Abstract
Background
Due to the overwhelming demand for trauma services, resulting from increasing emergency department attendances over the past decade, virtual fracture clinics (VFCs) have become the fashion to keep up with the demand and help comply with the BOA Standards for Trauma and Orthopaedics (BOAST) guidelines. In this article, we perform a systematic review asking, “How useful are VFCs?”, and what injuries and conditions can be treated safely and effectively, to help decrease patient face to face consultations. Our primary outcomes were patient satisfaction, clinical efficiency and cost analysis, and clinical outcomes.
Methods
We performed a systematic literature search of all papers pertaining to VFCs, using the search engines PubMed, MEDLINE, and the Cochrane Database, according to the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) checklist. Searches were carried out and screened by two authors, with final study eligibility confirmed by the senior author.
Results
In total, 21 records were relevant to our research question. Six orthopaedic injuries were identified as suitable for VFC review, with a further four discussed in detail. A reduction of face to face appointments of up to 50% was reported with greater compliance to BOAST guidelines (46.4%) and cost saving (up to £212,000).
Conclusions
This systematic review demonstrates that the VFC model can help deliver a safe, more cost-effective, and more efficient arm of the trauma service to patients.
Cite this article: Bone Joint Open 2020;1-11:683–690.
Introduction
The British Orthopaedic Association (BOA) published guidance in August 2013, as part of the Standards for Trauma for Fracture Clinic services (BOAST 7 guidelines), which states: “Following acute traumatic orthopaedic injury, patients should be seen in a new fracture clinic within 72 hours of presentation with the injury”.1 Due to the overwhelming demand for trauma services, from increasing emergency department (ED) attendances over the past decade, a rising number of fracture clinics in the UK are being over-stretched where demand is exceeding capacity.2 Trauma triage clinics or virtual fracture clinics (VFCs) have become increasingly widespread to keep up with the demand and help comply with the BOAST guidance. This has been used as an alternative to the traditional face-to-face fracture clinics.
In this article, we aim to assess “How useful are VFCs?” through a systematic review of the literature, with identification of injuries which may be safely and effectively managed through the VFC model. Specifically, our primary outcome measures were: patient satisfaction; clinical efficiency and cost analysis; and clinical outcomes including any need for further intervention or any adverse complications for any injuries assessed through a VFC. Finally, we discuss the evidence base for the safe treatment of commonly seen injuries in a VFC. To the authors’ knowledge, there has not been a systematic review assessing both the overall efficacy of VFCs and individual injuries routinely seen.
Virtual fracture clinic model
The VFC model was first introduced by the Glasgow Royal Infirmary (GRI) in 2011.3 Since its inception, over 40 different units have fully implemented the principles of the VFC model, with many more having introduced leaflets and planning a redesign.4
The general process and principles, as outlined by GRI, remain the same. However specific local nuances have varied from hospital to hospital. The following describes the overall process, both by GRI, and in the authors’ own institutions. The VFC is led by a consultant orthopaedic surgeon, who is the lead decision-maker, assisted by a nurse and administrative staff. All the referrals are collated together to form a virtual clinic list. The radiographs and other imaging should be preloaded on to the picture archiving and communication system (PACS). Clinical notes, including referral letters and ED notes, should be readily available with the patient notes. The cases are then reviewed and assigned one of three outcomes: virtual discharge with advice; review in general fracture clinic; or review in speciality fracture clinic. After the VFC, the patients are either telephoned or written to, with a copy of the letter sent to the GP.3,4 Many centres also supply their own patient advice leaflets and websites to give patients access to their individual rehabilitation plans and allow other health care professionals to review the resources.
Method
We performed a systematic literature search of all papers pertaining to VFCs, using the search engines PubMed, MEDLINE, and the Cochrane Database, according to the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) checklist. The search terms were, “virtual fracture clinic OR virtual fracture clinics”, as individual injuries yielded more than 100,000 results. The review focused on articles from 2014 onwards, reflecting the introduction of the VFC. Our exclusion criteria involved: articles not published in English; duplicate articles; and opinion letters. A detailed search strategy is outlined in Figure 1.
