Abstract
Objectives
Salubrinal is a synthetic agent that elevates phosphorylation of eukaryotic translation initiation factor 2 alpha (eIF2α) and alleviates stress to the endoplasmic reticulum. Previously, we reported that in chondrocytes, Salubrinal attenuates expression and activity of matrix metalloproteinase 13 (MMP13) through downregulating nuclear factor kappa B (NFκB) signalling. We herein examine whether Salubrinal prevents the degradation of articular cartilage in a mouse model of osteoarthritis (OA).
Methods
OA was surgically induced in the left knee of female mice. Animal groups included age-matched sham control, OA placebo, and OA treated with Salubrinal or Guanabenz. Three weeks after the induction of OA, immunoblotting was performed for NFκB p65 and p-NFκB p65. At three and six weeks, the femora and tibiae were isolated and the sagittal sections were stained with Safranin O.
Results
Salubrinal suppressed the progression of OA by downregulating p-NFκB p65 and MMP13. Although Guanabenz elevates the phosphorylation level of eIF2α, it did not suppress the progression of OA.
Conclusions
Administration of Salubrinal has chondroprotective effects in arthritic joints. Salubrinal can be considered as a potential therapeutic agent for alleviating symptoms of OA.
Cite this article: Bone Joint Res 2015;4:84–92
Article focus
The goal was to examine whether daily administration of Salubrinal to a mouse model of osteoarthritis (OA) alleviates the degradation of articular cartilage in the femur and tibia.
Key messages
Salubrinal suppressed the progression of OA by downregulating the phosphorylation of nuclear factor kappa B p65 and the activity of matrix metalloproteinase 13.
Although both Salubrinal and Guanabenz suppress stress to the endoplasmic reticulum, daily administration of Guanabenz did not prevent the progression of OA.
Strength and limitations
Strengths: This is a pre-clinical study that indicates novel treatment of patients with OA. Salubrinal is a synthetic agent that provides beneficial effects, not only by delaying the progression of OA, but also by preventing bone loss in a separate mouse model of osteoporosis.
Limitation: The observed effects on OA should be further examined using both female and male mice at different time points and dosages of Salubrinal.
Introduction
Osteoarthritis (OA) is the most common form of arthritis, resulting from multiple factors including ageing, traumatic injuries and abnormal gait biomechanics, as well as genetic and metabolic elements linked to obesity and inflammation.1-4 Approximately 630 million people are affected worldwide, but injured cartilage does not heal spontaneously. In many cases, cartilage defects are replaced by fibrous cartilage that exhibits significantly inferior mechanical properties.5-7 The progression of OA is represented by multiple detrimental events, starting with the death of chondrocytes, followed by the upregulation of proteolytic enzymes.8,9 Weight loss, low-impact exercise and the strengthening of muscles are generally recommended to help slow its progression. A common practice also includes administration of non-steroidal anti-inflammatory medicines, as well as injection of cortisone and hyaluronic acid.10 Surgical treatments might be an ultimate choice. However, it introduces the risk of infection and damage to surrounding structures.11,12
Pre-clinical and clinical studies have been conducted with naturally derived chemicals, synthetic agents, and biological molecules.13-17 In this study, we focused on Salubrinal (Tocris Bioscience, Bristol, United Kingdom, C21H17C13N4OS, 480 Da), a synthetic chemical, as a potential chondroprotective agent. Salubrinal has been shown to prevent bone loss by elevating the phosphorylation level of eukaryotic translation initiation factor 2 alpha (eIF2α).18 This elevation upregulates activating transcription factor 4 (ATF4), which is one of the key transcription factors in bone formation.19,20 Furthermore, an increase in eIF2α phosphorylation is reported to inhibit bone resorption by inactivating the nuclear factor of activated T-cells, cytoplasmic 1 (NFATc1).20,21 Because of Salubrinal’s dual beneficial role in protecting and rebuilding bone, an intriguing issue is its potential effect on cartilage. We have shown previously that Salubrinal downregulates expression and activity of matrix metalloproteinase 13 (MMP13) in C28/I2 chondrocytes.22 However, its efficacy in the treatment of OA needs to be examined.
Herein, we address a pair of questions using primary chondrocytes and a mouse model of post-traumatic OA: does Salubrinal chondroprotect the damaged articular cartilage? If so, what signalling pathway mediates its effect? Based on our previous study using C28/I2 chondrocytes, we focused on nuclear factor kappa B (NFκB) signalling and assayed MMP13 activity. We used Guanabenz (Tocris Bioscience) as a positive control as a regulator of eIF2α phosphorylation. We also evaluated the response to TNFα in primary and C28/I2 chondrocytes, and examined the efficacy of Salubrinal in a mouse model of OA using histology.23,24
Materials and Methods
Cell culture
Human primary chondrocytes (PC136121A1-C, Asterand Bioscience, Cambridge, Massachusetts) and human chondrocyte cell line, C28/I2, were cultured in DMEM/F12 and DMEM mediums, respectively, which were supplemented with 10% fetal bovine serum and antibiotics (Life Technologies, Grand Island, New York). Cells were maintained at 37°C and 5% CO2 in a humidified incubator. After ten hours of serum-free conditions, cells were incubated with 10 ng/ml TNFα (R& D Systems, Minneapolis, Minnesota) in the presence and absence of 5 µM Salubrinal or 5 µM Guanabenz (TOCRIS Bioscience, Ellisville, Missouri). One µM thapsigargin (Santa Cruz Biotechnology, Santa Cruz, California) was used as a positive control (PC) for phosphorylation of eIF2α.
A mouse model of OA and administration of Salubrinal or Guanabenz
OA was surgically induced in the left knees of 118 C57/BL6 female mice (approximately nine weeks old) by transecting the medial collateral ligament and removing the medial meniscus.23 Animal groups included age-matched sham control (CN), OA placebo, and OA treated with Salubrinal (OA + Sal). The sham surgery consisted of incision and suture. We also employed additional age-matched sham control and two OA groups treated with Guanabenz and its solvent (placebo). A total of three days after the induction of OA, Salubrinal (1.5 mg/kg) or Guanabenz (2.0 mg/kg) was administered daily into an intra-articular space, while their solvents (49.5% PEG 400 and 0.5% Tween 80 in PBS for Salubrinal; and distilled water including 5% glucose for Guanabenz) were used in the placebo groups. Mice were anaesthetised, after which injection was conducted to the intercondylar fossa from the patellar tendon in a sagittal plane to avoid potential damage to the load-bearing cartilage surface.
Western blot analysis
Human primary chondrocytes (15 minutes after addition of TNFα) and tibia cartilage (three weeks after the induction of OA) were lysed in a radioimmunoprecipitation assay buffer.22 We chose a tibia sample as they were able to be harvested with fewer potential contaminations with subchondral bone or bone marrow than femur samples. Isolated proteins were gel-fractionated and electro-transferred to Immobilon-P membranes (Millipore, Billerica, Massachusetts). The antibodies used were phosphorylated NFκB p65, NFκB p65 (Cell Signaling, Beverly, Masachusetts) and β-actin (Sigma, St Louis, Missouri). Images were taken with a luminescent image analyser (LAS-3000, Fuji Film, Tokyo, Japan), and signal intensities were quantified with Image J software (National Institute of Health, Bethesda, Maryland). Data were presented with reference to control intensities of β-actin.
Safranin O staining
Knee samples were decalcified in 10% ethylenediaminetetraacetic acid (EDTA) for two weeks, embedded in paraffin and sectioned at 4 µm thickness. After deparaffinisation and rehydration, slides were stained with Weigert’s iron haematoxyline solution for five minutes. They were differentiated in 1% acid–alcohol, and stained with 0.02% fast green solution. They were then rinsed in 1% acetic acid, stained in 1% Safranin O solution for 30 minutes and treated with graded ethyl alcohol and xylene.25
Histological score for symptoms of osteoarthritis
Tissue sections (approximately 50 sections per mouse) were graded using the scoring system described by Glasson et al.24 Because of the specific procedure taken for OA induction, we focused on the histological evaluation of the medial side that exhibited more severe symptoms than the lateral side. Accordingly, the grade was assigned by two independent scorers blinded to treatment allocation (KH, AN) as follows: “0” = normal; “0.5” = loss of Safranin O without structural changes; “1” = small fibrillations without loss of cartilage; “2” = vertical clefts down to the layer immediately below the superficial layer and some loss of surface lamina; and “3” to “6” = vertical clefts/erosion to the calcified cartilage extending to < 25%, 25% to 50%, 50% to 75%, and > 75% of the articular surface, respectively.
Determination of thickness of subchondral bone and synovial score
To evaluate the effects of OA induction on subchondral bone, its average thickness was determined using the procedure described previously.26 In brief, the area of subchondral bone was measured using Image J software. The average thickness was then determined as a ratio of subchondral bone area to its weight-bearing width. We also determined synovial scores for evaluating inflammation of the synovium using the procedure described previously.27
MMP13 activity
Proteins were isolated from primary chondrocytes or tibial cartilage samples (three weeks after the induction of OA) and lysed in a radioimmunoprecipitation assay buffer. MMP13 activity was analysed with a SensoLyte 520 MMP-13 assay kit (AnaSpec, Fremont, California) according to the manufacturer’s instruction. In brief, the lysates were incubated with APMA at 37°C for 40 minutes. The mixtures were then combined with MMP13 substrate solutions and incubated at 37°C for 30 minutes. Fluorescence intensity for MMP13 activity was determined at 485 nm (excitation) and 528 nm (emission).
Statistical analysis
For in vitro experiments, three or four independent experiments were conducted and the Student’s t-test was employed. For the evaluation of histological scores, thickness of subchondral bone, and synovial scores, non-parametric statistical analysis (Kruskal–Wallis test and Mann–Whitney U test) was conducted. For the interpretation of in vivo protein samples, one-way analysis of variance followed by Dunnett’s post hoc test, was conducted. Data were expressed as mean and standard deviation (sd), and statistical significance was evaluated at p < 0.05. The single and double asterisks indicate p < 0.05 and p < 0.01, respectively.
Results
In vitro suppression of TNFα-induced NFκB phosphorylation and MMP13 activity by Salubrinal
In response to 10 ng/ml of TNFα, primary chondrocytes (PC136121A1-C) elevated the level of phosphorylated NFκB (p-NFκB) without altering the total level of NFκB (Fig. 1a) elevated the level of phosphorylated NFκB (p-NFκB) without altering the total level of NFκB (Fig. 1a) without altering the total level of NFκB (Fig. 1a). Their incubation with TNFα also increased MMP13 activity (Fig. 1b). However, simultaneous application of 5 µM of Salubrinal with TNFα significantly reduced the level of p-NFκB as well as MMP13 activity (Figs 1a and 1b). Although both Salubrinal and Guanabenz elevate the phosphorylation level of eIF2α, Guanabenz did not alter the level of p-NFκB (Fig. 1c). Although both Salubrinal and Guanabenz elevate the phosphorylation level of eIF2α, Guanabenz did not alter the level of p-NFκB (Fig. 1c) or MMP13 activity (Fig. 1d).
