Abstract
Mechanical alignment has been a fundamental tenet of total knee arthroplasty (TKA) since modern knee replacement surgery was developed in the 1970s. The objective of mechanical alignment was to infer the greatest biomechanical advantage to the implant to prevent early loosening and failure. Over the last 40 years a great deal of innovation in TKA technology has been focusing on how to more accurately achieve mechanical alignment. Recently the concept of mechanical alignment has been challenged, and other alignment philosophies are being explored with the intention of trying to improve patient outcomes following TKA.
This article examines the evolution of the mechanical alignment concept and whether there are any viable alternatives.
Evolution of alignment concepts
Anatomists started detailing the morphology of the knee in the mid 1800s. The concept of improving lower limb alignment through osteotomy can be traced back to 1875 when Volkmann wrote on tibial osteotomies to improve a deformity of the knee.1 Zuppinger carried out the first radiological study of the knee in 1904 (Fig. 1).2 Early osteotomies concentrated on straightening the leg and distributing load symmetrically across the joint. Debeyre and Patte were the first to report on a series of corrective osteotomies in osteoarthritis of the knee, concluding that they redistributed the load across the joint.3
Fig. 1
Zuppinger’s early manuscript containing early radiographic studies of the knee.2
By the mid twentieth century, radiographs were becoming more widespread in clinical work, and consequently the bony morphology could be visualised and various angles around the knee could be measured. The term ‘femorotibial angle’ was coined as the measurement of the intersection in the coronal plane of the long axis of femur and tibia at the knee joint and today is often referred to as the tibiofemoral angle (Fig.2). This angle gained popularity in knee osteotomies as a way of determining the degree of correction. The first published paper in the UK to reference the femorotibial angle in osteotomies was by Jackson and Waugh in 1961, 4 and they measured 50 healthy knees and found the femorotibial angle on average to be 2°. Kettelkamp et al5 later disputed this figure in 1976 and suggested that the normal femorotibial valgus angulation was 7°, which is more in line with what we accept today.
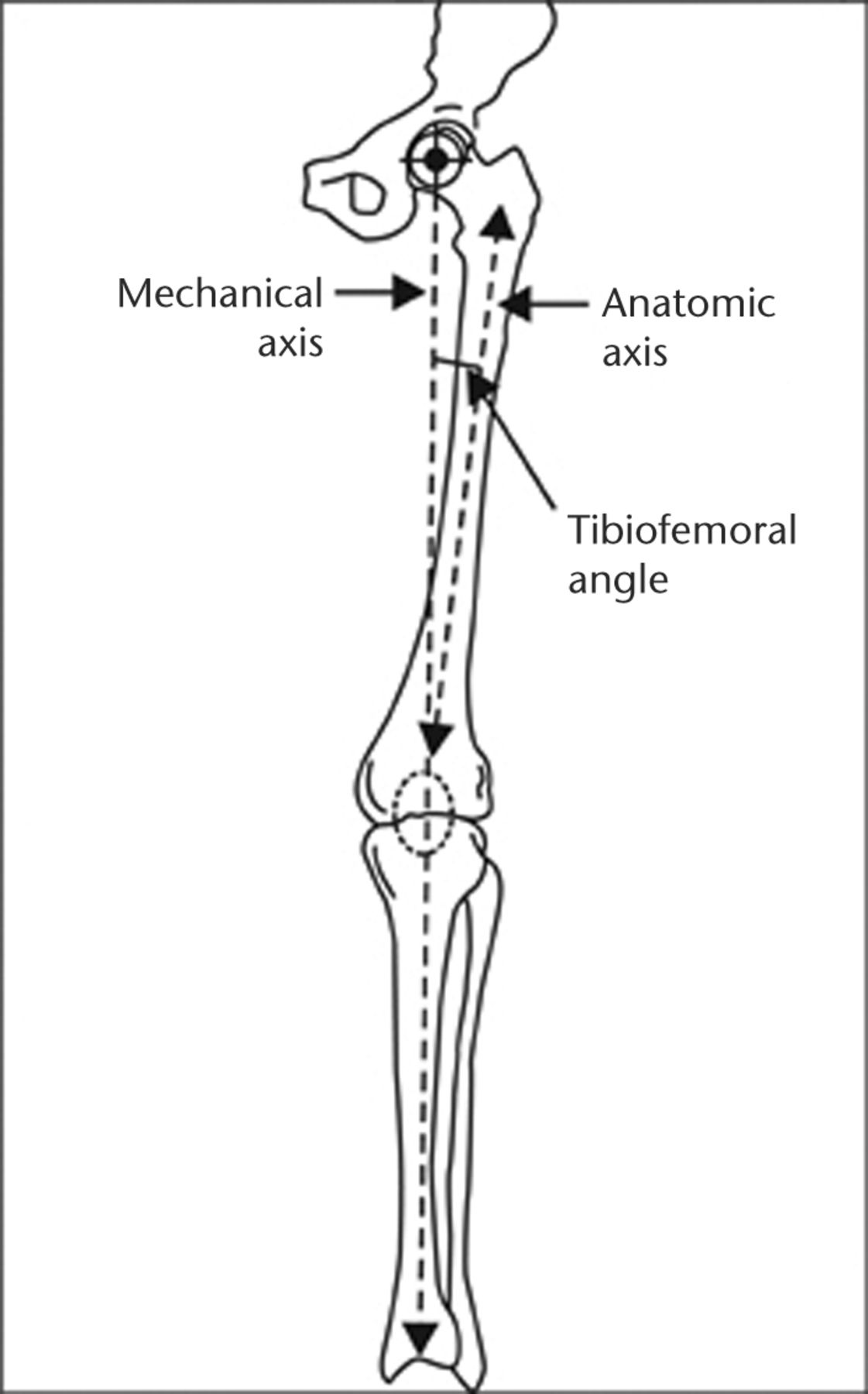
Fig. 2
The relationship between the mechanical and anatomic axis demonstrating the tibiofemoral angle.
The concept of the mechanical axis was introduced around the same time in Maquet’s ‘Quelques remarques sur les radiographies’.6 Alignment correction operations (osteotomies) were being planned on the basis of measurements made from full length radiographs of the affected leg, taken with the patient balancing on that extremity demonstrating an angle formed by the mechanical axisof the femur, connecting the centre of the femoral head and the intercondylar notch and the mechanical axis of the tibia between the tibial spines and the centre of the ankle.
