Abstract
Objectives
This study tests the biomechanical properties of adjacent locked plate constructs in a femur model using Sawbones. Previous studies have described biomechanical behaviour related to inter-device distances. We hypothesise that a smaller lateral inter-plate distance will result in a biomechanically stronger construct, and that addition of an anterior plate will increase the overall strength of the construct.
Methods
Sawbones were plated laterally with two large-fragment locking compression plates with inter-plate distances of 10 mm or 1 mm. Small-fragment locking compression plates of 7-hole, 9-hole, and 11-hole sizes were placed anteriorly to span the inter-plate distance. Four-point bend loading was applied, and the moment required to displace the constructs by 10 mm was recorded.
Results
We found that a 1 mm inter-plate distance supported greater moments than a 10 mm distance in constructs with only lateral plates. Moments supported after the addition of a 9- or 11-hole anterior plate were greater for both 10 mm and 1 mm inter-plate distance, with the 11-hole anterior plate supporting a greater moment than a 9-hole plate. Femurs with a 7-hole anterior plate fractured regardless of lateral inter-plate distance size.
Conclusion
This suggests that the optimal plate configuration is to minimise lateral inter-plate distance and protect it with an anterior plate longer than seven holes.
Cite this article: Bone Joint Res 2015;4:23–8.
Article Focus
Are constructs with a 1 mm lateral inter-plate distance stiffer than constructs with a 10 mm inter-plate distance?
Does the addition of an anterior plate increase the construct stiffness?
Does the length of the anterior plate alter construct stiffness?
Key messages
Optimum plate configuration minimises inter-plate distance and protects the inter-plate distance stress riser with an anterior plate
An anterior plate should be longer than seven holes
Strengths and limitations
Synthetic femurs allow for uniform results and testing of the construct itself rather than construct–bone interface
Synthetic femurs may not accurately reflect in vivo bone
This study tests single plane moments, which does not reflect all moments seen in vivo
Introduction
Interprosthetic femoral fractures occur between proximal and distal devices. Proximal devices can include sliding hip screw side plates, cephalomedullary devices, angled blade plates and total hip arthroplasty (THA) implants. Distal devices can include distal femoral locking plates, condylar blade plates, short retrograde medullary devices and total knee arthroplasty (TKA) implants.Fractures between these devices may occur in osteoporotic stress-shielded bone. Fixation constructs are challenged by the presence of pre-existing devices and poor bone quality. One strategy employed with success when treating interprosthetic femoral fractures occurring between stable joint replacement implants is lateral plating, with the construct spanning both joint arthroplasty implants.1,2 The purpose of spanning the interprosthetic region with the lateral plate is to neutralise any potential stress risers caused by the gap between the two rigid constructs in osteopaenic or osteoporotic bone.
Whereas fixation of a fracture distal to a proximal implant (THA) can be managed with a single lateral plate spanning the entire length of the femur, short length distal plate constructs may expose a segment of femoral diaphysis to risk of fracture.3 The presence of a laterally-based proximal femoral plate construct (e.g. sliding hip screw, angled blade plate, proximal femoral locking plate) does not allow for a single lateral plate to protect the interprosthetic zone. Treating surgeons should understand biomechanical behaviour and consequences of fixation constructs when facing the dilemma of treating subsequent fractures between proximal and distal constructs. If a distal femoral plate is deemed appropriate to address the fracture, an inter-plate gap will exist between the new implant and the pre-existing proximal plate. That gap may represent a further ‘at risk’ zone for future fracture.
Our approach to these fractures has evolved to include direct fracture reduction with distal femoral locking plate minimising inter-device distance with the pre-existing proximal femoral implant, followed by orthogonal plating of the femur along the anterior cortex to span the inter-device distance (Fig. 1). We are currently unaware of any data to suggest the optimal inter-device distance between two lateral constructs, or the optimal size of an anterior plate. For the purposes of this study, we will refer to the inter-device distance as the inter-plate distance (IPD) for clarification and simplicity.

Fig. 1
Anteroposterior radiograph of left femur showing orthogonal plate fixation of a patient with an interprosthetic femoral fracture between a stable total knee arthroplasty and proximal blade plate. The fracture was treated with a distal lateral femoral locking plate, and anterior small fragment locking plate to protect the lateral inter-plate distance. This image was obtained at a six month post-operative visit and shows uneventful union.
