Abstract
Objective
A clinical investigation into a new bone void filler is giving first data on systemic and local exposure to the anti-infective substance after implantation.
Method
A total of 20 patients with post-traumatic/post-operative bone infections were enrolled in this open-label, prospective study. After radical surgical debridement, the bone cavity was filled with this material. The 21-day hospitalisation phase included determination of gentamicin concentrations in plasma, urine and wound exudate, assessment of wound healing, infection parameters, implant resorption, laboratory parameters, and adverse event monitoring. The follow-up period was six months.
Results
Systemic exposure to gentamicin after implantation was very low as local gentamicin concentrations were measured in wound exudate after six to ten hours. There were no signs of infectious complication throughout the clinical phase. Four patients had recurrent infections several weeks to months after implantation. The outcome was deemed successful by remission of infection in 16 (80%) of these problematic long-term treated patients. Safety laboratory measurements did not indicate nephrotoxic or hepatotoxic effects.
Conclusions
Local application of calcium sulphate/carbonate bone void filler comprising gentamicin revealed sufficient active local levels of the antibiotic by simultaneous significant low systemic exposure in patients with mostly chronic osteomyelitis/osteitis. The material was safe and well tolerated.
Cite this article: Bone Joint Res 2014;3:223–9.
Article focus
This article focuses on the pharmacokinetic release of locally administered gentamicin – we hoped to get some clarification that the relevant release profile of the novel bone void filler would not jeopardise safety for systemic resistance in the patient
We assess the safety and tolerability of the new bone void filler
Key messages
The local antibiotic concentration levels were sufficient to protect against or eradicate persistent relevant bone and joint infection criteria
The systemic antibiotic concentration was low and thus unproblematic in the sense of a critical antibiotic level resulting in development of a resistance
Even though the follow-up period was relatively short, good tolerability and safety could be attributed to the new bone void filler. This, in particular, was used to assess recurrence or persistence of infection
Strengths and limitations
A study group of 20 patients is adequate to determine a release profile
The follow-up period of six months is sufficient to evaluate a post-operative antibiotic concentration level
The short follow-up time is a limitation to assess a basic clinical outcome, in particular for late onset infections
Introduction
Bone infections occurring after exposed fracture or orthopaedic surgeries such as total arthroplasty of the hip or knee, can progress to a chronic stage and lead to severe complications such as osteitis, osteonecrosis, sepsis or amputation.1 Despite the variety of available treatment options, including surgical procedures and antimicrobial therapy, bone infections are still a medical challenge as they are difficult to treat and cure.2 An optimal therapy should stabilise the bone, promote biological repair of the skeletal defects and eradicate the bacterial infection. In many cases, keeping the infection at bay has to be accepted as a successful outcome after surgical and antibacterial management. Systemic antibiotics are part of the standard therapy after debridement of infected bone, but their efficacy may be limited due to impaired blood supply and a low penetration rate at the site of infection.3 Furthermore, long-term treatment and high doses are associated with severe side effects. In contrast, antibiotic-impregnated bone void fillers or cements can act as local anti‑infective drug release systems, which not only fill up the dead space after surgical debridement but also deliver high antibiotic concentrations at the site of potential infection, without increasing serum antibiotic levels.4-8 Gentamicin-containing polymethylmethacrylate (PMMA) beads, for the local treatment of orthopaedic infections, have been in clinical use for more than 30 years.9-11 A disadvantage of PMMA is that the material is non-biodegradable, making subsequent invasive procedures necessary to remove the implant in many cases.12 New antibiotic bone substitution materials/bone void fillers are based on biodegradable or resorbable materials such as polylactic acid, chitosan or new combinations based on calcium sulfate.13 These permanently implantable materials do not have to be removed after a time, unlike for example PMMA chains, and they meet the requirements for application in the final step of bone defect therapy. Calcium sulfate is a well-studied, non-immunogenic, biocompatible bone void filler used in orthopaedic applications since the 19th century.14-16 It has been shown to stimulate new bone formation comparable with autogenous bone12,17-20 and is also a suitable carrier for aminoglycoside antibiotics.13,19-21 In a recent study, calcium sulfate pellets impregnated with tobramycin were as effective as PMMA beads in the treatment of chronic osteomyelitis and infected nonunion.12 Surgical-grade calcium sulfate pellets pre-loaded with tobramycin (Osteoset® T, Wright Medical Technologies Inc., Arlington, Tennessee) have been commercially available for over a decade. Occasionally, non-infectious inflammatory reactions have been observed after the implantation, which are suspected to be caused by calcium-rich fluid generated in the process of rapid graft resorption.22,23
The investigated calcium sulfate-calcium carbonate-tripalmitate new composite is a recently developed bone graft substitute/bone void filler with antibacterial properties, which had its market entry in 2010. Very little clinical data have been published so far on the administration of this bone void filler.24 The aim of this prospective investigation was primarily to determine gentamicin concentrations in blood plasma, urine and wound exudate of patients with post-traumatic or post-operative bone infections after surgical debridement of infected areas and implantation of this substance. Clinical effects and safety of the beads were also evaluated. This study was approved by the Ethical Committee of the Landesärztekammer Hessen under FF 10/2008.