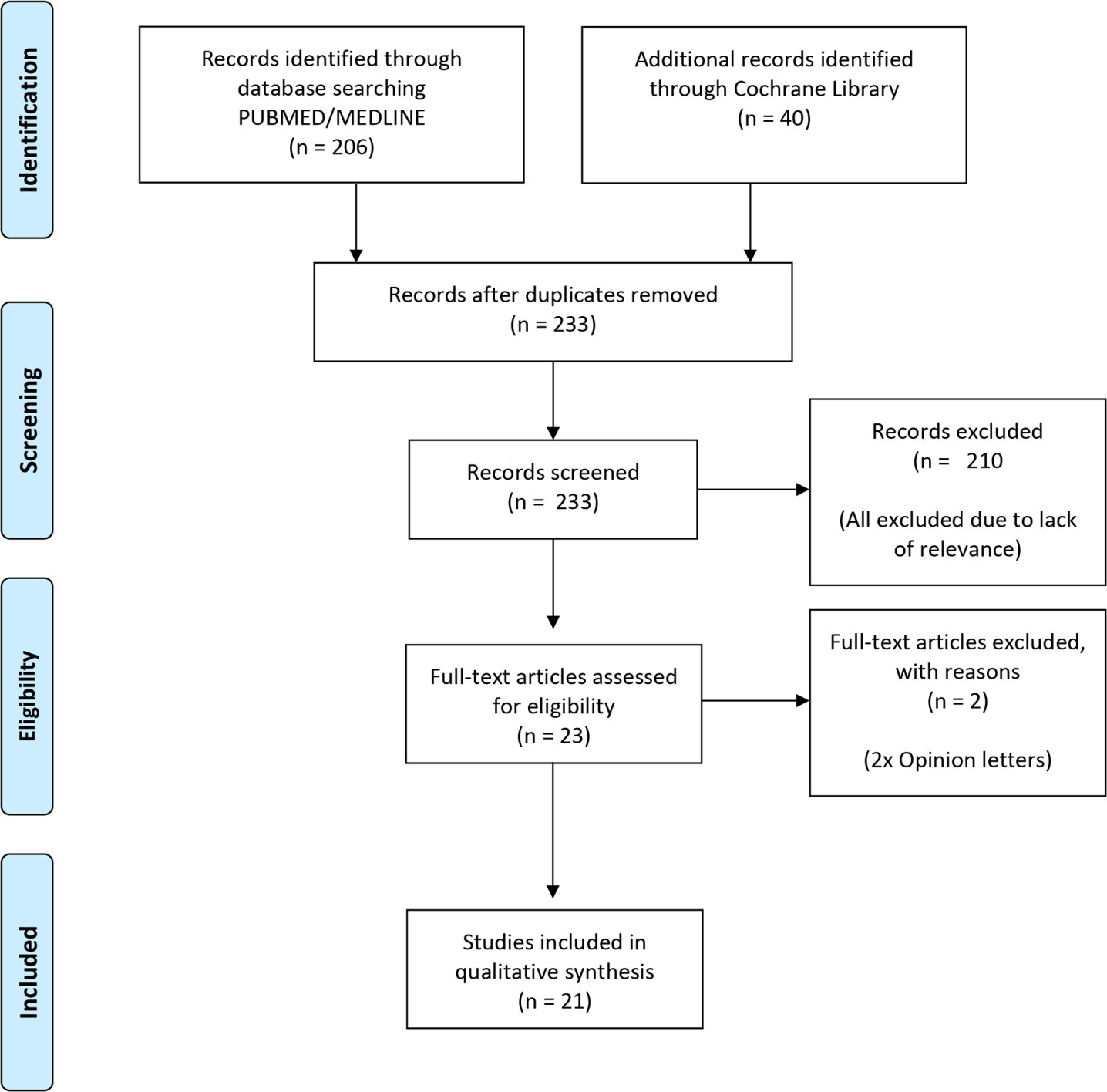
Fig. 1
A flow diagram depicting the phases and decision making process for a systematic review looking at virtual fracture clinic(s).
Two reviewers independently conducted the same literature search (SK, CH) and the results of each search were compared. Two other reviewers evaluated the articles’ eligibility by screening the title, the abstract, followed by the full text analysis. Consensus on the eligibility of the articles was sought and approved by the senior reviewer.
Our primary measures were: patient reported satisfaction; cost analyses and clinical efficiency; and clinical outcomes, including need for further intervention and complications from being seen in VFC. In addition to the above, we noted common conditions seen in VFCs and performed a review of the literature to provide an evidence base for recommendations on their management in a VFC setting.
Results
In total, 233 records were identified, of which 13 were duplicates. Screening of abstract and title resulted in the exclusion of 210 records due to a lack of relevance to our research question. Further screening of full text articles excluded two more articles, as they were purely opinion letters responding to an article. This gave a total of 21 records which were of relevance to our research question. Out of the final 21 included records, there were no level 1 evidence or randomized controlled trials. There was insufficient quantitative data, alongside the large diversity in study outcome measures, meaning it was not feasible to perform a meta-analysis.
The majority of data available is the result of audit and quality improvement projects or simple retrospective, historical, institutional data. End outcome measures are varied and cover a range of areas including cost, patient satisfaction, patient outcome, and clinic usage. Almost every paper (18) included level 1 or 2 evidence related to the injury for which they were discussing the use of VFC.
Patient satisfaction
Four studies reported on patient satisfaction,5-8 with overall satisfaction of between 91% to 97%. They also report satisfaction with the information provided to be between 86% to 95%.
Costs and clinical efficiency
Vardy et al4 report an overall positive outcomes in their assessment of VFCs on the ED. They report a decrease in patient reattendance from missed fracture clinic appointments, and no increase in unplanned reattendance. Time to treatment and discharge from ED remained the same.
