Abstract
Objectives
Acetabular retractors have been implicated in damage to the femoral and obturator nerves during total hip replacement. The aim of this study was to determine the anatomical relationship between retractor placement and these nerves.
Methods
A posterior approach to the hip was carried out in six fresh cadaveric half pelves. Large Hohmann acetabular retractors were placed anteriorly, over the acetabular lip, and inferiorly, and their relationship to the femoral and obturator nerves was examined.
Results
If contact with bone was not maintained during retractor placement, the tip of the anterior retractor had the potential to compress the femoral nerve by passing superficial to the iliopsoas. If pressure was removed from the anterior retractor, the tip pivoted on the anterior acetabular lip, and passed superficial to the iliopsoas, overlying and compressing the femoral nerve, when pressure was reapplied. The inferior retractor pierced the obturator membrane in all specimens medial to the obturator nerve, with subsequent retraction causing the tip to move laterally, making contact with the nerve.
Conclusion
Iliopsoas can only offer protection to the femoral nerve if the retractor passes deep to the muscle bulk. The anterior retractor should be reinserted if pressure is removed intra-operatively. Vigorous movement of the inferior retractor should be avoided.
Cite this article: Bone Joint Res 2014;3:212–6.
Article Focus
This article examines the relationship between the retractors used during acetabular preparation in total hip replacement and nerves surrounding the acetabulum, to determine their vulnerability during the procedure.
Key Messages
Care should be taken when placing retractors around the acetabulum during total hip replacement.
The anterior acetabular retractor may compress the femoral nerve if contact with the bone of the acetabular wall is lost during placement.
Vigorous movement of the inferior retractor should be prevented in order to protect the obturator nerve.
Strengths and Limitations
Strength: Provides clear anatomical evidence to support previous electrophysiological data on the aetiology of nerve injury during total hip replacement.
Limitation: The study uses a cadaveric material which is not fully representative of the operative experience.
Introduction
Nerve injury is a recognised complication of total hip replacement (THR). The clinical incidence of nerve damage following primary THR is reported to range between 0.17% and 3.7%,1,2 rising to 7.5% in revision procedures.3 In the majority of these cases, a full recovery is never achieved.1 A total of 80% of patients who sustain a neuropathy have persistent neurological dysfunction of motor weakness, paraesthesia or neuropathic pain.4,5 This results in a negative impact on the post-operative rehabilitation of patients and reduced patient satisfaction.6
However, it is felt that clinical examination alone underestimates the true incidence of nerve compromise following THR.7 Electromyographic studies have suggested that the incidence of subclinical nerve compromise may be as high as 70%,8 highlighting that routine aspects of the procedure place nerves at risk. Direct trauma, cement extrusion, compression by a haematoma, ischaemia, retraction, laceration and leg lengthening have all been implicated in the aetiology of peripheral nerve damage following THR.4,9 However, in over 50% of cases, a clear cause is not identified.5 Concerns have been expressed regarding the ability of retractors to cause nerve damage. Following evidence of damage to the femoral and obturator nerves on EMG studies, Weale et al7 hypothesised that retractors placed around the acetabulum were responsible for these injuries. Despite this, the anatomical relationship between retractor placement and these nerves has not been elucidated.
The aim of this study was to determine the relationship between retractor placement and the femoral and obturator nerves, in order to provide an anatomical explanation for the association between direct nerve injury and retraction in THR.
Materials and Methods
A total of six fresh-frozen cadaveric half pelves were obtained from the Laboratory of Human Anatomy at the University of Glasgow. The specimens had been detached superior to the iliac crest and superior to the knee joint, leaving all tissues of the gluteal region and hip joint intact. To facilitate dissection, the remaining abdominal and pelvic viscera were removed. The cadavers were left to thaw at room temperature prior to the experimental procedure. None of the cadavers showed any evidence of previous hip or pelvic surgery. The specimens came from two men and one woman with a mean age of 86 (78 to 92). The work was carried out in accordance with the Anatomy Act (1984) and its amendments under the Human Tissue (Scotland) Act 2006, so did not require ethical approval.
