Abstract
Aims
The aim of this study is to determine the effects of the UK lockdown during the COVID-19 pandemic on the orthopaedic admissions, operations, training opportunities, and theatre efficiency in a large district general hospital.
Methods
The number of patients referred to the orthopaedic team between 1 April 2020 and 30 April 2020 were collected. Other data collected included patient demographics, number of admissions, number and type of operations performed, and seniority of primary surgeon. Theatre time was collected consisting of anaesthetic time, surgical time, time to leave theatre, and turnaround time. Data were compared to the same period in 2019.
Results
There was a significant increase in median age of admitted patients during lockdown (70.5 (interquartile range (IQR) 46.25 to 84) vs 57 (IQR 27 to 79.75); p = 0.017) with a 26% decrease in referrals from 303 to 224 patients and 37% decrease in admissions from 177 to 112 patients, with a significantly higher proportion of hip fracture admissions (33% (n = 37) vs 19% (n = 34); p = 0.011). Paediatric admissions decreased by 72% from 32 to nine patients making up 8% of admissions during lockdown compared to 18.1% the preceding year (p = 0.002) with 66.7% reduction in paediatric operations, from 18 to 6. There was a significant increase in median turnaround time (13 minutes (IQR 12 to 33) vs 60 minutes (IQR 41 to 71); p < 0.001) although there was no significant difference in the anaesthetic time or surgical time. There was a 38% (61 vs 38) decrease in trainee-led operations.
Discussion
The lockdown resulted in large decreases in referrals and admissions. Despite this, hip fracture admissions were unaffected and should remain a priority for trauma service planning in future lockdowns. As plans to resume normal elective and trauma services begin, hospitals should focus on minimising theatre turnaround time to maximize theatre efficiency while prioritizing training opportunities.
Clinical relevance
-
Lockdown has resulted in decreases in the trauma burden although hip fractures remain unaffected requiring priority
-
Theatre turnaround times and training opportunities are affected and should be optimised prior to the resumption of normal services.
Cite this article: Bone Joint Open 2020;1-8:494–499.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is one of the largest public health crises that we have faced, and has had a significant impact on the provision and delivery of healthcare worldwide.1 Like other countries, the response and message from the UK government to the public has centred around self-isolation and social distancing. The government introduced a lockdown on 23 March 2020, whereby the public were only permitted to leave the house to go to work if a key worker or unable to work from home, to buy food, or for up to one hour of exercise a day. Within hospitals, all elective orthopaedic operations were cancelled from mid-March in order to free up staff and space for the potential influx of patients suffering from COVID-19, as well as to protect patients and staff. While planned procedures have ceased, trauma services have continued.2
The British Orthopaedic Association (BOA) and NHS have produced guidance on the management of trauma patients in the UK with an emphasis on providing an acute trauma service while minimising operations that could potentially be delayed and to minimize admissions where feasible.3-5 The aim was to free up resources including bed space and anaesthetic staff as well as reduce the risk of disease transmission. Other measures, such as managing patients with suspected COVID-19 in separate theatres, have been undertaken, with the routine use of personal protective equipment for all orthopaedic operations. The impact of such changes is likely to impact the number of referrals, admissions, and operations and affect practicalities in theatre such as theatre time and training opportunities.
With the possibility of future infection peaks and the reinstatement of lockdown precautions, such knowledge would enable hospitals to optimise the delivery of trauma services as well as to plan for the challenges associated with the resumption of normal services. Therefore, the aim of this paper is to analyze the effect of the UK lockdown on trauma referrals, admissions and operations and to determine its impact on training opportunities and theatre efficiency at a large district general hospital.
Methods
The type of presentation and number of orthopaedic referrals to the on-call orthopaedic team, including the number of patients admitted under the orthopaedic team or sent home following review, were recorded during the periods 1 April to 30 April 2019 and compared to 1 April to 30 April 2020. The April 2019 data was collected retrospectively and the data during the lockdown period was collected prospectively. Data were collected at the completion of each 24 hour on-call period from a combination of the daily trauma meeting and the on-call orthopaedic trauma sheets, which record details of all patients referred to the on-call team requiring a review during a 24 hour period.
