Abstract
This review examines the future of total hip arthroplasty, aiming to avoid past mistakes
Introduction
Having been named the “operation of the century” by the Lancet,1 then commemorated with a stamp by the Royal Mail and acknowledged as one of the most cost-effective surgical procedures in terms of improvement in quality of life,2 total hip arthroplasty (THA) is universally regarded as a surgical success story. Last year over 76,000 primary THAs were performed in England & Wales.3
Against that positive background however, there have been dark days. In the 1990s, the Capital Hip (3M, Loughborough, UK) was widely implanted partly on the back of its similarity to an established device, but also perhaps because it was cheaper. There was a national scandal when it was subsequently found to have a high failure rate.4,5 The National Joint Registry in England & Wales (NJR) was founded, in part, as a response to concerns raised by this issue. More recently, the search for a more durable bearing surface and a reduced rate of dislocation led to the widespread increased use of large head metal-on-metal articulations resulting in well-documented problems and a significant number of catastrophic outcomes for our patients.6 While more implants are introduced to the market, others are withdrawn and one wonders whether the lessons of the Capital hip have not been learnt. The primary lesson in both these situations is that implants and bearing surface combinations must be properly evaluated before they are introduced. Similarly, it cannot be assumed that a ‘me-too’ implant will function in the same way as the design on which it is based.
As we move into the 21st Century, with an increasingly ageing yet active population, against a background of increasing medical co-morbidity and obesity our patients will, understandably, demand and require improved clinical outcomes and reliable longevity. This review examines some of the current issues and the future of THA, aiming to avoid past mistakes.
A new era: the end of the dabbler?
2013 saw a new phenomenon in UK orthopaedic practice: publication of individual surgeons’ outcomes. Initially this was restricted to 90-day mortality following THA. More recently, additional information on procedure numbers and implant usage has been made available. Individual surgeons have been given access to their own revision rates in a ‘Surgeon Profile’; perhaps the logical next step would be for these to be made publicly available. There have been arguments for and against publication of this data: some would argue that sharing this data might make surgeons more risk-averse (although this is not a worry borne out by publication of cardiothoracic surgery outcomes, where high risk patients have not seemingly been turned down for surgery).7 How many of us would not want to know our own surgeon’s outcomes before undergoing a similar procedure ourselves?
There is good evidence that those who perform over 35 THAs per year have improved outcomes.8 Rather surprisingly last year 54% of surgeons performing primary THAs performed fewer than this number.9 It is simple probability theory that a high-volume surgeon might be better able to absorb the occasional adverse outcome without ‘risking’ becoming an outlier than a low volume colleague. Similarly an unwise choice of bearing surface, implant or surgical approach, could have a significant effect on a surgeon’s published performance (Fig. 2). All of this could drive lower-volume surgeons to reconsider their hip arthroplasty practice.
If publication of outcomes is to succeed there are issues that need to be addressed. While data accuracy and revision linkability are increasing year-on-year, data quality concerns remain. Surgeons have been asked to validate their own recent data in the NJR. Thus there are ongoing efforts to improve data accuracy; similarly there needs to be improvement in the accuracy of coding diagnoses and case attribution. In time the significance of case mix complexity will need to be investigated. As things stand, data accuracy and completeness is the joint responsibility of surgeons, hospital administration and the registries themselves.
Back to the future – a return to tried and tested prostheses?
Most orthopaedic departments in England by now will have had a visit from Professor Tim Briggs, the immediate past British Orthopaedic Association President and his Getting It Right First Time (GIRFT) initiative. One of the metrics used to evaluate a unit’s performance has been their use of implants given a 10A rating by the Orthopaedic Device Evaluation Panel (ODEP). With an abundance of prostheses available,10 our patients will want to know that implants selected have either an established track record or have significant potential benefits that are being actively and carefully evaluated. As already identified ‘me-too’ implant copies have no guarantee of improved or even equivalent clinical outcome.
Despite well-publicised data from the Scandinavian joint registries,11 with supportive evidence in both the NJR3 and Australian registries12, showing improved outcomes from cemented THR, it might have been expected in the light of the ASR debate that there would be a gradual swing back towards cemented fixation with a return to tried and tested prostheses. Economic pressures might also have been expected to have supported such a move. This has not proved to be the case. The proportion of uncemented THAs increased rapidly from 2003 to 2010 and has been relatively stable since then, although there has been a small decrease in 2013.3 The proportion of cemented prostheses has fallen to 33%, while hybrid THRs have increased to 20% of the total (Fig. 1).