Patients and Methods
Study design and patient population
The open-label, exploratory, phase II investigation was performed at the Trauma Hospital (BGU), Frankfurt/Main, Germany. A total of 20 adults (16 male, 4 female, ≥ 18 years) suffering from post-traumatic or post-operative bone infection (osteomyelitis/osteitis) of the upper or lower extremities with potentially gentamicin-sensitive bacteria and with an indication for implantation of a bone void filler material were included in the investigation. The size of the bone defect after surgical debridement had to be between 10 cm3 and 50 cm3 ; the minimum volume was due to the size of the beads and relevant bone voids, the maximum volume to the dosage of gentamicin permitted. Patients with renal impairment, a significant allergic disposition, sensorineural hearing loss, and known hypersensitivity to gentamicin or other aminoglycosides were excluded. Pregnant or nursing women, and women for whom the possibility of pregnancy could not be excluded, were also not eligible for inclusion in the study.
Systemic or local gentamicin treatment, other than the implantation of resorbable gentamicin beads, was not allowed. A total of seven patients received a concomitant systemic antibiotic treatment (other than gentamicin) according to the antibiogram performed after microbiological sampling of the infected bone. This was performed according to a particular risk management of those patients. The clinical part (hospitalisation phase) of the investigation was continued up to day 21 after the implantation.
Materials and implantation
Herafill® beads G (Heraeus Medical GmbH, Wehrheim, Germany) are biconvex, rounded, cylindrical (6 mm × 6 mm) calcium sulfate-calcium carbonate beads containing glycerin tripalmitate as bonding additive and 1% gentamicin sulfate (2.5 mg gentamicin base) as antibacterial agent. The beads were implanted into the cavity of the bone after radical surgical debridement of the infected area (Fig. 1) are biconvex, rounded, cylindrical (6 mm × 6 mm) calcium sulfate-calcium carbonate beads containing glycerin tripalmitate as bonding additive and 1% gentamicin sulfate (2.5 mg gentamicin base) as antibacterial agent. The beads were implanted into the cavity of the bone after radical surgical debridement of the infected area (Fig. 1) calcium sulfate-calcium carbonate beads containing glycerin tripalmitate as bonding additive and 1% gentamicin sulfate (2.5 mg gentamicin base) as antibacterial agent. The beads were implanted into the cavity of the bone after radical surgical debridement of the infected area (Fig. 1) as antibacterial agent. The beads were implanted into the cavity of the bone after radical surgical debridement of the infected area (Fig. 1). The number of implanted Herafill® beads G ranged between 13 and 190 per patient (mean 74.8). There was a surgical decision to exceed the manufacturer’s recommendation of 1 bead/kg body weight in six patients (30%, five male, one female) in order to fill up the bone void entirely. A minimum of one intralesional microbiological sample was taken during surgery as a standardised procedure.
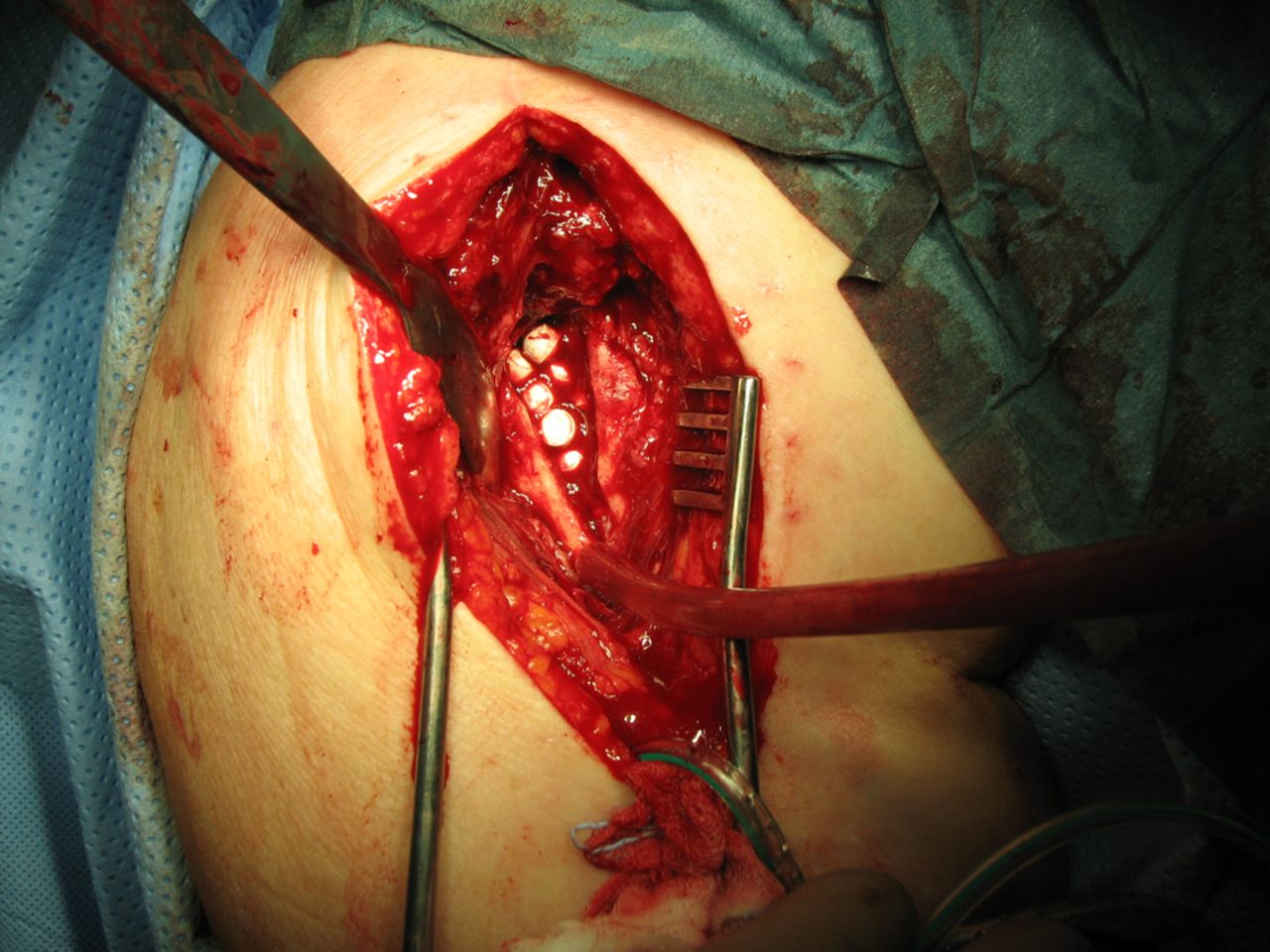

Figs. 1a - 1b
Figure 1a – photograph showing in situ demonstration of applied beads in a debrided bone void. Figure 1b – radiograph of the implant’s position in a chronically infected tibial zone.