Using the hospital trauma software system (Bluespier International, Droitwich, UK), the number of patients who underwent an orthopaedic trauma operation and the type of operation were recorded during 1 April to 30 April 2020 and 1 April to 30 April 2019 along the seniority of the primary operating surgeon (consultant or trainee). The anaesthetic start time, time to enter the operating theatre, procedure completion time, and the time to leave the operating theatre were also recorded. Where any of these times were not recorded the entire dataset was excluded. The median length of theatre time was determined as the time of arrival to anaesthetic room to the time leaving the operating theatre. The anaesthetic time was recorded as the time of arrival to the anaesthetic room to the time of entering the operating room and the surgical time recorded as the time of entry to the operating room to the completion of procedure. The time to leave theatre was recorded as the time between completing the procedure and leaving the operating theatre. The ‘turnaround time’ was recorded as the time during which neither the operating theatre nor the anaesthetic room were being utilized. This consisted of the time between cases i.e. the time between the patient leaving the operating theatre and the next patient arriving in the anaesthetic room. For the first case of the day this was recorded as the time between the first patient day arriving in the anaesthetic room and the official daily start time (8:30 am). Eight cases were performed under local anaesthetic in April 2019 and none during April 2020, possibly due to a number of local anaesthetic procedures being managed in the emergency department. To avoid skewing results, cases completed under local anaesthetic only were not included.