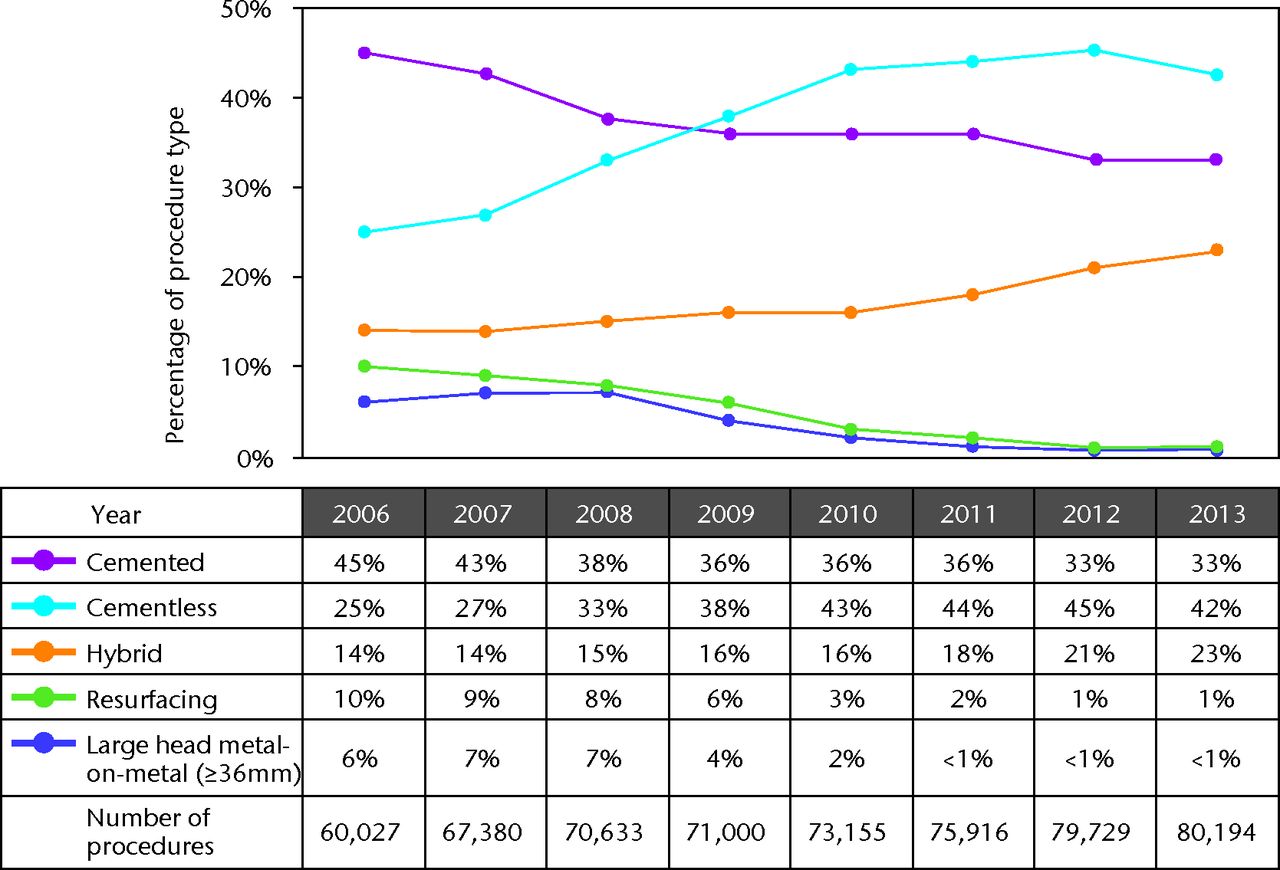
Fig. 1
Temporal changes in percentages of each fixation method used in primary hip arthroplasties.
[]FigNote]]Reproduced with permission from the National Joint Registry 2014 (www.njrreports.org.uk).
One very important factor is that the most common failure mechanism in THR is related to bearing surface wear and osteolysis. The significance of the bearing surface combination in implant survival has to date, in our opinion, been under-evaluated. Recent registry reports have identified this as an extremely important variable. In this regard it is not surprising to note that the use of large diameter metal bearings (both THA and resurfacing) (Fig. 2) have decreased to their lowest ever level.
