Abstract
Aims
To analyze outcomes reported in studies of Ponseti correction of idiopathic clubfoot.
Methods
A systematic review of the literature was performed to identify a list of outcomes and outcome tools reported in the literature. A total of 865 studies were screened following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and 124 trials were included in the analysis. Data extraction was completed by two researchers for each trial. Each outcome tool was assigned to one of the five core areas defined by the Outcome Measures Recommended for use in Randomized Clinical Trials (OMERACT). Bias assessment was not deemed necessary for the purpose of this paper.
Results
In total, 20 isolated outcomes and 16 outcome tools were identified representing five OMERACT domains. Most outcome tools were appropriately designed for children of walking age but have not been embraced in the literature. The most commonly reported isolated outcomes are subjective and qualitative. The quantitative outcomes most commonly used are ankle range of motion (ROM), foot position in standing, and muscle function.
Conclusions
There is a diverse range of outcomes reported in studies of Ponseti correction of clubfoot. Until outcomes can be reported unequivocally and consistently, research in this area will be limited. Completing the process of establishing and validating COS is the much-needed next step.
Cite this article: Bone Joint Open 2020;1-8:457–464.
Introduction
The Ponseti method has revolutionized the care of children with clubfoot. Primary correction rate is generally high and fewer surgical procedures are required to correct the deformity.1-3 The Ponseti method is low cost, can be delivered successfully by various members of the healthcare team,4-10 and has been adopted worldwide with good results. Although primary correction can be achieved, there is less certainty around the long-term outcomes of treatment. Data on relapse rates, functional outcome, and quality of life is inconsistently defined11,12 The two most commonly used assessment methods of club foot are the Pirani13 and Diméglio14 scores. These are validated and repeatable assessments of the foot at initial presentation with good interobserver repeatability between orthopaedic surgeons, physiotherapists, and trained Ponseti practitioners.5-9 Other early classification systems15,16 aimed to provide an assessment of the foot during treatment or after initial correction. These classification systems make a descriptive, static assessment of the foot. They do not consider function, pain, patient or parent satisfaction, or psychological wellbeing of the child or caregiver. They are also not validated for use in older children but can possibly still be helpful in static assessment of the primary correction. There has been a noticeable effort in the literature to develop tools to assess outcomes of treatment of club foot across a broader range of domains.17-21 These systems combine aspects of physical examination, gait assessment and parental and child reported outcomes (PROMS).
Most recently, assessment tools have been developed and specifically designed for low-income healthcare settings22,23 showing good interobserver repeatability between physiotherapists and Ponseti practitioners.24 Other classification systems which integrate gait analysis and paedobarography, 25–29 or isokinetic muscle strength assessment,26,30 provide additional information but may not be feasible in most settings. The use of plain radiographs to assess bone/joint alignment, as an adjunct in the assessment of clubfoot correction,31,32 has shown poor correlation with function and relapse.33 There is a risk of creating a ‘flooded marketplace’ of clubfoot outcome measures, with no clear guidance or evidence on which tool is best utilized in each clinical environment at each stage of treatment.
Measuring and comparing clubfoot treatment success as well as indications for further intervention is currently hindered by the lack of agreed outcomes by the treating community. Core Outcome Sets (COS), defined as the minimum standardized collection of outcomes to be measured and reported in all research for a specific clinical area,34 have been developed for several musculoskeletal conditions35,36 but not for clubfoot management. In the absence of a COS we have used the COMET (Core Outcome Measures in Effectiveness Trials) initiative principles37 to identify the outcome tools reported following Ponseti correction of idiopathic clubfoot and analyze them according to domains and acceptance.
Methods
A systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.38 It was prospectively registered on the PROSPERO international prospective register of systematic reviews (CRD42018089517) and on the Core Outcome Measures in Effectiveness Trials (COMET) database.
The National Institute for Health and Care Excellence Databases Advanced Search interface was used to search EMBASE, Medline and CINAHL databases between 01 January 2012 and 01 May 2019. The search strategy terms are listed in the supplementary material. The original registration related to a project developing a core outcome set for the assessment of congenital talipes equionvarus (CTEV). An initial study was limited to assessing relapse as an outcome measure11 and the search dates were later extended for the purpose of this study which looks at other methods of assessment. Included were studies published in English, which addressed primary correction of idiopathic clubfoot using the Ponseti method. All study designs were considered.
Study titles, abstracts and full texts were screened independently by two authors (KH, AF). A senior author (YG) was consulted in the case of disagreement over the suitability of a text for inclusion. Disagreements were resolved by consensus. Data were extracted with use of the Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia) and a data collection table on Microsoft Excel, (Microsoft, Redmond, Washington, USA).