Early techniques for knee arthroplasty were being developed around the same time as lower limb osteotomies were being popularised. The first metallic mould was introduced into the knee as a primitive form of arthroplasty by Campbell in 1940,7 and attempts were made to correct alignment with acrylic tibial plateau prostheses by MacIntosh in 1958,8 although it was not really until the 1970s that prototypes recognisable as similar to the TKAs in use today were developed.
The early condylar total knee designs of the 1970s fell into two broad categories; the anatomic approach and the functional approach. The anatomic approach was based on preservation of the soft-tissue constraints with replacement or resurfacing of the articular surface. The Gunston polycentric knee9 was an example of an anatomical knee, as was the UCI knee,10 but with more constrained implants, replicating the femoral condyles and tibial plateau using casting techniques.
In the case of the Gunston polycentric knee arthroplasty,9 it was designed to simulate opposing joint surfaces by separate implants for each joint surface. Collateral and cruciate ligaments were both retained to maintain joint stability. The polycentric knee reported to provide significant relief of pain in 86% of 500 knees, and the independence and activity levels of the patients increased dramatically. It was used predominantly in rheumatoid arthritis, however, it was prone to failure because the patellofemoral joint was not addressed and dislocation and subluxations were common as a consequence of ligamentous laxity in the presence of unbalanced soft tissues. To further compound the problems, high rates of loosening of the tibial components were also seen.11,12 The stumbling block with these anatomical designs at the time were that these complex geometries were difficult to manufacture, the surgery was technically demanding, and deformity correction was not always possible without extensive soft-tissue resection.
The alternative to the anatomical approach was the functional approach, whereby the mechanics of the knee were simplified by resection of the condyles and the cruciate ligaments so the implant could be seated on a flat cancellous bone surface. The concept of the mechanical axis used in osteotomies was taken and used as a guide for implanting the prostheses.
Freeman stated in his implant design objectives13 that the prosthetic component should be fitted to the bone by a means that spread the load over the largest possible area of the bone prosthesis interface. Instruments were designed to assist alignment and for checking the balance of the knee. Functional knee replacements ignored the natural obliquity of the joint (the lateral distal femoral angle and medial proximal tibial angle (Fig. 3)14 in favour of a flat surface for the implant to sit on (Fig. 4).