The percentage of patients reviewed within 72 hours in clinic (VFC), as per BOAST 7 guidelines ranged from 46% to 100%.9,10 Jenkins et al11 and McKirdy et al9 both report a reduction in the overall number of referrals from ED to traditional fracture clinics by 15% to 28% with implementation of a VFC. Anderson et al12 concur and show an overall 65% reduction in face to face consultations.12 The discharge rate from VFC is reported between 33% to 60%.5,9
Cost analysis are predominantly reported by the team in Glasgow. Jenkins et al predict national adaption of a VFC pathway may have resulted in a £3,535,808 saving between 2009 to 2014.11 Annual savings are reported between £67,385 to £212,705.9,11,13 On an individual patient basis, O’Reilly et al5 report a decrease of €129 to €28, and Anderson et al12 report a decrease of £36 to £22. Anderson et al also describe significantly reduced resources required per clinic across the multidisciplinary team, adding to cost savings. One study reported a 75% reduction in ‘Did Not Attend’ at six months after VFC implementation, which normally would waste resources, thus adding to cost savings.9
Clinical outcomes
Encouragingly, there are no reports within the literature of significantly adverse outcomes following VFC consultation. The GRI report no current medico-legal cases, following 30,000 VFC patient visits.12 Only one study reports two patients needing to return to their GP or ED for further advice or analgesia.6
Discussion
One of the reoccurring advantages in the literature was a reduced requirement for face to face in person consultations.5,7-9,12,14-20 In some units this has been reported as a reduction of almost 50% in outpatient appointments and improved waiting times from referral to first orthopaedic review in clinic.7–9 As a result, many authors reported a significant cost saving, through appointments, staffing and even materials.14–20 There was variability in the reporting of the total saving but there is no report of increased cost.5,9,11,12,14,16,19-23
There is evidence of improved adherence to the BOAST guidelines, in particular BOAST 7 in seeing patients within a timely manner,10 and BOAST 3 (5.1% pre intervention, 46.4% post intervention; p < 0.001) when associated with the implementation of a VFC.24 Satisfaction was still high among the patient cohort, with no reported measurable reduction in safety/outcome compared with traditional fracture clinic management.5–8,12,19,20,25
Two underlying themes appear to be common in units implementing a VFC model. Firstly there needs to be clear documented patient pathways specific to injury types. Secondly it is crucial that there is buy in from all key stakeholders of the multidisciplinary team who may be involved. Most notably the ED must be engaged as they will place patients in the appropriate pathway. In addition it has been shown protocolisation and VFC can improve ED performance.3,26 The physiotherapy team must also be involved from the start of the planning process as some patients may enter a physio-led stream with the option of referral back to the trauma and orthopaedic team. The evidence available suggests this interdepartment relationship and teamworking is critical to success.3,5,7-9,12,14-20
Furthermore, there is a wealth of information systems, internet based patient information, care packs, and communication that have been developed by individual centres.27–33 This has been crucial to help build the patient interface part of the service. Certainly in our institutions, providing patients with the right information in the best readable format has been a key facet to help reduce the amount of face to face appointments so that patients feel adequately informed, without the need to return.
Our systematic review shows there are many stable fractures that can be managed non-peratively, without the need for fracture clinic review. The GRI include a list of six orthopaedic injuries which could be discharged directly from the ED without follow-up.3 Here, we discuss the six common injuries identified by GRI. In addition, we review other common injuries that the authors routinely see in fracture clinic, which can be safely reviewed in VFCs. Recommendations on their management in the VFC are made on the background of available level 1 and 2 evidence from the literature, including that of our systematic review. A summary of our recommendations on the discussed conditions and their optimum management plan is found in Table I.
Table I.
Summary of injuries which can be reviewed in a VFC model, with best evidence outcome.
| Diagnosis | Initial management | VFC outcome |
|---|---|---|
| Shoulder | ||
| Undisplaced clavicle fractures | Broad arm sling | Virtual discharge |
| Elbow | ||
| Mason 1 radial head fracture | Broad arm sling | Virtual discharge |
| Mason 2 radial head fracture | Broad arm sling | Virtual fracture clinic review |
| Elbow ‘fat pad’ sign | Broad arm sling | Virtual discharge |
| Hand | ||
| Fifth metacarpal neck fracture | Neighbour strapping | Virtual discharge |
| Metacarpal shaft fracture | Neighbour strapping±splint | Fracture clinic review |
| Soft tissue mallet finger | Mallett splint | Virtual fracture clinic review |
| Bony mallet injury | Mallett Splint | Virtual fracture clinic review |
| Ankle | ||
| Ankle sprain | Walking orthosis | Virtual discharge |
| Weber A fracture | Walking orthosis | Virtual discharge |
| Weber B fracture (no talar shift) | Walking orthosis | Virtual fracture clinic review |
| Achilles tendon rupture | Walking orthosis with wedges | Virtual fracture clinic review |
| Foot | ||
| Fifth metatarsal base fracture (excluding Jones fracture) | Walking orthosis | Virtual discharge |
| Paediatric | ||
| Taurus wrist/forearm fractures | Below elbow soft cast/splint | Virtual discharge |
Upper limb
Clavicle fractures
Despite a recent trend toward surgical fixation of displaced fractures, the majority treated nonoperatively have good outcomes with low rates of mal- or nonunion.34,35 One study demonstrated a 45% virtual discharge rate, 84% of which were undisplaced fractures. A very high majority (90.9%) of the virtually discharged patients were satisfied with the recovery from the injury, with no patient reporting functional limitation.8
Paediatric clavicle fractures have even better results, with one study concluding that there is no need for follow-up of children with isolated, uncomplicated clavicle fractures.36 Another study demonstrated no difference in outcome between children treated operatively v non-operatively for distal clavicle fractures over a 25 year period.37
Recommendation
All undisplaced clavicle fractures can be virtually discharged from VFC (Level 3 evidence).
