Abstract
Aims
The primary aim of this study was to determine the rates of return to work (RTW) and sport (RTS) following a humeral shaft fracture. The secondary aim was to identify factors independently associated with failure to RTW or RTS.
Methods
From 2008 to 2017, all patients with a humeral diaphyseal fracture were retrospectively identified. Patient demographics and injury characteristics were recorded. Details of pre-injury employment, sporting participation, and levels of return post-injury were obtained via postal questionnaire. The University of California, Los Angeles (UCLA) Activity Scale was used to quantify physical activity among active patients. Regression was used to determine factors independently associated with failure to RTW or RTS.
Results
The Work Group comprised 177 patients in employment prior to injury (mean age 47 years (17 to 78); 51% female (n = 90)). Mean follow-up was 5.8 years (1.3 to 11). Overall, 85% (n = 151) returned to work at a mean of 14 weeks post-injury (0 to 104), but only 60% (n = 106) returned full-time to their previous employment. Proximal-third fractures (adjusted odds ratio (aOR) 4.0 (95% confidence interval (CI) 1.2 to 14.2); p = 0.029) were independently associated with failure to RTW. The Sport Group comprised 182 patients involved in sport prior to injury (mean age 52 years (18 to 85); 57% female (n = 104)). Mean follow-up was 5.4 years (1.3 to 11). The mean UCLA score reduced from 6.9 (95% CI 6.6 to 7.2) before injury to 6.1 (95% CI 5.8 to 6.4) post-injury (p < 0.001). There were 89% (n = 162) who returned to sport: 8% (n = 14) within three months, 34% (n = 62) within six months, and 70% (n = 127) within one year. Age ≥ 60 years was independently associated with failure to RTS (aOR 3.0 (95% CI 1.1 to 8.2); p = 0.036). No other factors were independently associated with failure to RTW or RTS.
Conclusion
Most patients successfully return to work and sport following a humeral shaft fracture, albeit at a lower level of physical activity. Patients aged ≥ 60 yrs and those with proximal-third diaphyseal fractures are at increased risk of failing to return to activity.
Cite this article: Bone Jt Open 2022;3(3):236–244.
Take home message
The majority of patients successfully return to work and sport following a humeral shaft fracture.
Patients with proximal-third diaphyseal fractures are at increased risk of failure to return to work, and older patients are at increased risk of failure to return to sport.
These findings will be useful for surgeons counselling patients about expected return to activity after a humeral shaft fracture.
Introduction
Humeral diaphyseal fractures comprise 1.2% of all adult fractures,1 with an annual incidence of around 12 per 100,000 population.2 Although nonoperative management using a functional brace remains the default strategy in many centres,3 there has been a recent increase in the number of patients managed operatively, partly driven by a desire to improve return to employment and sporting activity.4,5
However, there are few studies documenting the rates of return to work and/or sport following a humeral diaphyseal fracture. Most studies reporting on return to work only examine those managed nonoperatively6 or operatively,7-11 with those reporting return to sport focusing upon throwing athletes, manual labourers, or patients undergoing specific management such as external fixation.11-14 The authors are not aware of any studies exploring factors associated with failure to return to activity after a humeral shaft fracture, which may help manage patient expectations regarding their recovery.
The primary aim of this study was to determine the rates of return to work and sport following a humeral diaphyseal fracture. The secondary aim was to identify factors independently associated with failure to return to work or sport following a humeral diaphyseal fracture.
Methods
Study cohort
Patients were retrospectively identified from an established trauma database held at the study centre.2 All adult patients (aged ≥ 16 years) sustaining an acute fracture of the humeral diaphysis between January 2008 and December 2017 were identifed.15 Other fracture patterns, refractures, pathological fractures, periprosthetic fractures, and non-residents were excluded. All living, cognitively intact patients with available contact details and complete radiological follow-up (n = 504) were sent an activity questionnaire by post.16 Cognitive status was determined through review of the patient’s electronic medical record. Of the questionnaire respondents (n = 291), 177 (61%) were in employment prior to their injury (Work Group) and 182 (63%) were involved in sport (Sport Group); together these formed the study cohort. In total, 127 patients were included in both the Work Group and the Sport Group. This study was part of a larger audit of humeral shaft fractures managed in the study centre, was reviewed by the local NHS Research Ethics Service (NR/161AB6) and registered with the local musculoskeletal quality improvement committee.
Patient and injury characteristics
Patient demographic data, and medical and social background, were documented. Height and weight were used to calculate a BMI which was classified according to WHO guidelines.17 Social deprivation was assessed using the Scottish Index of Multiple Deprivation (SIMD)18 with patients assigned a deprivation score according to their postcode at the time of injury (Table I).
Table I.
Baseline patient and injury characteristics for patients in employment (Work Group) and involved in sport (Sport Group) prior to humeral diaphyseal fracture.
