Abstract
Aims
To compare results of institutional preferences with regard to treatment of soft tissues in the setting of open tibial shaft fractures.
Methods
We present a retrospective review of open tibial shaft fractures at two high-volume level 1 trauma centres with differing practices with regard to the acute management of soft tissues. Site 1 attempts acute primary closure, while site 2 prefers delayed closure/coverage. Comparisons include percentage of primary closure, number of surgical procedures until definitive closure, percentage requiring soft tissue coverage, and percentage of 90-day wound complication.
Results
Overall, there were 219 patients at site 1 and 282 patients at site 2. Differences in rates of acute wound closure were seen (168 (78%) at site 1 vs 101 (36%) at site 2). A mean of 1.5 procedures for definitive closure was seen at site 1 compared to 3.4 at site 2. No differences were seen in complication, nonunion, or amputation rates. Similar results were seen in a sub-analysis of type III injuries.
Conclusion
Comparing outcomes of open tibial shaft fractures at two institutions with different rates initial wound management, no differences were seen in 90-day wound complications, nonunion rates, or need for amputation. Attempted acute closure resulted in a lower number of planned secondary procedures when compared with planned delayed closure. Providers should consider either acute closure or delayed coverage based on the injury characteristics, surgeon preference and institutional resources without concern that the decision at the time of index surgery will lead to an increased risk of complication.
Cite this article: Bone Joint Open 2020;1-8:481–487.
Introduction
Treatment protocols for open fractures vary based on anatomical location, fracture pattern, level of contamination, and soft tissue injury. Institutional bias and training background, extreme variations in patients and injury patterns, and non-standardized definitions of outcomes such as infection and nonunion have contributed to disagreement regarding the timing of wound closure.1-13 Historic reports of unacceptably high infection rates associated with the acute closure of open fractures have resulted in caution at the time of initial debridement, especially for areas with limited vascularity, such as the tibia.5,8 Delayed closure or coverage, often with the use of negative pressure wound therapy as an intermediate step, remains common.14-17 More recent studies would indicate that acute primary wound closure may be beneficial for the majority of open fractures as long as a thorough debridement is possible, modern antibiotic treatment is employed, and definitive or temporary fracture stabilization is achieved.1,6,7,9,18 For these reasons, controversy exists when deciding to close traumatic wounds associated with open fractures in an acute or delayed fashion.
The decision to close an open fracture acutely is often made at the discretion of the treating surgeon after accounting for variables including contamination level, vascular insult, wound size and character, and the overall physiological status of the patient. The Gustilo-Anderson classification system10 is widely used as a measure of injury severity. Despite moderate to poor interobserver agreement,19 it is commonly used to guide treatment when deciding on acute versus delayed wound closure with injuries classified as more severe (type 3) often being left open. Furthermore, the same fracture could be classified as type 3A or type 3B based on chosen treatment and not necessarily injury characteristics. More recently, studies have suggested that the Orthopaedic Trauma Association open fracture classification (OTA-OFC),20 which include five variables (skin, muscle, arterial, contamination, bone loss) has improved interobserver reliability when compared to the Gustilo-Anderson classification,21 and may be more predictive of both surgeon treatment choice with regard to wound management and clinical outcome.22,23
It was the goal of this study to compare short-term clinical outcomes of a large series of patients treated for open tibial shaft fractures at two high-volume trauma centres with differing protocols for the acute management of soft tissue injuries resulting from these injuries (acute primary closure vs delayed closure or coverage). We hypothesize that there will be no difference in 90-day return to operating room (OR), infection rates or nonunion rates between the two cohorts, but that the number of operative procedures will be higher at the institution favoring delayed closure.
Methods
Institutional Review Board approval was obtained at both site 1 (Harborview Medical Centre, Seattle, Washington, USA) and site 2 (University of Texas Health Science Centre at Houston, Houston, Texas, USA) to conduct retrospective review of fracture registries. Both centres are regional referral centres and manage a high volume of acute orthopaedic injuries, including tibial shaft fractures. These two centres were chosen as they have differing practices regarding the acute management of soft tissue injuries in open fractures due to varying institutional preferences and resources, but similar referral patterns. At both sites, fellowship-trained orthopaedic trauma surgeons manage all call responsibilities with experience ranging from first year in practice to more than 25 years of experience. Site 1 practices acute, primary closure of traumatic wounds in the setting of open fractures when it could be done in conjunction with an acceptable debridement, surgical stabilization and a tension free closure and provided the patient can tolerate the procedure. When necessary, a microvascular surgeon is consulted for delayed rotational or free soft-tissue transfer in conjunction with negative pressure wound therapy.
