Abstract
Many aspects of total knee arthroplasty have changed since its inception. Modern prosthetic design, better fixation techniques, improved polyethylene wear characteristics and rehabilitation, have all contributed to a large change in revision rates. Arthroplasty patients now expect longevity of their prostheses and demand functional improvement to match. This has led to a re-examination of the long-held belief that mechanical alignment is instrumental to a successful outcome and a focus on restoring healthy joint kinematics. A combination of kinematic restoration and uncemented, adaptable fixation may hold the key to future advances.
Cite this article: Bone Joint J 2015;97-B(10 Suppl A):16–19.
The pioneers of total knee arthroplasty (TKA) faced very different challenges to those of modern--day surgeons. The early failures in linked, hinge-like prostheses gave rise to total condylar, unlinked designs1,2 and knee arthroplasty was reserved for highly disabled patients with extensive joint damage and large resultant deformities. Surgeons and implant designers were left with the significant problem of how to relieve pain and restore function, and in doing so offer a solution with longevity. Initial results, although a great improvement on previous treatments, do not compare with their modern counterparts. Alongside good functional results and pain relief, both Freeman and Insall reported high rates of re-operation and revision highlighting the complexity of the surgical technique of TKA.3,4 In his 1983 report of the five- to nine-year outcomes of his total condylar prosthesis, Insall concluded “The majority of failures in our series were attributed to errors in surgical technique”.5 Efforts to avoid these were, in particular, focused on achieving neutral mechanical alignment with the tibial tray at 90° to the limb’s mechanical axis.
Modern prosthetic design, better fixation techniques, improved polyethylene wear characteristics and rehabilitation have all contributed to a factorial change in rates of revision. Arthroplasty patients now expect not only longevity of their prostheses but also equally high functional performance. This has led to re-evaluation of the belief that mechanical alignment is paramount, focusing instead on the restoration of healthy joint kinematics.
Mechanical alignment – the key to longevity?
The mechanical axis of the femur corresponds to a line drawn from the centre of the femoral head to the mid-point of the distal femoral condyles and that of the tibia from the mid-point of the tibial condyles to the centre of the ankle joint. In the absence of tibial deformity, this mechanical axis is coincident with the anatomical axis (Fig. 1). Neutral mechanical alignment refers to implantation of the components of a TKA in such a way as to align femoral and tibial mechanical axes (Fig. 1).
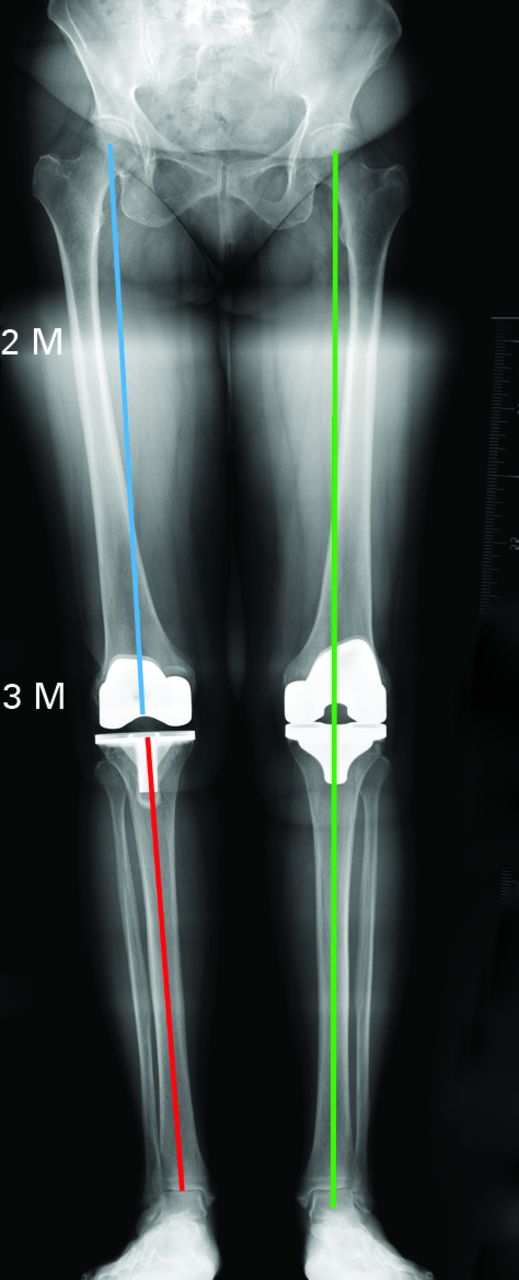
Fig. 1
Radiograph showing the femoral mechanical axis (blue line), tibial mechanical axis (red line) and mechanical alignment (green line).