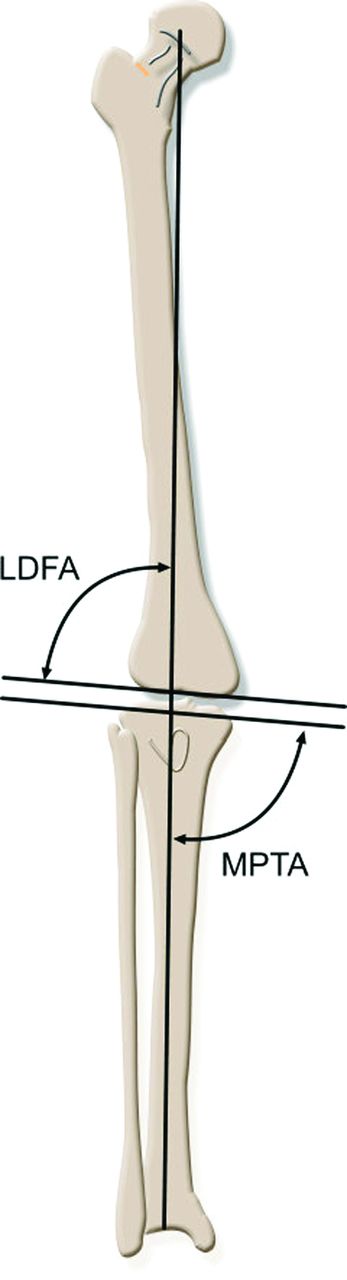
Fig. 3
Lateral Distal Femoral Angle (LDFA) and Medial Proximal Tibial Angle (MPTA), demonstrating the natural joint line obliquity.
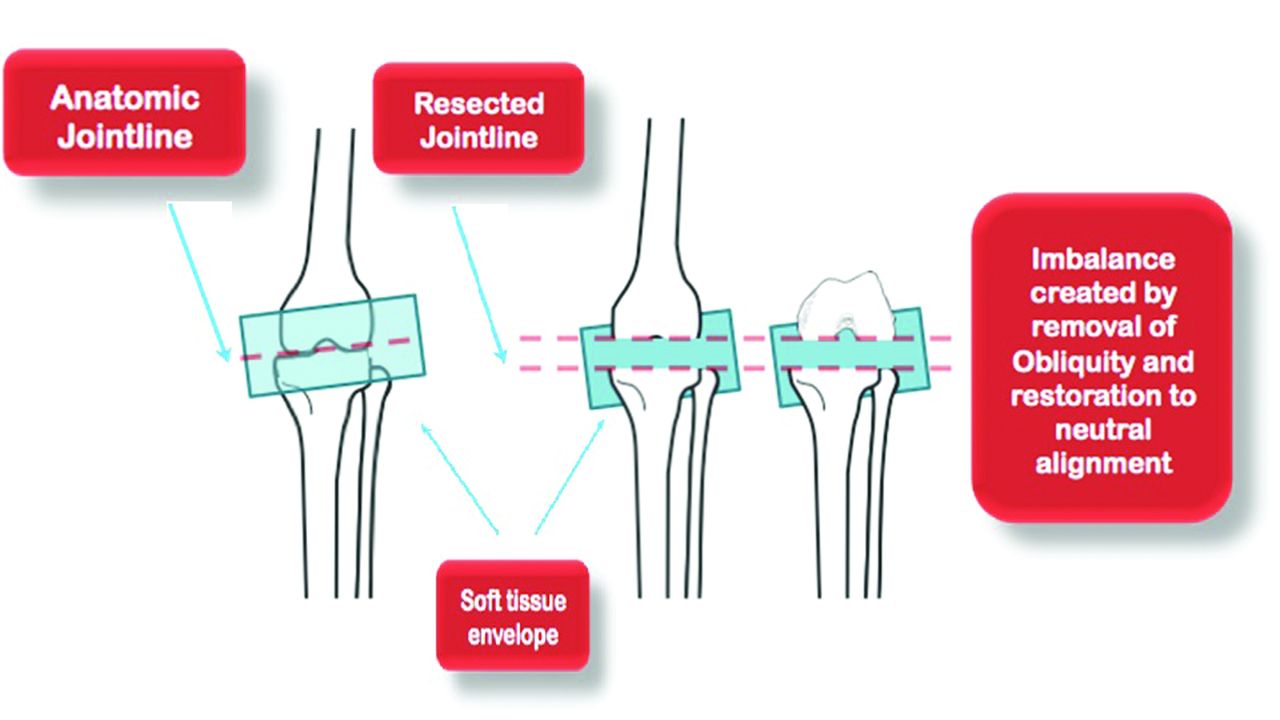
Fig. 4
A cut perpendicular to the mechanical axis. Ignoring the natural joint line obliquity creates a soft-tissue imbalance.
Success in knee arthroplasty has long been measured by the survivorship of the implant. This was no different in the 1970s, and at this stage the functional approach was yielding improved survivorship over the anatomic approach, thus implants such as the Gunston quickly became obsolete.