| Characteristic | Work Group (n = 177) |
Sport Group (n = 182) |
|---|---|---|
| Sex, n (%) | ||
| Male | 87 (49.2) | 78 (42.9) |
| Female | 90 (50.8) | 104 (57.1) |
| Mean age at injury, yrs (SD) | 47.0 (14.2) | 52.9 (16.8) |
| Comorbidities, n (%) | ||
| None | 84 (47.5) | 75 (41.2) |
| ≥ 1 | 93 (52.5) | 107 (58.8) |
| Smoking status, n (%) | ||
| No | 147 (83.1) | 160 (87.9) |
| Yes | 27 (15.3) | 16 (8.8) |
| Unknown | 3 (1.7) | 6 (3.3) |
| Alcohol excess, n (%) | ||
| No | 174 (98.3) | 179 (98.4) |
| Yes | 2 (1.1) | 2 (1.1) |
| Unknown | 1 (0.6) | 1 (0.5) |
| Mean BMI, kg/m 2 (SD) | 28.3 (7.2) | 28.1 (6.7) |
| Obesity classification, n (%) | ||
| Underweight | 3 (1.7) | 3 (1.6) |
| Normal | 38 (21.5) | 44 (24.2) |
| Overweight | 51 (28.8) | 55 (30.2) |
| Obese class I | 14 (7.9) | 20 (11.0) |
| Obese class II | 17 (9.6) | 12 (6.6) |
| Obese class III | 4 (2.3) | 6 (3.3) |
| Unknown | 50 (28.2) | 42 (23.1) |
| SIMD quintile, n (%) | ||
| 1 (most deprived) | 15 (8.5) | 15 (8.2) |
| 2 | 35 (19.8) | 33 (18.1) |
| 3 | 38 (21.5) | 34 (18.7) |
| 4 | 32 (18.1) | 34 (18.7) |
| 5 (least deprived) | 57 (32.2) | 66 (36.3) |
| Injury mechanism, n (%) | ||
| Fall from standing | 107 (60.5) | 113 (62.1) |
| Fall from height | 8 (4.5) | 10 (5.5) |
| Sport | 31 (17.5) | 32 (17.6) |
| Road traffic accident | 15 (8.5) | 13 (7.1) |
| Other | 13 (7.3) | 11 (6.0) |
| Unknown | 3 (1.7) | 3 (1.6) |
| Injury energy, n (%) | ||
| Low | 142 (80.2) | 147 (80.8) |
| High | 32 (18.1) | 32 (17.6) |
| Unknown | 3 (1.7) | 3 (1.6) |
| Side of injury, n (%) | ||
| Right | 85 (48.0) | 85 (46.7) |
| Left | 92 (52.0) | 97 (53.3) |
| Side of injury, n (%) | ||
| Dominant | 83 (46.9) | 89 (48.9) |
| Non-dominant | 93 (52.5) | 93 (51.1) |
| Unknown | 1 (0.6) | 0 |
| Fracture location, n (%) | ||
| Proximal | 44 (24.9) | 44 (24.2) |
| Middle | 85 (48.0) | 96 (52.7) |
| Distal | 48 (27.1) | 42 (23.1) |
| AO-OTA type, n (%) | ||
| A | 108 (61.0) | 116 (63.7) |
| B | 64 (36.2) | 63 (34.6) |
| C | 5 (2.8) | 3 (1.6) |
| AO-OTA group, n (%) | ||
| A1 | 59 (33.3) | 66 (36.3) |
| A2 | 10 (5.6) | 12 (6.6) |
| A3 | 39 (22.0) | 37 (20.3) |
| B2 | 55 (31.1) | 55 (30.2) |
| B3 | 9 (5.1) | 9 (4.9) |
| C2 | 3 (1.7) | 1 (0.5) |
| C3 | 2 (1.1) | 2 (1.1) |
| Open fracture, n (%) | ||
| No | 173 (97.7) | 179 (98.4) |
| Yes | 4 (2.3) | 3 (1.6) |
| Radial nerve palsy, n (%) | ||
| No | 169 (95.5) | 170 (93.4) |
| Yes | 8 (4.5) | 12 (6.6) |
| Associated injury, n (%)* | ||
| No | 140 (79.1) | 146 (80.2) |
| Yes | 35 (19.8) | 34 (18.7) |
| Unknown | 2 (1.1) | 2 (1.1) |
| Primary management, n (%) | ||
| Operative | 50 (28.2) | 46 (25.3) |
| Nonoperative | 127 (71.8) | 136 (74.7) |
-
*
Associated minor injuries included uncomplicated head injuries, simple soft-tissue injuries (contusions, lacerations, abrasions, incised wounds with no underlying structural injury) and ligament sprains; associated major injuries included other skeletal fractures or dislocations, soft-tissue injuries with underlying neurovascular or tendon damage, or any solid organ injury.
-
SD, standard deviation; SIMD, Scottish Index of Multiple Deprivation.
Mechanism of injury was recorded for all patients. All radiographs were assessed by a single author (WMO) using a picture archiving and communication system (Carestream Vue PACS; Carestream Health, USA). Fractures were classified by location within the humeral diaphysis and according to the AO-Orthopaedic Trauma Association (AO-OTA) classification.15 The presence of an open fracture, concomitant radial nerve palsy, and associated injuries was also documented.
Management and complications
Management for all patients was determined by consultant orthopaedic trauma surgeons (including SGM and TOW). Operative management for both groups comprised either open reduction and internal fixation (ORIF) or intramedullary (IM) nailing. Standard nonoperative management involved placement into a plaster of Paris ‘U-slab’ in the Emergency Department, which was replaced by a humeral brace following outpatient review. The exact timing of conversion to a humeral brace was at the discretion of the treating surgeon, but study centre protocol is that this usually occurs within the first two weeks following injury.
Details of any complications were obtained through review of medical records and radiographs. Union was considered to have occurred if patients reported reduced/absent pain at the fracture site, and there was bridging callus across all fracture cortices/obliteration of all cortical fracture lines on radiographs prior to clinic discharge.19,20 Nonunion was defined as a failure to unite within six months of nonoperative treatment,21,22 and/or where the treating surgeon considered that nonunion surgery was required beyond 12 weeks post-injury.23,24
Employment and sport
Pre- and post-injury employment and sporting participation were obtained via a postal questionnaire. For the Work Group (n = 177), patients were asked to describe the physical demands of their employment prior to their fracture (sedentary, light manual, moderate manual, heavy manual, other). Patients then indicated whether they had returned to work since their injury, and if so in what capacity (full-time to previous job, part-time to previous job, full-time to a different job, part-time to a different job) and how long it had taken (in weeks). If they had not returned to work, they were asked to describe their current circumstances (on sick leave, retired, on benefits, student, other).
For the Sport Group (n = 182), overall activity level was assessed quantitatively using the University of California Los Angeles (UCLA) Activity Scale.25 This is a ten-point score, in which patients record their level of activity between one (‘wholly inactive, dependent on others, and cannot leave residence’) and ten (‘regularly participates in impact sports’). Patients were asked to indicate which score best described their activity level before and after their fracture. The UCLA Activity Scale has been shown to be accurate and reliable in the assessment of activity following total joint replacement26,27 and extracapsular hip fracture fixation.28 Compared with other activity scores, the UCLA Activity Scale has also demonstrated better completion rates and discrimination between insufficiently and sufficiently active patients following total joint replacement.27 Patients were also asked to indicate their main sport before their fracture. Sports were classified into three broad domains by a single author (WMO): walking, non-contact sport (e.g. running, cycling, swimming, racquet sports, golf), and contact sport (e.g. football, rugby, basketball, martial arts). Finally, patients were asked to indicate whether they had returned to their main sport following their fracture and how long it had taken (less than three months, three to six months, six to 12 months, more than 12 months).