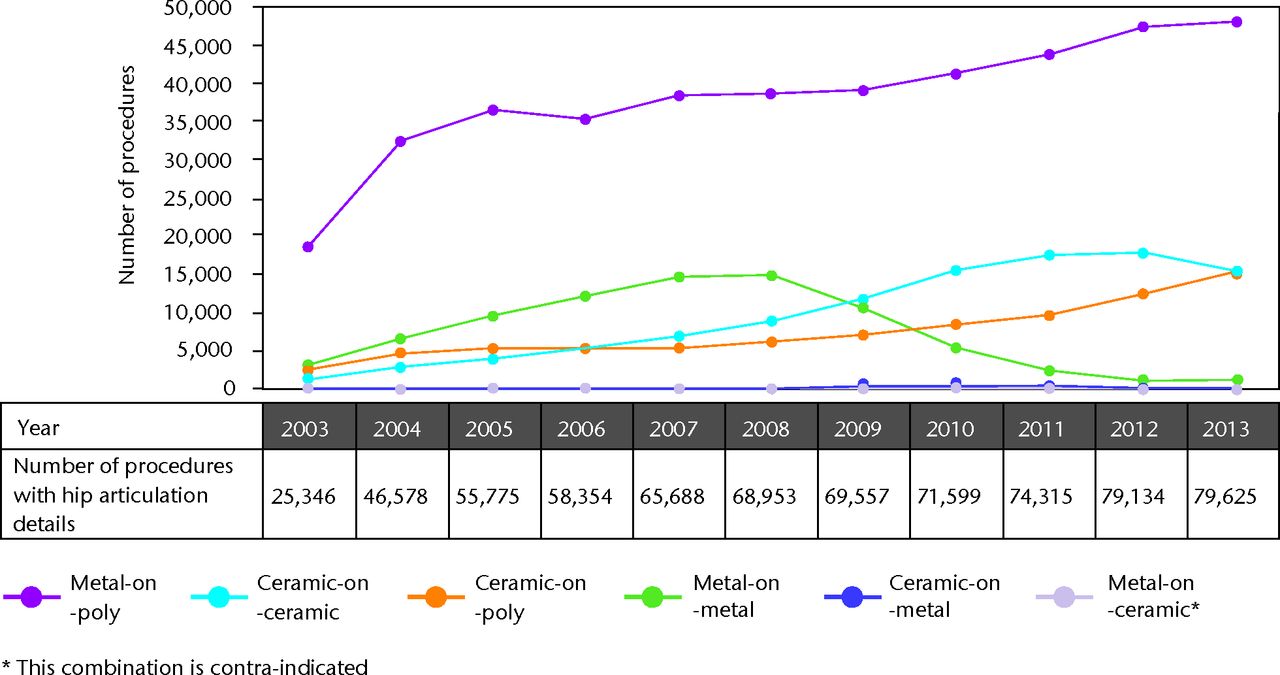
Fig. 2
Hip articulation bearing surface trends 2003-2013.
Reproduced with permission from the NJR (www.njrreports.org.uk)
There has been concern that this approach to implant utilisation may stifle innovation and indeed it is important to identify that implants as yet unclassified or classified at a 3A level by ODEP may in time prove to be just as good and perhaps even better than the current 10A standard. In part due to well-publicised problems with the inadequate CE mark regulatory framework,13 the BOA has introduced the Beyond Compliance programme designed to follow and evaluate new implants, allowing their introduction in a controlled fashion in an attempt to avoid the problems that have affected new implants in the past.14
The perfect hip arthroplasty
There are a wide variety of variables that a surgeon must bear in mind when deciding on which implant. Different concepts in fixation and bearing surface must be considered to give the optimum result for any one patient. One size quite simply does not fit all. As well as the primary concern of longevity, factors such as the age of the patient, activity requirements, bone quality, comorbidities, bone stock, and the general likelihood that a patient might require a revision must all be considered. There are recent controversies in all of these areas and the contribution of all of these variables must be evaluated to allow the surgeon to decide on personalised optimised arthroplasty for each patient. Hip arthroplasty is a complex intervention and like all complex interventions each factor acts not in isolation but as part of a complete treatment episode. Simple changes (such as trunnion design, surgical approach, or rehabilitation regimes) can have unintended knock-on consequences.
