Abstract
Objectives
To investigate the differences of open reduction and internal fixation (ORIF) of complex AO Type C distal radius fractures between two different models of a single implant type.
Methods
A total of 136 patients who received either a 2.4 mm (n = 61) or 3.5 mm (n = 75) distal radius locking compression plate (LCP DR) using a volar approach were followed over two years. The main outcome measurements included motion, grip strength, pain, and the scores of Gartland and Werley, the Short-Form 36 (SF-36) and the Disabilities of the Arm, Shoulder, and Hand (DASH). Differences between the treatment groups were evaluated using regression analysis and the likelihood ratio test with significance based on the Bonferroni corrected p-value of < 0.003.
Results
The groups were similar with respect to baseline and injury characteristics as well as general surgical details. The risk of experiencing a complication after ORIF with a LCP DR 2.4 mm was 18% (n = 11) compared with 11% (n = 8) after receiving a LCP DR 3.5 mm (p = 0.45). Wrist function was also similar between the cohorts based on the mean ranges of movement (all p > 0.052) and grip strength measurements relative to the contralateral healthy side (p = 0.583). In addition, DASH and SF-36 component scores as well as pain were not significantly different between the treatment groups throughout the two-year period (all p ≥ 0.005). No patient from either treatment group had a step-off > 2 mm.
Conclusions
Differences in plate design do not influence the overall final outcome of fracture fixation using LCP.
Article focus
We conducted a comparative study to identify differences in the functional outcome of 136 complex (AO Type C) distal radius fracture patients treated with a distal radius locking compression plate (LCP DR) of either 2.4 mm or 3.5 mm
The null hypothesis states that there is no difference between the two groups regarding the final outcome at two years
Key messages
All patients achieved adequate functional outcome by the two-year follow-up
There was no significant difference in the final outcome between the two sizes of LCP DR
Strengths and limitations
The dataset is relatively large compared with similar studies that have assessed the performance of LCP DR in the treatment of distal radius fractures
The study focuses on only a single fracture type, allowing for a more comprehensive understanding of the exact influence of the different plate types on a standardised fracture
Both groups were documented prospectively in separate groups of clinics using a similar study protocol
Despite statistical adjustments for baseline factors, residual confounding cannot be excluded in this observational study
Introduction
The advantages of operative treatment for distal radius fractures have been highlighted.1-3 In addition, a number of studies have reported the successful use of volar locking plates to stabilise intra- and extra-articular fractures, as this type of fixation enables adequate functional post-operative treatment.4-6 Consequently, the popularity of volar angle stable plate fixation has increased, as has the number of implants available on the market. Variations in plate design include adaptations to the shape and contour of the plate,7 the size and angle of the screws, the locking screw mechanism,8 and the type of plate material.9
There are special requirements in the treatment of complex AO Type C2 and C3 distal radius fractures. Comminution of the dorsal cortex places high demand on the stability of the implant and locking mechanism of the plate/screw interface. Displaced fragments of the joint surface (especially in the case of a C3 fracture) also require several options for the fixation of specific fragments with screws of small diameter.
Using the database of two large prospective multicentre studies on the locking compression plate distal radius (LCP DR) system (Synthes AG, Bettlach, Switzerland),10,11 we performed a comparative analysis of a subset of patients with an AO Type C fracture treated with either a LCP DR 2.4 mm or 3.5 mm. The main purpose was to investigate the outcomes following open reduction and internal fixation (ORIF) using two different models of a single implant type.
