Abstract
Aims
Return to sport following undergoing total (TKA) and unicompartmental knee arthroplasty (UKA) has been researched with meta-analyses and systematic reviews of varying quality. The aim of this study is to create an umbrella review to consolidate the data into consensus guidelines for returning to sports following TKA and UKA.
Methods
Systematic reviews and meta-analyses written between 2010 and 2020 were systematically searched. Studies were independently screened by two reviewers and methodology quality was assessed. Variables for analysis included objective classification of which sports are safe to participate in postoperatively, time to return to sport, prognostic indicators of returning, and reasons patients do not.
Results
A total of 410 articles were found, including 58 duplicates. Seven articles meeting inclusion criteria reported that 34% to 100% of patients who underwent TKA or UKA were able to return to sports at 13 weeks and 12 weeks respectively, with UKA patients more likely to do so. Prior experience with the sport was the most significant prognostic indicator for return. These patients were likely to participate in low-impact sports, particularly walking, cycling, golf, and swimming. Moderate-impact sport participation, such as doubles tennis and skiing, may be considered on a case-by-case basis considering the patient’s prior experience. There is insufficient long-term data on the risks to return to high-impact sport, such as decreased implant survivorship.
Conclusion
There is a consensus that patients can return to low-impact sports following TKA or UKA. Return to moderate-impact sport was dependent on a case-by-case basis, with emphasis on the patient’s prior experience in the sport. Return to high-impact sports was not supported. Patients undergoing UKA return to sport one week sooner and with more success than TKA. Future studies are needed to assess long-term outcomes following return to high-impact sports to establish evidence-based recommendations. This review summarizes all available data for the most up-to-date and evidence-based guidelines for returning to sport following TKA and UKA to replace guidelines based on subjective physician survey data.
Cite this article: Bone Jt Open 2022;3(3):245–251.
Take home message
This review summarizes all available data for the most up-to-date and evidence-based guidelines for returning to sport following total knee arthroplasty and unicompartmental knee arthroplasty.
Patients may return to low-impact sports. They may return to moderate-impact sports if they have prior experience with the sport. There is insufficient evidence for return to high-impact sport.
Positive prognostic indicators include younger age, lower BMI, male sex, and no other joint pain, and patients did not return to sport mostly due to surgeon recommendation.
Introduction
Patients with knee osteoarthritis (OA) are often progressively limited in their function, and are unable to continue sport and recreational activities. Total (TKA) and unicompartmental (UKA) knee arthroplasty are safe and effective treatments for OA. As these procedures are increasing in frequency,1,2 and performed in younger populations,2 physicians are commonly asked what the expectations are for returning to sport (RTS) following a TKA or UKA. It is important to note that UKAs have shorter operating times, hospital stays, and recovery times compared to TKAs,3 which may bear relevance on their ability to and timing of RTS.
Current recommendations for RTS, including those from The American Association of Hip and Knee Surgeons (AAHKS)4 and The Knee Society,5 are largely based on physician preference and survey data, as well as loosely defined categories of low-impact, moderate-impact, and high-impact sports. Outside of surveys, Vail et al6 classified sport impact level and provided post-arthroplasty recommendations based on degree of repetition, magnitude of joint loading, and potential for violence. Their classification of sport impact level has been widely used in studies published in the last 20 years investigating return to sport. Additional published data on outcomes and sports participation after arthroplasty have been previously analyzed with systematic reviews and meta-analyses, however these are of varying quality.
Given these accumulated data on sport participation following TKA and UKA, it is now possible to move towards replacing subjective survey recommendations with evidence-based guidelines. An umbrella review consolidating systematic reviews and meta-analyses on RTS following TKA and UKA has not been published to date. A similar umbrella review successfully consolidated hip arthroplasty data into consensus guidelines regarding returning to sport.7 The purpose of this umbrella review is to provide the most evidence-based guidelines for when patients can RTS and which sports that patients can return to following TKA and UKA.
Methods
This study followed the Joanna Briggs Institute (JBI) methodology on conducting an umbrella review;8 the systematic reviews and meta-analyses examined were published between 1 January 2010 and 15 March 2020.
Search strategy
A systematic search was conducted for published systematic reviews and meta-analyses on RTS following TKA and/or UKA in the Medline, Embase, and Cochrane databases on 15 March 2020. The search used a combination of keywords and controlled vocabulary for the concepts: RTS, TKA, and UKA.