Statistical analysis
Statistical analysis was performed using SPSS v. 25.0 (IBM, USA). Odds ratios (ORs) were calculated for contingency tables. The statistical relationship between categorical variables was assessed using a chi-squared test or Fisher’s exact test (where the value of any cell was < 5). The relationship between two groups of continuous non-parametric data was assessed using the Mann-Whitney U test. The change in UCLA score from pre- to post-injury was assessed using the Wilcoxon signed-rank test. The age threshold most strongly associated with failure to return to sport was determined using a receiver operating characteristic curve. Variables found to be associated with failure return to work or sport on bivariate analysis (p < 0.05) were entered into binary logistic regression models, to determine factors independently associated with failure to return to work or sport. Significance was set at p < 0.05; 95% confidence intervals (CIs) and two-tailed p-values were reported.
Results
Work Group
The mean age of patients in the Work Group (n = 177) was 47 years (17 to 78) and 50.8% (n = 90) were female. Overall, 28.2% (n = 50) were managed operatively and 71.8% (n = 127) nonoperatively (Table I). ORIF was performed in 90% undergoing surgery (n = 45), with the remainder (n = 5; 10%) undergoing intramedullary (IM) nailing. Treatment-related complications were found in 19.2% of patients (n = 34) and nonunion occurred in 17.5% (n = 31; Table II). A total of 29 patients underwent nonunion surgery at a mean of 7.3 months (3.3 to 13.6). Nonunion surgery was successful in achieving union in all but two patients.
Table II.
Treatment-related complications and nonunion rate for patients in employment (Work Group) and involved in sport (Sport Group) prior to humeral diaphyseal fracture.
| Complication | Work Group (n = 177) |
Sport Group (n = 182) |
|---|---|---|
| Radial nerve palsy, n (%) | ||
| No | 176 (99.4) | 178 (97.8) |
| Yes | 1 (0.6) | 4 (2.2) |
| Other skin/wound complications, n (%) | ||
| No | 157 (88.7) | 162 (89.0) |
| Yes | 20 (11.3) | 20 (11.0) |
| Superficial infection, n (%) | ||
| No | 168 (94.9) | 171 (94.0) |
| Yes | 9 (5.1) | 11 (6.0) |
| Deep infection, n (%) | ||
| No | 176 (99.4) | 181 (99.5) |
| Yes | 1 (0.6) | 1 (0.5) |
| Failure of fixation, n (%) | ||
| No | 176 (99.4) | 182 (100) |
| Yes | 1 (0.6) | 0 |
| Shoulder capsulitis, n (%) | ||
| No | 169 (95.5) | 177 (97.3) |
| Yes | 8 (4.5) | 5 (2.7) |
| Nonunion, n (%) | ||
| No | 146 (82.5) | 150 (82.4) |
| Yes | 31 (17.5) | 32 (17.6) |
Return to work
Mean follow-up for patients in the Work Group was 5.8 years (1.3 to 11). Overall, 85.3% (n = 151) returned to work at a mean of 14 weeks post-injury (0 to 104). However, only 59.9% (n = 106) returned full-time to their previous employment, with the remainder returning either part-time (10.7%; n = 19) or changing to a different job (14.7%; n = 26; Figure 1).
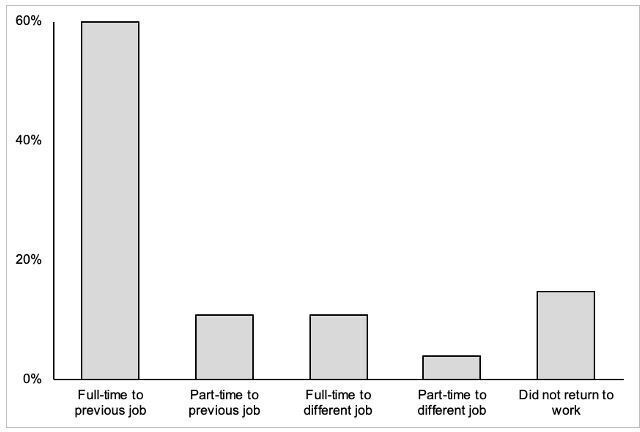
Fig. 1
Return to employment following a humeral diaphyseal fracture (n = 177).
Female sex (p = 0.042, chi-squared test), being in heavy manual work (reference sedentary work; OR 5.49 (95% CI 1.19 to 25.38; p = 0.031, Fisher’s exact test), sustaining a right-sided (p = 0.019, chi-squared test) or dominant-sided injury (p = 0.044, chi-squared test) or a proximal-third fracture (reference distal-third fracture; OR 4.61 (95% CI 1.37 to 15.49); p = 0.014, Fisher’s exact test) were associated with failure to return to work on unadjusted analysis. There was a non-significant trend between failing to achieve fracture union after initial management (either operative or nonoperative) and failure to return to work (p = 0.054, chi-squared test; Table III).
Table III.