Radial head fractures and elbow ‘fat pad’ sign
Traditionally, Mason type 1 fractures38 are managed conservatively and types 3 and 4 are treated operatively. Controversy still lies around type 2, but evidence has reported excellent outcomes if these patients are managed conservatively and offered intervention only when there is ongoing restriction.39 Using this background, a group were able to replicate similar outcomes, using a VFC model. They were able to discharge over 90% patents, with Mason type 1 and 2 fractures, virtually and directly from the ED, with high satisfaction rates (95%) with no significant functional limitation.7 No formal patient recorded outcome measures (PROMS) were assessed in this study.
The same group also looked at suspected elbow fractures with and without the presence of the ‘fat pad’ sign. They once again demonstrated a high rate of discharge (79.6%) with high satisfaction rates (95%) among the group.7 However, another prospective study has shown that the sensitivity for radial head/neck fracture is 85.4%, while the specificity is only 50%. Therefore, the absence of a fat-pad sign is a more reliable indicator of the absence of a radial head/ neck fracture.40
Recommendation
Mason 1 radial head fractures can be virtually discharged from a VFC and Mason 2 radial head fractures can be reviewed in a VFC (Level 3 evidence).
Fifth metacarpal neck fractures
Due to the high degree of acceptable angulation in these fractures (40° to 70°), these can be managed conservatively.41,42 Evidence demonstrates that these injuries can be treated with immediate immobilization with a pressure bandage for one week, if the angulation of the fracture is not greater than 70°.43 Furthermore, it has been suggested that these patients can be discharged on first review with an appropriate splint, with no difference in functional outcome and a sooner return to work.44 Based on this evidence, these type of injuries are ideal for the VFC model.
It must be noted that the management of metacarpal head, shaft and base fractures differ greatly and may require more aggressive treatment. Therefore, the rules above do not apply to these.
Recommendation
All fifth metacarpal neck fractures with an angulation < 70° can be virtually discharged from a VFC (Level 3 evidence).
Mallet finger injury
The optimum treatment for mallet finger injuries remains controversial. However, splinting is the most common initial treatment for either soft tissue or bony mallet finger.45 Regardless of the treatment option, patients still develop a slight extensor lag and prominent bump on the finger, but this does not correlate with poor patient satisfaction.46 In fact, many trials have demonstrated that splinting seems to be just as effective as surgical intervention.47 The best outcomes occur in patients who comply with the strict splinting regimen i.e. six weeks of full time splinting, followed by two to six weeks of night-time splinting.45 Therefore, all bony or soft tissue mallet fingers are best treated initially with splints, and can be treated in VFCs. However, bony mallet injuries, which involve more than 30% of the articular surface with joint subluxation, are better managed surgically.45 In the initial stages, these are ideal injuries that could be reviewed in the VFC setting, and are currently being done so in many centres, including the VFC hub at Glasgow.3
Recommendation
Mallet injures with no significant articular involvement can be virtually reviewed in a VFC and discharged at six weeks if there is no residual extensor lag (Level 1 evidence).
Other hand and wrist injuries
Not much evidence currently exists for other injuries of the hand and wrist. A pilot study was initiated at St Mary’s Hospital, London, which showed that a VFC model was able to streamline patients to enable quicker decision making for time critical injuries. In addition, patients were seen by hand therapists quicker, which reduced unnecessary hospital visits prior to therapy appointments.25 However, no current protocols or guidance exists to which other hand and wrist injuries have had successful outcomes using a VFC model.
Recommendation
No clear advice can be given for assessing other hand and wrist injuries in a VFC model at this time.
Lower limb
Ankle fractures
Ankle sprains and Weber A ankle fractures48 have established evidence to be treated conservatively in a walking orthosis.49 Much level 1 evidence already exists showing good outcomes in managing stable Weber B ankle fractures (those with no radiological signs of syndesmotic widening, talar shift, or an associated medial malleolar fracture) nonoperatively in a walking boot or plaster.24,49–51 A large RCT demonstrated no difference in function or pain at six, twelve, or 52 weeks if immobilized in a six week cast, a three week cast, or three week simple orthosis.52 Furthermore, a major trauma centre demonstrated that radiological stable Weber B ankle fractures can be managed using the VFC model.14 Treatment selection based upon stability and surgeon’s judgment led to the best overall good clinical outcome. Therefore, these fractures can be reviewed in a VFC and treated pragmatically by the consultant orthopaedic surgeon.
Recommendation
All stable Weber B ankle fractures can be reviewed in a VFC and potentially discharged at three weeks (Level 1 evidence).
