Abstract
Objectives
To review the current best surgical practice and detail a multi-disciplinary approach that could further reduce joint replacement infection.
Methods
Review of relevant literature indexed in PubMed.
Results
Surgical site infection is a major complication following arthroplasty. Despite its rarity in contemporary orthopaedic practice, it remains difficult to treat and is costly in terms of both patient morbidity and long-term health care resources.
Conclusions
Emphasis on education of patients and all members of the health-care team and raising awareness in how to participate in preventative efforts is imperative.
Article focus
This article reviews the evidence for methods of reducing surgical site infection in joint replacement
We describe a multidisciplinary approach to prevent surgical site infection
Key messages
Surgical site infection in arthroplasty is potentially a devastating complication
There are many factors that contribute to cause surgical site infections
A multidisciplinary approach can reduce infection rates
Strengths and limitations
Strengths: this review of the current literature provides the reader with a concise summary of evidence-based advice with which to make an informed decision on how to best prevent surgical site infections in lower limb arthroplasty using a multidisciplinary approach
Limitations: there are gaps in knowledge that require further research
Introduction
Joint replacement is safe and cost effective.1 Prosthetic infection is a major, but infrequent, complication with a risk of between 0.54% and 0.63% in England.2 Revision of infected implants is associated with substantial morbidity and economic cost.3-5 Surgical site infection (SSI) is multifactorial, involving patient, surgical and environmental factors. This paper reviews the current best surgical practice and describes how a multi-disciplinary approach can reduce peri-operative joint infection.
Surgical site infection
SSI is present when pathogenic organisms multiply in a wound causing local signs and symptoms, and eventually a systemic inflammatory response. Figure 1 shows the common pathogenic organisms responsible for orthopaedic SSIs.6 Infection rates increase with a greater number of patient or surgery specific risk factors7,8 (Table I).
Table I
Methods for reducing surgical site infection in joint replacement
| Risk factor | Summary* |
|---|---|
| Patient factors | |
| Diabetes mellitus | Aggressive glucose control |
| Rheumatoid arthritis | DMARDs and methotrexate should not be stopped |
| Peri-operative steroids are generally not required | |
| Balance the risks and benefits of stopping anti-TNF – stop at 3 to 5 half-lives pre-operative, restart after wound healing and no evidence of infection | |
| Nitrous oxide should be avoided in patients on methotrexate | |
| Obesity | Dietician input to encourage weight loss |
| Adjust peri-operative antibiotic doses appropriately | |
| In extremely obese consider bariatric surgery before surgery | |
| Smoking | Consider a smoking cessation programme |
| Carrier screening | MRSA and MSSA screening based on local guidelines, and decolonise before admission |
| Pre-operative factors | |
| Patient preparation | Shower on day of surgery |
| If shaving required, use electric clippers on day of surgery | |
| Avoid oil-based skin moisturisers | |
| Antibiotics | Prophylactic antibiotics should be given as early as possible in the anaesthetic room, and continued for 24 hours post-operatively (antibiotic type dependent on local guidelines) |
| Administer antibiotics at least 5 minutes before tourniquet inflation | |
| If cementation is required, antibiotic-impregnated should be used | |
| Peri-operative factors | |
| Theatre | Use laminar flow where possible |
| Keep theatre door opening to a minimum | |
| Personnel | Hand wash with antiseptic surgical solution, using a single-use brush or pick for the nails |
| Before subsequent operations hands should be washed with either an alcoholic hand rub or an antiseptic surgical solution | |
| Double glove and change gloves regularly | |
| Polyprophylene non-woven gowns with adequate mask and hat coverage | |
| Skin preparation | Use an alcohol pre-wash followed by a 2% chlorhexadine-alcohol scrub solution |
| Anaesthetic | Maintain normothermia |
| Maintain normovolaemia | |
| A higher inspired oxygen concentration peri-operatively and for 6 hours post-operative may be of benefit | |
| Drapes | Use of iodine-impregnated incise drapes may be of benefit (in patients without allergy) |
| Blood transfusion | Optimise pre-operative haemoglobin |
| If possible, transfusion should be avoided intra-operatively and if anticipated should be given more than 48 hours before surgery | |
| Antifibrinolytics may indirectly reduce SSI by reducing the need for transfusion | |
| Post-operative factors | |
| Dental procedures | Insufficient evidence to recommend the use of prophylactic antibiotics for patients undergoing routine dental procedures following joint replacement |
-
* DMARDs, disease-modifying anti-rheumatic drugs; TNF, tumour necrosis factor; MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-sensitive S. aureus; SSI, surgical site infection
