Abstract
Aims
The aim of this study is to report the results of a case series of olecranon fractures and olecranon osteotomies treated with two bicortical screws.
Methods
Data was collected retrospectively for all olecranon fractures and osteotomies fixed with two bicortical screws between January 2008 and December 2019 at our institution. The following outcome measures were assessed; re-operation, complications, radiological loss of reduction, and elbow range of flexion-extension.
Results
Bicortical screw fixation was used to treat 17 olecranon fractures and ten osteotomies. The mean age of patients being treated for olecranon fracture and osteotomy were 48.6 years and 52.7 years respectively. Overall, 18% of olecranon fractures were classified as Mayo type I, 71% type II, and 12% type III. No cases of fracture or osteotomy required operative re-intervention. There were two cases of loss of fracture reduction which occurred in female patients ≥ 75 years of age with osteoporotic bone. In both cases, active extension and a functional range of movement was maintained and so the loss of reduction was managed non-operatively. For the fracture fixation cohort, at final follow-up mean elbow extension and flexion were -5° ± 5° and 136° ± 7°, with a mean arc of motion of 131° ± 11°.
Conclusion
This series has shown that patients regain near full range of elbow flexion-extension and complication rates are low following bicortical screw fixation of olecranon fractures and osteotomy.
Cite this article: Bone Joint Open 2020;1-7:376–382.
Introduction
Minimally displaced olecranon fractures (Mayo Type I) can be treated non-operatively, provided there is no displacement with active extension.1 Displaced, non-comminuted fractures (Mayo Type IIA) are the most common type, accounting for 60% of olecranon fractures, and are akin to olecranon osteotomy.2 Operative fixation is recommended for most displaced fractures. The objectives of operative intervention are anatomical reduction of the olecranon sigmoid notch, stable fixation, early mobilization, and evasion of complications.
The most common operative intervention for Type IIA olecranon fractures is tension band wiring (TBW) with Kirschner wires (K-wires).3 It was first described by Weber and Vasey4,5 in 1963, popularized by AO (Arbeitsgemeinschaft für Osteosynthesefragen) and remains the benchmark that new methods of fixation are compared against. A tension band works by converting tensile forces to compressive forces by shifting the centre of rotation towards the tension band. TBW fixation of olecranon fractures relies on a non-comminuted articular surface and so comminuted and unstable (Type IIB and Type III) fractures are usually treated with plate fixation.6
Complication rates following olecranon fracture TBW fixation are high and so multiple authors have suggested alternative techniques to improve patient outcomes.5,7-12 The main issues associated with TBW fixation are loss of reduction, non- or malunion, K-wire migration and discomfort from prominent metalwork. Alternatives to TBW fixation are plate fixation and a single intramedullary bone screws which can be performed in combination with a tension band .13 However, these alternative methods of fixation are not free from complications and a Cochrane review of surgical interventions for olecranon fracture concluded that there was not sufficient evidence to establish best treatment for olecranon fractures.3
In 1973, Wadsworth14 described the use of a single lag screw perpendicular to the fracture line gaining purchase in the anterior cortex of the ulna for olecranon fracture fixation. A specific ‘olecranon’ screw was developed for this purpose; however, this technique did not gain popularity.15 More recently, a variation of this technique has been described using two bicortical screws passing across the fracture site and through the anterior cortex of the ulna to achieve interfragmentary compression and rotational stability.16,17 The reported results of fixation with two bicortical screws for olecranon fracture are promising with lower complication rates than TBW fixation.16-18 The aim of this study is to report the results of a case series of olecranon fractures and olecranon osteotomies treated with two bicortical screws.
Methods
Data was collected retrospectively for all olecranon fractures and olecranon osteotomies that were fixed with two bicortical screws between January 2008 and December 2019 at our institution. The patients’ electronic notes were reviewed to record demographic data, fracture classification, operative details, postoperative elbow range of movement, and complications. Radiographs were reviewed to classify fracture type and assess trajectory of screw fixation in the sagittal plane, measured from the posterior cortical surface of the ulna and to assess for postoperative loss of reduction (Figure 1). All olecranon fractures were classified using the Mayo classification.1 The following outcome measures were assessed; re-operation, complications, radiological loss of reduction, and elbow range of flexion-extension. Data collection and descriptive statistics were performed with Excel version 16 (Microsoft, Redmond, Washington, USA).