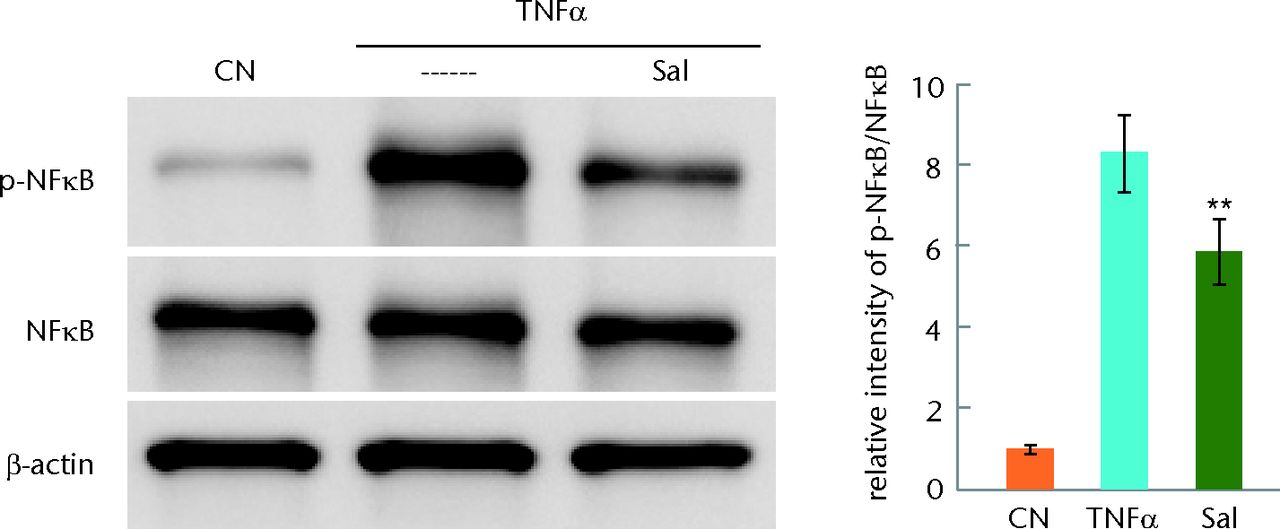
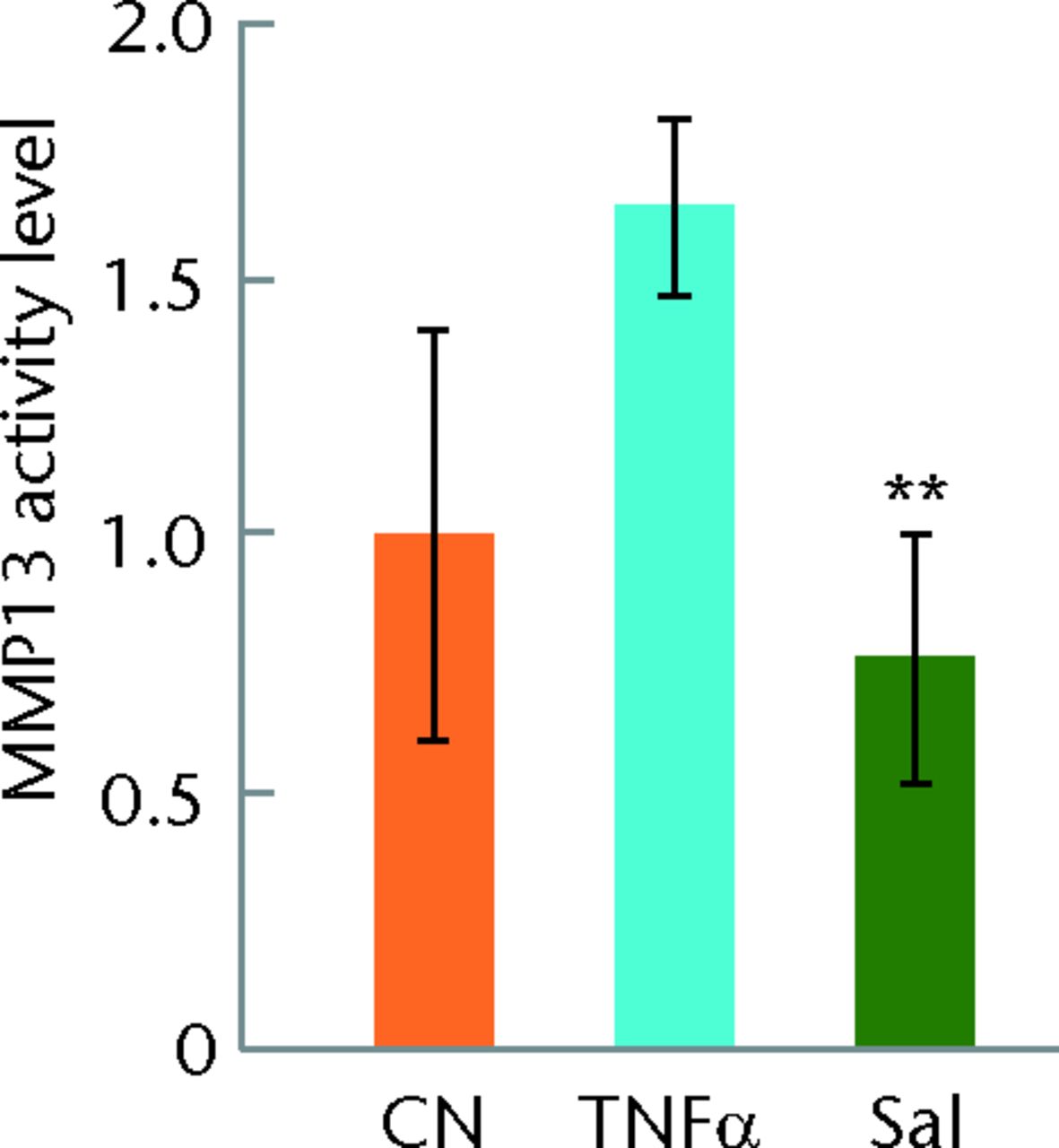
Figs. 1a - 1d
Graphs and staining showing the response of human primary chondrocytes to tumour necrosis factor alpha (TNFα) in the presence and absence of Salubrinal (Sal) or Guanabenz (Gu), with a) activation of nuclear factor kappa B (NFκB) by TNFα for 15 minutes and partial deactivation by Salubrinal, b) matrix metalloproteinase (MMP)13 activity induced by TNFα and suppressed by 5 µM Salubrinal, c) no detectable effect of Guanabenz on the level of p-NFκB and d) no detectable change of MMP13 activity by Guanabenz shown. CN, vehicle.
Reduced cartilage degradation by Salubrinal into the intra-articular space
In the mouse model of osteoarthritis, the sagittal sections stained with Safranin O indicated degradation of articular cartilage on the tibial and femoral surfaces in the knee joint (Fig. 2). The intensity of Safranin O staining decreased in the samples harvested three and six weeks after the induction of OA. However, daily administration of Salubrinal at a dose of 1.5 mg/kg from three days after the induction of OA partially restored Safranin O staining.
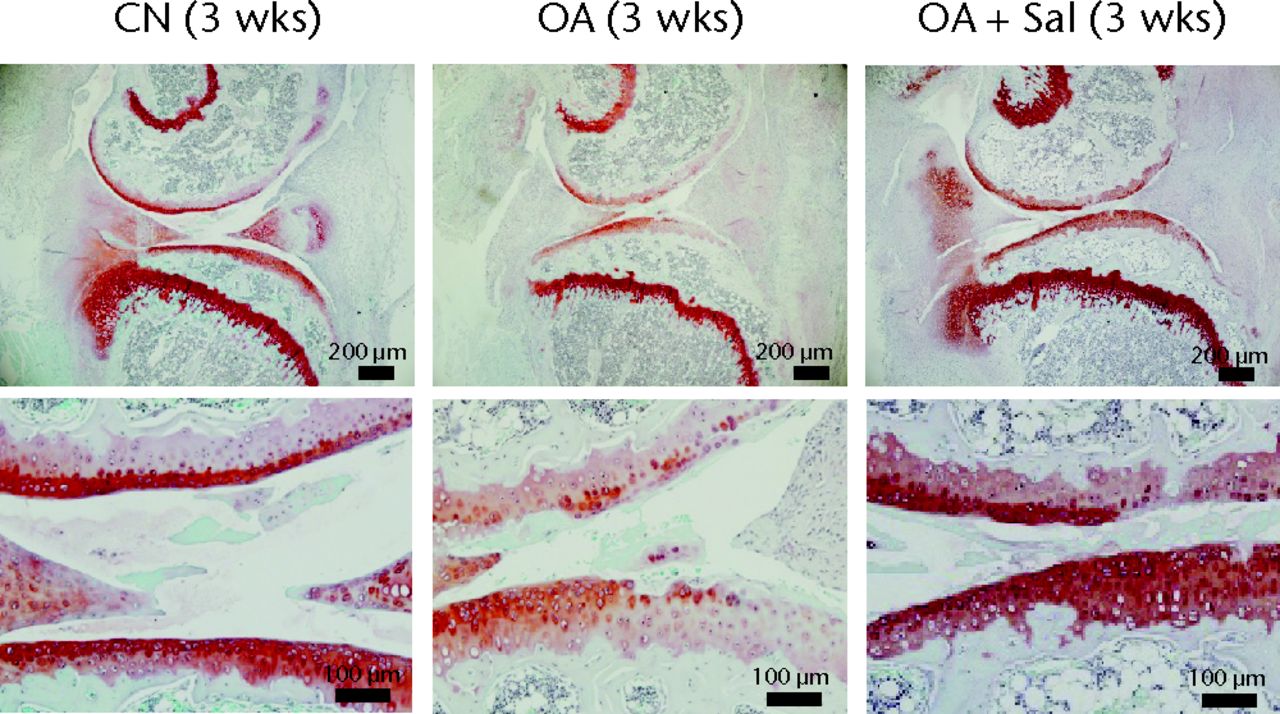
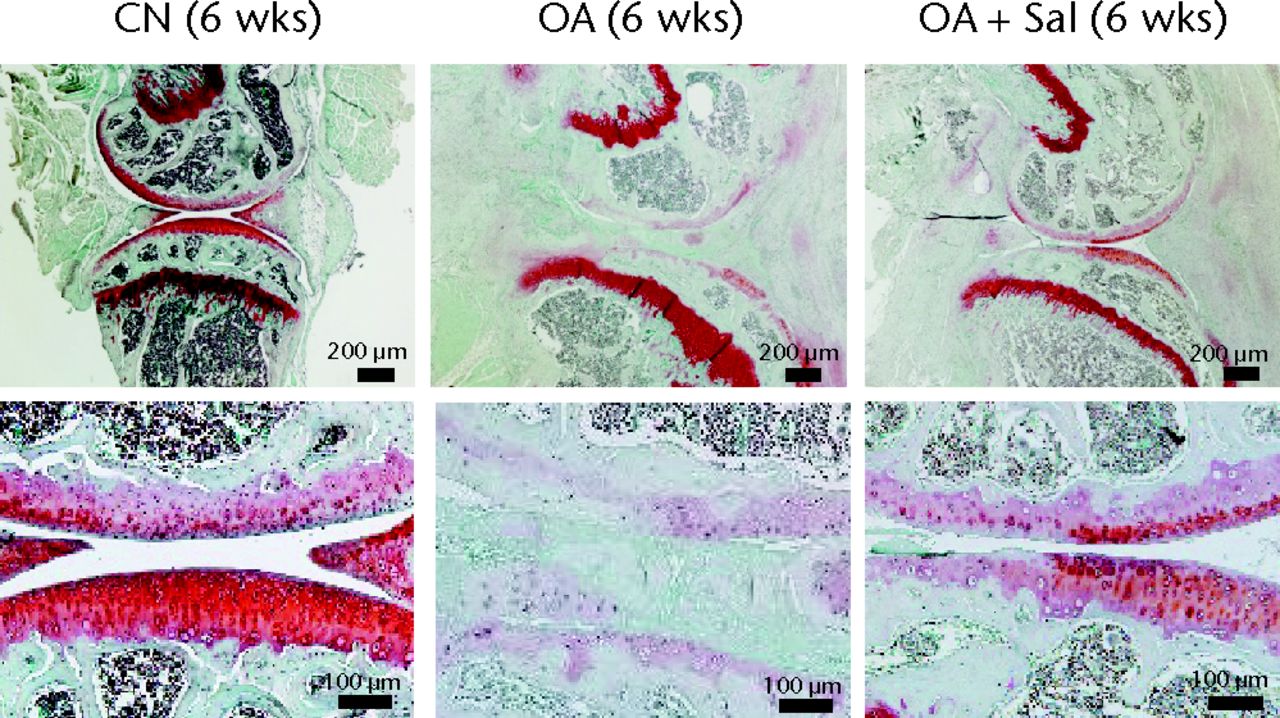
Figs. 2a - 2b
Images of safranin O staining of the sagittal knee joint section, with a) samples three weeks after induction of osteoarthritis (OA, placebo sample; OA + Sal, Salubrinal-treated OA sample; CN, sham control sample) and b) samples six weeks after induction of OA shown. The three panels in the top row show an entire knee section (bar = 200 µm), while the three panels in the bottom row depict their enlarged images (bar = 100 µm). The top section in each panel is the femur, and the bottom section is the tibia.