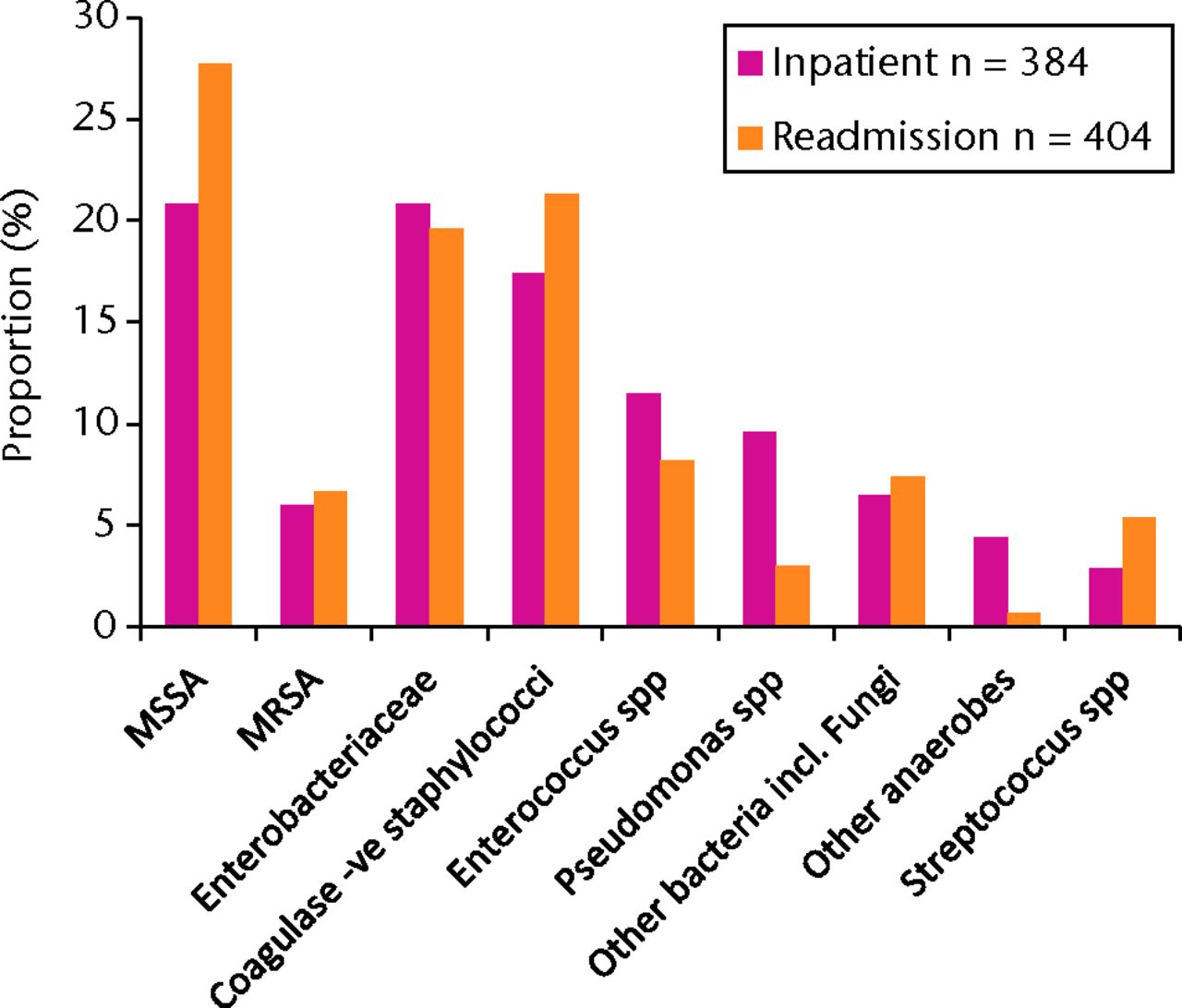
Fig. 1
Bar chart showing the distribution of micro-organisms reported as causing surgical site infections (SSIs) in mandatory orthopaedic categories, England, 2011/12 (MSSA, methicillin-sensitive Staphylococcus aureus; MRSA, methicillin-resistant S. aureus; -ve, negative; ‘Other bacteria’, mostly comprising isolates reported as ‘unspecified diphtheroids’, corynebacterium spp. and ‘other gram-positive organisms’). Adapted with permission from the Health Protection Agency.6
Modifiable patient risk factors
Patient-related factors, such as diabetes mellitus (DM) and rheumatoid arthritis (RA), are modifiable and certain aspects of management can be optimised to reduce infection.
Diabetes mellitus
Wound infection has been shown to be more common in patients with diabetes after arthroplasty, and in non-diabetic patients who developed transient post-operative hyperglycaemia.9 Hyperglycaemia is associated with increased monocyte susceptibility to apoptosis10 and impaired neutrophil function (impaired chemotactic, phagocytic and bactericidal capability).11 Blood glucose levels > 11.1 mmol/l are associated with SSIs in cardiac surgery,12 and in general surgical patients, immediate post-operative hyperglycaemia is associated with SSI.13 The potential to improve in vivo neutrophil phagocytic function by aggressive glucose control (using infusion delivery) has also been demonstrated in cardiopulmonary bypass patients.14
Rheumatoid arthritis
RA is an independent risk factor for infection in arthroplasty, but also for revision and subsequent re-infection; pertinent given that these patients often present earlier for arthroplasty.
Local and systemic corticosteroids have been shown to delay wound-healing, increase the risk of wound infection and cause adrenal insufficiency.15 A recent Cochrane review has questioned the historical practice of providing long-term users with additional peri-operative steroids (which may amplify immunosuppression at time of surgery).16
Although disease-modifying anti-rheumatic drugs (DMARDs) increase the risk of prosthetic joint infection,8 the British Society for Rheumatology (BSR) guidelines suggest that in most cases these should not be stopped before joint replacement.17 Methotrexate is a commonly used first-line drug18 and, despite its inclusion within the DMARD group, is not considered to increase wound infection risk, and should not be discontinued before orthopaedic surgery.19 However, nitrous oxide should be excluded from the anaesthetic regimen as the interaction can induce immuno-suppression.20
Tumour necrosis factor (TNF)-α is an inflammatory cytokine (highly concentrated in the synovial tissue of RA patients) implicated in joint destruction.21 Any increase in risk of infection in patients who received anti-TNF therapy before surgery is debatable.22,23 The BSR state that the potential benefit of preventing post-operative infections (by stopping treatment) should be balanced against the risk of a peri-operative disease flare. If anti-TNF therapy is to be withheld, it should be discontinued between five and 20 days before surgery (three to five times the half-life of the drug), restarting when there is good wound healing and no evidence of infection.24
Obesity
The effect of obesity on SSI, defined as a body mass index (BMI) ≥ 30 kg/m2,25 is well documented.26 In a prospective study of over 2800 knee and hip replacements, Namba et al27 found that the odds ratio was between 4.2 and 6.7 times the risk for infection in obese total knee and hip patients, respectively, compared with non-obese patients. Increased length and complexity of surgery, and poorer vascularisation of the subcutaneous layer may contribute to this elevated risk. Obese patients also require a significantly higher fraction of inspired oxygen (FIO2) to reach an adequate arterial oxygen level.28 Referral to a dietician may be necessary. In extremely obese patients (≥ 50 kg/m2), bariatric surgery may be indicated. In patients undergoing both bariatric surgery and lower limb arthroplasty, the rate of wound infection was 3.5 times lower in patients who had bariatric surgery first.29 Communication with the anaesthetist is recommended in order to evaluate the risk and to discuss increased doses of peri-operative antibiotics.30
Smoking
Smoking is associated with impaired wound healing and infection.31 Patients randomised to a cessation programme six to eight weeks before arthroplasty surgery had significantly fewer wound complications (5% versus 31%), shorter length of stay, fewer re-operations and non-quantified cardiovascular benefits compared with those who had continued smoking.32
Screening and decolonisation
The costs associated with treatment of infections due to methicillin-resistant organisms are 1.5 times higher compared with sensitive organisms.33 A methicillin-resistant Staphylococcus aureus (MRSA) screening programme for all planned NHS surgery was implemented in April 2009,34 with a positive result prompting decolonisation before admission.