The normal tibia is in 2° to 3° of varus in the frontal plane, and the distal femur 7° to 9° of valgus. Thus, in the normal knee, the joint line is oblique.
While a neutral mechanical alignment is not anatomic, biomechanical data suggest it is favourable in terms of the longevity of components. The effects of malalignment of the tibial tray on bone6,7 and polyethylene8,9 have been examined. The patient-specific finite element analysis performed by Perillo--Marconeet et al,6 which adjusted for relative bone density, showed that varus and valgus angulation of the tibial tray resulted in increased loading of the medial and lateral tibial condyles, respectively. In their series, higher bone density was found in the medial tibial condyle and so greater risk was occasioned by valgus positioning of the tray, resulting in increased loading of the relatively weaker lateral tibia.
Wong et al7 demonstrated strain in the medial tibia beyond fatigue threshold by loading it with a component malaligned in varus. This raises the possibility of fatigue failure being another independent mode of failure of TKA.
Liau et al8 and D’Lima et al9 found that the stress within the polyethylene component of a TKA varied by design and position, with the highest stresses seen in malpositioned, highly-conforming flat-on-flat designs. They highlighted the importance of both prosthetic design and positioning on resultant stresses, with D’Lima et al9 also noting condylar lift-off as a risk factor for increased stress.
All of these studies contribute to the concept that factors predicting longevity are not limited to the coronal alignment of the implants, but include bone quality and implant design, conformity and positioning.
Kinematic alignment – a solution to functional limitation following TKA?
One strategy to combat the functional limitations of a prosthetic knee has been to restore knee kinematics by aligning the prosthetic joint with the axes of rotation of the healthy knee.
Howell et al10 described the use of custom cutting guides to restore knee alignment, resulting in 75% of patients undergoing implantation of the tibial component in greater than 3° of varus. Despite this, no catastrophic failures were seen at a mean follow-up of 38 months (31 to 43). Similar results were seen in Dossett et al’s11 randomised controlled trial of kinematically versus mechanically aligned TKAs with two year follow-up. The authors aimed to achieve the same mechanical alignment in both groups but the kinematically aligned group had an oblique joint line in 2.5° of varus, whereas the mechanically aligned group had a neutral one. The authors found better functional results and pain relief in the kinematic group; while 38 months only offers short-term follow-up, the absence of early failures is reassuring.
The target parameters in kinematic knee arthroplasty are derived from biomechanical investigation of the native knee, which has focused on identifying the location of its flexion-extension axis (FEA). A number of authors have suggested that this is coincident with the transepicondylar axis (TEA), a line joining the origins of the medial and lateral collateral ligaments.12-15 In the axial plane this has been shown to hold true15 but Eckhoff et al have demonstrated that these axes are significantly different in coronal and sagittal location, with the FEA lying posterior and internally rotated in relation to the TEA (Fig. 2).16,17
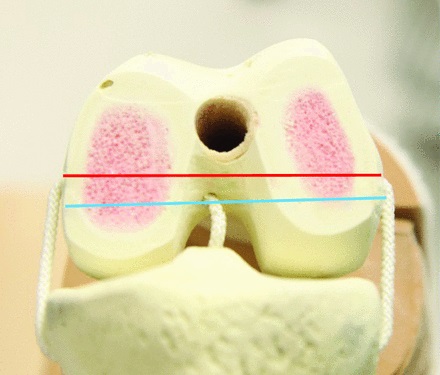
Fig. 2
A sawbone model of the distal femur illustrating the relationship between the trans--epicondylar axis (red line) and flexion-extension axis (blue line) after Eckhoff et al.17
Kinematic knee alignment seeks to align the prosthetic joint with the FEA, differing from conventional TKA mainly by relative internal rotation of the femoral component as a result of symmetrical posterior femoral resections, and varus positioning of the tibial component. This results in greater physiological laxity of the lateral collateral ligament, increased joint line obliquity and also allows the knee to flex about its pre-existing axis within an already balanced soft-tissue envelope.