Achilles tendon ruptures
The optimal treatment option is still controversial, with randomized controlled trials and meta-analysis favouring both operative and nonoperative options with similar rerupture rates.53,54 These studies have also favoured accelerated rehabilitation in a boot, which has improved function and calf muscle strength compared to casting.54 Although some cases may be suitable for operative management, the nonoperative cases have shown favourable results (3.82% rerupture rate; 64.6% painless weight-bearing at discharge) when being streamlined in to a VFC model, which can be initiated in the ED.15 The limitations of this study were that no PROMS or patient satisfaction levels were assessed. In addition, only 64.8% of patients had an ultrasound proven Achilles tendon (TA) rupture, meaning that the remaining patients had an alternate diagnosis, which did not need to be started on the TA pathway. Therefore, an orthopaedic specialist should be consulted to confirm the diagnosis, before initiating the TA rupture pathway.
Recommendation
All TA ruptures can be started on a standardized TA rupture pathway and referred to the VFC for review, as long as an orthopaedic specialist has reviewed the patient prior to referral to VFC (Level 3 evidence).
Fifth metatarsal fractures
This common fracture has traditionally been treated nonoperatively in casts for three to 12 weeks until radiological and clinical signs of union.55 However, newer studies have introduced treating these injuries in a weight-bearing orthosis, with casting causing a delay to full function.56,57 This injury was adopted by the original Glasgow VFC model, which showed a good satisfaction rate (79%) among patients. Similar results were replicated in another study and supported the use of VFC system, using a standardized protocol to immediately fully weight-bear all fifth metatarsal fractures from the ED.16 The main resistance was the fear of missing Jones’ fractures16 due to the high non-union risk, which did not occur in any of the 663 cohort. All cases were reviewed by a consultant orthopaedic surgeon the following day, eliminating that fear of missing significant injuries.
Recommendation
Fifth metatarsal fractures can be virtually discharged from a VFC (Level 3 evidence).
Soft tissue knee injuries
There is currently no literature exploring the management of soft tissue knee injuries in a VFC. The very nature of the injury, which relies heavily on reliable clinical examination and advanced imaging methods of MRI or CT over and above simple radiographs, makes it difficult to be manged virtually.
There is clear evidence that there is improvement in final clinical outcome. if such injuries are fast tracked to treatment. A number of studies surrounding the advent of acute knee clinics’ (AKC) have shown clear improvement in time to diagnosis and time to surgery, which have led to avoidance of secondary injuries such as meniscal or osteochondral damage. Ball and Haddad58 report 89% reduction in waiting time to see a specialist, with Sapsford and Sutherland59 reporting a similar 90%. They also showed 95% of patients seen in AKC had surgery performed within 12 months, as opposed to 53% via triage through elective clinics.
Recommendation
No clear advice can be given for assessing soft tissue knee injuries in the VFC model. However, we recommend that patients with these injuries be triaged through to an AKC using the VFC model.
Paediatric injuries
Paediatric wrist fractures (torus/buckle)
Many studies have demonstrated that a minimalist approach to managing these fractures, has shown improved function, reduced return time to school along with reduced cost and medical time.60,61 Recent research has guided the use of soft casts or splints rather than rigid casts,62 and this has been advocated by the most recent National Institute for Health and Care Excellence (NICE) guidelines for the management of torus fractures.63 A recent retrospective study also demonstrated increased efficiency and cost reduction in managing these injuries in a VFC setting.21
Recommendation
All paediatric torus fractures can be virtually discharged from VFC (Level 2 evidence).
Other paediatric fractures
The controversy of VFC for paediatric cases stems from the fact that we tend to rely on the objective clinical examination findings to a greater extent with children, rather than history. Despite this, the use of VFC and home management protocols in children has been increasing over the past few years.4,36,37 However, only one group have managed to restructure and re-organise a paediatric VFC model, in which strict protocols were made for common and stable (undisplaced) paediatric injuries.22 As well as the cost savings (staff costs, materials costs, appointment tariff), they hypothesised a paediatric VFC would mean less time missed in education and less disruption to parents and siblings routine. Patients who requested face to face appointments, were keen to receive more reassurance and guidance, rather than due to poor functional outcome.22
Recommendation
Other undisplaced paediatric fractures can be reviewed in a VFC, as long as there are measures in place for parents to access urgent face to face review if they have concerns (Level 4 evidence).
Conclusion
This systematic review demonstrates that there are several orthopaedic conditions that can be managed nonoperatively. In this article, we highlight many of them that are suitable for a VFC service. The VFC model has shown to decrease the burden on fracture clinic appointments, improve adherence to BOAST guidelines, and shown a large cost saving benefit.
Our trauma service demand is ever increasing and being put to the test and all orthopaedic professionals are having to adapt the way they deliver their service. The VFC model provides one option of delivering urgent care and, for the conditions discussed in this article, where there is a robust evidence base. We would encourage colleagues to embrace the VFC model to help deliver a better, more cost-effective and more efficient arm of the trauma service to our patients. If widespread adoption of VFC occurs, this would also present the possibility for a pragmatic multicentre regional study to generate further data and refine the evidence base for remote consulting in trauma and orthopaedics.
