Abstract
Aims
To determine if the results of treatment of adolescents with coccydynia are similar to those found in adults. Adult patients with coccydynia may benefit from injection therapy or operative treatment. There is little data evaluating treatment results in adolescents. We have treated adolescent patients similarly to adults and compared the outcomes.
Methods
Overall, 32 adolescents with coccydynia were treated at our institution during a seven-year period; 28 responded to final follow-up questionnaires after a minimum of one year, 14 had been treated with only injection therapy, and 14 had been operated with coccygectomy. We collected data with regards to pain while sitting, leaning forward, rising from a sitting position, during defecation, while walking or jogging, and while travelling in trains, planes, or automobiles. Pain at follow-up was registered on a numeric pain scale. Each adolescent was then matched to adult patients, and results compared in a case control fashion. The treatment was considered successful if respondents were either completely well or much better at final follow-up after one to seven years.
Results
Out of the 28 treated adolescents, 14 were regarded as successfully treated. Seven were somewhat better, and the remaining seven were unchanged. In the adult control group the corresponding number was 15 successfully treated, eight patients were somewhat better, and five were unchanged. Six of the 14 successfully treated adolescents had been operated. There were no significant differences between the groups in the various registered domains, or on numeric pain scale.
Conclusion
Treatment results in adolescent patients seem similar to those in adults. The long-term success rate of injection therapy is low. In case of injection treatment failure, operation may be considered, also in adolescents.
Introduction
Coccydynia is a condition associated with pain around the lower end of the spine, particularly when sitting. The exact prevalence of this condition is not known,1 but Ghormley in 1958 found that it encompassed 2.7% of all hospital presentations with back pain.2
Most review papers on coccydynia conclude that both corticosteroid injections and surgery can be beneficial.3-7 However, published papers also indicate a seeming reluctance to employing these methods in young patients. This is particularly noticeable with regard to surgery. We have found 24 relevant papers on coccygectomy in the literature.8-31 Although coccydynia may certainly affect adolescents, only seven of these included patients under the age of 18 years.25-31
We have treated our patients without regard to age. Coccydynia in adolescents has a serious impact on daily social activities, sports and, most importantly, on their school education which usually involves long periods of sitting. We have reviewed our own patients in order to compare our results in adolescents to those in adult patients in a case-control fashion.