The pelvis was securely fixed in the lateral position and the hip was exposed through a standard posterior approach. A small incision was made in the anterior capsule to facilitate retractor placement. A large Hohmann retractor was placed through the capsule and over the anterior lip of the acetabulum at the three o’clock position (Fig. 1). It was inserted around the natural curve of the anterior acetabular wall and, once in position, gently pulled to gain an adequate view of the acetabulum through retraction of the femur. A second Hohmann retractor was placed around the inferior border of the acetabulum, at the six o’clock position (Fig. 2). It was moved around the curve of the inferior acetabulum, and, once in position, pressure was applied in order to improve visualisation by retracting the inferior soft tissues. During retractor placement, the surgeon (AWGK) had a view of the acetabulum consistent with that obtained during an operative procedure, and was therefore unable to see, and thus influence, the route of the retractors once passed over the lip of the acetabulum.
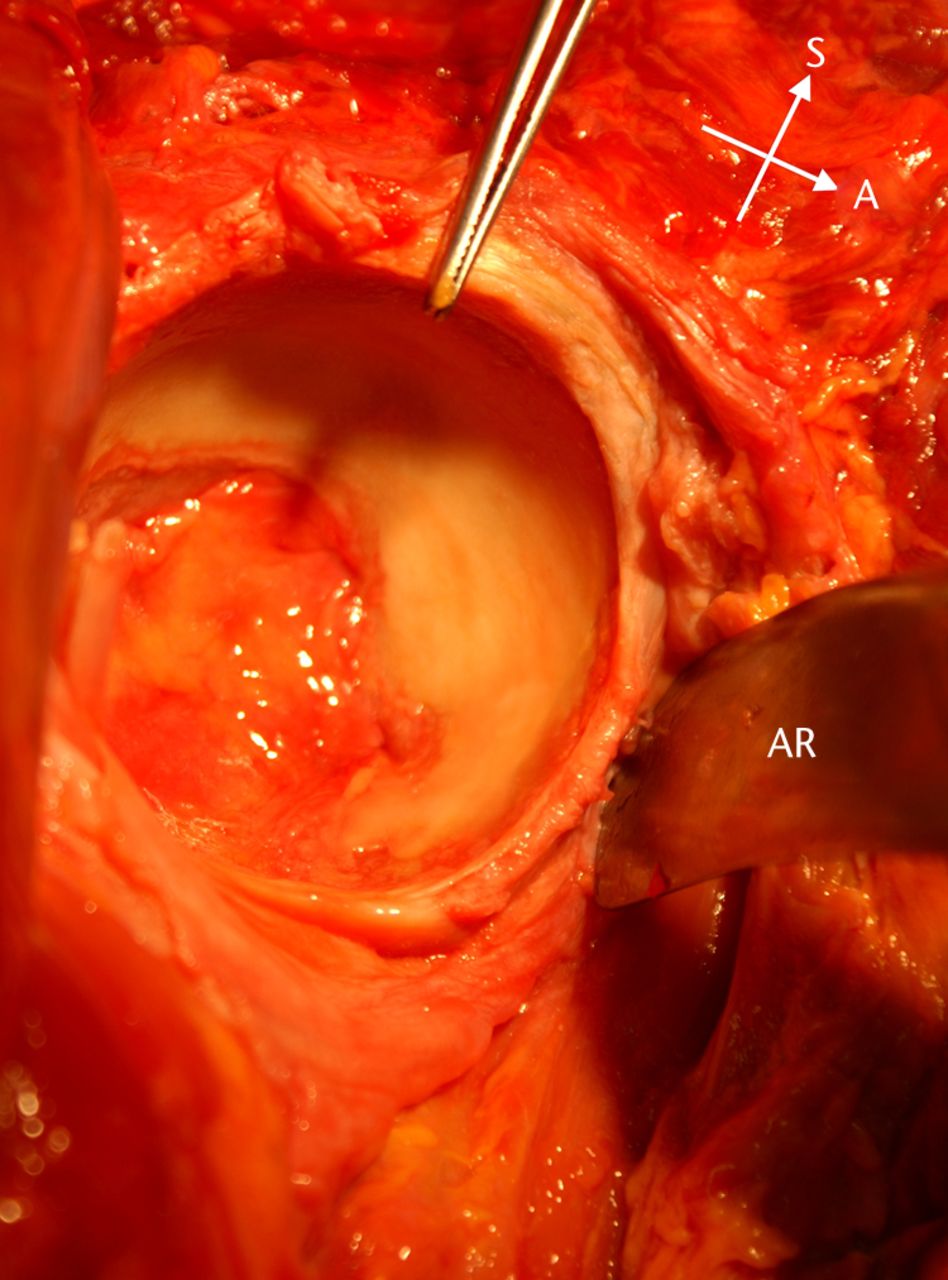
Fig. 1
Photograph showing the anterior retractor (AR) in situ around the anterior wall of the acetabulum. Forceps indicate 12 o'clock position on acetabulum.
