref PubMed Google Scholar
10. Eschler A , Brandt S , Gierer P , Mittlmeier T , Gradl G . Angular stable multiple screw fixation (Targon FN) versus standard shs for the fixation of femoral neck fractures . Injury . 2014 ; 45 ( Suppl 1 ): S76 – S80 . Crossref PubMed Google Scholar
11. Griffin XL , Parsons N , Achten J , Costa ML . The Targon Femoral Neck hip screw versus cannulated screws for internal fixation of intracapsular fractures of the hip . Bone Joint J . 2014 ; 96-B ( 5 ): 652 – 657 . Crossref PubMed Google Scholar
12. Brandt E , Verdonschot N , van Vugt A , van Kampen A . Biomechanical analysis of the sliding hip screw, cannulated screws and Targon® FN in intracapsular hip fractures in cadaver femora . Injury . 2011 ; 42 ( 2 ): 183 – 187 . Google Scholar
13. Nakamura T , Turner CH , Yoshikawa T , et al. Do variations in hip geometry explain differences in hip fracture risk between Japanese and white Americans? J Bone Miner Res . 1994 ; 9 ( 7 ): 1071 – 1076 . Crossref PubMed Google Scholar
14. Meinberg EG , Agel J , Roberts CS , Karam MD , Kellam JF . Fracture and dislocation classification Compendium—2018 . J Orthop Trauma . 2018 ; 32 ( Suppl 1 ): S1 – S10 . Google Scholar
15. Bartoníček J . Pauwels' classification of femoral neck fractures: correct interpretation of the original . J Orthop Trauma . 2001 ; 15 ( 5 ): 358 – 360 . Crossref PubMed Google Scholar
16. Schwachmeyer V , Damm P , Bender A , et al. In vivo hip joint loading during post-operative physiotherapeutic exercises . PLoS One . 2013 ; 8 ( 10 ): e77807 . Crossref PubMed Google Scholar
17. Toogood PA , Abdel MP , Spear JA , et al. The monitoring of activity at home after total hip arthroplasty . Bone Joint J . 2016 ; 98-B ( 11 ): 1450 – 1454 . Crossref PubMed Google Scholar
18. Claes LE , Heigele CA , Neidlinger-Wilke C , et al. Effects of mechanical factors on the fracture healing process . Clin Orthop Relat Res . 1998 ; 355S ( 355 Suppl ): S132 – S147 . Crossref PubMed Google Scholar
19. Ghiasi MS , Chen J , Vaziri A , Rodriguez EK , Nazarian A . Bone fracture healing in mechanobiological modeling: a review of principles and methods . Bone Reports . 2017 ; 6 : 87 – 100 . Crossref PubMed Google Scholar
20. Gregersen M , Krogshede A , Brink O , Damsgaard EM . Prediction of reoperation of femoral neck fractures treated with cannulated screws in elderly patients . Geriatr Orthop Surg Rehabil . 2015 ; 6 ( 4 ): 322 – 327 . Crossref PubMed Google Scholar
21. Deneka DA , Simonian PT , Stankewich CJ , et al. Biomechanical comparison of internal fixation techniques for the treatment of unstable basicervical femoral neck fractures . J Orthop Trauma . 1997 ; 11 ( 5 ): 337 – 343 . Crossref PubMed Google Scholar
22. Stoffel K , Zderic I , Gras F , et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: a comparison with the dynamic hip screw and cannulated screws . J Orthop Trauma . 2017 ; 31 ( 3 ): 131 – 137 . Crossref PubMed Google Scholar
23. Cha Y-H , Yoo J-I , Hwang S-Y , et al. Biomechanical evaluation of internal fixation of Pauwels type III femoral neck fractures: a systematic review of various fixation methods . Clin Orthop Surg . 2019 ; 11 ( 1 ): 1 – 14 . Crossref PubMed Google Scholar
24. Stockton DJ , Lefaivre KA , Deakin DE , et al. Incidence, magnitude, and predictors of shortening in young femoral neck fractures . J Orthop Trauma . 2015 ; 29 ( 9 ): e293 – e298 . Crossref PubMed Google Scholar
25. Zlowodzki M , Brink O , Switzer J , et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip . J Bone Joint Surg Br . 2008 ; 90-B ( 11 ): 1487 – 1494 . Crossref PubMed Google Scholar
26. Harris I , Hatfield A , Walton J . Assessing leg length discrepancy after femoral fracture: clinical examination or computed tomography? ANZ J Surg . 2005 ; 75 ( 5 ): 319 – 321 . Google Scholar
27. Haider T , Schnabel J , Hochpöchler J , Wozasek GE . Femoral shortening does not impair functional outcome after internal fixation of femoral neck fractures in non-geriatric patients . Arch Orthop Trauma Surg . 2018 ; 138 ( 11 ): 1511 – 1517 . Google Scholar
28. Yih-Shiunn L , Chien-Rae H , Wen-Yun L . Surgical treatment of undisplaced femoral neck fractures in the elderly . Int Orthop . 2007 ; 31 ( 5 ): 677 – 682 . Crossref PubMed Google Scholar