Methods
In all, 358 patients with chronic coccydynia were referred to our institution during the period 2009 to 2016. A total of 43 (12%) of these were adolescents with a mean age of 15 years (11 to 17). There were 36 girls and seven boys.
The patients were referred to our institution by general practitioners and other hospitals after having failed conservative therapy. All adolescent patients were investigated, diagnosed and treated in a similar manner to adults.
The diagnosis of coccydynia was made by a senior spinal surgical consultant (RGK) based on a thorough medical history, clinical examination and imaging with either coccygeal radiographs, MRI, or both (Figures 1 and 2).
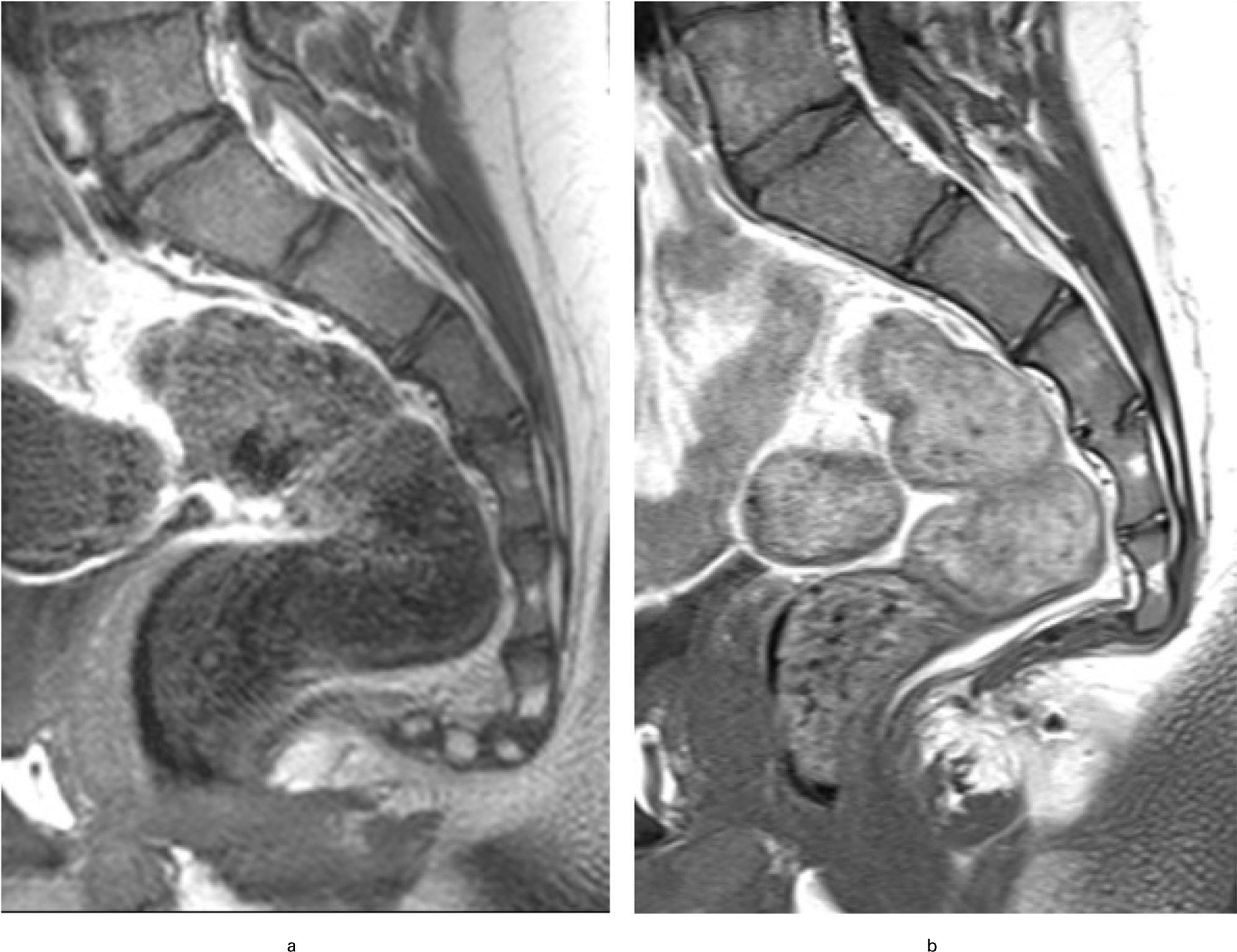
Fig. 1
a) 13-year-old boy at referral. b) After surgery.

Fig. 2
MRI of 15-year-old boy with bony spicula from coccyx.
Patient characteristics were recorded, including the aetiology of the coccygeal pain and the history of onset (Table I). A total of 31 (72%) had experienced a trauma, while one girl had coccydynia after giving birth at age of 15 years. The remaining 11 did not know the cause of their pain. The condition was regarded as chronic if patients had been symptomatic for more than two months.
Table I.
Causes of coccydynia in adolescents.
| Cause | n |
|---|---|
| Fall | 10 |
| Winter sport | 5 |
| Bicycle/skating/horse riding | 3 |
| Gym/sports/play | 11 |
| Other trauma | 2 |
| Birth-related | 1 |
| Not known | 11 |
| Total | 43 |
We recorded the presence of pain in the following domains: sitting, leaning forward, rising from a sitting position, during defecation, while walking or jogging, and while travelling in trains, planes, or automobiles.
Rectal examination was feasible in most cases, usually with a parent alongside the patient. On this examination, we noted the presence of pain from local pressure, reproduction of pain by manipulation of the coccyx, and coccygeal hypermobility.
Almost all patients had been advised some form of conservative treatment during the months between referral and out-patient examination. All patients were therefore offered a targeted lidocaine/corticosteroid injection either at the first or a subsequent out-patient visit. In all, 11 adolescents received no treatment and were excluded from further consideration. We used a standardized method of direct injection in the most painful level of the coccyx, usually the sacrococcygeal or Co1-Co2 level, under digital intrarectal control without fluoroscopic imaging as described by Kersey32 and Finsen.33 A total of 21 had one injection, four had two injections, and two had three injections. Patients who were afraid of possible injection pain and refused treatment were offered injection during a short intravenous anaesthesia.