The histological score (0 for normal, and 6 for worst OA) revealed that Salubrinal significantly reduced OA-linked tissue degeneration (Fig. 3) revealed that Salubrinal significantly reduced OA-linked tissue degeneration (Fig. 3). In week three samples, the histological mean scores for the medial femoral condyle (MFC) were 0.8, sd 0.3 (control; CN), 3.8, sd 1.2 (OA placebo; OA), and 2.5, sd 0.5 (OA Salubrinal; OA + Sal) (CN vs OA, p < 0.01; and OA vs OA + Sal, p = 0.045), while the scores for the medial tibial plateau (MTP) were 0.3, sd 0.5 (CN), 2.8, sd 1.0 (OA), and 2.2, sd 0.8 (OA + Sal) (CN vs OA, p < 0.01; and OA vs OA + Sal, p = 0.530). In week six samples, the scores for MFC were 0.6, sd 0.2 (CN), 5.1, sd 0.8 (OA), and 4.0, sd 1.9 (OA + Sal) (CN vs OA, p < 0.01; and OA vs OA + Sal, p = 0.163), while the scores for MTP were 0.6, sd 0.4 (CN), 5.3, sd 0.7 (OA), and 3.7, sd 1.8 (OA + Sal) (CN vs OA, p < 0.01; and OA vs OA + Sal, p = 0.027).
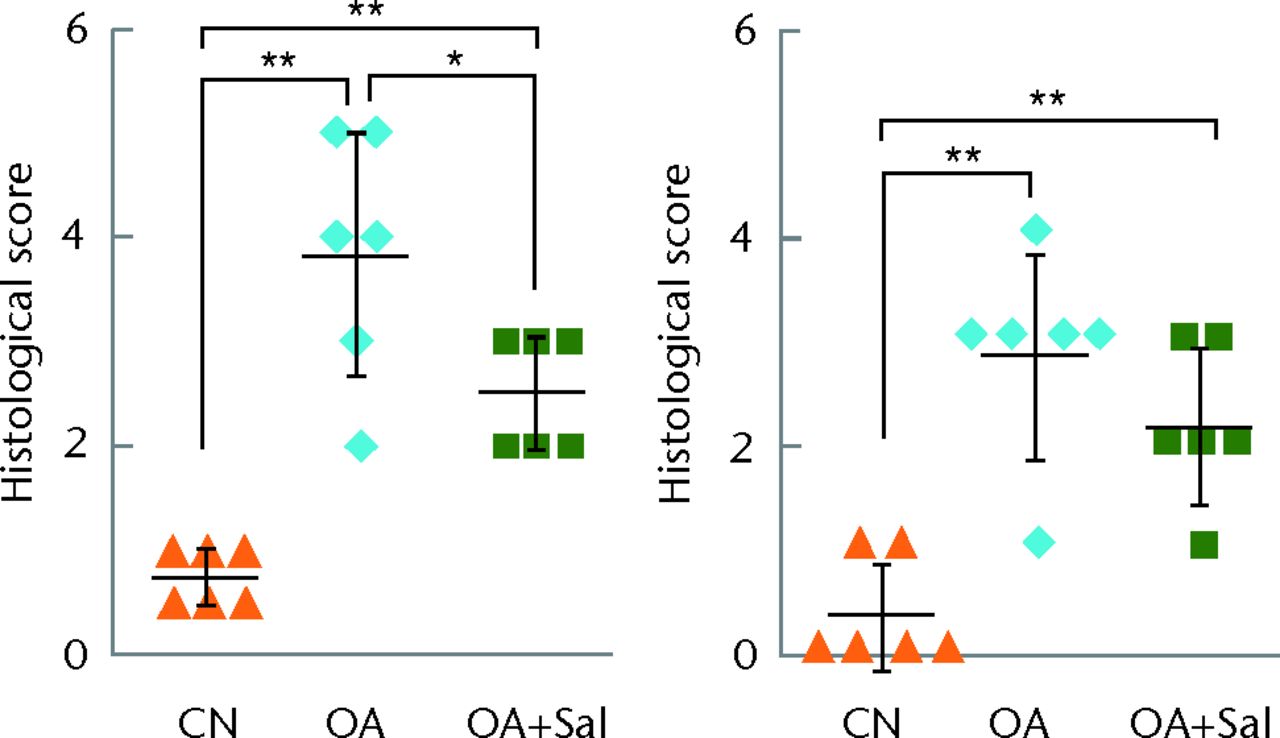
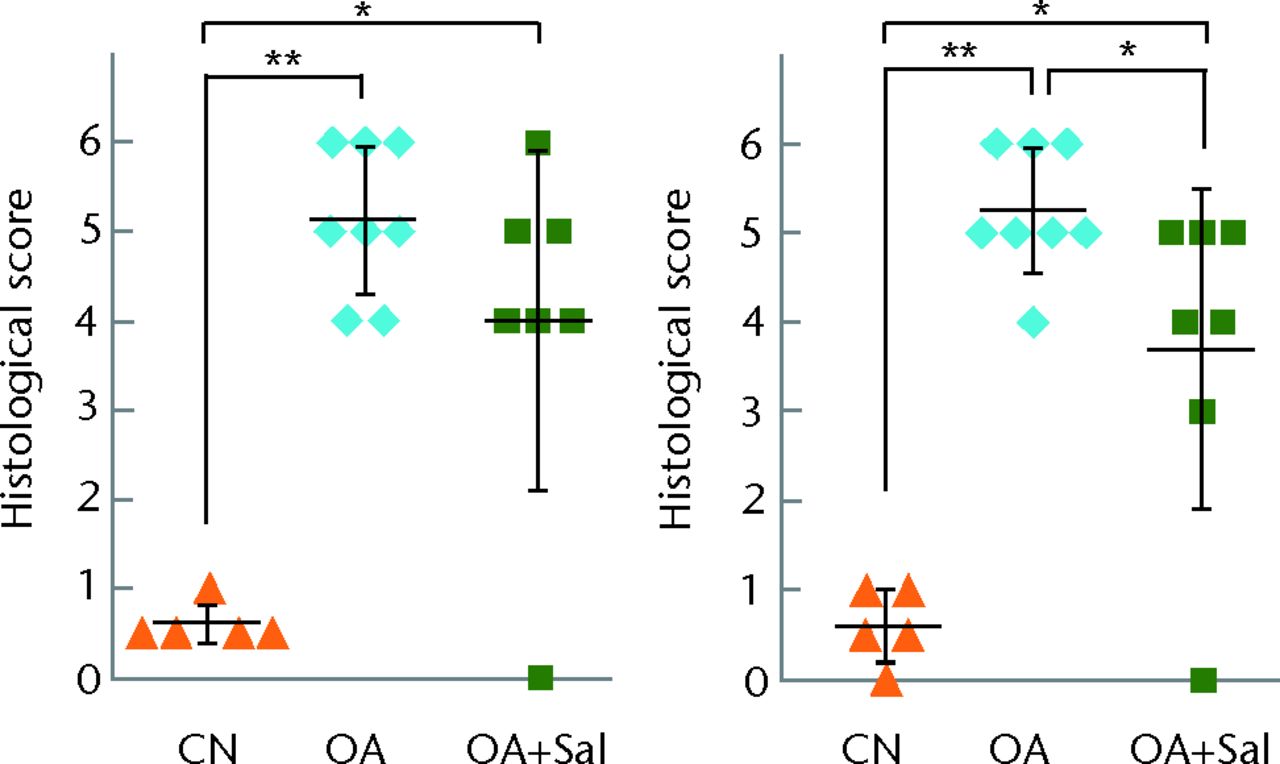
Figs. 3a - 3b
Graphs showing histological scores for progression of osteoarthritis (OA), for a) medial femoral condyle (MFC) (left) and medial tibial plateau (MTP) (right) three-week samples (n = 6) and b) for MFC (left) and MTP (right) six-week samples (n = 5 sham control, CN, 8 OA + placebo, and 7 OA + Salubrinal (Sal)) are shown; *p < 0.05; **p < 0.01.
Increased subchondral bone formation and marginal osteophyte development are part of the joint pathology in OA. In the mouse model of OA in this study, the thickness of subchondral bone was not altered in week three samples, but it was significantly increased in MFC and MTP in week six samples (Fig. 4a). Administration of Salubrinal did not alter the thickness of MFC and MTP at either time points. Regarding synovial inflammation, induction of OA worsened the synovial score in week three and week six samples (Fig. 4b). Salubrinal reduced the score in both samples, although statistically significant reduction was observed only in week three samples.
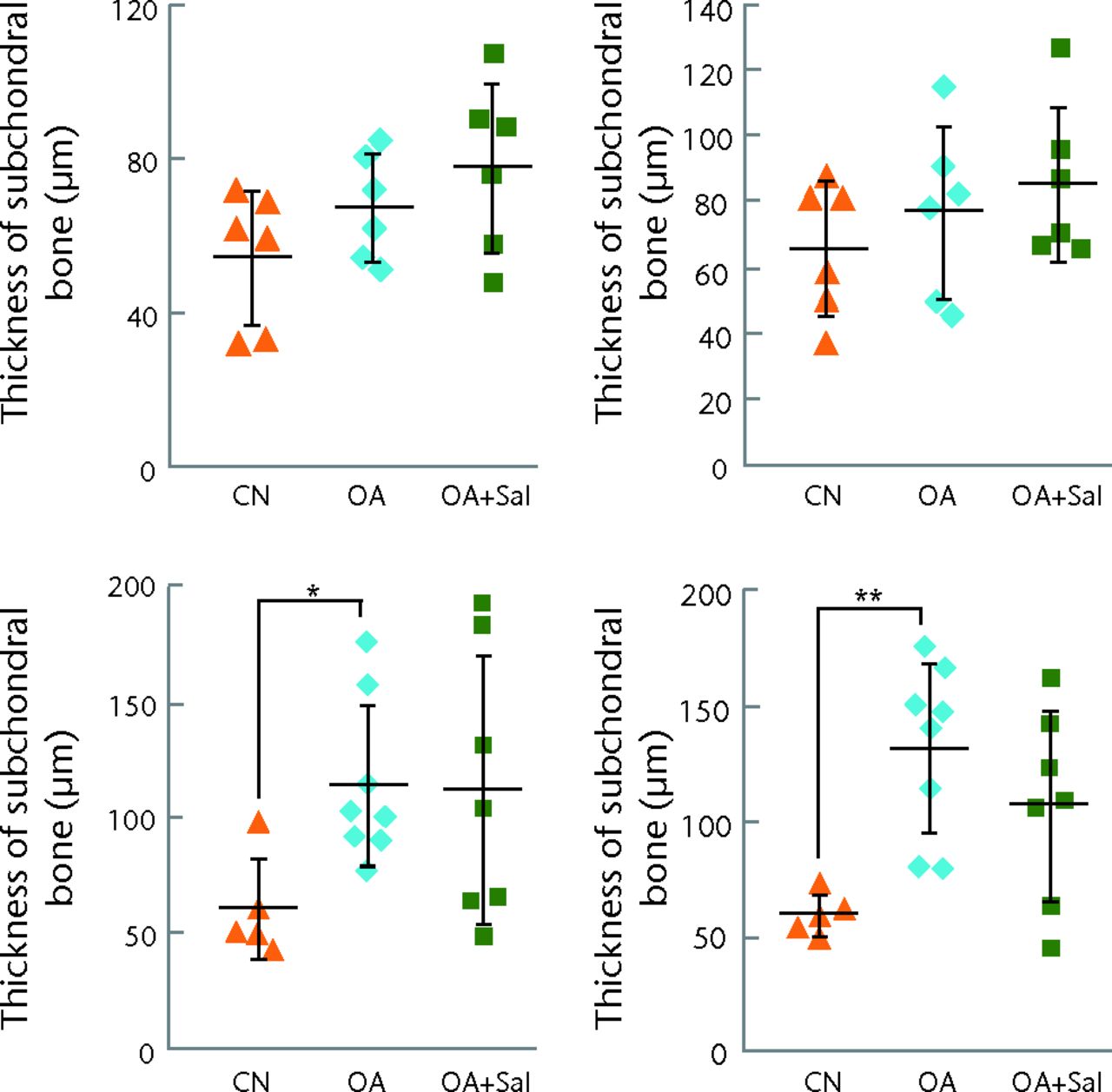
Figs. 4a - 4b
Graphs showing the effects of Salubrinal on subchondral bone and synovium, with a) thickness of subchondral bone in the medial femoral condyle (MFC) (left) and medial tibial plateau (MTP) (right) (three weeks top row, six weeks bottom row) and b) synovial score for three-week (left) and six-week (right) samples. *p < 0.05; **p < 0.01.