29. Nowotarski PJ , Ervin B , Weatherby B , et al. Biomechanical analysis of a novel femoral neck locking plate for treatment of vertical shear Pauwel's type C femoral neck fractures . Injury . 2012 ; 43 ( 6 ): 802 – 806 . Crossref PubMed Google Scholar
30. Samsami S , Saberi S , Sadighi S , Rouhi G . Comparison of three fixation methods for femoral neck fracture in young adults: experimental and numerical investigations . J Med Biol Eng . 2015 ; 35 ( 5 ): 566 – 579 . Crossref PubMed Google Scholar
31. Li J , Zhao Z , Yin P , Zhang L , Tang P . Comparison of three different internal fixation implants in treatment of femoral neck fracture—a finite element analysis . J Orthop Surg Res . 2019 ; 14 ( 1 ): 76 . Google Scholar
32. Scheck M . The significance of posterior comminution in femoral neck fractures . Clin Orthop Relat Res . 1980 ; 152 : 138 – 142 . PubMed Google Scholar
33. Huang T-W , Hsu W-H , Peng K-T , Lee C-Y . Effect of integrity of the posterior cortex in displaced femoral neck fractures on outcome after surgical fixation in young adults . Injury . 2011 ; 42 ( 2 ): 217 – 222 . Crossref PubMed Google Scholar
34. Acklin YP , Zderic I , Inzana JA , et al. Biomechanical evaluation of a new gliding screw concept for the fixation of proximal humeral fractures . Bone Joint Res . 2018 ; 7 ( 6 ): 422 – 429 . Crossref PubMed Google Scholar
35. Yang J-J , Lin L-C , Chao K-H , et al. Risk factors for nonunion in patients with intracapsular femoral neck fractures treated with three cannulated screws placed in either a triangle or an inverted triangle configuration . J Bone Joint Surg Am . 2013 ; 95 ( 1 ): 61 – 69 . Crossref PubMed Google Scholar
36. Li J , Wang M , Zhou J , et al. Optimum configuration of cannulated compression screws for the fixation of unstable femoral neck fractures: finite element analysis evaluation . Biomed Res Int . 2018 ; 2018 ( 1 ): 1271762 – 10 . Crossref PubMed Google Scholar
37. Zlowodzki MP , Wijdicks CA , Armitage BM , Cole PA . Value of Washers in internal fixation of femoral neck fractures with cancellous screws . J Orthop Trauma . 2015 ; 29 ( 2 ): e69 – e72 . Crossref PubMed Google Scholar
38. Kemker B , Magone K , Owen J , et al. A sliding hip screw augmented with 2 screws is biomechanically similar to an inverted triad of cannulated screws in repair of a Pauwels type-III fracture . Injury . 2017 ; 48 ( 8 ): 1743 – 1748 . Crossref PubMed Google Scholar
39. Makki D , Mohamed AM , Gadiyar R , Patterson M . Addition of an anti-rotation screw to the dynamic hip screw for femoral neck fractures . Orthopedics . 2013 ; 36 ( 7 ): e865 – e868 . Crossref PubMed Google Scholar
40. Kalsbeek JH , van Walsum ADP , Vroemen JPAM , et al. Displaced femoral neck fractures in patients 60 years of age or younger: results of internal fixation with the dynamic locking blade plate . Bone Joint J . 2018 ; 100-B ( 4 ): 443 – 449 . Crossref PubMed Google Scholar
Author contributions
E. Bliven: Prepared the manuscript draft, Performed the experiments, Collected the data, Revised, read, and approved the final manuscript.
S. Sandriesser: Performed the experiments, Collected the data, Revised, read, and approved the final manuscript.
P. Augat: Designed the study, Prepared the manuscript draft, Revised, read, and approved the final manuscript.
C. von Rüden: Performed the specimen preparation, Revised, read, and approved the final manuscript.
S. Hackl: Designed the study, Performed the specimen preparation, Revised, read, and approved the final manuscript.
Funding statement
Although none of the authors has received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article, benefits have been or will be received but will be directed solely to a research fund, foundation, educational institution, or other non- profit organization with which one or more of the authors are associated.
ICMJE COI statement
All of the authors report provision of materials and payment for biomechanical tests (paid to BG Unfallklinik Murnau) from Smith & Nephew USA, related to this study.
Acknowledgements
The authors would like to gratefully acknowledge and thank Martin Winkler for his valuable help and insight provided throughout the completion of this study.
This study did not require ethical approval.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