Concern exists over a widespread adoption of this approach. Although the aforementioned studies have demonstrated some encouraging results, these are yet to be replicated more widely. It also remains to be seen whether this alignment can be achieved with standard instrumentation.18 Internal rotation of the femoral component may also result in patellofemoral maltracking, particularly in components with a narrow trochlea.
Although it has been demonstrated that an increased risk of loosening exists when implanting the tibial component in varus, Howell et al10 showed that in kinematically-aligned TKA, varus positioning of the tibia is compensated for by valgus positioning of the femoral component.
Should kinematic alignment gain widespread acceptance, the multi-factorial aetiology of failure in TKA should stimulate improvements in implant design and fixation, in order to accommodate the increased stresses generated by a kinematically--aligned joint. Biological, uncemented tibial fixation with the capacity to adapt and remodel may provide long-lasting fixation in less mechanically favourable conditions.
Uncemented fixation in TKA
Cemented fixation featured in 95% of TKAs submitted to the National Joint Registry (NJR) for England and Wales in 2014 (Fig. 3).19 While TKA as a whole exhibits good longevity, the survival in the under 55 age group is substantially less than in the over 80 age group and the choice of fixation may have some bearing on this.
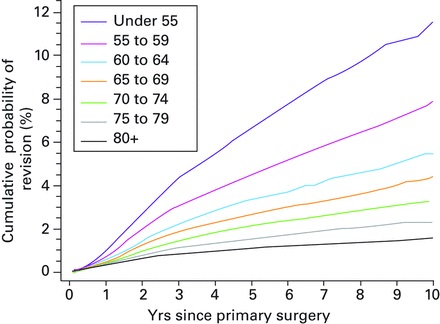
Fig. 3
Kaplan-Meier curve of the cumulative percentage probability of a first revision of primary knee arthroplasty by age group (From: NJR 11th Annual Report 2014).19
The direct fixation of implants to host bone offers several advantages. Biological fixation may have the capacity to remodel in response to injury or disruption. The avoidance of cement also confers a theoretical reduction in the volume of debris introduced to the joint and resultant third body wear. Long-term stability requires achieving solid primary fixation and bony ingrowth or on-growth. Uncemented fixation in TKA has not yet seen the same uptake as in total hip arthroplasty.19 characterised by a very different biomechanical environment and the ability to achieve solid primary fixation with either press-fit, equatorial grip on the acetabular side or interference fit on the femoral side. By contrast, knee prostheses are not contained by the bones they resurface and must therefore achieve primary stability by a combination of different methods. On the femoral side, this is achieved through press-fit of the implant to -precisely cut and sized femoral condyles. On the tibial side, different methods have been employed, ranging from press-fit interference lugs to screw fixation. With good implant design and meticulous surgical technique, however, good results can be achieved with uncemented TKA. Pulido et al20 described similar five-year results for tantalum tibial components whether or not they were implanted with cement. Furthermore, the NJR report of 2014 found that uncemented designs have a ten-year survivorship of 92% to 97% depending on the design.19 This echoes Cross and Parish’s21 ten-year survivorship of 99% in 1000 patients with hydroxyapatite-oated uncemented components, similar in turn to Oliver et al’s22 93% survivorship at 11 years. There exists, however, insufficient data on unconventional component positioning in uncemented TKA.
The high demands of modern arthroplasty patients dictate that both prostheses and the surgical technique by which they are implanted must evolve in order to keep pace with these expectations. Such evolution must address alignment and fixation.