Fig. 1
Angle measured between bicortical screw and dorsal cortex of ulna.
Surgical technique
Bicortical screw fixation was performed with two 4.0 mm partially threaded cannulated screws and washers (Smith and Nephew, Memphis, Tennessee, USA). All procedures were performed or supervised by the senior surgeon. After the induction of general anaesthesia, the patient is placed in the lateral decubitus position with the arm placed over an L-bar. A curvilinear posterior midline incision is used, and the incision is curved to the radial side over the olecranon to avoid placing the scar directly over the prominence of the tip of the olecranon.
In the case of olecranon fracture, the fracture site is exposed and cleared of bone debris, haematoma and soft tissue. Hereafter, the technique for fixation of olecranon fracture and osteotomy are identical. The fracture is reduced and then held with the reduction clamp inserted into a drill hole on the posterior cortex of the ulna. With the reduction forceps applied, two 1.3 mm guide wires are inserted into the olecranon across the fracture site, aiming to pass just underneath the articular surface of the sigmoid notch and penetrate the anterior cortex of the olecranon close to the base of the coronoid. In the coronal plane, the wires should be aimed along the longitudinal axis of the ulna. The guide wires should be parallel and spaced approximately 10 mm apart in transverse plain. In order to select the correct screw length, the guide wires should be inserted so that they just penetrate the anterior cortex of the ulna. The cannulated screws should be inserted sequentially by drilling over one wire, inserting the appropriate length screw and washer before drilling over the second guide wire. The screws should be inserted to achieve finger tight compression.
Screw position should be checked with image intensifier. Fracture fixation stability is assessed through a full arc of flexion and extension under image intensifier (Figure 2). Range of pronation and supination are also checked to ensure there is no impingement of the distal tip of the screw in the proximal radioulnar joint. The wound is irrigated and closed in layers. In most cases, the elbow is dressed with a bulky bandage and a collar and cuff sling is applied. In the case of minimally displaced olecranon fractures, a percutaneous technique can be performed. This involves making four separate stab incisions; two for the application of the bone reduction clamp and two for screw insertion.

Fig. 2
Intra-operative assessment of fracture bicortical screw fixation stability with image intensifier: a) flexion; b) extension; c) anteroposterior.
The postoperative protocol is for commencement of active range of movement exercises after attending clinic for a wound check ten to 14 days after surgery. Patients were advised against heavy lifting or resisted extension for at least six weeks. Routine radiographs of the elbow are performed six weeks postoperatively and patients are followed-up in the outpatient clinic by an orthopaedic surgeon until union is confirmed radiologically or clinically.
Results
Between January 2008 and December 2019, there were 27 cases of olecranon fixation utilizing two bicortical screws. Bicortical screw fixation was used to treat 17 olecranon fractures and following ten chevron olecranon osteotomies performed to approach distal humeri intra-articular fractures (Figure 3). The patient, fracture, and fixation characteristics of all cases are displayed in Table I. The mean age of males compared to females was less for both the olecranon fracture and olecranon osteotomy groups; 39.2 years versus 59.1 years, and 40.5 years versus 60.4 years. One case of bicortical screw olecranon fracture fixation was a successful revision procedure for a Mayo IIA olecranon fracture which had been fixed with TBW but subsequently lost reduction.