At site 2, wounds are frequently left open and initially treated with negative pressure wound therapy dressing. Additional trips to the operating room are planned for delayed primary closure, local soft tissue rearrangement, rotational or free muscle flap coverage at a later date. During the study inclusion period, site 2 had a microvascular surgeon dedicated to the reconstruction of traumatic wounds, including those associated with open fractures, as well as an orthopaedic surgeon specializing in circular external fixation. External fixation was used at the discretion of treating surgeons with definitive surgical stabilization being completed at the same time as or as close to definitive coverage as possible at both sites. Antibiotic use and duration varied based on surgeon preference and injury characteristics, but in general, was initiated as soon as possible and discontinued within 24 hours or definitive soft tissue coverage. Wound cultures were not routinely obtained at either site.
Patients treated for open tibial shaft fractures without proximal or distal articular extension (OTA 42)24 between August 2010 and September 2015 were identified. Exclusion criteria included being aged less than 18 years. OTA/AO fracture classification,24 Gustilo-Anderson type10 and OTA-OFC20 were collected prospectively at site 1 and retrospectively at site 2. Additional perioperative variables collected retrospectively include patient demographics, comorbidities, smoking status, fixation type, number of procedures until definitive coverage, and type of definitive coverage. Clinical outcomes include 90-day wound complication (superficial or deep infection, wound dehiscence), the diagnosis of a nonunion and treatment with amputation. Superficial infection was defined as any wound requiring antibiotic management but not a return to the OR; deep infection was defined as a return to the OR with positive cultures; nonunion was defined as an additional, unplanned surgical procedure to achieve union. Patients without complete 90-day follow-up were only included in the analysis if they had data for the variable of interest (Figure 1).
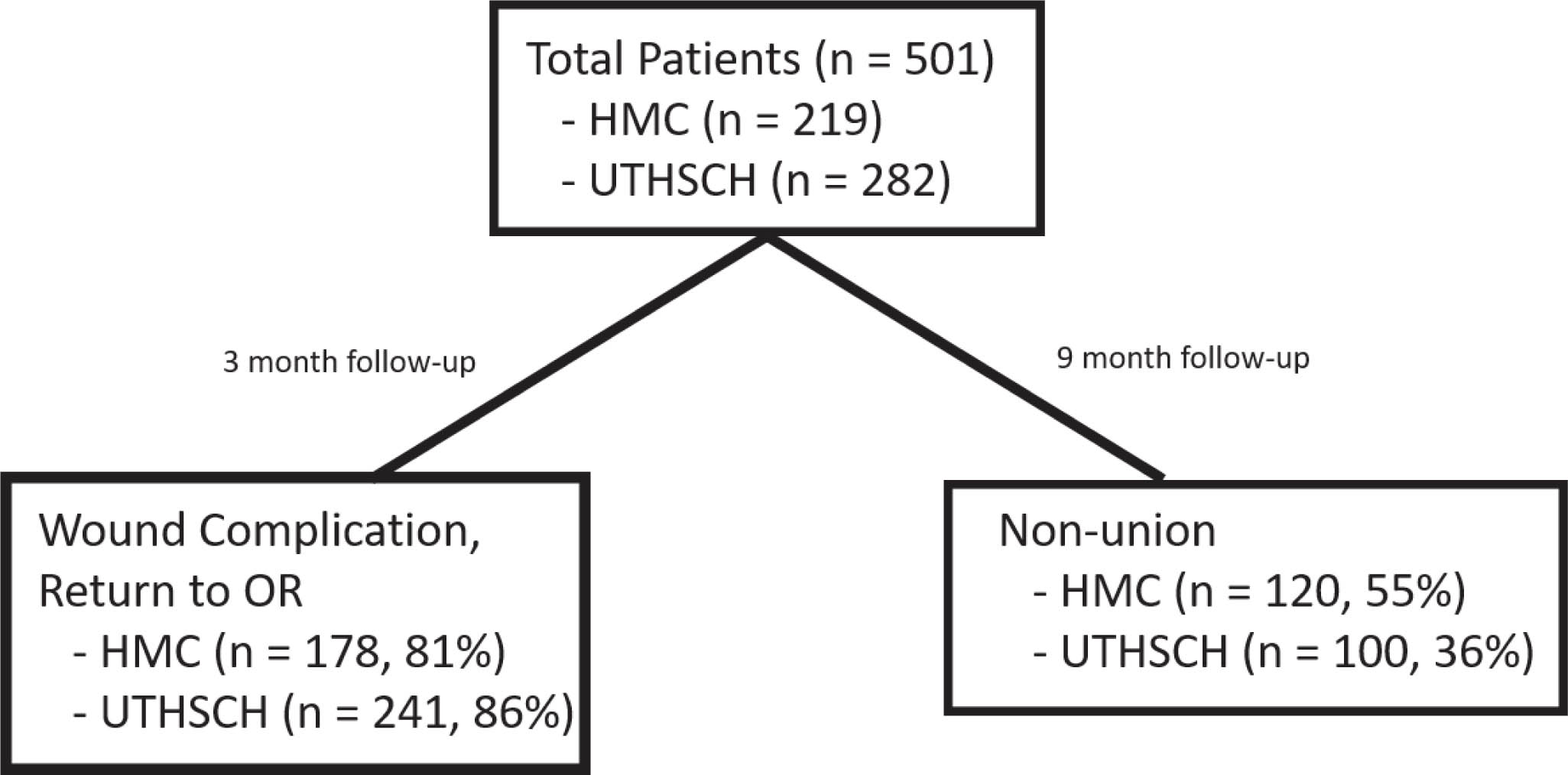
Fig. 1
Number of patients with follow-up data for each variable of interest for each participating center. HMC, Harborview Medical Center; UTHSCH, University of Texas Health Science Center at Houston.