‘Thou shalt not varus’
As mechanical alignment became the norm, clinical studies began to examine the correlation between position of the TKA and clinical outcome and survivorship. An early example of this was Lotke and Ecker in 1977,15 examining 76 TKAs between 1972 and 1974. Short knee radiographs were compared with a knee evaluation index and revealed a strong correlation between good positioning of the prosthesis and good early clinical results, although there was no statistically significant correlation of mechanical failure and radiograph alignment scores.
One of the first large series comparing alignment and outcome in the same type of knee implant was by Hood, Vanni and Insall in 1981,16 measuring tibiofemoral angles on short leg films before and after implantation of Insall-Burstein knee replacements in 225 patients (tibiofemoral valgus of 7°; +/- 5°deemed satisfactory). Of the three failures, none were outside the limits that Hood had chosen. In 1983 Bargren and Blaha17 initiated a biomechanical study to assess the effects of eccentric loading on tibial component failure using the Freeman Swanson implant. The clinical outcome with relation to alignment in patients with the same implant using the small area tibial component between 1971 and 1975 was also reviewed. Taking into consideration that 1° to 13° of tibiofemoral valgus was deemed satisfactory, they found that 91% of the varus knees failed, 100% of the neutral knees failed and 11% of the valgus knees failed, demonstrating that the functionally designed early TKAs also had poor survivorship, even if the prostheses were implanted in the desired alignment. Tew and Waugh18 picked up the subject again in 1985, pointing out that although the relationship between alignment and failure may have seemed too obvious to need substantiating, there was little evidence to support it. Their paper reviewed 428 TKAs of six different designs between 1972 and 1983 and found that those in extremes of varus and valgus did have significantly higher rates of failure.
Interest in the association between coronal alignment of the TKA and failure gathered momentum through the course of the 1990s. A number of clinical papers were published looking at prostheses predominantly implanted in the 1970s to 1980s,19,20 suggesting that deviation from the mechanical axis would lead to premature failure, leading to the now commonly expressed adage ‘thou shalt not varus’. It is worth considering at this stage a number of important factors. These studies were examining functional TKAs that were designed to be implanted on a flat surface. Long leg radiographs were not commonplace and most of the studies had examined coronal alignment on short knee films. The correlation between tibiofemoral angle from knee radiographs and the mechanical axis obtained from full-limb radiographs ranges from 0.65 to 0.88.21-23 Also, only one aspect of the multifaceted complex issue of alignment was being investigated; that of coronal alignment in extension. Little or no attention was being paid to alignment in the sagittal and axial planes, and how this might contribute to failure, or indeed soft-tissue balance and level of the joint line.
Research in the late 1990s shifted slightly from the simple relationship between coronal alignment and failure to trying to quantify the mode of failure. In 1999 a correlation between alignment and wear was established by Miura et al.24 A tibial retrieval analysis of 89 Depuy PFC TKAs implanted between 1984 and 1998 by Collier et al25 found shelf age of the polyethylene, patient age and varus alignment of greater than 5° all independently contributed to increased medial polyethylene wear. Biomechanical evidence suggested that varus tibial alignment led to increased posteromedial tibial surface strain in cadaver and knee simulator studies.26-29
The relationship between coronal mechanical alignment and its association with survivorship had built a weight of evidence and this in turn led to innovations in ways of more accurately reproducing mechanical alignment. Improvements with intra- and extramedullary guidance jigs enhanced the reproducibility of achieving overall mechanical alignment in the coronal plane, however, rotational alignment still relied on interpretation of anatomical landmarks.
The modern era: Improved accuracy of alignment? Improved survivorship? Improved patient satisfaction?
By the end of the 1990s, TKAs were achieving better patient satisfaction, improved function and > 90% implant survival at 15 years.30-32 The development of crosslinking UHMWPE was shown to reduce rates of wear in the hip33 and was now being translated to the knee.34
Computer navigation (CN) was introduced as a new technology with the potential to further increase the accuracy of alignment,35 enabling quantification of alignment parameters in multiple planes, but on the premise that increased accuracy would result in increased survivorship and outcome.
The advent of CN led to the publication of numerous trials utilising the technology. Meta-analysis of studies using CN suggested that improved accuracy of desired alignment is achieved using the technique.35
There has also been renewed debate as to whether the more modern implants with improved wear characteristics do fail earlier if a degree of deviation from mechanical alignment exists; the evidence is conflicting. Morgan et al36 in 2008 published a series of 197 Kinemax knees implanted from 1990 to 1993 with a mean follow-up of nine years and was unable to demonstrate any difference in revision rates between alignment groups.