Approach
There have been long-running arguments between orthopaedic surgeons over the ‘ideal’ surgical approach for a THA. Traditionally this has been between proponents of the posterior and lateral (including Hardinge) approaches, but in more recent years the Direct Anterior Approach (DAA), more commonly used in Europe, has gained popularity. In UK practice, 65% of THAs are implanted via the posterior approach, 31% via lateral approaches, < 1% using the trochanteric osteotomy approach and 4% via other approaches.3 In recent years there has been a trend towards the posterior approach and away from the various lateral approaches.
Each approach has its advantages and disadvantages. Traditionally the lateral approach has been associated with a historically lower dislocation rate but a higher rate of abductor dysfunction and has the potential for Trendelenburg-positive gait. However, more recent studies using improved soft-tissue repair, modular implants and larger bearing surfaces show that there are a few differences between the approaches in terms of complication rate, all-cause revision and revision for dislocation rate at 12 months.15 However for those patients where patient-reported outcome measures (PROMS) are available, the posterior approach results in higher Oxford Hip Scores and EQ5D scores.15-17 It has also been suggested in a review from the NJR that the posterior approach is associated with a significantly reduced mortality risk compared with other approaches,18 although it is difficult to be sure that this causally linked.
More recently the direct anterior approach (DAA) has gained popularity both in the UK and abroad. Implant companies have proposed components specifically intended for use with this approach, producing not only the implant but also specialist equipment and operating tables. Proponents of the DAA report a quicker recovery due to the muscle-sparing nature of the approach as well as the small size of the incision. It is widely accepted that the approach does have a learning curve quoted to be anywhere from 2019 to 100 cases.20 A recent comparison of DAA with a mini-posterior approach showed that the DAA was associated with higher visual pain analogue scores, longer operative times and increased use of walking aids at two weeks. There was no difference in the hospital length of stay. By eight weeks, the DAA cohort had a higher Harris Hip Score but a lower rate of return to work and driving.21 Interestingly, this study also showed a higher rate of wound complications in the posterior approach group, but another study by Christensen et al showed that the anterior approach had more wound issues requiring a return to theatre22, and Amlie et al16 showed no PROMS differences between the anterior and posterior approaches.17 The evidence, certainly for the moment, is not clear on the benefits or otherwise of the DAA.
It is not the first time that smaller incisions and less traumatic approaches have been developed in an attempt to improve recovery following THR. While increased complication rates have been shown using some minimally invasive (MIS) approaches and the dual-incision approach is now rarely used, reduced access and ‘adequately invasive surgery’, in both lateral and posterior approaches, has become popular.
Literature in this area has been mixed. In a well-designed RCT, MIS performed by an experienced surgeon conferred no benefit in terms of pain scores, blood loss or blood transfusion requirements, or analgesic use.23 Although this study found no difference in the rate of component malposition, it should be noted that other studies have found significant differences not only in terms of adverse component orientation but also increased wound complications, despite the MIS patients being generally healthier and thinner than the standard-incision control group.24
While the debates surrounding surgical approach will continue, it is important to recognise that the discussion has influenced clinical practice and very likely patient experience and outcome. Few surgeons are performing hip arthroplasty with the same size of incision and with same extent of soft-tissue release and exposure as they were 5-10 years ago. Similarly, the advances in, and appreciation of the value of patient education and expectation, as well as in anaesthetic techniques and rehabilitation have had an influence every bit as significant to our patients as that of an ‘enhanced’ surgical exposure.
Implant Choice – fixation
There is supportive evidence that both cemented and uncemented fixation have produced excellent results in hip arthroplasty, yet the debate continues (Fig. 3). It is important to appreciate that there are many reasons why implant revision might be required yet frequently all are combined in reported revision rates. Implant loosening itself can occur for many reasons. Aseptic loosening with fixation failure occurs most commonly secondary to implant wear and the associated biological response. Infection can result in loosening and revision, similarly poor surgical technique might be relevant when cemented or uncemented implants loosen. Revision for dislocation can be required secondary to component malposition, impingement, patient non-compliance and wear. Similarly, with peri-prosthetic fractures revision can be required for reasons that may not directly be associated with failure of fixation. For this reason merely looking at long-term survivorship may not give the whole picture. Surgeons will use techniques which are familiar and they know give good outcomes in their hands. There are however a number of variables that might influence implant fixation choice.