The data were assessed for normal distribution using the Shapiro-Wilk test. Median and interquartile ranges (IQR) are presented for non-normally distributed data with differences compared using the Mann-Whitney U test. Means and standard deviations are presented for normally distributed data and compared using an independent-samples two tailed t-test. Categorical data were compared using Fisher’s exact test. All analyses were completed with SPSS v. 20 (IBM, Armonk, New York, USA). Results were deemed significant if p < 0.05.
Results
Referrals and admissions
There was a 26% reduction in the number of referrals in the April 2020 period compared to April 2019, from 303 patients to 224 patients, with a 37% reduction in admissions (177 in 2019 vs 112 in 2020; Figure 1). A higher proportion of patients were admitted in April 2019 compared to April 2020 (58% vs 50%) from 177 patients to 112 patients although this did not reach statistical significance (p = 0.063, Fisher's exact test). Similarly, a higher proportion of patients were sent home after review in the 2020 period compared to 2019 (33% (n = 74) vs 31% (n = 94); Figure 1).
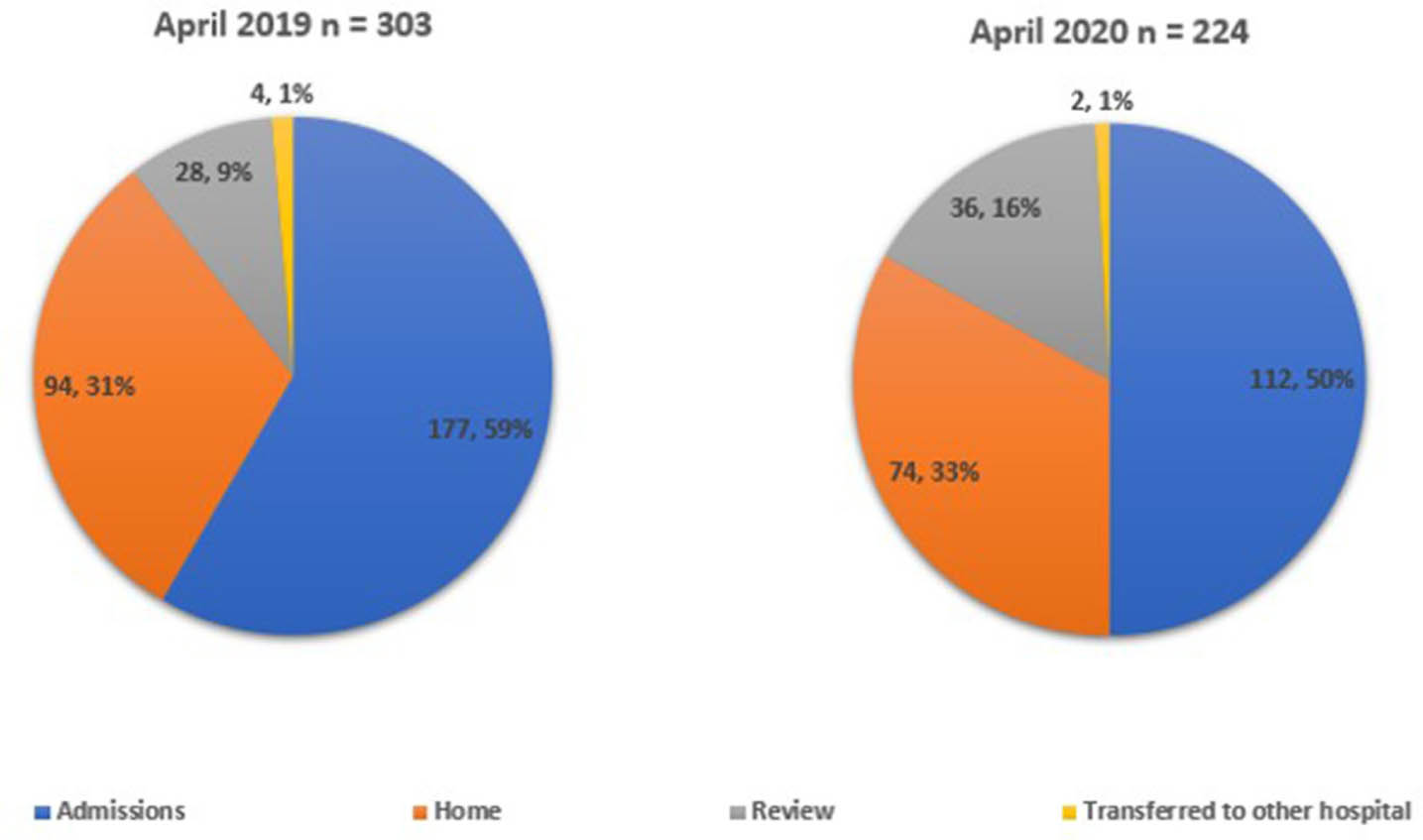
Fig. 1
Pie charts demonstrating patient referrals to the orthopaedic team and outcomes in April 2019 and April 2020.
Despite the overall reduction in patients admitted there was a 9% increase in hip fracture admissions from 34 to 37 patients and a 125% increase in head injury patient admissions from four to nine patients (Table I). The large reduction in overall admissions combined with a slight increase in hip fracture admissions resulted in hip fractures contributing to a significantly higher proportion of the total admissions in April 2020 compared to the preceding year (33% (n = 37) vs 19% (n = 34)) (p = 0.011, Fisher's exact test). Head injuries also increased between April 2019 to April 2020 as a proportion of total admissions from 2.3% to 8% (p = 0.037, Fisher's exact test) from four to nine patients.
Table I.
Admissions by presenting complaint in April 2019 and April 2020 and percentage change.