References
1. BOA Standards for Trauma (BOASTs) . BOAST 7: fracture clinic services, August 2013. British orthopaedic association . 2020 . http://www.boa.ac.uk/publications/boast-7-fracture-clinic-services (date last accessed 26th June 2020 ). Google Scholar
2. NHS England . A&E Attendances and Emergency Admissions . 2020 . https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ (date last accessed 26th June 2020 ). Google Scholar
3. Fracture Pathway . Redesign at Glasgow Royal Infirmary . 2020 . http://www.fractureclinicredesign.org. (date last accessed 26th June 2020 ). Google Scholar
4. Vardy J , Jenkins PJ , Clark K , et al. Effect of a redesigned fracture management pathway and 'virtual' fracture clinic on ED performance . BMJ Open . 2014 ; 4 ( 6 ): e005282 . Crossref PubMed Google Scholar
5. O' Reilly M , Breathnach O , Conlon B , Kiernan C , Sheehan E . Trauma assessment clinic: virtually a safe and smarter way of managing trauma care in Ireland . Injury . 2019 ; 50 ( 4 ): 898 – 902 . Crossref PubMed Google Scholar
6. Breathnach O , O'Reilly M , Morrissey K , Conlon B , Sheehan E . Electronic referrals for virtual fracture clinic service using the National integrated medical imaging system (NIMIS) . Ir J Med Sci . 2019 ; 188 ( 2 ): 371 – 377 . Crossref PubMed Google Scholar
7. Jayaram PR , Bhattacharyya R , Jenkins PJ , Anthony I , Rymaszewski LA . A new "virtual" patient pathway for the management of radial head and neck fractures . J Shoulder Elbow Surg . 2014 ; 23 ( 3 ): 297 – 301 . Crossref PubMed Google Scholar
8. Bhattacharyya R , Jayaram PR , Holliday R , Jenkins P , Anthony I , Rymaszewski L . The virtual fracture clinic: reducing unnecessary review of clavicle fractures . Injury . 2017 ; 48 ( 3 ): 720 – 723 . Crossref PubMed Google Scholar
9. McKirdy A , Imbuldeniya AM . The clinical and cost effectiveness of a virtual fracture clinic service: an interrupted time series analysis and before-and-after comparison . Bone Joint Res . 2017 ; 6 ( 5 ): 259 – 269 . Crossref PubMed Google Scholar
10. Holgate J , Kirmani S , Anand B . Virtual fracture clinic delivers British orthopaedic association compliance . Annals . 2017 ; 99 ( 1 ): 51 – 54 . Crossref PubMed Google Scholar
11. Jenkins PJ , Morton A , Anderson G , Van Der Meer RB , Rymaszewski LA . Fracture clinic redesign reduces the cost of outpatient orthopaedic trauma care . Bone Joint Res . 2016 ; 5 ( 2 ): 33 – 36 . Crossref PubMed Google Scholar
12. Anderson GH , Jenkins PJ , McDonald DA , et al. Cost comparison of orthopaedic fracture pathways using discrete event simulation in a Glasgow Hospital . BMJ Open . 2017 ; 7 ( 9 ): e014509 . Crossref PubMed Google Scholar
13. Jenkins P , Gilmour A , Murray O , Anthony I , Nugent MP . The Glasgow fracture pathway: a virtual clinic . BJJ News . 2014 . Google Scholar
14. Bellringer SF , Brogan K , Cassidy L , Gibbs J . Standardised virtual fracture clinic management of radiographically stable Weber B ankle fractures is safe, cost effective and reproducible . Injury . 2017 ; 48 ( 7 ): 1670 – 1673 . Crossref PubMed Google Scholar
15. Robertson A , Godavitarne C , Bellringer S , et al. Standardised virtual fracture clinic management of Achilles tendon ruptures is safe and reproducible . Foot Ankle Surg . 2019 ; 25 ( 6 ): 782 – 784 . Crossref PubMed Google Scholar
16. Brogan K , Bellringer S , Akehurst H , et al. Virtual fracture clinic management of fifth metatarsal, including Jones', fractures is safe and cost-effective . Injury . 2017 ; 48 ( 4 ): 966 – 970 . Crossref PubMed Google Scholar
17. Logishetty K . Adopting and sustaining a Virtual Fracture Clinic model in the District Hospital setting - a quality improvement approach . BMJ Qual Improv Rep . 2017 ; 6 ( 1 ): u220211.w7861 . Crossref PubMed Google Scholar
18. Kelly M , O'Keeffe N , Francis A , et al. Connolly Hospital trauma assessment clinic (Tac): a virtual solution to patient flow . Ir J Med Sci . 2020 ; 189 ( 2 ): 425 – 429 . Crossref PubMed Google Scholar
19. Mackenzie SP , Carter TH , Jefferies JG , et al. Discharged but not dissatisfied: outcomes and satisfaction of patients discharged from the Edinburgh trauma triage clinic . Bone Joint J . 2018 ; 100-B ( 7 ): 959 – 965 . Google Scholar
20. Ferguson KB , McGlynn J , Jenkins P , Madeley NJ , Kumar CS , Rymaszewski L . Fifth metatarsal fractures - Is routine follow-up necessary? Injury . 2015 ; 46 ( 8 ): 1664 – 1668 . Crossref PubMed Google Scholar