Materials and Methods
Patients with fractures of the distal radius aged between 18 and 80 years who provided written informed consent were originally recruited as part of two larger prospective studies to evaluate LCP DR 2.4 mm and 3.5 mm implants (Fig. 1); these studies were approved by the respective Institutional Review Boards for each participating centre.10,11 For this analysis, patients with AO Type C distal radius/ulna fractures (i.e. complex articular fractures affecting the joint surface and the metaphyseal area)12 who received plate fixation using a volar approach with either implant within ten days of injury were selected. Further details concerning the original study inclusion and exclusion criteria have been previously described.10,11
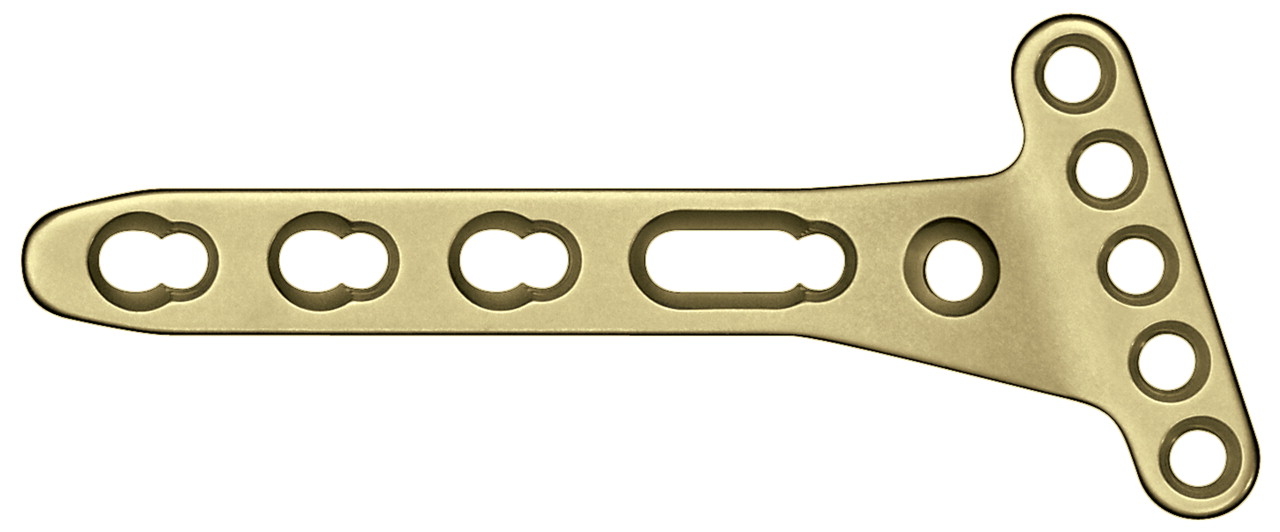
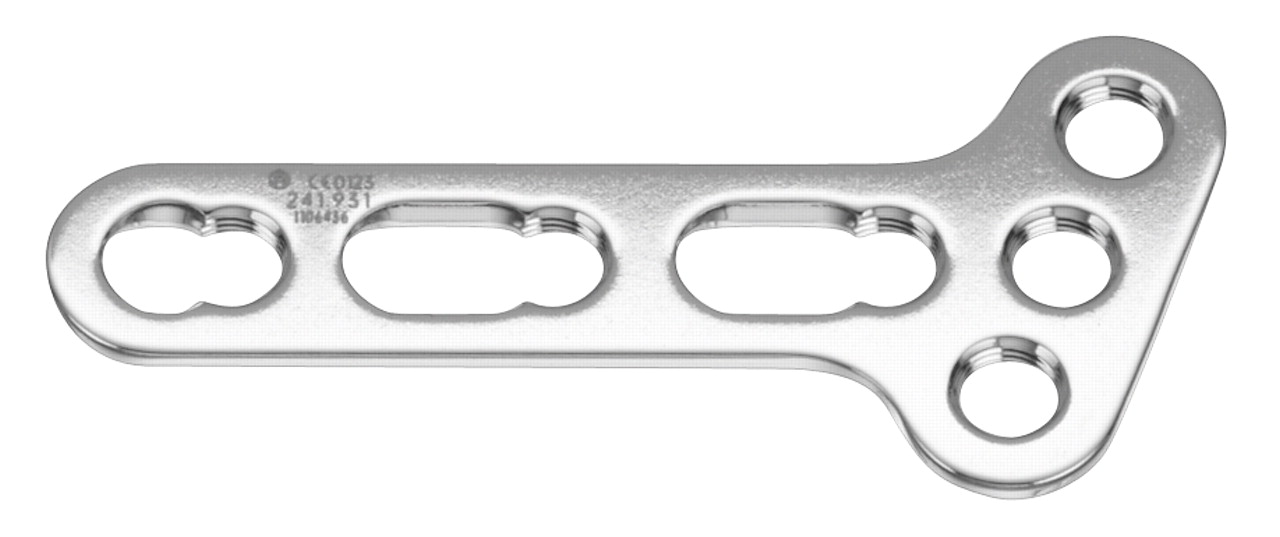
Figs. 1a - 1b
Photographs of distal radius locking compression plates (LCP DR) used in the volar fixation of AO Type C fractures of the distal radius, showing a) the juxta-articular 2.4 mm and b) the T-plate 3.5 mm types.
Baseline and outcome evaluation
All patient evaluations have been described in detail by Jupiter et al.10 Briefly, general patient demographics and accident/fracture characteristics were documented on case report forms during hospitalisation. Baseline measurements of the Disabilities of the Arm, Shoulder and Hand (DASH) score13 (i.e. the patient-rated function of the upper limb at one week prior to injury) and pain (at rest and during motion) using a visual analogue scale (VAS; 0 indicates no pain and 10 represents very severe pain) were completed for each patient. Anteroposterior (AP) and lateral radiographs were obtained upon admission, intra-operatively, and immediately post-operatively as well as on subsequent scheduled follow-up evaluations.
Patients were followed up at six months, and at one and two years. The examinations included: measurement of wrist and forearm motion with a goniometer, and grip strength using a Jamar dynamometer (Sammons Preston Roylan, Bolingbrook, Illinois); functional assessments using the DASH and Short-Form 36 (SF-36) scores14 as well as the physician-rated Gartland and Werley score15; and pain and satisfaction ratings using the 0 to 10 VAS, where 0 was not satisfied at all and 10 was absolutely satisfied for the latter.