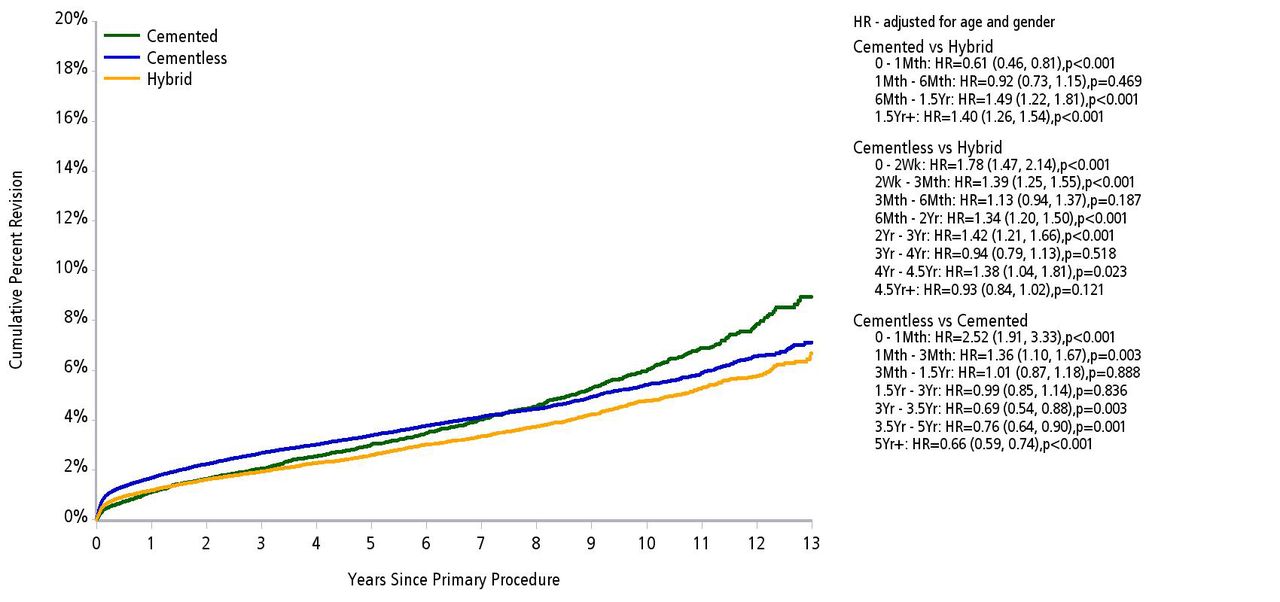
Fig. 3
Cumulative percent revision of primary total conventional hip arthroplasty by fixation (primary diagnosis OA).
Reproduced with permission from the Australian National Joint Replacement Registry Report 2013.
Bone quality and morphology can influence fixation choice. Achieving excellent cement inter-digitation can be a challenge in a ‘Dorr A’ type femur with thick distal cortices and a very narrow canal. Incidentally, this is also a frequently underestimated challenge as the surgeon endeavours to ensure a perfect biomechanical reconstruction. Similarly, a ‘Dorr C’ ‘stovepipe’ femur may be a challenge in which to achieve satisfactory fixation with a number of uncemented stems. The likelihood and complexity of revision, particularly in young and active patients, is a factor to consider. Though with the routine use of improved bearing surface options, the introduction of shorter metaphyseal loading uncemented stems and the advent of ‘cement in cement’ revision techniques25 may be less of an issue in future than it has been in the past.
It is important to understand that uncemented stems are not necessarily technically easier – indeed they have been associated with a higher incidence of leg length discrepancy,26 peri-prosthetic fracture and thigh pain,27 as well as medical negligence litigation.28 There is a significantly increased risk of revision with uncemented implants within the first few weeks of surgery12 that is most likely to be attributed to these potential complications. Ensuring perfect leg length and version can be a challenge when using uncemented fixation, a limitation that is inherent in the design of the stems. Surgeons should appreciate that different concepts in design of uncemented implants may lend themselves to different femoral morphologies.