This study asks the following questions: first, are constructs with a 1 mm lateral IPD stiffer than constructs with a 10 mm IPD? Second, does addition of an anterior plate increase the construct stiffness? Third, does the length of the anterior plate alter construct stiffness? We hypothesise that decreasing lateral IPD will result in biomechanically stiffer constructs and that addition of an anterior plate will increase the stiffness of the construct and mitigate the potential risk for inter-device fracture. In addition, we hypothesise that increasing anterior plate length will not significantly increase stiffness of the construct.
Patients and Methods
A total of 23 plastic femurs (Sawbones left foam femurs, #1129; Pacific Research Laboratories, Vashon, Washington) were tested using different plate combinations and IPDs. Even though plastic femurs may not simulate osteoporotic bone, they were used in order to have a consistent geometry and uniform properties for each comparative test. Each femur was positioned in a four-point bend fixture (Fig. 2) were tested using different plate combinations and IPDs. Even though plastic femurs may not simulate osteoporotic bone, they were used in order to have a consistent geometry and uniform properties for each comparative test. Each femur was positioned in a four-point bend fixture (Fig. 2) such that the loading occurred in the sagittal plane with tensile forces seen on the anterior face of the femur. Four-point bending was chosen as it applies a uniform moment between the upper two supports. Three-point bending would have focused the maximum moment directly beneath the middle roller positioned over the gap between the lateral plates. Each femur was positioned in order for the midpoint between subsequently attached lateral plates to be centred between the two upper supports.
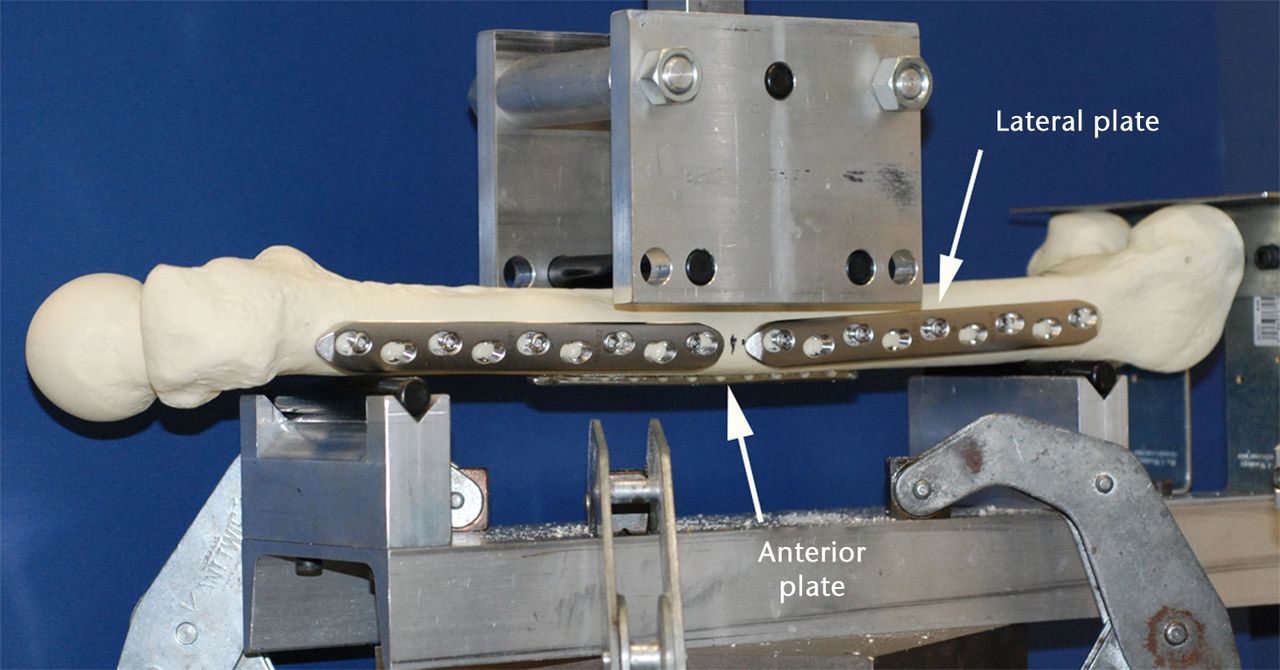
Fig. 2
Photograph showing the four-point bend testing fixture that was used to load each femur in the sagittal plane. Each femur was positioned in a four-point bend fixture such that the loading occurred in the sagittal plane with tensile forces seen on the anterior face of the femur.