In case of treatment failure with injection therapy, patients were offered surgery with partial or total coccygectomy, with the technique described by Key.34 Surgery was performed in 12 such adolescents. In addition, five were operated without previous injection.
All treated patients were reviewed clinically three months after the last injection or surgery. At a minimum of 12 months after treatment, the patients were further followed-up with mailed questionnaires. Patients who had not responded to the questionnaires were contacted by telephone after six weeks as a reminder. They received new questionnaires if they wished. The mean time to final follow-up was 34 months (12 to 86).
Pain in the previously registered domains and overall result were at follow-up scored in the following fashion: completely well, much better, somewhat better, unchanged, or worse. Patients who were completely well or much better at final follow-up were regarded as successfully treated. If the patients were either somewhat better, unchanged, or worse we regarded them as treatment failures. Patients who were not satisfied with the results of injection therapy and therefore continued to operative treatment were automatically regarded as failures of injection therapy.
In addition, patients scored pain during the last week on numeric pain scales from 0 to 10. The operated patients were also asked whether they would have consented to the operation if they had known the outcome in advance.
Overall, 28 treated adolescents (88%) responded to our final follow-up and constitute the index patients of our review (Figure 3). The four who were lost to follow-up were equally distributed between the operative and non-operative groups. Of the index patients, 14 received only injection therapy, with a mean follow-up of 37 months (18 to 66), and 14 were operated upon, with a mean follow-up of 35 months (14 to 64).
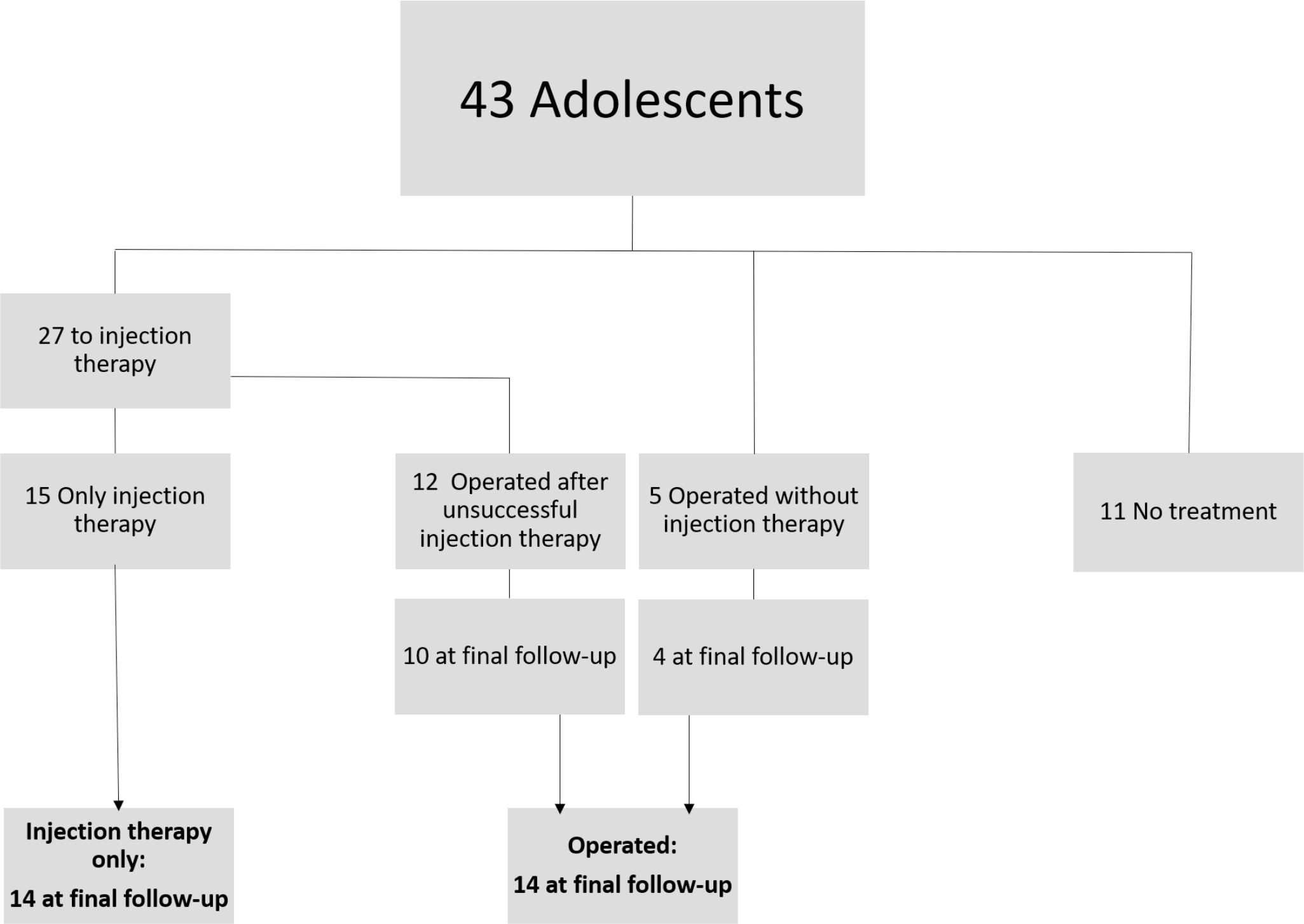
Fig. 3
Flowchart of patients included in study.
Each adolescent was then matched to adult controls who had undergone the same treatment for coccydynia during the same time-period. The matching was done for sex, number of injections given, whether they were subsequently operated, and duration of follow-up (± six months) after final injection or operation. When there were multiple available matches, median results were recorded. No match was available for one child and the follow-up duration had to be extended by two extra months in order to find a match.