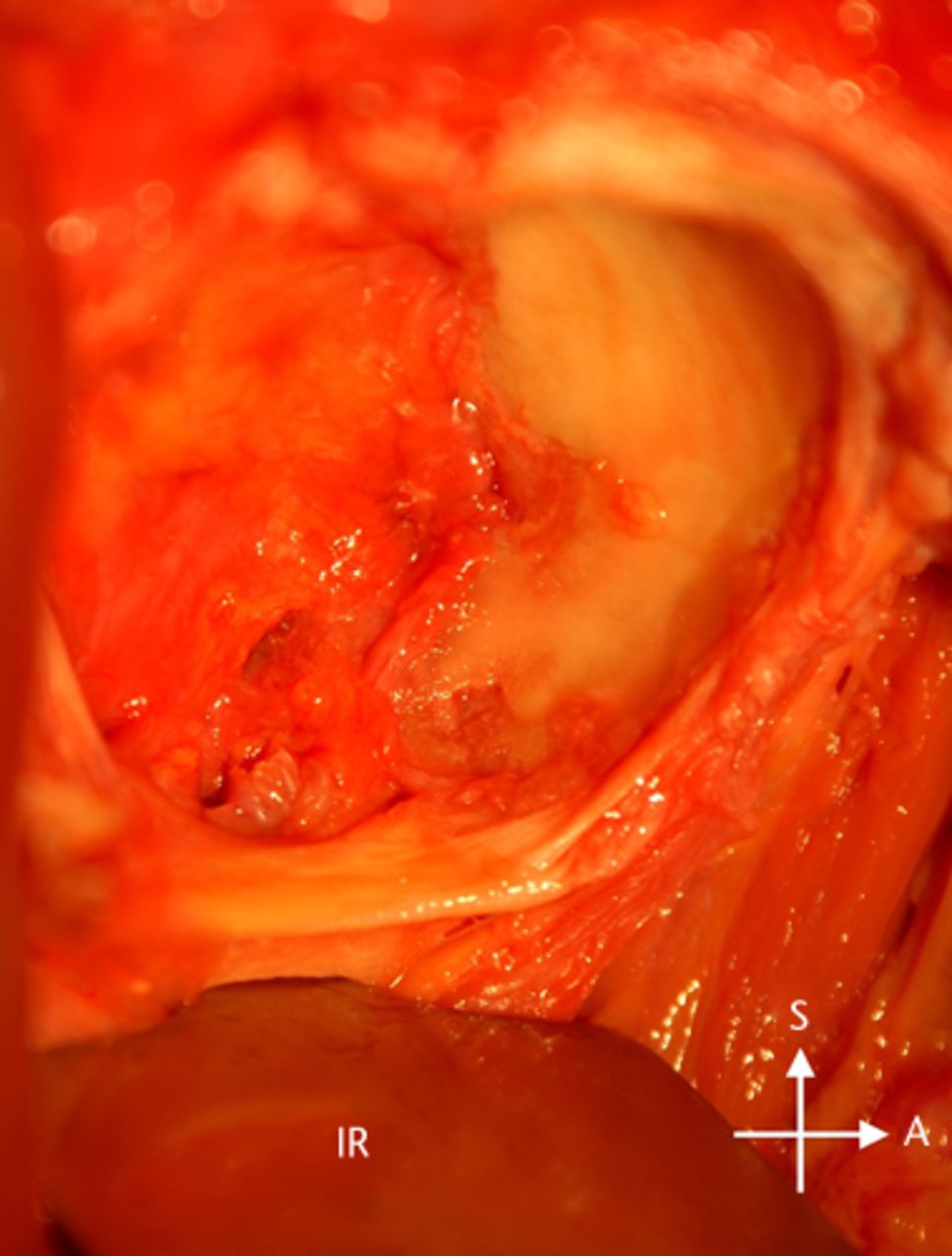
Fig. 2
Photograph showing the inferior retractor (IR) placed under the transverse acetabulum ligament, around the inferior wall of the acetabulum.
The femoral nerve was exposed following placement of the anterior retractor and its relationship to the tip of the retractor was examined. The path taken by the retractor to reach its final position was noted in relation to surrounding structures. Measurements were taken using calipers, by one observer, from the acetabular lip at the ‘three o’clock’ position, to the most posterior surface of the femoral nerve, as it passes over this point with the cadaver in the lateral operative position.
