Abstract
Aims
The aim of this study was to conduct a cross-sectional, observational cohort study of patients presenting for revision of a total hip, or total or unicompartmental knee arthroplasty, to understand current routes to revision surgery and explore differences in symptoms, healthcare use, reason for revision, and the revision surgery (surgical time, components, length of stay) between patients having regular follow-up and those without.
Methods
Data were collected from participants and medical records for the 12 months prior to revision. Patients with previous revision, metal-on-metal articulations, or hip hemiarthroplasty were excluded. Participants were retrospectively classified as ‘Planned’ or ‘Unplanned’ revision. Multilevel regression and propensity score matching were used to compare the two groups.
Results
Data were analyzed from 568 patients, recruited in 38 UK secondary care sites between October 2017 and October 2018 (43.5% male; mean (SD) age 71.86 years (9.93); 305 hips, 263 knees). No significant inclusion differences were identified between the two groups. For hip revision, time to revision > ten years (odds ratio (OR) 3.804, 95% confidence interval (CI) (1.353 to 10.694), p = 0.011), periprosthetic fracture (OR 20.309, 95% CI (4.574 to 90.179), p < 0.001), and dislocation (OR 12.953, 95% CI (4.014 to 41.794), p < 0.001), were associated with unplanned revision. For knee, there were no associations with route to revision. Revision after ten years was more likely for those who were younger at primary surgery, regardless of route to revision. No significant differences in cost outcomes, length of surgery time, and access to a health professional in the year prior to revision were found between the two groups. When periprosthetic fractures, dislocations, and infections were excluded, healthcare use was significantly higher in the unplanned revision group.
Conclusion
Differences between characteristics for patients presenting for planned and unplanned revision are minimal. Although there was greater healthcare use in those having unplanned revision, it appears unlikely that routine orthopaedic review would have detected many of these issues. It may be safe to disinvest in standard follow-up provided there is rapid access to orthopaedic review.
Cite this article: Bone Joint J 2022;104-B(1):59–67.
Take home message
Indications for revision of hip and knee (total and unicompartmental) arthroplasties in the ten years post-primary surgery are symptomatic.
Unplanned revision of hip arthroplasty was more likely for patients with arthroplasty in situ > ten years, and if revised for periprosthetic fracture or dislocation; there was no similar pattern for knee arthroplasty.
The indication from this study is that disinvestment in routine follow-up services before ten years does not adversely affect revision surgery for hips or knees, provided that rapid access self-referral is available for symptomatic patients.
Introduction
More than 200,000 total hip and knee arthroplasties are carried out annually in the UK.1 Arthroplasty failure rates for standard implants are low, at < 5% at ten years. British Orthopaedic Association (BOA) guidelines recommend following joint replacement follow-up is undertaken at one, seven, and every three years thereafter (and more often with novel or modified implants).2 However, recent Scottish Committee for Orthopaedics and Trauma guidance recommends discontinuation of routine follow-up for Orthopaedic Data Evaluation Panel (ODEP) 10A rated implants.3 Rarely, catastrophic failure can occur if problems are not detected early, which may lead to more complex, costly revision surgery.
With modern surgical techniques and implant improvements, there is now often less urgency to proceed to revision for asymptomatic changes. Anecdotal evidence suggests that there are also fewer asymptomatic impending failures. Furthermore, evidence suggests that due to increasing financial pressures and waiting list demands, many hospitals have reduced or stopped routine arthroplasty follow-up.4 In the post-COVID-19 era, such pressures on orthopaedic services may increase further.5 Understanding the impact of disinvestment in hip and knee arthroplasty follow-up services for the individual patients is therefore timely.
We conducted a cross-sectional, observational study of patients presenting for revision of a total hip, and total or unicompartmental knee arthroplasty. The primary objective was to determine the proportion of revision patients who undergo ‘planned’ revision surgery identified through regular orthopaedic review. The secondary objective was to explore differences in symptoms, healthcare use, reason for revision, and the revision surgery (time in surgery, components, length of stay) between those patients identified for revision through regular follow-up (planned revision) and those identified outside an orthopaedic/follow-up pathway (unplanned revision).
Methods
Setting and participants
A cross-sectional, observational study of elective and emergency patients presenting for revision hip or knee arthroplasty surgery was carried out. In all, 568 articipants were recruited between October 2017 and October 2018 from 38 hospitals in England, selected to provide regional spread, which consisted of a mix of district general hospitals and tertiary referral centres. Inclusion criteria included age ≥ 18 years, and elective or emergency presentation for revision surgery of primary hip or knee arthroplasty. Exclusion criteria were previous revision surgery, metal-on-metal primary hip arthroplasty, and hip hemiarthroplasty.
Ethics, consent, and permissions
Ethical approval was received from the North West Haydock Research Ethics Committee Yorkshire (17/NW/0469). All participants provided written informed consent.
Data collection
Data were captured from participants during their inpatient stay post-revision surgery and from medical records. Data collected included social status, working status, experience of orthopaedic follow-up pathway, and pathway to current revision surgery. Participant data were corroborated and supplemented with data from medical notes: demographic details; general practitioner (GP) and orthopaedic appointments, medication related to recent problems with the arthroplasty; medical history; primary arthroplasty history; reasons for scheduling revision; and details of revision surgery (Supplementary Material).
