Abstract
Aims
Elective operating was halted during the COVID-19 pandemic to increase the capacity to provide care to an unprecedented volume of critically unwell patients. During the pandemic, the orthopaedic department at the Aneurin Bevan University Health Board restructured the trauma service, relocating semi-urgent ambulatory trauma operating to the isolated clean elective centre (St. Woolos’ Hospital) from the main hospital receiving COVID-19 patients (Royal Gwent Hospital). This study presents our experience of providing semi-urgent trauma care in a COVID-19-free surgical unit as a safe way to treat trauma patients during the pandemic and a potential model for restarting an elective orthopaedic service.
Methods
All patients undergoing surgery during the COVID-19 pandemic at the orthopaedic surgical unit (OSU) in St. Woolos’ Hospital from 23 March 2020 to 24 April 2020 were included. All patients that were operated on had a telephone follow-up two weeks after surgery to assess if they had experienced COVID-19 symptoms or had been tested for COVID-19. The nature of admission, operative details, and patient demographics were obtained from the health board’s electronic record. Staff were assessed for sickness, self-isolation, and COVID-19 status.
Results
A total of 58 surgical procedures were undertaken at the OSU during the study period; 93% (n = 54) of patients completed the telephone follow-up. Open reduction and internal fixation of ankle and wrist fractures were the most common procedures. None of the patients nor members of their households had developed symptoms suggestive of COVID-19 or required testing. No staff members reported sick days or were advised by occupational health to undergo viral testing.
Conclusion
This study provides optimism that orthopaedic patients planned for surgery can be protected from COVID-19 nosocomial transmission at separate COVID-19-free sites.
Cite this article: Bone Joint Open 2020;1-6:302–308.
Introduction
The COVID-19 pandemic has demanded an unprecedented restructuring of hospital systems across the world. Planned elective surgical procedures have been put on standby across the UK and in many other countries. Hospitals urgently increased critical care capacity and diverted the workforce to support frontline areas in contact with this disease.1-3 Surgeons and theatre teams were redeployed to support intensive care units in caring for critically ill patients.4 Reducing elective activities has protected patients from potential in-hospital viral transmission and associated postoperative complications. Limiting hospital attendances to emergency and urgent presentations has reduced hospital footfall and likely reduced exposure of COVID-19 to both clinical staff and patients.1,3,5
The COVID-19 surgery group led by Bhangu et al1 have estimated that there have been 28,404,603 cases cancelled during the peak 12 weeks of disruption globally. Should countries resume 20% of their average surgical volume, it would take 45 weeks just to clear the backlog. The impact and health consequences to patients because of delayed surgical care is currently unknown. Health systems will have to adapt to a “new normal” way of working as elective surgery restarts.
During the COVID-19 pandemic, the orthopaedic department at Aneurin Bevan University Health Board (ABUHB) underwent rapid restructuring by cancelling elective operating while providing a safe and timely trauma service to a population of 591,225.4,6 Restructuring involved dividing the trauma workload between two different hospital sites. This freed up operating theatre space for potential critical care expansion. Nonambulatory trauma (predominantly neck of femur fractures) continued to be treated at the main COVID-19-receiving hospital (Royal Gwent Hospital). Ambulatory and semi-urgent trauma was treated at the orthopaedic surgical unit (OSU) in St. Woolos’ Hospital.
Surgical teams nationally have limited evidence and guidance on how departments will need to restructure their elective units to provide a service that is safe for patients and healthcare staff that is cost-effective and reproducible. Early experience in the literature supports “COVID-19-free” units separate from COVID-19 patients, analogous to “ring-fenced” orthopaedic surgical beds as a mode of limiting nosocomial transmission of COVID-19.7–9 This paper explores our local experience of delivering orthopaedic trauma care using this model.
In this article, we present our early outcomes of providing short stay trauma surgery in a COVID-19 free surgical unit during the coronavirus pandemic. This may provide guidance to protect patients during the pandemic and confidence restarting routine elective surgery in the future.
Methods
The site protocol at St. Woolos’ Hospital (a COVID-19-free site) is detailed below.
Preoperative pathway
Trauma patients were assessed in the minor injuries unit (MIU) by a trained emergency nurse practitioner. MIU was restructured in the Royal Gwent Hospital, having been relocated from the main accident and emergency (A&E) department to the orthopaedic fracture clinic. This increased the A&E department’s capacity to manage patients presenting with COVID-19. New orthopaedic trauma patients were therefore separated from incoming suspected positive or confirmed COVID-19-positive patients in the main A&E department.