All clubfoot specific tools and classification systems were included, as well as isolated outcomes when no specific tool was used. For each clubfoot-specific assessment instrument, a separate literature search was performed to identify papers reporting the instrument’s interobserver repeatability. Repeatability was presented as reported by the relevant paper. Categorization of each verbatim outcome definition to an outcome name, and each outcome name to an outcome domain, has been performed independently by two researchers from different backgrounds (KH, AF). These two researchers worked on this process and two senior authors (YG, DME) were available to resolve differences and make final decisions.
Each outcome term was assigned to one of the five core areas defined by the Outcome Measures Recommended for use in Randomized Clinical Trials (OMERACT) Filter 2.0.39 The OMERACT framework describes five key domains; adverse events, life impact, resource use, pathophysiological manifestations, and death. The sixth domain of ‘technical considerations and feasibility of use in clinical practice’, suggested by Dorman et al36 for technical or surgical outcomes relevant to surgeons, was also included. Death was deemed nonapplicable for this analysis. As the purpose of this study was to collect all outcomes of treatment regardless of data quality, a bias assessment or appraisal of methodological quality of data has not been included.
Results
The initial literature search resulted in a total of 865 articles. The PRISMA flowchart for study selection is presented in Figure 1. A total of 124 studies fulfilled the inclusion criteria and were analyzed (Supplementary Material). The 124 included studies contributed 12,376 patients with 16,935 clubfeet. The demographic data is presented in Table I.
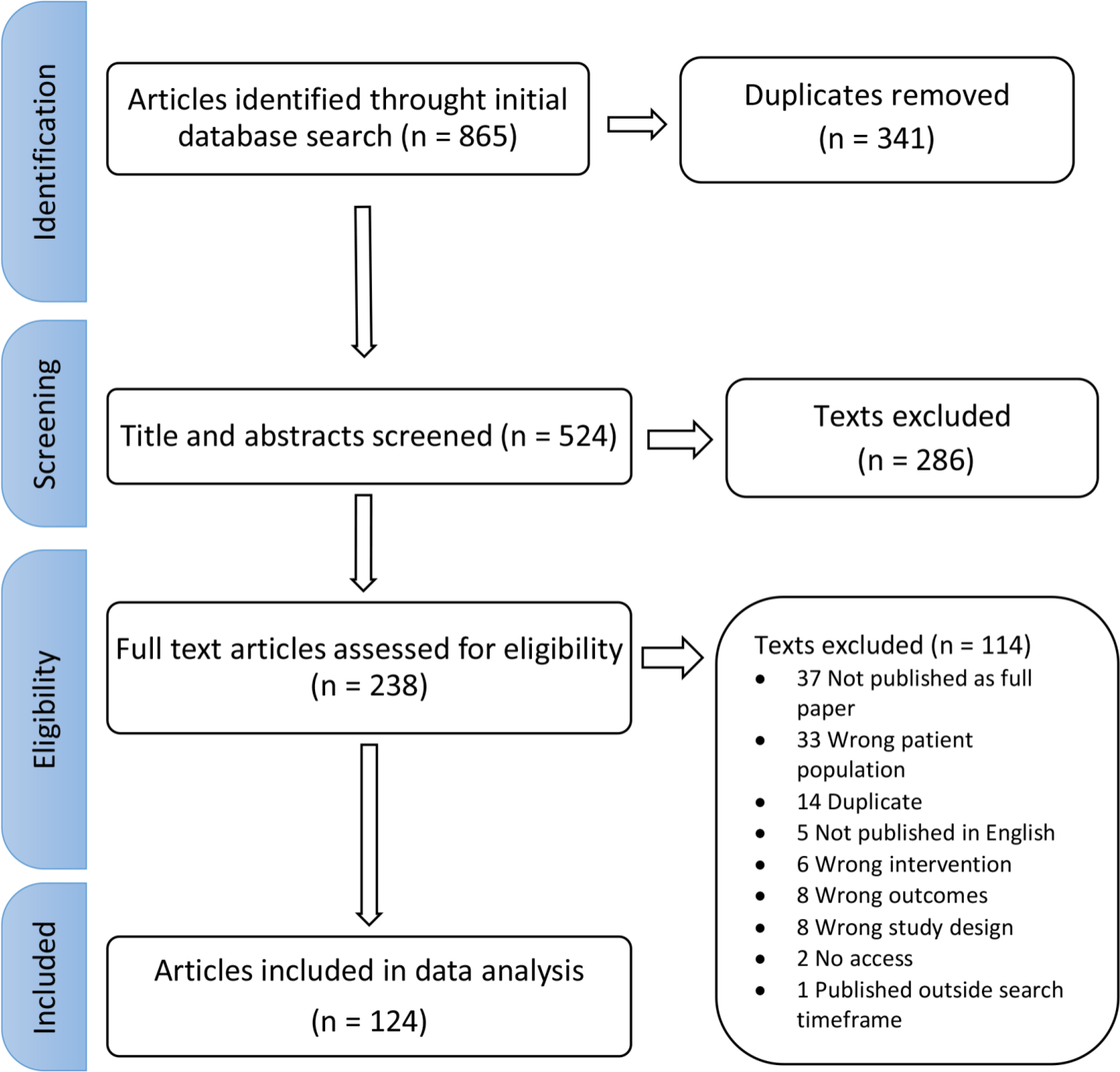
Fig. 1
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart for study selection.