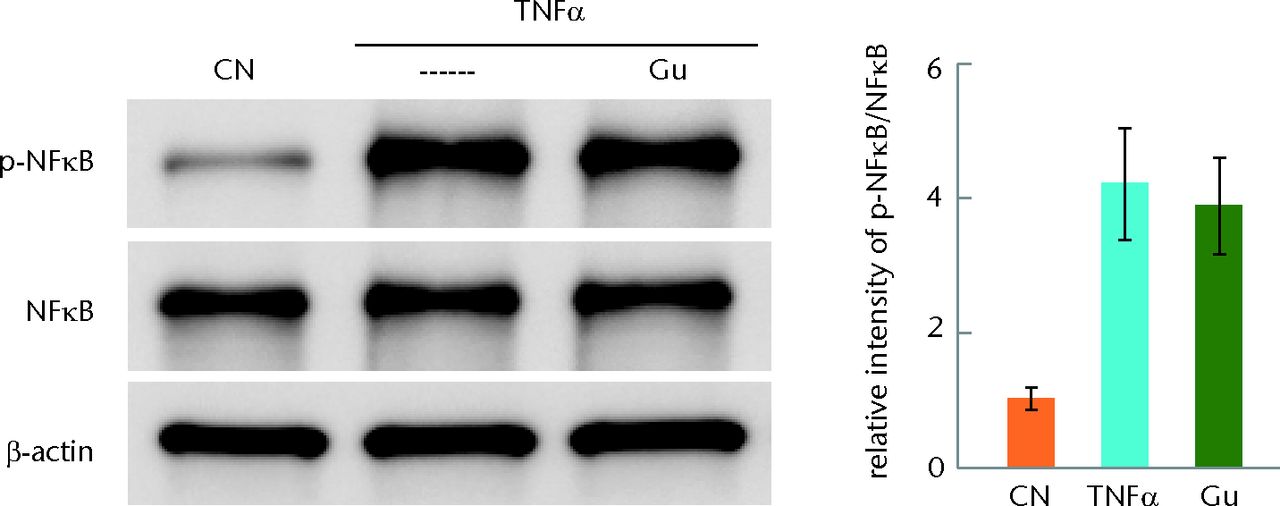
In vivo suppression of OA-induced NFκB phosphorylation and MMP13 activity by Salubrinal
Protein samples harvested from the tibial cartilage, showed upregulation of p-NFκB as well as MMP13 activity compared with the age-matched sham control (Fig. 5). Consistent with the in vitro result, daily administration of Salubrinal significantly reduced p-NFκB (p-NFκB/β-actin CN vs OA, p = 0.001; OA vs OA + Sal, p = 0.023; and p-NFκB/NFκB CN vs OA, p = 0.285; OA vs OA + Sal, p = 0.042) as well as MMP13 activity (CN vs OA, p < 0.001; and OA vs OA + Sal, p < 0.001). Of note, TNFα in the in vitro assay did not alter the level of total NFκB, however, OA protein samples presented an elevated level of NFκB. We also evaluated the levels of p-eIF2α in the mouse cartilage samples as well as C28/I2 chondrocytes, in which 1 µM thapsigargin was employed as a positive control (PC) of elevation of p-eIF2α. In the cartilage samples, the significant elevation of p-eIF2α was not detected (Fig. 6a) of elevation of p-eIF2α. In the cartilage samples, the significant elevation of p-eIF2α was not detected (Fig. 6a). In vitro chondrocyte samples did not also present statistically significant elevation of p-eIF2α in response to TNFα with and without 5 µM Salubrinal (Fig. 6b). Collectively, the result showed that Salubrinal-driven suppression of p-NFκB was not directly linked to the regulation of p-eIF2α.
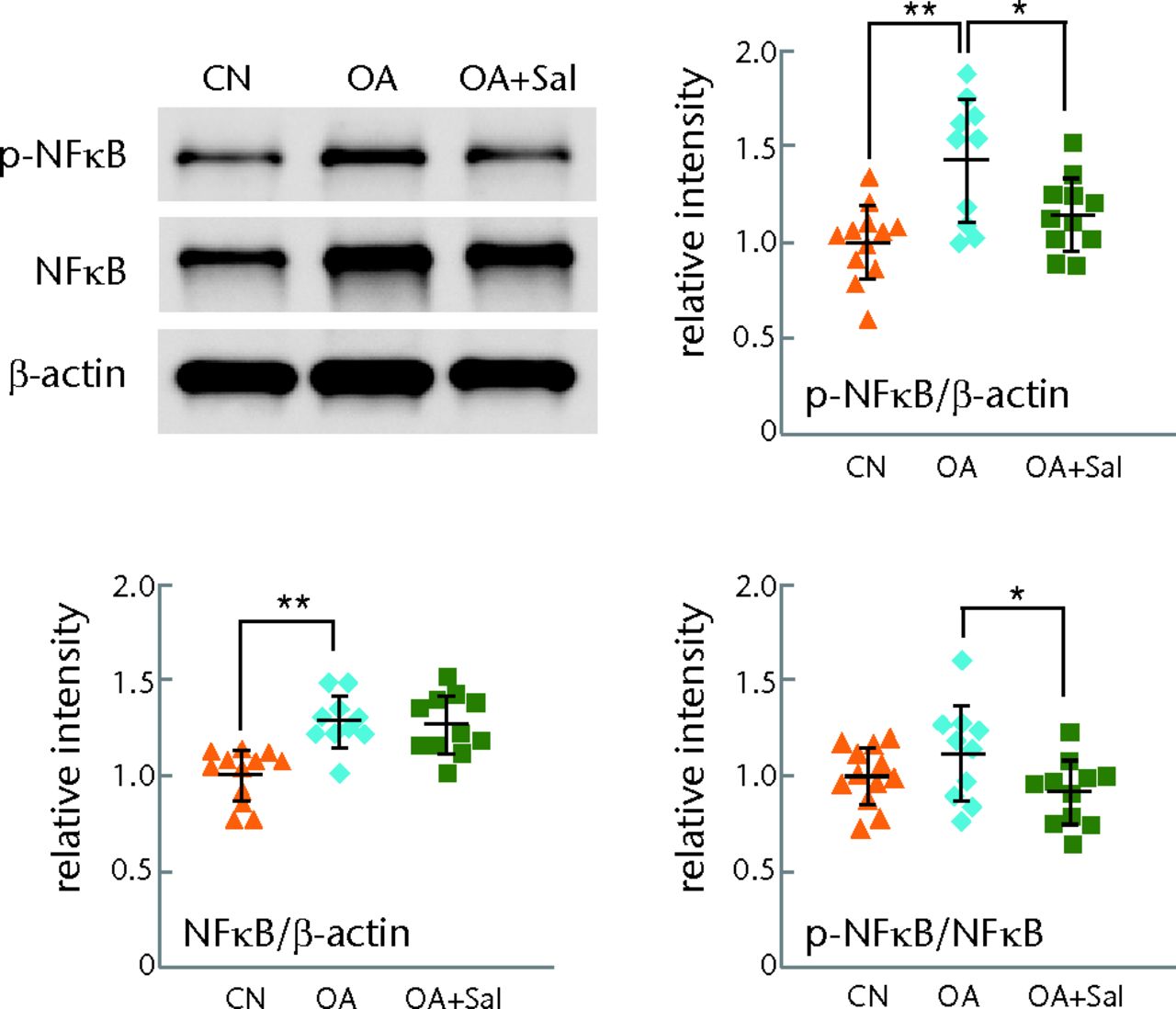
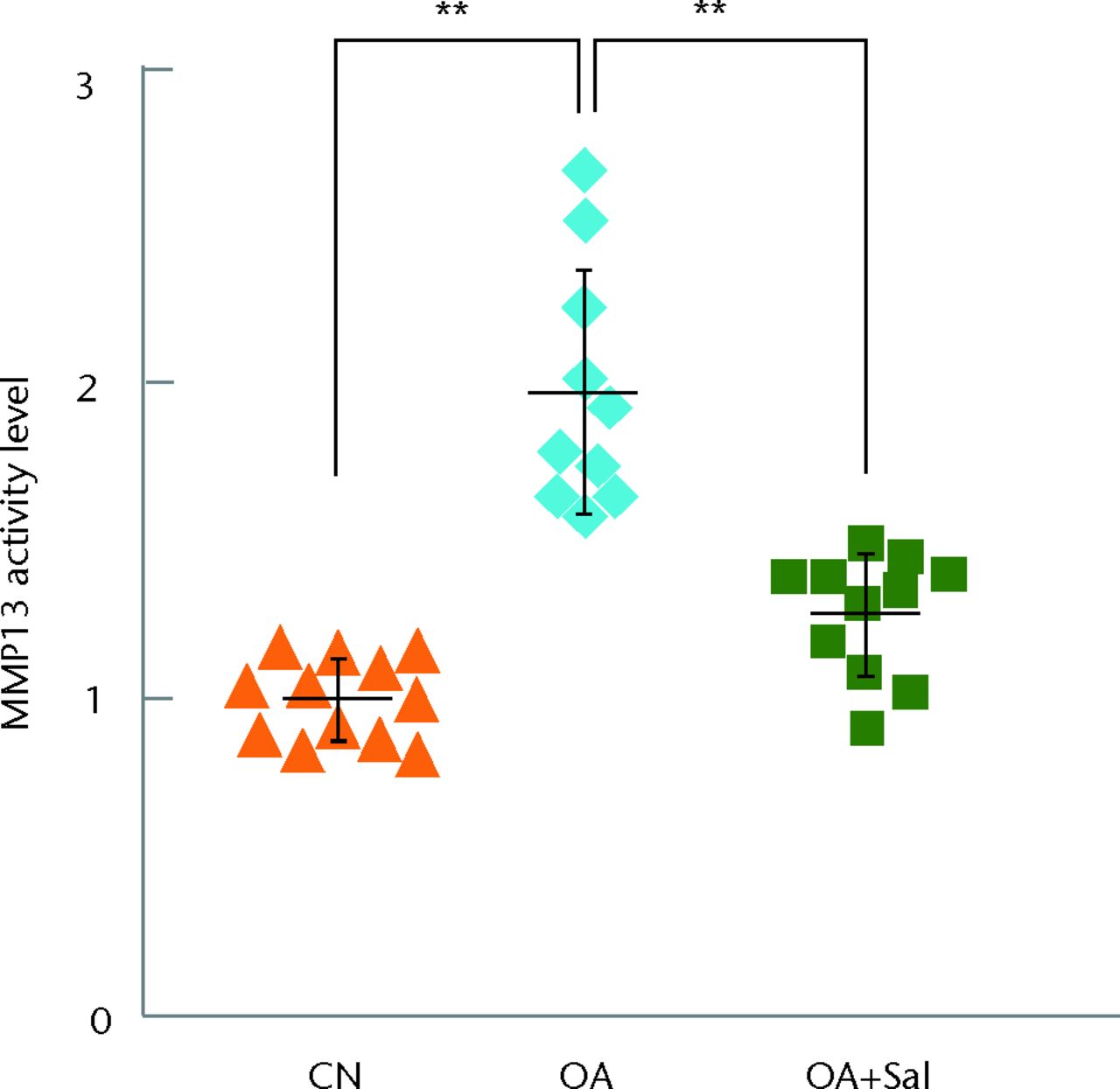
Figs. 5a - 5b
Graphs showing suppression of p-nuclear factor kappa B (p-NFκB) p65 and activity of matrix metalloproteinase 13 (MMP13) by Salubrinal in a mouse model of osteoarthritis; (n = 12 CN, sham control, 10 OA placebo, and 11 OA + Salubrinal (Sal)), with a) attenuation of the level of p-NFκB p65 by Sal and b) suppression of activity of MMP13 by Sal shown.