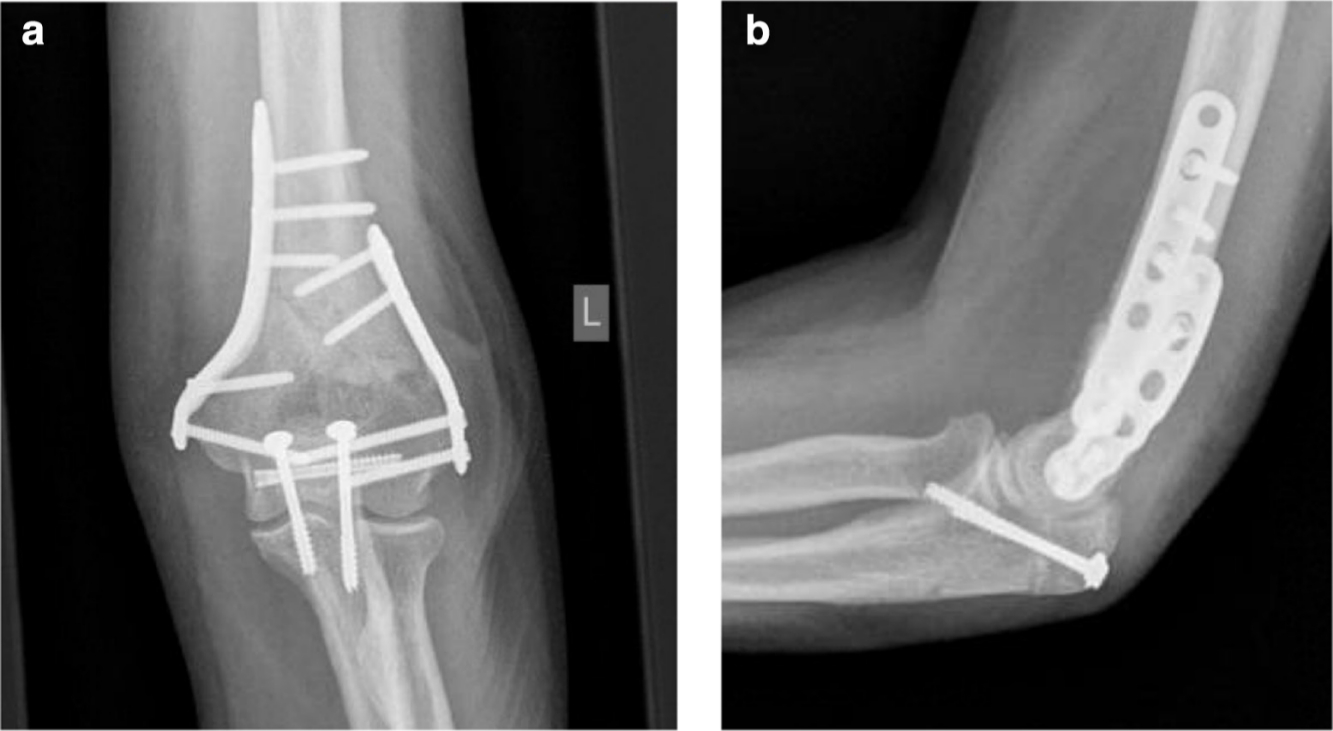
Fig. 3
Radiographs of bicortical screw fixation of olecranon osteotomy: a) anteroposterior; b) lateral.
Table I.
Patient, fracture, and fixation characteristics.
| Variables | Olecranon fracture (n = 17) | Olecranon osteotomy (n = 10) |
|---|---|---|
| Age (years), mean ± SD | 48.6 ± 25.1 | 52.7 ± 25.4 |
| Range | 16.2 to 81.5 | 22.5 to 87.3 |
| Sex, male % | 52.9 | 55.6 |
| Laterality, right % | 47.1 | 44.4 |
| Mayo fracture classification | ||
| IA (%) | 11.8 | N/A |
| IB (%) | 5.9 | N/A |
| IIA (%) | 52.9 | N/A |
| IIB (%) | 17.6 | N/A |
| IIIA (%) | 0 | N/A |
| IIB (%) | 11.8 | N/A |
| Time from diagnosis to fixation (hours), mean ± SD | 31 ± 30 | 41 ± 32 |
| Screw angle (°), mean ± SD | 23.4 ± 6.4 | 28.7 ± 2.8 |
Two cases of olecranon fracture and one case of osteotomy were not local residents to our institution and so following operative intervention they did not attend outpatient follow-up. There was one postoperative death two weeks following open reduction and internal fixation of distal humeri fracture utilizing an olecranon osteotomy. The cause of death was pulmonary oedema in an 87-year-old female patient. There was one case of superficial wound infection which was successfully treated with antibiotics in a patient treated for olecranon fracture. This occurred in a 77-year-old female, who at the time of olecranon fracture also suffered an ipsilateral surgical neck of humeri fracture which was managed non-operatively.