Table I.
Demographic data for included studies and participants.
| Characteristic | Total |
|---|---|
| Studies, n | 124 (100) |
| Evidence level n (%) | |
| 1b | 7 (6) |
| 2b | 92 (75) |
| 3b | 3 (2) |
| 4 | 21 (17) |
| Continent of origin of publication n (%) | |
| Asia | 56 (46) |
| Europe | 31 (25) |
| North America | 23 (19) |
| Africa | 8 (7) |
| Australasia | 3 (2) |
| South America | 3 (2) |
| Patient demographics | |
| Female, n % | 32 (26) |
| Mean age at start of casting, wks (range) | 32.3 (0.3 to 384) |
| Ponseti treatment | |
| Mean Achilles tenotomies performed, % (range) | 75.8 (22.4 to 100) |
| Mean follow-up period, mths (range) | 47.4 (2.5 to 360) |
| Ponseti practitioner, n (%) | n = 61 |
| Orthopaedic surgeon | 50 (82) |
| Physiotherapist | 9 (15) |
| Plaster technician | 2 (3) |
These studies presented a wide variety of isolated outcomes and outcome scores. The list of the 20 verbatim outcomes generated along with the number of times they have been used is available in Table II.
Table II.
Clubfoot verbatim outcomes.
| Outcome measure, n | Studies reporting outcome (n = 124) |
|---|---|
| Heel (hindfoot) position | 23 |
| Forefoot position | 16 |
| Footwear | 6 |
| Foot size | 1 |
| Calf size | 1 |
| Foot position in standing | 5 |
| Foot position in walking | 4 |
| Ankle ROM, passive and active | 34 |
| Subtalar ROM, passive and active | 12 |
| Pre-chosen gait parameters (squatting, stair climbing, walking) | 10 |
| Qualitative muscle activity and function | 10 |
| Quantitative muscle strength | 3 |
| Pain | 7 |
| ‘Need’ for surgical intervention (surgeon’s perspective) | 44 |
| Recurrence (qualitative) | 67 |
| Recurrence (quantitative) | 3 |
| Angles from plain radiographs | 18 |
| Paedobarograph | 3 |
| Gait analysis | 8 |
| PROMs (parents) | 28 |
| PROMs (patients) | 11 |
| PROMs (both patients and parents) | 4 |
-
PROMs, parental and child reported outcomes; ROM, range of motion.
The outcome scores identified, of which there were 16, are presented in Table III. Each score was labelled as containing descriptive, functional, and/or prognostic elements. The stage at data collection and the repeatability of the score, if reported, were also documented. All scores presented a descriptive component, and the majority (13/16; 81%) offered an additional functional component with variable detail, but only three systems incorporated a prognostic component.
Table III.
Clubfoot-specific outcome tools presented in chronological order, with most recent first.