Following on from an article in 1994,19 Ritter 37 published results in 2009 to re-establish the importance of mechanical alignment. This was a continuation of his work with Berend 38. This study used multiple different versions of the AGC implants from 1983 to 2006. Short knee radiographs were used for measurements. The failure rate out with neutral alignment from 2.4° to 7.2° tibiofemoral valgus was found to be significantly higher and as with his previous paper (it was largely the same cohort of patients) varus failure was mostly due to medial tibial collapse. This was in response to research published by Parratte et al.39 Parratte analysed 398 knee implants between 1985 and 1990 with long leg alignment films and a 15-year follow-up. The results showed that there was no difference in revision rate between prostheses implants in neutral (mechanical alignment 0+/-3°) and those in misalignment. This has again been supported by recent research showing there doesn’t appear to be a correlation between misalignment and clinical outcome following TKA.40
The last publication to date adds further weight to the ambiguity of the subject. Bonner et al41 analysed a total of 501 TKAs divided into an aligned group with a neutral mechanical axis (± 3°) and a misaligned group where the mechanical axis deviated from neutral by > 3°. At 15 years’ follow-up there was no significant difference in revision for aseptic loosening between the two groups.
The literature on alignment and implant survivorship encompasses a huge diversity and evolution of implant and polyethylene designs over the last 40 years. There is a large variation in study methodology and analysis. Implants fail for a variety of reasons and the more recent literature would suggest that coronal alignment alone is not a good discriminator of implant longevity.
Regarding patient satisfaction, data from the National Joint Registries Annual Report 201342 suggests that the majority of TKAs have a > 95% survivorship at nine years. Perhaps more pertinent is the patient perception of their outcome following surgery. Of the 132,019 patients who had a primary knee operation in 2012/2013 with an associated patient-reported outcome measure entry, 16.4% described their outcome as fair or poor, compared with 8.2% of patients who underwent primary hip surgery.
CN has undoubtedly improved accuracy of desired alignment but what CN has not been able to adequately demonstrate is that achieving mechanical alignment improves patient satisfaction following the TKA.43
The functional versus anatomical implant debate reignited
Accuracy of desired alignment is improving, survivorship is improving but, importantly, patient satisfaction in TKA remains disappointing compared with hip surgery. Belleman’s recent work confirms the concept of constitutional varus. ‘An important fraction of the normal population has a natural alignment at the end of growth of 3° varus or more (Fig. 5). Restoration of mechanical alignment to neutral in these cases may not be desirable and would be unnatural for them’ (Fig. 6).44