Screening and inclusion/exclusion criteria
Two authors (DL, CB) independently screened articles for inclusion. Articles published prior to 2010, duplicates, and articles not written in English were excluded. Studies were reviewed first by abstract and title, followed by the full text. Articles were included if they described RTS following TKA, UKA, or both, and were true systematic reviews or meta-analyses. Articles were excluded if they did not provide data on primary or secondary outcomes.
Data extraction and methodological assessment
The primary outcome was determination of sports that patients are able to participate in post-TKA or post-UKA. Secondary outcomes included percentage of patients who RTS, differences between RTS after UKA versus TKA, and prognostic indicators of success or failure to RTS including age, sex, BMI, pre-sport participation, and sport impact level. Data were extracted by the lead author (DL) using the JBI protocol, which considers both qualitative and quantitative factors.
An assessment of the methodological quality of articles was included after the full-text review using the JBI clinical appraisal checklist.8 The checklist consists of ten questions specifically designed to evaluate the quality of systematic reviews for use in an umbrella review. Each checklist item was assigned a score of 0 or 1 based on if the article clearly answered the checklist item. Studies that totaled 10 to 8 were graded as high-quality, 7 to 4 were moderate-quality, and 3 to 0 were low-quality.
Results
The search yielded a total of 410 articles, including 58 duplicates. After screening of the remaining 352 articles by abstract and title, 36 articles remained, which were then screened by full text. Seven articles were included in the final analysis. Details on the selection and screening process can be found in the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram in Figure 1.9
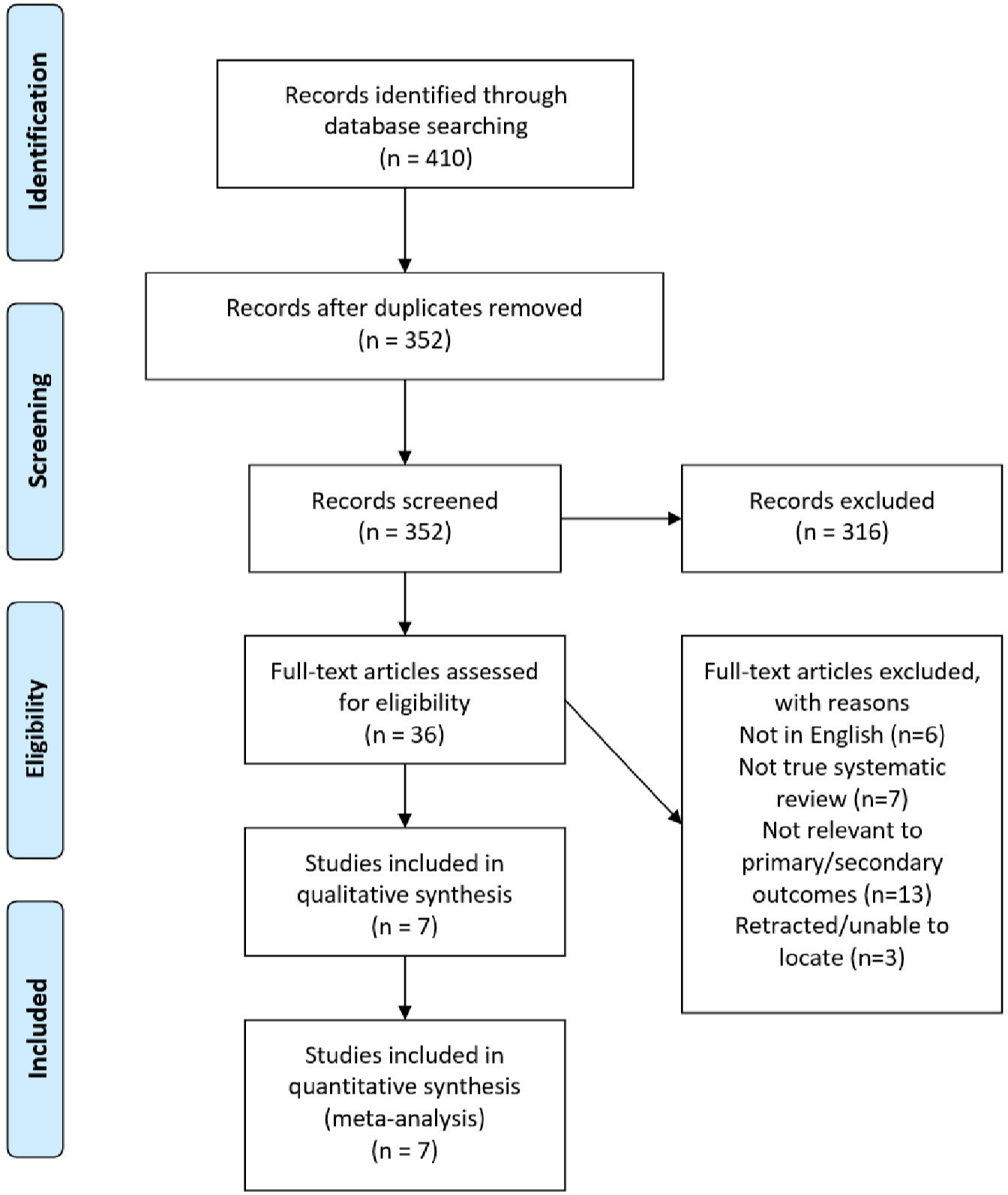
Fig. 1
Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram.9
Characteristics of included reviews
The seven selected studies were published between 2011 and 2018.10-16 Four studies analyzed TKAs alone, one study analyzed UKAs alone, and two studies analyzed both TKAs and UKAs. They contained data from 162 studies including 12,042 TKAs, 3,298 UKAs, and an additional 19,830 patients where the breakdown between TKA, UKA, and other joint arthroplasties, including total hip and total shoulder arthroplasties, were not specified. The full study characteristics table can be found in Supplementary Tables i and ii.
Methodological quality assessment
The methodological quality scores based on the JBI umbrella review protocol clinical appraisal checklist ranged from 3 to 9, with Witjes et al16 and Waldenstein et al15 being deemed high-quality, Barber-Westin and Noyes,10 Jassim et al,11 and Oljaca et al12 scoring as moderate-quality, and Papaliodis et al13 and Vogel et al14 rated as low-quality. Higher-quality studies were considered more significant when forming the final recommendations for returning to sport. The checklist questions and scoring can be found in Supplementary Table iii.
Primary outcome