Statistical analysis included descriptive statistics, t-test for comparison of continuous variables and chi-squared or Fisher’s Exact test for comparison of categorical variables. Excel 2016 (Microsoft, Redmond, Washington, USA), SPSS v26 (IBM, Armonk, New York, USA), and Medcalc v12 (Ostend, Belgium) were used for analysis.
Sources of funding
No external sources of funding were required for this study.
Results
Over the study period, a total of 538 (230 at site 1 and 308 at site 2) open tibial shaft fractures were treated at both centres. In all, 11 patients (4.8%) were excluded at site 1 and 26 (8.4%) at site 2 for being under the age of 18 years, leaving a total of 501 for analysis. Patient populations were similar with regard to demographics as can be seen in Table I. Differences were seen in OTA fracture type18 (Table II), Gustilo-Anderson Classification and Orthopaedic Trauma Association-Open Fracture Classification (Tables III and IV). Acute wound closure at the time of index procedure was performed in 269 patients total (168 (78%) at site 1 and 101 (36%) at site 2). Delayed primary closure was performed in 18 of the remaining patients (11 (5.1%) at site 1 and seven (2.5%) at site 2). Closure in the form of rotational flap or free muscle transfer was performed in 162 patients (14 (6.5%) at site 1 and 148 (52.7%) at site 2).
Table I.
Demographics for patients treated for open tibia fractures at Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| Variable | Site 1 | Site 2 | p-value |
|---|---|---|---|
| Number of patients | 219 | 282 | |
| Mean age, yrs | 41.9 | 38.8 | 0.024* |
| Sex, male % | 81 | 79 | 0.629† |
| Comorbidities, % | |||
| Diabetes | 4 | 5 | 0.567† |
| Peripheral vascular disease | 1 | 3 | 0.203‡ |
| Hypertension | 19 | 19 | 0.961† |
| Hyperlipidemia | 9 | 7 | 0.354† |
| Smoker | 38 | 30 | 0.062† |
| Alcohol abuse | 17 | 12 | 0.122† |
| Immunocompromised§ | 5 | 2 | 0.063‡ |
| Body mass index, % | |||
| < 20 | 6 | 4 | 0.158† |
| 20 to 25 | 31 | 26 | |
| 25 to 30 | 42 | 40 | |
| > 30 | 22 | 30 | |
-
*
Student’s t-test,
-
†
Chi-squared test,
-
‡
Fisher’s exact test.
-
§
Immunocompromised patients who report taking prescribed medications that suppress the immune system.
Table II.
OTA/AO fracture classification comparison between Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| OTA/AO fracture classification | Site 1, n (%) | Site 2, n (%) |
|---|---|---|
| 42A | 56 (28.4) | 111 (39.4) |
| 42B | 73 (37.1) | 93 (32.9) |
| 42 C | 68 (34.5) | 78 (27.7) |
Table III.
Gustilo-Anderson classification comparison between Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| Gustilo-Anderson classification | Site 1, n (%) | Site 2, n (%) |
|---|---|---|
| Type 1 | 25 (11.6) | 18 (6.4) |
| Type 2 | 60 (27.9) | 60 (21.3) |
| Type 3 | 130 (60.4) | 204 (72.3) |
| A | 96 (73.8) | 38 (18.5) |
| B | 15 (11.5) | 141 (68.8) |
| C | 19 (14.6) | 25 (12.3) |
Table IV.