Nasal carriers of methicillin-sensitive S. aureus (MSSA) also have an increased risk of infection. In a large, randomised multicentre trial, the risk of developing hospital-associated S. aureus infection in MSSA-carrier patients who were decolonised on admission to hospital (mupirocin nasal ointment and chlorhexidine soap) fell by nearly 60% compared with placebo – a significant reduction from 7.7% to 3.4%.35 Nasal carriage of MSSA is common (approximately 20%35), and United Kingdom hospitals are beginning to decolonise patient carriers before joint replacement.
Pre-operative phase surgical risk factors
Patient preparation before theatre
Patients should shower with soap on the morning of surgery.36 Washing with an antiseptic reduces skin bacteria (microflora), but there is little evidence of a reduction in risk of SSI.37,38 Dry shaving with a razor may irritate the skin and increase the bacterial count, so if hair removal is necessary, electric clippers or depilatory creams on the day of surgery are favoured.36,39
Type of antibiotic prophylaxis
The role of parenteral prophylactic antibiotics has been studied and accepted across most surgical specialties,40,41 and may be the single most important factor in the prevention of deep wound infection following lower limb arthroplasty.42
Although many different groups of antibiotics can be used for prophylaxis, there is insufficient evidence of a significant difference in the efficacy of cephalosporins, teicoplanin or penicillin-derivatives, or a benefit of one generation of cephalosporins over another.43 Cephalosporin use has been associated with Clostridium difficile colitis, especially in the elderly, but rates are low after joint replacement (1.7 per 1000 replacements).44
Aminoglycosides, such as gentamicin, can be administered locally (in the cement) or parenterally. In a review of 15 000 primary total hip replacements from the Norwegian Arthroplasty Register, the lowest risk of revision was found in patients who received both systemic and local (in cement) antibiotics.45
Timing of antibiotic prophylaxis
The United Kingdom National Institute of Health and Clinical Excellence (NICE) recommends a single intravenous dose of antibiotic prophylaxis on starting anaesthesia, with a repeat dose if the operation is longer than the half-life of the antibiotic, or if blood loss is a significant.46,47 The American Academy of Orthopaedic Surgeons (AAOS) state that the administration of antibiotic should precede the skin incision by one hour, and duration of prophylaxis should not exceed 24 hours.48 Rates of infection have been found to be lowest for patients who received an antibiotic within two hours of the incision,40 and there was no difference between one- and three-day courses of prophylactic antibiotics in terms of deep-infection rate.49 It would seem prudent to give antibiotics as early as possible in the anaesthetic room, well before (at least 5 minutes) tourniquet inflation limits any further rise in tissue antibiotic concentration.50
Peri-operative phase surgical risk factors
Theatre etiquette
The World Health Organization recommends that all surgical staff should keep doors to the operating room closed, except as needed for the passage of equipment, personnel and the patient.51 Staff should store essential equipment in the operating room to decrease theatre traffic.51 Frequency of theatre door-opening is a positive predictor of raised bacterial counts.52
Alcohol rub used in preparation for surgery may be as effective as hand scrubbing in preventing SSIs.53 There is no evidence to suggest that any particular alcohol rub is better than another.54,55
Surgical site preparation in theatre
Skin moisturisers appear to inhibit the ability of aqueous preparations to decolonise the skin, and may increase skin bacteria counts. Avoidance of oil based moisturisers and de-greasing with alcohol pre-wash is recommended.56
A randomised trial of 849 patients undergoing clean-contaminated surgery in which pre-operative skin preparation was performed with either 2% chlorhexidine-alcohol or aqueous povidone-iodine and paint found that the rate of SSI was significantly lower in the chlorhexidine-alcohol group.57
Theatre design
Airborne contaminants are the largest single contributor to infection.58 One billion skin cells are shed daily per person,59 with up to 10% carrying bacteria.60 For orthopaedic surgery, laminar-flow ventilation systems have been advocated,61 although they are not in universal use. These employ high-efficiency particulate air filters where particles larger than 0.3 µm are removed (5 µm for conventional theatres). Ultra-clean air has reduced bacterial and particle concentrations.62 Ultraclean air and prophylactic antibiotics have independent and additive effects on reducing infections after joint arthroplasty.63 There is no dispute that the air within an effective laminar flow theatre is extremely clean. However, Brandt et al64 found laminar flow to have no protective effect against SSI in 99 230 patients. When 88 311 arthroplasty patients from the New Zealand joint registry were analysed, revision rates for deep infection were significantly higher in laminar flow theatres, despite adjustment for other known variables.65 As a result of these findings, the authors questioned the routine use of laminar air flow in arthroplasty, feeling that the added expense to the health service was not justified.65 Before abandoning laminar flow, the interaction with forced air warming should be examined. A recent study demonstrated that air from outside the canopy may be drawn into the surgical wound area when forced air warming (FAW) devices are used, and deep infection rates were reduced when FAW was abandoned in favour of contemporary conductive fabric warming in joint replacement.66
Operating personnel clothing
NICE recommends double gloving in arthroplasty surgery.46,67 Glove perforation increases the risk of transmission of blood-borne diseases and breaks the asepsis barrier, potentially allowing contamination of the wound and thus increasing the risk of infection.68,69 Studies have shown that use of a blunt needle compared with a sharp needle during surgery reduces glove perforation rates significantly.70,71 Most perforations are unnoticed (61.5%) and are caused by shearing rather than penetration by sharps.68 A Cochrane systematic review supported the use of double gloving, despite no evidence of a reduction in SSI.72 Glove changing at regular intervals is an effective way to decrease the length of exposure to bacterial contamination during total hip replacement.69 Latex-free gloves have significantly higher perforation rates when compared with latex gloves.73
Hooper et al,65 in their ten-year New Zealand joint registry study, found that the rate of revision for early deep infection had not been reduced by space suits compared with a normal theatre gown and mask, when analysed independently of laminar flow.