Classification of route to revision
Based on collected data, participants were classified as ‘unplanned revision identified outside a clear orthopaedic pathway’ (UR) or ‘planned revision identified through an orthopaedic/follow-up pathway’ (PR) according to an algorithm (Figure 1). The decision algorithm incorporated data collected by the research nurse (RN) and from the patient-reported questionnaire (Supplementary Material). The algorithm was developed following a pilot study on this topic,6 and the knowledge that, if a patient was receiving follow-up, regular orthopaedic review would have preceded the revision surgery. Collected data were used to identify those who came to revision through this route compared with those patients with minimal or no orthopaedic review prior to revision. A 12-month cut-off from time of referral from primary care to revision surgery was incorporated because, at the time of the study, the period from referral to surgery was approximately nine months (22- to 24-week wait to first orthopaedic appointment, eight to ten weeks for screening and results, and two to three weeks from preoperative evaluation to surgery). The choice of a 12-month cut-off was designed to differentiate between those participants who came to revision surgery without regular orthopaedic assessment (UR), and those who were in a regular follow-up programme or were being monitored for progression of potentially damaging changes around the joint replacement (PR).
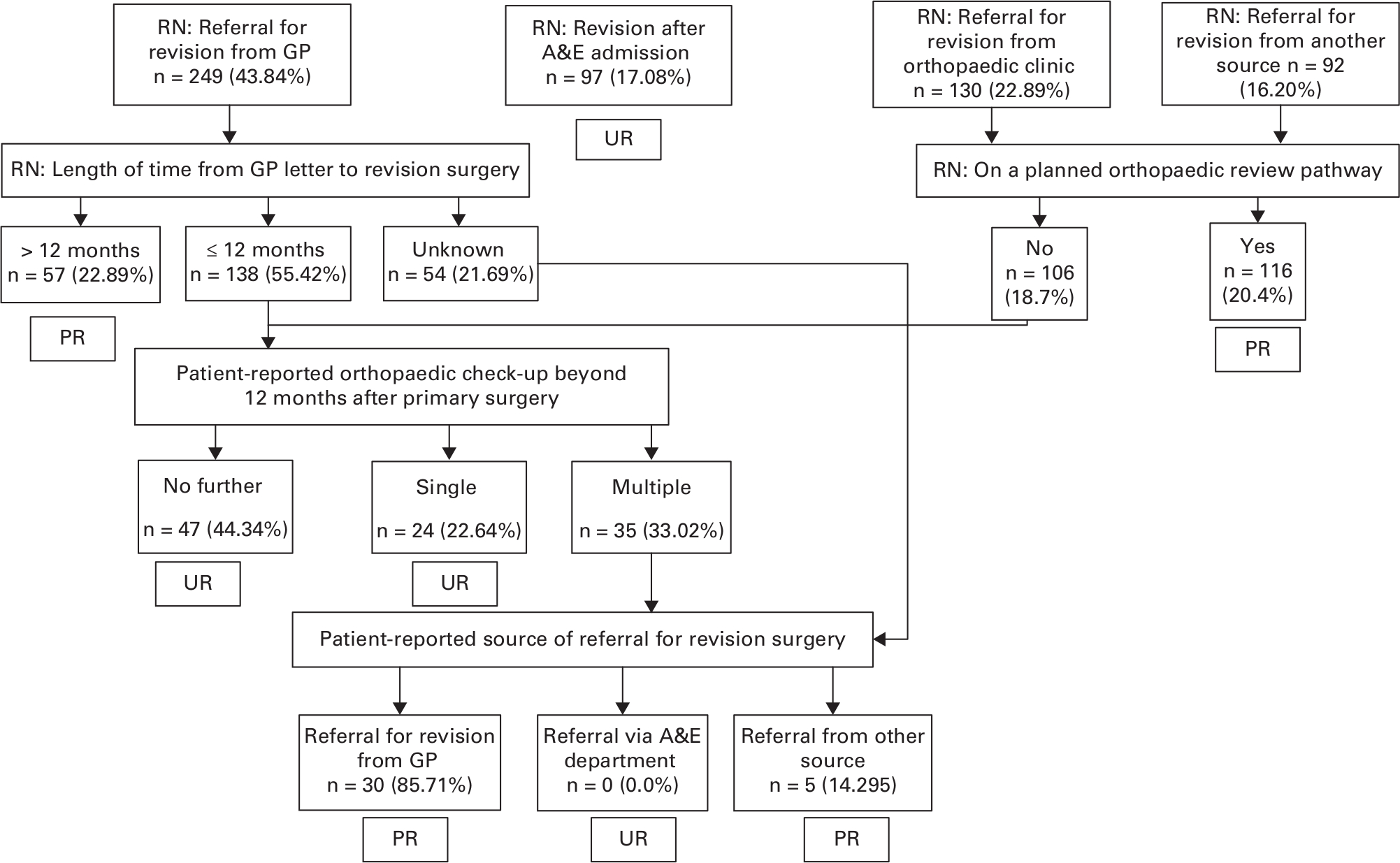
Fig. 1
Algorithm for classification of 568 participants into the planned (PR) and unplanned revision (UR) groups. A&E, accident and emergency; GP, general practitioner; RN: information collected by Research Nurse.
Outcomes
The primary outcome was ‘revision identified through routine orthopaedic/follow-up pathway’. Three cost variable outcomes were used for the exploratory cost analysis: length of stay (LOS) in acute hospital for revision surgery (days), time in surgery (hours), and consultation with any health professionals in the 12 months prior to revision. Components used in revision surgery were categorized as standard primary implants, off-the-shelf revision implants, or custom-made components.
Predictors
The following predictors of ‘planned’ revision surgery were examined: reason for primary surgery (pathology); complications at time of primary operation; ability to live independently before revision; caring responsibilities or receiving care prior to revision; reason for revision; time from primary to revision surgery; comorbidities (Charlson Comorbidity Index); age at revision; and sex.