The consensus finding of these studies is that patients are able to return to low- to moderate-impact sports following both TKA and UKA, with a predominance of participation in low-impact sports, and sports in which they had previously participated. Full details of the results from each study can be found in Table I.
Table I.
Primary and secondary outcomes.
| Study | Classification of sports that patients are able to return to after TKA/UKA | Time to RTS | Prognostic indicators of RTS | Reasons patients do not RTS |
|---|---|---|---|---|
| Barber-Westin and Noyes10 | Most common activities participated in are 65% walking, 35% biking, 30% swimming, 25% hiking, 15% dance, less than 10% golf. Between 34% and 100% of patients returned to recreational activities. |
Not reported. | Not addressed in included studies. | Unable to determine from included studies. |
| Jassim et al11 | Majority of patients (54% to 98%) can RTS with some qualification but it is highly variable. Patients tend to return to low impact over high impact sports. Implant survival is not reduced in active patients, but long-term follow-up is needed as some studies show higher radiological wear in active populations. UKA patients were able to return to sport more often than TKA. |
Survey data shows 2/3 physicians allow RTS after TJR at 6 months, 1/3 say 3 months. | Low age, male sex, low BMI, preoperative sport participation, and no other joint pain. | Pain, apprehension, instructions from surgeon. |
| Oljaca et al12 | Recommend returning to low and intermediate impact sports Recommend against returning to high impact and contact sports. New recommendations should be considered to allow returning to jogging and singles and doubles tennis. 88% who regularly practice sports continued at 1 year follow-up |
Not reported | Not Reported | Not reported |
| Papaliodis et al13 | It is safe to return to golf following knee arthroplasty. | Patients can return to putting at 4 to 6 weeks and progress to full at 6 to 10 months. | Not reported |
Not reported |
| Vogel et al14 | Sports that create high knee joint loads (running) or high impact (football) are not recommended. High risk sports such as skiing are okay with prior experience and with proper patient education of risk. |
May take as long as 3 months to RTS |
Increased bone density helps prevent loosening |
Precaution due to surgeon instruction |
| Waldstein et al15 | No sport-specific recommendations, however suggests patients can return to activities in line with Knee Society recommendations. | Not reported. | Not reported | Preservation of implant |
| Witjes et al16 | Patients are able to return to both low and high impact sports, however patients tend to return to lower impact sports. For some patients, some types of high-impact sports are possible following knee arthroplasty. There is no consensus on long term implant survival with high impact sports. Advocate for “intelligent participation”. Allow patient’s prior experience and well as joint impact to help guide recommendations |
Patients return to sport at 12 weeks following UKA, 91% of which were low impact. 13 weeks for TKA, 95% of which were low impact. |
Patients are more likely to return to sport following UKA. Preoperative sports participation is a prognostic indicator for RTS. |
Surgeon instruction |
-
RTS, returning to sports; TJR, total joint replacement; TKA, total knee arthroplasty; UKA, unicompartmental knee arthroplasty.