21. Seewoonarain S , Babu S , Sangoi D , Avasthi A , Ricketts D . Introducing a virtual fracture clinic increases efficiency and reduces costs in Torus fracture management . Pediatr Qual Saf . 2019 ; 4 ( 6 ): e202 . Crossref PubMed Google Scholar
22. Robinson PM , Sim F , Latimer M , Mitchell PD . Paediatric fracture clinic re-design: incorporating a virtual fracture clinic . Injury . 2017 ; 48 ( 10 ): 2101 – 2105 . Crossref PubMed Google Scholar
23. Gamble D , Jenkins PJ , Edge MJ , et al. Satisfaction and functional outcome with "self-care" for the management of fifth metacarpal fractures . Hand . 2015 ; 10 ( 4 ): 607 – 612 . Crossref PubMed Google Scholar
24. Rowley DI , Norris SH , Duckworth T . A prospective trial comparing operative and manipulative treatment of ankle fractures . J Bone Joint Surg Br . 1986 ; 68 ( 4 ): 610 – 613 . Crossref PubMed Google Scholar
25. Evans D , Hardman J , Middleton SD , Anakwe RE . Developing a virtual fracture clinic for hand and wrist injuries . J Hand Surg Eur Vol . 2018 ; 43 ( 8 ): 893 – 894 . Crossref PubMed Google Scholar
26. Ramasubbu B , McNamara R , Deiratany S , Okafor I . An evaluation of the accuracy and necessity of fracture clinic referrals in a busy pediatric emergency department . Pediatr Emerg Care . 2016 ; 32 ( 2 ): 69 – 70 . Crossref PubMed Google Scholar
27. Virtual Fracture Clinic . Welcome to BSUH virtual fracture clinic . 2017 . https://www.fracturecare.co.uk Google Scholar
28. NHS . Virtual fracture clinic (VFC) . https://www.mtw.nhs.uk/service/trauma-orthopaedics/virtual-fracture-clinic-vfc/ Google Scholar
29. NHS . Virtual fracture clinic . 2017 . https://www.uhs.nhs.uk/OurServices/Traumaandorthopaedics/Virtual-fracture-clinic/Virtual-fracture-clinic.aspx Crossref PubMed Google Scholar
30. NHS . Virtual fracture clinic for adults . 2020 . https://www.leedsth.nhs.uk/a-z-of-services/virtual-fracture-clinic-for-adults/ Google Scholar
31. NHS . Virtual fracture clinic (VFC) . 2020 . https://www.rlbuht.nhs.uk/departments/medical-specialisms/acute-and-emergency-care/trauma-and-orthopaedics/virtual-fracture-clinic-vfc/ Google Scholar
32. NHS . Virtual fracture clinic . 2020 . https://www.royalfree.nhs.uk/services/services-a-z/trauma-and-orthopaedics/virtual-fracture-clinic/ Crossref PubMed Google Scholar
33. NHS . Virtual fracture clinic . 2020 . https://www.porthosp.nhs.uk/departments-and-services/virtual-fracture-clinic/96350 Crossref PubMed Google Scholar
34. Ahrens PM , Garlick NI , Barber J , Tims EM , Clavicle Trial Collaborative Group . The clavicle trial: a multicenter randomized controlled trial comparing operative with Nonoperative treatment of displaced Midshaft clavicle fractures . J Bone Joint Surg Am . 2017 ; 99 ( 16 ): 1345 – 1354 . Crossref PubMed Google Scholar
35. Canadian Orthopaedic Trauma Society . Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial . J Bone Joint Surg Am . 2007 ; 89 ( 1 ): 1 – 10 . Crossref PubMed Google Scholar
36. Calder JDF , Solan M , Gidwani S , Allen S , Ricketts DM . Management of paediatric clavicle fractures--is follow-up necessary? An audit of 346 cases . Ann R Coll Surg Engl . 2002 ; 84 ( 5 ): 331 – 333 . Crossref PubMed Google Scholar
37. Nenopoulos SP , Gigis IP , Chytas AA , Beslikas TA , Nenopoulos AS , Christoforidis JE . Outcome of distal clavicular fracture separations and dislocations in immature skeleton . Injury . 2011 ; 42 ( 4 ): 376 – 380 . Crossref PubMed Google Scholar
38. Mahmoud SSS , Moideen AN , Kotwal R , Mohanty K . Management of Mason type 1 radial head fractures: a regional survey and a review of literature . Eur J Orthop Surg Traumatol . 2014 ; 24 ( 7 ): 1133 – 1137 . Crossref PubMed Google Scholar
39. Duckworth AD , Watson BS , Will EM , et al. Radial head and neck fractures: functional results and predictors of outcome . J Trauma . 2011 ; 71 ( 3 ): 643 – 648 . Crossref PubMed Google Scholar
40. Irshad F , Shaw NJ , Gregory RJ . Reliability of fat-pad sign in radial head/neck fractures of the elbow . Injury . 1997 ; 28 ( 7 ): 433 – 435 . Crossref PubMed Google Scholar
41. Diaz-Garcia R , Waljee JF . Current management of metacarpal fractures . Hand Clin . 2013 ; 29 ( 4 ): 507 – 518 . Crossref PubMed Google Scholar
42. Hunter JM , Cowen NJ . Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty-three cases . J Bone Joint Surg Am . 1970 ; 52 ( 6 ): 1159 – 1165 . PubMed Google Scholar