| Outcome instrument (year) | Parameters assessed | Descriptive/ Functional/ Prognostic | Stage at treatment to be used | Repeatability/predictive value | Studies, n* |
|---|---|---|---|---|---|
| PBS tool18 (2019) | Foot position in standing Prechosen gait parameters Ankle ROM Subtalar ROM |
D/F | Walking age | Interobserver agreement: 0.9319 | 1 |
| Assessing Clubfoot Treatment tool40 (2017) | Ankle ROM Pain Footwear Parental PROM |
D/F | Walking age | Detecting need for further intervention: Sensitivity: 79.2% Specificity: 100%23,25 |
2 |
| Evertor score41 (2014) | Ankle ROM and subjective muscle strength | D/F/P | After initial treatment | Predicting recurrence and need for further intervention PPV and NPV |
4 |
| Bangla clubfoot tool assessment23,42 (2014) | Parental PROM of foot appearance, footwear, pain, function Prechosen gait parameters Foot position in standing Ankle ROM |
D/F/P | Walking age | Predicting need for referral for further treatment: Interobserver agreement: 0.92 Sensitivity: 79.2% Specificity: 79.5% 24,25 |
4 |
| Bhaskar relapse assessment tool43 (2013) | Ankle and foot ROM Prechosen gait parameters Foot position |
D/F | Walking age | 3 | |
| IMAR Clubfoot Scale25 (2009) | Ankle ROM Foot position in standing Foot and calf appearance Gait (GAITRite system) Paedobarograph (dynamic and static) Parental PROM |
D/F | Walking age | Interobserver agreement: 0.79635 | 2 |
| Richards Classification44 (2008) | Ankle ROM Need for surgical correction |
D/F | After initial treatment | 3 | |
| Clubfoot Assessment Protocol21 (2005) | Ankle/foot ROM Muscle strength Foot position Prechosen gait parameters |
D/F | After initial treatment | Interobserver agreement range: 0.35 to 0.38 Interobserver agreement range: 0.54 to 1.0022 |
1 |
| International Clubfoot Study Group classification system31 (2003) | Foot position Ankle/foot ROM Muscle function Prechosen gait parameters Pain Angles from plain radiographs |
D/F | Walking age | Interobserver agreement: 0.7345 | 3 |
| Roye’s disease-specific instrument19 (2001) | Parental PROM of foot appearance, footwear, pain, function, gait | D/F/P | Walking age | Internal consistency reliability of 0.74 to 0.85 (Cronbach’s α)21 Predicting need for referral for further treatment: Sensitivity: 31.8% Specificity: 100%25 |
5 |
| Ezra clubfoot score46 (2000) | Ankle/subtalar ROM Hind/forefoot position in standing Tibialis Anterior function Prechosen gait parameters Footwear Functional limitations Pain Parental PROM |
D/F | Walking age | 3 | |
| Pirani Score13 (1999) | Hind/mid/forefoot position Ankle dorsiflexion |
D | Before, during and after initial correction | Interobserver agreement: 0.909 Pearson r : 0.8947 |
82 |
| Diméglio Score14 (1995) | Hind/forefoot position Ankle/subtalar ROM |
D/F | Before, during and after initial correction | Interobserver agreement: 0.839 Pearson r : 0.8548 |
36 |
| Catterall Classification16 (1991) | Hind/forefoot position | D | During treatment | Interobserver agreement range: 0.15 to 0.448 | 4 |
| Harrold and Walker Classification15 (1983) | Ankle ROM Hindfoot position | D | Pretreatment | Interobserver agreement range: 0.4 to 0.748 | 2 |
| Laaveg and Ponseti functional rating system17 (1980) | Parental PROM Pain Foot position in standing Ankle/foot ROM Prechosen gait parameters |
D/F | Walking age | 5 |
-
*
Absolute number out of 124 papers
-
PBS, Pirani/Böhm/Sinclair; PROM, parental and child reported outcomes; ROM, range of motion
Seven assessment tools were relevant to the peritreatment period and nine were designed for walking age children, and therefore required an appropriate follow-up time period. The individual outcomes distributed as per OMERACT Framework are presented in Table IV. The identified outcome instruments are mapped in Table V according to the OMERACT domains, defining which outcome score falls under each domain.
Table IV.
Outcomes as per Outcome Measures Recommended for use in Randomized Clinical Trials framework.
| Core area | Core domains | Outcomes |
|---|---|---|
| Adverse event | Adverse events | Relapse, residual deformity |
| Life impact | Quality of life | Quality of life, squatting, stair climbing, pain, participation in sports activities, functional score, footwear, foot appearance |
| Resource use | Economic/hospital/ need for intervention | Further surgery, further casting, appropriate for low income setting |
| Pathophysiological manifestations | Musculoskeletal | Muscle strength, ankle and subtalar range of movement, gait analysis, paedobarograph |
| Death | N/A | N/A |
| Technical considerations | Technical considerations | Radiological measurements, Feasibility of use in clinical setting |
-
N/A, not applicable.
Table V.
Mapping of outcome instruments into Outcome Measures Recommended for use in Randomized Clinical Trials domains
| Outcome instrument (year) | Domains | ||||
|---|---|---|---|---|---|
| Adverse event | Life impact | Resource use | Pathophysiological manifestations | Technical considerations | |
| PBS tool18 (2019) | X | X | |||
| Assessing Clubfoot Treatment tool40 (2017) | X | X | X | X | |
| Evertor score41 (2014) | X | X | X | ||
| Bangla Clubfoot Tool23,42 (2014) | X | X | X | X | |
| Bhaskar relapse assessment tool43 (2013) | X | X | X | ||
| IMAR-Clubfoot scale25 (2009) | X | X | |||
| Richards classification44 (2008) | X | X | |||
| Clubfoot Assessment Protocol21 (2005) | X | X | |||
| International Clubfoot Study Group31 (2003) | X | X | X | ||
| Roye’s disease-specific instrument19 (2001) | X | ||||
| Ezra clubfoot score46 (2000) | X | X | X | ||
| Pirani score13 (1999) | X | X | X | ||
| Diméglio score14 (1995) | X | X | X | ||
| Catterall classification16 (1991) | X | X | |||
| Harrold and Walker classification15 (1983) | X | X | |||
| Laaveg and Ponseti functional rating system17 (1980) | X | X | X | ||
-
PBS, Pirani/Böhm/Sinclair.