Recently, cemented hip arthroplasty has been linked with increased mortality, and unhelpful articles about “toxic”29 and “killer”30 hip replacements have caused concern amongst our patients. McMinn et al31 suggested that cemented THAs had long-term higher mortality rates than other fixation methods, although a previous study by Parvizi et al32 showed no significant difference in mortality from the fixation method. A more recent large-scale study of over 400 000 THAs adjusting for multiple co-morbidities also found that fixation was not a significant risk factor for mortality.18
Cost however is very much an issue, and it has been suggested that increased use of cemented components could save health economies large amounts of money, both in terms of implant cost and in decreased revision rates.33 Hybrid THAs have been shown to be the most cost-effective34 and in a related publication the authors demonstrated that uncemented cups with their improved PROMS scores, combined with the lower revision rates of a cemented stem, meant that hybrid THAs performed extremely well overall.35
Implant ‘personalisation’
The concept that each hip replacement should be ‘personalised’ to a particular patient, in an attempt to get the best results, has been put forward by surgeons, implant manufacturers and interestingly some patients. A number of options in this regard have been utilised. There has been an increase in the use of modular necks, perhaps as a consequence of some of the component positioning limitations associated with uncemented stem fixation. This modularity allows the surgeon to compensate for variation in version, varus/valgus angles as well as leg-length and offset. These implants have not been without complications and the addition of another “bearing interface” with potential for trunnion/taper-related problems, corrosion and wear is of the greatest concern (Fig. 4).36 The authors have noted that many implant companies have quietly dropped these from their advertising literature.
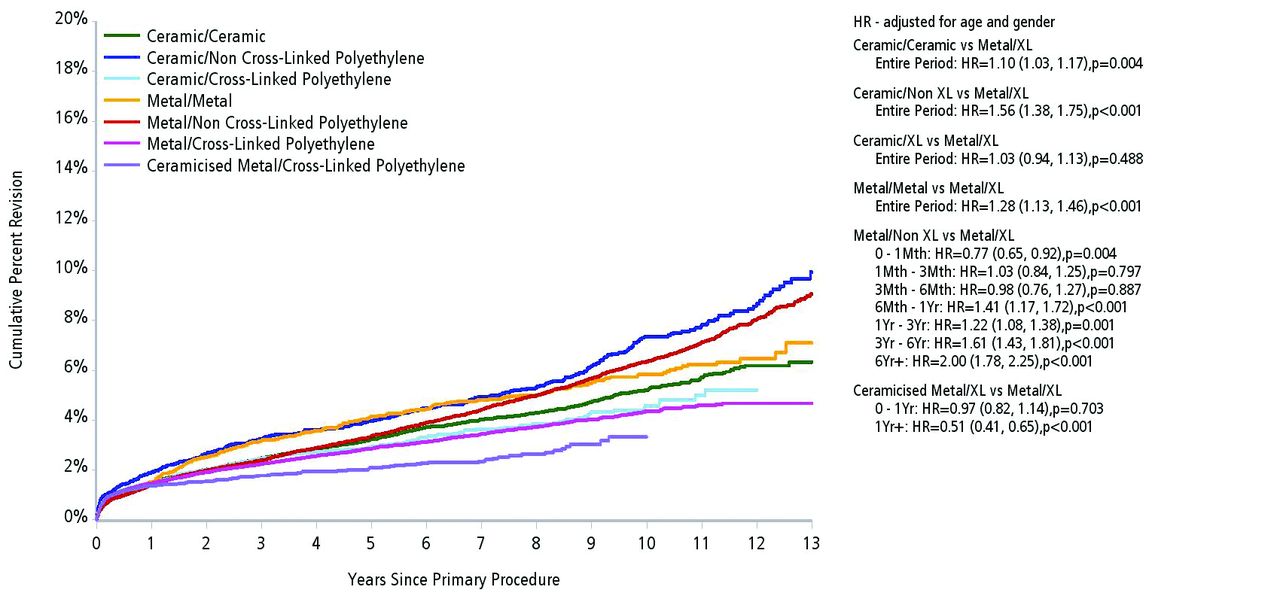
Fig. 4
Cumulative percent revision of primary conventional total hip arthroplasty by bearing surface (primary diagnosis OA). Reproduced with permission from the Australian National Joint Replacement Registry Report 2013.
In total knee arthroplasties (TKAs), there has been a lot of interest in the use of Patient Specific Instrumentation (PSI), although studies generally show benefits in alignment but not in clinical outcomes. Indeed, several papers and review articles have suggested that there is currently no proven value in PSI TKAs.37-39 At present there is little evidence for their use in THA, although one paper shows improved anteversion accuracy when PSI is used.40
Over recent years there has been an increasing interest in the use of computer navigation to improve component alignment and, it is hoped, clinical outcome and implant longevity. Cup position has been improved with navigation,41 and leg-length discrepancy has also been reduced from 1.8 to 0.3 mm with no determinable effect on outcomes from the patient perspective (with PROMS or perception of LLD).42 Present navigation systems can increase surgical time, require additional expense, and can potentially add to complications such as fracture through the drill holes used for array stabilisation. We feel that navigation is unlikely to become more widely adopted without improved simplicity, accuracy and the introduction of more cost effective, largely pin-free systems.