43. Statius Muller MG , Poolman RW , van Hoogstraten MJ , Steller EP . Immediate mobilization gives good results in boxer's fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization . Arch Orthop Trauma Surg . 2003 ; 123 ( 10 ): 534 – 537 . Crossref PubMed Google Scholar
44. Bansal R , Craigen MAC , C CMa . Fifth metacarpal neck fractures: is follow-up required? J Hand Surg Eur Vol . 2007 ; 32 ( 1 ): 69 – 73 . Crossref PubMed Google Scholar
45. Alla SR , Deal ND , Dempsey IJ . Current concepts: mallet finger . Hand . 2014 ; 9 ( 2 ): 138 – 144 . Crossref PubMed Google Scholar
46. Cheung JPY , Fung B , Ip WY . Review on mallet finger treatment . Hand Surg . 2012 ; 17 ( 3 ): 439 – 447 . Crossref PubMed Google Scholar
47. Handoll HHG , Vaghela MV . Interventions for treating mallet finger injuries . Cochrane Database Syst Rev . 2004 ( 3 ): CD004574 . Crossref PubMed Google Scholar
48. Goost H , Wimmer MD , Barg A , Kabir K , Valderrabano V , Burger C . Fractures of the ankle joint: investigation and treatment options . Dtsch Arztebl Int . 2014 ; 111 ( 21 ): 377 – 388 . Crossref PubMed Google Scholar
49. Yde J , Kristensen KD . Ankle fractures. Supination-eversion fractures stage II. primary and late results of operative and non-operative treatment . Acta Orthop Scand . 1980 ; 51 ( 4 ): 695 – 701 . Crossref PubMed Google Scholar
50. Makwana NK , Bhowal B , Harper WM , Hui AW . Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age. A prospective, randomised study . J Bone Joint Surg Br . 2001 ; 83 ( 4 ): 525 – 529 . Crossref PubMed Google Scholar
51. Phillips WA , Schwartz HS , Keller CS , et al. A prospective, randomized study of the management of severe ankle fractures . J Bone Joint Surg Am . 1985 ; 67 ( 1 ): 67 – 78 . PubMed Google Scholar
52. Kortekangas T , Haapasalo H , Flinkkilä T , et al. Three week versus six week immobilisation for stable Weber B type ankle fractures: randomised, multicentre, non-inferiority clinical trial . BMJ . 2019 ; 364 : k5432 . Crossref PubMed Google Scholar
53. Deng S , Sun Z , Zhang C , Chen G , Li J . Surgical Treatment Versus Conservative Management for Acute Achilles Tendon Rupture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials . J Foot Ankle Surg . 2017 ; 56 ( 6 ): 1236 – 1243 . Google Scholar
54. Willits K , Amendola A , Bryant D , et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation . J Bone Joint Surg Am . 2010 ; 92 ( 17 ): 2767 – 2775 . Crossref PubMed Google Scholar
55. Torg JS , Balduini FC , Zelko RR , Pavlov H , Peff TC , Das M . Fractures of the base of the fifth metatarsal distal to the tuberosity. classification and guidelines for non-surgical and surgical management . J Bone Joint Surg Am . 1984 ; 66 ( 2 ): 209 – 214 . PubMed Google Scholar
56. Polzer H , Polzer S , Mutschler W , Prall WC . Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence . Injury . 2012 ; 43 ( 10 ): 1626 – 1632 . Crossref PubMed Google Scholar
57. Shahid MK , Punwar S , Boulind C , Bannister G . Aircast walking boot and below-knee walking cast for avulsion fractures of the base of the fifth metatarsal: a comparative cohort study . Foot Ankle Int . 2013 ; 34 ( 1 ): 75 – 79 . Crossref PubMed Google Scholar
58. Ball S , Haddad FS . The impact of an acute knee clinic . Ann R Coll Surg Engl . 2010 ; 92 ( 8 ): 685 – 688 . Crossref PubMed Google Scholar
59. Sapsford H , Sutherland AG . Reducing time to surgery after anterior cruciate ligament injury . Scott Med J . 2016 ; 61 ( 2 ): 84 – 87 . Crossref PubMed Google Scholar
60. van Bosse HJP , Patel RJ , Thacker M , Sala DA . Minimalistic approach to treating wrist Torus fractures . J Pediatr Orthop . 2005 ; 25 ( 4 ): 495 – 500 . Crossref PubMed Google Scholar
61. Williams BA , Alvarado CA , Montoya-Williams DC , Matthias RC , Blakemore LC . Buckling down on Torus fractures: has evolving evidence affected practice? J Child Orthop . 2018 ; 12 ( 2 ): 123 – 128 . Crossref PubMed Google Scholar
62. Witney-Lagen C , Smith C , Walsh G . Soft cast versus rigid cast for treatment of distal radius buckle fractures in children . Injury . 2013 ; 44 ( 4 ): 508 – 513 . Crossref PubMed Google Scholar
63. National Institute for Health and Care Excellence . Fractures (non-complex): assessment and management (NG 38 , 2020 . Google Scholar
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.