The evaluation of joint alignment, fracture healing and reduction, arthritis grading according to Knirk and Jupiter16 and the degree of displacement was made on post-operative radiographs. All radiological measurements including radial angle, radial length, ulnar variance, and articular step-off and gap were evaluated by an independent radiologist and recorded according to the criteria of Kreder et al.17
All complications were documented up to two years.
Study population
A total of 317 patients recruited consecutively from 18 participating clinics were screened. Of these, 136 patients had an AO Type C fracture treated with either an LCP DR 3.5 mm (n = 75) or 2.4 mm (n = 61) using a volar approach, and were included in the analysis (Fig. 2). In the 3.5 mm group there were 21 men and 54 women with a mean age of 55.5 years (25 to 80), and in the 2.4 mm group there were 19 men and 42 women with a mean age of 51.9 years (18 to 78). Over 70% of the patients had no signs of arthritis and a baseline DASH score between 0 and 5 (Table I). Overall, both groups were similar, although a significantly higher proportion of 3.5 mm patients had a concomitant general disease (44% vs 11%; Fisher’s exact test, p < 0.001) and were right-handed (96% vs 85%; Fisher’s exact test, p = 0.036) compared with the 2.4 mm cohort (Table I).
Table I
Baseline patient demographics
| LCP DR 3.5 mm (n = 75) | LCP DR 2.4 mm (n = 61) | p-value* | |
|---|---|---|---|
| Mean (sd) age (yrs) | 55.5 (15.9) | 51.9 (15.3) | 0.211† |
| Male gender (n, %) | 21 (28) | 19 (31) | 0.709 |
| Mean (sd) BMI‡ (kg/m2) | 26.7 (5.4) | 26.0 (4.1) | 0.796† |
| Work before the accident (n, %) | 1.000 | ||
| Yes | 35 (47) | 28 (46) | |
| No | 39 (52) | 33 (54) | |
| Data missing | 1 (1) | - | |
| DASH score group (n, %)§ | 0.188 | ||
| 0 | 35 (56) | 43 (73) | |
| 1 to 5 | 17 (27) | 9 (15) | |
| 6 to 10 | 4 (6) | 3 (5) | |
| 11 to 15 | 5 (8) | 1 (2) | |
| > 15 | 2 (3) | 3 (5) | |
| Median DASH score (range) | 0 (0 to 63) | 0 (0 to 50) | |
| Concurrent general disease (n, %) | < 0.001 | ||
| Yes | 33 (44) | 7 (11) | |
| No | 42 (56) | 54 (89) | |
| Knirk and Jupiter16 arthritis grade (n, %)¶ | 0.699 | ||
| 0 | 54 (72) | 46 (75) | |
| 1 | 20 (27) | 13 (21) | |
| 2 | 1 (1) | 2 (3) | |
| 3 | - | - | |
| AO classification (n, %) | 0.228 | ||
| Type C1 | 1 (1) | 1 (2) | |
| Type C2 | 25 (33) | 13 (21) | |
| Type C3 | 49 (65) | 47 (77) | |