| Complaint | April 2019, n (%) (n = 177) | April 2020, n (%) (n = 112) | Percentage change |
|---|---|---|---|
| Atraumatic joint pain/swelling | 18 (10.2) | 7 (6.3) | −61.1 |
| Chest injury | 4 (2.3) | 4 (3.6) | 0.0 |
| Foreign body | 2 (1.1) | 0 (0) | −100.0 |
| Head injury | 4 (2.3) | 9 (8) | 125.0* |
| Hip fracture | 34 (19.2) | 37 (33) | 8.8* |
| Infection | 19 (10.7) | 10 (8.9) | −47.4 |
| Lower limb injury | 28 (15.8) | 19 (17.0) | −32.1 |
| Other | 3 (1.7) | 0 (0) | −100.0 |
| Post op | 1 (0.6) | 0 (0) | −100.0 |
| Soft tissue injury | 11 (6.2) | 5 (4.5) | −54.5 |
| Spine | 24 (13.6) | 12 (10.7) | −50.0 |
| Upper limb injury | 22 (12.4) | 7 (6.3) | −68.2 |
| Repat | 5 (2.8) | 0 (0) | −100.0 |
| Pelvic | 2 (1.1) | 2 (1.8) | 0.0 |
| Total | 177 | 112 | −36.7 |
-
*
Increase.
During this period there was also a significant decrease in the proportion of paediatric admissions from 18.1% in April 2019 to 8% in April 2020 whereas adult admissions increased as a proportion from 81.2% in April 2019 to 92% in April 2020 (p = 0.024, Fisher's exact test). There was an overall reduction of paediatric admissions by 71.9% compared to 29% in adults between April 2019 and April 2020 (Table II). There was a similar change in the number of paediatric operations compared to adult operations and although the change in the proportion of paediatric trauma cases compared to adult cases did not reach significance (p = 0081, Fisher's exact test), there was a 66.7% reduction in paediatric operations in this period. The median age of patients admitted in April 2019 was significantly lower at 57 (IQR 27 to 79.75) compared to 70.5 (IQR 46.25 to 84) years in April 2020 (p = 0.017, Mann-Whitney U Test).
Table II.
Paediatric and adult admissions and trauma operations in April 2019 and April 2020.
| Category | Admissions | Surgery | ||||
|---|---|---|---|---|---|---|
| April 2019 | April 2020 | Percentage change | April 2019 | April 2020 | Percentage change | |
| Paediatric, n (%) | 32 (18.1) | 9 (8) | −71.9 | 18 (14.5) | 6 (6.6) | −66.7 |
| Adult, n (%) | 145 (81.9) | 103 (92) | −29.0 | 106 (85.5) | 85 (93.4) | −19.8 |
| Total | 177 | 112 | −36.7 | 124 | 91 | −26.6 |
Operations
A total of 124 trauma operations were performed between 1 April and 30 April 2019 compared to 91 operations in the same period in 2020, a decrease of 26.6%. Despite this decrease, the number of hip fracture operations increased by one to 34 in April 2020 compared to 33 the year before (Figure 2). Three open long bone fractures were admitted and managed in April 2020 with no open fractures being referred to the orthopaedic team in 2019. The types of operations are detailed in Table III.
Table III.
Type of operations undertaken in April 2019 and April 2020 and percentage change.
| Type | April 2019, n (%) | April 2020, n (%) | Percentage change |
|---|---|---|---|
| MUA ± percutaneous pinning | 23 | 12 | −47.8 |
| External fixator/frame | 6 | 1 | −83.3 |
| Removal of metal | 1 | 0 | −100.0 |
| Soft tissues/other | 9 | 6 | −33.3 |
| ORIF | 24 | 25 | 4.2* |
| IM nail for NOF | 4 | 5 | 25.0* |
| DHS | 10 | 14 | 40.0* |
| Hemiarthroplasty | 11 | 8 | −27.3 |
| Joint aspiration/washout | 15 | 3 | −80.0 |
| THA | 8 | 6 | −25 |
| Hip revision | 3 | 0 | −100 |
| Tendon repair | 5 | 3 | −40.0 |
| IM nail other | 3 | 2 | −33.3 |
| Abscess I&D | 1 | 3 | 200.0* |
| Spine decompression | 1 | 3 | 200.0* |
| Total | 124 | 91 | −26.6 |
-
*
Increase.