The results were then analyzed, comparing the index patients to adult controls with chi-square testing of dichotomous results, non-parametric testing for all functional domains and independent samples t-tests to compare numeric pain scores. The study protocol was reviewed by the regional committee for medical and health research ethics in central Norway who found that it did not need their approval.
Results
Out of the 28 treated adolescents, 14 were regarded as successfully treated (seven completely well and seven much better at final follow-up). Seven were somewhat better and the remaining seven were unchanged. For the adult controls, 15 were regarded as successfully treated (four completely well and 11 much better), eight were somewhat better, and the remaining five were unchanged.
The average 0 to 10 pain score among all treated adolescents at final follow-up was 3.4, while it was 3.3 in the adult control group.
Injection therapy
In our short-term results (three months after final injection), we found that seven of the 24 patients were completely well, seven were somewhat better, five had experienced a temporary period of relief before relapsing, and five had no improvement. At the final follow-up, injection therapy was successful in eight injected index patients (completely well or much better).
In the adult control group, four were completely well at the short-term follow-up, seven were somewhat better, five had temporary relief followed by a relapse, and eight had not experienced any improvement. At the final follow-up five adults were found to be successfully treated by injection therapy. There were no adverse events from the injections.
Operative treatment
Operative treatment was successful in six out of 14 adolescents. In the adult control group, nine out of 14 were considered a success. On a scale from 0 to 10, the operated adolescents had a mean pain score of 3.9 at final follow-up, while it was 2.6 in the adult control group. When asked whether they would have consented to the operation if they had known the result in advance ten out of the 14 operated adolescents, answered yes. In the adult control group 13 answered yes.
Operative treatment was complicated by two deep infections in the adolescent group, requiring surgical debridement. This was also the case in the adult control group.
On statistical testing we found no significant differences between the adolescents and the adult controls, regardless of which treatment modality had been used, with regard to both numeric pain scores or the various pain domains (Table II).
Table II.