Patient, injury, and management factors associated with failure to return to work on bivariate analysis (n = 177); all variables were analyzed, only data for selected variables (significant relationships, management, complications, union outcome) are shown.
| Factor | Returned to work (n = 151) | Did not return (n = 26) | OR (95% CI) | p-value |
|---|---|---|---|---|
| Sex, n (%) | 2.47 (1.01 to 6.02) | 0.042* | ||
| Male | 79 (52.3) | 8 (30.8) | ||
| Female | 72 (47.7) | 18 (69.2) | ||
| Pre-injury work type, n (%) | 0.004* | |||
| Sedentary | 56 (37.1) | 3 (11.5) | ||
| Light manual | 31 (20.5) | 3 (11.5) | ||
| Moderate manual | 36 (23.8) | 8 (30.8) | ||
| Heavy manual | 17 (11.3) | 5 (19.2) | ||
| Other | 11 (7.3) | 7 (26.9) | ||
| Side of injury, n (%) | 2.82 (1.16 to 6.89) | 0.019* | ||
| Left | 84 (55.6) | 8 (30.8) | ||
| Right | 67 (44.4) | 18 (69.2) | ||
| Side of injury, n (%) | 2.40 (1.01 to 5.74) | 0.044* | ||
| Non-dominant | 84 (55.6) | 9 (34.6) | ||
| Dominant | 66 (43.7) | 17 (65.4) | ||
| Unknown | 1 (0.7) | 0 | ||
| Fracture location, n (%) | 0.005* | |||
| Proximal | 31 (20.5) | 13 (50.0) | ||
| Middle | 76 (50.3) | 9 (34.6) | ||
| Distal (reference) | 44 (29.1) | 4 (15.4) | ||
| Primary management, n (%) | 2.41 (0.79 to 7.39) | 0.157† | ||
| Operative | 46 (30.5) | 4 (15.4) | ||
| Nonoperative | 105 (69.5) | 22 (84.6) | ||
| Treatment complications, n (%) | 0.73 (0.24 to 2.29) | 0.789† | ||
| No | 121 (80.1) | 22 (84.6) | ||
| Yes | 30 (19.9) | 4 (15.4) | ||
| Initial union outcome, n (%) | 2.47 (0.96 to 6.36) | 0.054* | ||
| Union | 128 (84.8) | 18 (69.2) | ||
| Nonunion | 23 (15.2) | 8 (30.8) | ||
| Underwent nonunion surgery, n (%) | 2.16 (0.81 to 5.74) | 0.116* | ||
| No | 129 (85.4) | 19 (73.1) | ||
| Yes | 22 (14.6) | 7 (26.9) | ||
| Final union outcome, n (%) | 6.21 (0.84 to 46.2) | 0.103† | ||
| Union | 149 (98.7) | 24 (92.3) | ||
| Nonunion | 2 (1.3) | 2 (7.7) |
-
*
Chi-squared test.
-
†
Fisher's exact test.
-
CI, confidence interval; OR, odds ratio.
Sustaining a proximal-third fracture was the only factor independently associated with failure to return to work on regression modelling (adjusted OR (aOR) 4.03 (95% CI 1.15 to 14.16; p = 0.029)).
Sport Group
The mean age of patients in the Sport Group (n = 182) was 52 years (18 to 85) and 57.1% (n = 104) were female. Overall, 25.3% (n = 46) were managed operatively and 74.7% (n = 136) were managed nonoperatively (Table I). ORIF was performed in 91% undergoing surgery (n = 42), with the remainder (n = 4; 9%) undergoing IM nailing. Treatment-related complications were found in 18.7% of patients (n = 34) and nonunion occurred in 17.6% (n = 32; Table II). A total of 30 patients in the Sport Group underwent nonunion surgery at a mean of 7.7 months (3.3 to 19.4). Nonunion surgery was successful in achieving union in all but one patient.
Return to sport
Mean follow-up for patients in the Sport Group was 5.4 years (1.3 to 11). The mean UCLA score prior to humeral diaphyseal fracture was 6.9 (95% CI 6.6 to 7.2) and the mean score after injury was 6.1 (95% CI 5.8 to 6.4; Figure 2). This difference was statistically significant (p < 0.001, Wilcoxon signed-rank test).
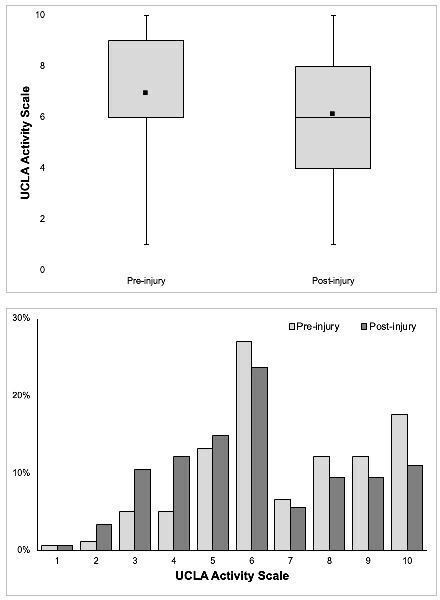
Fig. 2
Pre- and post-injury activity level for patients with a humeral diaphyseal fracture, according to the University of California, Los Angeles (UCLA) Activity Scale (n = 182).
Overall, 89.0% (n = 162) returned to sport following their fracture. Of those who returned to sport, 8.6% (n = 14) did so within three months, 38.2% (n = 62) within six months, 78.4% (n = 127) within 12 months, and 21.6% (n = 35) beyond 12 months. The patients who returned to sport did so at a lower level of participation (mean pre-injury UCLA score 7.0 (95% CI 6.7 to 7.3); mean post-injury UCLA score 6.3 (95% CI 6.0 to 6.6)). Patients managed nonoperatively returned to sport sooner than those managed operatively (p < 0.001, Mann-Whitney U test), despite no significant difference in the type of pre-injury sport between the groups (Table IV). Overall, 11% of patients (n = 20) did not return to sport after their fracture (Figure 3).
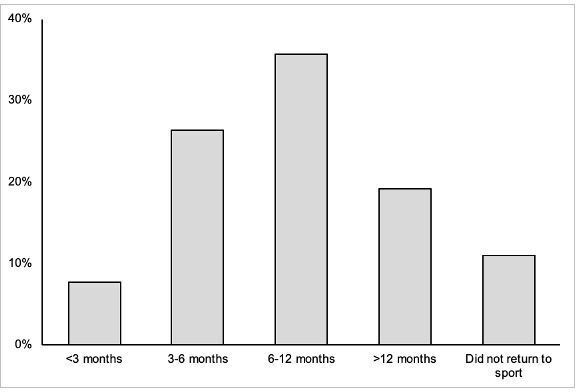
Fig. 3
Time of return to sport following a humeral diaphyseal fracture (n = 182).
Table IV.