The ABUHB health board abided by the “Green, Red, Amber” zone recommendations for personal protective equipment (PPE) agreed to by Public Health Wales defining the risk of COVID-19 transmission.10 Green zone pertains to non-patient contact areas, Amber zone relates to inpatient contact within two metres, with Red zone defined as area with an aerosol-generating procedure (AGP). All patients were assessed with "Amber (inpatient contact – non-AGP)" protective equipment precautions (Figure 1).6,10,11 All patients requiring follow-up or possible operative intervention were discussed with the on-call orthopaedic consultant based in the MIU. Out-of-hours patients were discussed in the following morning trauma meeting.
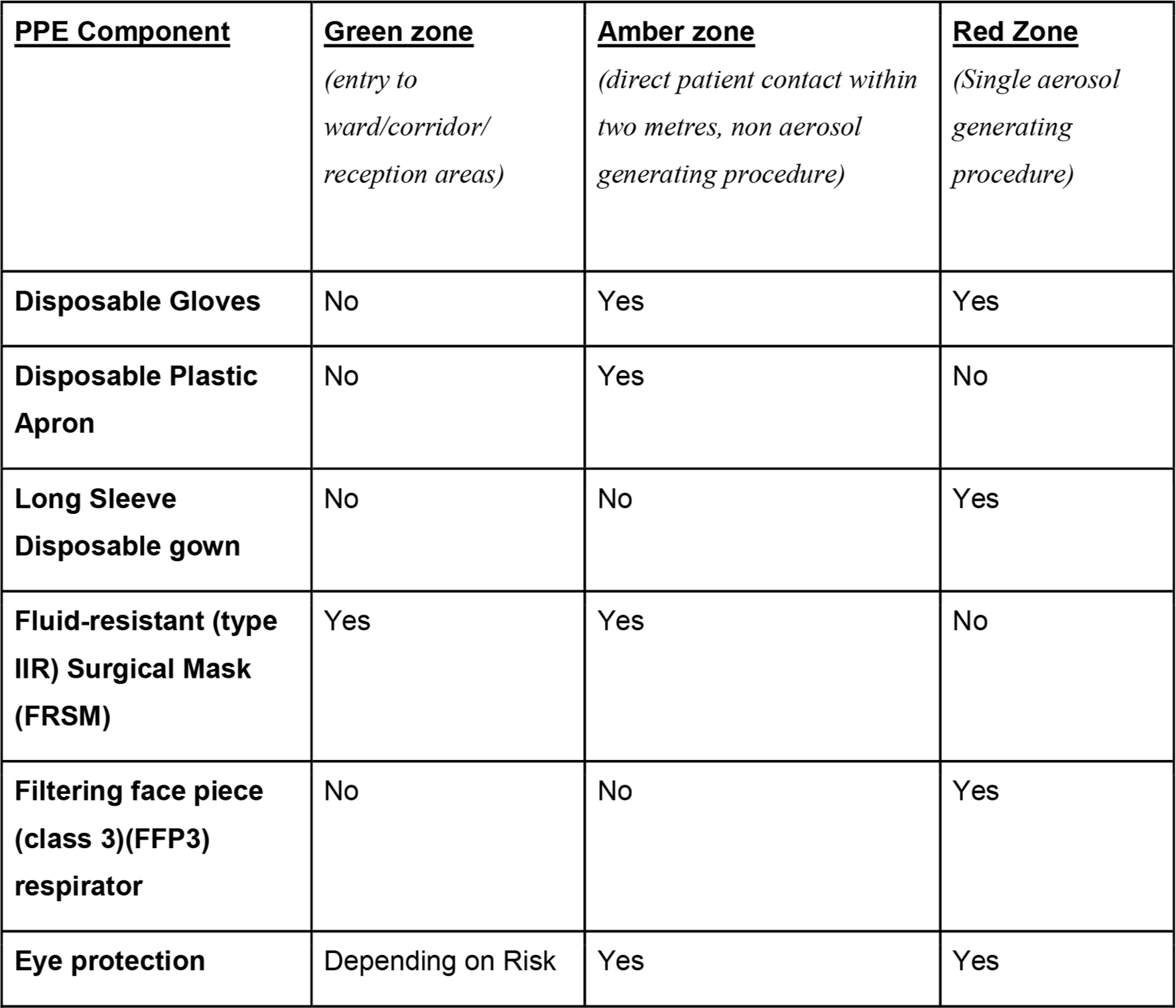
Fig. 1
Personal protective equipment designated zones utilized at the Aneurin Bevan University Health Board supported by Public Health Wales.10 FFP, filtering face piece; FRSM, fluid-resistant surgical mask.