Surgical drapes
NICE recommend an incise drape impregnated with iodophore should be used unless the patient has an iodine allergy.46 Although a Cochrane review concluded that these drapes did not make any difference to infection rates,74 only one trial involved orthopaedic surgery, which showed no difference in post-operative wound infection rates following hip fracture surgery with or without non-impregnated Opsite (Smith & Nephew Wound Management, Hull, United Kingdom).75
Body core temperature
Peri-operative hypothermia is common during major surgery and causes vasoconstriction, resulting in a reduction in subcutaneous tissue perfusion and an increased risk of infection.76 Peri-operative hypothermia is associated with increased blood loss, cardiac events, increased transfusion requirements and longer peri-operative hospital stay.77 Heat loss in theatre is largely conductive and convective, with a small amount of radiated heat. Laminar flow significantly increases convective heat loss in exposed patients, mitigated by active warming.
Warming patients undergoing clean general surgery significantly reduces wound infection.78 A similar report of cholecystectomy patients found nearly a six-fold difference in the incidence of wound infection between normothermic and hypothermic patients.79 The importance of maintaining peri-operative normothermia has been recognised in the recent NICE guidelines.80 However, it is notable that warming has never been proven to reduce SSIs in orthopaedic implant surgery, and their effect on laminar flow and clean air needs further study.
Oxygen delivery and fluid management
Increasing tissue oxygen concentrations has been hypothesised to increase the killing potential of phagocytes and thus decrease infective complications in the peri-operative period.81 Enhancement of tissue oxygen delivery can be achieved via improvement of cardiac output and/or oxygen content of the blood. Increased subcutaneous oxygen concentrations can be achieved by increasing the inspired oxygen concentration intra-operatively (from 30% to 80%), and by providing supplemental oxygen post-operatively. There are studies supporting the use of supplemental oxygen to reduce wound infections in general surgery, but these have never been extrapolated to arthroplasty surgery.82-84
Both hypovolaemia and hypervolaemia (oedema) can be detrimental to tissue oxygenation. Current guidance would support optimal tissue oxygenation by maintenance of a normovolaemic state throughout the peri- and early post-operative period by judicious use of intravenous fluids.85,86
Anaesthetic technique
The question of whether regional anaesthesia is superior to general anaesthesia has yet to be adequately assessed, although a recent retrospective population based study found a significantly lower 30-day rate of SSI in patients undergoing lower limb arthroplasty under a spinal anaesthetic compared with patients undergoing similar procedures under general anaesthetic.87 An RCT examining the potentially beneficial effect of nitrous oxide avoidance failed to show a reduction in SSI. Co-administered anaesthetic and sedative agents may impair immune responses directly, thereby increasing infection,88 and regional anaesthesia may offer particular benefits such as improved tissue oxygen delivery (through vasodilation). Randomised controlled trials are required to address whether choice of agent (such as use of an alpha-2 adrenergic versus GABAergic sedative) affects outcome.88,89
Anaemia
In a prospective cohort study pre-operative anaemia was associated with increased post-operative infections in patients undergoing hip arthroplasty.90 This effect was associated with an increase in post-operative blood transfusion.
Blood transfusion
There are no specific recommendations from NICE regarding transfusions. Though it is clear that blood loss is primarily a surgical responsibility, regional anaesthetic techniques and attention to peri-operative normothermia are associated with reduced blood loss. Transfusion related immunomodulation is recognised in trauma patients91 with a 5% increase risk of infection for every unit of red cells given.92 A significant increase in infection rates following hip replacement are seen in patients receiving allogeneic red blood cells, with higher risk with more units transfused.93 There is clearly a risk-benefit balance between immunosuppression and enhancing oxygen supply to hypoperfused tissue. If possible, blood transfusion should be avoided intra-operatively94 and, if anticipated, should be administered at least 48 hours before surgery to maximise oxygen transportation of transfused blood. Addressing pre-operative anaemia reduces post-operative transfusion requirements.
The use of antifibrinolytics, such as tranexamic acid, prevent blood loss following major arthroplasty.95 Although there is insufficient data to comment on their ability to prevent post-operative infection, they may indirectly reduce the risk by reducing transfusion requirement and improving the wound environment.