The obturator nerve was identified and its route through the pelvis examined. The route of the nerve outside the pelvis was not traced prior to retractor placement, in order to minimise disruption to the surrounding tissues, which could alter the route of the retractor. Following the placement of the Hohmann retractor inferiorly, the relationship between the tip of the retractor and the obturator nerve was examined. The extrapelvic route of the nerve was then identified with the retractor in situ. The anterior and posterior branches of the obturator nerve were defined, following their emergence through the obturator canal and their relationship to the body of the examined retractor.
Results
Anterior retractor
When the retractor was placed through the capsule and direct contact with the bony wall of the anterior acetabulum was maintained, the curved part of the retractor slid between the bulk of the iliopsoas and the acetabulum. The tip could be palpated directly under the femoral nerve, however, the bulk of the iliopsoas protected the femoral nerve from direct contact. If contact with the wall of the acetabulum was lost during placement, the retractor body passed either superficial to the iliopsoas or through the bulk of the iliopsoas muscle, resulting in the tip lying over the femoral nerve. When pressure was applied to the retractor handle to obtain adequate acetabular exposure, the tip compressed the femoral nerve, resulting in visible distortion of the nerve bundle (Fig. 3).
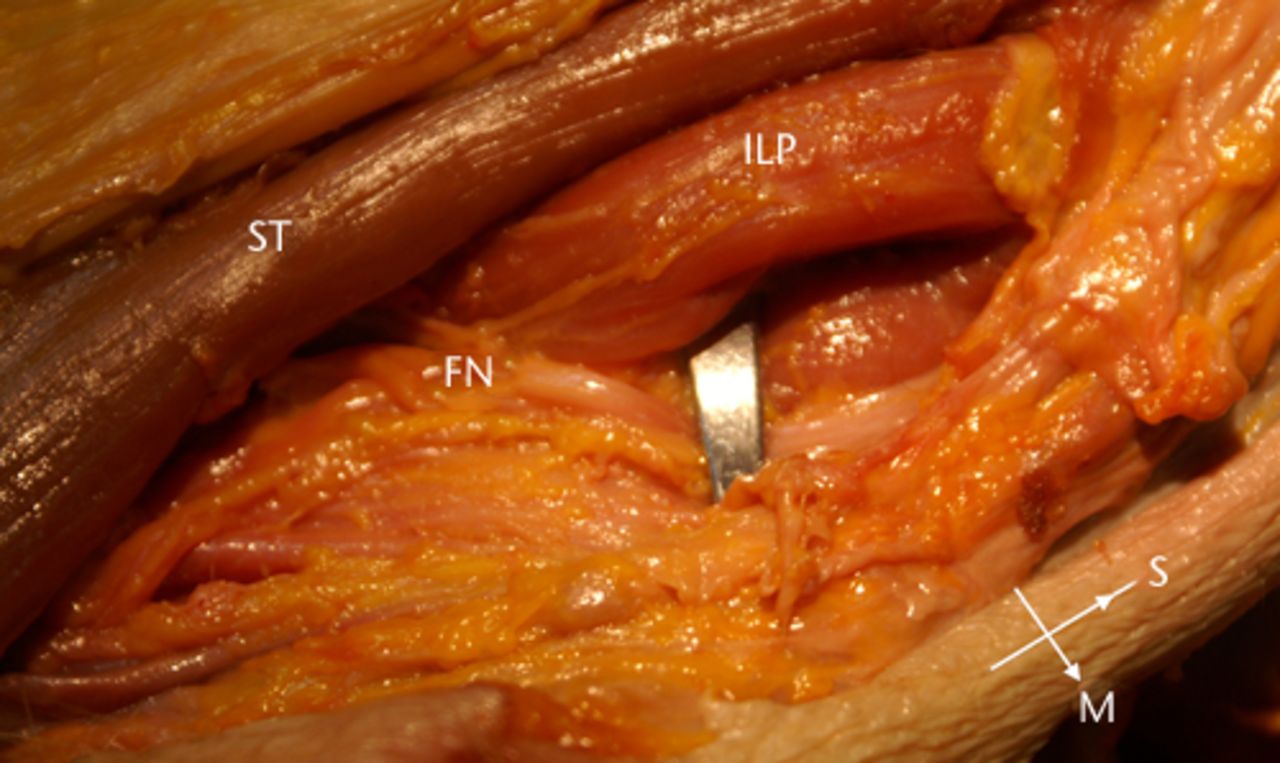
Fig. 3
Photograph of the anterior retractor compressing the femoral nerve (FN) as it passes through the femoral triangle, overlying the iliopsoas (ILP); ST, Sartorius.