| Dexterity (dominant hand) (n, %) | 0.036 | ||
| Right | 71 (95) | 52 (85) | |
| Left | 3 (4) | 9 (15) | |
| Data missing | 1 (1) | - | |
| Smoker (n, %) | 0.430 | ||
| Yes | 21 (28) | 13 (21) | |
| No | 53 (71) | 48 (79) | |
| Data missing | 1 (1) | - | |
| Bone graft** (n, %) | 0.136 | ||
| Yes | 4 (5) | 8 (13) | |
| No | 71 (95) | 53 (87) | |
-
* Fisher’s exact test, unless otherwise indicated † Wilcoxon rank-sum test ‡ BMI, body mass index. Data was available for 74 patients in the LCP DR 3.5 mm group and 59 in the 2.4 mm group § DASH, Disabilities of the Arm, Shoulder, and Hand (scored from 0 to 100). Data was available for 63 patients in the LCP DR 3.5 mm group and 59 in the 2.4 mm group ¶ 0, no arthritis; 1, slight joint space narrowing; 2, marked joint space narrowing, osteophyte formation; 3, bone-on-bone, osteophyte formation, cyst formation ** baseline surgery characteristic considered during statistical adjustment of the regression analyses
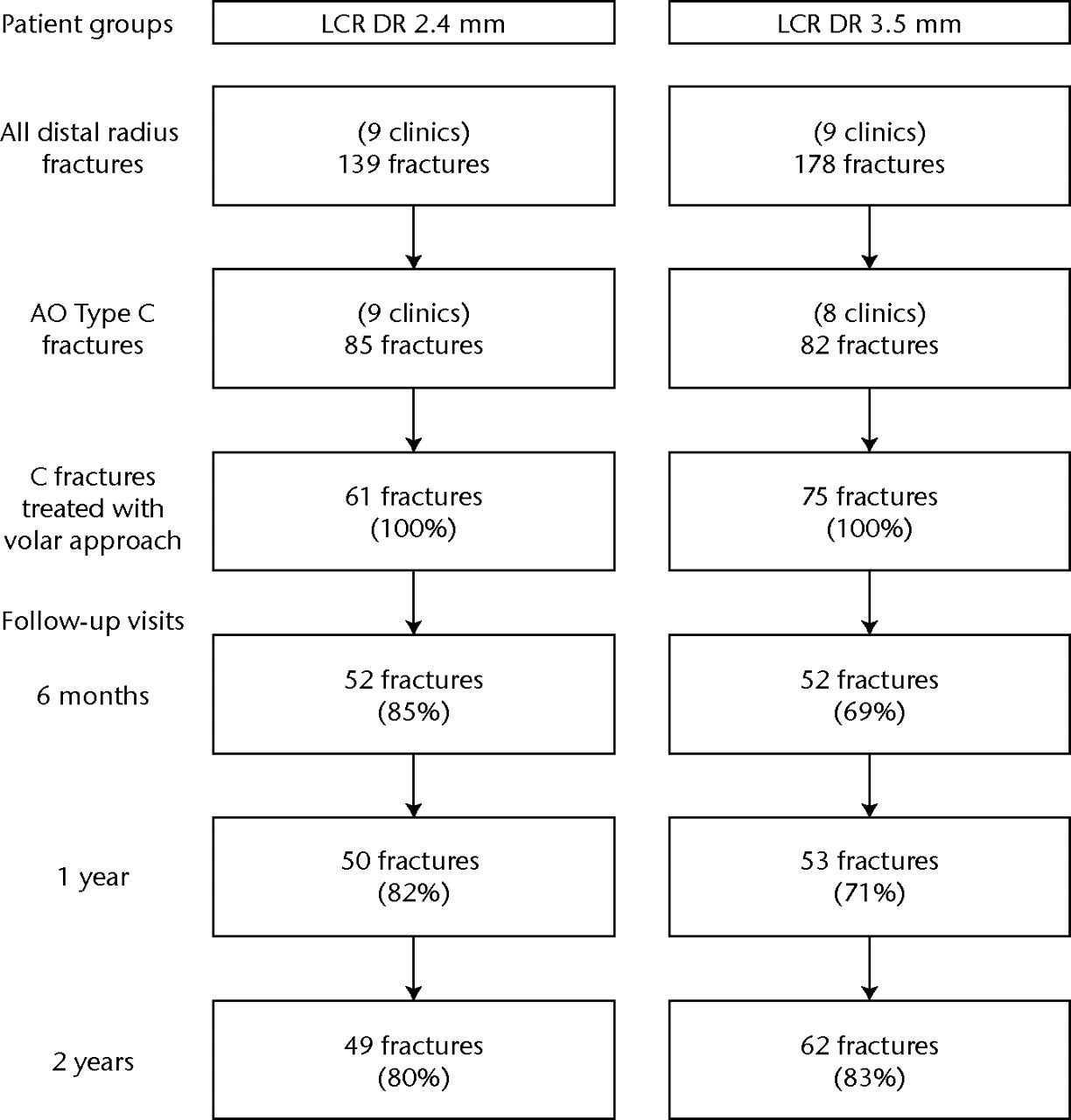
Fig. 2
Flow chart showing the screening of distal radius fracture cases treated with either a 2.4 mm or 3.5 mm distal radius locking compression plate (LCP DR) using a volar approach and the follow-up rates throughout the two-year period.
According to the AO classification, the majority of fractures were categorised as Type C3 fractures (65% and 77% for the 3.5 mm and 2.4 mm groups, respectively). The remainder were all Type C2 fractures, except for one Type C1 fracture in each group (Table I). There was no significant group difference based on the distribution of C-fracture subtypes (Fisher’s exact test, p = 0.23).
Statistical analysis
Baseline characteristics between the groups treated with an LCP DR 3.5 mm or an LCP DR 2.4 mm were compared using the Fisher’s exact and Kruskal-Wallis tests and clinical judgment. Differences in function and health status were assessed at six months and one and two years, at which time point the rates of follow-up were 76%, 76%, and 82%, respectively (Fig. 2).
For each of the 19 outcome parameters, all data were pooled and analysed together in one overall linear regression model, while taking the repeated measurements across the follow-up examinations into account. Analyses were statistically adjusted for age, dominant side fractures, concomitant diseases, baseline DASH score, fracture subtype C3, and the use of bone graft.