Post-operative period
Thromboembolic prophylaxis
NICE guidelines state that patients undergoing lower limb joint replacements should have either prophylactic low-molecular-weight heparin (LMWH) or an orally active direct factor Xa inhibitor for 28 (or 35) days following hip replacement and 14 days following a knee replacement.96 No increased risk of infection was found with LMWH97 but prolonged ooze is a recognised risk,98 and each day of prolonged wound drainage increases risk of wound infection by between 29% and 42% following arthroplasty.98 Wound related complications following arthroplasty may increase in patients who receive a factor Xa inhibitor for thromboprophylaxis.99
Dental care and other procedures
It has been suggested that patients requiring dental care post-arthroplasty should receive prophylactic antibiotics.100 Other authors argue that there is little evidence to suggest that bacteraemia associated with dental procedures causes prosthetic joint infection101; simple tasks, such as brushing teeth and chewing, can produce a greater bacteraemia than one dental procedure and it would be better practice for the surgeon to ensure dentition and oral health are up to standard before elective orthopaedic surgery. Currently in the United Kingdom, the British Dental Association does not recommend antibiotics in patients undergoing dental procedures and who are at risk of infective endocarditis.102
Conclusions
SSI following routine surgery can have disastrous consequences for the patients and causes a significant drain on the resources of healthcare providers. A multidisciplinary approach is essential in order to reduce infection rates. Every possible step must be exercised to reduce contamination of the surgical wound and to optimise the patient’s capacity to eradicate any colony forming units entering the wound. Common sense approaches are required to minimise or correct physiological disturbances and attention should be given to theatre design and etiquette, identification and control of MSSA carriers and the appropriate and timely use of prophylactic antibiotics. It is important to emphasise the need to educate the patient and all members of the health-care team, and to increase awareness of the importance of their participation in preventive efforts.
1 Ethgen O , BruyèreO, RichyF, DardennesC, ReginsterJY. Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Joint Surg [Am]2004;86-A(5):963–974. Google Scholar
2 Health Protection Agency. Sixth report of the mandatory surveillance of surgical site infection in orthopaedic surgery, 2011. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1287147699571 (date last accessed 7 January 2013). Google Scholar
3 Darouiche RO . Treatment of infections associated with surgical implants. N Engl J Med2004;350:1422–1429.CrossrefPubMed Google Scholar
4 Edwards C , CounsellA, BoultonC, MoranCG. Early infection after hip fracture surgery: risk factors, costs and outcome. J Bone Joint Surg [Br]2008;90-B:770–777.CrossrefPubMed Google Scholar
5 Bozic KJ , RiesMD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg [Am]2005;87-A:1746–1751.CrossrefPubMed Google Scholar
6 Health Protection Agency. Surveillance of surgical site infections in NHS hospitals in England 2011/2012. http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1317137334452 (date last accessed 18 March 2013). Google Scholar
7 Gurkan I , WenzJF. Perioperative infection control: an update for patient safety in orthopedic surgery. Orthopedics2006;29:329–339.CrossrefPubMed Google Scholar
8 Moucha CS , ClyburnT, EvansRP, ProkuskiL. Modifiable risk factors for surgical site infection. J Bone Joint Surg [Am]2011;93-A:398–404.PubMed Google Scholar
9 Mraovic B , DonghunS, JacovidesC, ParviziJ. Perioperative hyperglycemia and postoperative infection after lower limb arthroplasty. J Diabetes Sci Technol2011;5:413–418.CrossrefPubMed Google Scholar
10 Komura T , SakaiY, HondaM, et al.CD14+ monocytes are vulnerable and functionally impaired under endoplasmic reticulum stress in patients with type 2 diabetes. Diabetes2010;59:634–643.CrossrefPubMed Google Scholar
11 Turina M , FryDE, PolkHC Jr. Acute hyperglycemia and the innate immune system: clinical, cellular, and molecular aspects. Crit Care Med2005;33:1624–1633.CrossrefPubMed Google Scholar
12 Golden SH , Peart-VigilanceC, KaoWH, BrancatiFL. Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care1999;22:1408–1414.CrossrefPubMed Google Scholar
13 Ata A , LeeJ, BestleSL, DesemoneJ, StainSC. Postoperative hyperglycemia and surgical site infection in general surgery patients. Arch Surg2010;145:858–864.CrossrefPubMed Google Scholar
14 Rassias AJ , MarrinCA, ArrudaJ, et al.Insulin infusion improves neutrophil function in diabetic cardiac surgery patients. Anesth Analg1999;88:1011–1016.CrossrefPubMed Google Scholar
15 Wicke C , HallidayB, AllenD, et al.Effects of steroids and retinoids on wound healing. Arch Surg2000;135:1265–1270.CrossrefPubMed Google Scholar
16 Yong SL , MarikP, EspositoM, CoulthardP. Supplemental perioperative steroids for surgical patients with adrenal insufficiency. Cochrane Database Syst Rev2009;4:CD005367.CrossrefPubMed Google Scholar
17 Luqmani R , HennellS, EstrachC, et al.British Society for Rheumatology and British Health Professionals in Rheumatology guideline for the management of rheumatoid arthritis (after the first 2 years). Rheumatology (Oxford)2009;48:436–439.CrossrefPubMed Google Scholar