When the retractor was placed correctly, with the body lying against the wall of the acetabulum and the femoral nerve protected, pressure was removed from the handle and then reapplied, without reinsertion of the retractor. The retractor pivoted on the anterior acetabular lip and the tip moved superficial to the iliopsoas, to lie directly above the femoral nerve. When the pressure was reapplied, the tip compressed the nerve bundle.
The tip of the large Hohmann retractor measures 3.5 cm. The mean distance between the anterior rim of the acetabulum and the most posterior aspect of the femoral nerve as it passes over this point is 1.8 cm (1.4 to 2.2). Therefore, should the retractor pass superficial to the iliopsoas, the femoral nerve is located within its path.
Inferior retractor
The tip of the inferior retractor was found to be within the pelvis during all placements of the inferior retractor. To reach this position, the retractor punctured the obturator externus, the obturator membrane and fibres of the obturator internus. The tip of the retractor was located medial to the obturator nerve in all specimens. When the retractor was pulled to gain exposure of the acetabulum, the tip moved laterally, and made direct contact with the obturator nerve, making it vulnerable to laceration by the sharp tip of the retractor (Fig. 4). The obturator vessels were also in contact with the retractor during this maneouvre. The extra-pelvic branches of the obturator nerve, the anterior and posterior divisions, were not in close proximity to the retractor following their emergence through the obturator canal. Both branches were observed to course medially, moving away from the body of the retractor.
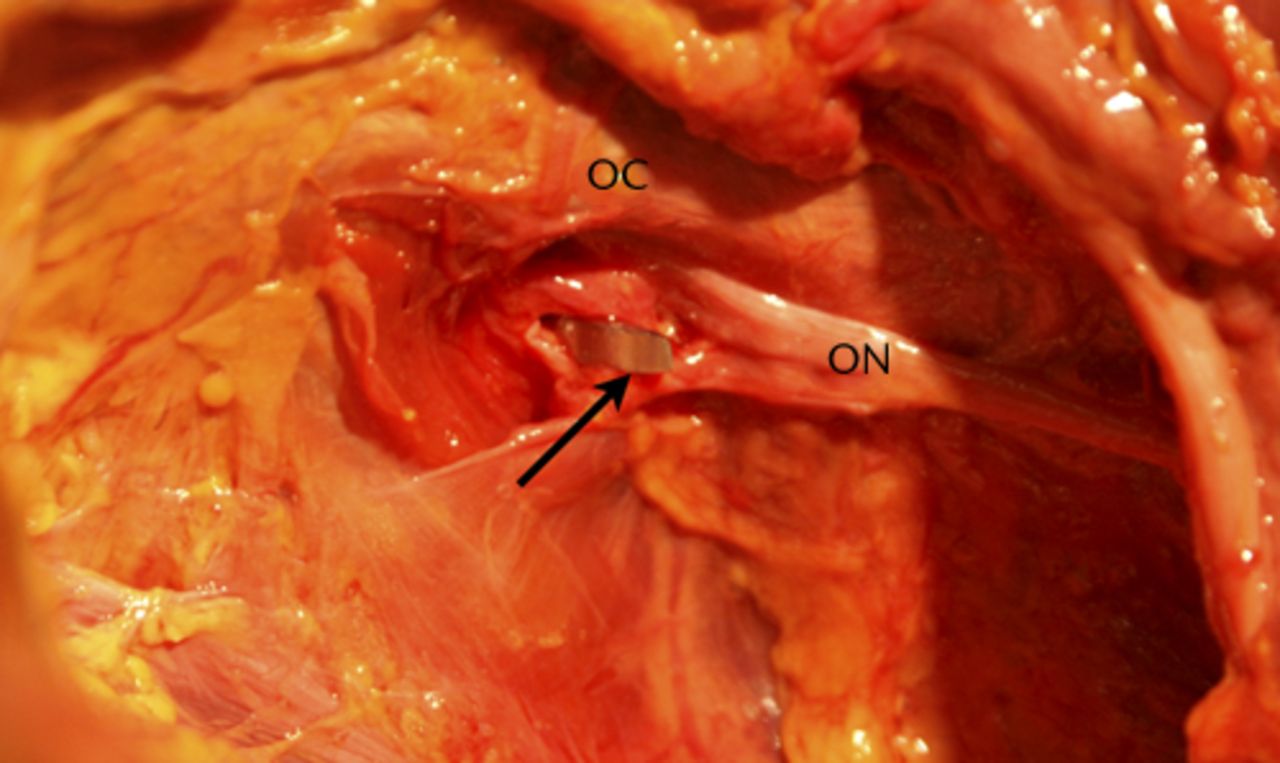
Fig. 4
Photograph showing the inferior retractor piercing the obturator membrane, lateral to the obturator nerve (ON) as it passes through the obturator canal (OC).