No cases in either the olecranon fracture or osteotomy group required revision intervention. There were no cases of loss of reduction in the olecranon osteotomy cohort and two in the olecranon fracture cohort. In total, two cases out of 15 (13%) which were follow-up until union suffered loss of reduction. One case of loss of reduction occurred in an 81-year-old female with a Mayo IIA olecranon fracture; her past medical history included osteoporosis, and she suffered a fall four weeks post-fixation, which resulted in loss of reduction (Figure 4). The second case of loss of reduction occurred in a 77-year-old female and was detected with radiographs two weeks postoperatively. In both cases, revision fixation was considered; however, active extension and a functional range of movement was maintained and so the loss of reduction was managed non-operatively.

Fig. 4
Lateral radiographs of elbow: a) displaced olecranon fracture (Mayo IIA); b) postoperative fixation with two bicortical screws; c) loss of reduction.
A percutaneous approach was used for three cases, all of which were minimally displaced olecranon fractures. In one of these cases, the patient, a 19-year-old male, suffered a fall playing football five weeks post-fracture fixation and broke one of the bicortical screws (Figure 5). There was no loss of reduction and full range of flexion-extension (0° to 140°) was preserved and so no surgical intervention was required.
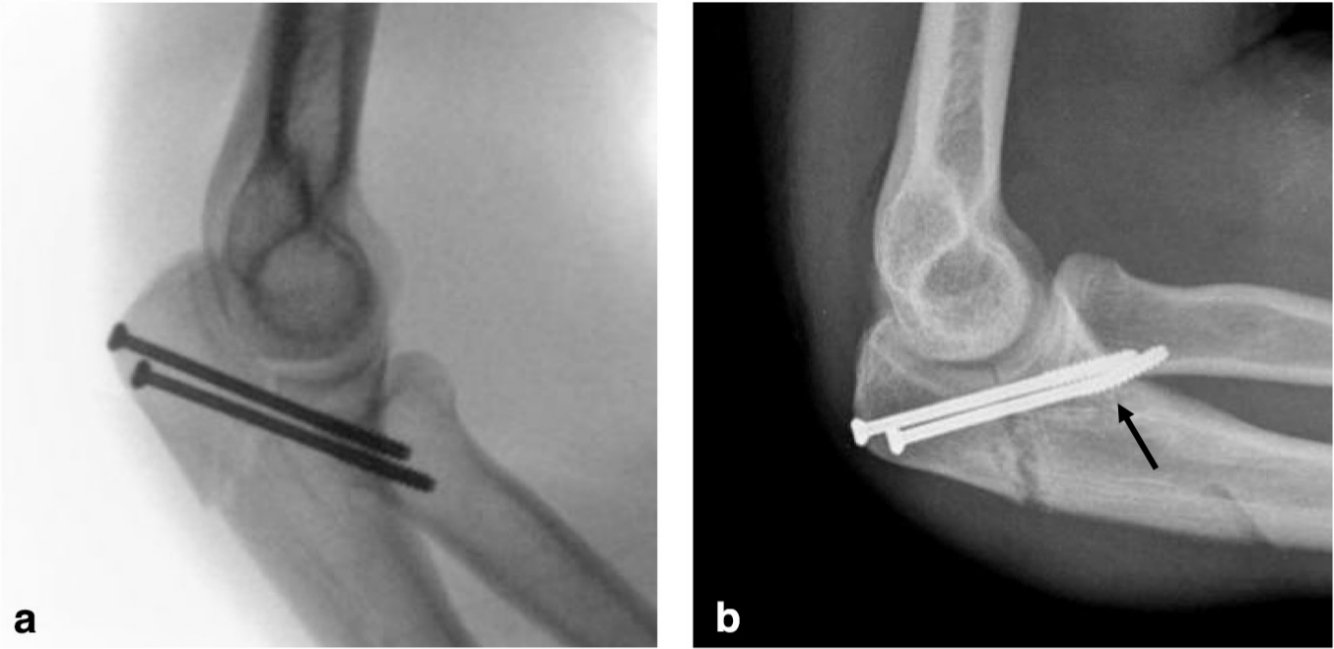
Fig. 5
a) image intensifier lateral of percutaneous olecranon fracture fixation with bicortical screws; b) lateral radiograph of elbow showing fracture of inferior screw indicated by arrow.