In hip arthroplasty for more complex femoral morphologies, while the ‘flexibility’ in terms of component position of cemented fixation may be of benefit, the use of custom made uncemented femoral stems in cases of previous osteotomy, developmental dysplasia, osteopetrosis, Legg-Calvé-Perthes disease and following trauma has been proposed. There is one system based on 3D CT scanning which has shown an all-cause revision rate of 2.4% at ten years with no incidence of aseptic loosening.43 Other systems using computer-aided design and manufacture to produce custom-made femoral stems have equally good 10 to 17 year outcomes.44 Although it is likely that the majority of patients can be managed with a more standard approach with either cemented or uncemented fixation, these components may still provide a useful addition to the armamentarium in particularly complex cases.
Bearing choices
The search for the optimal bearing surface continues. Catastrophic failures in metal-on-metal bearings (Fig. 2), particularly large diameter metal-on-metal (LDMOM) THA,6,45 has resulted in a precipitous fall in their utilisation. Away from that, metal-on-polyethylene (MOP) continues to have the best outcomes in terms of revision rates3 but ceramic-on-polyethylene (COP) revision rates are equivalent to those of MOP at 12 years.12 Like however needs to be compared with like; the improvements in clinical wear rate between highly cross-linked and traditional polyethylene is widely reported.46 This is likely to result in reduced revision rates for aseptic loosening. While there was no reported advantage of ceramic over metal femoral heads against cross-linked polyethylene in the AOANJRR,12 there may yet be a reduction in revision rates for head fracture with more modern ceramic femoral heads, the outcomr of which will need to be determined over a longer follow-up interval. Polyethylene wear debris can cause osteolysis and loosening, and can be associated with marked bone loss at revision. This has led to the search for a better, harder wearing bearing surface for younger patients likely to need revision during their lifetime.
Ceramic-on-ceramic (COC) is a hard wearing, biologically inert bearing surface that has good wear properties. It does have potential complications, particularly those of fracture and squeaking. Ceramic fracture is perhaps more of a historical worry with the increased use of delta ceramics, and is probably related to implant orientation47 and has been reported to be more common in some implants and in certain implant combinations.48 Therefore outcomes with this bearing, and particularly satisfaction rates, are likely to be implant choice and surgical technique-dependent. Patients are however much more likely to notice an intrusive noise in a COC bearing than a MOM, MOP or COP one.49 Other bearing surfaces such as ceramic-on-metal (COM) have also been tried, but in fairly small numbers and with poor results in the NJR (Fig. 2).3
Polyethylene wear can be reduced by cross-linking resulting in better wear rate characteristics albeit at the potential expense of reduced fatigue strength.50 Concern has also been raised regarding the size of XLPE debris particles which may have a greater osteolytic potential.51 However a meta-analysis comparing XLPE with traditional ultra-high molecular weight polyethylene (UHMWPE) shows decreased radiological osteolysis with XLPE52 and this is maintained at five years.46 While it is noted that long-term XLPE studies are currently lacking, there are encouraging mid-term results in the AOANJRR.12,54
Vitamin E has been used as an antioxidant in polyethylene as an alternative to re-melting; the aim being to improve longer-term oxidative stability and to avoid the reduction in fatigue strength.51 Although in vitro studies are promising with no discernable oxidation at three years,55 there is little clinical in vivo evidence to either support or refute their use. This has not however prevented implant companies from releasing vitamin E diffused polyethylene onto the market.
The use of ceramicised metal such as Oxinium (Oxidised Zirconium, Smith & Nephew Inc., Memphis, Tennessee) is increasing with encouraging results when combined with XLPE in the AOANJRR,12 but again there are few papers detailing clinical evidence and outcomes uip top thirteen years.53
Outcomes
Patient-reported outcome measures (PROMS) are used to assess the success of THA in England & Wales. Each patient has Oxford Hip Score (OHS), EQ-5D and a Visual Analogue Score (VAS) collected pre-operatively and at six months post-operatively. While it is clearly important to ensure our patients do as well as possible and to have an independent review of their own perception of their clinical outcome and the effectiveness of our intervention, just how those parameters can best be determined is unclear. One approach may not fit all in this respect. Different patient populations will have different expectations and single ‘standard’ outcome scoring systems may not reflect this.