Concentration measurements of gentamicin
Blood samples were taken within six hours before the implantation (baseline) and post-operatively after two, four, six, ten, and 24 hours, and on days 2 to 7. Pre-surgical urine was collected over a 24-hour period. Post-surgically, 0 to ten hours and ten to 24 hours, urine samples were collected on day 1 and 24-hour urine samples were collected on days two to seven. Wound exudate was collected from wound tissue immediately before implantation of the beads and from the drainage bottles at two, four, six, ten, 24, 48, and 72 hours after surgery. All patients except one had only one subfascial drain inserted. In the one case with two inserted drains, only the fluid collected from the drain adjacent to the wound was used for the calculation of mean gentamicin concentrations. Plasma, urine and wound exudate samples were stored at -20°C. Gentamicin concentrations were measured using a High Performance Hybrid Mass Spectrometer (Applied Biosystems 4000 Q TRAP® LC/MS/MS, Foster City, California). The lower levels of quantification (LLOQ) were 0.001 µg/mL in both plasma and wound exudate and 0.0025 µg/mL in urine.
Clinical parameters and safety evaluations
The course of infection was monitored by determination of C-reactive protein (CRP) levels and leukocyte count; blood samples were taken at baseline, 24 hours after surgery, and on days 2, 4, 6, 10, 14, and 21. Wound healing was assessed on days 2, 4, 6, 8, 10, and 12, and at the time of removal of sutures. Resorption of implanted beads and bony reconstruction were evaluated by means of radiographs obtained at two to four days and at approximately three and six months after implantation. Radiographs were taken for study purposes only when indicated and as part of the clinical standard assessment process. Final follow-up to evaluate pharmacokinetic release rates came six months after surgery or at the time of early termination; during this observation period no recurrence of infection could be found.
Adverse events were monitored during the entire study. Blood samples for safety laboratory tests (serum creatinine, urea, total bilirubin, liver enzymes) were taken at baseline, 24 hours after surgery, and on days 2, 4, 6, 10 and 14.
Statistical analysis
Deviations from baseline in infection and safety laboratory parameters were analysed by Wilcoxon signed rank tests. Statistical significance was set at p < 0.05.
Results
Patient population
A total of 20 patients (mean age 51.1+13.4 years (24 to 79), 16 male, four female) were treated with Herafill® beads G (Heraeus Medical GmbH) from April 2008 to April 2011. All patients had a clinical history of previous indication-related surgeries. A chronic course of osteomyelitis/osteitis was reported in at least 12 (60%, ten males, two females) of the patients. The remaining eight patients had acute osteomyelitis for other reasons including excidents. The mean time interval since the occurrence of the primary traumatic event was approximately six years (24 days to 30 years). Demographic data and details of the medical history of the patients are presented in Table I. A total of 18 patients were ranked in ASA (American Society for Anesthesiology)25,26 Score 1 and two in ASA 3, indicating that the majority of the patient population was in a good state of health (χ = 1.3). All patients completed the clinical phase of the investigation. Follow-up data collected at both three and/or six months after surgery were only available for one patient due to poor patient compliance at both follow-up points.
Table I
Demographic data and medical history
| Characteristic | Values |
|---|---|
| Age (yrs) mean (range) | 51 (24 to 79) |
| Weight (kg), mean (range) | 84 (60 to 120) |
| Sex, n (%), male/female | 16 (80)/4 (20) |
| Race, n (%), Caucasian/Asian | 19 (95)/1 (5) |
| Primary traumatic event n (%) | |
| Fracture/injury/other trauma | 16 (80) |
| Consequence of surgery | 3 (15) |
| Haematogenous osteomyelitis | 1 (5) |
| Location of osteomyelitis | |
| Tibia (proximal, distal, shaft) | 11 (55) |
| Femur (proximal, distal, shaft) | 7 (35) |
| Other (humeral head, metatarsal bone) | 2 (10) |
Systemic and local exposure to gentamicin
The mean plasma concentration of gentamicin was below the LLOQ at baseline (Fig. 2) and remained very low after implantation of Herafill® beads G. A peak mean concentration of 0.2 µg/mL (sd 0.2 (0.05 to 0.6)) was measured at 24 hours after surgery. After 48 hours, the mean concentration had decreased to 0.06 µg/mL (sd 0.04 (0.002 to 0.2)). Individual plasma gentamicin concentrations did not exceed 0.6 µg/mL.