For the fracture fixation cohort, all patients apart from the two cases of loss of reduction had united at final follow-up which, was at a mean of 12.9 weeks after fracture fixation. Mean elbow extension and flexion at final follow-up were -5° ± 5° and 136° ± 7°, which gives a mean arc of motion of 131° ± 11°.
Discussion
The key findings of this study are that no cases of olecranon fixation with bicortical screws required revision surgery, there were two cases (13%) loss of reduction in the fracture fixation group and patients regain excellent range of elbow flexion-extension.
Apart from the previous publication by the senior author, there are only two other publications which report the clinical results of bicortical screw fixation of olecranon fractures and the results were equally as promising as those reported in the present study.16-18 Uhlmann et al17 reported the results of a prospective series of 13 Schatzker type A (minimally displaced, transverse) olecranon fractures treated with percutaneous bicortical screw fixation these were compared to a control group of 26 patients treated with TBW fixation. The mean and maximum ages of patients treated in Ullmann et al’s series with bicortical screws was 43.6 years and 67.1 years, which was less than those treated in the present series. For bicortical compared to TBW fixation, Uhlmann et al reported no intra-operative complications, half the rate of metalwork removal (38.5% vs 73.1%) and a superior arc of flexion (145° vs 130°) (p < 0.001). In the present study, a percutaneous technique was utilized for three cases, the broken screw which occurred in one of these cases was not thought to be linked to the percutaneous technique. The higher rate of metalwork removal reported by Ullmann et al compared to the present study could be due to the cultural, economic and geographical variations in surgical practice between Germany and the UK.17
Bhattacharyya et al18 conducted a randomized controlled trial (RCT) of TBW versus bicortical screw fixation for transverse olecranon fractures in patients between the ages of 18 years and 70 years. In all, 20 patients were randomized to each treatment group. Bhattacharyya et al did not report any cases of loss of reduction or re-operation in the bicortical screw fixation group.18
In the present study, no cases required re-operation for removal of metalwork or revision fixation. The two cases of loss of reduction occurred in patients > 75 years with osteoporotic bone. Because of age, neither of these patients would have been included in the RCT performed by Bhattacharyya et al.18 One of the cases of loss of reduction occurred as the result of a further fall four weeks postoperatively and screw insertion too close to the fracture (Figure 4). On review of the intra-operative imaging, the second case of loss of reduction may have been caused by suboptimal placement of one of the bicortical screws resulting in compromised screw thread hold on the anterior ulna cortex.