The likelihood ratio test was used to study the overall effect of the 2.4 mm over the 3.5 mm plate on each outcome parameter. Statistical significance was adjusted for multiple testing using a Bonferroni correction: a p-value < 0.003 (i.e. 0.05 divided by the 19 parameters) was considered significant. For each outcome showing an overall significant plate type effect, group differences at follow-up time points were estimated and tested (Wald test).
While the original studies10,11 were not designed for such a group comparison, a post-hoc two-sided analysis with group sizes of 49 and 62 patients at two years indicated a power of 83% to identify an effect size (standardised difference in a continuous outcome) of 0.75 at a Bonferroni-corrected significance level of 0.003. An effect size of 0.5 represents a moderate difference and 0.8 a large difference.18,19
All statistical analyses were conducted with the software Intercooled Stata Version 9 (StataCorp LP, College Station, Texas).
Results
Complications
The risk of experiencing a complication after fixation with a LCP DR 3.5 mm was 11% (8 of 75) compared with 18% (11 of 61) associated with the 2.4 mm plate (Table II). The relative risk of a complication was calculated to be 1.7 (95% confidence interval 0.73 to 3.9; p = 0.32).
Table II
List of reported complications
| Complications | LCP DR 3.5 mm | LCP DR 2.4 mm |
|---|---|---|
| Soft tissue/wound | 6 | 6 |
| Infection | 1 | - |
| Healing problems | 1 | - |
| Carpal tunnel syndrome | 2 | 1 |
| Tendinitis | 1 | 4 |
| Tendon rupture | 1 | - |
| Other soft-tissue problems | - | 1 |
| Implant / surgery | 2 | 1 |
| Loss of reduction | 1 | - |
| Screw pull out | 1 | 1 |
| Bone / fracture | n.r.† | 3 |
| Loss of reduction | - | 2 |
| Healing problems | - | 1 |
| General | n.r. | 1 |
| Death | - | 1 |
| Total number of complications | 8 | 11 |
| Complication risk (%)* | 11% | 18% |
-
* the complication risk estimation for experiencing at least one local complication. There were eight local complications arising from 75 fractures for the 3.5 mm group and ten local complications from 61 fractures for the 2.4 mm. There was no difference between the complication risks estimated for the treatment groups (Fisher's exact test, p = 0.45) † n.r., not reported
Functional outcomes
There were no significant differences in the range of movement of the wrist between patients treated with either the 3.5 mm or 2.4 mm plate (likelihood ratio test; all p ≥ 0.052) (Table III). The mean grip strength measurements compared with the healthy contralateral side increased beyond 80%, and Gartland and Werley scores were also categorised as good or excellent for over 80% of patients from both cohorts (Table IV). In addition, patient health status in both treatment groups was not significantly different based on the DASH (p = 0.301) and SF-36 component scores (p = 0.019 and p = 0.089 for physical and mental components, respectively), as well as assessment of pain throughout the two-year period (p = 0.014 and p = 0.005 for pain at rest and movement, respectively; all likelihood ratio test).
Table III
Mean range of movement (ROM, with sd) for patients receiving a distal radius locking compression plate of either 3.5 mm or 2.4 mm during the two-year follow-up
| Baseline (healthy side) | 6 months | 1 year | 2 years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range of motion (o) | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | p-value* | |||
| Palmar flexion | 68 (13) | 70 (13) | 55 (16) | 57 (15) | 56 (16) | 60 (15) | 55 (16) | 60 (15) | 0.490 | |||
| % of contralateral side | - | - | 80 | 82 | 80 | 85 | 81 | 87 | 0.432 | |||
| Dorsal extension | 68 (11) | 72 (10) | 59 (16) | 62 (16) | 60 (16) | 67 (13) | 59 (16) | 68 (13) | 0.052 | |||
| % of contralateral side | - | - | 89 | 86 | 88 | 93 | 88 | 93 | 0.095 | |||
| Radial deviation | 25 (8) | 26 (7) | 19 (7) | 21 (9) | 22 (7) | 23 (9) | 24 (10) | 25 (7) | 0.296 | |||
| % of contralateral side | - | - | 77 | 85 | 88 | 91 | 97 | 100 | 0.296 | |||