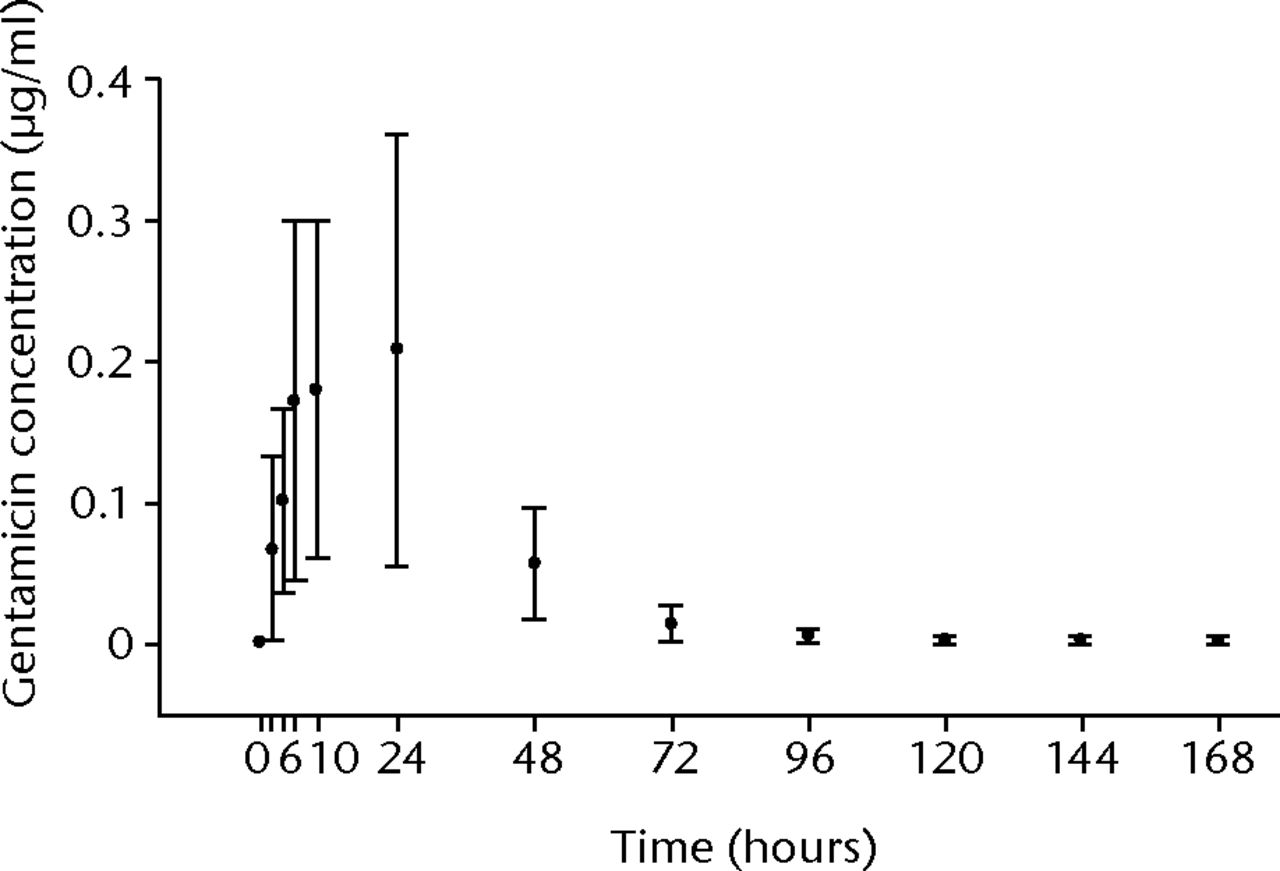
Fig. 2
Graph showing mean (n = 18 to 20) plasma gentamicin concentrations at baseline (0 hours: within six hours prior to surgery) and after implantation of HERAFILL® beads G (Heraeus Medical GmbH) (error bars = standard deviation)
Very low amounts of gentamicin were detectable in urine samples of seven patients already at baseline, resulting in a mean baseline level of 0.2 µg/mL (sd 0.4) (Fig. 3) (Fig. 3). Mean urine gentamicin concentrations were low after implantation, with a peak of 7.6 µg/mL (sd 6.4 (0.7 to 22.9)) in the ten to 24 hour sample. The mean concentration had decreased to 0.7 µg/mL (sd 0.4 (0.2 to 1.4)) in the last sample taken on day 7. Individual urine gentamicin concentrations did not exceed 22.9 µg/mL.