Secondary outcomes
Overall, a substantial percentage of patients were able to RTS following TKA and UKA.10-13,15,16 However, there was significant variability between studies regarding the proportion of patients able to do so. For TKA, the 19 studies included in Barber-Westin and Noyes10 reported a RTS range of 34% to 100%, while ten studies included in Wtijes et al16 reported 36% to 89%. For UKA, patients had a RTS rate of 74% to over 100% according to seven studies from Witjes et al16 Comparison between TKA and UKA by Witjes et al16 showed higher rates of return, participation in a greater number of sports, and higher physical activity scores following UKA compared to TKA. This finding is supported by Jassim et al,11 with two studies showing sports performance was better following UKA compared to TKA.
Data from Witjes et al16 showed time to RTS was similar between TKA and UKA at 13 and 12 weeks respectively, with most of these sports being low-impact. Papaliodis et al13 detailed a return to golf protocol, with patients putting at four to six weeks and returning without restriction at six to ten months. Jassim et al11 included recommendations from physician surveys that aligned with these data, with one-third of physicians recommending three months and two-thirds recommending six months to RTS postoperatively. Conclusions from Vogel et al14 are similar, cautioning patients to wait months to see significant improvement.
Jassim et al,11 Vogel et al,14 and Witjes et al16 commented on prognostic indicators for RTS. Younger age was supported by seven studies, male sex by 11 studies, low BMI by seven studies, and no other joint pain by three studies. The strongest prognostic indicator supported by the overall findings of the reviews was preoperative participation in the sport. The only reason to not RTS cited by any of the studies was surgeon recommendation due to fears of implant wear and failure.11,14-16
Discussion
There is a consensus that patients can return to sport following both TKA and UKA. Select recommendations can be found in Table II, and complete recommendations can be found in Table III. While there was significant variability in the rate of RTS across the studies, a majority of patients in the included studies were able to RTS and impact levels that are allowed in our recommendations. Patients have demonstrated success returning to low- and moderate-impact sports, as well as some select high-impact sports. Patients were able to RTS more frequently following a UKA compared to TKA, however there is no difference in the specific sport recommendations between TKA and UKA. Patients were able to return to low-impact sports at 12 weeks following UKA and 13 weeks following TKA. The biggest predictor of patients returning to moderate- to high-impact sports is prior experience participating in the sport,11,14,16 whereas the most commonly cited reason for patients to avoid RTS was the recommendation of their surgeon.11,14 While there is agreement that low-impact sports are safe for the patient and implant, there is optimism that moderate- to high-impact sports are safer than current guidelines state.12,14,16 It should be cautioned that patients may return to moderate- to higher-impact sports when the participant has prior experience with the sport, as they have the learned muscle control and proprioception to safely return.
Table II.
Select recommendations for return to sport.
| Recommendation status | Activity |
|---|---|
| Recommended | Walking |
| Golf | |
| Biking | |
| Recommended with experience | Hiking |
| Doubles tennis | |
| Downhill skiing | |
| Not recommended, but a collective decision between patient and physician can be made | Baseball |
| Basketball | |
| Running | |
| Soccer |
Table III.