Loss of reduction and metalwork complications following olecranon fixation are extremely common. Numerous studies have reported high complications rates following TBW fixation.5,7-12 In some series, prominent metalwork has been reported in up to 82% of cases, metalwork removal in up to 81% of cases and loss of reduction in up to 63% of cases.5,11,12 Rommens et al19 recommend routine TBW metal work removal after fracture union due to the incidence of patient dissatisfaction related to the implant. Van der Linden et al11 performed a retrospective review of 59 olecranon fractures treated with TBW and showed that K-wire instability, evidenced by a fracture gap occurred in 78% of cases when the K-wires were intramedullary compared to in 36% of cases with bicortical K-wire positioning. Chalidis et al5 conducted a retrospective review of 62 cases of TBW fixation and despite reporting prominent, symptomatic metalwork in 82% of cases, reported good to excellent Mayo Elbow Performance Scores in 86%. Chalidis et al went on to conclude that TBW fixation remains the “gold standard” for the treatment of displaced and minimally comminuted olecranon fractures.5 The range of movement recovery reported in our study is in line with range of movement reported following bicortical screw and TBW fixation in the literature.11,12,17 Van der Linden et al and Karlsoon et al12 in separate studies reported average arcs of flexion-extension of 128° and 134° respectively.11,12
A biomechanical study has shown olecranon fracture fixation with two bicortical screws to be equivalent to TBW fixation. Jones et al20 performed a biomechanical study comparing TBW to bicortical screw fixation in 25 synthetic ulnae. They concluded that in a synthetic bone model of simple transverse olecranon fractures, bicortical screw fixation provided equivalent strength as compared with TBW.20 Jones et al used a similar fixation technique to that described in our study and reported a screw insertion angle of 20°. This is comparable to the mean screw insertion angle for olecranon fracture fixation in the present study which was 23.4° ± 6.4°. In the present study, screw insertion angle varied depending on the morphology of the proximal ulna and fracture.
The complication rate following TBW fixation of olecranon fracture in elderly patients are so high that a number of authors advocate non-operative management for this group of patients with satisfactory results.21-23 Duckworth et al24 conducted a RCT comparing TBW versus non-operative management for patients ≥ 75 years with an olecranon fracture. The trial was stopped prematurely as the rate of complications was 9/11 (81.8%) in the TBW fixation group. The present study included five patients ≥ 75 years and fixation failed in two of these cases. Patients ≥ 75 years with an olecranon fracture remain a challenging group to treat operatively, regardless of technique because of the poor quality of bone.
Plate fixation of olecranon fractures also has limitations. In a recent RCT comparing TBW to plate fixation in patients ≤ 75 years, Duckworth et al25 reported a 63% complication rate associated with TBW fixation compared to 38% associated with plate fixation. Removal of symptomatic metalwork was 50% vs 22% for TBW versus plate osteosynthesis and loss of reduction was 27% vs 13%. Four infections of which two required surgical intervention and three revision surgeries were performed in the plate group compared to none in the TBW group. The authors concluded that although complications were more frequent in the TBW group more serious complications occurred following plate fixation. Although locking plates are more expensive, Duckworth et al did not find a significant difference in the total cost of care per patient compared to fixation with TBW.25 Cannulated screws are significantly cheaper than olecranon specific locking plates and non-cannulated screws are a cheaper alternative for bicortical screw fixation.
Bicortical screw fixation of olecranon osteotomy has not been described in the literature outside of this series, Ulmann et al and Bhattacharyya et al reported on cases of olecranon fracture fixation with two bicortical screws but not fixation of olecranon osteotomy.16 Ocalan et al reported the results of olecranon osteotomy fixation with TBW in 22, intramedullary screws in 11 and plate fixation in four cases.26 Implant removal was performed in 18% of TBW, 18% of intramedullary screw fixation and 75% of plate fixation, with an overall removal rate of 24.3%.26 Hewins et al27 reported plate fixation of 17 olecranon osteotomies using a contoured 3.5 mm reconstruction plate and reported one case of revision for a screw which was too long and had penetrated the radioulnar joint and one case of plate removal for prominent symptomatic metalwork. The present study reported no cases of loss of reduction or requirement for metalwork removal following olecranon osteotomy fixation with two bicortical screw. Range of elbow motions following olecranon osteotomy is likely influenced most by severity and successful reduction of the intra-articular distal humeri fracture and so is not a good marker with which to judge outcome of olecranon osteotomy fixation.
Bicortical screw fixation has several advantages over TBW fixation. Firstly, it is safe and has been shown to have a low complication and re-operation rate.16-18 Secondly, unlike both TBW and plate fixation there is no metalwork overlying the subcutaneous dorsal proximal ulna which is often a source of discomfort if present. Thirdly, in the case of minimally displaced olecranon fractures it can be performed percutaneously.16,17 And finally, unlike TBW, it is not a difficult technique to learn how to perform. Schneider et al28 conducted a retrospective radiological review of 239 olecranon fractures fixed with TBW and revealed an average of 4.2 imperfections in TBW construct per intervention, they concluded that TBW fixation is not as easy as surgeons and the literature suggest.