Comparison of return to activity by initial humeral diaphyseal fracture management.
| Factor | Operative | Nonoperative | OR (95% CI) | p-value |
|---|---|---|---|---|
| Pre-injury employment, n (%) | 0.799* | |||
| Sedentary | 20 (40) | 39 (30.7) | ||
| Light manual | 9 (18) | 25 (19.7) | ||
| Moderate manual | 10 (20) | 34 (26.8) | ||
| Heavy manual | 6 (12) | 16 (12.6) | ||
| Other | 5 (10) | 13 (10.2) | ||
| Return to work, n (%) | 2.41 (0.79 to 7.39) | 0.157† | ||
| Yes | 46 (92) | 105 (82.7) | ||
| No | 4 (8) | 22 (17.3) | ||
| Mean time of return to work, wks (SD) | 13.4 (10.3) | 14.3 (15.6) | 0.659‡ | |
| Return to work category, n (%) | 0.643* | |||
| Full-time to same job | 32 (70) | 74 (70.5) | ||
| Part-time to same job | 4 (9) | 15 (14.3) | ||
| Full-time to different job | 7 (15) | 12 (11.4) | ||
| Part-time to different job | 3 (6) | 4 (3.8) | ||
| Mean change in UCLA Activity Scale (SD) | -0.76 (2.05) | -0.85 (1.61) | 0.825‡ | |
| Pre-injury sport, n (%) | 0.294* | |||
| Walking | 10 (22) | 39 (28.7) | ||
| Non-contact | 28 (61) | 84 (61.8) | ||
| Contact | 8 (17) | 13 (9.6) | ||
| Return to sport, n (%) | 1.02 (0.35 to 2.97) | 0.976* | ||
| Yes | 41 (89) | 121 (89.0) | ||
| No | 5 (11) | 15 (11.0) | ||
| Time of return to sport, n (%) | < 0.001‡ | |||
| < 3 mths | 2 (5) | 12 (9.9) | ||
| 3 to 6 mths | 6 (15) | 42 (34.7) | ||
| 6 to 12 mths | 16 (39) | 49 (40.5) | ||
| > 12 mths | 17 (42) | 18 (14.9) |
-
*
Chi-squared test.
-
†
Fisher's exact test.
-
‡
Mann-Whitney U test.
-
CI, confidence interval; OR, odds ratio; SD, standard deviation; UCLA, University of California, Los Angeles.
Older age at injury was associated with failure to return to sport (p = 0.016, Mann-Whitney U test) on unadjusted analysis, and receiver operating characteristic curve modelling determined that patients aged ≥ 60 years were at increased risk of this outcome (sensitivity 65%, specificity 66%; Figure 4). Having medical comorbidities (p = 0.015, Fisher’s exact test), being unemployed or retired (p = 0.002, chi-squared test), sustaining a radial nerve palsy (p = 0.030, Fisher’s exact test), and failing to ultimately achieve union (p = 0.032, Fisher’s exact test) were also associated with failure to return to sport on unadjusted analysis (Table V).
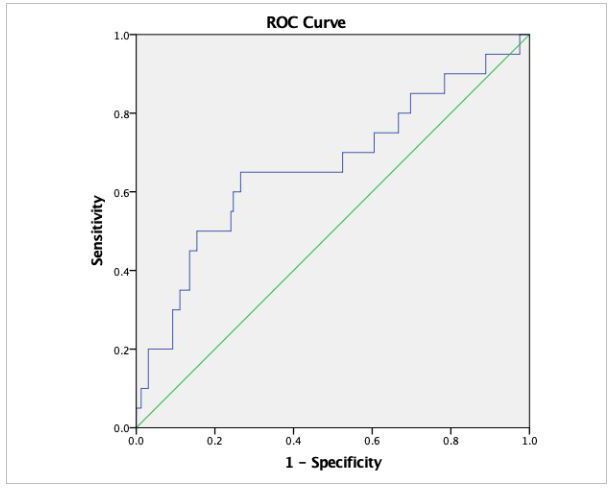
Fig. 4
Receiver operating characteristic (ROC) curve for the relationship between patient age at humeral diaphyseal fracture and return to sport; area under curve 0.665 (95% confidence interval 0.523 to 0.808); p = 0.016.
Table V.
Patient, injury, and management factors associated with failure to return to sport on bivariate analysis (n = 182); all variables were analyzed; only data for selected variables (significant relationships, management, complications, union outcome) are shown.
| Factor | Returned to sport (n = 162) |
Did not return (n = 20) |
OR (95% CI) | p-value |
|---|---|---|---|---|
| Mean age at injury, yrs (SD) | 52.0 (16.4) | 60.9 (18.3) | 0.016* | |
| Comorbidities, n (%) | 4.53 (1.28 to 16.1) | 0.015† | ||
| None | 72 (44.4) | 3 (15.0) | ||
| ≥ 1 | 90 (55.6) | 17 (85.0) | ||
| Pre-injury employment status, n (%) | 4.15 (1.59 to 10.8) | 0.002‡ | ||
| Employed | 119 (73.5) | 8 (40.0) | ||
| Unemployed/retired | 43 (26.5) | 12 (60.0) | ||
| Radial nerve palsy, n (%) | 4.81 (1.30 to 17.8) | 0.030† | ||
| No | 154 (95.1) | 16 (80.0) | ||
| Yes | 8 (4.9) | 4 (20.0) | ||
| Primary management, n (%) | 1.02 (0.35 to 2.97) | 0.976‡ | ||
| Operative | 41 (25.3) | 5 (25.0) | ||
| Nonoperative | 121 (74.7) | 15 (75.0) | ||
| Treatment complications, n (%) | 0.21 (0.03 to 1.59) | 0.130† | ||
| No | 129 (79.6) | 19 (95.0) | ||
| Yes | 33 (20.4) | 1 (5.0) | ||
| Initial union outcome, n (%) | 1.67 (0.56 to 4.97) | 0.356‡ | ||
| Union | 135 (83.3) | 15 (75.0) | ||
| Nonunion | 27 (16.7) | 5 (25.0) | ||
| Underwent nonunion surgery, n (%) | 1.31 (0.41 to 4.23) | 0.748† | ||
| No | 136 (84.0) | 16 (80.0) | ||
| Yes | 26 (16.0) | 4 (20.0) | ||
| Final union outcome, n (%) | 17.9 (1.55 to 207) | 0.032† | ||
| Union | 161 (99.4) | 18 (90.0) | ||
| Nonunion | 1 (0.6) | 2 (10.0) |
-
*
Mann-Whitney U test.