Sample size
Sample size was calculated based on sampling within 25 orthopaedic centres. Accounting for variation in size, with an anticipation of about 45 patients per centre, and assuming a 60% recruitment rate, a conservative assumption of 27 patients per centre was made, giving a total of 675. The intraclass correlation coefficient (ICC) for our primary outcome was unknown, but from previous research,4 indicated a conservative ICC = 0.05. This gave a design factor of 2.3 and an effective sample size of 293 after accounting for clustering. The enrolment of 38 centres reduced the design factor to 1.6 and the minimum sample size required to 455. From previous research,4 the rate of our primary outcome (‘planned’ revision identified through routine orthopaedic follow-up) was estimated at 20%. The effective number of events would be 58. As estimated by Peduzzi et al,7 there would be sufficient power for robust logistic regression for up to five potential risk factors. There would be 12 effective events per risk factor, greater than the ten recommended providing sufficient power for the primary analysis.
Statistical analysis
Patient characteristics, characteristics of primary surgery, and outcomes of interest were cross-tabulated by planned/unplanned revision status. To indicate association, two-sample t-tests were used for continuous variables, Pearson’s chi-squared tests for categorical variables, and Mann-Whitney U tests for comparing medians. Using multilevel logistic regression incorporating a random-intercept for hospital, an adjusted model was used to establish the propensity for follow-up, as the study data were derived from a convenience sample. Odds ratios (ORs) complete with 95% confidence intervals (CIs) were reported for each factor and covariate retained in the final parsimonious propensity model. Intraclass correlation was reported to reflect the hospital contribution and the range of ORs associated with the random effects.
To explore potential cost implications of planned versus unplanned revision surgery, propensity score matching was undertaken to construct PR and UR cohorts balancing covariates that predict membership of the two groups. A propensity model was constructed for the propensity, or probability, of a patient receiving UR. Patients from the PR group were matched 1:1 with patients from the UR group by selecting the patient with the nearest matching propensity score (calculated probability). This produced a cohort of patients where the propensity for UR was matched, based on the patient characteristics that were known to be associated with group membership. These matching variables were complications prior to primary surgery; hip or knee arthroplasty; infection, periprosthetic fracture (PPF), or dislocation as the reason for revision; and time to revision (Supplementary Table ii). Since two separate analytical approaches were used a correction factor was applied to the level of significance, reducing the threshold for statistical significance from a p-value = 0.05 to 0.025 (p = 0.05/2).
Results
Participants
A total of 647 participants were enrolled; however, 79 were subsequently excluded due to ineligibility (revision-of-revision (n = 23), second-stage revision (n = 10), metal-on-metal (n = 4), hemiarthroplasty (n = 1), primary surgery (n = 1), surgery delayed/cancelled (n = 19), withdrawal of consent (n = 9), or missing data (n = 12)). Data were therefore analyzed from 568 participants, 43.5% male (247/568), mean age 72 years (standard deviation (SD) 9.9) (9.9) (Table I). Of these, 305 presented for revision of a total hip arthroplasty and 263 for revision of a total or unicompartmental knee arthroplasty (Table II). Time from primary surgery to revision in the combined group was < five years for 179 cases (32%), five to ten years for 109 (19%), > ten years for 222 (39%), and unspecified in 58 cases (10%) (Table II).
Table I.
Participant characteristics.
| Characteristic | Hip | Knee | ||||
|---|---|---|---|---|---|---|
| Unplanned revision (n = 199) |
Planned revision (n = 106) |
p-value* | Unplanned revision (n = 161) |
Planned revision (n = 102) |
p-value* | |
| Male, n (%) | 93 (46.7) | 42 (39.6) | 0.285 | 70 (43.5) | 42 (41.2) | 0.810 |
| Mean age (SD) | 74.08 (10.78) | 71.58 (10.4) | 0.053 | 70.87 (8.68) | 69.32 (8.67) | 0.161 |
| Mean CCI (SD) | 3.52 (1.64) | 3.35 (1.78) | 0.408 | 3.21 (1.65) | 3.04 (1.62) | 0.408 |
| Able to live independently prior to revision surgery, n (%) | 177 (88.9) | 87 (82.9) | 0.189 | 142 (88.2) | 89 (88.1) | > 0.999 |
| Caring responsibilities, n (%) | 28 (14.1) | 13 (12.5) | 0.839 | 25 (15.7) | 14 (13.7) | 0.792 |
| Receiving care, n (%) | 30 (15.2) | 21 (20.2) | 0.352 | 29 (18.2) | 18 (17.8) | > 0.999 |
| Employed/self-employed prior to revision surgery, n (%) | 36 (18.4) | 24 (23.1) | 0.413 | 32 (20.0) | 25 (25.3) | 0.403 |
| ASA grade, n (%) | 0.293† | 0.161† | ||||
| 1 | 12 (6.5) | 9 (8.7) | 7 (4.5) | 4 (4.0) | ||
| 2 | 90 (48.4) | 57 (55.3) | 78 (50.3) | 63 (62.4) | ||
| 3 | 80 (43) | 37 (35.9) | 70 (45.2) | 33 (32.7) | ||
| 4 | 4 (2.2) | 0 | 0 | 1 (1.00) | ||
| Smoking, n (%) | 0.586 | 0.789 | ||||
| No | 122 (63.2) | 60 (57.1) | 101 (63.9) | 61 (61.6) | ||
| Yes | 12 (6.2) | 8 (7.6) | 8 (5.1) | 7 (7.1) | ||
| Ex | 59 (32.2) | 37 (35.2) | 49 (31) | 31 (31.3) | ||
-
*
Chi-squared test.
-
†
ASA Grades 3 and 4 were combined for the chi-squared test.