Patients booked for surgery underwent a fitness for surgery assessment completed by trained pre-assessment nurses. The pre-admission unit was situated adjacent to the new MIU allowing immediate assessment following initial trauma care. Patients were assessed by telephone if a decision to offer surgery was made out of hours or following discharge from MIU. Patients were screened for COVID-19 symptoms and viral swab testing offered if symptomatic.
Patients who had decision of surgery made in MIU were consented on the same day by the on-call orthopaedic team. The risks of contracting COVID-19 and postoperative risks were documented on the consent form and in the patient’s clinical notes. These were then transferred to OSU. The other group of patients who had the decision of surgery made out of hours were consented on the day of surgery by the operating surgeon in OSU. The same risks of COVID-19 were documented in the patient’s consent form and clinical notes.
OSU ward structure
All patients were admitted to OSU on the day of surgery and provided with standard surgical masks to wear. Patients were rescreened for COVID-19 symptoms on admission. Patients were isolated in single side rooms. No open bays were utilized to prevent cross-contamination. Amber PPE protocols were utilized for all patient contact (Figure 1). Patients underwent same-day anaesthetic assessment.
OSU was staffed with a resident medical doctor who provided ward cover solely to OSU and did not cover COVID-19-positive wards. Ward patients were cared for by nursing staff and allied health care professionals who did not cover COVID-19-positive areas.
Theatre structure and design
Red PPE protocol (Figure 1) was required in theatre where AGP were carried out, which followed Department of Health Public Health Wales guidelines.10–12 The policy from our health board was initially to switch off laminar flow during surgery. This was a decision led by the anaesthetic department as there was concern that this may deliver viral particles to adjacent theatre corridors were unprotected scrub staff are situation. This has been reversed as guidance from the Royal College and the Department of Health Public Health Wales have clarified the safety of use of laminar flow.13 Intubation, extubating, and surgery using high-speed devices were considered AGP.13 In all, 2o minutes elapsed before the staff could exit the operating room following an AGP. This was taken as the average time for aerosol to settle to safely remove PPE. Department of Health Public Health Wales guidelines10 on donning and doffing technique were strictly followed.
Postoperative care
Patients were nursed in a dedicated recovery area with staff utilizing amber PPE (Figure 1). Once recovered, they returned to their cubicle and were discharged home when safe.
All patients operated at OSU during the COVID-19 pandemic were identified retrospectively from our Operating Room Management Information System (ORMIS) over a period of one month from 23 March 2020 to 24 April 2020. A telephone interview was undertaken at a minimum of two weeks post-discharge to assess for symptoms suggestive of COVID-19 infection. The symptom checklist included any fever, cough, sore throat, anosmia, headache, shortness of breath, and gastrointestinal symptoms. Patients were also asked if family members were symptomatic and whether the patient or any family members, required self-isolation since surgery.
Details of operative notes, patient demographics, comorbidities, and any COVID-19 swab results were obtained from our electronic clinical record.
The ward and theatre managers were interviewed to assess the prevalence of staff sickness, self-isolation, and viral swab status.
A Medline and PubMed search was performed encompassing a variety of terms, including ‘coronavirus’, ‘COVID-19’, ‘orthopaedic,’ ‘PPE,’ ‘cancellations’ and ‘elective surgery.’
Results
A total of 58 patients were identified as having undergone surgery at OSU during the study period. All patients had consultant-led operative decision making and a preoperative assessment. Only one patient (1.7%) reported that they had had symptoms suggestive of COVID-19 preoperatively. This patient had symptoms of a cough and upper airway respiratory symptoms. An oropharyngeal SARS-CoV-2 RNA PCR swab test performed following the local health board policy was negative. The patient had no comorbidities, denied close contacts with known cases, and was considered low-risk of COVID-19 infection and was therefore offered surgery at OSU. Their symptoms had resolved by the day of surgery and was deemed fit by the anaesthetist.
The mean patient age was 45 years (15 to 76), 57% were male (33/58), and 43% were female (25/58). In total, 53% of patients were American Society of Anesthesiologists (ASA) grade14 1 (30/58), 44% were ASA grade 2 (30/58), and 3% ASA grade 3 (1/58). Overall, 45% had surgery under regional block (26/58), and 55% had a general anaesthetic (32/58) (Figure 2).