Orthopaedic Trauma Association open fracture classification comparison between Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| OTA-OFC classification | Site 1, n (%) | Site 2, n (%) |
|---|---|---|
| OTA-OFC skin | ||
| 1 | 181 (82.7) | 107 (37.9) |
| 2 | 13 (5.9) | 129 (45.7) |
| 3 | 25 (11.4) | 46 (16.3) |
| OTA-OFC muscle | ||
| 1 | 106 48.4) | 151 (53.7) |
| 2 | 84 (38.4) | 91 (32.4) |
| 3 | 29 (13.2) | 39 (13.9) |
| OTA-OFC arterial | ||
| 1 | 186 (84.9) | 183 (65.0) |
| 2 | 16 (7.3) | 69 (24.5) |
| 3 | 17 (7.8) | 30 (10.6) |
| OTA-OFC contamination | ||
| 1 | 117 (53.4) | 72.2 (203) |
| 2 | 81 (37.0) | 50 (17.8) |
| 3 | 21 (9.6) | 28 (10.0) |
| OTA-OFC bone loss | ||
| 1 | 141 (64.4) | 157 (55.9) |
| 2 | 67 (30.6) | 87 (31.0) |
| 3 | 11 (5.0) | 37 (13.2) |
At site 1, the mean number of procedures required to achieve definitive closure was 1.5 compared with 3.4 at site 2. At the time of index surgery, external fixation was used 16.4% (36/219) of the time at site 1 and 53.5% (129/281) of the time at site 2. Of those patients, 20 (55.6%) were closed acutely at site 1 compared to 14 (10.9%) at site 2. Within this subset, wounds were reopened after closure at the time of definitive fixation in three patients at site 1 and four patients at site 2. Definitive fixation was primarily achieved with intramedullary fixation at both sites (Table V). Complete or partial 90-day data was available for 419 patients (178 at site 1 and 241 at site 2). 90-day wound complication rates were comparable (20 (11.2%) at site 1 and 25 (10.4%) at site 2). Of those patients, 18 (10.1%) at site 1 and 22 (9.1%) at site 2 required an unplanned return to the OR for treatment of a wound complication. Each centre had 20 documented nonunions. In all, 43 patients underwent definitive amputation (19 (8.7%) at site 1 and 24 (8.5%) at site 2). Comparative data is summarized in Table V.
Table V.
Clinical outcomes and complications within 90 days for Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| Variable | Site 1 | Site 2 |
|---|---|---|
| Closed at index surgery, n (%) | 168/216 (78) | 101/281 (36) |
| Closed with rotational or free soft tissue transfer, n (%) | 14/216 (6.5) | 148/281 (52.7) |
| Number of procedures for closure, mean | 1.5 | 3.4 |
| External fixator at index surgery, n (%) | 36/219 (16.4) | 129/281 (53.5) |
| Definitive fixation or amputation, n (%) | ||
| Intramedullary device | 190/219 (86.8) | 215/281 (76.5) |
| Plate fixation | 4.6 (10/219) | 6.8 (19/281) |
| External fixation | 0/219 (0) | 24/281 (8.5) |
| Amputation | 19/219 (8.7) | 24/281 (8.5) |
| 90-day wound complications | 0/178 (11.2) | 25/241 (10.4) |
A sub-analysis of Gustilo-Anderson type 3 fractures was performed. At site 1, 130 type 3 open tibia fractures were treated over the study period compared to 204 at Site 2. Acute closure was performed more frequently at site 1 (64 (62.7%) vs 24 (13.6%)). Delayed primary closure was performed in eight (6.2%) of site 1 patients and one (< 1%) of site 2. Rotational flap or free soft tissue transfer was used in 12 (11.8%) of site 1 patients and 131 (74.4%) of site 2 patients. The mean number of procedures was 2.0 at site 1 and 4.5 at site 2. Results are summarized in Table VI.
Table VI.
Clinical outcomes and complications for Gustilo-Anderson Type 3 injuries at Harborview Medical Centre (site 1) and University of Texas Health Science Centre at Houston (site 2).