-
ASA, American Society of Anesthesiologists; CCI, Charlson Comorbidity Index; SD, standard deviation.
Table II.
Characteristics of primary and revision surgery. All p-values were calculated using chi-squared test.
| Characteristic | Hip | Knee | ||||
|---|---|---|---|---|---|---|
| Unplanned revision (n = 199) |
Planned revision (n = 106) |
p-value* | Unplanned revision (n = 161) |
Planned revision (n = 102) |
p-value* | |
| Diagnosis at primary surgery | ||||||
| OA | 135 (67.8) | 66 (62.3) | 0.395 | 116 (72.0) | 79 (77.5) | 0.406 |
| Arthritis | 14 (7.0) | 7 (6.6) | 1.000 | 14 (8.7) | 9 (8.8) | > 0.999 |
| Trauma | 16 (8.0) | 10 (9.4) | 0.842 | 11 (6.8) | 6 (5.9) | 0.962 |
| Congenital | 4 (2.0) | 3 (2.8) | 0.957 | 1 (0.6) | 0 (0.0) | > 0.999 |
| Other | 29 (14.6) | 15 (14.2) | 1.000 | 23 (14.3) | 11 (10.8) | 0.525 |
| Don’t know | 11 (5.5) | 10 (9.4) | 0.296 | 9 (5.6) | 3 (2.9) | 0.484 |
| Complications after first operation on hip/knee | 57 (28.9) | 46 (43.8) | 0.014 | 62 (38.5) | 47 (47.0) | 0.221 |
| Infection | 10 (5.0) | 16 (15.1) | 0.005 | 18 (11.2) | 12 (11.8) | > 0.999 |
| Dislocation | 29 (14.6) | 8 (7.5) | 0.108 | 5 (3.1) | 2 (2.0) | 0.866 |
| Other | 24 (12.1) | 25 (23.6) | 0.014 | 49 (30.4) | 39 (38.2) | 0.241 |
| Mean time to revision, yrs (SD) | 0.142 | 0.092 | ||||
| < 5 (reference) | 46 (23.12) | 36 (33.96) | 51 (31.68) | 46 (45.10) | ||
| 5 to 10 | 41 (20.60) | 14 (13.21) | 33 (20.50) | 21 (20.59) | ||
| > 10 | 89 (44.72) | 46 (43.40) | 58 (36.02) | 29 (28.43) | ||
| Not specified | 23 (11.56) | 10 (9.4) | 19 (11.80) | 6 (5.88) | ||
| Reason for revision | ||||||
| Infection | 15 (7.5) | 12 (11.3) | 0.370 | 32 (19.9) | 14 (13.7) | 0.266 |
| Aseptic loosening | 85 (42.7) | 50 (47.2) | 0.532 | 60 (37.3) | 32 (31.4) | 0.399 |
| Stiffness | 2 (1.0) | 3 (2.8) | 0.470 | 9 (5.6) | 5 (4.9) | > 0.999 |
| Pain | 69 (34.7) | 56 (52.8) | 0.003 | 85 (52.8) | 59 (57.8) | 0.500 |
| Wear | 14 (7.0) | 11 (10.4) | 0.427 | 16 (9.9) | 14 (13.7) | 0.458 |
| Osteolysis | 13 (6.5) | 13 (12.3) | 0.136 | 7 (4.3) | 3 (2.9) | 0.802 |
| Periprosthetic fracture | 33 (16.6) | 3 (2.8) | 0.001 | 9 (5.6) | 0 (0.0) | 0.037 |
| Implant failure | 9 (4.5) | 3 (2.8) | 0.678 | 12 (7.5) | 6 (5.9) | 0.810 |
| OA progression | 0 (0.0) | 0 (0.0) | - | 5 (3.1) | 6 (5.9) | 0.435 |
| Dislocation | 47 (23.6) | 10 (9.4) | 0.004 | 5 (3.1) | 0 (0.0) | 0.182 |
| Instability | 3 (1.5) | 3 (2.8) | 0.719 | 12 (7.5) | 8 (7.8) | > 0.999 |
| Other | 5 (2.5) | 1 (0.9) | 0.612 | 0 (0.0) | 0 (0.0) | |
-
*
Chi-squared test.
-
OA, osteoarthritis; SD, standard deviation.
Route to revision surgery
Applying the algorithm (Figure 1), 208 patients (37%) were classified as having had planned revision surgery through an orthopaedic/follow-up pathway (PR group; 106 hips, 102 knees) and 360 were classified as having unplanned revision surgery (UR group; 199 hips, 161 knees). Of the latter, 97 participants (17%) had revision surgery following admission via the emergency department.
There were no significant differences in participant characteristics between the two groups for either hip or knee (Table I and Table II). Participants in the hip PR group were more likely than the UR group to have had complications following their primary surgery (p = 0.014, chi-squared test) and to present with pain as a reason for revision (p = 0.003, chi-squared test). For both hip and knee patients, PPF as the reason for revision was more likely for UR (p = 0.001) (Table II).
We found that revision after ten years was more likely for those who were younger at primary surgery, regardless of route to revision (Table III). Patients having earlier revision (< ten years post-primary) for knee were younger at time of primary surgery (knee, mean age 64.25 years (SD 8.401); hip, mean age 67.10 years (SD 10.68); p = 0.013, two-sample t-test), than they were for hip. For later revision (> ten years), there were no differences in age at primary surgery between hip or knee.
Table III.