Complete recommendations.
| Impact per Vail et al6 | Sport | Recommendation | Vail et al6 | Healy et al5 | AAHKS |
|---|---|---|---|---|---|
| Low | Stationary cycling | A | A | A | A |
| Callisthenics | A | A | N/A | A | |
| Golf | A | A | A | A | |
| Stationary skiing | A | A | AE | A | |
| Walking | A | A | A | A | |
| Ballroom dancing | A | A | A | A | |
| Water aerobics | A | A | N/A | A | |
| Potentially low | Bowling | A | A | A | A |
| Fencing | A | A | No consensus | A | |
| Rowing | A | A | AE | A | |
| Isokinetic weightlifting | A | A | N/A | A | |
| Sailing | A | A | N/A | A | |
| Speed walking | A | A | A | A | |
| Cross-country skiing | A | A | A | A | |
| Table tennis | A | A | N/A | A | |
| Jazz dancing and ballet | A | A | N/A | A | |
| Bicycling | A | A | A | A | |
| Intermediate | Free weightlifting | AE | AE | No consensus | AE |
| Hiking | AE | AE | A | AE | |
| Horseback riding | AE | AE | AE | AE | |
| Ice skating | AE | AE | AE | AE | |
| Rock climbing | AE | AE | No consensus | AE | |
| Low-impact aerobics | AE | AE | AE | AE | |
| Doubles tennis | AE | AE | N/A | AE | |
| In-line skating | AE | AE | No consensus | AE | |
| Downhill skiing | AE | AE | AE | AE | |
| High | Baseball Softball |
NR | NR | No consensus | NR |
| Basketball and volleyball |
NR | NR | NR | NR | |
| American football/rugby | NR | NR | NR | NR | |
| Handball and racquetball |
NR | NR | No consensus | NR | |
| Jogging and running |
NR | NR | NR | NR | |
| Lacrosse | NR | NR | N/A | NR | |
| Soccer | NR | NR | NR | NR | |
| Singles tennis | NR | NR | No consensus | NR | |
| Waterskiing | NR | NR | N/A | NR | |
| Karate | NR | NR | N/A | Undecided |
-
A, allowed; AAHKS, American Association of Hip and Knee Surgeons; AE, allowed with experience; N/A, not available; NR, not recommended (although a collective decision between patient and physician can be made).
Smaller studies have shown that patients have been able to successfully return to reasonably high-impact and high-risk sports, like judo17 and high-level tennis,18 if they have significant experience with the sport prior to arthroplasty. These studies suggest that the concern for trauma in high-impact sports can be at least partially mitigated by patient expertise. However, the potential risk of acute traumatic injuries, and the possibility that increased loading cycles of impact on the implant could cause wear or aseptic loosening (eventually necessitating revision surgery), underlie the apprehension to allow high-impact sports. McCalden et al19 found increased revision rates in younger populations due to aseptic loosening and instability, and hypothesized that increased activity and more complex preoperative issues were the cause. While sports have not been directly linked to the early revisions seen in younger populations, it is reasonable to caution patients that increased activity may contribute to the earlier revisions seen. Interestingly, Jassim et al11 found that while there was increased radiological wear seen in sporting populations, there was no increase in revision rates. In fact, polyethylene wear is a decreasing cause of revision surgeries compared to other indications such as infection or instability.20 Further, a review from 2015 did not find a correlation between physical activity and aseptic loosening in TKAs.21 In contrast, activity does appear to affect wear in total hip arthroplasty.21 Oljaca et al12 argued that jogging and both singles and doubles tennis should be regarded as safe sports from this perspective, due to multiple studies demonstrating no increase in revision rates at a mean follow-up time of 4.8 years for jogging and seven to eight years for tennis. Despite this optimism, there is currently a lack of long-term data to recommend patients can safely return to all high-impact sports. The papers included in this study show that patients are not attempting to return to high-impact sports, likely due to surgeons recommending against it. This recommendation is out of an abundance of caution, and not necessarily due to concrete evidence that high-impact sports are unsafe. However, patients have demonstrated success returning to doubles tennis and downhill skiing with prior experience. We believe that these sports represent the current upper limit of impact to which a patient can expect to return after knee arthroplasty that is supported by the data.
It is clear that certain sports predispose the participant to traumatic injury, and these factors are considered in this classification system and recommendations put forth by Vail et al6 This considers not only the degree of repetition and magnitude of joint loading, but also the potential for violence. The findings of this review correlate well with these recommendations in addition to those by AAHKS4 and The Knee Society.5 It is universally accepted that low-impact sports are safe to return to, and moderate-impact sports are safe with prior experience. High-impact sports are not recommended, largely due to the risk of traumatic injury and increased loading cycles. It could be argued that patients who are participating in high-impact sports at the highest level may have the expertise to return to these sports, however, we feel inherent risk and unpredictability of contact sports, as well as the unknown long-term outcomes, may preclude safe return.