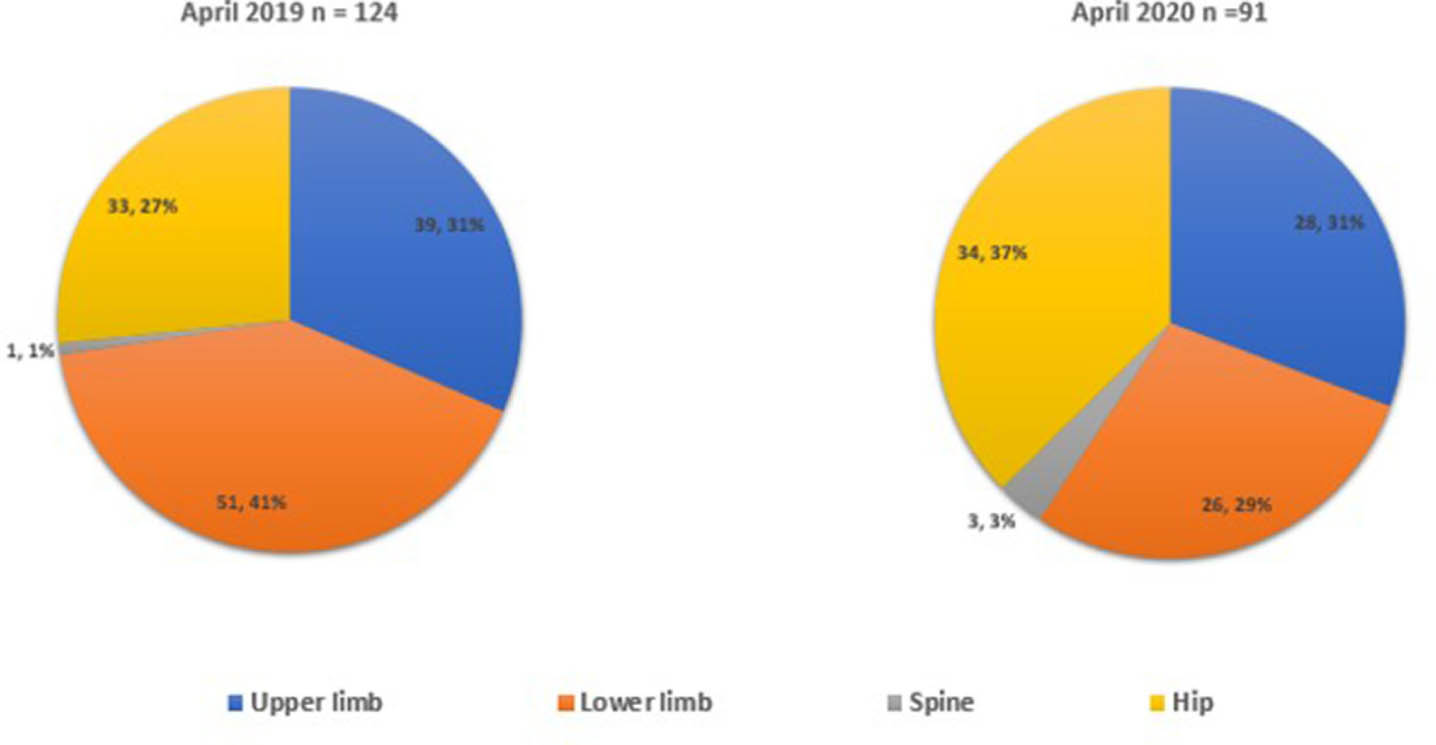
Fig. 2
Pie charts demonstrating site of operations during April 2019 and April 2020.
Primary surgeon and theatre time
Trainees were recorded as the primary surgeon in 61 of 124 trauma operations (51%) in April 2019 compared to 38 of 91 during lockdown (42%). Although the proportion of operations carried out by trainees did not change significantly (p = 0.209, Fisher's exact test), combined with a reduction in overall operations, this led to a 37.7% reduction in trainee performed operations (Table IV).
Table IV.