Each femur was preconditioned by first applying a 10 N compressive force (using an MTS machine, MTS, Eden Prairie, Minnesota) to the four-point bend fixture to preload the bone, and then applying a ramp displacement of 10 mm to the fixture 100 times. The force was applied by the MTS actuator to the upper pair of rollers, and the corresponding displacement of the rollers was measured. Each femur was preconditioned to reduce the potential effect of any history dependence on them, as it was a viscoelastic material. During the first ten cycles of preconditioning, slight decreases in peak moment were seen. Each femur was then tested while intact and after different plate configurations were applied. In these tests, a 10 N force was first applied and five cycles of 10 mm displacement performed. The peak-applied compressive force during the fifth cycle was determined and converted to an applied sagittal moment by knowing the location of the end supports and the intermediate loading bars. Using these measurements, from a strength of materials approach the applied moment is equal to:
- Moment (N-m) = F * (L - a)/ 4
- where F = applied force in N
- L = distance between the outer rollers
- a = distance between the inter rollers
Thus, the applied moment = 0.0572 * the applied force.
In eight femurs, after testing the intact bone, two large-fragment lateral locking compression plates (LCP) (Synthes, Paoli, Philadalphia) were applied using five 5 mm locking screws distributed equally along the plate in bicortical locked mode, with a 10 mm IPD between the plates, and subsequently tested using the four-point fixture (Fig. 2) (Synthes, Paoli, Philadalphia) were applied using five 5 mm locking screws distributed equally along the plate in bicortical locked mode, with a 10 mm IPD between the plates, and subsequently tested using the four-point fixture (Fig. 2) were applied using five 5 mm locking screws distributed equally along the plate in bicortical locked mode, with a 10 mm IPD between the plates, and subsequently tested using the four-point fixture (Fig. 2). A 9-hole small-fragment LCP plate was placed anteriorly using three 3.5 mm locking screws distributed equally in unicortical lock mode on each side of the lateral plate gap, and the bone tested again. The 9-hole plate was removed and an 11-hole anterior plate was applied and tested, again using three 3.5 mm locking screws in unicortical lock mode on either side of the lateral plate gap. Finally, the 9-hole plate was reapplied and the femur retested to verify that the application and testing of the 9-hole plate first did not affect the results with the 11-hole plate.
In eight additional femurs, the same testing was performed as above, with the only difference being that a 1 mm IPD between the lateral plates was used.
In four additional femurs, the same testing protocol was applied with a 10 mm lateral IPD and a 7-hole anterior plate. In the last three femurs, the same testing protocol was applied with a 1 mm lateral IPD with a 7-hole anterior plate.
Statistical analysis
To compare the maximum moment supported by different plate combinations for a given IPD, a one-way repeated measures analysis of variance was used. To compare the effect of a 1 mm or 10 mm IPD for each plate combination, a two-way independent measures analysis of variance was used (one factor being the plate combination, the other factor being the gap distance). If a difference between the two gap distances was found, additional one-way analysis of variance tests were performed to examine the effect of gap distance for each plate combination. In all cases, a Bonferroni adjustment for multiple pairwise comparisons was used with a level of significance of p < 0.05.
To determine the necessary number of femurs to test, a power study was performed based on the first three specimens tested. To show a difference between the laterally plated femurs and the intact femur, or to show a difference between anterior plates with differing number of holes, a minimum of seven specimens would be required to have 80% power with a level of 95% significance. Thus, a sample size of eight femurs was used.
To determine whether the moments we applied in this testing were comparable with in vivo moments, we compared the moments created by the four-point fixture with those measured in vivo by Taylor et al.4 They found the peak sagittal moments from one subject to be approximately 25 Nm during level walking or for rising from a chair and to be approximately 40 Nm while ascending stairs. During our testing, our applied moments ranged from 40 Nm to 65 Nm, suggesting that we were comparable with, or greater than, in vivo loading.
Results
When only lateral plates are applied, the moment supported with a 1 mm IPD had a trend to be greater than that supported with a 10 mm IPD (Table I, p = 0.052). Constructs with a 9-hole anterior plate and a 1 mm IPD supported a significantly greater moment than a 10 mm IPD (p = 0.025). Similarly, constructs with an 11-hole anterior plate and a 1 mm IPD had a significantly greater moment than a 10 mm IPD (p = 0.008).