Limitations of this study include the lack of a universally accepted classification system for sport impact level. We considered that that the classification by Vail et al6 was the most complete, however not every article we assessed used this system. During data extraction and formulation of recommendations, we considered these differences and the strength of the reviews to provide the most objective and evidence-based recommendations. A second limitation of the study is the quality of the data contained within the systematic reviews and meta-analyses. Barber-Westin and Noyes10 were unable to come to a conclusion for concrete sport recommendations due to the heterogeneity of the data, which is a common theme among many of the articles we included in this study. Witjes et al16 hypothesized that some of this heterogeneity is due to inconsistencies defining preoperative sport participation as immediately before surgery, at any point during a patient’s life, or anywhere between, leading to variable rates of RTS. We believe that because this is an umbrella review, it pools far more data than any one systematic review, allowing us to make stronger claims than any individual review. Additionally, the included studies often considered walking as a sport. While there is some debate around whether walking should be considered a true sport, returning to walking is generally accepted, and returning to low-impact sports beyond walking is strongly supported. The classification of walking as a sport does not impact the final recommendations and was left in the guidelines for completeness.
In conclusion, as the population of TKA and UKA patients become increasingly younger, it is important for physicians to be able to answer questions about RTS after these procedures. Based on the available evidence, we conclude that patients can return to low-impact sports irrespective of prior experience, and moderate-impact sports with prior experience. There are insufficient long-term data to provide recommendations on high-impact sports. When deciding between a TKA and a UKA, patients are more successful in RTS following a UKA and do so earlier, however there is no difference in the sports in which they eventually participate. Future studies are needed to evaluate the revision and failure rates of patients who return to high-impact sports to determine appropriate recommendations regarding return to high-impact sports after knee arthroplasty.
References
1. Kurtz S , Ong K , Lau E , Mowat F , Halpern M . Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030 . J Bone Joint Surg Am . 2007 ; 89-A ( 4 ): 780 – 785 . Crossref PubMed Google Scholar
2. Maradit Kremers H , Larson DR , Crowson CS , et al. Prevalence of total hip and knee replacement in the United States . J Bone Joint Surg Am . 2015 ; 97-A ( 17 ): 1386 – 1397 . Crossref PubMed Google Scholar
3. Wilson HA , Middleton R , Abram SGF , et al. Patient relevant outcomes of unicompartmental versus total knee replacement: systematic review and meta-analysis . BMJ . 2019 ; 364 : l352 . Crossref PubMed Google Scholar
4. No authors listed . Resuming sports after knee replacement . American Association of Hip and Knee Surgeons . https://hipknee.aahks.org/wp-content/uploads/2019/01/resuming-sports-after-knee-replacement-AAHKS.pdf ( date last accessed 18 February 2022 ). Google Scholar
5. Healy WL , Sharma S , Schwartz B , Iorio R . Athletic activity after total joint arthroplasty . J Bone Joint Surg Am . 2008 ; 90-A ( 10 ): 2245 – 2252 . Crossref PubMed Google Scholar
6. Vail TP , Mallon WJ , Liebelt RA . Athletic activities after joint arthroplasty . Sports Med Arthrosc Rev . 1996 ; 4 ( 3 ): 298 . Crossref Google Scholar
7. Sowers CB , Carrero AC , Cyrus JW , Ross JA , Golladay GJ , Patel NK . Return to sports after total hip arthroplasty: an umbrella review for consensus guidelines . Am J Sports Med . 2021 . Crossref PubMed Google Scholar
8. Aromataris E , Fernandez R , Godfrey CM , Holly C , Khalil H , Tungpunkom P . Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach . Int J Evid Based Healthc . 2015 ; 13 ( 3 ): 132 – 140 . Crossref PubMed Google Scholar