| Ulnar deviation | 37 (9) | 39 (9) | 29 (9) | 32 (9) | 34 (11) | 33 (11) | 33 (10) | 35 (10) | 0.380 | |||
| % of contralateral side | - | - | 78 | 86 | 93 | 87 | 93 | 92 | 0.151 | |||
| Pronation angle | 86 (7) | 87 (5) | 81 (12) | 83 (10) | 84 (14) | 85 (7) | 85 (8) | 87 (6) | 0.201 | |||
| % of contralateral side | - | - | 94 | 96 | 97 | 98 | 98 | 100 | 0.293 | |||
| Supination angle | 85 (10) | 87 (5) | 79 (14) | 80 (12) | 82 (13) | 85 (8) | 78 (17) | 85 (8) | 0.588 | |||
| % of contralateral side | - | - | 93 | 93 | 95 | 98 | 93 | 98 | 0.670 | |||
-
* likelihood ratio test for detecting a difference between the groups during the first two years
Table IV
Comparison of mean functional outcome results for patients receiving either a distal radius locking compression plate of 3.5 mm or 2.4 mm during the two-year follow-up
| Baseline | 6 months | 1 year | 2 years | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | 3.5 mm | 2.4 mm | p-value* | |||
| Mean (sd) DASH score† | 3.4 (8.7)† | 2.3 (7.4)† | - | - | 12.7 (15.9) | 7.0 (11.8) | 13.2 (17.8) | 6.9 (12.3) | 0.301 | |||
| Mean (sd) Gartland & Werley score | - | - | 4.5 (4.0) | 3.7 (3.1) | 4.1 (5.0) | 3.2 (3.9) | 4.3 (5.1) | 2.4 (2.7) | 0.141 | |||
| Gartland & Werley category (%) | ||||||||||||
| Excellent | - | - | 36 | 48 | 46 | 60 | 43 | 62 | ||||
| Good | - | - | 46 | 42 | 42 | 30 | 41 | 34 | ||||
| Fair / poor | - | - | 18 | 10 | 12 | 10 | 16 | 4 | ||||
| Mean (sd) VAS for pain‡ | ||||||||||||
| During rest | 3.4 (2.5)‡ | 4.3 (2.6)‡ | 1.2 (1.4) | 0.4 (0.5) | 1.3 (1.8) | 0.5 (0.8) | 1.4 (2.1) | 0.4 (0.7) | 0.014 | |||
| With motion | - | - | 1.5 (1.7) | 1.2 (1.5) | 1.9 (2.2) | 0.7 (1.1) | 1.7 (2.1) | 0.9 (1.6) | 0.005 | |||
| Mean (sd) Short-Form 36 | ||||||||||||
| Physical component | - | - | - | - | 49.0 (9.8) | 52.8 (8.0) | 46.4 (10.9) | 53.7 (6.7) | 0.019 | |||
| Mental component | - | - | - | - | 50.1 (11.2) | 56.2 (5.9) | 52.2 (10.0) | 55.3 (7.1) | 0.089 | |||
| Mean (sd) grip strength (kg) | 32 (14)§ | 31 (13)§ | 23 (12) | 22 (11) | 25 (14) | 27 (11) | 28 (15) | 28 (11) | ||||
| % contralateral side | - | - | 71 | 73 | 81 | 89 | 87 | 94 | 0.583 | |||
-
* likelihood ratio test for detecting a difference between the groups during the first two years † DASH, Disabilities of the Arm, Shoulder, and Hand. Baseline DASH is based on patient-rated function of the upper limb at one week prior to injury ‡ VAS, visual analogue scale. Baseline VAS for pain corresponds to the immediate post-operative period (within three days of surgery) § mean baseline grip strength measurements are those for the contralateral (healthy side)
Radiological outcomes
The mean radiological measurements at two years were similar between the two groups. For the 3.5 mm and 2.4 mm groups, the mean radial inclination was 23.5° and 23.4°, respectively (p = 0.181), the mean palmar tilt 3.2° and 2.6°, respectively (p = 0.556), and the mean ulnar variance 0.03 mm and 0.0 mm, respectively (p = 0.348; all likelihood ratio test).
Of 69 patients in the LCP DR 3.5 mm group with complete data, 27 (39%) with generally no baseline signs of arthritis showed a worsening of arthritis grade by at least one point on the system of Knirk and Jupiter,16 and two patients increased by three points between the follow-up assessments at one and two years. Of 54 patients in the LCP DR 2.4 mm group with complete data, 16 (30%) worsened by one grade and four (7%) by two grades. This was a smaller worsening than that seen in the 3.5 mm group, but it did not reach statistical significance after applying the Bonferroni corrected level (Fisher’s exact test; p = 0.04).
At one year, an articular step-off was recorded for one of 53 patients (2%) in the 3.5 mm group compared with eight of 50 (16%) in the 2.4 mm group (Fisher’s exact test; p = 0.014); this outcome was also not significant based on the Bonferroni corrected significance level. By two years, only three of 49 patients (6%) in the 2.4 mm group were reported to have a step-off. No patient from either treatment group had a step-off > 2 mm.