The core areas reported were principally distributed between three domains (pathophysiological manifestations, life impact, and resource use) with the most common quantitative outcome being ankle ROM (27%; 34/124). None of the studies reported death. The two outcome measures most commonly used are recurrence rates in 54% (67/124) (with or without a qualitative definition) and need for surgical intervention in 35% (43/124), again without any definition of which aspect of the deformity required treatment. The most reported outcome tools were Pirani (66%; 82/124) and Diméglio (29% 36/124). None of the outcome systems designed for after walking age were used frequently (between one and five times each). The outcomes systems designed for walking age included more functional components than the mostly descriptive tools designed for correction age (Table III). PROMs were used in 31% (39/124) of the studies, mostly parent reported (Table II). Outcomes from the life impact core area, such as foot appearance, foot and calf size and function, were not frequently used by the treating clinician, but are emphasized in PROMs.
Discussion
The Ponseti method has become the standard of care for idiopathic clubfoot correction. The number of reported studies has increased steeply in the last two decades and all show consistent success in initial correction. However the long-term outcomes are not clearly defined, therefore limiting high-quality systematic reviews and treatment decisions. This systematic review reports all individual outcomes and assessment tools used in patients who have undergone the Ponseti method and allocates outcomes to the six core areas as per the OMERACT framework.
The majority of assessment tools were appropriately designed and tested in ambulatory children. The assessment tools require a broad range of clinical expertise, time, parental input, and equipment. Some tools use PROMs alone, such as Roye’s disease-specific instrument.19 PROMs combine clubfoot-related symptoms such as pain and shoe wear and other more holistic assessments such as involvement with play, missing time at school and emotional impact. Other outcome tools use clinical examination findings alone.15,18,21 Different tools dictate different degrees of detail for clinical examination – ranging from binary ‘yes’ or ‘no’ outcomes (for example, for a plantigrade foot) to quantitative measures of range of movement.
Several tools use a combination of PROMs and examination findings.17,23,31 Gait was assessed in a variety of ways, from simple parental-reported functional measures (such as ability to squat or run23), qualitative gait pattern observed in clinic,19 or a comprehensive assessment in the gait laboratory.25 While outcomes at a given end point are important, to the treating clinician it may be important to recognize the ‘failing’ foot and thus scores that contain a prognostic element may have more relevance.19,23,41
Most tools were developed in high-income countries with some notable exceptions.22,23 It should be acknowledged that different parameters will be important to the parents and the child at different ages and different outcomes will have different significance in different parts of the world.
After excluding assessment tools that were not condition specific, we have identified 20 outcomes and 16 assessment tools and defined their acceptability and, where assessed, reported their repeatability (as stated in the initial paper). While the infant applicable classification systems of Pirani13 and Diméglio14 are widely accepted, none of the true outcome tools have been similarly accepted by the treating community. There were seven outcome systems found to be applicable to walking age children. They all include ankle ROM and foot position in standing. Three include muscle function assessment and five included various PROMS with different degrees of detail adaptable to the local setting.
The most commonly reported outcome measures are quantitative and surgeon subjective. As previously reported11 recurrence rate was reported in more than half of the papers with a broad interpretation of the term. The broad term “need for surgical intervention” has been reported as an outcome in 35% of the papers. Both of these outcome measures cannot serve as a part of the COS and their use in publications is not helpful for either clinical decision-making or research.
This study does have limitations. The systematic review is limited to the English language and therefore might be missing valuable information. The focus of this study was to collect as many outcomes measures as possible and therefore no studies were excluded by their level of evidence. There was also no threshold for minimum follow-up and thus a variable follow-up distribution within the included studies.
Clubfoot in the walking age child must be assessed more comprehensively and more appropriately than using the popular infant applicable Pirani13 and Diméglio14 scores. These are validated and repeatable assessments of the foot at initial presentation with good interobserver repeatability between orthopaedic surgeons, physiotherapists, and trained Ponseti practitioners.5-9 There is an obvious trade-off between a comprehensive, time-consuming tool that requires expertise and training and a short, basic tool that can be used by all in every setting. The absence of clear outcomes has resulted in a wide diversity of treatments being recommended at various stages in the management of clubfoot and for various indications.
The ‘ideal’ CTEV assessment tool would be easy to use, comprehensive, adaptable to local resources, and tailored to geographical area. It would provide a multifaceted assessment including a static and dynamic clinical examination and basic PROMs, adaptable to different stages of treatment, and validated and repeatable by all Ponseti practitioners. A COS will provide a basic uniform building block from the overall diverse outcome system.