18 Kameda H , KanbeK, SatoE, et al.Continuation of methotrexate resulted in better clinical and radiographic outcomes than discontinuation upon starting etanercept in patients with rheumatoid arthritis: 52-week results from the JESMR study. J Rheumatol2011;38:1585–1592.CrossrefPubMed Google Scholar
19 Grennan DM , GrayJ, LoudonJ, FearS. Methotrexate and early postoperative complications in patients with rheumatoid arthritis undergoing elective orthopaedic surgery. Ann Rheum Dis2001;60:214–217.CrossrefPubMed Google Scholar
20 Sanders RD , WeimannJ, MazeM. Biologic effects of nitrous oxide: a mechanistic and toxicologic review. Anesthesiology2008;109:707–722.CrossrefPubMed Google Scholar
21 Choy EH , PanayiGS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med2001;344:907–916.CrossrefPubMed Google Scholar
22 Dixon WG LM , WatsonKD, HyrichKL, SymmonsDP. Anti-TNF therapy and the risk of serious post-operative infection: results from the BSR Biologics register (BSRBR). Ann Rheum Dis2007;66(Suppl II):118. Google Scholar
23 Bibbo C , GoldbergJW. Infectious and healing complications after elective orthopaedic foot and ankle surgery during tumor necrosis factor-alpha inhibition therapy. Foot Ankle Int2004;25:331–335.CrossrefPubMed Google Scholar
24 Ding T , LedinghamJ, LuqmaniR, et al.BSR and BHPR rheumatoid arthritis guidelines on safety of anti-TNF therapies. Rheumatology (Oxford)2010;49:2217–2219.CrossrefPubMed Google Scholar
25 World Health Organization. Obesity and overweight factsheet. http://www.who.int/mediacentre/factsheets/fs311/en/ (date last accessed 18 March 2013). Google Scholar
26 Dowsey MM , ChoongPF. Early outcomes and complications following joint arthroplasty in obese patients: a review of the published reports. ANZ J Surg2008;78:439–444.CrossrefPubMed Google Scholar
27 Namba RS , PaxtonL, FithianDC, StoneML. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty2005;20(Suppl 3):46–50.CrossrefPubMed Google Scholar
28 Fleischmann E , KurzA, NiedermayrM, et al.Tissue oxygenation in obese and non-obese patients during laparoscopy. Obes Surg2005;15:813–819.CrossrefPubMed Google Scholar
29 Kulkarni A , JamesonSS, JamesP, WoodcockS, MullerS, ReedMR. Does bariatric surgery prior to lower limb joint replacement reduce complications?Surgeon2011;9:18–21.CrossrefPubMed Google Scholar
30 Freeman JT , AndersonDJ, HartwigMG, SextonDJ. Surgical site infections following bariatric surgery in community hospitals: a weighty concern?Obes Surg2011;21:836–840.CrossrefPubMed Google Scholar
31 Kwiatkowski TC , HanleyEN Jr, RampWK. Cigarette smoking and its orthopedic consequences. Am J Orthop (Belle Mead NJ)1996;25:590–597.PubMed Google Scholar
32 Moller AM , VillebroN, PedersenT, TonnesenH. Effect of preoperative smoking intervention on postoperative complications: a randomised clinical trial. Lancet2002;359:114–117.CrossrefPubMed Google Scholar
33 Parvizi J , PawasaratIM, AzzamKA, et al.Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplasty2010;25(Suppl):103–107.CrossrefPubMed Google Scholar
34 Department of Health. MRSA Screening: Operational Guidance, 2008. http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_092845.pdf (date last accessed 18 March 2013). Google Scholar
35 Bode LG , KluytmansJA, WertheimHF, et al.Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med2010;362:9–17.CrossrefPubMed Google Scholar
36 Leaper D , Burman-RoyS, PalancaA, et al.Prevention and treatment of surgical site infection: summary of NICE guidance. BMJ2008;337:1924.CrossrefPubMed Google Scholar
37 Webster J , OsborneS. Preoperative bathing or showering with skin antiseptics to prevent surgical site infection. Cochrane Database Syst Rev2006;2:CD004985.CrossrefPubMed Google Scholar
38 Jakobsson J , PerlkvistA, Wann-HanssonC. Searching for evidence regarding using preoperative disinfection showers to prevent surgical site infections: a systematic review. Worldviews Evid Based Nurs2011;8:143–152.CrossrefPubMed Google Scholar
39 Tanner J , WoodingsD, MoncasterK. Preoperative hair removal to reduce surgical site infection. Cochrane Database Syst Rev2006;3:CD004122.CrossrefPubMed Google Scholar
40 Classen DC , EvansRS, PestotnikSL, et al.The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med1992;326:281–286.CrossrefPubMed Google Scholar
41 Prokuski L , ClyburnTA, EvansRP, MouchaCS. Prophylactic antibiotics in orthopaedic surgery. Instr Course Lect2011;60:545–555.PubMed Google Scholar
42 Hanssen AD , OsmonDR. Prevention of deep wound infection after total hip arthroplasty: the role of prophylactic antibiotics and clean air technology. Semin Arthroplasty1994;5:114–121.PubMed Google Scholar
43 AlBuhairan B , HindD, HutchinsonA. Antibiotic prophylaxis for wound infections in total joint arthroplasty: a systematic review. J Bone Joint Surg [Br]2008;90-B:915–919.CrossrefPubMed Google Scholar
44 Jenkins PJ , TeohK, SimpsonPM, et al.Clostridium difficile in patients undergoing primary hip and knee replacement. J Bone Joint Surg [Br]2010;92-B:994–998.CrossrefPubMed Google Scholar
45 Engesaeter LB , LieSA, EspehaugB, et al.Antibiotic prophylaxis in total hip arthroplasty: effects of antibiotic prophylaxis systemically and in bone cement on the revision rate of 22,170 primary hip replacements followed 0-14 years in the Norwegian Arthroplasty Register. Acta Orthop Scand2003;74:644–651.CrossrefPubMed Google Scholar
46 National Institute for Health and Clinical Excellence. Surgical site infection: prevention and traetment of surgical site infection, 2008. http://www.nice.org.uk/nicemedia/pdf/CG74NICEGuideline.pdf. (date last accessed 18 March 2013). Google Scholar