Table I
Moment supported by the intact bone or with different plate combinations (Nm). (Standard deviations in parentheses; IPD, inter-plate distance)
| 10 mm IPD | 1 mm IPD | |
|---|---|---|
| Intact bone | 43.2 (4.0) | 40.1 (1.5) |
| Two lateral plates | 49.2 (4.0) | 53.3 (1.3) |
| Addition of 9-hole anterior plate | 57.4 (3.7) | 62.4 (1.9) |
| Addition of 11-hole anterior plate | 59.8 (3.6) | 65.1 (1.1) |
The addition of a 9-hole or 11-hole anterior plate to constructs with either 10 mm lateral IPD or 1 mm lateral IPD resulted in constructs that supported significantly greater moments than constructs with only lateral plates (Table I, p < 0.001).
When comparing moments supported by the 11-hole plate with those supported by the 9-hole plate, the 11-hole anterior plate supported significantly more moment than the 9-hole plate in both the 10 mm (p = 0.047) and the 1 mm IPD constructs (p = 0.025). There was no difference in moments supported by the 9-hole plate either before or after testing the 11-hole plate in both groups (p < 0.99).
In testing the seven femurs with a 7-hole anterior plate, with either a 10 mm IPD or a 1 mm IPD, all femurs failed. In six, the Sawbones fractured through either the most proximal or most distal screw hole of the anterior plate and, in one, the screws failed and the plate pulled out upon application of load.
Discussion
Described treatments of interprosthetic femoral fractures between both a stable THA and TKA include intramedullary fixation, plate constructs, as well as allograft strut and cerclage constructs.1,2,5-18 Interprosthetic femoral fractures may also occur between arthroplasty implants and plate constructs. These fractures may not be amenable to intramedullary fixation in the presence of non-compatible TKA implants, or the presence of screws from the proximal femoral plate, preventing placement of an intramedullary device. If the pre-existing proximal femoral fracture is healed, it is reasonable to remove either screw or plate to allow the passage of an intramedullary device, or to place a longer plate. However, if the pre-existing fracture has not healed, the proximal femoral plate construct may need to be retained, precluding the use of a single long lateral locking plate to span the fracture and implants. This study is designed to test the biomechanical characteristics of the protocol we have developed for treating these fractures by minimising lateral IPD and protecting it with an anterior plate.
Potential limitations in this study include the use of a synthetic femur rather than cadaveric bone. We elected to use synthetic material to obtain uniform results which would not be possible in cadaveric bone. Third generation sawbone femurs have been shown to have similar stiffness to cadaveric bone, with more uniform structural properties when compared with previous Sawbones.19 This provides a uniform material that would allow us to test the construct itself, rather than the construct–bone interface. A synthetic osteoporosis Sawbones model is available for use, however, we are unaware of any published data relating to the reliability of that model to approximate osteoporotic bone in biomechanical testing. A second potential limitation may be the use of four-point bend exclusively in the anteroposterior plane. This may represent a type of stress seen in vivo, but it does not address varus or valgus stress or torsional stress that may be experienced by the femur during the course of daily life. Finally, our constructs were composed of plates placed in the locking configuration, which may only provide a mechanical advantage in osteoporotic bone.20
The present study confirms our hypothesis that when the IPD distance is reduced from 10 mm to 1 mm, there is an increase in the moment required to displace the femur. Although this was not significant when only lateral plates were applied, this trend did become significant after a 9- or 11-hole anterior plate was applied. This suggests that minimising the lateral IPD increases the overall stiffness of the construct and may reduce the ‘stress riser’ phenomenon21 anticipated by leaving an unprotected area of poor quality bone between two rigid constructs.