Age at primary surgery.
| Mean age at primary surgery, yrs (SD) | Hip | Knee | ||||
|---|---|---|---|---|---|---|
| Time to revision ≤ 10 yrs (n = 137) | Time to revision > 10 yrs (n = 135) | p-value* | Time to revision ≤ 10 yrs (n = 151) | Time to revision > 10 yrs (n = 87) | p-value* | |
| Planned revision | 66.58 (10.37) | 55.18 (12.21) | < 0.001 | 63.91 (8.92) | 55.94 (12.26) | < 0.001 |
| Unplanned revision | 67.41 (10.89) | 57.60 (11.10) | 0.001 | 64.54 (8.00) | 57.61 (9.94) | < 0.001 |
-
*
Two-sample t-test.
-
SD, standard deviation.
For hip revision, there were no differences in the reasons for seeking medical help between PR and UR; however, PR patients were more likely to report that their other hip was causing a problem. For knee revision, PR patients were more likely to report difficulty walking or that something did not feel right in the affected knee (Table IV). However, no difference was found in responses to, ‘did your hip/knee feel safe to walk on?’ between UR and PR for either hip or knee (Supplementary Table i).
Table IV.
Route to revision surgery.
| Reason for seeking medical help, n (%) | Hip | Knee | ||||
|---|---|---|---|---|---|---|
| Unplanned revision (n = 199) |
Planned revision (n = 106) |
p-value* | Unplanned revision (n = 161) |
Planned revision (n = 102) |
p-value* | |
| A health professional told me it needed to be redone | 59 (29.6) | 33 (31.1) | 0.809 | 39 (24.2) | 26 (25.5) | 0.782 |
| I had pain in the affected hip/knee | 116 (58.3) | 73 (68.9) | 0.078 | 122 (75.8) | 74 (72.5) | 0.649 |
| I had difficulty walking on the affected hip/knee | 79 (39.7) | 53 (50.0) | 0.090 | 87 (54.0) | 69 (67.6) | 0.022 |
| Something did not feel right in the affected hip/knee | 74 (37.2) | 35 (33.0) | 0.451 | 67 (41.6) | 55 (53.9) | 0.043 |
| My other hip/knee was causing a problem | 5 (2.5) | 9 (8.5) | 0.023 | 17 (10.6) | 11 (10.8) | > 0.999 |
-
*
Chi-squared test.
Reasons for revision
For hip revisions occurring < five years post-primary surgery, dislocation and PPF were the most common reasons for revision in the UR group, and pain and infection in the PR group (Table V). For hip revisions occurring five to ten years post-primary surgery, pain was the most common reason for revision in both groups, followed by aseptic loosening. Beyond ten years, aseptic loosening was the most common reason for revision in both groups.
Table V.
Most common reasons for revision by joint, follow-up pathway, and time to revision.
| Time to revision | Hip, n (%) | Knee, n (%) | ||||||
|---|---|---|---|---|---|---|---|---|
| Unplanned revision | Planned revision | Unplanned revision | Planned revision | |||||
| < 5 yrs | ||||||||
| Dislocation | 15 (32.6) | Pain | 18 (50) | Pain | 25 (49) | Pain | 25 (54.3) | |
| Periprosthetic fracture | 13 (28.3) | Infection | 10 (27.8) | Infection | 16 (31.4) | Infection | 13 (28.3) | |
| Pain | 12 (26.1) | Dislocation | 7 (19.4) | Aseptic loosening | 15 (29.4) | Aseptic loosening | 9 (16.9) | |
| Infection | 7 (15.2) | Aseptic loosening | 6 (16.7) | Instability | 7 (13.7) | Implant failure | 4 (8.7) | |
| Aseptic loosening | 6 (13) | Stiffness | 2 (5.6) | Stiffness | 5 (9.8) | Stiffness | 3 (6.5) | |
| 5 to 10 yrs | ||||||||
| Pain | 15 (36.6) | Pain | 11 (78.6) | Pain | 20 (60.6) | Pain | 15 (71.4) | |
| Aseptic loosening | 15 (36.6) | Aseptic loosening | 7 (50) | Aseptic loosening | 11 (33.3) | Aseptic loosening | 6 (28.6) | |
| Dislocation | 13 (31.7) | Infection | 1 (7.1) | Infection | 8 (24.2) | Instability | 4 (19) | |
| Infection | 5 (12.2) | Dislocation | 1 (7.1) | Instability | 3 (9.1) | Wear | 3 (14.3) | |
| Periprosthetic fracture | 4 (9.8) | Osteolysis | 1 (7.1) | Periprosthetic fracture | 3 (9.1) | Implant failure | 2 (9.5) | |
| > 10 yrs | ||||||||
| Aseptic loosening | 55 (61.8) | Aseptic loosening | 31 (67.4) | Pain | 33 (56.9) | Pain | 16 (55.2) | |
| Pain | 32 (36) | Pain | 23 (50.0) | Aseptic loosening | 27 (46.6) | Aseptic loosening | 14 (48.3) | |
| Osteolysis | 12 (13.5) | Wear | 8 (17.4) | Wear | 10 (17.2) | Wear | 9 (31) | |
| Periprosthetic fracture | 11 (12.4) | Osteolysis | 8 (17.4) | Implant failure | 6 (10.3) | Osteolysis | 3 (10.3) | |
| Wear | 11 (12.4) | Dislocation | 2 (4.3) | Osteolysis | 4 (6.9) | OA progression | 2 (6.9) | |
-
OA, osteoarthritis.
For knee arthroplasty, pain was the most common reason for revision in both groups and at all timepoints post-primary surgery. However, for earlier revisions (< five years), infection was the second most common reason for revision in both groups, while for later timepoints aseptic loosening was the second most common reason.
Predictors of route of presentation for revision surgery
Hospital effect: the ICC was 0.081, indicating that 8% of the follow-up pathway is explained by between-hospital differences. The likelihood ratio statistic was 101.73 (one degree of freedom), providing strong evidence that the between-hospital variance was not zero.