47 Swoboda SM , MerzC, KostuikJ, TrentlerB, LipsettPA. Does intraoperative blood loss affect antibiotic serum and tissue concentrations?Arch Surg1996;131:1165–1171.CrossrefPubMed Google Scholar
48 American Academy of Orthopaedic Surgeons. Recommendations for the use of intravenous antibiotic prophylaxis in primary total joint arthroplasty, 2004. http://www.aaos.org/about/papers/advistmt/1027.asp. (date last accessed 18 March 2013). Google Scholar
49 Mauerhan DR , NelsonCL, SmithDL, et al.Prophylaxis against infection in total joint arthroplasty: one day of cefuroxime compared with three days of cefazolin. J Bone Joint Surg [Am]1994;76-A:39–45. Google Scholar
50 Bannister GC , AuchinclossJM, JohnsonDP, NewmanJH. The timing of tourniquet application in relation to prophylactic antibiotic administration. J Bone Joint Surg [Br]1988;70-B:322–324.CrossrefPubMed Google Scholar
51 World Health Organization. Emergency and essential surgical care. www.who.int/surgery (date last accessed 7 January 2013). Google Scholar
52 Scaltriti S , CencettiS, RovestiS, MarchesiI, BargelliniA, BorellaP. Risk factors for particulate and microbial contamination of air in operating theatres. J Hosp Infect2007;66:320–326.CrossrefPubMed Google Scholar
53 Parienti JJ , ThibonP, HellerR, et al.Hand-rubbing with an aqueous alcoholic solution vs traditional surgical hand-scrubbing and 30-day surgical site infection rates: a randomized equivalence study. JAMA2002;288:722–727.CrossrefPubMed Google Scholar
54 Tanner J , SwarbrookS, StuartJ. Surgical hand antisepsis to reduce surgical site infection. Cochrane Database Syst Rev2008;1:CD004288.CrossrefPubMed Google Scholar
55 Jarral OA , McCormackDJ, IbrahimS, ShipoliniAR. Should surgeons scrub with chlorhexidine or iodine prior to surgery?Interact Cardiovasc Thorac Surg2011;12:1017–1021.CrossrefPubMed Google Scholar
56 Mahadeva D , RankinKS, MullerSD. Skin moisturisers and surgical site preparation: a slippery problem?J Hosp Infect2007;67:386–388.CrossrefPubMed Google Scholar
57 Darouiche RO , WallMJ, ItaniKM, et al.Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med2010;362:18–26.CrossrefPubMed Google Scholar
58 Lidwell OM . Air, antibiotics and sepsis in replacement joints. J Hosp Infect1988;11(Suppl C):18–40.CrossrefPubMed Google Scholar
59 Whyte W . The role of clothing and drapes in the operating room. J Hosp Infect1988;11(Suppl C):2–17.CrossrefPubMed Google Scholar
60 Noble WC . Dispersal of skin microorganisms. Br J Dermatol1975;93:477–485.CrossrefPubMed Google Scholar
61 Franco JA , BaerH, EnnekingWF. Airborne contamination in orthopedic surgery: evaluation of laminar air flow system and aspiration suit. Clin Orthop Relat Res1977;122:231–243. Google Scholar
62 Hansen D , KrabsC, BennerD, BrauksiepeA, PoppW. Laminar air flow provides high air quality in the operating field even during real operating conditions, but personal protection seems to be necessary in operations with tissue combustion. Int J Hyg Environ Health2005;208:455–460.CrossrefPubMed Google Scholar
63 Lidwell OM , ElsonRA, LowburyEJ, et al.Ultraclean air and antibiotics for prevention of postoperative infection: a multicenter study of 8,052 joint replacement operationsActa Orthop. Scand1987;58:4–13. Google Scholar
64 Brandt C , HottU, SohrD, DaschnerF, GastmeierP, RudenH. Operating room ventilation with laminar airflow shows no protective effect on the surgical site infection rate in orthopedic and abdominal surgery. Ann Surg2008;248:695–700.CrossrefPubMed Google Scholar
65 Hooper GJ , RothwellAG, FramptonC, WyattMC. Does the use of laminar flow and space suits reduce early deep infection after total hip and knee replacement?: the ten-year results of the New Zealand Joint Registry. J Bone Joint Surg [Br]2011;93-B:85–90.CrossrefPubMed Google Scholar
66 McGovern PD , AlbrechtM, BelaniKG, et al.Forced-air warming and ultra-clean ventilation do not mix: an investigation of theatre ventilation, patient warming and joint replacement infection in orthopaedics. J Bone Joint Surg [Br]2011;93-B:1537–1544. Google Scholar
67 Demircay E , UnayK, BilgiliMG, AlatacaG. Glove perforation in hip and knee arthroplasty. J Orthop Sci2010;15:790–794.CrossrefPubMed Google Scholar
68 Chan KY , SinghVA, OunBH, ToBH. The rate of glove perforations in orthopaedic procedures: single versus double gloving: a prospective study. Med J Malaysia2006;61(Suppl B):3–7. Google Scholar
69 Al-Maiyah M , BajwaA, MackenneyP, et al.Glove perforation and contamination in primary total hip arthroplasty. J Bone Joint Surg [Br]2005;87-B:556–559.CrossrefPubMed Google Scholar
70 Mingoli A , SapienzaP, SgarziniG, et al.Influence of blunt needles on surgical glove perforation and safety for the surgeon. Am J Surg1996;172:512–516.CrossrefPubMed Google Scholar
71 Wright KU , MoranCG, BriggsPJ. Glove perforation during hip arthroplasty: a randomised prospective study of a new taperpoint needle. J Bone Joint Surg [Br]1993;75-B:918–920. Google Scholar
72 Tanner J , ParkinsonH. Double gloving to reduce surgical cross-infection. Cochrane Database Syst Rev2006;3:CD003087.PubMed Google Scholar
73 Aldlyami E , KulkarniA, ReedMR, MullerSD, PartingtonPF. Latex-free gloves: safer for whom?J Arthroplasty2010;25:27–30.CrossrefPubMed Google Scholar
74 Webster J , AlghamdiAA. Use of plastic adhesive drapes during surgery for preventing surgical site infection. Cochrane Database Syst Rev2007;4:CD006353.CrossrefPubMed Google Scholar
75 Chiu KY , LauSK, FungB, NgKH, ChowSP. Plastic adhesive drapes and wound infection after hip fracture surgery. Aust N Z J Surg1993;63:798–801.CrossrefPubMed Google Scholar