| Variable | Site 1 | Site 2 |
|---|---|---|
| Closed at index surgery, n (%) | 64/102 (62.7) | 24/176 (13.6) |
| Number of procedures for closure, mean | 2.0 | 4.5 |
| Cclosed with rotational or free soft tissue transfer, n (%) | 12/102 (11.8) | 131/176 (74.4) |
| 90-day wound complications, n (%) | 17/102 (16.7) | 21/176 (11.9) |
| Amputation, n (%) | 19/130 (14.6) | 24/204 (11.7) |
Discussion
The results of our large retrospective comparison of two high-volume referral centres with different institutional preferences with regard to the management of open tibia fractures would indicate that attempted acute closure or delayed closure/coverage is appropriate with similar complication rates. As would be expected, acute closure resulted in a lower number of surgical procedures to achieve definitive coverage and less use of external fixation at index surgery, but there was no difference identified in 90-day wound complications, nonunions, or amputation rates (Table V). This trend was also observed for more severe, Gustilo-Anderson type 3 open fractures (Table VI). There are many reasons results may be comparable despite differing approaches. Site 1 and site 2 are high-volume regional academic referral centres. At both, all call responsibility is managed by a fellowship-trained orthopaedic trauma surgeon who is experienced in the evaluation and treatment of open tibia fractures. Site 1 has five annual orthopaedic trauma fellows compared to four at site 2. Residents and medical students are the primary surgical assistants at both sites. Both centres have the infrastructure in place to manage these injuries with either acute or delayed coverage.
The only obvious differences between the two sites is that during the period of study, site 2 employed a microvascular surgeon who was tasked with closure of traumatic wounds as well as a surgeon who specializes in circular ringed fixators. These two factors can explain the increase in delayed closures, flap coverage and definitive external fixation seen at site 2. Based on the data presented, along with recent literature published using modern surgical techniques,6,7,18 providers should consider either acute closure or delayed coverage based on surgeon preference, injury characteristics and institutional resources without concern that the decision at the time of index surgery will lead to an increased risk of short-term complications. Attempted acute primary closure, when possible, will decrease the number of return trips to the OR and has the potential to decrease cost and limit hospital length of stay. It also limits reliance on additional sub-specialist for wound coverage, which may simplify patient care logistics. This is especially relevant in community hospitals or smaller trauma centres that may not have microvascular/free muscle transfer options available.
Historically, the acute closure of open fractures was avoided due to influential articles reporting unacceptable clinical outcomes. In 1974, Brown et al5 reported a series of 27 patients who had acute closure of open fractures prior to developing clostridial infections leading to disastrous results. A close evaluation of this cohort relevels that many of these patients had gross contamination, yet they were treated with acute primary closure, often in the Emergency Department. This was followed closely in 1976 by Gustilo and Anderson10 in their landmark paper supporting the role of delayed closure/coverage of all Type III injuries. Russell et al8 drew similar conclusions and stated that “there is no place for primary closure of any open tibial fracture,” based on their series of 90 open tibia fractures. They showed a 20% deep infection rate after acute primary wound closure and only 3% with delayed wound management. They further noted that eight of nine nonunions were in the acute primary closure group. With a better understanding of debridement strategies, antibiotic prophylaxis and the role of fracture stabilization, newer findings suggest the opposite: that acute closure is beneficial with regard to infection rates.6,7 With tertiary referral centres being equipped to manage these injuries with either attempted, acute primary closure or to offer delayed coverage, our results provide more information in an effort to direct surgeon’s decision-making.
If immediate closure is attempted, principles established by Rajasekaran et al6 should be employed to the extent possible, including: 1) debridement within 12 hours; 2) no skin loss primarily or secondarily during debridement; 3) skin approximation possible without tension; 4) no farmyard or gutter contamination; 5) debridement performed to the satisfaction of the surgeon; and 6) no vascular insufficiency. Time to initial debridement may not be as important as transfer to a tertiary care centre and timing of antibiotics.25-27 Closure of these wounds can often be performed using 3 to 0 nylon sutures in vertical mattress or Allgower-Donati pattern.28 Each suture is thrown, cut and snapped as seen in Figure 2A. Several sutures are then pulled across the wound to approximate the skin edges while the suture remaining at the end can then be tied (Figure 2B-C). This prevents excess forces at the site of the knot and permits even tension across the wound. An example of an acute tibia fracture closed with this technique is shown in Figure 3A-B.

Fig. 2
Clinical photograph of a tension free fasciotomy using the described suture technique: (a) Each suture is thrown and snapped; (b) Even tension is then pulled across each suture to approximate the skin edges prior to tying resulting in (c) a well approximated, tension-free closure.

Fig. 3
Clinical photograph of a severe open tibia fracture before (a) and after (b) acute closure.
This study has several strengths. It includes over 500 patients from two high-volume academic level 1 trauma centres. Patients were identified prospectively which improves the chances of identifying all or most patients with open tibia fractures. However, several weaknesses exist as well. For our results to be considered valid we make the assumption that patient and fracture characteristics are similar between both centres and that a selection bias does not exist favoring less or more severe injuries at one site or the other. We have made attempts to compare patients with regard to demographics, comorbidities, OTA fracture pattern, Gustilo-Anderson Type and OTA-OFC as can be seen in Tables I–IV.