Results among operated adolescents.
| Number before operation | At review | ||||||
|---|---|---|---|---|---|---|---|
| No pain | Much better | A bit better | No change | Worse | |||
| Pain on symmetrical sitting | 14 | 3 | 2 | 6 | 2 | 1 | |
| Adult controls | 14 | 3 | 6 | 3 | 1 | 1 | |
| Pain on rising | 11 | 3 | 2 | 2 | 4 | 1 | |
| Adult controls | 11 | 7 | 2 | 0 | 2 | 0 | |
| Pain on defecation | 11 | 8 | 2 | 2 | 0 | 0 | |
| Adult controls | 11 | 9 | 1 | 1 | 0 | 0 | |
| Pain on walking | 13 | 6 | 4 | 1 | 2 | 0 | |
| Adult controls | 13 | 5 | 4 | 3 | 0 | 1 | |
| Pain in public transport | 14 | 1 | 1 | 6 | 2 | 2 | |
| Adult controls | 14 | 2 | 7 | 2 | 3 | 0 | |
Discussion
As this review did not involve randomized control groups, there is a potential for selection bias despite systematic matching. Adult patients may be more positive towards undergoing both injection therapy and operative treatment than adolescents, which could influence the choice of treatment. In addition, as this is a relatively uncommon condition the number of index patients is low. Furthermore, we did not match the patients and controls with regard to aetiology as this would have left many adolescents without controls.
Like in all studies of adults, there was a strong preponderance of females. It is unlikely that girls are more physically active than boys at this age and injure themselves more often. We presume therefore, like others authors, that the reason for the sex ratio of 5:1 may be due to anatomical differences in the shape of the pelvis.3 Woon found that female coccyges were shorter and straighter and may be more prone to retroversion.35
We have found only one paper where the focus is on the treatment of adolescents.36 It reported on a retrospective follow-up of 53 adolescent patients, which comprised 7% of their total coccydynia population. We found that 12% of our patient population with coccygeal pain were adolescents. The authors, Maigne et al, included patients below 17 years of age, whereas we have included patients below 18 years, which harmonizes with the definition of childhood in most countries, and this may explain a higher prevalence.
In Maigne and co-workers’ study, only three patients had surgery, although not before turning 18 years, when they were no longer adolescents. They investigated 47 adolescents who received injection therapy. At two-month follow-up 19 (40%) had an excellent result, ten (21%) had partial relief or relapse, and there was insufficient or no benefit in 18 (38%). At their final follow-up, one to four years from initial presentation, they did not specify the results of the injected patients, but in their total patient cohort 32 of 53 (60%) patients were reported as totally or almost pain free, 12 (23%) had moderate pain, and nine (17%) had severe pain and major functional impairment.
Our results were not as good. In our short-term results (three months after final injection), we found that only 7/24 were completely well, 12/24 had partial relief or relapse, and 5/24 had no improvement. In our long-term results, injection therapy was rated as successful (completely well or much better) in 8/24 of injected adolescents.
Our long-term results of injection therapy indicate that such injections are unlikely to provide lasting results in most patients. Only one-third of our injected adolescents and around one-fifth of their adult controls were completely well or much better from this modality. We do, however, regard it as a safer option than operative treatment in terms of adverse events and believe that injection therapy should still be tried before operative treatment.
The discussion whether to operate on adolescents or wait until skeletal maturity is challenging, and very little literature on this topic exists. The fact that juveniles seem to make up 7% to 12% of the patient populations, but only a few are reported in the literature to have been operated, seems to indicate a reluctance to submit them to surgery.
Reviewing the published evidence, we found seven papers presenting operative treatment that included adolescents, but none reported the specific results of the adolescents.25-31 Only Margo26 reported results of four operated adolescents, but only included results after one to two months' follow-up.
There is thus no comparative literature available, but our long-term results show that less than half of our operated adolescents can be regarded as successfully treated, compared to around two thirds in the adult control group. However, our definition of success only included patients who were found to be completely well or much better at final follow-up. Seven of the operated adolescents that we classified as failures at final follow-up still reported that they were somewhat better. This may explain why as many as ten out of 14 adolescents reported that they would have consented to the operation if they had known the result in advanced.
The operative results seem better than our results of injection therapy, but since surgical coccygectomy involves a higher risk of complications, we believe that it is reasonable to reserve surgery for the most severe cases.
This is by far the greatest number of operated adolescents with coccydynia reported in the literature, but the number is still small and unlikely to reveal statistically significant differences. Even so, our results do give the general impression that, seen together, results are similar to those obtained among adults. We shall therefore continue to offer our adolescent patients cortisone injections and to consider the possibility of surgery when neither sitting aids, painkillers, or repeated injection therapy has had sufficient effect.