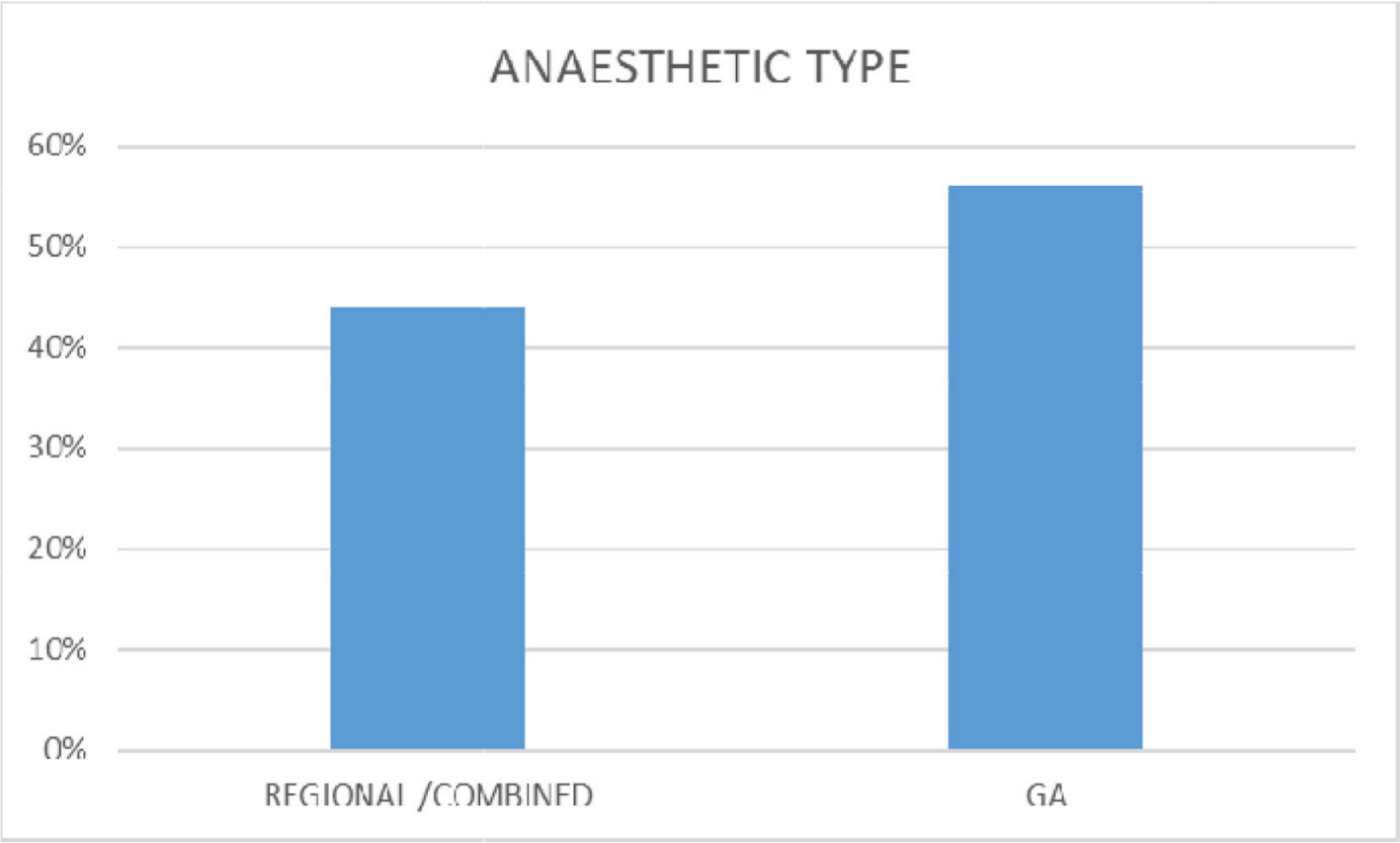
Fig. 2
Anaesthetic type used in St. Woolos' Hospital. GA, general.
The most common procedures performed at OSU were open reduction internal fixation (ORIF) of ankle and distal radius fractures. Of the 58 patients, 41 (72 %) were discharged on the same day, with six (10%) of patients discharged on postoperative day one, and three (5%) discharged on postoperative day two (Figure 3). The patients discharged on postoperative day one and day two were patients treated for lower limb injuries and required further inpatient physiotherapy to allow for safe discharge.