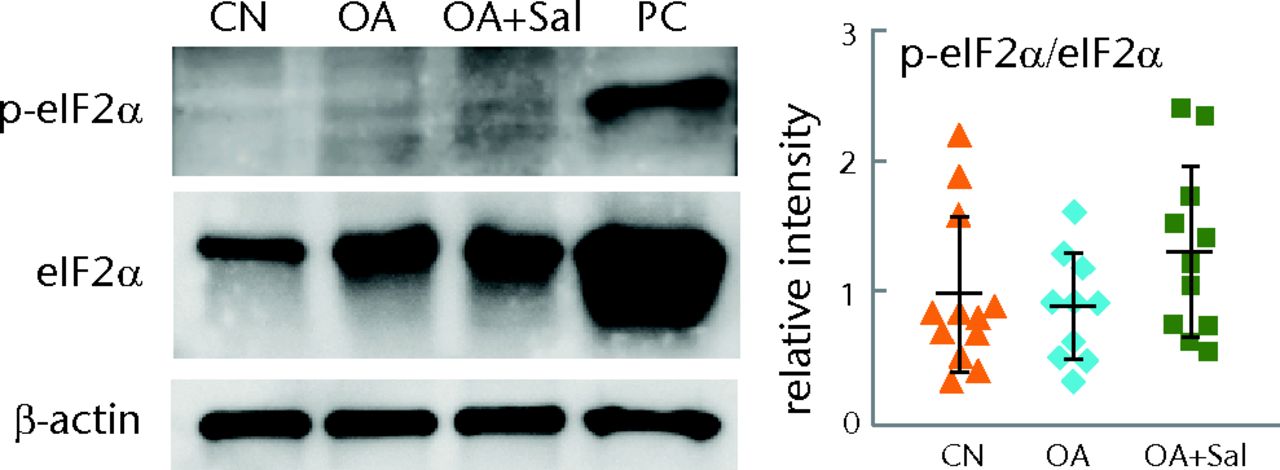
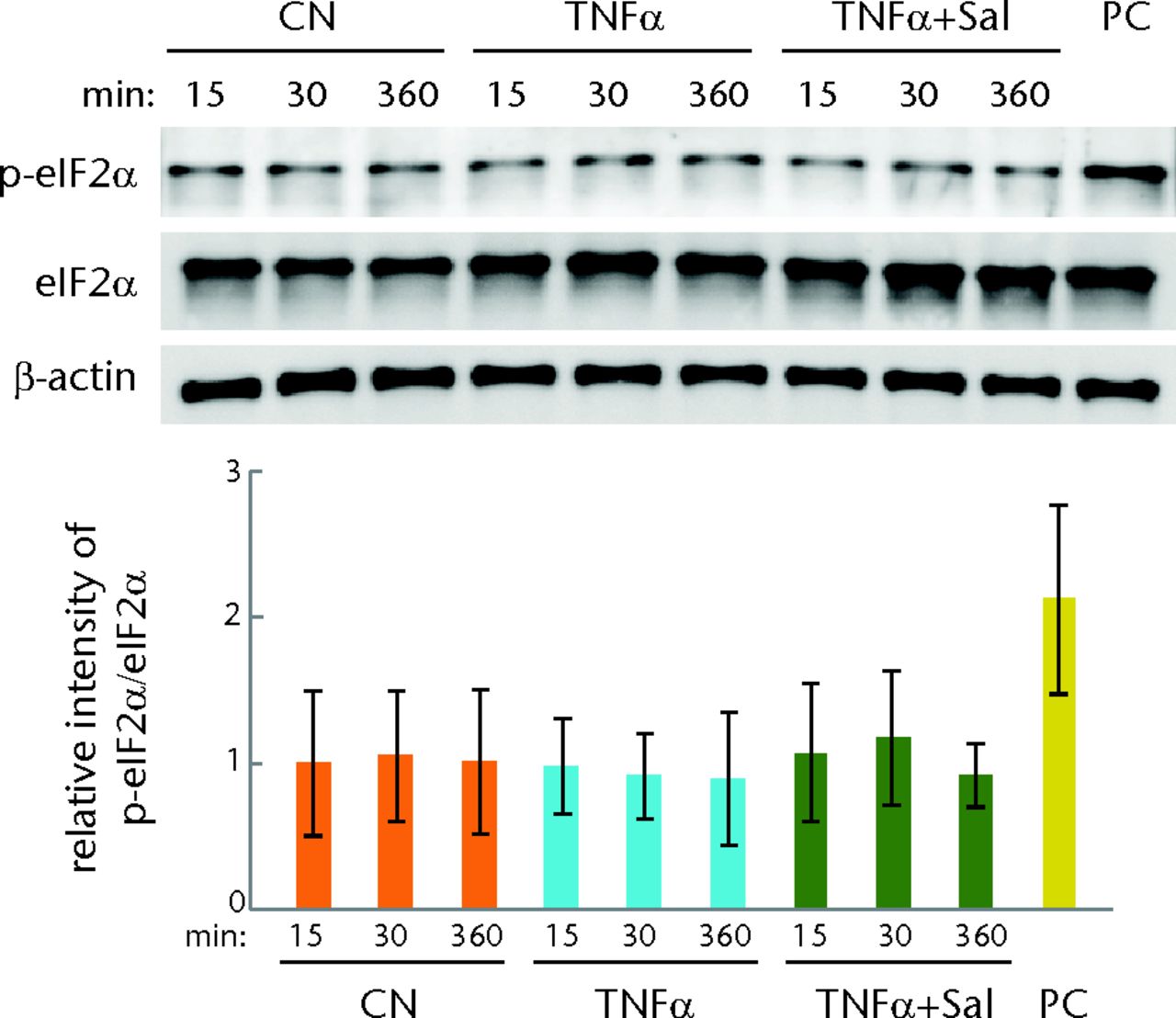
Figs. 6a - 6b
Graphs and staining showing evaluation of the phosphorylation level of eukaryotic translation initiation factor 2 alpha (eIF2α) in cartilage samples and C28/I2 chondrocytes, with a) levels of p-eIF2α in tibial cartilage samples (three weeks after the induction of osteoarthritis; OA); (n = 12 CN, sham control, 10 OA placebo, and 11 OA + Salubrinal (Sal)) and b) levels of p-eIF2α in C28/I2 chondrocytes treated with TNFα in the presence and absence of 5 µM Salubrinal for 15, 30, and 360 minutes shown. Thapsigargin at 1 µM was used as a positive control (PC) for p-eIF2α.
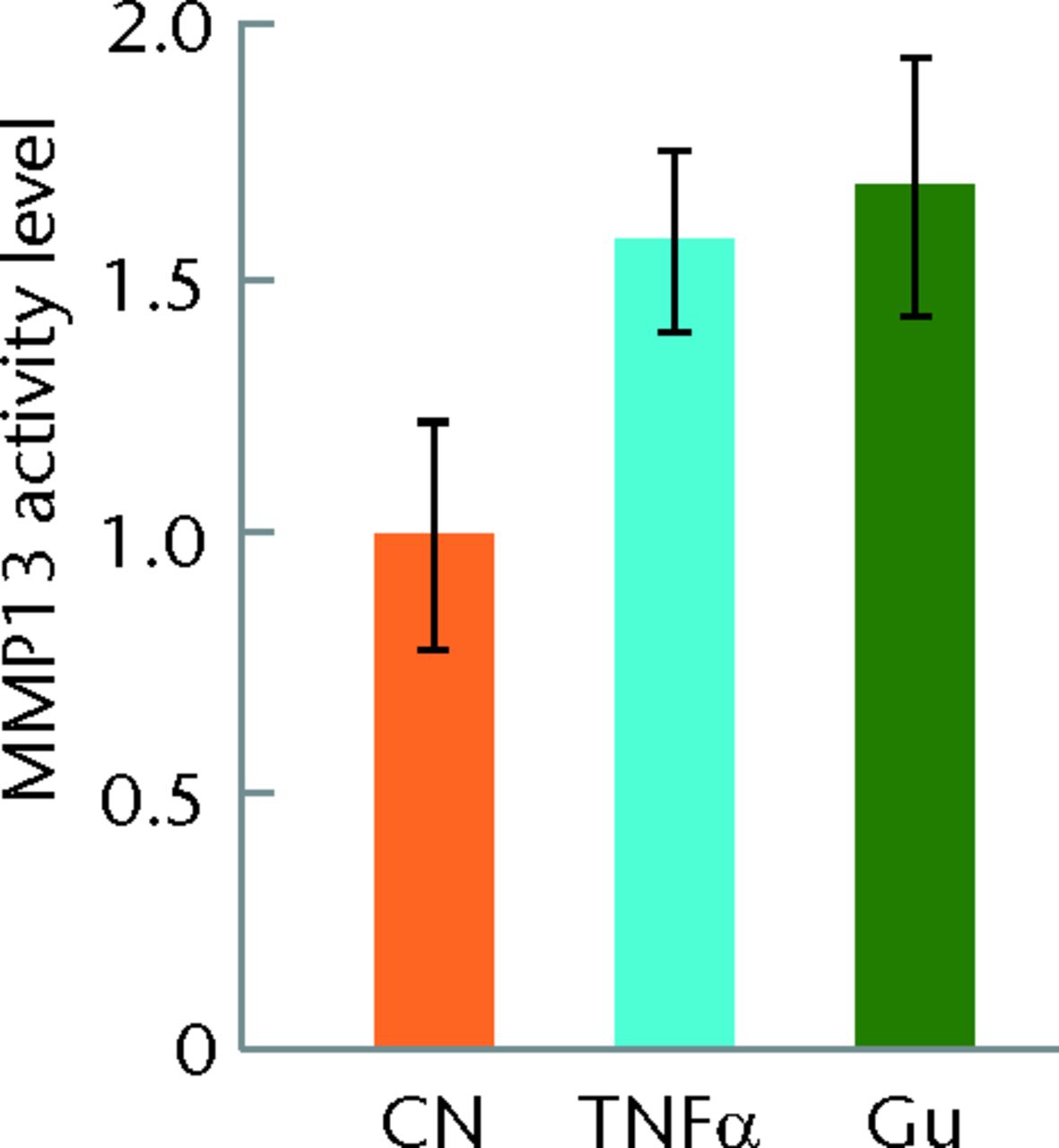
No suppressive effects to OA progression with Guanabenz
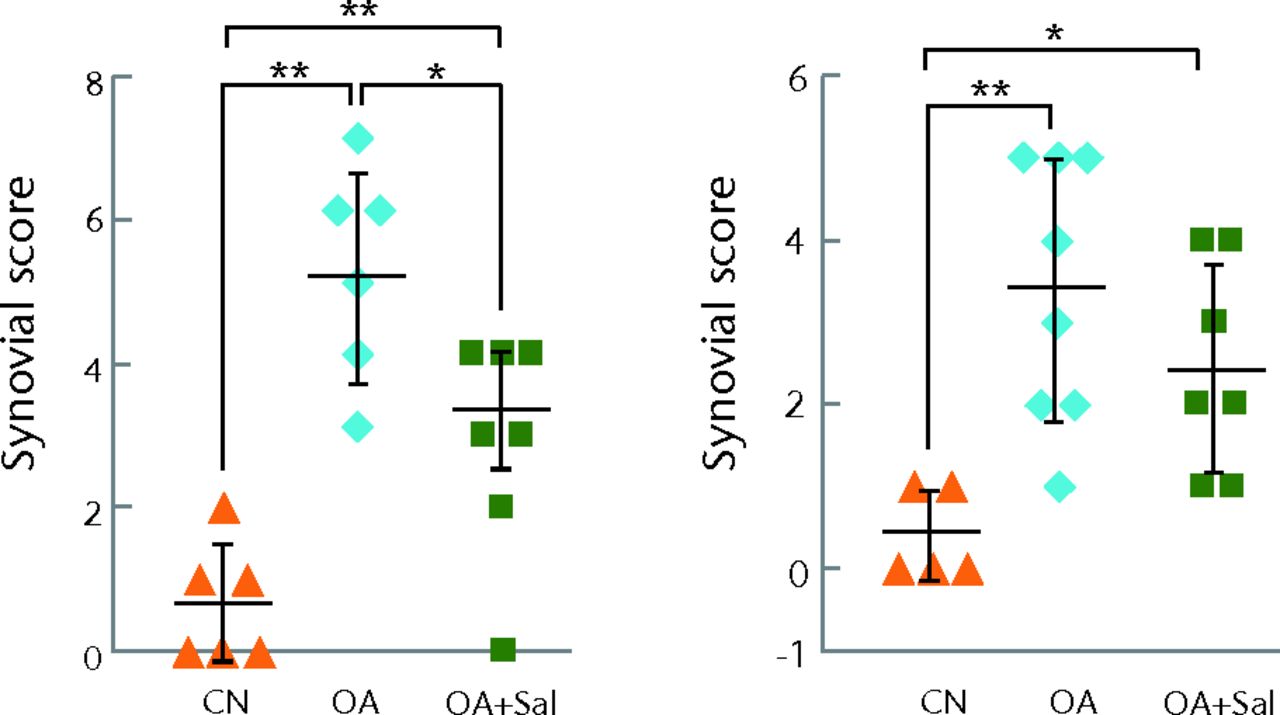
In response to Guanabenz, the progression of OA was not detectably changed in the femur (MFC) and the tibia (MTP) both in week three and week six samples (Fig. 7) and the tibia (MTP) both in week three and week six samples (Fig. 7) both in week three and week six samples (Fig. 7). In week six samples, for example, the histological score for MFC was 0.8, sd 0.3 (CN), 5.1, sd 0.8 (OA), and 5.2, sd 0.7 (OA + Gu) (CN vs OA, p < 0.01; and OA vs OA + Gu, p = 0.772), while the score for MTP was 0.6, sd 0.4 (CN), 4.8, sd 0.7 (OA), and 