If the retractor was not fully in position, when pressure was applied to the retractor, with the body curving around the inferior acetabulum, the tip pierced the wall of the acetabular notch, lying in the fatty tissue within this space. In this position, neither the intra-pelvic nor extra-pelvic portions of the obturator nerve were at risk from direct injury.
Discussion
Nerve injury is a recognised complication of THR and in the majority of cases results in a poor functional outcome.1-6 Weale et al7 hypothesised that anterior and inferior retractors placed around the acetabulum were responsible for subclinical damage to the femoral and obturator nerves. The striking proximity of the acetabular retractors to these nerves demonstrated in this study supports this hypothesis and raises the strong possibility that the routine placement of acetabular retractors may play a significant role in the aetiology of nerve damage following THR.
The femoral nerve arises from the posterior division of the second to fourth lumbar ventral rami and enters the pelvis obliquely, through the fibres of the iliopsoas. As it passes distal to the inguinal ligament, it is closely related to the anterior wall of the acetabulum, passing on average 1.8 cm from the anterior lip, with only the bulk of iliopsoas lying in between. This anatomical relationship is similar to that highlighted by Davis et al,10 who reported a mean distance of 2.2 cm between the femoral nerve and the anterior capsule on MRI studies in healthy individuals.
It is in the region of the anterior acetabulum that the femoral nerve is at risk of direct injury from retractor placement. The iliopsoas muscle has been reported to offer a degree of protection to the femoral nerve from surgical instruments in this area.11,12 We have demonstrated that this protection is only conferred when the retractor passes deep to the iliopsoas, with very little, if indeed any, protection offered from direct injury if the retractor does not maintain contact with the bone of the anterior acetabular wall. This suggests that risk to the femoral nerve from direct trauma can be minimised when the anterior retractor lies between the iliopsoas and the bony wall of the anterior acetabulum. In order to achieve this position, the tip of the retractor must make contact with the anterior lip of the acetabulum, and this contact must be maintained when moving the retractor into position. Should pressure be removed from the retractor, as may occur if the assistant were to reach for another instrument, the retractor must be re-sited using the aforementioned principles. The removal of pressure allows the tip of the retractor to move superficial to the iliopsoas by pivoting on the anterior acetabular lip. When pressure is applied with the retractor in this position, the femoral nerve is crushed.
This position not only protects the femoral nerve from direct trauma, but also from damage due to compression at the level of the inguinal ligament. Heller et al12 demonstrated a reduction in pressure around the femoral nerve at the point where it passes below the inguinal ligament when the anterior retractor was placed in this manner. However, this position does not guarantee complete protection of the femoral nerve from compression, particularly when the nerve is distal to the inguinal ligament, within the femoral triangle. Slater et al13 illustrated that placement of the anterior acetabular retractor was the surgical maneouvre that resulted in the greatest pressure adjacent to the femoral nerve during THR.13 Therefore, although we have shown that the femoral nerve is protected from direct nerve trauma through correct placement of the anterior acetabular retractor, injuries due to nerve compression should not be discounted.
Injury of the nerve at this level clinically presents as quadriceps weakness with or without sensory loss over the anteromedial thigh and medial leg.14 Quadriceps weakness following THR is often overlooked, leading to a suspected under-reporting of femoral nerve injuries.15 The signs of femoral nerve palsy may also be masked by the use of post-operative rehabilitation aids, such as crutches, thus delaying the clinical diagnosis.16 With the demonstrated anatomical risk to the femoral nerve by the placement of an anterior acetabular retractor, a full clinical examination of both the motor and sensory function of the femoral nerve is essential, to allow for early diagnosis and the optimisation of post-operative rehabilitation strategies.