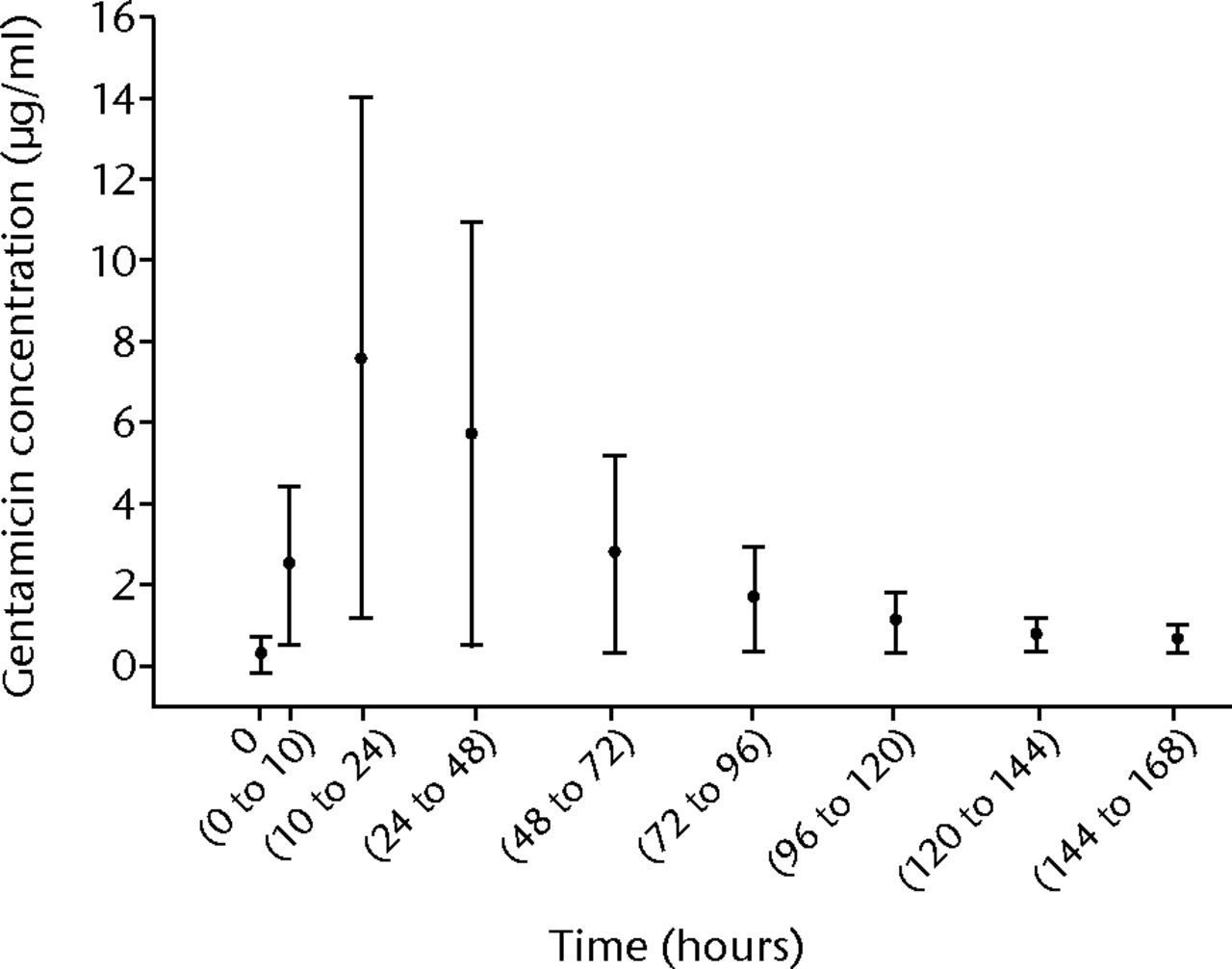
Fig. 3
Graph showing mean (n = 16-20) urine gentamicin concentrations at baseline (0 hours: 24-hour collection within six hours prior to surgery) and after implantation of HERAFILL® beads G (Heraeus Medical GmbH) (error bars = standard deviation)
The concentration of gentamicin in wound exudate was below the LLOQ in all patients at baseline. High levels of gentamicin were measured in wound exudate post-operatively. The mean concentration peaked in the six to ten hour sample, with 1110 µg/mL (sd 540 (234 to 2235)) and was still at 170 µg/mL (sd 135) in the last sample taken after 48 to 72 hours (Fig. 4) in the last sample taken after 48 to 72 hours (Fig. 4). The highest individual gentamicin concentration in wound exudate was 2404 µg/mL.
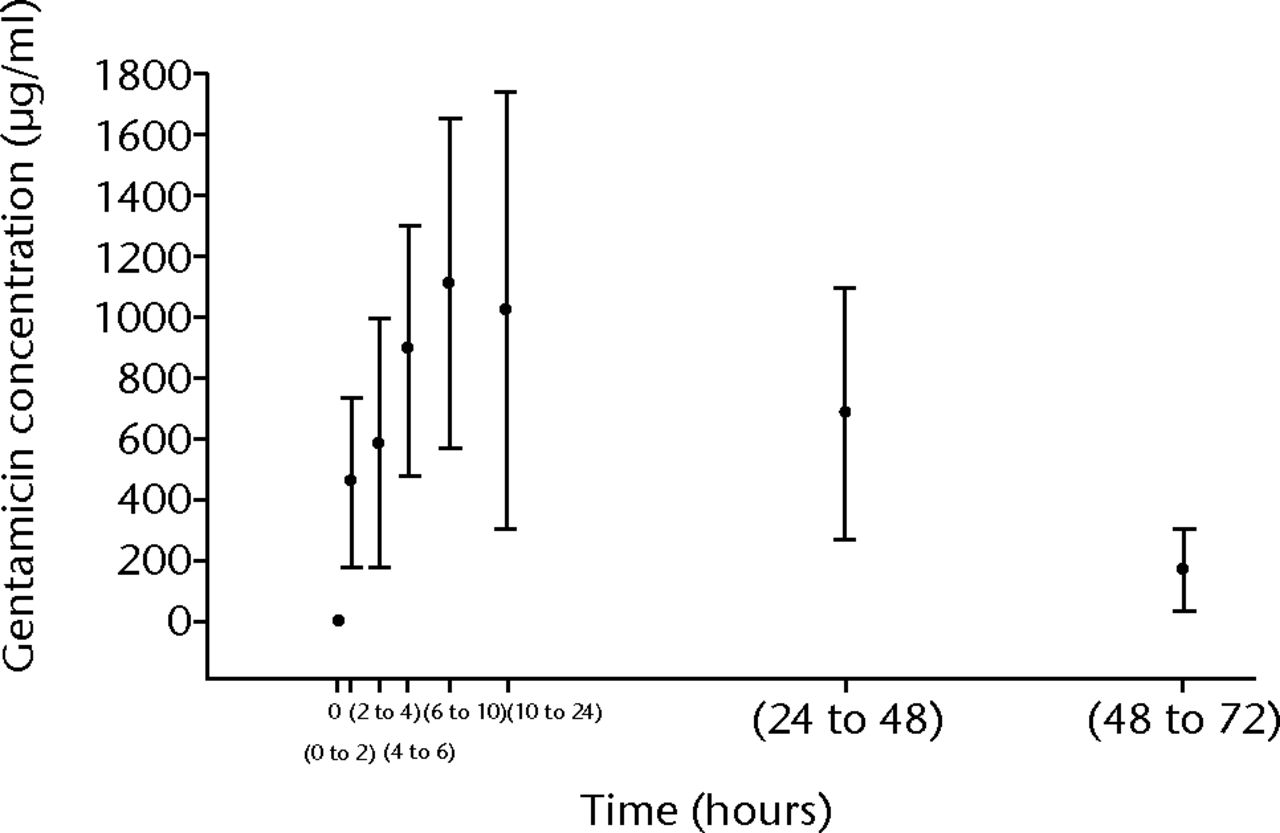
Fig. 4
Graph showing mean (n = 18 to 20) gentamicin concentrations in wound-exudate at baseline (0 hours: sample taken during surgery) and after implantation of Herafill® beads G (Heraeus Medical GmbH) (error bars = standard deviation)
Clinical effects
A radiological implant evaluation after approximately six months showed that bony integration of the beads could be assessed as good, and/or individual beads were no longer discernible in 12 out of 14 patients for whom an evaluation was available (Fig. 5). In the remaining two patients, a process of bead dissolution was revealed at that time.




Figs. 5a - 5d
Radiographs showing HERAFILL® beads G (Heraeus Medical GmbH) after implantation into a distal tibial bone void a) pre-operatively, b) post-operatively, c) three and d) six months post-operatively.
Primary wound healing occurred in 17 patients and secondary wound healing in three patients. The clinical outcome after six months (or at the time of early termination) amounted to successful treatment assessed as remission of infection in 16 patients (80%) over the time of observation. A total of four patients (20%) had recurrent infections requiring a revision surgery probably related to uncompleted surgical infection management. This rate was due to the selection of ‘at risk’ patients suffering from long-term osteitis and several surgeries, and the ratio of the low patient number available.
Mean leukocyte counts were within the normal laboratory range and did not indicate infectious complications during the first 21 days after surgery. The mean post-surgical changes in leukocyte counts were not statistically significant from baseline in patients with complete data (n = 14, p-value day 2 = 0.5; p-value day 21 = 0.2). As expected, the mean CRP value increased shortly after surgery, with a peak of 2.3 mg/dL (sd 1.3) on day 2, and then gradually decreased to 0.5 mg/dL (sd 0.4) on day 21.
Safety