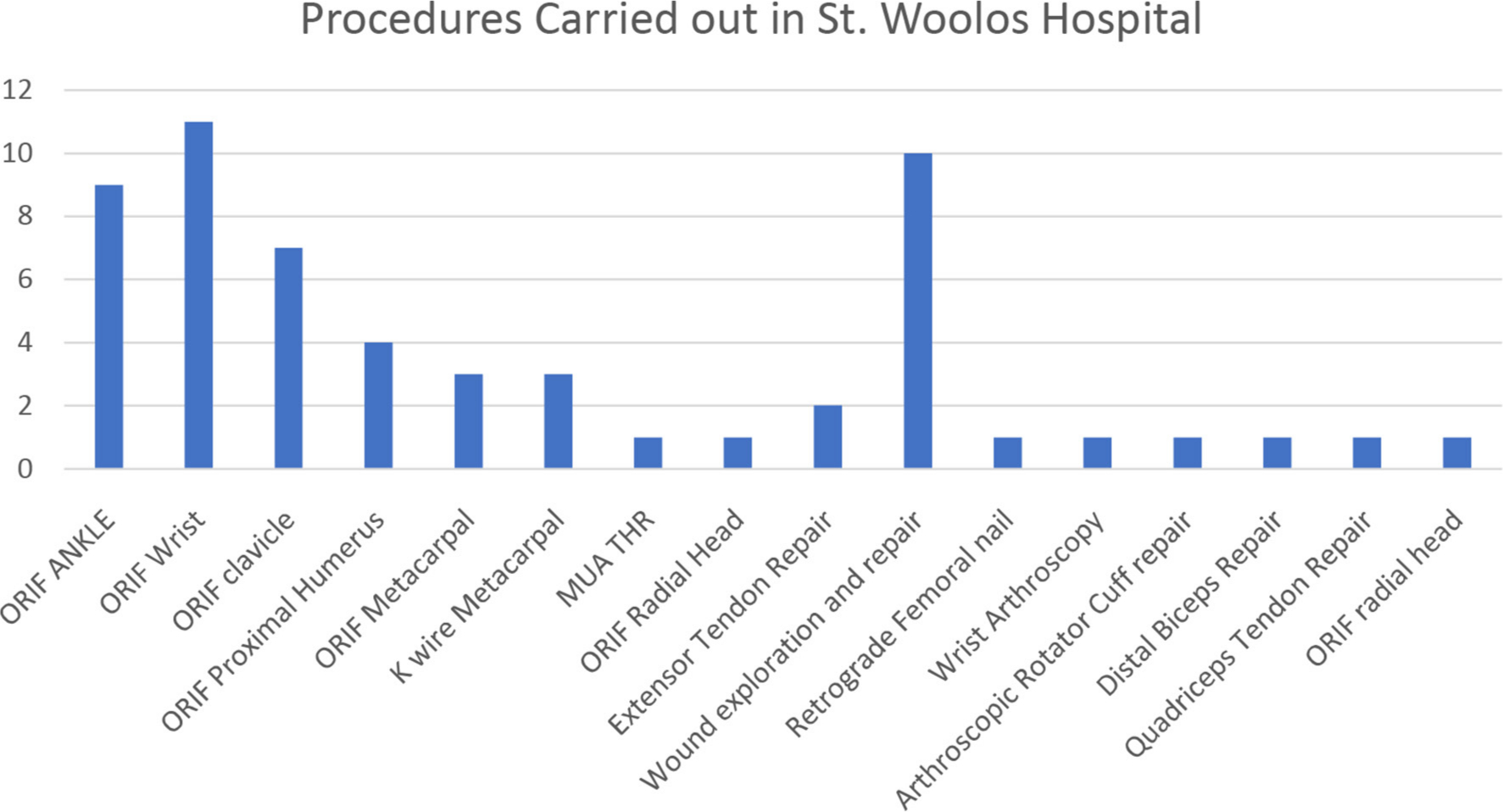
Fig. 3
Procedures performed at the Orthopaedic Surgical Unit from 23 March 2020 to 24 April 2020. K-wire, Kirschner wire; MUA THR, manipulation under anaesthesia total hip replacement; ORIF, open reduction internal fixation.
In total, 54 out of 58 (93%) responded to the telephone interview. None of the patients reported symptoms suggestive of COVID-19, nor were any close relatives reported as symptomatic. None of the patients required self-isolation postoperatively (Figure 4).