Results are mixed with some variables demonstrating more severe injury patterns at site 1 while others would suggest injuries are more severe at site 2. Although all of this data except for patient demographics and comorbidities was collected prospectively at site 1, it was recorded retrospectively at site 2. This makes it difficult to compare patients as elements of each classification system are influenced by treatments already rendered. One could argue that it is not possible to directly compare patients based on Gustilo-Anderson type or OTA-OFC without a prospective study that utilizes an impartial, unbiased reviewer who can independently assess and classify each injury without accounting for definitive soft-tissue management. Retrospective data collection also makes defining outcomes such as infection and nonunion challenging. We were forced to rely data points identified in electronic medical records instead of prospective assessments such as surgical site infection criteria noted by the National Nosocomial Infections Surveillance (NNIS) System29 or Radiographic Union Score in Tibial (RUST) Fractures.30
The presented cohort may also be an over-representation of more severe injuries. Less severe injuries are often managed at surrounding centres rather than being transferred to a tertiary referral centre. With that in mind, we may have had improved outcomes had this population been captured. Length of hospital stay was not considered as several confounding variables existed beyond treatment choice for the open tibia fracture. As with many regional referral centres, long-term follow-up for this cohort is poor. This, along with the retrospective collection of outcome variables, resulted in missing data points. For this reason, in addition to sample size, statistical comparisons for data reported in Tables II–VI are not reported.
Although follow-up was limited, it was likely that patients with major complications, including those that would require a return trip to the operating room, would be referred to these centres for management. Ideally, extended follow-up to 12 months or beyond would available to capture late wound complications, nonunions and delayed amputations. Had this data been available, we would expect to see a greater number of nonunions and possibly amputations at each centre. Lastly, we did not address patients with compartment syndrome or focus on patients who were treated with acute free muscle transfer as has been described and recommended by many.31-33 This is not currently standard practice at either institution.
The information presented is useful to both the orthopaedic trauma surgeon and the general orthopaedic surgeon, but there is much that we did not consider that deserves mention. The use of negative-pressure dressings has become more common, as has the single-stage “fix and flap” technique.31,33,34 Neither of these were addressed in our study. Plate assisted nailing was also not a variable considered.35,36 Recently, a group from the UK has advocated for a two-stage approach to Gustilo-Anderson type IIIB fractures, including the use internal plate fixation to provide both temporary stabilization and to ensure appropriate exposure of the zone of injury while limiting the risk of pin site infections.37 The same group has documented promising results with the retention of devitalized segments of bone termed “orthoplastic reconstruction using mechanically relevant devitalized bone (ORDB).”37,38 Future studies may look to evaluate these techniques.
Conclusion
The management of traumatic wounds in open tibial shaft fractures can be challenging, but the results of this large, retrospective series would suggest that acute primary closure and delayed closure/coverage have similar results, although delayed treatment results in more surgical procedures. Surgeons should feel confident pursuing treatment that is in line with their preferences and training background while considering patient factors, injury characteristics, and institutional resources without concern that it will lead to an increase in adverse events.
References
1. Weitz-Marshall AD , Bosse MJ . Timing of closure of open fractures . J Am Acad Orthop Surg . 2002 ; 10 ( 6 ): 379 – 384 . Crossref PubMed Google Scholar
2. Benson DR , Riggins RS , Lawrence RM , et al. Treatment of open fractures: a prospective study . J Trauma . 1983 ; 23 ( 1 ): 25 – 30 . Google Scholar