This study has a number of limitations. Firstly, it is a retrospective case series and secondly the numbers included in the study are relatively small. Further research is required to determine the outcome, complication rate and reliability of this procedure when used more widely.
In conclusion, olecranon fixation performed with two bicortical screws is safe for treating olecranon fractures and osteotomies. This case series has shown that patients regain near full range of elbow flexion-extension, fixation of minimally displaced fractures can be performed via a percutaneous approach, and complication and reintervention rates are low.
References
1. Cabanela M , Morrey B . The Elbow and Its Disorders. Philidelphia PA , ed . 2nd . USA : WB Saunders , 1993 . Google Scholar
2. Duckworth AD , Clement ND , Aitken SA , et al. The epidemiology of fractures of the proximal ulna . Injury . 2012 ; 43 ( 3 ): 343 – 346 . Crossref PubMed Google Scholar
3. Matar HE , Ali AA , Buckley S , et al. Surgical interventions for treating fractures of the olecranon in adults . Cochrane Database Syst Rev . 2014 ; 2014 ( 11 ): CD010144 . Crossref PubMed Google Scholar
4. Weber BG , Vasey H . [Osteosynthesis in Olecranon Fractures] . Z Unfallmed Berufskr . 1963 ; 56 : 90 – 96 . Google Scholar
5. Chalidis BE , Sachinis NC , Samoladas EP , et al. Is tension band wiring technique the ‘gold standard’ for the treatment of olecranon fractures? A long term functional outcome study . J Orthop Surg Res . 2008 ; 3 : 9 . Google Scholar
6. Newman SDS , Mauffrey C , Krikler S . Olecranon fractures . Injury . 2009 ; 40 ( 6 ): 575 – 581 . Crossref PubMed Google Scholar
7. Holdsworth BJ , Mossad MM . Elbow function following tension band fixation of displaced fractures of the olecranon . Injury . 1984 ; 16 ( 3 ): 182 – 187 . Crossref PubMed Google Scholar
8. Wolfgang G , Burke F , Bush D , et al. Surgical treatment of displaced olecranon fractures by tension band wiring technique . Clin Orthop Relat Res . 1987 ( 224 ): 192 – 204 . PubMed Google Scholar
9. Hume MC , Wiss DA . Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation . Clin Orthop Relat Res . 1992 ( 285 ): 229 – 235 . PubMed Google Scholar
10. Ahmed AR , Sweed T , Wanas A . The role of cancellous screw with tension band fixation in the treatment of displaced olecranon fractures, a comparative study . Eur J Orthop Surg Traumatol . 2008 ; 18 ( 8 ): 571 – 576 . Google Scholar
11. van der Linden SC , van Kampen A , Jaarsma RL . K-wire position in tension-band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures . J Shoulder Elb Surg . 2012 ; 21 ( 3 ): 405 – 411 . Crossref PubMed Google Scholar
12. Karlsson MK , Hasserius R , Besjakov J , et al. Comparison of tension-band and figure-of-eight wiring techniques for treatment of olecranon fractures . J Shoulder Elb Surg . 2002 ; 11 ( 4 ): 377 – 382 . Crossref PubMed Google Scholar
13. MacAusland WR . The Treatement of Fractures of the Olecranon by Longitudinal Screw or Nail Fixation . Ann Surg . 1942 ; 116 ( 2 ): 293 – 296 . Google Scholar
14. Wadsworth TG . Screw fixation of the olecranon after fracture or osteotomy . Clin Orthop Relat Res . 1976 ; 119 : 197 – 201 . Google Scholar
15. Wadsworth TG . Screw fixation of the olecranon . Lancet . 1976 ; 2 ( 7995 ): 1118 – 1119 . Google Scholar