This study confirms our hypothesis that placement of either a 9- or an 11-hole LCP significantly increases the overall stiffness of the construct. The goal of the anterior plate is to protect the anticipated stress riser that exists between the lateral plate constructs. Studies have attempted to define the nature of these stress risers, with particular emphasis on intramedullary implants.3,21-23 Although the exact nature of stress risers has yet to be defined, it seems prudent to neutralise any that may occur between two stiff implants in poor quality bone that has already failed with a low-energy mechanism. Our testing protocol uses four-point bend to displace the femur and plate constructs. This creates a tension moment on the anterior cortex and, therefore, it is expected that placement of an anterior plate should increase the overall stiffness of the construct when subjected to the bend, and mitigate the effects of any potential stress riser. Interestingly, our data show that both 9- and 11-hole anterior plate constructs were stiffer when the lateral IPD was only 1 mm. This confirms the trend we observed in the first part of our study when using only lateral plates to evaluate the IPD.
Our protocol calls for placement of an anterior plate onto the femur to span the lateral IPD. We recognise this technique necessitates additional soft-tissue dissection from the anterior femur and, as such, it is our goal to minimise the soft-tissue insult by reducing the size of the anterior plate. Thus, we wished to discover whether anterior plate length altered the biomechanics of the construct. This study found that 11-hole LCP constructs require greater moment to displace the femur than the 9-hole LCP constructs. These rely on the angular stability created by the screwhead–LCP interface. Better stress distribution is achieved with fewer screws and increased distance between screws, in a bridge plating technique.24-26 Our study would indicate that the stress riser should be considered in terms of a comminuted segment that would benefit from distribution of the stress along a bridge-type anterior construct. It is not surprising, then, that 11-hole LCP constructs support greater moments than 9-hole constructs. We did not expect, however, that this difference would be statistically significant, as our original hypothesis indicates.
Our final finding related to the anterior plates was unanticipated. All 7-hole LCP constructs reliably failed when in four-point bend. In the six 7-hole LCP constructs that failed by fracture, the fracture occurred through either the most distal or most proximal screw hole of the anterior LCP. In some studies the LCP can act as a stress concentrator, and result in implant or construct failure.25 It is possible that the 7-hole LCP construct failed because it was of insufficient length to neutralise the stress riser, and may have acted as a stress concentrator, particularly at the most proximal and distal screws of the anterior plate. The 9- and 11-hole anterior plate constructs may not have failed because those constructs were able to distribute the tension forces due to the applied moment over a greater distance and, thus, avoid failure.
In conclusion, our study would suggest that the optimal configuration when plating an interprosthetic femoral fracture between a TKA and a proximal femoral plate construct is to minimise the lateral IPD, and to protect this gap with an anterior small fragment plate with more than seven holes.
1 Bryant GK , MorshedS, AgelJ, et al.Isolated locked compression plating for Vancouver type B1 periprosthetic femoral fractures. Injury2009;40:1180–1186.CrossrefPubMed Google Scholar
2 Mamczak CN , GardnerMJ, BolhofnerB, et al.Interprosthetic femur fractures. J Orthop Trauma2010;12:740–744.CrossrefPubMed Google Scholar
3 Peindl RD, Mazurek MT, Bosse MJ, et al Fixation of mid- and distal-third femoral fractures in the presence of a THA component: a biomechanical assessment. [abstract] Annual Meeting of the Orthopaedic Trauma Association, 2003 http://www.hwbf.org/ota/am/ota03/otapo/OTP03018.htm (date last accessed 11 February 2015). Google Scholar
4 Taylor SJG , WalkerPS, PerryJS, CannonSR, WoledgeR. The forces in the distal femur and the knee during walking and other activities measured by telemetry. J Arthroplasty1998;13:428–437.CrossrefPubMed Google Scholar
5 Buttaro MA , FarfalliG, ParedesNM, CombaF, PiccalugaF. Locking compression plate fixation of Vancouver type-B1 periprosthetic femoral fractures. J Bone Joint Surg [Am]2007;89-A:1964–1969.CrossrefPubMed Google Scholar