1 Freeman MA , SwansonSA, ToddRC. Total replacement of the knee using the Freeman-Swanson knee prosthesis. Clin Orthop Relat Res1973;94:153–170.CrossrefPubMed Google Scholar
2 Jones EC , InsallJN, InglisAE, RanawatCS. GUEPAR knee arthroplasty results and late complications. Clin Orthop Relat Res1979;140:145–152.PubMed Google Scholar
3 Insall J , ScottWN, RanawatCS. The total condylar knee prosthesis. A report of two hundred and twenty cases. J Bone Joint Surg [Am]1979;61-A:173–180.PubMed Google Scholar
4 Freeman MA , SculcoT, ToddRC. Replacement of the severely damaged arthritic knee by the ICLH (Freeman-Swanson) arthroplasty. J Bone Joint Surg [Br]1977;59-B:64–71.CrossrefPubMed Google Scholar
5 Insall JN , HoodRW, FlawnLB, SullivanDJ. The total condylar knee prosthesis in gonarthrosis. A five to nine-year follow-up of the first one hundred consecutive replacements. J Bone Joint Surg [Am]1983;65-A:619–628.PubMed Google Scholar
6 Perillo-Marcone A , TaylorM. Effect of varus/valgus malalignment on bone strains in the proximal tibia after TKR: an explicit finite element study. J Biomech Eng2007;129:1–11.CrossrefPubMed Google Scholar
7 Wong J , SteklovN, PatilS, et al.Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J Orthop Res2011;29:347–353.CrossrefPubMed Google Scholar
8 Liau JJ , ChengCK, HuangCH, LoWH. The effect of malalignment on stresses in polyethylene component of total knee prostheses--a finite element analysis. Clin Biomech (Bristol, Avon)2002;17:140–146.CrossrefPubMed Google Scholar
9 D’Lima DD , ChenPC, ColwellCW Jr. Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res2001;392:232–238.CrossrefPubMed Google Scholar
10 Howell SM , HowellSJ, KuznikKT, CohenJ, HullML. Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category?Clin Orthop Relat Res2013;471:1000–1007.CrossrefPubMed Google Scholar
11 Dossett HG , EstradaNA, SwartzGJ, LeFevreGW, KwasmanBG. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J2014;96-B:907–913.CrossrefPubMed Google Scholar
12 Hollister AM , JatanaS, SinghAK, SullivanWW, LupichukAG. The axes of rotation of the knee. Clin Orthop Relat Res1993;290:259–268.PubMed Google Scholar
13 Churchill DL , IncavoSJ, JohnsonCC, BeynnonBD. The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res1998;356:111–118.CrossrefPubMed Google Scholar
14 Akagi M , YamashitaE, NakagawaT, AsanoT, NakamuraT. Relationship between frontal knee alignment and reference axes in the distal femur. Clin Orthop Relat Res2001;388:147–156.CrossrefPubMed Google Scholar
15 Asano T , AkagiM, NakamuraT. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty2005;20:1060–1067.CrossrefPubMed Google Scholar
16 Eckhoff DG , BachJM, SpitzerVM, et al.Three-dimensional morphology and kinematics of the distal part of the femur viewed in virtual reality. Part II. J Bone Joint Surg [Am]2003;85-A (suppl 4):97–104.CrossrefPubMed Google Scholar
17 Eckhoff D , HoganC, DiMatteoL, RobinsonM, BachJ. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res2007;461:238–244.CrossrefPubMed Google Scholar
18 Howell SM , PapadopoulosS, KuznikKT, HullML. Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc2013;21:2271–2280.CrossrefPubMed Google Scholar
19 No authors listed. The National Joint Registry 11thAnnual Report. http://www.njrcentre.org.uk/njrcentre/LinkClick.aspx?link=http%3a%2f%2fwww.njrreports.org.uk%2f& tabid=86& portalid=0& mid=418 (date last accessed 17 July 2015). Google Scholar
20 Pulido L , AbdelMP, LewallenDG, et al.Trabecular Metal Tibial Components Were Durable and Reliable in Primary TotalKnee Arthroplasty: A Randomized Clinical Trial. Clin Orthop Relat Res2015;473:34–42. Google Scholar
21 Cross MJ , ParishEN. A hydroxyapatite-coated total knee replacement: prospective analysis of 1000 patients. J Bone Joint Surg [Br]2005;87-B:1073–1076.CrossrefPubMed Google Scholar
22 Oliver MC , Keast-ButlerOD, HinvesBL, ShepperdJA. A hydroxyapatite-coated Insall-Burstein II total knee replacement: 11-year results. J Bone Joint Surg [Br]2005;87-B:478–482.CrossrefPubMed Google Scholar
This is an open-access article distributed under the terms of the Creative Commons Attributions licence CC-BY-NC, which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
Author contributions:
S. Oussedik: Wrote first draft.
M. P. Abdel: Amended first draft, approved subsequent changes.
M. B. Cross: Amended first draft, approved subsequent changes.
F. S. Haddad: Original concept, approved subsequent changes.
This research/ study/ project was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This article was primary edited by P. Page.