Participant characteristics: in the hip revision group, time to revision > ten years (OR 3.804, 95% CI (1.353 to 10.694), p = 0.011), PPF (OR 20.309, 95% CI (4.574 to 90.179), p < 0.001), and dislocation (OR 12.953, 95% CI (4.014 to 41.794), p < 0.001) were associated with UR (Table VI). For knee revision, there were no associations with UR.
Table VI.
Table of odds ratios for the multilevel regression model.
| Variable | Hip | Knee | ||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Intercept | 0.201 (0.040 to 1.003) | 0.050 | 0.897 (0.189 to 4.266) | 0.891 |
| Primary surgery due to OA | 0.993 (0.523 to 1.887) | 0.983 | 0.511 (0.235 to 1.108) | 0.089 |
| Complications at primary surgery | 0.542 (0.265 to 1.107) | 0.093 | 0.806 (0.417 to 1.559) | 0.522 |
| CCI | 0.891 (0.709 to 1.119) | 0.320 | 1.020 (0.811 to 1.284) | 0.865 |
| Lived independently prior to revision | 2.536 (0.930 to 6.916) | 0.069 | 1.328 (0.566 to 3.114) | 0.515 |
| Caring responsibilities | 1.143 (0.465 to 2.808) | 0.771 | 1.425 (0.576 to 3.528) | 0.443 |
| Receiving care | 0.971 (0.390 to 2.416) | 0.949 | 0.897 (0.189 to 4.266) | 0.891 |
| Employed/self-employed | 0.735 (0.315 to 1.716) | 0.477 | 0.511 (0.235 to 1.108) | 0.089 |
| Reason for revision (surgical report) | ||||
| Infection | 2.461 (0.747 to 8.112) | 0.139 | 2.946 (1.046 to 8.298) | 0.041 |
| Aseptic loosening | 1.473 (0.698 to 3.107) | 0.309 | 1.356 (0.629 to 2.922) | 0.437 |
| Stiffness | 0.687 (0.082 to 5.767) | 0.730 | 2.425 (0.545 to 10.780) | 0.245 |
| Pain | 0.969 (0.501 to 1.877) | 0.926 | 1.037 (0.530 to 2.030) | 0.915 |
| Wear | 0.981 (0.339 to 2.835) | 0.971 | 0.706 (0.272 to 1.832) | 0.474 |
| Osteolysis | 0.706 (0.249 to 2.003) | 0.513 | 1.861 (0.286 to 12.133) | 0.516 |
| Periprosthetic fracture | 20.309 (4.574 to 90.170) | < 0.001 | - | - |
| Implant failure | 2.622 (0.494 to 13.921) | 0.258 | 2.756 (0.791 to 9.599) | 0.111 |
| Dislocation | 12.953 (4.014 to 41.794) | 0.000 | - | - |
| OA progression | - | - | 0.695 (0.170 to 2.850) | 0.613 |
| Instability | 2.724 (0.371 to 20.025) | 0.325 | 1.401 (0.442 to 4.444) | 0.567 |
| Time since primary surgery, yrs (< 5 yrs (reference)) | ||||
| 5 to 10 | 2.321 (0.889 to 6.059) | 0.085 | 1.404 (0.613 to 3.216) | 0.422 |
| > 10 | 3.804 (1.353 to 10.694) | 0.011 | 2.337 (1.007 to 5.419) | 0.048 |
| Not specified | 3.619 (1.012 to 12.946) | 0.048 | 2.306 (0.632 to 8.421) | 0.206 |
| Age > 70 | 1.357 (0.599 to 3.075) | 0.566 | 1.173 (0.558 to 2.466) | 0.674 |
| Male sex | 1.975 (1.083 to 3.602) | 0.026 | 1.090 (0.577 to 2.059) | 0.791 |
-
Models were adjusted for age and sex.
-
CCI, Charlson Comorbidity Index; CI, confidence interval; OA, osteoarthritis; OR, odds ratio.
Cost analysis with propensity score matching
Based on the propensity matched cohort, time in surgery was significantly longer for UR (UR, mean 2.72 hours (SD 1.24); PR 2.48 hours (SD 1.13), p = 0.014, two-sample t-test); however when the hip and knee groups were analyzed separately this difference was no longer significant (Table VII). No other significant differences in cost outcomes, access to a health professional or complexity of revision surgery (defined by type of implant used) were found between the two groups for either hip or knee patients. There was a trend for increased LOS and increased time in surgery in the hip UR group. We reasoned that LOS may be higher in patients presenting with acute events such as PPF and dislocation, since such patients may be inpatients for a longer period prior to surgery and/or recovery time may be slower. In addition, patients presenting with infection require more complex surgery with enhanced recovery time. We therefore repeated the analysis for hips excluding all patients who presented with PPF, dislocation, or infection. Interestingly, the trend for increased LOS and increased time in surgery were lost in these exploratory analyses, suggesting these trends were driven by these three reasons for revision. However, of note, a significant difference emerged for an increased frequency of seeing a health professional prior to revision surgery (p = 0.018, chi-squared test) for UR. In addition, there was a trend for UR participants to be more likely to require a revision prosthesis (n = 49, 59%) rather than a standard primary implant (n = 30, 41%), whereas this pattern was reversed for PR participants (primary implant n = 42 (58%); revision prosthesis n = 34 (41%); p = 0.031, chi-squared test), although this did not reach significance.
Table VII.