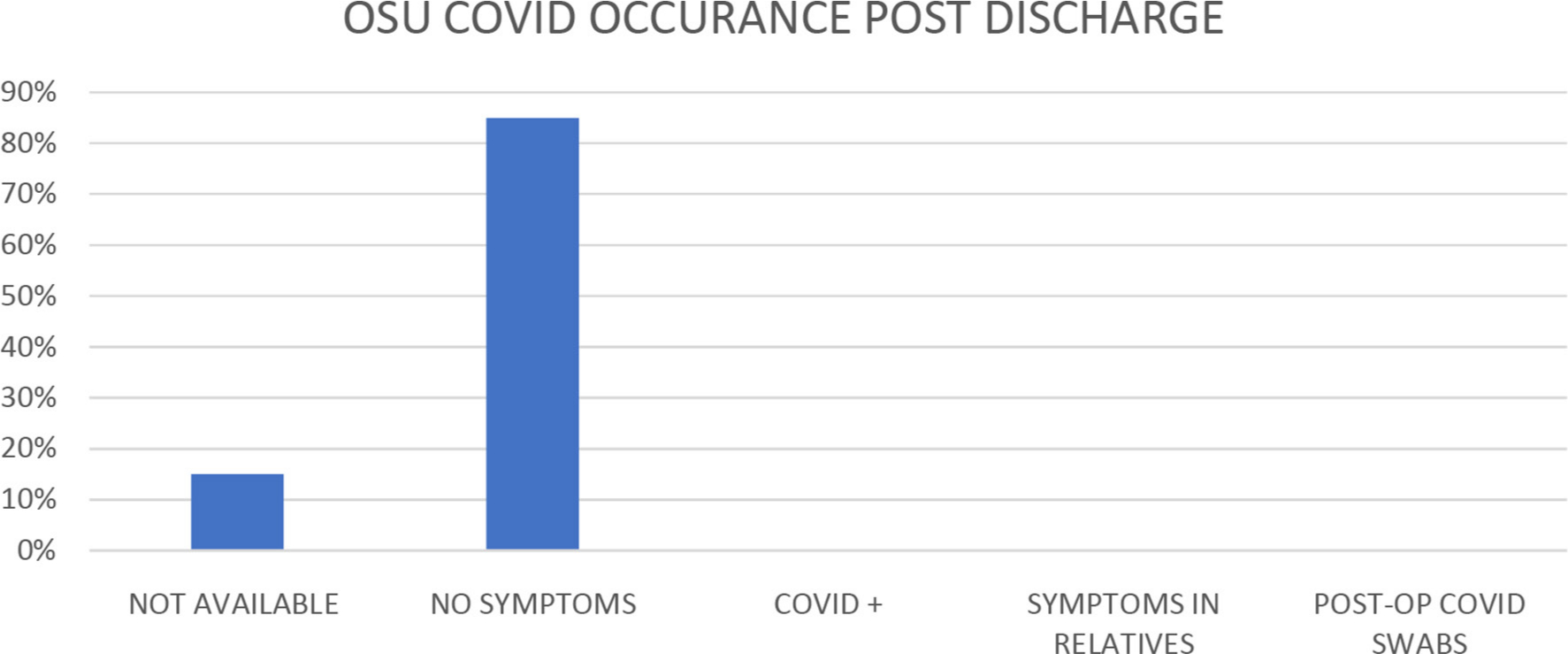
Fig. 4
Symptoms suggestive of COVID-19 occurrence at two weeks postoperatively. OSU, Orthopaedic Surgical Unit.
Discussion
Elective orthopaedic procedures have been classified as nonessential to help conserve and divert resources during the COVID-19 pandemic.1 The effects of cancelling and further delaying elective orthopaedic have had a significant impact on society as patients are left with untreated debilitating and disabling conditions.2,3,15,16 It has been reported that it will cost over £2 billion to clear the UK’s current backlog of cancelled elective operations as a result of the COVID-19 pandemic.
If SARS-CoV-2 follows similar infection patterns as other infective pandemics we should anticipate repeated waves of infection, leading to additional periods of cancellation of elective surgery. Strategies to safely maintain surgical volume during these periods must be explored to ensure elective operating is not as drastically disrupted as it has been during this COVID-19 pandmeic.1,17
The early experience reported in Wuhan highlights the risk of introducing routine elective surgery with limited precautions to prevent nosocomial transmission.18–20 In their series, 44% required ICU admission and 20% died from COVID-19 postoperative complications.18 This included 34 patients that were all operated within the incubation period of SARS-CoV-2 infection. Surgeons and trust managers need to be confident, that the systems in place minimize the exposure of patients undergoing elective orthopaedic surgery to COVID-19. The personal and medicolegal consequences of such complications arising are significant and must be borne in mind.18–20
This study provides support to the current consensus of a designated “COVID-19-free” surgical unit, analogous to “ring-fenced” orthopaedic beds. We have shown low nosocomial transmission rates in our patient group and staff. This model was also functional with the reduced workforce available during the peak of the pandemic while allowing for expansion of critical care capacity. We believe this model will be sustainable throughout subsequent repeated waves of SARS-CoV-2 infection. The ideal surgical candidate for this would be a day case, low-risk patient, who will be unlikely to require a postoperative intensive care bed.8,9,21,22
Our paper adds to the confidence of low COVID-19 hospital-acquired infection in COVID-19-free sites. A similar result published in a ‘letter to the editor’ by a group of South Korean surgeons showed no hospital COVID-19 transmission in 96 patients offered elective surgery, although it is unclear on how they restructured their unit.23 In a series by Chui et al,7 12 hip fracture patients with no clinical suspicion of COVID-19 were treated in unused elective orthopaedicbeds and theatrespace from the private sector.