Recorded primary surgeon for trauma cases and percentage change between April 2019 and April 2020
| Primary surgeon | April 2019, n (%) | April 2020, n (%) | Percentage change |
|---|---|---|---|
| Consultant | 58 (49) | 53 (58) | −8.6 |
| Trainee | 61 (51) | 38 (42) | −37.7 |
| Not recorded | 5 (4) | 0 (0) | −100 |
| Total | 119 | 91 | −23.5 |
There was missing data regarding recorded surgical times for 10 patients in the April 2019 dataset with 8 patients having local anaesthetic procedures, whereas there was missing data for 45 patients in April 2020 with no local anaesthetic procedures. As such the theatre time data for 106 patients in April 2019 and 46 patients in April 2020 were recorded.
There was no significant change in median surgical time, median anaesthetic time or median total theatre time for trauma cases between April 2019 and April 2020 (Table V). There was, however, a significant increase in mean time to leave theatre in April 2020 of 6 minutes (IQR 4 to 9) compared to 8 minutes (IQR 7.25 to 23.75) in April 2019 (p < 0.001). Median turnaround time also increased significantly by 46.5 minutes from 13.0 minutes (IQR 12.0 to 33.0 minutes) in April 2019 to 59.5 minutes (40.50 to 71.25 minutes) during lockdown (p < 0.001).
Table V.
Median theatre time per trauma case compared between April 2019 and April 2020 with percentage change.
| Category | April 2019 (n = 106) | April 2020 (n = 46) | Percentage change | p-value* |
|---|---|---|---|---|
| Median anaesthetic mean time, mins (IQR) | 22 (15 to 34) | 22 (15 to 29) | −2.27 | 0.687 |
| Median surgical time, mins (IQR) | 81 (51 to 114) | 78 (50 to 108) | −3.70 | 0.890 |
| Median time to leave operating room, mins (IQR) | 6 (4 to 9) | 14 (7 to 24) | 133.33 | < 0.001 |
| Median total theatre time, mins (IQR) | 119 (82 to 154) | 122 (82 to 153) | 2.95 | 0.965 |
| Median turnaround time, mins (IQR) | 13 (2 to 33) | 60 (41 to 71) | 357.69 | < 0.001 |
-
*
Mann-Whitney U Test
-
IQR, interquartile range.
Discussion
This study demonstrates the UK lockdown has had a major impact on the trauma burden, training opportunities, and theatre efficiency at our institution. The large reduction in referrals (26%) and admissions (37%) seen correspond with the national decrease in accident and emergency department attendances and are likely a result of the nationwide lockdown measures during the COVID-19 crisis leading to fewer injuries with less patients willing to come to hospital with minor injuries.6 As a result of this, and the drive to manage patients nonoperatively where possible, we also saw a large reduction in trauma operations.
Despite the 37% reduction in trauma admissions, hip fractures were not affected with a 9% increase in hip fracture admissions. As a result, a significantly higher proportion of trauma operations carried out were for hip fractures during the lockdown. These findings highlight that fragility hip fractures in the elderly are unaffected by lockdown measures. As such, hip fracture services remain a priority during future lockdowns including the provision of orthogeriatric support as per the BOA guidance.3
There was a large decrease in paediatric admissions (71.9%) and operations (66.7%) during lockdown compared to the previous year. This decrease is larger than that seen in adults. The cause is likely multifactorial with closure of schools, social distancing, and overall lockdown measures reducing the incidence of paediatric trauma with some patients likely avoiding seeking medical attention in order to shield themselves from COVID-19. During the COVID-19 crisis there has also been a shift towards the nonoperative management of potentially suitable fractures, a strategy well-suited to the younger population due to their higher potential for bone remodelling.7 The long-term implications of the decrease in trauma operations in the paediatric population warrants future research to determine if this is due to a reduction in paediatric trauma or an increase in nonoperative management and if it is the latter, the long term implications of this.8 It may be beneficial to have specialist orthopaedic cover for minor injuries units in a future lockdown in order to maximize the quality of manipulations and casting in this population.