Healthcare factors of revision surgery with cost implications.
| Factor | Hip | Hip (excluding PPF, dislocation, and infection) |
Knee | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Unplanned revision | Planned revision | p-value | Unplanned revision | Planned revision | p-value | Unplanned revision | Planned revision | p-value | |
| Median LOS for revision surgery, days (IQR) | 6.00 (3.75 to 9.75) | 5.00 (3 to 8) | 0.053* | 4.50 (3 to 7) | 5.00 (3 to 7) | 0.406* | 5.00 (3 to 8) | 4.00 (3 to 8) | 0.745* |
| Mean time for surgery, hrs (SD) | 3.00 (1.35) | 2.69 (1.31) | 0.073† | 2.94 (1.60) | 2.69 (1.61) | 0.176† | 2.48 (1.06) | 2.38 (0.86) | 0.144† |
| Seen any health professionals in last 12 months about the hip/knee arthroplasty on which you have just had an operation, n (%) | 84 (83.16) | 80 (80) | 0.691‡ | 74 (92.5) | 62 (79.5) | 0.018‡ | 77 (83.7) | 79 (84.9) | 0.158‡ |
-
*
Mann-Whitney U test.
-
†
Two-sample t-test.
-
‡
Chi-squared test.
-
IQR, interquartile range; LOS, length of stay; PPF, periprosthetic fracture; SD, standard deviation.
Discussion
In this 568-participant cross-sectional cohort, we determined the proportion of patients undergoing planned revision surgery through a clear orthopaedic pathway in 38 UK hospitals. In addition, we explored differences between these patients and those having ‘unplanned’ revision surgery. We found that 37% of participants progressed to revision surgery through an orthopaedic follow-up pathway, which was higher than the 20% predicted from our previous survey of orthopaedic follow-up routes.4 As anticipated, there was a clear nesting of outcome based on hospital, suggesting that defined pathways were still in existence in some hospitals at the time of this study, in line with previous work demonstrating wide variation in follow-up practice across the UK. It should be noted that, as a result of the COVID-19 pandemic, further practice changes are likely to have been implemented since our study was conducted.
Our exploratory analysis of differences between ‘unplanned’ and ‘planned’ revision surgery found that unplanned surgery was more likely for patients having hip revision surgery > ten years post-primary surgery and for those having surgery for PPF or dislocation. In hip revision surgery, we observed that participants having unplanned surgery required substantially more health professional appointments in the 12 months prior to revision, after we had removed diagnoses of infection, PPF and dislocation from the propensity score matching.
Discounting post-surgical problems, the need for revision is associated with longevity of the prosthesis in situ.1 In line with this, we found the highest numbers of revisions after ten years, followed by less than five years, with fewer cases presenting in the medium term. Approximately half the revision cases were identified through follow-up at < five years post-primary surgery, reducing to only one-third of cases at > ten years post-primary surgery. This may reflect local practice to reduce follow-up frequency beyond ten years,4 or to discharge patients, for example due to age, comorbidities, or because they have had no problems to date. In addition, it may be argued that revision is occurring earlier in those patients in the PR group due to more timely identification of problems. Further work is needed to understand whether these observations are due to existing patterns of service delivery, or whether there are more complex issues that affect patient care.
The finding that revision after ten years was more likely for those who were younger at primary surgery, regardless of route to revision, may reflect the prosthesis out-surviving the older patient or contraindications preventing revision. Of note, earlier knee revision participants (< ten years post-primary) were more likely to be younger than earlier hip revision participants. This potentially relates to the pooling of unicompartmental and total knee arthroplasties within our analysis.
We noted more hip revision surgeries for PPF and dislocation in the UR group. These events are highly symptomatic, occurring suddenly, with minimal or no prior detectable radiological changes. Patients will seek medical intervention acutely, therefore appearing automatically in our UR group if they attend via the emergency department (ED), whether or not they are under routine review.8 The higher incidence of infection in knee revision cases in the UR may also be explained by the rapid onset of systemic symptoms in knee infection patients.9 These patients often present through ED, with early progression to surgery. While we cannot rule out that for some patients routine follow-up may have detected earlier problems with the joint, such as implant failure, migration, or wear that subsequently progressed to dislocation or PPF, for most patients it is unlikely that follow-up would have altered their pathway.
For both hip and knee, our results show that indications for surgery < ten years post-primary surgery are symptomatic problems, suggesting routine follow-up may not be needed during this period provided there is readily available access for symptomatic individuals to patient-initiated orthopaedic review. Previous single-centre hip studies suggest that early discharge was safe for uncomplicated, ODEP-10A* rated hip arthroplasties.10,11 Beyond ten years, the highest proportion of revisions were for aseptic loosening, which is not always symptomatic, especially in earlier stages. The silent aseptic failures of joint arthroplasty are a function of implant wear, therefore occurring after ten years.12 Further work is needed to explore the need for targeted follow-up in the second decade after hip or knee arthroplasty. Potentially, registry forms collected at the time of revision surgery could be modified and extended to inform this.
We initially observed a trend for longer LOS and increased time in surgery for hips in the UR group. We reasoned that this may be driven by UR patients presenting with PPF, dislocation, and infection, since they were more likely to present acutely through the ED, resulting in an extended inpatient stay preoperatively and/or more complex surgery with increased postoperative recovery time. The trends in both LOS and time in surgery were lost once these patients were excluded. However, we observed that patients presenting for other reasons for revision, such as pain, aseptic loosening, and lysis, were substantially more likely to consult other health professionals in the previous 12 months. Whether this was driven by symptoms or purely enhanced follow-up by the surgeon is not known. It does suggest that patients requiring revision surgery may self-present if a suitable pathway to secondary care is in place. There was also a trend for greater use of revision implants in the UR group which, although readily available, are more costly than primary implants. While this did not reach significance and numbers were small, it highlights a need for further work.