We recommend that the global clubfoot community embrace one classification system for the assessment of clinical outcome. Currently, this validated tool is not available and collaborative efforts would be recommended in order to establish one. Currently, there are a large variety of outcome measures reported following clubfoot correction with no established COS. Until outcomes can be reported unequivocally and consistently, research in this area will be limited. Completing the process of establishing and validating COS is the much-needed next step.
References
1. Hughes K , Gelfer Y , Cokljat M , et al. Does idiopathic congenital talipes equinovarus have an impact on attainment of developmental milestones? A multicentre international study . J Child Orthop . 2019 ; 13 ( 4 ): 353 – 360 . Crossref PubMed Google Scholar
2. Morcuende JA , Dolan LA , Dietz FR , Ponseti IV . Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method . Pediatrics . 2004 ; 113 ( 2 ): 376 – 380 Crossref PubMed Google Scholar
3. Jaqueto PA , Martins GS , Mennucci FS , Bittar CK , Zabeu JLA . Functional and clinical results achieved in congenital clubfoot patients treated by Ponseti’s technique . Rev Bras Ortop . 2016 ; 51 ( 6 ): 657 – 661 . Google Scholar
4. Dunkley M , Gelfer Y , Jackson D , et al. Mid-Term results of a physiotherapist-led Ponseti service for the management of non-idiopathic and idiopathic clubfoot . J Child Orthop . 2015 ; 9 ( 3 ): 183 – 189 . Crossref PubMed Google Scholar
5. Shaheen S , Jaiballa H , Pirani S . Interobserver reliability in Pirani clubfoot severity scoring between a paediatric orthopaedic surgeon and a physiotherapy assistant . J Pediatr Orthop B . 2012 ; 21 ( 4 ): 366 – 368 . Crossref PubMed Google Scholar
6. Pirani S , Hodges D . Sekeramayi F. A reliable & valid method of assessing the amount of deformity in the congenital clubfoot deformityitle . Orthop Proc . 2008 ; 90 ( SUPP_I ): 53 . Google Scholar
7. Sharma P , Verma R , Gaur S . Interobserver reliability of pirani clubfoot severity scoring between an orthopedic surgeon, a resident doctor, and a nonmedical counsellor at a clubfoot clinic . Indian J Orthop . 2018 ; 52 ( 6 ): 645 . Crossref PubMed Google Scholar
8. Jain S , Ajmera A , Solanki M , Verma A . Interobserver variability in Pirani clubfoot severity scoring system between the orthopedic surgeons . Indian J Orthop . 2017 ; 51 ( 1 ): 81 – 85 . Crossref PubMed Google Scholar
9. Flynn JM , Donohoe M , Mackenzie WG . An independent assessment of two clubfoot-classification systems . J Pediatr Orthop . 1998 ; 18 ( 3 ): 323 – 327 . PubMed Google Scholar
10. Shack N , Eastwood DM . Early results of a physiotherapist-delivered Ponseti service for the management of idiopathic congenital talipes equinovarus foot deformity . J Bone Joint Surg Br . 2006 ; 88-B ( 8 ): 1085 – 1089 . Crossref PubMed Google Scholar
11. Gelfer Y , Wientroub S , Hughes K , Fontalis A , Eastwood DM . Congenital talipes equinovarus: a systematic review of relapse as a primary outcome of the Ponseti method . Bone Joint J . 2019 ; 101-B ( 6 ): 639 – 645 . Crossref PubMed Google Scholar
12. Hussain FN . The role of the Pirani scoring system in the management of club foot by the Ponseti method . J Bone Joint Surg Br . 2007 ; 89-B ( 4 ): 561 – 561 . Crossref PubMed Google Scholar
13. Pirani S , Outerbridge HK , Sawatzky B , Stothers K . A reliable method of clinically evaluating a virgin clubfoot evaluation . 21st SICOT Congress . 29 , 1999 : 2 – 30 . Google Scholar
14. Diméglio A , Bensahel H , Souchet P , Mazeau P , Bonnet F . Classification of clubfoot . J Pediatr Orthop B . 1995 ; 4 ( 2 ): 129 – 136 . Crossref PubMed Google Scholar
15. Harrold AJ , Walker CJ . Treatment and prognosis in congenital club foot . J Bone Joint Surg Br . 1983 ; 65-B ( 1 ): 8 – 11 . Crossref PubMed Google Scholar
16. Catterall A . A method of assessment of the clubfoot deformity . Clin Orthop Relat Res . 1991 ; 264 : 48 – 53 . PubMed Google Scholar
17. Laaveg SJ , Ponseti IV . Long-Term results of treatment of congenital club foot . J Bone Joint Surg Am . 1980 ; 62 ( 1 ): 23 – 31 PubMed Google Scholar