4.7, sd 0.5 (OA + Gu) (CN vs OA, p < 0.01; and OA vs OA + Gu, p = 0.758). Compared with the OA control samples, administration of Guanabenz did not alter the thickness of subchondral bone of MFC and MTP at either time points (Fig. 8a) (CN vs OA, p < 0.01; and OA vs OA + Gu, p = 0.758). Compared with the OA control samples, administration of Guanabenz did not alter the thickness of subchondral bone of MFC and MTP at either time points (Fig. 8a). Compared with the OA control samples, administration of Guanabenz did not alter the thickness of subchondral bone of MFC and MTP at either time points (Fig. 8a). Unlike Salubrinal, which significantly reduced the synovial score in week three samples, Guanabenz did not change the synovial score both in week three and week six samples (Fig. 8b).
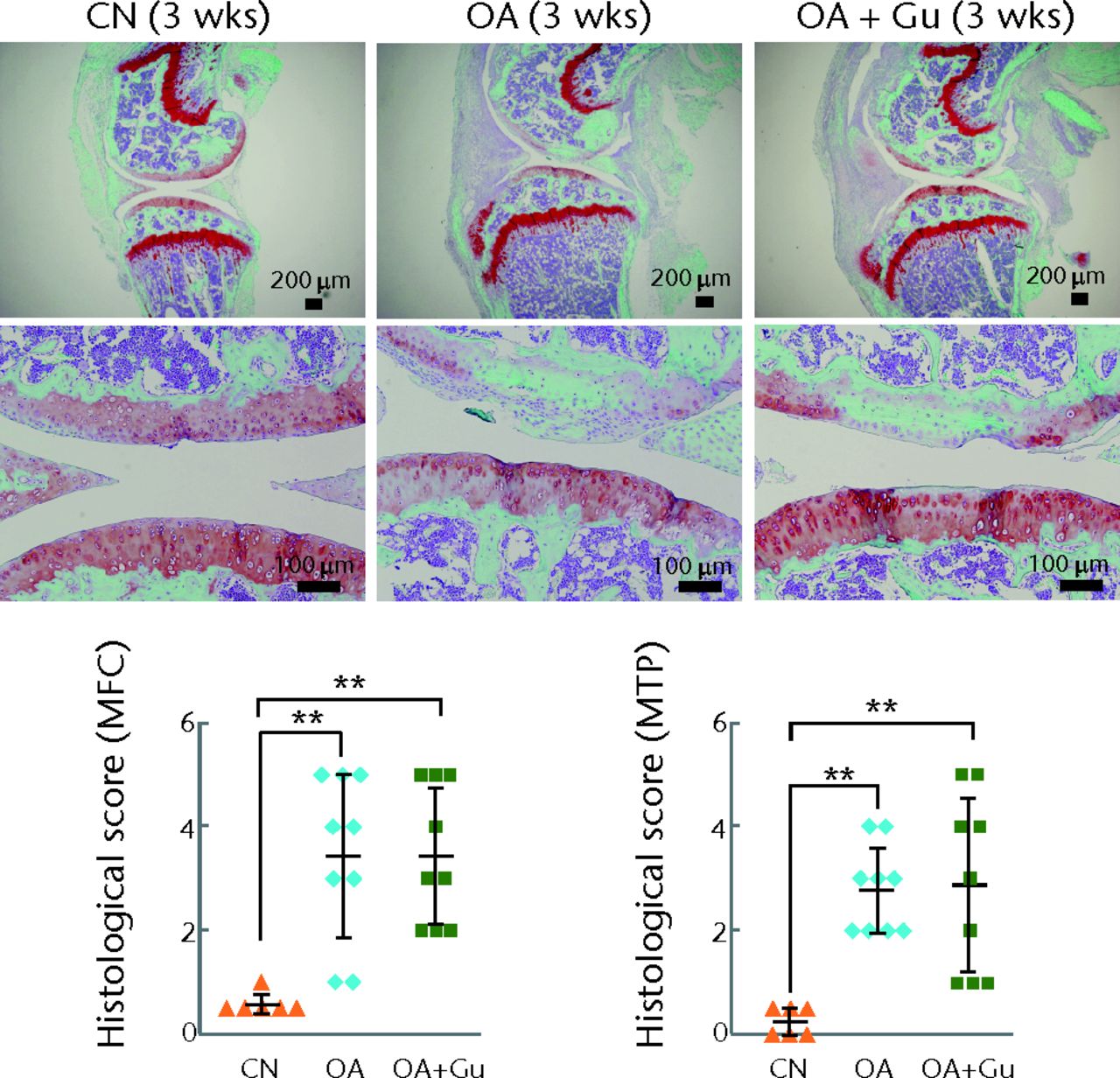
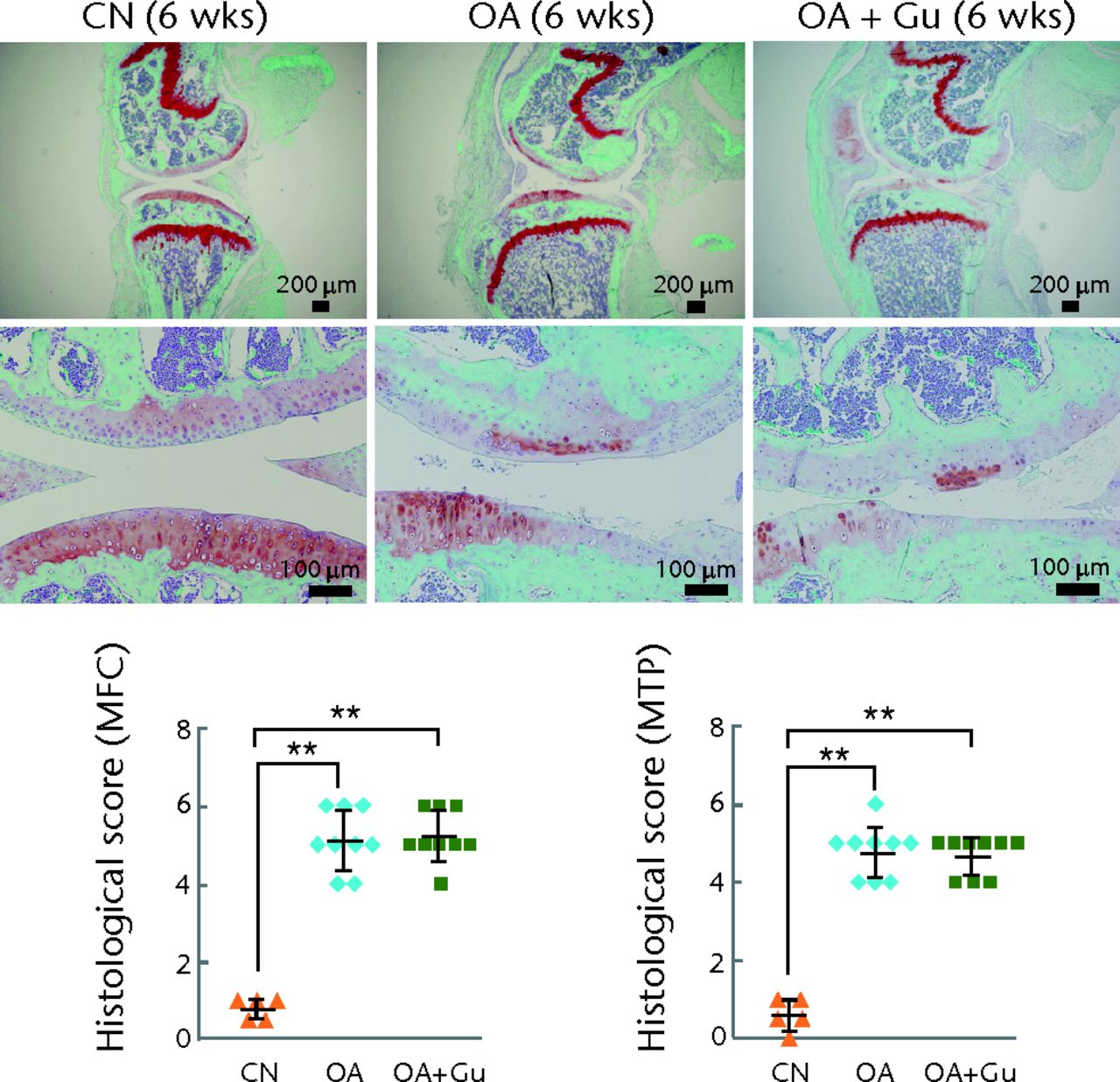
Figs. 7a - 7b
Histological images and graphs showing no significant prevention of the progression of osteoarthritis (OA) by Guanabenz (Gu). Safranin O staining of the sagittal knee joint section and histological scores, with a) samples three weeks after induction of OA; (n = 6 CN, control sham, 9 OA placebo and OA + Gu) and b) samples six weeks after induction of OA; (n = 5 CN, and 9 OA, and OA + Gu) shown. OA, OA placebo sample; OA + Gu-treated OA sample.