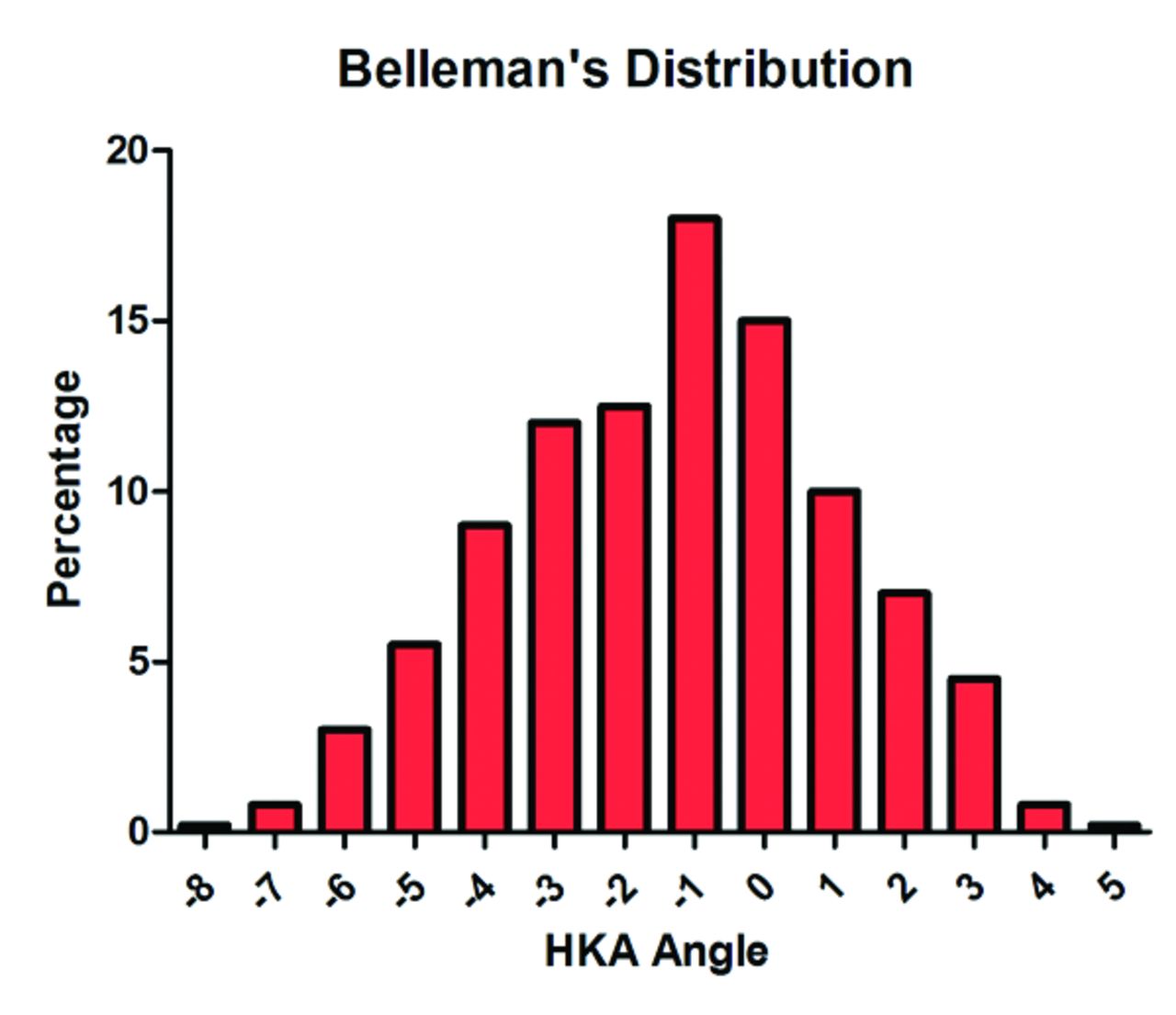
Fig. 5
Belleman’s graph demonstrating the overall Hip Knee Ankle (HKA) axis in the general population is in overall varus. Data taken from Bellemans et al.44
Fig. 6
A clear illustration of the variation in normal lower limb alignment.
The consequence of this ambiguity in the relationship between alignment and outcome has led to renewed interest in trying to achieve a more anatomical prosthesis akin to those made obsolete in the 1970s. The increasing use of more detailed imaging and computer software means it is now possible to critically look at alignment in three dimensions; this is the foundation for Patient Specific Instrumentation (PSI). CT and MRI scanning have enabled detailed three-dimensional pre- and post-operative assessment of the knee joint, which in turn has enabled custom PSI instrumentation. PSI offers the opportunity to accurately quantify alignment in every plane for the individual patient, and the cutting guides not only set the appropriate coronal orientation, but also the depth of resection, rotation, slope and flexion and extension axis based on the pre-operative template.
The majority of PSI manufacturers produce the guides to accurately create neutral mechanical lower limb alignment. Some companies, however, are now using this imaging technology to create a template to implant the TKA prosthesis in a position that is more anatomical (Stryker Shapematch). This is supposed to recreate the alignment of the patient’s limb in their pre-arthritic state, taking into consideration natural individual variation in the alignment of the normal knee.45 There has been recent research that has suggested that there is a single flexion-extension axis about the distal femur bisecting the femoral condyles but it does not correspond exactly to that of the epicondylar axis (Fig. 7).45 With the use of MRI or CT for pre-operative planning, this flexion-extension axis can be defined by creating a single axis through the femoral condyles (Fig. 8)46 and the PSI could then be produced to recreate it.

Fig. 7
A cylinder is superimposed onto the femoral condyle to define a single flexion and extension axis. Reprinted with permission from The Journal of Bone and Joint Surgery Inc.45

Fig. 8
Three-dimensional knee model construction , illustrating the difference between with epicondylar (yellow) and cylindrical (green) axes. Reprinted with permission from The Journal of Bone and Joint Surgery Inc.45
Similarly the ConforMIS iTotal system is designed to cut the femur and tibia perpendicular to the mechanical axis but then aims to recreate the natural joint line by building in obliquity, if necessary, to both the tibial polyethylene and condyles of the femoral implant. Overall, neutral mechanical alignment is still maintained.