6 Fink B , FuerstM, SingerJ. Periprosthetic fractures of the femur associated with hip arthroplasty. Arch Orthop Trauma Surg2005;125:433–442.CrossrefPubMed Google Scholar
7 Gliatis J , MegasP, PanagiotopoulosE, LambirisE. Midterm results of treatment with a retrograde nail for supracondylar periprosthetic fractures of the femur following total knee arthroplasty. J Orthop Trauma2005;19:164–170.CrossrefPubMed Google Scholar
8 Haddad FS , MarstonRA, Muirhead-AllwoodSK. The Dall-Miles cable and plate system for periprosthetic femoral fractures. Injury1997;28:445–447.CrossrefPubMed Google Scholar
9 Kelley SS . Periprosthetic femoral fractures. J Am Acad Orthop Surg1994;2:164–172.CrossrefPubMed Google Scholar
10 Kenny P , RiceJ, QuinlanW. Interprosthetic fracture of the femoral shaft. J Arthroplasty1998;13:361–364.CrossrefPubMed Google Scholar
11 Kregor PJ , HughesJL, ColePA. Fixation of distal femoral fractures above total knee arthroplasty utilizing the Less Invasive Stabilization System (LISS). Injury2001;32:SC64–SC75. Google Scholar
12 Meyer C , AltV, SchroederL, HeissC, SchnettlerR. Treatment of periprosthetic femoral fractures by effective lengthening of the prosthesis. Clin Orthop Relat Res2007;463:120–127.CrossrefPubMed Google Scholar
13 O’Toole RV , GobezieR, HwangR, et al.Low complication rate of LISS for femur fractures adjacent to stable hip or knee arthroplasty. Clin Orthop Relat Res2006;450:203–210. Google Scholar
14 Pike J , DavidsonD, GarbuzD, et al.Principles of treatment for periprosthetic femoral shaft fractures around well-fixed total hip arthroplasty. J Am Acad Orthop Surg2009;17:677–688.CrossrefPubMed Google Scholar
15 Ponzer S , TidemarkJ, TornkvistH. Retrograde nailing of femoral fractures distal to a Moore prosthesis. J Orthop Trauma1998;12:588–591.CrossrefPubMed Google Scholar
16 Ricci WM , BorrelliJ Jr. Operative management of periprosthetic femur fractures in the elderly using biological fracture reduction and fixation techniques. Injury2007;38:S53–S58.CrossrefPubMed Google Scholar
17 Ricci WM , HaidukewychGJ. Periprosthetic femoral fractures. Instr Course Lect2009;58:105–115.CrossrefPubMed Google Scholar
18 Ricci WM , LoftusT, CoxC, BorrelliJ. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma2006;20:190–196.CrossrefPubMed Google Scholar
19 Heiner AD , BrownTD. Structural properties of a new design of composite replica femurs and tibias. J Biomech2001;34:773–781. Google Scholar
20 Kubiak EN , FulkersonE, StraussE, EgolKA. The evolution of locked plates. J Bone Joint Surg [Am]2006;88-A:189–200.CrossrefPubMed Google Scholar
21 Iesaka K , KummerFJ, Di CesarePE. Stress risers between two ipsilateral intramedullary stems: a finite-element and biomechanical analysis. J Arthoplasty2005;20:386–391.CrossrefPubMed Google Scholar
22 Lehmann W , RupprechtM, HellmersN, et al.Biomechanical evaluation of peri- and interprosthetic fractures of the femur. J Trauma2010;68:1459–1463.CrossrefPubMed Google Scholar
23 Rupprecht M , SellenschlohK, GrossterlindenL. Biomechanical evaluation for mechanisms or periprosthetic femoral fractures. J Trauma2011;70:E62–E66. Google Scholar
24 Leunig M , HertelR, SiebenrockKA, et al.The evolution of indirect reduction techniques for the treatment of fractures. Clin Orthop Relat Res2000;375:7–14.CrossrefPubMed Google Scholar
25 Sommer C , GautierE, MullerM, HelfetDL, WagnerM. First clinical results of the Locking Compression Plate (LCP). Injury2003;34:43–54.CrossrefPubMed Google Scholar
26 Tornqvist H , HearnTC, SchatzkerJ. The strength of plate fixation in relation to the number and spacing of bone screws. J Orthop Trauma1996;10:204–208.CrossrefPubMed Google Scholar
Funding statement:
F. W. Werner owns stock in Moximed, however, no materials or other support was received from Moximed in relation to this article. D. A. Auston and R. B. Simpson have received expenses from Smith & Nephew and Zimmer, respectively, none of which is related to this article. F. W. Werner reports a grant received from Stryker Orthopaedics to SUNY Upstate Medical University which is not related to this article.
Author contributions:
D. A. Auston: Project design, Data collection, Data analysis, Writing and editing paper
F. W. Werner: Project design, Data collection, Data analysis, Writing paper
R. B. Simpson: Project design, Data analysis, Writing paper
ICMJE Conflict of Interest:
None declared
©2015 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