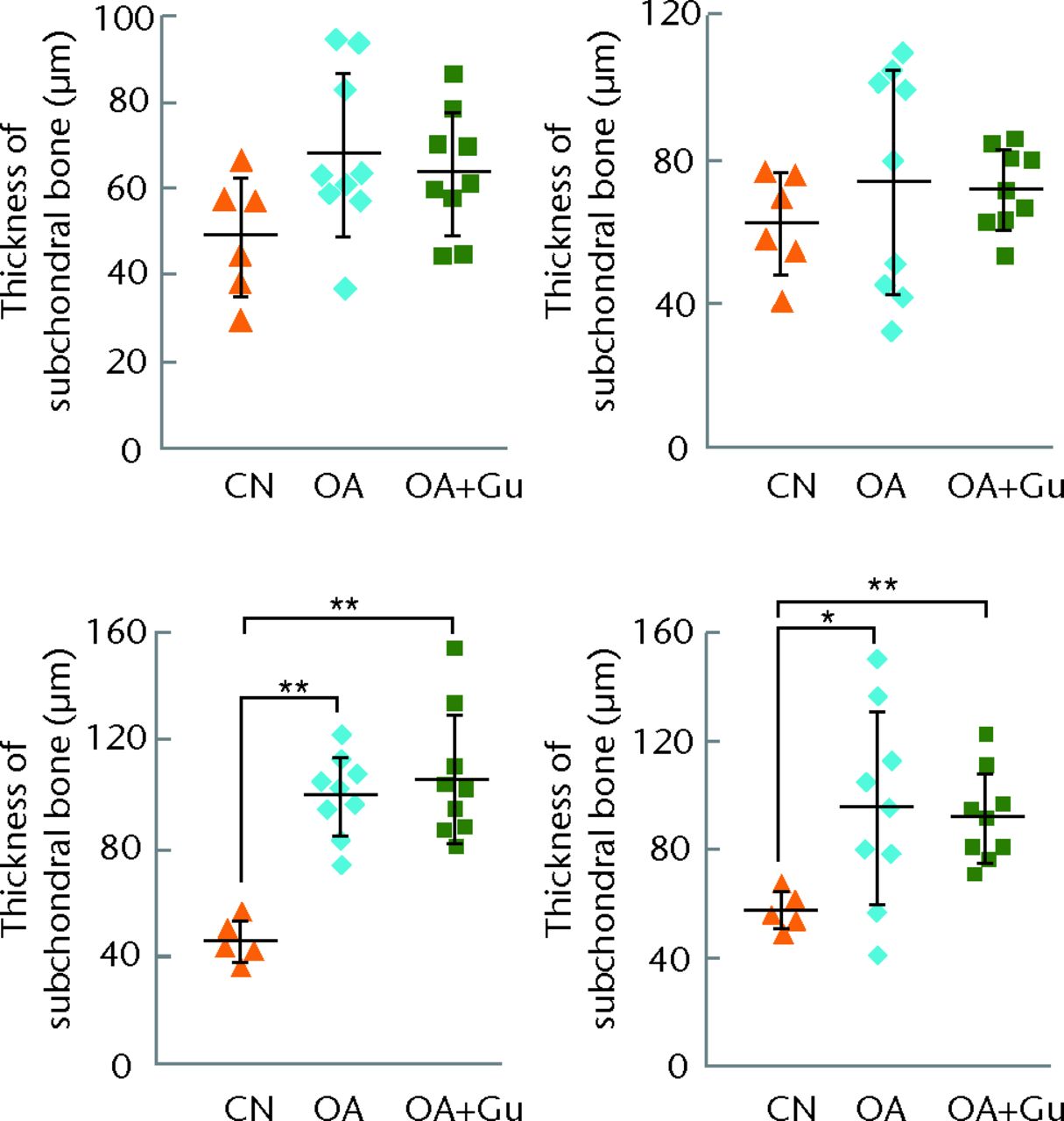
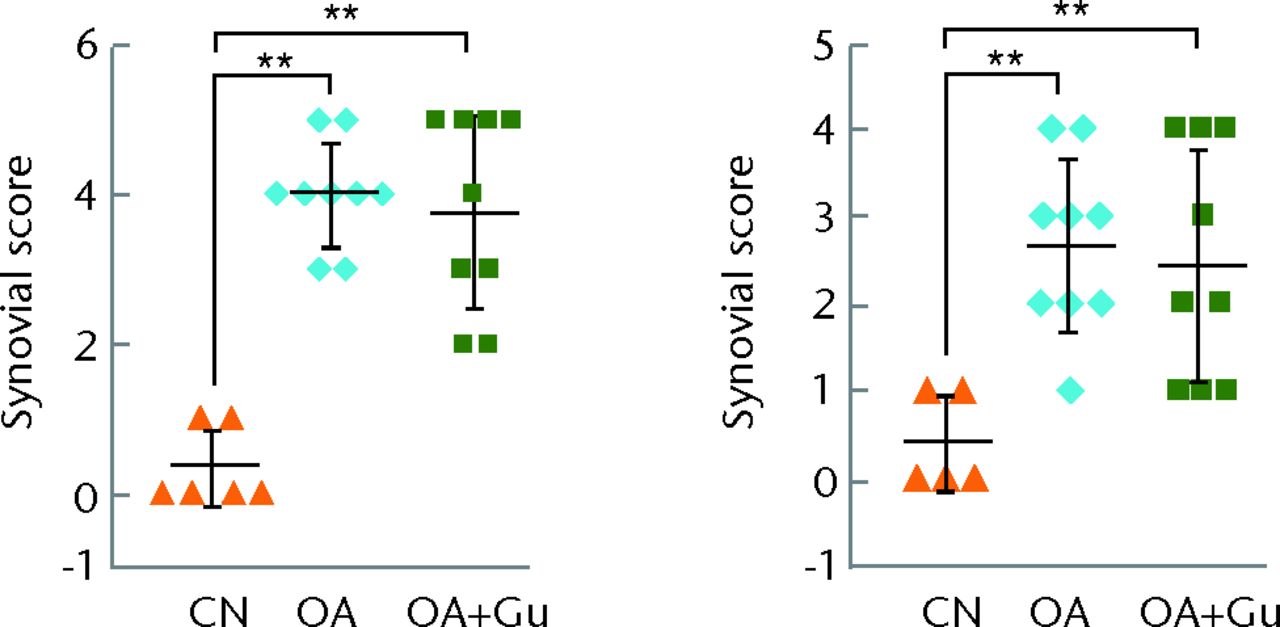
Figs. 8a - 8b
Graphs showing the effects of Guanabenz on subchondral bone and synovium, with a) thickness of subchondral bone for three-week (top) and six-week (bottom) samples in the medial femoral condyle (MFC) (left) and medial tibial plateau (MTP) (right) and b) synovial score for three-week (left) and six-week (right) samples.*p < 0.05; **p < 0.01.
No significant effects on the contralateral knee
Examination of the contralateral knee, which did not receive surgery for OA induction or administration of Salubrinal or Guanabenz, revealed that no significant effects were detected on thickness of subchondral bone or histological scores.
Discussion
This study demonstrates that daily administration of Salubrinal attenuates the degradation of the tibial and femoral articular cartilage and the inflammation of synovium by downregulating NFκB signalling. Salubrinal’s suppressive effects on the proteolytic activity of MMP13, as well as its elevation of the phosphorylation of NFκB p65 in the mouse model of OA, were consistent with in vitro data. The OA model in the current study induced damage in the medial collateral ligament and the medial meniscus. As post-traumatic OA may cause injuries in those regions, the results shown in this study may support the idea that Salubrinal can be applied to treat OA resulting from traumatic joint injuries.
The progression of symptoms of OA differed between the tibia and femur, and the efficacy of Salubrinal depended on time points. In response to Salubrinal, significant suppression of cartilage degradation was identified three weeks after the induction of OA in the femur, while in the tibia it was six weeks. Although the mean histological score at week three for the Salubrinal-treated OA group was similar in the femur (2.5, sd 0.5) and the tibia (2.2, sd 0.8), the mean week three score for the OA placebo group was 3.8, sd 1.2 (femoral) and 2.8, sd 1.0 (tibial), indicating that the initial phase was more severe in the femur than in the tibia. In the week six OA placebo group, the mean score approached the worst score of six in the femur (5.1, sd 0.8) and in the tibia (5.3, sd 0.7). Significant suppression of OA symptoms was detected only in the tibia samples, although the actual mean histological score was close between the femur (4.0, sd 1.9) and the tibia (3.7, sd 1.8).