Many units might not have the infrastructure to offer COVID-19-free centres, and many patients that require a higher level of postoperative care or medical support may need to be carried out in the main hospital treating COVID-19 patients. Research in the form of comprehensive, collaborative research or multicentre trials will be valuable in discerning the safest and most cost-effective way of returning to elective surgery.
At the time of this study, viral testing in Wales was restricted to symptomatic inpatients and healthcare staff following occupational health approval. In an ideal scenario, all patients should have undergone pre and postoperative viral swabbing, and staff would undergo repeated viral swabbing to ensure negative status and self-isolate if positive.
There has been wide variation worldwide in the reported percentage of asymptomatic patients who test positive for SARS-CoV-2 ranging from 5% to 80%. A review from St Bartholomew's Hospital in London carried out during the same period as this study demonstrated that 27% of staff that tested positive had no symptoms either in the week preceding or following testing.24 Therefore, there may be a cohort of our postoperative patients who have contracted the virus but remain asymptomatic, and therefore untested. None of our patients came to any appreciable harm from occult COVID-19 infection, which is reassuring. However, this does not mean that a continuous flow of asymptomatic COVID-19 positive patients could not propagate viral spread, putting staff and other patients at potential risk. It is, therefore, our future aim to screen all patients and staff for SARS-CoV-2 as testing capacity is expanded. 24,25
We hope this paper inspires optimism in the orthopaedic community in restoring semiurgent and elective surgery. As hospitals in the UK have already undergone unprecedented restructuring to increase capacity to fight COVID-19, they will need to do so once again and adapt to a “new normal” to offer elective surgical care to patients. The same efficient, enthusiastic mindset used during initial restructuring, must be adopted by the surgical community to provide high-quality evidence to identify the ideal surgical unit model for the COVID-19 era.
COVID-19 free sites may offer protection from nosocomial COVID-19 transmission. Managers should consider this model when resuming elective surgery following COVID-19 pandemic. Further study is required to identify the safest, cost-effective model. This may be carried out as a wide-scale collaborative project or multicentre trial.
References
1. COVIDSurg Collaborative . Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, 2020 May 12] . Br J Surg . 2020 ; 10 : 10.1002/bjs.11746 . Google Scholar
2. COVIDSurg Collaborative . Global guidance for surgical care during the COVID-19 pandemic . Br J Surg . 2020 : 10.1002/bjs.11646 . Crossref PubMed Google Scholar
3. Spinelli A , Pellino G . COVID-19 pandemic: perspectives on an unfolding crisis . Br J Surg . 2020 ; 107 ( 7 ): 785 – 787 . Crossref PubMed Google Scholar
4. Gonzi G , Gwyn R , et al. Our experience as Orthopaedic Registrars redeployed to the ITU emergency rota during the COVID-19 pandemic . British Orthopaedic Association . 2020 . https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/our-experience-as-orthopaedic-registrars.html (date last accessed 16 June 2020 ). Google Scholar
5. Dayananda KSS , Yasin T , Jemmett P , Trickett RW , et al. COVID-19: The Impact and Changes to Trauma Services in Cardiff . British Orthopaedic Association . 2020 . https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/covid-19-the-impact-and-changes-to-trauma-services.html (date last accessed 16 June 2020 ). Google Scholar
6. StatsWales . Population estimates by local health boards and age . Welsh Government, Statistics Wales . 2020 . https://statswales.gov.wales/Catalogue/Population-and-Migration/Population/Estimates/Local-Health-Boards/populationestimates-by-lhb-age (date last accessed 16 June 2020 ). Google Scholar
7. Chui K , Thakrar A , Shankar S . Evaluating the efficacy of a two-site (‘COVID-19’ and ‘COVID-19-free’) trauma and orthopaedic service for the management of hip fractures during the COVID-19 pandemic in the UK . Bone Joint Open ; 2020 : 190 – 197 . Google Scholar
8. De Caro F , Hirschmann TM , Verdonk P . Returning to orthopaedic business as usual after COVID-19: strategies and options. knee surgery, sports traumatology, arthroscopy. knee surgery, sports Traumatology . Arthroscopy . 2020 ; 28 : 1699 – 1704 . Google Scholar
9. Chang Liang Z , Wang W , Murphy D , Po Hui JH . Novel coronavirus and orthopaedic surgery: early experiences from Singapore . J Bone Joint Surg Am . 2020 : e000236 . Crossref PubMed Google Scholar