References
1. Lirette LS , Chaiban G , Tolba R , Eissa H . Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain . Ochsner J . 2014 ; 14 ( 1 ): 84 – 87 . PubMed Google Scholar
2. Ghormley RK . An etiologic study of back pain . Radiology . 1958 ; 70 ( 5 ): 649 – 653 . Crossref PubMed Google Scholar
3. Aarby NS , Trollegaard AM , Hellberg S . Coccygectomy can be a treatment option in chronic coccygodynia (In Danish) . Ugeskr Laeger . 2011 ; 173 ( 7 ): 495 – 500 . Google Scholar
4. Elkhashab Y , Ng A . A review of current treatment options for Coccygodynia . Curr Pain Headache Rep . 2018 ; 22 ( 4 ): 28 . Crossref PubMed Google Scholar
5. Fogel GR , Cunningham PY , Esses SI . Coccygodynia: evaluation and management . J Am Acad Orthop Surg . 2004 ; 12 ( 1 ): 49 – 54 . Crossref PubMed Google Scholar
6. Karadimas EJ , Trypsiannis G , Giannoudis PV . Surgical treatment of coccygodynia: an analytic review of the literature . Eur Spine J . 2011 ; 20 ( 5 ): 698 – 705 . Crossref PubMed Google Scholar
7. Nathan ST , Fisher BE . Roberts Cs. Coccydynia . J Bone Joint Surg [Br] . 2010 ; 92-B : 1622 – 1627 . Google Scholar
8. Antoniadis A , Ulrich NH-B , Senyurt H . Coccygectomy as a surgical option in the treatment of chronic traumatic coccygodynia: a single-center experience and literature review . Asian Spine J . 2014 ; 8 ( 6 ): 705 – 710 . Crossref PubMed Google Scholar
9. Bilgic S , Kurklu M , Yurttas Y , et al. Coccygectomy with or without periosteal resection . Int Orthop . 2010 ; 34 ( 4 ): 537 – 541 . Google Scholar
10. Cebesoy O , Guclu B , Kose KC , et al. Coccygectomy for coccygodynia: do we really have to wait? Injury . 2007 ; 38 ( 10 ): 1183 – 1188 . Crossref PubMed Google Scholar
11. Cheng SW , Chen QY , Lin ZQ , et al. Coccygectomy for stubborn coccydynia . Chin J Traumatol . 2011 ; 14 ( 1 ): 25 – 28 . PubMed Google Scholar
12. Doursounian L , Maigne J-Y , Faure F , Chatellier G . Coccygectomy for instability of the coccyx . Int Orthop . 2004 ; 28 ( 3 ): 176 – 179 . Crossref PubMed Google Scholar
13. Doursounian L , Maigne JY , Jacquot F . Coccygectomy for coccygeal spicule: a study of 33 cases . Eur Spine J . 2015 ; 24 ( 5 ): 1102 – 1108 . Crossref PubMed Google Scholar
14. Haddad B , Prasad V , Khan W , Alam M , Tucker S . Favourable outcomes of coccygectomy for refractory coccygodynia . 96 . England : Ann Royal Coll Surg , 2014 : 136 – 139 . Google Scholar
15. Hanley EN , Ode G , Jackson BJ III , Seymour R . Coccygectomy for patients with chronic coccydynia: a prospective, observational study of 98 patients . Bone Joint J . 2016 ; 4 ( 4 ): 526 – 533 . Crossref PubMed Google Scholar
16. Hodges SD , Eck JC , Humphreys SC . A treatment and outcomes analysis of patients with coccydynia . Spine J . 2004 ; 4 ( 2 ): 138 – 140 . Crossref PubMed Google Scholar
17. Kleimeyer JP , Wood KB , Lønne G , et al. Surgery for refractory coccygodynia: operative versus nonoperative treatment . Spine . 2017 ; 42 ( 16 ): 1214 – 1219 . Crossref PubMed Google Scholar
18. Kwon HD , Schrot RJ , Kerr EE , Kim KD . Coccygodynia and coccygectomy . Korean J Spine . 2012 ; 9 ( 4 ): 326 – 333 . Crossref PubMed Google Scholar