3. Cullen MC , Roy DR , Crawford AH , et al. Open fracture of the tibia in children . J Bone Joint Surg Am . 1996 ; 78 ( 7 ): 1039 – 1047 . Crossref PubMed Google Scholar
4. DeLong WG , Born CT , Wei SY , et al. Aggressive treatment of 119 open fracture wounds . J Trauma . 1999 ; 46 ( 6 ): 1049 – 1054 . Crossref PubMed Google Scholar
5. Brown PW , Kinman PB . Gas gangrene in a metropolitan community . J Bone Joint Surg Am . 1974 ; 56 ( 7 ): 1445 – 1451 . PubMed Google Scholar
6. Rajasekaran S . Early versus delayed closure of open fractures . Injury . 2007 ; 38 ( 8 ): 890 – 895 . Crossref PubMed Google Scholar
7. Jenkinson RJ , Kiss A , Johnson S , Stephen DJ , Kreder HJ . Delayed wound closure increases deep-infection rate associated with lower-grade open fractures: a propensity-matched cohort study . J Bone Joint Surg Am . 2014 ; 96 ( 5 ): 380 – 386 . Crossref PubMed Google Scholar
8. Russell GG , Henderson R , Arnett G . Primary or delayed closure for open tibial fractures . J Bone Joint Surg Br . 1990 ; 72 ( 1 ): 125 – 128 . Google Scholar
9. Patzakis MJ , Harvey JP , Ivler D . The role of antibiotics in the management of open fractures . J Bone Joint Surg Am . 1974 ; 56 ( 3 ): 532 – 541 . PubMed Google Scholar
10. Gustilo RB , Anderson JT . Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses . J Bone Joint Surg Am . 1976 ; 58 ( 4 ): 453 – 458 . PubMed Google Scholar
11. Gustilo RB , Mendoza RM , Williams DN . Problems in the management of type III (severe) open fractures: a new classification of type III open fractures . J Trauma . 1984 ; 24 ( 8 ): 742 – 746 . Crossref PubMed Google Scholar
12. Davis AG . Primary closure of compound fracture wounds with immediate internal fixation, immediate skin graft, and compression dressings . J Bone Joint Surg Am . 1948 ; 30A ( 2 ): 405 – 415 . PubMed Google Scholar
13. Young K , Aquilina A , Chesser TJS , et al. Open tibial fractures in major trauma centres: A national prospective cohort study of current practice . Injury . 2019 ; 50 ( 2 ): 497 – 502 . Crossref PubMed Google Scholar
14. Virani SR , Dahapute AA , Bava SS , Muni SR . Impact of negative pressure wound therapy on open diaphyseal tibial fractures: A prospective randomized trial . J Clin Orthop Trauma . 2016 ; 7 ( 4 ): 256 – 259 . Crossref PubMed Google Scholar
15. Kim JH , Lee DH . Negative pressure wound therapy vs. conventional management in open tibia fractures: Systematic review and meta-analysis . Injury . 2019 ; 50 ( 10 ): 1764 – 1772 . Crossref PubMed Google Scholar
16. Sirisena R , Bellot GL , Puhaindran ME . The Role of Negative-Pressure Wound Therapy in Lower-Limb Reconstruction . Indian J Plast Surg . 2019 ; 52 ( 1 ): 73 – 80 . Crossref PubMed Google Scholar
17. Schlatterer DR , Hirschfeld AG , Webb LX . Negative pressure wound therapy in grade IIIB tibial fractures: fewer infections and fewer flap procedures? Clin Orthop Relat Res . 2015 ; 473 ( 5 ): 1802 – 1811 . Crossref PubMed Google Scholar
18. Halawi MJ , Morwood MP . Acute Management of Open Fractures: An Evidence-Based Review . Orthopedics . 2015 ; 38 ( 11 ): e1025 – 1033 . Crossref PubMed Google Scholar
19. Brumback RJ , Jones AL . Interobserver agreement in the classification of open fractures of the tibia. The results of a survey of two hundred and forty-five orthopaedic surgeons . J Bone Joint Surg Am . 1994 ; 76 ( 8 ): 1162 – 1166 . Crossref PubMed Google Scholar
20. Orthopaedic Trauma Association . Open fracture Study Group. A new classification scheme for open fractures . J Orthop Trauma . 2010 ; 24 ( 8 ): 457 – 464 . Google Scholar
21. Agel J , Evans AR , Marsh JL , et al. The OTA open fracture classification: a study of reliability and agreement . J Orthop Trauma . 2013 ; 27 ( 7 ): 379 – 384 . discussion 84-5 . Crossref PubMed Google Scholar
22. Agel J , Rockwood T , Barber R , Marsh JL . Potential predictive ability of the orthopaedic trauma association open fracture classification . J Orthop Trauma . 2014 ; 28 ( 5 ): 300 – 306 . Crossref PubMed Google Scholar
23. Johnson JP , Karam M , Schisel J , Agel J . An Evaluation of the OTA-OFC System in Clinical Practice: A Multi-Center Study With 90 Days Outcomes . J Orthop Trauma . 2016 ; 30 ( 11 ): 579 – 583 . Crossref PubMed Google Scholar
24. Marsh JL , Slongo TF , Agel J , et al. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association classification, database and outcomes committee . J Orthop Trauma . 2007 ; 21 ( 10 Suppl ): S1 – 133 . Crossref PubMed Google Scholar