The advent of PSI, CN and more modern, wear resistant implants has re-opened the debate that was started in the 1970s regarding functional and anatomical implants. The reasons for ignoring the normal anatomy of the knee have changed slightly 40 years on. Complex geometries are now easier to manufacture and the surgery is less technically demanding. What remains an unknown at present is whether patient satisafaction will improve or survivorship of the implant will be compromised if the current generation of prostheses are designed in a more anatomical position. ‘Thou shalt not varus’- only time will tell.
1 Pinskerova V , MaquetP, FreemanMA. Writings on the knee between 1836 and 1917. J Bone Joint Surg [Br]2000;82-B:1100–1102.CrossrefPubMed Google Scholar
2 Zuppinger H . Die aktive Flexion im unbelasteten Kniegelenk. Anatomische Hefte1904;25:701–764. Google Scholar
3 Scott WN. Insall & Scott Surgery of the Knee. 4th Ed. Philidelphia: Churchill Livingstone, 2006. Google Scholar
4 Jackson JP , WaughW. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg [Br]1961;43-B:746–751. Google Scholar
5 Kettelkamp DB , WengerDR, ChaoEY, ThompsonC. Results of proximal tibial osteotomy. The effects of tibiofemoral angle, stance-phase flexion-extension, and medial-plateau force. J Bone Joint Surg [Am]1976;58-A:952–960.PubMed Google Scholar
6 De Marchin P , MaquetP, FontaineJ. Quelques remarques sur la radiographie des genoux arthrosiques, Utilité des clichés ‘en charge’. Rev. Méd. Liege1963;18:148. Google Scholar
7 Campbell WC . Interposition of vitallium plates in arthroplasties of the knee. Preliminary report. By Willis C. Campbell, 1940. Clin Orthop Relat Res1988;226:3–5.PubMed Google Scholar
8 Macintosh DL . Hemiarthroplasty of the knee using a space occupying prosthesis for painful varus and valgus deformities. In: Proceedings of the Joint Meeting of the Orthopaedic Associations of the English-Speaking World. J Bone Joint Surg [Am]1958;40-A:1428–1441. Google Scholar
9 Gunston FH . Polycentric knee arthroplasty: prosthetic simulation of normal knee movement. 1971. Clin Orthop Relat Res2006;446:11–12.CrossrefPubMed Google Scholar
10 Evanski PM , WaughTR, OrofinoCF, AnzelSH. UCI knee replacement. Clin Orthop Relat Res1976;120:33–38.PubMed Google Scholar
11 Jones WT , BryanRS, PetersonLF, IlstrupDM. Unicompartmental knee arthroplasty using polycentric and geometric hemicomponents. J Bone Joint Surg [Am]1981;63-A:946–954.PubMed Google Scholar
12 Lewallen DG , BryanRS, PetersonLF. Polycentric total knee arthroplasty. A ten-year follow-up study. J Bone Joint Surg [Am]1984;66-A:1211–1218.PubMed Google Scholar
13 Freeman MA , SwansonSA, ToddRC. Total replacement of the knee using the Freeman-Swanson knee prosthesis. Clin Orthop Relat Res1973;94:153–170.CrossrefPubMed Google Scholar
14 Saran N , RathjenKE. Guided growth for the correction of pediatric lower limb angular deformity. JAAOS2010;18:528–536.CrossrefPubMed Google Scholar
15 Lotke PA , EckerML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg [Am]1977;59-A:77–79.PubMed Google Scholar
16 Hood RW , VanniM, InsallJN. The correction of knee alignment in 225 consecutive total condylar knee replacements. Clin Orthop Relat Res1981;160:94–105.PubMed Google Scholar
17 Bargren JH , BlahaJD, FreemanMA. Alignment in total knee arthroplasty. Correlated biomechanical and clinical observations. Clin Orthop Relat Res1983;173:178–183.PubMed Google Scholar
18 Tew M , WaughW. Tibiofemoral alignment and the results of knee replacement. J Bone Joint Surg [Br]1985;67-B:551–556.CrossrefPubMed Google Scholar
19 Jeffery RS , MorrisRW, DenhamRA. Coronal alignment after total knee replacement. J Bone Joint Surg [Br]1991;73-B:709–714.CrossrefPubMed Google Scholar
20 Ritter MA , FarisPM, KeatingEM, MedingJB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res1994;299:153–156.PubMed Google Scholar
21 Issa SN , DunlopD, ChangA, et al.Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum2007;57:398–406.CrossrefPubMed Google Scholar
22 Kraus VB , VailTP, WorrellT, McDanielG. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum2005;52:1730–1735.CrossrefPubMed Google Scholar