10. Public Health England . COVID-19: Infection prevention and control guidance. First published 24/03/2020 . https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/886215/COVID-19_Infection_prevention_and_control_guidance_complete.pdf (date last accessed 19/05/2020 ). Google Scholar
11. Key T , Mathai NJ , Venkatesan AS , et al. Personal protective equipment during the COVID-19 crisis: a snapshot and recommendations from the frontline of a university teaching hospital . Bone & Joint Open . 2020 ; 1 ( 5 ): 131 – 136 . Crossref PubMed Google Scholar
12. Baldock TE , Bolam SM . Infection prevention measures for orthopaedic departments during the COVID-2019 pandemic: a review of current evidence . Bone Joint Online . 2020 ; 1-4 : 74 – 79 . Crossref PubMed Google Scholar
13. Royal College of surgeons . COVID-19: good practice for surgeons and surgical teams . 2020 . https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/ (date last accessed 21/05/2020 ). Google Scholar
14. Saklad M . Grading of patients for surgical procedures . Anesthesiology . 1941 ; 2 ( 3 ): 281 – 284 . Google Scholar
15. Giorgi P , Gallazzi E , Capitani P , et al. How we managed elective, urgent and emergency orthopaedic surgery during the COVID-19 pandemic . Bone & Joint Open ; 1 ( 5 ). Google Scholar
16. Mayol J , Fernández Pérez C . Elective surgery after the pandemic: waves beyond the horizon . Br J Surg . 2020 . Crossref PubMed Google Scholar
17. Leung K , Wu T , Liu D , Leung GM . First-wave COVID19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment . Lancet . 2020 ; 395 ( 10233 ): 1382 – 1393 . Google Scholar
18. Lei S , Jiang F , Xia Z , et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. [published online ahead of print, 2020 Apr 5] . EClinicalMedicine . 2020 : 21:100331 . Google Scholar
19. Huang G . The importance of preventing COVID-19 in surgical wards cannot be overemphasized . Br J Surg . 2020 ; 107 ( 7 ): e198 . Crossref PubMed Google Scholar
20. Ives J , Huxtable R . Surgical ethics during a pandemic: moving into the unknown? [published online ahead of print, 2020 Mar 30] . Br J Surg ; 107 : 10.1002/bjs.11638 . Google Scholar
21. Radhaab S , Afzalb I . Evidence based suggestions for the return to elective orthopaedic surgery following the COVID-19 pandemic. Transient Journal of Orthopaedic and Coronavirus. Published online 01 May 2020 . https://www.boa.ac.uk/policy-engagement/journal-of-trauma-orthopaedics/journal-of-trauma-orthopaedics-and-coronavirus/evidence-based-suggestions-for-the-return.html?fbclid=IwAR01SiCbBvy_NHylhUajv0RV9kDKU46-dCLrJ4lC4YDUvpSPUhpE7SjXYXY (date last accessed 19 May 2020 ). Google Scholar
22. Ross GL . Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. What are the implications for the commencement of elective surgery? EClinicalMedicine . 2020 : 100385 . Crossref PubMed Google Scholar
23. Low TY , B.Y S , et al. Elective surgeries during the COVID-19 outbreak . British Journal of surgery . 2020 . Crossref PubMed Google Scholar
24. Heneghan C , Brassey J , Jefferson T . COVID-19: What proportion are asymptomatic? . The Centre for Evidence-Based Medicine . 2020 . https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/ (date last accessed 16 June 2020 ). Google Scholar
25. Treibel T et al. COVID-19: PCR screening of asymptomatic healthcare workers at London hospital. Published 07/05/20 . https://www.thelancet.com/action/showPdf?pii=S0140-6736%2820%2931100-4 (date last accessed 20/05/2020 ). Google Scholar
Author contributions
G. Gonzi: Led and designed study. Collected and analysed the data. Wrote and revised manuscript.
K. Rooney: Designed the study, Analyzed the data, Revised the manuscript.
R. Gwyn: Designed the study, Analyzed the data, Revised the manuscript.
K. Roy: Designed the study, Analyzed the data, Revised the manuscript.
M. Horner: Designed the study, Analyzed the data, Revised the manuscript.
R. Jenkins: Collected the data, Completed telephone interviews, Revised the manuscript.
J. Lloyd: Analyzed the data, Edited the manuscript.
H. Pullen: Designed the study, Analyzed the data, Edited the manuscript, Provided overall supervision.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Acknowledgements
The authors would like to acknowledge the contribution of all trauma and orthopaedic department team members at the Aneurin Bevan University Health board during the COVID-19 pandemic, including all anaesthetic, operating theatre, minor injuries, pre-assessment, management, and secretarial team members.
Follow G. Gonzi @GonziGianluca
Follow R. Gwyn @rhodrigwyn
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.