18. Böhm S , Sinclair MF . The PBS Score - a clinical assessment tool for the ambulatory and recurrent clubfoot . J Child Orthop . 2019 ; 13 ( 3 ): 282 – 292 . Crossref PubMed Google Scholar
19. Roye BD , Vitale MG , Gelijns AC , Roye DP . Patient-Based outcomes after clubfoot surgery . J Pediatr Orthop . 2001 ; 21 ( 1 ): 42 – 49 . Crossref PubMed Google Scholar
20. Dietz FR , Tyler MC , Leary KS , Damiano PC . Evaluation of a disease-specific instrument for idiopathic clubfoot outcome . Clin Orthop Relat Res . 2009 ; 467 ( 5 ): 1256 – 1262 . Crossref PubMed Google Scholar
21. Andriesse H , Hägglund G , Jarnlo G-B . The clubfoot assessment protocol (CAP); description and reliability of a structured multi-level instrument for follow-up . BMC Musculoskelet Disord . 2005 ; 6 : 40 . Crossref PubMed Google Scholar
22. Smythe T , Mudariki D , Gova M , Foster A , Lavy C . Evaluation of a simple tool to assess the results of Ponseti treatment for use by clubfoot therapists: a diagnostic accuracy study . J Foot Ankle Res . 2019 ; 12 ( 1 ): 14 . Crossref PubMed Google Scholar
23. Evans AM , Perveen R , Ford-Powell VA , Barker S . The Bangla clubfoot tool: a repeatability study . J Foot Ankle Res . 2014 ; 7 ( 1 ): 27 . Crossref PubMed Google Scholar
24. Smythe T , Gova M , Muzarurwi R , Foster A , Lavy C . A comparison of outcome measures used to report clubfoot treatment with the Ponseti method: results from a cohort in Harare, Zimbabwe . BMC Musculoskelet Disord . 2018 ; 19 ( 1 ): 450 . Crossref PubMed Google Scholar
25. Ramanathan AK , Herd F , Macnicol M , Abboud RJ . A new scoring system for the evaluation of clubfoot: the IMAR-Clubfoot scale . Foot . 2009 ; 19 ( 3 ): 156 – 160 . Crossref PubMed Google Scholar
26. Jeans KA , Karol LA , Erdman AL , Stevens WR . Functional outcomes following treatment for clubfoot: ten-year follow-up . J Bone Joint Surg Am . 2018 ; 100 ( 23 ): 2015 – 2023 . Crossref PubMed Google Scholar
27. Švehlík M , Floh U , Steinwender G , et al. Ponseti method is superior to surgical treatment in clubfoot - Long-term, randomized, prospective trial . Gait Posture . 2017 ; 58 : 346 – 351 . Crossref PubMed Google Scholar
28. Manousaki E , Czuba T , Hägglund G , Mattsson L , Andriesse H . Evaluation of gait, relapse and compliance in clubfoot treatment with custom-made orthoses . Gait Posture . 2016 ; 50 ( PG-8-13 ): 8 – 13 . Crossref PubMed Google Scholar
29. Banskota B , Banskota AK , Regmi R , et al. The Ponseti method in the treatment of children with idiopathic clubfoot presenting between five and ten years of age . Bone Joint J . 2013 ; 95-B ( 12 ): 1721 – 1725 . Crossref PubMed Google Scholar
30. Gray K , Burns J , Little D , Bellemore M , Gibbons P . Is tibialis anterior tendon transfer effective for recurrent clubfoot? Clin Orthop Relat Res . 2014 ; 472 ( 2 ): 750 – 758 . Crossref PubMed Google Scholar
31. Bensahela H , Kuo K , Duhaime M , International Clubfoot Study Group . Outcome evaluation of the treatment of clubfoot: the International language of clubfoot . J Pediatr Orthop B . 2003 ; 12 ( 4 ): 269 – 271 . Crossref PubMed Google Scholar
32. Sætersdal C , Fevang JM , Bjørlykke JA , Engesæter LB . Ponseti method compared to previous treatment of clubfoot in Norway. A multicenter study of 205 children followed for 8-11 years . J Child Orthop . 2016 ; 10 ( 5 PG-445–452 ): 445 – 452 . Google Scholar
33. Richards BS , Faulks S , Razi O , Moualeu A , Jo C-H . Nonoperatively corrected clubfoot at age 2 years . J Bone Joint Surg . 2017 ; 99 ( 2 ): 155 – 160 . Crossref PubMed Google Scholar
34. Williamson PR , Altman DG , Blazeby JM , et al. Developing core outcome sets for clinical trials: issues to consider . Trials . 2012 ; 13 ( 1 ): 132 . Crossref PubMed Google Scholar
35. Leo DG , Leong WY , Gambling T , et al. The outcomes of Perthes’ disease of the hip: a study protocol for the development of a core outcome set . Trials . 2018 ; 19 ( 1 ): 374 . Google Scholar