9. Moher D , Liberati A , Tetzlaff J , Altman DG , PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement . Ann Intern Med . 2009 ; 151 ( 4 ): 264 – 269 . Crossref PubMed Google Scholar
10. Barber-Westin SD , Noyes FR . Aerobic physical fitness and recreational sports participation after total knee arthroplasty . Sports Health . 2016 ; 8 ( 6 ): 553 – 560 . Crossref PubMed Google Scholar
11. Jassim SS , Douglas SL , Haddad FS . Athletic activity after lower limb arthroplasty: a systematic review of current evidence . Bone Joint J . 2014 ; 96-B ( 7 ): 923 – 927 . Crossref PubMed Google Scholar
12. Oljaca A , Vidakovic I , Leithner A , Bergovec M . Current knowledge in orthopaedic surgery on recommending sport activities after total hip and knee replacement . Acta Orthop Belg . 2018 ; 84 ( 4 ): 415 – 422 . PubMed Google Scholar
13. Papaliodis DN , Photopoulos CD , Mehran N , Banffy MB , Tibone JE . Return to golfing activity after joint arthroplasty . Am J Sports Med . 2017 ; 45 ( 1 ): 243 – 249 . Crossref PubMed Google Scholar
14. Vogel LA , Carotenuto G , Basti JJ , Levine WN . Physical activity after total joint arthroplasty . Sports Health . 2011 ; 3 ( 5 ): 441 – 450 . Crossref PubMed Google Scholar
15. Waldstein W , Kolbitsch P , Koller U , Boettner F , Windhager R . Sport and physical activity following unicompartmental knee arthroplasty: a systematic review . Knee Surg Sports Traumatol Arthrosc . 2017 ; 25 ( 3 ): 717 – 728 . Crossref PubMed Google Scholar
16. Witjes S , Gouttebarge V , Kuijer P , van Geenen RCI , Poolman RW , Kerkhoffs G . Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis . Sports Med . 2016 ; 46 ( 2 ): 269 – 292 . Crossref PubMed Google Scholar
17. Lefevre N , Rousseau D , Bohu Y , Klouche S , Herman S . Return to judo after joint replacement . Knee Surg Sports Traumatol Arthrosc . 2013 ; 21 ( 12 ): 2889 – 2894 . Crossref PubMed Google Scholar
18. Mont MA , Rajadhyaksha AD , Marxen JL , Silberstein CE , Hungerford DS . Tennis after total knee arthroplasty . Am J Sports Med . 2002 ; 30 ( 2 ): 163 – 166 . Crossref PubMed Google Scholar
19. McCalden RW , Robert CE , Howard JL , Naudie DD , McAuley JP , MacDonald SJ . Comparison of outcomes and survivorship between patients of different age groups following TKA . J Arthroplasty . 2013 ; 28 ( 8 Suppl ): 83 – 86 . Crossref PubMed Google Scholar
20. Thiele K , Perka C , Matziolis G , Mayr HO , Sostheim M , Hube R . Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery . J Bone Joint Surg Am . 2015 ; 97-A ( 9 ): 715 – 720 . Crossref PubMed Google Scholar
21. Cherian JJ , Jauregui JJ , Banerjee S , Pierce T , Mont MA . What host factors affect aseptic loosening after THA and TKA? Clin Orthop Relat Res . 2015 ; 473 ( 8 ): 2700 – 2709 . Crossref PubMed Google Scholar
Author contributions
D. Lester: Investigation, Formal analysis, Writing – original draft, Writing – review & editing.
C. Barber: Investigation, Formal analysis, Writing – original draft.
C. B. Sowers: Conceptualization, Writing – original draft.
J. W. Cyrus: Investigation, Writing – review & editing.
A. R. Vap: Formal analysis, Writing – review & editing.
G. J. Golladay: Conceptualization, Formal analysis, Writing – review & editing.
N. K. Patel: Conceptualization, Formal analysis, Writing – review & editing.
Funding statement
The authors received no financial or material support for the research, authorship, and/or publication of this article.
ICMJE COI statement
A. R. Vap reports payment for expert testimony from GEICO Insurance Company, and support for attending meetings from MCVP Physicians, unrelated to this study. G. J. Golladay reports royalties from Stryker, a leadership role on the Virginia Orthopaedic Society and AAHKS Publications Committee, and an editor stipend for Arthroplasty Today, all unrelated to this study. N. K. Patel is an editorial board member on the Journal of Arthroplasty.
Open access funding
The authors confirm that the open access fee for this study was self-funded.
Supplementary material
Characteristics of the reviews as well as the methodological quality scoring.
© 2022 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/