-
†
Fisher's exact test.
-
‡
Chi-squared test.
-
CI, confidence interval; OR, odds ratio; SD, standard deviation.
There was a positive correlation between the presence of comorbidities and patient age, and a strongly positive correlation between pre-injury employment status and patient age. As medical comorbidities and unemployment/retirement are inherently dependent upon patient age, these were omitted from the regression model. With patient age, radial nerve palsy, and union outcome entered into the regression model, only age ≥ 60 years was independently associated with failure to return to sport (aOR 2.97 (95% CI 1.08 to 8.18); p = 0.036).
Discussion
This study provides important prognostic data on return to work and sport for a cohort of unselected adult patients with a humeral diaphyseal fracture. Most patients (85%) returned to work at just over three months post-injury on average, but only 60% returned on a full-time basis to their previous employment. A majority of patients (89%) successfully returned to sport, over three-quarters doing so within a year of injury. Specific patient and injury factors were associated with failure to return to work and sport. These findings offer important data to surgeons counselling patients regarding return to activity following a humeral shaft fracture.
The rate and timing of return to work for patients in our study is in keeping with previous literature that reports rates of between 79% and 94%8,11,29-31 at typically between nine and 18 weeks post-injury.7,9,10,32,33 It is notable that in our study we found that only 60% of patients returned full-time to their previous employment, with no other literature examining the circumstances in which patients returned to work following a humeral diaphyseal fracture. Our data did not demonstrate any difference between patients managed operatively and nonoperatively in terms of return to work, time of return to work, or employment circumstances. These findings are consistent with other comparative studies that have failed to demonstrate the benefit of primary operative management in facilitating return to work after a humeral shaft fracture.29-31,33,34
We identified that sustaining a proximal-third diaphyseal fracture was independently associated with failure to return to work. We are not aware of any existing studies exploring risk factors for failure to return to work after a humeral shaft fracture. Proximal-third fractures are increasingly considered as fragility fractures,2 and have been linked with poorer functional outcome,35,36 but this is the first study to identify an independent relationship between proximal fracture location and failure to return to work. Measuring the socioeconomic outcome of orthopaedic trauma is complex and multifaceted,37 with many factors (including patient age, psychological profile, smoking status, education level, income, injury severity, involvement in compensation proceedings, self-efficacy, and social support network) all proven to influence return to work.38 Interestingly, we also observed a non-significant association between failure to achieve union after initial management and failure to return to work. This may be a product of the suggested link between proximal-third fractures and humeral shaft nonunion,35,39-41 and highlights the importance of achieving union with initial management (whether operative or nonoperative).
There are very few studies specifically reporting on the rate and timing of return to sport after a humeral diaphyseal fracture. Smaller studies involving recreational baseball players,12 manual labourers and overhead athletes,11 or survey responses from experienced upper limb surgeons13 document excellent rates of return to sport (92% to 100%) at between two and five months post-injury. However, these studies involve highly selected patient cohorts with short-term follow-up, and many of these patients were managed surgically. Our results provide novel data that are more generalizable to a typical humeral shaft fracture population in circumstances where initial nonoperative management is commonly used. This will be of use to surgeons managing expectations among active adult patients with these injuries.
We found that patients aged over 60 years at the time of injury were at an increased risk of failing to return to their pre-injury sport. A recent study of modern humeral shaft fracture epidemiology indicated a gradual increase in age at which these injuries are sustained,2 and our findings are likely to be of particular importance to this older but nonetheless physically active population. Interestingly, although others have indicated that operative fixation results in more rapid return to sporting activity,13,30 our results did not support this observation. Indeed, patients managed nonoperatively in the present study reported returning to sport earlier than those managed operatively, regardless of the type of activity in which they were involved. The reasons for this may reflect patient perceptions of injury severity, or a feeling they should protect their operated limb following fixation. In any event, we did not find operative management to be advantageous in improving the success or timing of return to sport after a humeral diaphyseal fracture.
To our knowledge, this is the first study reporting the effect of humeral diaphyseal fractures upon overall physical activity. Five years on from their injury, we observed a general reduction in activity as measured by the UCLA Activity Scale, from a mean score of 6.9 to 6.1. Although a formal minimally important clinical difference has not been reported for this score, UCLA scores of six or more have been found to reflect being ‘sufficiently active’ according to the International Physical Activity Questionnaire.27,42 We interpret this finding to indicate that, for the majority of patients, overall activity level is not significantly impaired following a humeral shaft fracture in the longer-term.
The principal limitation of this study is the retrospective design. Patients were asked to recall details of their preoperative activity and employment at the point of longer-term follow-up and we acknowledge it would have been preferable to obtain these data contemporaneously. It was not possible to qualitatively assess reasons why individual patients did not return to their pre-injury work or sport, and we acknowledge their humeral shaft fracture may not have been the only contributory factor in some cases. Although this is the largest study assessing return to activity following a humeral diaphyseal fracture, a larger cohort may have strengthened our ability to identify risk factors for failure to return to work or sport.