25. Hendrickson SA , Wall RA , Manley O , et al. Time to Initial Debridement and wound Excision (TIDE) in severe open tibial fractures and related clinical outcome: A multi-centre study . Injury . 2018 ; 49 ( 10 ): 1922 – 1926 . Crossref PubMed Google Scholar
26. Schenker ML , Yannascoli S , Baldwin KD , Ahn J , Mehta S . Does timing to operative debridement affect infectious complications in open long-bone fractures? A systematic review . J Bone Joint Surg Am . 2012 ; 94 ( 12 ): 1057 – 1064 . Crossref PubMed Google Scholar
27. Lack WD , Karunakar MA , Angerame MR , et al. Type III open tibia fractures: immediate antibiotic prophylaxis minimizes infection . J Orthop Trauma . 2015 ; 29 ( 1 ): 1 – 6 . Crossref PubMed Google Scholar
28. Mueller M , Allgower M , Scheider R , Willenegger H . Manual of Internal Fixation . Techniques recommended by the AO-ASIF group . 3rd ed , 1995 . Google Scholar
29. National Nosocomial Infections Surveillance System . National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 to June 2002, issued August 2002 . Am J Infect Control . 2002 ; 30 ( 8 ): 458 – 475 . Crossref PubMed Google Scholar
30. Whelan DB , Bhandari M , Stephen D , et al. Development of the radiographic union score for tibial fractures for the assessment of tibial fracture healing after intramedullary fixation . J Trauma . 2010 ; 68 ( 3 ): 629 – 632 . Crossref PubMed Google Scholar
31. Levin LS . Early versus delayed closure of open fractures . Injury . 2007 ; 38 ( 8 ): 896 – 899 . Crossref PubMed Google Scholar
32. Lister G , Scheker L . Emergency free flaps to the upper extremity . J Hand Surg Am . 1988 ; 13 ( 1 ): 22 – 28 . Crossref PubMed Google Scholar
33. Nambi GI , Salunke AA , Thirumalaisamy SG , et al. Single stage management of Gustilo type III A/B tibia fractures: Fixed with nail & covered with fasciocutaneous flap . Chin J Traumatol . 2017 ; 20 ( 2 ): 99 – 102 . Crossref PubMed Google Scholar
34. Stannard JP , Singanamala N , Volgas DA . Fix and flap in the era of vacuum suction devices: What do we know in terms of evidence based medicine? Injury . 2010 ; 41 ( 8 ): 780 – 786 . Crossref PubMed Google Scholar
35. Stoddart MT , Al-Hourani K , Fowler T , Khan U , Kelly MB . Plate-Assisted Intramedullary Nailing of Gustilo Type IIIB Open Tibial Diaphyseal Fractures: Does Adjunctive Plate Retention Affect Complication Rate? J Orthop Trauma . 2020 ; 34 ( 7 ): 363 – 369 . Crossref PubMed Google Scholar
36. Haller JM , Githens M , Scolaro J , Firoozabadi R . Does Provisional Plating of Closed Tibia Fractures Have Higher Complication Rates? J Orthop Trauma . 2017 ; 31 ( 10 ): 554 – 558 . Crossref PubMed Google Scholar
37. Al-Hourani K , Fowler T , Whitehouse MR , Khan U , Kelly M . Two-Stage Combined Ortho-Plastic Management of Type IIIB Open Diaphyseal Tibial Fractures Requiring Flap Coverage: Is the Timing of Debridement and Coverage Associated With Outcomes? J Orthop Trauma . 2019 ; 33 ( 12 ): 591 – 597 . Crossref PubMed Google Scholar
38. Al-Hourani K , Stoddart M , Khan U , Riddick A , Kelly M . Orthoplastic reconstruction of type IIIB open tibial fractures retaining debrided devitalized cortical segments: the Bristol experience 2014 to 2018 . Bone Joint J . 2019 ; 101-B ( 8 ): 1002 – 1008 . Crossref PubMed Google Scholar
Author contributions
M. R. Garner: Designed the study, Collected the data, Prepared and submitted the manuscript.
S. J. Warner: Collected the data, Prepared the manuscript.
J. A. Heiner: Collected the data.
Y. T. Kim: Collected the data.
J. Agel: Designed the study, Collected and analyzed the data, Prepared and submitted the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
ICMJE COI statement
M. R. Garner reports consultancy and grants/grants pending from DePuy and Synthes, grants/grants pending from the Orthopaedic Trauma Association, and stock/stock options from ROM3 Rehab, all of which are unrelated to this article. S. J. Warner reports consultancy from Synthes, and grants/grants pending and payment for lectures (including service on speakers bureaus) from AONA, all of which are unrelated to this article.
Acknowledgements
The author’s would like to acknowledge Sean Nork, MD, for his contributions to this study.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.