The obturator nerve arises from the ventral rami of L2, L3 and L4 spinal nerves. It travels around the lateral wall of the lesser pelvis to reach the obturator canal, where it leaves the pelvis and divides into the anterior and posterior branches. Cement extrusion with subsequent entrapment17 and perforation of the medial wall of the acetabulum by fixation screws placed in the anterior inferior quadrant are identified causes of obturator nerve damage in THR.18,19 The obturator nerve is vulnerable to injury by retractors as it exits the pelvis through the obturator canal, in the superolateral region of the obturator foramen. Damage in this area would be expected to result in a loss of cutaneous sensation over the medial thigh, with or without weakness of hip adduction. However, persistent and debilitating pain in the groin is often the only presenting feature.20 It is accepted that the diagnosis of obturator nerve palsy is difficult to make based on clinical examination alone,21 as testing adductor muscle function is unreliable and difficult, particularly in the early post-operative period.22 The diagnosis may be further complicated by anatomical variations in the obturator nerve. The nerve divides into the anterior and posterior divisions within the pelvis in 23% of the population, with the posterior branch lying most medially.23 Bearing in mind the demonstrated anatomical risk to the obturator nerve, a thorough examination of obturator nerve function, including cutaneous sensation, is essential in patients presenting with groin pain following hip replacement. Injury from retraction should be considered if other causes of obturator palsy, such as cement extrusion or fixation screws, are excluded.
This study does have certain limitations. Cadaveric tissue is not truly representative of that of a patient undergoing hip replacement. This was minimised by using fresh-frozen material to study retractor placement. This is closer in soft-tissue texture and mobility than fixed material, and is thus truer to the operative experience. The specimens used were all elderly at the time of death. Although this is consistent with the typical age range of patients undergoing hip replacement, young patients undergoing THR are more likely to have a larger muscle bulk surrounding the hip joint24 which could potentially impact on the route of the retractors around the acetabulum.
The acetabular wall has a direct impact on the correct placement of the retractors. During the surgical approach, no defects of the acetabulum were noted in any of the study specimens. However, not all patients undergoing THR will have an anatomically intact acetabulum, due either to congenital abnormalities or acquired pathology.5,25 Riouallan et al26 presented a case of femoral artery injury due to an anterior retractor placed on an acetabular wall with a large bony defect. Care should therefore be taken during retractor placement in cases where there is a known, or a high risk of, acetabular defect. Additionally, the prevalence of nerve injury is 2.5 times greater following revision procedures.5 This is likely due to anatomical distortion of the tissues and tethering of the nerve, rendering it immobile, suggesting that extra vigilance is required during both revision procedures, and in cases where pathological disruption of tissues is likely.
As the nature of the study was solely to focus on the anatomic relationships of retractors, it is not possible to determine the true clinical impact of these findings. However, bearing in mind that both femoral and obturator nerve injuries are under-reported, further work is warranted in order to elucidate the relationship between the demonstrated anatomical risk of the nerves and post-operative clinical outcomes. It was evident that vascular structures were also within the path of retractors. Further work is needed to examine the risk of direct injury to vascular structures by retractors in THR.
Conclusion
This study has provided anatomical evidence for the association between nerve compromise and retractor placement that has been previously highlighted in electrophysiological studies. Both the femoral and obturator nerves are at risk of direct damage through the routine placement of acetabular retractors during the posterior approach to the hip. This is particularly true if surgical access, and thus placement, is difficult during the procedure. We recommend that the anterior retractor should be removed and reinserted if pressure is removed intra-operatively, and vigorous movement of the inferior retractor should be avoided.