76 Sessler DI , AkcaO. Nonpharmacological prevention of surgical wound infections. Clin Infect Dis2002;35:1397–1404.CrossrefPubMed Google Scholar
77 Sessler DI . Complications and treatment of mild hypothermia. Anesthesiology2001;95:531–543.CrossrefPubMed Google Scholar
78 Melling AC , AliB, ScottEM, LeaperDJ. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomised controlled trial. Lancet2001;358:876–880.CrossrefPubMed Google Scholar
79 Flores-Maldonado A , Medina-EscobedoCE, Rios-RodriguezHM, Fernandez-DominguezR. Mild perioperative hypothermia and the risk of wound infection. Arch Med Res2001;32:227–231.CrossrefPubMed Google Scholar
80 National Institute of Health and Clinical Excellence. NICE Clinical Guidelines. Perioperative hypothermia: Management of inadvertent perioperative hypothermia in adults. http://www.nice.org.uk/guidance/index.jsp?action=byID& o=11639 (date last accessed 7 January 2013). Google Scholar
81 Babior BM . The respiratory burst of phagocytes. J Clin Invest1984;73:599–601. Google Scholar
82 Pryor KO , FaheyTJ 3rd, LienCA, GoldsteinPA. Surgical site infection and the routine use of perioperative hyperoxia in a general surgical population: a randomized controlled trial. JAMA2004;291:79–87.CrossrefPubMed Google Scholar
83 Belda FJ , AguileraL, Garcia de la AsuncionJ, et al.Supplemental perioperative oxygen and the risk of surgical wound infection: a randomized controlled trial. JAMA2005;294:2035–2042.CrossrefPubMed Google Scholar
84 Greif R , AkcaO, HornEP, KurzA, SesslerDI. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med2000;342:161–167.PubMed Google Scholar
85 Arkilic CF , TaguchiA, SharmaN, et al.Supplemental perioperative fluid administration increases tissue oxygen pressure. Surgery2003;133:49–55.CrossrefPubMed Google Scholar
86 Mauermann WJ , NemergutEC. The anesthesiologist’s role in the prevention of surgical site infections. Anesthesiology2006;105:413–421. Google Scholar
87 Chang CC , LinHC, LinHW. Anesthetic management and surgical site infections in total hip or knee replacement: a population-based study. Anesthesiology2010;113:279–284. Google Scholar
88 Sanders RD , HussellT, MazeM. Sedation and immunomodulation. Crit Care Clin2009;25:551–570. Google Scholar
89 Riker RR , ShehabiY, BokeschPM, et al.Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA2009;301:489–499.CrossrefPubMed Google Scholar
90 Myers E , O’GradyP, DolanAM. The influence of preclinical anaemia on outcome following total hip replacement. Arch Orthop Trauma Surg2004;124:699–701.CrossrefPubMed Google Scholar
91 Morales CH , EscobarRM, VillegasMI, CastanoA, TrujilloJ. Surgical site infection in abdominal trauma patients: risk prediction and performance of the NNIS and SENIC indexes. Can J Surg2011;54:17–24.CrossrefPubMed Google Scholar
92 Alexander JW , SolomkinJS, EdwardsMJ. Updated recommendations for control of surgical site infections. Ann Surg2011;253:1082–1093.CrossrefPubMed Google Scholar
93 Steinitz D , HarveyEJ, LeightonRK, PetrieDP. Is homologous blood transfusion a risk factor for infection after hip replacement?Can J Surg2001;44:355–358.PubMed Google Scholar
94 Kendall SJ , WeirJ, AspinallR, HendersonD, RossonJ. Erythrocyte transfusion causes immunosuppression after total hip replacement. Clin Orthop Relat Res2000;381:145–155.CrossrefPubMed Google Scholar
95 Sukeik M , AlshrydaS, HaddadFS, MasonJM. Systematic review and meta-analysis of the use of tranexamic acid in total hip replacement. J Bone Joint Surg [Br]2011;93-B:39–46.CrossrefPubMed Google Scholar
96 National Institute for Health and Clinical Excellence. CG92: reducing the risk of venous thromboembolism (deep vein thrombosis and pulmonary embolism) in patients admitted to hospital, 2010. http://www.nice.org.uk/nicemedia/pdf/CG92NICEGuidelinePDF.pdf (date last accessed 18 March 2013). Google Scholar
97 Jameson SS , CharmanS, ReedMR, GreggPJ, Van der MeulenJ. The effect of aspirin and LMWH on venous thromboembolism after hip replacement: a non-randomised comparison in the National Joint Registry. J Bone Joint Surg [Br]2011;93-B:1465–1470. Google Scholar
98 Patel VP , WalshM, SehgalB, et al.Factors associated with prolonged wound drainage after primary total hip and knee arthroplasty. J Bone Joint Surg [Am]2007;89-A:33–38.CrossrefPubMed Google Scholar
99 Jensen CD , StevalA, PartingtonPF, ReedMR, MullerSD. Return to theatre following total hip and knee replacement, before and after the introduction of rivaroxaban: a retrospective cohort study. J Bone Joint Surg [Br]2011;93-B:91–95.CrossrefPubMed Google Scholar
100 Tong D , TheisJC. Antibiotic prophylaxis and invasive dental treatment in prosthetic joint patients. N Z Med J2008;121:45–52.PubMed Google Scholar
101 Oswald TF , GouldFK. Dental treatment and prosthetic joints: antibiotics are not the answer!. J Bone Joint Surg [Br]2008;90-B:825–826. Google Scholar
102 British Dental Association. Infective endocarditis, 2008. http://www.bda.org/pct-healthbody/policyandcampaigns/science-health/public-health/infective-endocarditis.aspx (date last accessed 18 March 2013). Google Scholar
Funding statement:
None declared
Author contributions:
R. Johnson: Principal author of paper, literature searching
S. S. Jameson: Idea and principal author of initial drafts
R. D. Sanders: Co-authorship with regards to anaesthetics
N. J. Sargant: Co-authorship with regards to blood products and haematology
S. D. Muller: Help with editing of final draft
R. M. D. Meek: Ideas and advice
M. R. Reed: Senior author/supervisor of project
ICMJE Conflict of Interest:
None declared
©2013 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