36. Dorman SL , Shelton JA , Stevenson RA , et al. Management of medial humeral epicondyle fractures in children: a structured review protocol for a systematic review of the literature and identification of a core outcome set using a Delphi survey . Trials . 2018 ; 19 ( 1 ): 119 . Crossref PubMed Google Scholar
37. Williamson PR , Altman DG , Bagley H , et al. The comet Handbook: version 1.0 . Trials . 2017 ; 18 ( Suppl 3 ): 280 . Crossref PubMed Google Scholar
38. Liberati A , Altman DG , Tetzlaff J , et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration . BMJ . 2009 ; 339 : b2700 . Crossref PubMed Google Scholar
39. Boers M , Kirwan JR , Wells G , et al. Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0 . J Clin Epidemiol . 2014 ; 67 ( 7 ): 745 – 753 . Crossref PubMed Google Scholar
40. Smythe T , Wainwright A , Foster A , Lavy C . What is a good result after clubfoot treatment? A Delphi-based consensus on success by regional clubfoot trainers from across Africa . PLoS One . 2017 ; 12 ( 12 ): e0190056 . Crossref PubMed Google Scholar
41. Gelfer Y , Dunkley M , Jackson D , et al. Evertor muscle activity as a predictor of the mid-term outcome following treatment of the idiopathic and non-idiopathic clubfoot . Bone Joint J . 2014 ; 96-B ( 9 ): 1264 – 1268 . Crossref PubMed Google Scholar
42. Evans A , Perveen R , Barker S , et al. The Bangladesh clubfoot project: audit of two-year outcomes of Ponseti treatment in 400 children . Physiotherapy . 2015 ; 101 : e366 . Google Scholar
43. Bhaskar A , Patni P . Classification of relapse pattern in clubfoot treated with Ponseti technique . Indian J Orthop . 2013 ; 47 ( 4 ): 370 . Crossref PubMed Google Scholar
44. Richards BS , Faulks S , Rathjen KE , et al. A comparison of two nonoperative methods of idiopathic clubfoot correction: the Ponseti method and the French functional (physiotherapy) method . J Bone Joint Surg Am . 2008 ; 90 ( 11 ): 2313 – 2321 . Crossref PubMed Google Scholar
45. Celebi L , Muratli HH , Aksahin E , et al. Bensahel et al. and international clubfoot Study Group evaluation of treated clubfoot: assessment of interobserver and intraobserver reliability . J Pediatr Orthop B . 2006 ; 15 ( 1 ): 34 – 36 . Crossref PubMed Google Scholar
46. Ezra E , Hayek S , Gilai AN , Khermosh O , Wientroub S . Tibialis anterior tendon transfer for residual dynamic supination deformity in treated club feet . J Pediatr Orthop B . 2000 ; 9 ( 3 ): 207 – 211 . Crossref PubMed Google Scholar
47. Cosma D , Vasilescu DE . A clinical evaluation of the Pirani and Dimeglio idiopathic clubfoot classifications . J Foot Ankle Surg . 2015 ; 54 ( 4 ): 582 – 585 . Crossref PubMed Google Scholar
48. Wainwright AM , Auld T , Benson MK , Theologis TN . The classification of congenital talipes equinovarus . J Bone Joint Surg Br . 2002 ; 84 ( 7 ): 1020 – 1024 . PubMed Google Scholar
Author contributions
Y. Gelfer Conceptualized and designed the study, Contributed to data analysis, Wrote, reviewed, and approved the manuscript.
K. Hughes: Contributed to the study design, Contributed to data analysis, Wrote and approved the manuscript.
A. Fontalis: Contributed to the methodology of the study, Collected and analyzed the data, Critically reviewed and approved the manuscript.
S. Weintroub: Conceptualized and supervised the study, Critically reviewed and approved the manuscript.
D. M. Eastwood: Conceptualized the study, Wrote, edited, and approved the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.The authors have no disclosures of funding received from the National Institute of Health (NIH), welcome trust, Howard Hughes Medical Institute (HHMI), and others.
Ethical review statement
This study was prospectively registered on the PROSPERO international prospective register of systematic reviews (CRD42018089517) and on the Core Outcome Measures in Effectiveness Trials (COMET) database.
Follow Y. Gelfer @yaelgelfer
Follow K. P. Hughes @katiehughes
Follow A. Fontalis @AFontalis
Follow D. M. Eastwood @deboraheastwood
Supplementary material
Search terms used.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