Given the long timelines for revision post-primary surgery, a longitudinal study was not feasible. Consequently, data captured involved both long recall periods for the participant and data extraction from medical notes. Where possible, patient-reported data were corroborated with research nurse data and the latter were used in cases of discrepancy. However, for some data points, there were estimations (e.g. date of primary surgery > 20 years ago) and missing data (e.g. components used in primary surgery). We included both unicompartmental and total knee arthroplasties, but were unable to distinguish between these in our analysis. We accept that there may be recruitment biases, including ability to complete an English-language questionnaire. Patients presenting through primary care or acutely through the ED, such as for PFF, while on a long-term follow-up pathway, may have been incorrectly classified as ‘unplanned’. Due to the multicentre nature of the study, with both hip and knee patients recruited from 38 centres, and with primary surgery up to 25 years previously, the variation in implant type and fixation method was too large to enable meaningful grouping of components for cost analysis.
In conclusion, there appeared to be only minimal differences between patient characteristics for those undergoing planned or unplanned revision surgery. Although there was greater healthcare use in those having unplanned revision surgery, it appears unlikely that routine orthopaedic review would have detected many of these issues. Up to ten years, indications for revision surgery are symptomatic, suggesting that for most patients it may be safe to disinvest in routine follow-up provided there is a rapid access self-referral pathway to orthopaedic review. Future work should explore the most appropriate mechanisms for provision of access to specialist services.
References
1. No authors listed . 16th annual report 2019 National Joint Registry for England, Wales, Northern Ireland and the Isle of Man . National Joint Registry . 2019 . Google Scholar
2. No authors listed . 2017 commissioning guide: Pain arising from the hip in adults . British Orthopaedic Association . 2017 . https://www.boa.ac.uk/standards-guidance/commissioning-guides.html ( date last accessed 19 October 2021 ). Google Scholar
3. No authors listed . Statement regarding universal arthroplasty review programmes . Scottish Committee for Orthopaedics and Trauma . 2019 . http://www.scotorth.com/arthroplasty-review/ ( date last accessed 19 October 2021 ). Google Scholar
4. Smith LK . A survey of the current state of hip arthroplasty surveillance in the United Kingdom . Musculoskeletal Care . 2014 ; 12 ( 4 ): 232 – 238 . Crossref PubMed Google Scholar
5. Oussedik S , Zagra L , Shin GY , D’Apolito R , Haddad FS . Reinstating elective orthopaedic surgery in the age of covid-19 . Bone Joint J . 2020 ; 102-B ( 7 ): 807 – 810 . Crossref PubMed Google Scholar
6. Smith LK , Turner E , Lenguerrand E , Powell J , Palmer S . Pilot study: Is a long-term follow-up service beneficial for patients undergoing revision hip replacement surgery? Musculoskeletal Care . 2020 ; 19 ( 3 ): 259 – 268 . Crossref PubMed Google Scholar
7. Peduzzi P , Concato J , Kemper E , Holford TR , Feinstein AR . A simulation study of the number of events per variable in logistic regression analysis . J Clin Epidemiol . 1996 ; 49 ( 12 ): 1373 – 1379 . Crossref PubMed Google Scholar
8. Ramavath A , Lamb JN , Palan J , Pandit HG , Jain S . Postoperative periprosthetic femoral fracture around total hip replacements: Current concepts and clinical outcomes . EFORT Open Rev . 2020 ; 5 ( 9 ): 558 – 567 . Crossref PubMed Google Scholar
9. Zimmerli W . Clinical presentation and treatment of orthopaedic implant-associated infection . J Intern Med . 2014 ; 276 ( 2 ): 111 – 119 . Crossref PubMed Google Scholar
10. Lawton R , Silverwood R , Barnett K , Finlayson D . Is long-term follow-up after uncomplicated primary cemented total hip arthroplasty necessary . Orthop Proc . 2018 ; 94-B . https://online.boneandjoint.org.uk/doi/abs/10.1302/1358-992X.94BSUPP_XXXIX.BOA2011-176 Google Scholar
11. Cassidy RS , O hEireamhoin S , Beverland DE . Guidelines for the follow-up of total hip arthroplasty . Bone Joint J . 2019 ; 101-B ( 5 ): 536 – 539 . Crossref PubMed Google Scholar
12. Harris WH . Wear and periprosthetic osteolysis: The problem . Clin Orthop Relat Res . 2001 ; 393 : 66 – 70 . Crossref PubMed Google Scholar
Author contributions
S. R. Kingsbury: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
L. K. Smith: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
F. Shuweihdi: Formal analysis, Methodology, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
R. West: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Supervision, Validation, Visualization, Writing – review & editing.
C. Czoski Murray: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
P. G. Conaghan: Conceptualization, Funding acquisition, Methodology, Resources, Supervision, Validation, Visualization, Writing – review & editing.
M. H. Stone: Conceptualization, Funding acquisition, Investigation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding statement
This article presents independent research funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (14/70/146) and by the NIHR Leeds Biomedical Research Centre (BRC). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Acknowledgements
We would like to thank Lema Vernon for her support in coordinating this study, the orthopaedic surgeons and research nurses at our 38 recruitment sites who identified participants and extracted data from medical notes, and all the patients who took the time to complete the questionnaires following their revision surgery. This work formed part of a larger programme of work, the NIHR-funded UK SAFE programme.
Open access funding
The authors confirm that the open access fee was funded through NIHR HS&DR 14/70/146.
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
This article was primary edited by G. Scott.
Follow S. R. Kingsbury @srkingsbury
Supplementary material
Research Nurse and participant case report forms.