References
1. Court-Brown CM , Caesar B . Epidemiology of adult fractures: a review. Injury . 2006 ; 37 ( 8 ): 691 – 697 . Crossref PubMed Google Scholar
2. Oliver WM , Searle HKC , ZH N , Wickramasinghe NRL , Molyneux SG , White TO . Fractures of the proximal- and middle-thirds of the humeral shaft should be considered as fragility fractures: an epidemiological study of 900 consecutive injuries . Bone Joint J . 2020 ; 102-B ( 11 ): 1475 – 1483 . Google Scholar
3. Sarmiento A , Kinman PB , Galvin EG , Schmitt RH , Phillips JG . Functional bracing of fractures of the shaft of the humerus . J Bone Joint Surg Am . 1977 ; 59-A ( 5 ): 596 – 601 . Crossref PubMed Google Scholar
4. Huttunen TT , Kannus P , Lepola V , Pihlajamäki H , Mattila VM . Surgical treatment of humeral-shaft fractures: a register-based study in Finland between 1987 and 2009 . Injury . 2012 ; 43 ( 10 ): 1704 – 1708 . Crossref PubMed Google Scholar
5. Schoch BS , Padegimas EM , Maltenfort M , Krieg J , Namdari S . Humeral shaft fractures: national trends in management . J Orthop Traumatol . 2017 ; 18 ( 3 ): 259 – 263 . Crossref PubMed Google Scholar
6. Rosenberg N , Soudry M . Shoulder impairment following treatment of diaphysial fractures of humerus by functional brace . Arch Orthop Trauma Surg . 2006 ; 126 ( 7 ): 437 – 440 . Crossref PubMed Google Scholar
7. Lorich DG , Geller DS , Yacoubian SV , Leo AJ , Helfet DL . Intramedullary fixation of humeral shaft fractures using an inflatable nail . Orthopedics . 2003 ; 26 ( 10 ): 1011 – 1014 . Crossref PubMed Google Scholar
8. Changulani M , Jain UK , Keswani T . Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. A randomised controlled study . Int Orthop . 2007 ; 31 ( 3 ): 391 – 395 . Crossref PubMed Google Scholar
9. Lee TJ , Kwon DG , Na SI , Cha SD . Modified combined approach for distal humerus shaft fracture: anterolateral and lateral bimodal approach . Clin Orthop Surg . 2013 ; 5 ( 3 ): 209 – 215 . Crossref PubMed Google Scholar
10. Kim SJ , Lee SH , Son H , Lee BG . Surgical result of plate osteosynthesis using a locking plate system through an anterior humeral approach for distal shaft fracture of the humerus that occurred during a throwing motion . Int Orthop . 2016 ; 40 ( 7 ): 1489 – 1494 . Crossref PubMed Google Scholar
11. Mahajan AS , Kim YG , Kim JH , D’sa P , Lakhani A , Ok HS . Is anterior bridge plating for mid-shaft humeral fractures a suitable option for patients predominantly involved in overhead activities? A functional outcome study in athletes and manual laborers . Clin Orthop Surg . 2016 ; 8 ( 4 ): 358 – 366 . Crossref PubMed Google Scholar
12. Ogawa K , Yoshida A . Throwing fracture of the humeral shaft. An analysis of 90 patients . Am J Sports Med . 1998 ; 26 ( 2 ): 242 – 246 . Crossref PubMed Google Scholar
13. Altintas B , Anderson NL , Boykin R , Millett PJ . Operative treatment of torsional humeral shaft fractures in throwers leads to an earlier return to sport: a survey of expert shoulder and elbow surgeons . Knee Surg Sports Traumatol Arthrosc . 2019 ; 27 ( 12 ): 4049 – 4054 . Crossref PubMed Google Scholar
14. Costa GG , Aloj DC , Cerbasi S , et al. External fixation as a definitive treatment for humeral shaft fractures: radiographic and functional results with analysis of outcome predictors . J Orthop Trauma . 2019 ; 33 ( 7 ): 354 – 360 . Crossref PubMed Google Scholar
15. Meinberg EG , Agel J , Roberts CS , Karam MD , Kellam JF . Fracture and Dislocation Classification Compendium-2018 . J Orthop Trauma . 2018 ; 32 Suppl 1 ( Suppl 1 ): S1 – S170 . Crossref PubMed Google Scholar
16. Oliver WM , Searle HKC , Molyneux SG , White TO , Clement ND , Duckworth AD . Factors associated with patient-reported outcomes following a humeral shaft fracture: nonunion results in a poorer outcome despite union after surgical fixation . J Orthop Trauma . 2022 . Crossref PubMed Google Scholar
17. No authors listed . Body Mass Index - BMI. World Health Organisation . http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi ( date last accessed 22 August 2019 ). Google Scholar
18. No authors listed . Scottish Index of Multiple Deprivation: SIMD16 Technical Notes . Scottish Government . https://www.webarchive.org.uk/wayback/archive/3000/https://www.gov.scot/Resource/0050/00504822.pdf ( date last accessed 16 February 2022 ). Google Scholar
19. Morshed S , Corrales L , Genant H , Miclau T . Outcome assessment in clinical trials of fracture-healing . J Bone Joint Surg Am . 2008 ; 90-A ( Suppl 1 ): 62 – 67 . Crossref PubMed Google Scholar
20. Wiss DA , Garlich JM . Healing the index humeral shaft nonunion: risk factors for development of a recalcitrant nonunion in 125 patients . J Bone Joint Surg Am . 2020 ; 102-A ( 5 ): 375 – 380 . Crossref PubMed Google Scholar
21. Jawa A , McCarty P , Doornberg J , Harris M , Ring D . Extra-articular distal-third diaphyseal fractures of the humerus. A comparison of functional bracing and plate fixation . J Bone Joint Surg Am . 2006 ; 88-A ( 11 ): 2343 – 2347 . Crossref PubMed Google Scholar
22. Matsunaga FT , Tamaoki MJS , Matsumoto MH , Netto NA , Faloppa F , Belloti JC . Minimally invasive osteosynthesis with a bridge plate versus a functional brace for humeral shaft fractures: a randomized controlled trial . J Bone Joint Surg Am . 2017 ; 99-A ( 7 ): 583 – 592 . Crossref PubMed Google Scholar
23. Ali E , Griffiths D , Obi N , Tytherleigh-Strong G , Van Rensburg L . Nonoperative treatment of humeral shaft fractures revisited . J Shoulder Elbow Surg . 2015 ; 24 ( 2 ): 210 – 214 . Crossref PubMed Google Scholar