Safety laboratory measurements did not reveal any nephrotoxic or hepatotoxic effects of Herafill® beads G (Heraeus Medical GmbH) in the study patients. Mean concentrations of serum creatinine and urea were within the reference ranges, and post-surgical changes were not statistically significant from baseline (p-value serum creatinine 0.1 to 0.9, p-value urea 0.2 to 0.9). There was a significant decrease (p = 0.0001 to 0.037, Wilcoxen signed rank test) in mean total bilirubin after implantation, but all values were within the reference range. Increased liver enzymes were occasionally observed pre-and post-surgery in some of the patients. There were two cases of an early re-infection during the course of the study, likely related to an incomplete eradication of infected tissue occuring during the course of the study.
Discussion
Insufficient release of the antibacterial agent to the site of infected bone is a frequent problem associated with systemic antibiotic therapy and sometimes even with local drug delivery systems.3 After the implantation of Herafill® beads G (Heraeus Medical GmbH) in bone defects caused by osteomyelitis/osteitis in upper or lower extremities, very high gentamicin concentrations were measured in wound exudate during the first days after surgery. In the last sample collected (48 to 72 hours), concentrations still considerably exceeded the required concentration for efficient bacterial eradication and were above those measured in the wound exudate of patients after implantation of gentamicin-containing PMMA beads.4 In general, determination of antibiotics in wound exudate is difficult due to the fact that the consistency and volume of the exudate varies during the wound healing process. There are several factors, such as tissue debris, proteins, blood, and interstitial fluid, which show a high variability in amount and composition. It was therefore decided to use blood plasma – not wound exudate – as a model matrix for the determination of gentamicin concentrations in the wound exudate in order to avoid a potential impact of matrix variations on the standard analytical procedure. Thus, a general overestimation of the concentrations due to an analytical enhancement effect cannot be completely ruled out. However, even in the worst case of overestimation by a factor of 10, the initial gentamicin levels would still have been well above the minimal inhibitory concentration for relevant pathogens.
Plasma levels of gentamicin remained extremely low following the procedure and only traces of gentamicin were identified after a few days. The use of a modern high resolution LC/MS/MS detection method for analysis in this investigation led to low concentrations of gentamicin measured in urine prior to the implantation of Herafill® beads G (Heraeus Medical GmbH) in a few patients. These patients had been treated with gentamicin-containing biomaterials prior to the start of the investigation. It has been shown that after local application of antibiotic-loaded implants, antibiotic concentrations are detectable for up to six weeks in the surrounding tissue. Thus, small residual amounts of gentamicin from previous treatments were probably the basis for these pre-implantation levels.