Discussion
Our analysis confirms that there is no difference between the volar fixation of dorsally comminuted intra-articular distal radius fractures using either of the LCP systems. Our patient series achieved functional outcomes similar to that of other cohorts of patients with intra-articular distal radius fractures treated with a volar approach and locking plates.20-22 The complication rates are similar to those described by Souer et al23 of 11% and 21% for the 3.5 mm and 2.4 mm systems, respectively – although those authors focused on the treatment of AO Type A3.2 extra-articular fractures.23 Our radiological findings were similar to those described by Konstantinidis et al.21
The oblique 3.5 mm implant has only three distal screw holes with limited options for fixing specific fragments as well as size limitations for fixing broad wrists. The straight version has the option of applying up to four screws but due to its lack of ulnar angulation, this implant is restricted to fixing distal styloid fragments. It is also a thick implant that theoretically could lead to more interference with flexor tendons. Alternately, the 2.4 mm plate is an anatomically pre-shaped, low-profile plate designed to minimise soft-tissue irritations. There are up to five options for positioning distal interlocking screws, and with the use of smaller diameter screws, there are more options to fix specific comminuted fragments and position the plate in a more distal fashion compared with its 3.5 mm counterpart. Its screws are oriented proximally to avoid intra-articular placement but this could lead to insufficient subchondral support and secondary loss of reduction. In addition, the 2.4 mm implant may provide less stability due to the smaller screw diameter and reduced plate thickness. This possible difference in implant stability may affect successful rehabilitation and final functional outcome status of the patient.
For both groups, similar incidences of screw loosening and loss of reduction were reported. Breakage of the plate was not reported and those cases of screw loosening originated from bone/fracture or surgical technique problems, rather than the implant itself. A similar proportion (60%) of high grade unstable type C3 intra-articular fractures have been reported undergoing volar fixation with the 2.4 mm LCP implant21; single cases each of loss of reduction and early screw displacement were reported, which is comparable to the outcome of implant related complications in our study. Based on this, one cannot assume that the 2.4 mm implant is less stable than the 3.5 mm plate. Souer et al23 reported better restoration of volar angulation in their 3.5 mm group and attribute this to the aforementioned difference in plate design and not due to insufficient stability of fixation. There were no reports of flexor tendon irritation in our patients. We recommend placing the implant up to and not beyond the watershed line24 as a necessary step to avoid contact and injury to the flexor tendons, regardless of the type of plate used.
A plate offering more options for fixing specific fragments with smaller screws may lead to better anatomic reduction. This will result in a smaller step-off occurring in the joint surface, minimise the development of arthritis and ultimately provide better function of the wrist. One major goal in treating articular fractures is to prevent post-traumatic arthritis resulting from initial damage to the joint surface and the quality of reduction. It is generally accepted that a step-off < 2 mm is mandatory to reduce the likelihood of developing post-traumatic arthritis.16,25 There was a tendency towards a greater number of 2.4 mm treated patients reporting a step-off in our study, although all reported incidences in both groups were < 1 mm. Our data does not support the assumption that plates with more options for fixing specific fragments with smaller screws can lead to enhanced anatomic reduction. The degree of arthritis worsening over time was similar in both groups. Functionality is the sum of pain, range of movement and grip strength, which was achieved by all our patients.
Based on the observational nature of the study and the lack of patient randomisation, residual confounding cannot be excluded. Nevertheless, appropriate statistical adjustments for baseline factors were made. In addition, since both patient groups were documented prospectively in separate groups of clinics using a similar study protocol, this situation is less prone to allocation bias associated with treatment choice by the surgeons within a clinic. Our comparison is therefore valid and relevant given the many clinics that were involved. Our cohorts are relatively larger compared to the number of patients treated with the LCP 3.5 mm and 2.4 mm (n = 38 and 24, respectively) evaluated by Souer et al.23 Furthermore, our focus on a single fracture type allowed for a better understanding of the exact influence of the different plate types. A complex fracture of the distal radius must account for additional factors when considering their surgical fixation. In their discussion, Souer et al23 speculate on whether their outcome would apply to more complex fractures, particularly articular fractures. Our investigation supports the idea that both the 2.4 mm and 3.5 mm LCPs offer similar outcomes not only to patients with extra-articular fractures. Based on our findings from an observational database, it would be of interest to see whether the results from our study and that of Souer et al23 would be confirmed by a large, randomised controlled trial.
In conclusion, patients with complex distal radius fractures (i.e. complete multifragmentary articular fractures) can expect good functional outcome from the LCP systems. Our data did not support the theoretical benefits of the newly designed 2.4 mm implant. Both provide stable support to the wrist with the option of undertaking functional post-operative treatment.