At our institution, head injuries are managed by the orthopaedic team with advice provided by the neurosurgical team from the major trauma centre, with patients requiring intervention transferred. We found an increase in head injuries admitted from four patients to nine patients. We also managed three long bone open fractures which would normally be directed to the major trauma centre as per the BOA guidelines.9 Due to an increased requirement to manage such patients locally, consideration should be given to early tertiary speciality input to district general hospitals in future pandemics to facilitate early appropriate management of such patients.10
During lockdown we demonstrated a 358% increase in the median patient turnaround time (13 minutes vs 60 minutes; p < 0.001) compared to the preceding year. This can be attributed to several reasons, such as deep-cleaning of theatres between cases, and porter precautions when collecting patients. Such increases are likely to translate to fewer completed cases per day. The theatre practice changes seen during lockdown are likely to continue for the foreseeable future. Theatre efficiencies will need to be maximized in order to cope with the increases in trauma that are likely to result from the relaxation of lockdown measures alongside the reinstatement of elective services.11,12 Furthermore, if theatre efficiency is affected during the resumption of normal services this will likely have a further negative effect on training opportunities. A small but significant increase was also seen in the time for patients to leave theatre due to patients being extubated in the operating room rather than recovery. We expected to see an increase in anaesthetic and surgical times due to time spent donning personal protective equipment although this was not seen, potentially due to an increased consultant presence.
There was a 38% reduction in trainee-performed trauma operations in April 2020 compared to April 2019. Combined with the cancellation of elective services and postgraduate examinations the long-term implications in the form of extension of training, achievement of required competencies, and time to certificate of completion of training remain to be seen. This has already been highlighted by relevant bodies such as the Joint Committee on Surgical Training (JCST), Health Education England and the four surgical Royal colleges.10 As we try to resume normal services, attention should be given to training needs with other avenues in the form of simulation-based training or webinar teaching.13
With regards to the data on theatre times, four times were recorded on our theatre management software for patients; the time they entered the anaesthetic room, the time they entered the operating theatre, the procedure completion time, and the time they left the operating theatre. Where one of these times were not recorded, we decided to not use any of the times for that operation for our data analysis. This resulted in the theatre times not being used for several patients. This is a limitation of our study; however, by omitting all the time entries for the operations whereby a single data entry was missing, we aimed to limit any inaccuracies or inconsistencies in the data analysis. This occurred more in the April 2020 data possibly due to the theatre staff being preoccupied with the new changes and challenges of facilitating operations during the COVID-19 pandemic, such as the use of PPE, and hence giving less importance to recording all the theatre time entries.
By describing the effect of the UK lockdown on trends in trauma in a large district general hospital, this study aims to address the need to effectively plan and prioritise trauma service provisions in future lockdowns. To our knowledge this is the first study to describe the impact of the COVID-19 on orthopaedic theatre efficiency and training opportunities. Although this is a single-centre study, our findings are likely generalizable to other UK hospitals as our hospital is one of the largest district general hospitals in the UK.14 We also aimed to obtain data over a 30-day period in order to fully capture the effect of the lockdown on trauma service provisions over a time period where infections and lockdown measures were at their peak.15 To ensure our data collection was robust we cross-checked data from the on-call referral sheets and our theatre management record system. We also ensured the April 2020 on-call referral sheets were accurate by cross-checking patients with the on-call team at the daily trauma meeting and found no errors. Although this was not possible with the retrospectively collected April 2019 data, we can be confident that this data is also accurate.
As the COVID-19 crisis continues to unfold and the UK government begins to cautiously ease lockdown measures, there is a very real possibility of a second or even multiple further waves of infection. Our study provides data on observed trends of trauma workload at a district general hospital during a 30 day period when rates of infection and deaths attributed to COVID-19 were at its highest, comparing to the same time period one year ago without the burden of COVID-19. We recommend multidisciplinary hip fracture management services to remain in place and prioritised in future lockdowns. Theatre efficiency should also be optimized to minimize procedure turnaround time in preparation for the normalization of trauma and elective services with a priority placed on training opportunities.