After implantation of Herafill® beads G (Heraeus Medical GmbH), the mean urine concentrations remained below 8 µg/mL (0.7 to 7.6). The very low systemic exposure to gentamicin after treatment with Herafill® bead G (Heraeus Medical GmbH) minimises both the potential for toxic reactions and the induction of resistance of relevant bacterial strains coming from the systemic side. This is in line with the safety findings of this investigation, which did not indicate any nephrotoxic or hepatotoxic effects of gentamicin released from the Herafill® beads G (Heraeus Medical GmbH). Even in six patients who received a higher amount of beads than recommended by the manufacturer, no increased plasma gentamicin concentrations were observed when compared with those of the patients with smaller amounts implanted.
Radiographic analysis approximately six months after surgery showed progressive or complete resorption of the implanted Herafill® beads G (Heraeus Medical GmbH). A continuous remission of the infection was achieved in 16 patients (80%), whereby more than half of these patients did not receive concomitant systemic antibiotic therapy. In the treatment of chronic osteomyelitis, local antibiotic delivery is mainly used as an adjuvant to intravenous antibiotic therapy. By using antibiotic-impregnated bone void fillers/substitutes which are able to deliver high local antibiotic concentrations over an adequate period of time, the need for systemic antibiotics could potentially be reduced. Their high dosage side effects, as well as the low local concentrations, might thus be avoided. In a recent study, locally implanted synthetic calcium sulfate antibiotic beads successfully healed low-extremity osteomyelitis in 17 patients (86%) without the use of systemic antibiotics.27
In the current investigation, four patients (20%, three male, one female) developed recurrent infection several weeks or months after the implantation of Herafill® beads G (Heraeus Medical GmbH). Local gentamicin concentrations measured during the first 72 hours after implantation were adequately high in these patients. All four patients had undergone several previous indication-related operations, including implantation of gentamicin-containing cement or PMMA beads in three patients (15%, two male, one female). Antibiotic resistance can play a role in recurrent infections. Some bacterial strains are also capable of forming biofilms on biological and artificial surfaces, which makes treatment with antimicrobial agents very difficult. The increased resistance of the adhered bacteria to antimicrobial agents remains a problem in orthopaedic surgery. Adherence and persistent growth of bacteria on antibiotic-loaded bone cements and PMMA beads have been intensively investigated.28-30 Bacterial adherence and biofilm formation on antibiotic-impregnated calcium sulfate beads have not been the subject of studies to our knowledge so far. Further investigations with a longer detailed clinical outcome observation period (one to five years’ follow-up period) would help to assess the course of healing of infected bone defects under this treatment.
Conclusion
This investigation in adult patients with severe, chronic post-traumatic or post-operative bone infections and normal renal function demonstrated that these novel calcium sulfate-based bone void filler beads with gentamicin are a clinically useful local antibiotic delivery system and bone void filler/ bone substitute which can be used as an alternative to other anti-infective implants. The potential for systemic side effects appears minimal in patients with normal renal function. The implantation of the beads was safe and well tolerated in all patients. The investigated new bone void filler composite can, overall, provide adequate protection against bacterial infection in all those challenging, at risk, patients with chronic osteomyelitis/osteitis during the first weeks after implantation and to support the bone healing process. Subsequent procedures to remove implanted material and the recreation of dead space are avoided due to the ability of the beads to resorb.
1 Senthi S , MunroJT, PittoRP. Infection in total hip replacement: meta-analysis. Int Orthop2011;35:253–260.CrossrefPubMed Google Scholar
2 Trampuz A , ZimmerliW. Diagnosis and treatment of implant-associated septic arthritis and osteomyelitis. Curr Infect Dis Rep2008;10:394–403.CrossrefPubMed Google Scholar
3 Zilberman M , ElsnerJJ. Antibiotic-eluting medical devices for various applications. J Control Release2008;130:202–215.CrossrefPubMed Google Scholar
4 Wahlig H , DingeldeinE, BergmannR, ReussK. The release of gentamicin from polymethylmethacrylate beads: an experimental and pharmacokinetic study. J Bone Joint Surg [Br]1978;60-B:270–275. Google Scholar
5 Henry SL , GallowayKP. Local antibacterial therapy for the management of orthopaedic infections. Pharmacokinetic considerations. Clin Pharmacokinet1995;29:36–45.CrossrefPubMed Google Scholar
6 Härle A , RitzerfeldW. The release of gentamycin into the wound secretions from polymethylmethacrylate beads. A study with reference to the animal experiment. Arch Orthop Trauma Surg1979;95:65–70.CrossrefPubMed Google Scholar
7 Winkler H . Rationale for one stage exchange of infected hip replacement using uncemented implants and antibiotic impregnated bone graft. Int J Med Sci2009;6:247–252.CrossrefPubMed Google Scholar