1 Simic PM , WeilandAJ. Fractures of the distal aspect of the radius: changes in treatment over the past two decades. Instr Course Lect2003;52:185–195.PubMed Google Scholar
2 Simic PM , RobisonJ, GardnerMJ, et al.Treatment of distal radius fractures with a low-profile dorsal plating system: an outcomes assessment. J Hand Surg Am2006;31:382–386.CrossrefPubMed Google Scholar
3 Wright TW , HorodyskiM, SmithDW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am2005;30:289–299.CrossrefPubMed Google Scholar
4 Rozental TD , BlazarPE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg Am2006;31:359–365.CrossrefPubMed Google Scholar
5 Arora R , LutzM, HennerbicherA, KrappingerD, EspenD, GablM. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma2007;21:316–322.CrossrefPubMed Google Scholar
6 Rampoldi M , MarsicoS. Complications of volar plating of distal radius fractures. Acta Orthop Belg2007;73:714–719.CrossrefPubMed Google Scholar
7 Mudgal CS , JupiterJB. Plate and screw design in fractures of the hand and wrist. Clin Orthop Relat Res2006;445:68–80.CrossrefPubMed Google Scholar
8 Egol KA , KubiakEN, FulkersonE, KummerFJ, KovalKJ. Biomechanics of locked plates and screws. J Orthop Trauma2004;18:488–493.CrossrefPubMed Google Scholar
9 Cohen MS , TurnerTM, UrbanRM. Effects of implant material and plate design on tendon function and morphology. Clin Orthop Relat Res2006;445:81–90.CrossrefPubMed Google Scholar
10 Jupiter JB , Marent-HuberM. ; LCP Study Group. Operative management of distal radial fractures with 2.4-millimeter locking plates: a multicenter prospective case series. J Bone Joint Surg [Am]2009;91-A:55–65. Google Scholar
11 Matschke S , Marent-HuberM, AudigéL, WentzensenA. ; LCP Study Group. The surgical treatment of unstable distal radius fractures by angle stable implants: a multicenter prospective study. J Orthop Trauma2011;25:312–317. Google Scholar
12 Müller ME, Nazarian S, Koch P, Schatzker J. The comprehensive classification of fractures of long bones. Berlin: Springer-Verlag, 1990. Google Scholar
13 Hudak PL , AmadioPC, BombardierC. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med1996;29:602–608.CrossrefPubMed Google Scholar
14 Ware JE Jr , SherbourneCD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care1992;30:473–483.PubMed Google Scholar
15 Gartland JJ Jr , WerleyCW. Evaluation of healed Colles’ fractures. J Bone Joint Surg [Am]1951;33-A:895–907. Google Scholar
16 Knirk JL , JupiterJB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg [Am]1986;68-A:647–659.CrossrefPubMed Google Scholar
17 Kreder HJ , HanelDP, McKeeM, et al.X-ray film measurements for healed distal radius fractures. J Hand Surg Am1996;21:31–39.CrossrefPubMed Google Scholar
18 Cohen J. Statistical power analysis for the behavioural sciences. New York: Academic Press, 1977. Google Scholar
19 Kazis LE , AndersonJJ, MeenanRF. Effect sizes for interpreting changes in health status. Med Care1989;27(Suppl):S178–S189.CrossrefPubMed Google Scholar
20 Gruber G , GruberK, GiessaufC, et al.Volar plate fixation of AO type C2 and C3 distal radius fractures: a single-center study of 55 patients. J Orthop Trauma2008;22:467–472. Google Scholar
21 Konstantinidis L , HelwigP, StrohmPC, et al.Clinical and radiological outcomes after stabilisation of complex intra-articular fractures of the distal radius with the volar 2.4 mm LCP. Arch Orthop Trauma Surg2010;130:751–757.CrossrefPubMed Google Scholar
22 Rein S , SchikoreH, SchneidersW, AmlangM, ZwippH. Results of dorsal or volar plate fixation of AO type C3 distal radius fractures: a retrospective study. J Hand Surg Am2007;32:954–961. Google Scholar
23 Souer JS , RingD, MatschkeS, et al.Comparison of functional outcome after volar plate fixation with 2.4-mm titanium versus 3.5-mm stainless-steel plate for extra-articular fracture of distal radius. J Hand Surg Am2010;35:398–405.CrossrefPubMed Google Scholar
24 Orbay JL , TouhamiA. Current concepts in volar fixed-angle fixation of unstable distal radius fractures. Clin Orthop Relat Res2006;445:58–67.CrossrefPubMed Google Scholar
25 Rikli DA , RegazzoniP. Fractures of the distal end of the radius treated by internal fixation and early function: a preliminary report of 20 cases. J Bone Joint Surg [Br]1996;78-B:588–592. Google Scholar
Funding statement:
The work presented in this manuscript was supported by the AO Foundation
Author contributions:
J. von Recum: Data analysis, Writing the paper, Final proofing
S. Matschke: Data analysis, Writing the paper, Final proofing
J. B. Jupiter: Study design, Data collection, Writing the paper, Final proofing
D. Ring: Study design, Data collection, Writing the paper, Final proofing
J-S. Souer: Data collection, Writing the paper, Final proofing
M. Huber: Data collection, Writing the paper, Final proofing
L. Audigé: Study design, Data analysis, Writing the paper, Final proofing
ICMJE Conflict of Interest:
The authors were not supported by any outside funding, grants or additional benefits for this study
©2012 British Editorial Society of Bone and Joint Surgery. This is an open-access article distributed under the terms of the Creative Commons Attributions licence, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