References
1. Zhu N , Zhang D , Wang W , et al. A novel coronavirus from patients with pneumonia in China, 2019 . N Engl J Med . 2020 ; 382 ( 8 ): 727 – 733 . Crossref PubMed Google Scholar
2. COVIDSurg Collaborative . Global guidance for surgical care during the COVID-19 pandemic . Br Jour Surg . 2020 ; 23 . Crossref PubMed Google Scholar
3. No authors listed . BOAST Guidelines: Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic . British Orthopaedic Association . https://www.boa.ac.uk/resources/covid-19-boasts-combined.html (date last accessed 03 July 2020). Google Scholar
4. NHS England . Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic. [Online] Available from . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0274-Specialty-guide-Orthopaedic-trauma-v2-14-April.pdf Google Scholar
5. NHS England . Clinical guide for the perioperative care of people with fragility fractures during the coronavirus pandemic . 2020 . https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0086_Specialty-guide-_Fragility-Fractures-and-Coronavirus-v1-26-March.pdf (date last accessed 03 July 2020). Google Scholar
6. No authors listed . Emergency Department: Weekly Bulletins . Public Health England . 2020 . https://www.gov.uk/government/publications/emergency-department-weekly-bulletins-for-2020 (date last accessed 3 July 2020). Google Scholar
7. Wilkins KE . Principles of fracture remodeling in children . Injury . 2005 ; 36 ( 1 ): S3 – S11 . Crossref PubMed Google Scholar
8. Kosuge D , Barry M . Changing trends in the management of children’s fractures . Bone Joint J . 2015 ; 97-B ( 4 ): 442 – 448 . Google Scholar
9. British Orthopaedic Association . BOAST: Open Fractures. [Online] Available from . https://www.boa.ac.uk/resources/boast-4-pdf.html Google Scholar
10. Joint Commitee on Surgical Training . COVID 19: JCST Statement 19 March 2020. [Online] Available from . https://www.jcst.org/jcst-news/2020/03/19/covid-19/ (date last accessed Accessed March 2020). Google Scholar
11. Fletcher D , Edwards D , Tolchard S , Baker R , Berstock J . Improving theatre turnaround time . BMJ Qual Improv Rep . 2017 ; 6 ( 1 ) pp .: u219831.w8131 . Crossref PubMed Google Scholar
12. Roberts S , Saithna A , Bethune R . Improving theatre efficiency and utilisation through early identification of trauma patients and enhanced communication between teams . BMJ Quality Improvement Reports . 2015 ; 4 ( 1 ) pp .: u206641.w2670 . Crossref PubMed Google Scholar
13. Ali SR , Dobbs TD , Whitaker IS . Webinars in plastic and reconstructive surgery training - a review of the current landscape during the COVID-19 pandemic . J Plast Reconstr Aesthet Surg . 2020 ; 73 ( 7 ): 1357 – 1404 . Crossref PubMed Google Scholar
14. Royal Berkshire NHS Trust . Royal Berkshire Research and Development Page. [Online] Available from . https://www.royalberkshire.nhs.uk/For-Industry.htm Google Scholar
15. No authors listed . Corononavirus (COVID19) Cases in the UK . Public Health England . 2020 . https://coronavirus.data.gov.uk/ Google Scholar
Author contributions
M. Karia: Designed the study, Carried out data collection and analysis, Wrote the manuscript.
V. Gupta: Carried out data collection and analysis, Wrote the manuscript.
W. Zahra: Carried out data collection and analysis, Edited and reviewed the manuscript.
J. Dixon: Carried out data collection and analysis, Edited and reviewed the manuscript.
E. Tayton: Supervised the study and edited and reviewed the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Follow M. Karia @monilk24
Follow W. Zahra @zahra_wajiha
Follow E. Tayton @EdTaytonOrtho
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