24. Rämö L , Sumrein BO , Lepola V , et al. Effect of surgery vs functional bracing on functional outcome among patients with closed displaced humeral shaft fractures: the FISH randomized clinical trial. JAMA . 2020 ; 323 ( 18 ): 1792 – 1801 . Crossref PubMed Google Scholar
25. Amstutz HC , Thomas BJ , Jinnah R , Kim W , Grogan T , Yale C . Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty . J Bone Joint Surg Am . 1984 ; 66-A ( 2 ): 228 – 241 . Crossref PubMed Google Scholar
26. Zahiri CA , Schmalzried TP , Szuszczewicz ES , Amstutz HC . Assessing activity in joint replacement patients . J Arthroplasty . 1998 ; 13 ( 8 ): 890 – 895 . Crossref PubMed Google Scholar
27. Naal FD , Impellizzeri FM , Leunig M . Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res . 2009 ; 467 ( 4 ): 958 – 965 . Crossref PubMed Google Scholar
28. Ramoutar DN , Kodumuri P , Rodrigues JN , et al. The epidemiology and functional outcomes of operative fixation of extracapsular proximal femoral fractures (AO 31-A) in young adults . Eur J Orthop Surg Traumatol . 2017 ; 27 ( 2 ): 267 – 272 . Crossref PubMed Google Scholar
29. Denard A , Richards JE , Obremskey WT , Tucker MC , Floyd M , Herzog GA . Outcome of nonoperative vs operative treatment of humeral shaft fractures: a retrospective study of 213 patients . Orthopedics . 2010 ; 33 ( 8 ). Crossref PubMed Google Scholar
30. van Middendorp JJ , Kazacsay F , Lichtenhahn P , Renner N , Babst R , Melcher G . Outcomes following operative and non-operative management of humeral midshaft fractures: a prospective, observational cohort study of 47 patients . Eur J Trauma Emerg Surg . 2011 ; 37 ( 3 ): 287 – 296 . Crossref PubMed Google Scholar
31. Fırat A , Deveci A , Güler F , Oçgüder A , Oğuz T , Bozkurt M . Evaluation of shoulder and elbow functions after treatment of humeral shaft fractures: a 20-132-month follow-up study . Acta Orthop Traumatol Turc . 2012 ; 46 ( 4 ): 229 – 236 . Crossref PubMed Google Scholar
32. Koch PP , Gross DFL , Gerber C . The results of functional (Sarmiento) bracing of humeral shaft fractures . J Shoulder Elbow Surg . 2002 ; 11 ( 2 ): 143 – 150 . Crossref PubMed Google Scholar
33. Ristić V , Maljanović M , Arsić M , Matijević R , Milankov M . Comparison of the results of treatment of humeral shaft fractures by different methods . Med Pregl . 2011 ; 64 ( 9-10 ): 490 – 496 . Crossref PubMed Google Scholar
34. Hendy BA , Zmistowski B , Wells Z , Abboud JA , Namdari S . Humeral shaft fractures: surgical versus nonsurgical management in workers’ compensation . Arch Bone Jt Surg . 2020 ; 8 ( 6 ): 668 – 674 . Crossref Google Scholar
35. Broadbent MR , Will E , McQueen MM . Prediction of outcome after humeral diaphyseal fracture . Injury . 2010 ; 41 ( 6 ): 572 – 577 . Crossref PubMed Google Scholar
36. Shields E , Sundem L , Childs S , et al. Factors predicting patient-reported functional outcome scores after humeral shaft fractures . Injury . 2015 ; 46 ( 4 ): 693 – 698 . Crossref PubMed Google Scholar
37. O’Hara NN , Isaac M , Slobogean GP , Klazinga NS , O’Hara NN , Farouk O . The socioeconomic impact of orthopaedic trauma: a systematic review and meta-analysis. PLoS One . 2020 ; 15 ( 1 ): e0227907 . Crossref PubMed Google Scholar
38. Clay FJ , Newstead SV , McClure RJ . A systematic review of early prognostic factors for return to work following acute orthopaedic trauma . Injury . 2010 ; 41 ( 8 ): 787 – 803 . Crossref PubMed Google Scholar
39. Rutgers M , Ring D . Treatment of diaphyseal fractures of the humerus using a functional brace . J Orthop Trauma . 2006 ; 20 ( 9 ): 597 – 601 . Crossref PubMed Google Scholar
40. Ring D , Chin K , Taghinia AH , Jupiter JB . Nonunion after functional brace treatment of diaphyseal humerus fractures . J Trauma . 2007 ; 62 ( 5 ): 1157 – 1158 . Crossref PubMed Google Scholar
41. Serrano R , Mir HR , Sagi HC , et al. Modern results of functional bracing of humeral shaft fractures: a multicenter retrospective analysis . J Orthop Trauma . 2020 ; 34 ( 4 ): 206 – 209 . Crossref PubMed Google Scholar
42. Craig CL , Marshall AL , Sjöström M , et al. International physical activity questionnaire: 12-country reliability and validity . Med Sci Sports Exerc . 2003 ; 35 ( 8 ): 1381 – 1395 . Crossref PubMed Google Scholar
Author contributions
W. M. Oliver: Conceptualization, Project administration, Methodology, Investigation, Data curation, Formal analysis, Writing – original draft, Writing – review & editing.
S. G. Molyneux: Supervision, Investigation, Writing – review & editing.
T. O. White: Supervision, Investigation, Writing – review & editing.
N. D. Clement: Conceptualization, Methodology, Supervision, Investigation, Formal analysis, Writing – review & editing.
A. D. Duckworth: Conceptualization, Methodology, Supervision, Investigation, Formal analysis, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Acknowledgements
The authors would like to thank Deborah Ketchen, Deborah MacDonald, Henry Searle and Keri Swain for their invaluable assistance in administering postal surveys. The authors would also like to acknowledge the Scottish Orthopaedic Research Trust into Trauma (SORT-iT).
Ethical review statement
This study underwent NHS Research Ethics Service assessment (NR/161AB6) and was registered with the local musculoskeletal quality improvement committee.
Open access funding
Orthopaedic Trauma Endowment Fund, Royal Infirmary of Edinburgh.
Follow W. M. Oliver @OrthoOliver
Follow S. G. Molyneux @sgmolyneux
Follow A. D. Duckworth @DuckworthOrthEd
Follow Edinburgh Orthopaedics @EdinOrthopaedic
Follow Usher Institute, University of Edinburgh @EdinUniUsher
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/