1 Farrell CM , SpringerBD, HaidukewychGJ, MorreyBE. Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg [Am]2005;87-A;2619-2625.CrossrefPubMed Google Scholar
2 Wilson JN , ScalesJT. The Stanmore metal on metal total hip prosthesis using a three pin type cup: A follow up of 100 arthroplasties over 9 years. Clin Orthop Relat Res1973;95:239–249. Google Scholar
3 Amstutz HC , MaSM, JumahRH, MaiL. Revision of aseptic loose total hip arthroplasties. Clin Orthop Relat Res1982;170;21-32.PubMed Google Scholar
4 Johanson NA , PellicciPM, TsairisP, SalvatiEA. Nerve injury in total hip arthroplasty,. Clin Orthop Relat Res1983;179:214–222.PubMed Google Scholar
5 Schmalzried TP , AmstutzHC, DoreyFJ. Nerve palsy associated with total hip replacement: Risk factors and prognosis. J Bone Joint Surg [Am]1991;73-A:1074–1080. Google Scholar
6 Oldenburg M , MullerRT. The frequency, prognosis and significance of nerve injuries in total hip arthroplasty. Int Orthop1997;21:1–3.CrossrefPubMed Google Scholar
7 Weale AE , NewmanP, FergussonIT, BannisterGC. Nerve injury after posterior and direct lateral approaches for hip replacement: A clinical and electrophysiological study. J Bone Joint Surg [Br]1996;78-B:899–902. Google Scholar
8 Weber ER , DaubeJR, CoventryMB. Peripheral neuropathies associated with total hip arthroplasty. J Bone Joint Surg [Am]1976;58-A:66–69.PubMed Google Scholar
9 Lewallen DG . Neurovascular Injury Associated with Hip Arthroplasty - Instructional Course Lectures, The American Academy of Orthopaedic Surgeons. J Bone Joint Surg [Am]1997;79-A:1870–1880. Google Scholar
10 Davis ET , GalliePA, JamesSL, WaddellJP, SchemitschEH. Proximity of the femoral neurovascular bundle during hip resurfacing. J Arthroplasty2010;25:471–474.CrossrefPubMed Google Scholar
11 Simmons C , IzantTH, RothmanRH, BoothRE, BalderstonRA. Femoral neuropathy following total hip arthroplasty. J Arthroplasty1991;6:S59–S66.PubMed Google Scholar
12 Heller KD , PrescherA, BirnbaumK, ForstR. Femoral nerve lesion in total hip replacement: an experimental study. Arch Orthop Trauma Surg1998;117:153–155.CrossrefPubMed Google Scholar
13 Slater N , SinghR, SenasingheN, et al.Pressure monitoring of the femoral nerve during total hip arthroplasty: an explanation for iatropathic palsy. J R Coll Surg Edin2000;45:231–233. Google Scholar
14 Kim DH , MurovicJA, TielRL, KlineDG. Intrapelvic and thigh-level femoral nerve lesions: management and outcomes in 119 surgically treated cases. J Neurosurgery2004;100:989–996.CrossrefPubMed Google Scholar
15 Uskova AA , PlakseychukA, ChellyJE. The role of surgery in postoperative nerve injuries following total hip replacement. J Clin Anaesth2010;22:285–293.CrossrefPubMed Google Scholar
16 Goldberg G , GoldsteinH. AAEM Case Report: Nerve injury associated with hip arthroplasty. Muscle Nerve1998;21:519–527. Google Scholar
17 Mahadevan D , ChallandC, KeenanJ. Cement extrusion during hip arthroplasty causing pain and obturator nerve impingement. J Arthroplasty2009;24:158–160.CrossrefPubMed Google Scholar
18 Fricker RM , TroegerH, PfeifferKM. Obturator nerve palsy due to fixation of an acetabular ring with transacetabular screws: A case report. J Bone Joint Surg [Am]1997;79-A:444–446. Google Scholar
19 Wasielewski RC , CoopersteinLA, KrugerMP, RubashHE. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg [Am]1990;72-A:501–508.PubMed Google Scholar
20 Siliski JM , ScottRD. Obturator nerve palsy resulting from intrapelvic extrusion of cement during total hip replacement: Report of four cases. J Bone Joint Surg [Am]1985;67-A:1225–1228. Google Scholar
21 Kitagawa R , KimD, ReidN, KlineD. Surgical management of obturator nerve lesions. Neurosurgery2009;65:A24–A28.CrossrefPubMed Google Scholar
22 Fowble VA , SchmalzriedTP. Nerve palsy associated with total hip arthroplasty. Semin Arthro2005;16:114–118. Google Scholar
23 Anagnostopoulou S , KostopanagiotouG, ParaskeuopoulosT, et al.Anatomic variations of the obturator nerve in the inguinal region: implications in conventional and ultrasound regional anaesthesia techniques. Reg Anaesth Pain Med2009;34:33–39. Google Scholar
24 Kirkendall DT , GarrettWE. The effects of ageing and training on skeletal muscle. Am J Sports Med1998;26:598–602. Google Scholar
25 Romness DW , LewallenDG. Total hip arthroplasty after fracture of the acetabulum: long term results. J Bone Joint Surg [Br]1990;72-B:761–764. Google Scholar
26 Riouallon G , ZilberS, AllainJ. Common femoral artery intimal injury following total hip replacement: a case report and literature review. Ortho Traumatol Surg Res2009;95:154–158. Google Scholar
Funding statement:
None declared
Author contributions:
F. A. McConaghie: Conducting the research, Writing the paper
A. P. Payne: Supervising the research
A. W. G. Kinninmonth: Conducting the research, Writing the paper
ICMJE Conflict of Interest:
None declared
©2014 The British Editorial Society of Bone & Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