Although Salubrinal is known to reduce stress to the endoplasmic reticulum, the mechanism of Salubrinal’s action in the current study does not appear to be linked to eIF2α regulation. Guanabenz is another agent that upregulates phosphorylation of eIF2α. Unlike Salubrinal, however, Guanabenz does not alter the level of p-NFκB or reduce activity of MMP13. We have previously shown using C28/I2 chondrocytes that silencing NFκB p65 suppressed TNFα-driven upregulation of MMP13.22 In this study, in vivo and in vitro data support the notion that Salubrinal’s chondroprotection results from the downregulation of p-NFκB (Fig. 9). We evaluated MMP13 activity, as MMP13 degrades not only collagen, but also aggrecan, and it is the most highly expressed collagenase in patients with OA.28
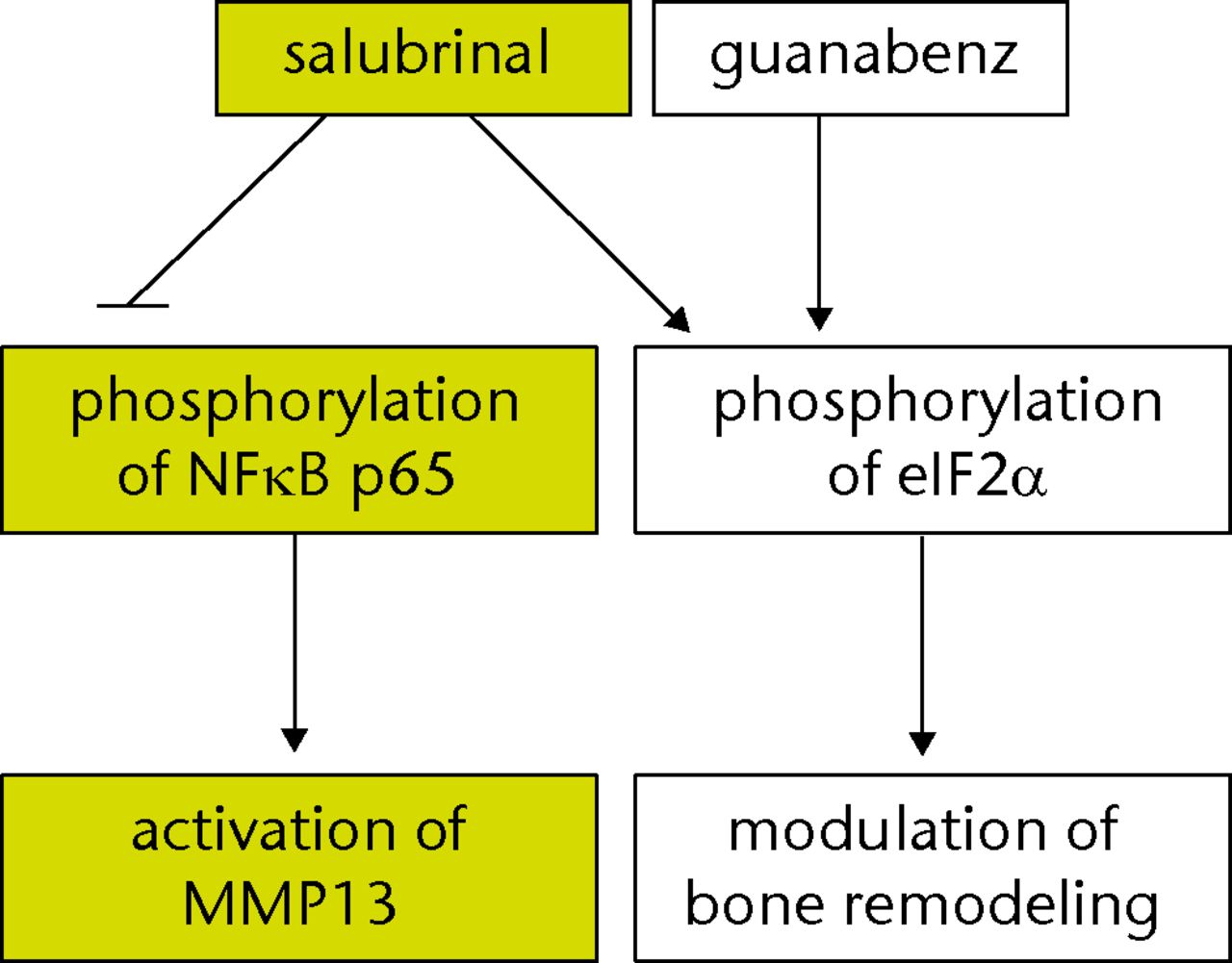
Fig. 9
Flow chart of the proposed signalling pathway driven by Salubrinal in a mouse model of osteoarthritis. NFκB, nuclear factor kappa B; MMP13, matrix metalloproteinase; eIF2α, eukaryotic translation initiation factor 2α
Regarding NFκB signalling, differential regulation of total protein levels of NFκB was observed in in vitro and in vivo experiments. Although the level of p-NFκB was elevated in both TNFα-stimulated primary chondrocytes and the OA tibial cartilage, the total protein level of NFκB was increased in the OA cartilage but not in TNFα-stimulated chondrocytes. This difference is potentially caused by the short incubation time (15 mins) with TNFα. Alternatively, in addition to TNFα, inflammatory factors such as IL1β likely contributed to the elevation of NFκB in the OA cartilage.29
Administration of Salubrinal for pre-clinical treatment of various diseases has been tested for diabetes,18 Alzheimer’s disease30 and osteoporosis.31 We, therefore, employed a mouse model of OA and showed that injection of Salubrinal into the intra-articular space delayed the progression of OA. Multiple strategies for treatment of OA have been considered, including transplantation of MSCs, antibodies directed to inflammatory cytokines, synthetic and natural chemical agents, and mechanical stimulation.25 Although Salubrinal prevents bone resorption and the stimulation of subchondral bone formation is part of the joint pathology in OA, the current mouse model of OA did not show any increase in thickness of subchondral bone in response to Salubrinal. Thus, Salubrinal is potentially able to attenuate the degradation of articular cartilage and the inflammation of synovium without causing a pathological thickening of subchondral bone.
There are several factors that might facilitate further evaluation of the efficacy of Salubrinal. First, an extended period of chondroprotection beyond three to six weeks could be evaluated by selecting proper dosages and administration frequencies. Second, daily intra-articular injection may not provide a convenient option in clinical situations. Sustained delivery of Salubrinal could be examined using implantable scaffolds or targeted nanoparticles.32 Third, with the exception of Salubrinal’s effects on chondroprotection, it is important to examine the effects on chondroregeneration including expression of matrix components such as type II collagen and aggrecan.
In conclusion, we have demonstrated that Salubrinal attenuated degradation of articular cartilage by inhibiting MMP13 activity through NFκB signalling. Further analysis regarding administration frequency and most effective dosage may warrant a future clinical trial in patients with OA.
Acknowledgement: Human C28/I2 chondrocyte cells were provided by M. Goldring. The authors appreciate the technical assistance of M. Hamamura and A. Chen.
1 Gelber AC , HochbergMC, MeadLA, et al.Joint injury in young adults and risk for subsequent knee and hip osteoarthritis. Ann Intern Med2000;133:321–328.CrossrefPubMed Google Scholar
2 Roos EM . Joint injury causes knee osteoarthritis in young adults. Curr Opin Rheumatol2005;17:195–200.CrossrefPubMed Google Scholar
3 Sudo A , MiyamotoN, HorikawaK, et al.Prevalence and risk factors for knee osteoarthritis in elderly Japanese men and women. J Orthop Sci2008;13:413–418.CrossrefPubMed Google Scholar
4 Gupta KB , DuryeaJ, WeissmanBN. Radiographic evaluation of osteoarthritis. Radiol Clin North Am2004;42:11–41.CrossrefPubMed Google Scholar
5 Convery FR , AkesonWH, KeownGH. The repair of large osteochondral defects. An experimental study in horses. Clin Orthop Relat Res1972;82:253–262.PubMed Google Scholar
6 Furukawa T , EyreDR, KoideS, GlimcherMJ. Biochemical studies on repair cartilage resurfacing experimental defects in the rabbit knee. J Bone Joint Surg [Am]1980;62-A:79–89.PubMed Google Scholar
7 Mankin HJ . The response of articular cartilage to mechanical injury. J Bone Joint Surg [Am]1982;64-A:460–466.PubMed Google Scholar
8 Naito K , TakahashiM, KushidaK, et al.Measurement of matrix metalloproteinases (MMPs) and tissue inhibitor of metalloproteinases-1 (TIMP-1) in patients with knee osteoarthritis: comparison with generalized osteoarthritis. Rheumatology (Oxford)1999;38:510–515.CrossrefPubMed Google Scholar
9 Naito S , ShiomiT, OkadaA, et al.Expression of ADAMTS4 (aggrecanase-1) in human osteoarthritic cartilage. Pathol Int2007;57:703–711.CrossrefPubMed Google Scholar
10 Zhang W , NukiG, MoskowitzRW, et al.OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage2010;18:476–499.CrossrefPubMed Google Scholar
11 Callahan CM , DrakeBG, HeckDA, DittusRS. Patient outcomes following tricompartmental total knee replacement. A meta-analysis. JAMA1994;271:1349–1357.PubMed Google Scholar
12 Carr AJ , RobertssonO, GravesS, et al.Knee replacement. Lancet2012;379:1331–1340.CrossrefPubMed Google Scholar
13 Khalifé S , ZafarullahM. Molecular targets of natural health products in arthritis. Arthritis Res Ther2011;13:102.CrossrefPubMed Google Scholar
14 Henrotin Y , GharbiM, DierckxsensY, et al.Decrease of a specific biomarker of collagen degradation in osteoarthritis, Coll2-1, by treatment with highly bioavailable curcumin during an exploratory clinical trial. BMC Complement Altern Med2014;14:159.CrossrefPubMed Google Scholar
15 Elmali N , EsenkayaI, HarmaA, et al.Effect of resveratrol in experimental osteoarthritis in rabbits. Inflamm Res2005;54:158–162.CrossrefPubMed Google Scholar
16 Yano F , HojoH, OhbaS, et al.A novel disease-modifying osteoarthritis drug candidate targeting Runx1. Ann Rheum Dis2013;72:748–753.CrossrefPubMed Google Scholar
17 Orth P , CucchiariniM, ZurakowskiD, et al.Parathyroid hormone [1-34] improves articular cartilage surface architecture and integration and subchondral bone reconstitution in osteochondral defects in vivo. Osteoarthritis Cartilage2013;21:614–624. Google Scholar
18 Boyce M , BryantKF, JousseC, et al.A selective inhibitor of eIF2α dephosphorylation protects cells from ER stress. Science2005;307:935–939. Google Scholar
19 Yang X , MatsudaK, BialekP, et al.ATF 4 is a substrate of RSK 2 and an essential regulator of osteoblast biology; implication for Coffin-Lowry Syndrome. Cell2004;117:387–398. Google Scholar
20 Hamamura K , TanjungN, YokotaH. Suppression of osteoclastogenesis through phosphorylation of eukaryotic translation initiation factor 2 alpha. J Bone Miner Metab2013;31:618–628.CrossrefPubMed Google Scholar
21 Takayanagi H , KimS, KogaT, et al.Induction and activation of the transcription factor NFATc1 (NFAT2) integrate RANKL signaling in terminal differentiation of osteoclasts. Dev Cell2002;3:889–901.CrossrefPubMed Google Scholar
22 Hamamura K , LinCC, YokotaH. Salubrinal reduces expression and activity of MMP13 in chondrocytes. Osteoarthritis Cartilage2013;21:764–772.CrossrefPubMed Google Scholar
23 Kamekura S , HoshiK, ShimoakaT, et al.Osteoarthritis development in novel experimental mouse models induced by knee joint instability. Osteoarthritis Cartilage2005;13:632–641.CrossrefPubMed Google Scholar
24 Glasson SS , ChambersMG, Van Den BergWB, LittleCB. The OARSI histopathology initiative - recommendations for histological assessments of osteoarthritis in the mouse. Osteoarthritis Cartilage2010;18 (Suppl 3):S17–S23.CrossrefPubMed Google Scholar
25 Hamamura K , ZhangP, ZhaoL, et al.Knee loading reduces MMP13 activity in the mouse cartilage. BMC Musculoskelet Disord2013;14:312.CrossrefPubMed Google Scholar
26 Pan J , WangB, LiW, et al.Elevated cross-talk between subchondral bone and cartilage in osteoarthritic joints. Bone2012;51:212–217.CrossrefPubMed Google Scholar
27 Krenn V , MorawietzL, BurmesterGR, et al.Synovitis score: discrimination between chronic low-grade and high-grade synovitis. Histopathology2006;49:358–364.CrossrefPubMed Google Scholar
28 Mitchell PG , MagnaHA, ReevesLM, et al.Cloning, expression, and type II collagenolytic activity of matrix metalloproteinase-13 from human osteoarthritic cartilage. J Clin Invest1996;97:761–768.CrossrefPubMed Google Scholar
29 Chen LX , LinL, WangHJ, et al.Suppression of early experimental osteoarthritis by in vivo delivery of the adenoviral vector-mediated NF-kappaBp65-specific siRNA. Osteoarthritis Cartilage2008;16:174–184.CrossrefPubMed Google Scholar
30 Huang X , ChenY, ZhangH, et al.Salubrinal attenuates β-amyloid-induced neuronal death and microglial activation by inhibition of the NFκB pathway. Neurobiol Aging2012;33:1007–1009. Google Scholar
31 Yokota H , HamamuraK, ChenA, et al.Effects of salubrinal on development of osteoclasts and osteoblasts from bone marrow-derived cells. BMC Musculoskelet Disord2013;14:197.CrossrefPubMed Google Scholar
32 Kang ML , KoJY, KimJE, ImGI. Intra-articular delivery of kartogenin-conjugated chitosan nano/microparticles for cartilage regeneration. Biomaterials2014;35:9984–9994.CrossrefPubMed Google Scholar
Funding statement:
None declared
Author contributions:
K. Hamamura: Conception and experimental design, Data collection and interpretation, Drafted manuscript
A. Nishimura: Conception and experiment design, Data collection and interpretation, Drafted manuscript
T. Iino: Data collection and interpretation
S. Takigawa: Data collection and interpretation
A. Sudo: Conception and experimental design
H. Yokota: Conception and experimental design, Drafted manuscript
ICMJE Conflict of Interest:
None declared
©2015 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
Supplementary material. Additional graphs showing no significant effects of osteoarthritis induction and administration of Salubrinal or Guanabenz on the contralateral knee are available with the online version of this article at www.bjj.boneandjoint.org.uk