8 Zalavras CG , PatzakisMJ, HoltomP. Local antibiotic therapy in the treatment of open fractures and osteomyelitis. Clin Orthop Relat Res2004;427:86–93.CrossrefPubMed Google Scholar
9 Klemm K . Treatment of chronic bone infection with gentamicin PMMA-chains and beads. Accid Surg1976;1:20–25. Google Scholar
10 Klemm K. Gentamicin-PMMA-beads in treating bone and soft tissue infections. Zentralbl Chir 1979;104:934-942.[Article in German]. Google Scholar
11 Klemm KW . Gentamicin-PMMA chains (Septopal chains) for the local antibiotic treatment of chronic osteomyelitis. Reconstr Surg Traumatol1988;20:11–35.PubMed Google Scholar
12 McKee MD , Li-BlandEA, WildLM, SchemitschEH. A prospective, randomized clinical trial comparing an antibiotic-impregnated bioabsorbable bone substitute with standard antibiotic-impregnated cement beads in the treatment of chronic osteomyelitis and infected nonunion. J Orthop Trauma2010;24:483–490.CrossrefPubMed Google Scholar
13 Thomas MV , PuleoDA. Calcium sulfate: Properties and clinical applications. J Biomed Mater Res B Appl Biomater2009;88:597–610.CrossrefPubMed Google Scholar
14 de Boer HH . The history of bone grafts. Clin Orthop Relat Res1988;226:292–298.PubMed Google Scholar
15 Kelly CM , WilkinsRM, GitelisS, et al.The use of a surgical grade calcium sulfate as a bone graft substitute: results of a multicenter trial. Clin Orthop Relat Res2001;382:42–50.CrossrefPubMed Google Scholar
16 Bösebeck H, Büchner H. In: Peters KM, König DP, ed. Fortbildung Osteologie 3. 1st ed. Berlin Heidelberg: Springer-Verlag, 2010:109-115. [in German]. Google Scholar
17 Coetzee AS . Regeneration of bone in the presence of calcium sulfate. Arch Otolaryngol1980;106:405–409.CrossrefPubMed Google Scholar
18 Peters CL , HinesJL, BachusKN, CraigMA, BloebaumRD. Biological effects of calcium sulfate as a bone graft substitute in ovine metaphyseal defects. J Biomed Mater Res A2006;76:456–462.CrossrefPubMed Google Scholar
19 McKee MD , WildLM, SchemitschEH, WaddellJP. The use of an antibiotic-impregnated, osteoconductive, bioabsorbable bone substitute in the treatment of infected long bone defects: early results of a prospective trial. J Orthop Trauma2002;16:622–627.CrossrefPubMed Google Scholar
20 Beuerlein MJ , McKeeMD. Calcium sulfates: what is the evidence?J Orthop Trauma2010;24(Suppl1):S46–S51.CrossrefPubMed Google Scholar
21 Mousset B , BenoitMA, DelloyeC, BouilletR, GillardJ. Biodegradable implants for potential use in bone infection. An in vitro study of antibiotic-loaded calcium sulphate. Int Orthop1995;19:157–161.CrossrefPubMed Google Scholar
22 Lee GH , KhouryJG, BellJE, BuckwalterJA. Adverse reactions to OsteoSet bone graft substitute, the incidence in a consecutive series. Iowa Orthop J2002;22:35–38.PubMed Google Scholar
23 Robinson D , AlkD, SandbankJ, FarberR, HalperinN. Inflammatory reactions associated with a calcium sulfate bone substitute. Ann Transplant1999;4:91–97.PubMed Google Scholar
24 Franceschini M , Di MatteoA, BösebeckH, BüchnerH, VogtS. Treatment of a chronic recurrent fistulized tibial osteomyelitis: administration of a novel antibiotic-loaded bone substitute combined with a pedicular muscle flap sealing. Eur J Orthop Surg Traumatol2012;22(Suppl1):245–249.CrossrefPubMed Google Scholar
25 Saklad M . Grading of patients for surgical procedures. Anesthesiology1941;2:281–284. Google Scholar
26 Mak PH , CampbellRC, IrwinMG. The ASA Physical Status Classification: inter-observer consistency (American Society of Anesthesiologists). Anaesth Intensive Care2002;30:633–640. Google Scholar
27 Gauland C . Managing lower-extremity osteomyelitis locally with surgical debridement and synthetic calcium sulfate antibiotic tablets. Adv Skin Wound Care2011;24:515–523.CrossrefPubMed Google Scholar
28 König DP , SchierholzJM, HilgersRD, et al.In vitro adherence and accumulation of Staphylococcus epidermidis RP 62 A and Staphylococcus epidermidis M7 on four different bone cements. Langenbecks Arch Surg2001;386:328–332.CrossrefPubMed Google Scholar
29 Anagnostakos K , HitzlerP, PapeD, KohnD, KelmJ. Persistence of bacterial growth on antibiotic-loaded beads: is it actually a problem?Acta Orthop2008;79:302–307.CrossrefPubMed Google Scholar
30 Neut D , de GrootEP, KowalskiRS, et al.Gentamicin-loaded bone cement with clindamycin or fusidic acid added: biofilm formation and antibiotic release. J Biomed Mater Res A2005;73:165–170.CrossrefPubMed Google Scholar
Funding statement:
This study was funded by Heraeus Medical. H. Bösebeck, S. Vogt and H. Büchner are employees of Heraeus Medical. G. Walter, R. Hoffmann, N. Fleiter and W. Hirschberger report financial allowances from Heraeus Medical paid to Berufsgenossenschaftliche Unfallklinik for clinical study related to this paper.
Author contributions:
N. Fleiter: Data collection, Performed surgeries, Editorial contribution
G. Walter: Data collection, Performed surgeries, Editorial contribution
H. Bösebeck: Data collection, Data analysis, Writing the paper, Editorial coordination
S. Vogt: Data analysis, Editorial contribution
H. Büchner: Data analysis, Editorial contribution
W. Hirschberger: Data collection, Performed surgeries, Editorial contribution
R. Hoffmann: Data collection, Editorial contribution, Principle investigator
ICMJE Conflict of Interest:
None declared
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