16. Haddad B , Khan W , Zaghloul A , et al. Fixation of olecranon fractures and osteotomies using compression screws: A simple solution to a common problem. A study of cases . Ortop Traumatol Rehabil . 2013 ; 15 ( 4 ): 341 – 346 . Crossref PubMed Google Scholar
17. Uhlmann M , Barg A , Valderrabano V , et al. Behandlung von isolierten Olekranonfrakturen: Perkutane Doppelschraubenosteosynthese vs. konventionelle Zuggurtung . Unfallchirurg . 2014 ; 117 : 614 – 623 . Google Scholar
18. Bhattacharyya DTD , Frank DHC , Hazarika DK , Mittal DS , et al. Treatment of transverse olecranon fractures: comparison between tension band wiring and transcortical screw . IOSR . 2016 ; 15 ( 09 ): 93 – 96 . Google Scholar
19. Rommens PM , Küchle R , Schneider RU , Reuter M . Olecranon fractures in adults: Factors influencing outcome . Injury . 2004 ; 35 ( 11 ): 1149 – 1157 . Crossref PubMed Google Scholar
20. Jones TB , Karenz AR , Weinhold PS , Dahners LE . Transcortical screw fixation of the olecranon shows equivalent strength and improved stability compared with tension band fixation . J Orthop Trauma . 2014 ; 28 ( 3 ): 137 – 142 . Crossref PubMed Google Scholar
21. Parker MJ , Richmond PW , Andrew TA , Bewes PC . A review of displaced olecranon fractures treated conservatively . J R Coll Surg Edinb . 1990 ; 35 ( 6 ): 392 – 394 . PubMed Google Scholar
22. Bruinsma W , Lindenhovius A , Mckee M , et al. Non-Union of Non-operatively treated displaced olecranon fractures . Shoulder Elbow . 2012 ; 4 : 273 – 276 . Google Scholar
23. Duckworth AD , Bugler KE , Clement ND , et al. Nonoperative management of displaced olecranon fractures in low-demand elderly patients . J Bone Joint Surg Am . 2014 ; 96 ( 1 ): 67 – 72 . Crossref PubMed Google Scholar
24. Duckworth AD , Clement ND , McEachan JE , et al. Prospective randomised trial of nonoperative versus operative management of olecranon fractures in the elderly . Bone Jt J . 2017 ; 99B : 964 – 972 . Google Scholar
25. Duckworth AD , Clement ND , White TO , et al. Plate versus Tension-Band wire fixation for olecranon fractures . The Journal of Bone and Joint Surgery . 2017 ; 99 ( 15 ): 1261 – 1273 . Crossref PubMed Google Scholar
26. Ocalan HI , Karakus O , Karakurum G . Comparison of olecranon fixation techniques following transolecranon approach in intra-articular fractures of distal humerus in adult patients . J Orthop Trauma Rehabil . 2019 . Google Scholar
27. Hewins EA , Gofton WT , Dubberly J , et al. Plate fixation of olecranon osteotomies . J Orthop Trauma . 2007 ; 21 ( 1 ): 58 – 62 . Crossref PubMed Google Scholar
28. Schneider MM , Nowak TE , Bastian L , et al. Tension band wiring in olecranon fractures: The myth of technical simplicity and osteosynthetical perfection . Int Orthop . 2014 ; 38 ( 4 ): 847 – 855 . Crossref PubMed Google Scholar
Author contributions
J. R. Gill: Designed the study, Collected, analyzed, and interpreted the data, Wrote and edited the manuscript.
L. Vermuyten: Designed the study, Collected, analyzed, and interpreted the data, Edited the manuscript.
S. A. Schenk: Designed the study, Collected, analyzed, and interpreted the data, Edited the manuscript.
J. C. Y. Ong: Designed the study, Collected, analyzed, and interpreted the data, Edited the manuscript.
W. Schenk: Developed the surgical technique, Designed the study, Analyzed and interpreted the data, Edited the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Follow J. R. Gill @james_r_gill