23 Hinman RS , MayRL, CrossleyKM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis?Arthritis Rheum2006;55:306–313.CrossrefPubMed Google Scholar
24 Matsuda S , MiuraH, NagamineR, et al.Changes in knee alignment after total knee arthroplasty. J Arthroplasty1999;14:566–570.CrossrefPubMed Google Scholar
25 Collier MB , EnghCA, McAuleyJP, EnghGA. Factors associated with the loss of thickness of polyethylene tibial bearings after knee arthroplasty. J Bone Joint Surg [Am]2007;89-A:1306–1314.CrossrefPubMed Google Scholar
26 Green GV , BerendKR, BerendME, GlissonRR, VailTP. The effects of varus tibial alignment on proximal tibial surface strain in total knee arthroplasty: The posteromedial hot spot. J Arthroplasty2002;17:1033–1039.CrossrefPubMed Google Scholar
27 D'Lima DD , ChenPC, ColwellCW. Polyethylene contact stresses, articular congruity, and knee alignment. Clin Orthop Relat Res2001;392:232–238.CrossrefPubMed Google Scholar
28 D'Lima DD , HermidaJC, ChenPC, ColwellCW. Polyethylene wear and variations in knee kinematics. Clin Orthop Relat Res2001;392:124–130.CrossrefPubMed Google Scholar
29 Werner FW , AyersDC, MaletskyLP, RullkoetterPJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech2005;38:349–355.CrossrefPubMed Google Scholar
30 Emmerson KP , MoranCG, PinderIM. Survivorship analysis of the Kinematic Stabilizer total knee replacement: a 10- to 14-year follow-up. J Bone Joint Surg [Br]1996;78-B:441–445.PubMed Google Scholar
31 Colizza WA , InsallJN, ScuderiGR. The posterior stabilized total knee prosthesis. Assessment of polyethylene damage and osteolysis after a ten-year-minimum follow-up. J Bone Joint Surg [Am]1995;77-A:1713–1720.CrossrefPubMed Google Scholar
32 Baker PN , van der MeulenJH, LewseyJ, GreggPJ. The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg [Br]2007;89-B:893–900.CrossrefPubMed Google Scholar
33 McKellop HA , ShenFW, CampbellP, OtaT. Effect of molecular weight, calcium stearate, and sterilization methods on the wear of ultra high molecular weight polyethylene acetabular cups in a hip joint simulator. J Orthop Res1999;17:329–339.CrossrefPubMed Google Scholar
34 Muratoglu OK , BragdonCR, JastyM, et al.Knee-simulator testing of conventional and cross-linked polyethylene tibial inserts. J Arthroplasty2004;19:887–897.CrossrefPubMed Google Scholar
35 Brin YS , NikolaouVS, JosephL, ZukorDJ, AntoniouJ. Imageless computer assisted versus conventional total knee replacement. A Bayesian meta-analysis of 23 comparative studies. Int Orthop2011;35:331–339.CrossrefPubMed Google Scholar
36 Morgan SS , BonshahiA, PradhanN, et al.The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop2008;32:639–642.CrossrefPubMed Google Scholar
37 Fang DM , RitterMA, DavisKE. Coronal alignment in total knee arthroplasty: just how important is it?J Arthroplasty2009;24(6Suppl):39–43.CrossrefPubMed Google Scholar
38 Berend ME , RitterMA, MedingJB, et al.Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res2004;428:26–34.CrossrefPubMed Google Scholar
39 Parratte S , PagnanoMW, TrousdaleRT, BerryDJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg [Am]2010;92-A:2143–2149.CrossrefPubMed Google Scholar
40 Matziolis G , AdamJ, PerkaC. Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg2010;130:1487–1491.CrossrefPubMed Google Scholar
41 Bonner TJ , EardleyWG, PattersonP, GreggPJ. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg [Br]2011;93-B:1217–1222.CrossrefPubMed Google Scholar
42 No authors listed. National Joint Registry, 2013. http://www.njrcentre.org.uk (date last accessed 28 April 2014). Google Scholar
43 Spencer JM , ChauhanSK, SloanK, TaylorA, BeaverRJ. Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg [Br]2007;89-B:477–480.CrossrefPubMed Google Scholar
44 Bellemans J , ColynW, VandenneuckerH, VictorJ. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res2012;470:45–53.CrossrefPubMed Google Scholar
45 Eckhoff D , HoganC, DiMatteoL, RobinsonM, BachJ. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res2007;461:238–244.CrossrefPubMed Google Scholar
46 Eckhoff DG , BachJM, SpitzerVM, et al.Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg [Am]2005;87-A(Suppl 2):71–80.CrossrefPubMed Google Scholar