19. Maigne JY , Lagauche D , Doursounian L . Instability of the coccyx in coccydynia . J Bone Joint Surg Br . 2000 ; 82 ( 7 ): 1038 – 1041 . Crossref PubMed Google Scholar
20. Mouhsine E , Garofalo R , Chevalley F , et al. Posttraumatic coccygeal instability of the coccyx . Spine J . 2006 ; 6 : 544 – 549 . Google Scholar
21. Perkins R , Schofferman J , Reynolds J . Coccygectomy for severe refractory sacrococcygeal joint pain . J Spinal Disord Tech . 2003 ; 16 ( 1 ): 100 – 103 . Crossref PubMed Google Scholar
22. Pyper JB . Excision of the coccyx for coccydynia; a study of the results in twenty-eight cases . J Bone Joint Surg Br . 1957 ; 39-B ( 4 ): 733 – 737 . Crossref PubMed Google Scholar
23. Wood KB , Mehbod AA . Operative treatment for coccygodynia . J Spinal Disord Tech . 2004 ; 17 ( 6 ): 511 – 515 . Crossref PubMed Google Scholar
24. Zayer M , Coccygodynia ZM . Coccygodynia . Ulster Med J . 1996 ; 65 ( 1 ): 58 – 60 . Crossref PubMed Google Scholar
25. Balain B , Eisenstein SM , Alo GO , et al. Coccygectomy for coccydynia: case series and review of literature . Spine . 2006 ; 31 ( 13 ): E414 – E420 . Crossref PubMed Google Scholar
26. Margo E . The painful terminal spine . South Med J . 1962 ; 55 ( 5 ): 461 – 470 . PubMed Google Scholar
27. Pennekamp PH , Kraft CN , Stütz A , et al. Coccygectomy for coccygodynia: does pathogenesis matter? J Trauma . 2005 ; 59 ( 6 ): 1414 – 1419 . Crossref PubMed Google Scholar
28. Postacchini F , Massobrio M . Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx . J Bone Joint Surg Am . 1983 ; 65 ( 8 ): 1116 – 1124 . PubMed Google Scholar
29. Sehirlioglu A , Ozturk C , Oguz E , et al. Coccygectomy in the surgical treatment of traumatic coccygodynia . Injury . 2007 ; 38 ( 2 ): 182 – 187 . Crossref PubMed Google Scholar
30. Trollegaard AM , Aarby NS , Hellberg S . Coccygectomy: an effective treatment option for chronic coccydynia: retrospective results in 41 consecutive patients . J Bone Joint Surg Br . 2010 ; 92 ( 2 ): 242 – 245 . Crossref PubMed Google Scholar
31. Wray CC , Easom S , Hoskinson J . Coccydinia . J Bone Joint Surg [Br] . 1991 ; 73-B : 335 – 338 . PubMed Google Scholar
32. Kersey PJ . Non-Operative management of coccygodynia . Lancet . 1980 ; 1 ( 8163 ): 318 . Crossref PubMed Google Scholar
33. Finsen V . Corticosteroid injection for coccygodynia (in Norwegian) . Tidsskr Nor Legeforen . 2001 ; 121 : 2832 – 2833 . Google Scholar
34. Key A . Operative treatment of coccygodynia . J Bone Joint Surg . 1937 ; 19 : 759 – 764 . Google Scholar
35. Woon JTK , Perumal V , Maigne J-Y , Stringer MD . CT morphology and morphometry of the normal adult coccyx . Eur Spine J . 2013 ; 22 ( 4 ): 863 – 870 . Crossref PubMed Google Scholar
36. Maigne J-Y , Pigeau I , Aguer N , Doursounian L , Chatellier G . Chronic coccydynia in adolescents. A series of 53 patients . Eur J Phys Rehabil Med . 2011 ; 47 ( 2 ): 245 – 251 . PubMed Google Scholar
Author contributions
A. M. Kalstad: Planning the study, collecting data, analysis of the data, writing the manuscript
R. G. Knobloch: Planning the study, collecting data, reviewing the manuscript
V. Finsen: Planning the study, analysis of the data, writing the manuscript
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/