Elsewhere there is concern that outcome scores may be affected by extrinsic factors. These vary from medical comorbidities and the existence of other affected joints and may even be influenced by the clinical environment in which patients are seen, whether pre-op scores are determined before or after they have been assessed and listed for surgery, or even the patient’s mood at the time they are completing the forms. This could be influenced by their experience of trying to park at the hospital on the morning of their clinic or a delay waiting for an x-ray!
The use of the OHS as a threshold for referral has been introduced in some healthcare systems; this was not the purpose for which the score was developed and there is no evidence to support its use in this way. At present outcomes are only measured once at around six months; it is perhaps better appreciated with TKAs but also in hips that improvement can continue beyond six months and that patients unhappy at one stage can become very much improved as time progresses (Fig. 4).
Ongoing Controversies
Resurfacing arthroplasty remains a controversial topic. Although it does have a higher failure rate in the NJR, it remains a potentially useful option. Baker et al54 demonstrated that patients with a resurfacing showed improved Oxford Hip Scores, UCLA activity scores and EuroQOL scores compared with THA at the medium term. Hip resurfacing as a procedure has been adversely affected by the more general poor results of metal-on-metal bearings and LDMOM THAs. There are tried and established prostheses on the market such as the Birmingham Hip Resurfacing (BHR, Smith and Nephew, Memphis, Tennessee), which have good medium term outcomes in both designer57,58 and independent59 series and in a young and active population. Excellent surgical technique, sound component alignment, careful patient selection and patient education are important variables in the use of this technology. Although the numbers of resurfacing arthroplasties undertaken are at the lowest level ever recorded in the NJR, it appears that the BHR has increased its market share at the expense of other designs.3 It is likely that resurfacing will be performed by a small number of surgeons and mostly reserved for men with a large femoral head size; as such, and in younger patients it can still be an excellent femoral bone-preserving procedure.
The search for bone preservation has led to the development and introduction of shorter stemmed versions of standard THAs as well as more novel designs aiming to fix either in the neck with no shaft extension or in the proximal metaphysis. A review of these stem designs and a proposed classification is described by Feyen and Shimmin.60 There are multiple short stems available and only a few medium term studies; as such there is no long-term outcome data behind these implants. There is no readily available literature supporting the use of neck-bearing prostheses, and it is perhaps concerning that the use of these implants continues to be encouraged despite a lack of evidence.
Conclusion
Total hip arthroplasty remains an excellent operation that frequently transforms the quality of life of our patients. While there has been, and will always be debate about the potential benefits of different approaches, fixation concepts, implants, bearing surfaces and a variety of rehabilitation protocols, we feel that the best outcomes will be obtained by a versatile approach. Surgeons should consider each patient’s individual needs, anatomy and outcome expectations. Surgeons who perform the procedure should ensure their approach allows excellent visualisation to ensure perfect component orientation, soft-tissue balance and biomechanics. Versatility in fixation and bearing surface options is likely to be helpful as we continue to strive for perfection in total hip arthroplasty surgery.
1 Learmonth ID , YoungC, RorabeckC. The operation of the century: total hip replacement. Lancet2007;370:1508–1519.CrossrefPubMed Google Scholar
2 Chang RW , PellisierJM, HazenGB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA1996;275:858–865.PubMed Google Scholar
3 No authors listed. National Joint Regsistry: 11th Annual Report, 2014. http://www.njrcentre.org.uk/njrcentre/NewsandEvents/NJR11thAnnualReport/tabid/363/Default.aspx (date last accessed 12 January 2015). Google Scholar
4 Massoud SN , HunterJB, HoldsworthBJ, WallaceWA, JuliussonR. Early femoral loosening in one design of cemented hip replacement. J Bone Joint Surg [Br]1997;79-B:603–608.CrossrefPubMed Google Scholar
5 Muirhead-Allwood SK . Lessons of a hip failure. BMJ1998;316:644.PubMed Google Scholar
6 Langton DJ , JamesonSS, JoyceTJ, et al.Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg [Br]2011;93-B:1011–1016.CrossrefPubMed Google Scholar
7 Bridgewater B , GraysonAD, BrooksN, et al.Has the publication of cardiac surgery outcome data been associated with changes in practice in northwest England: an analysis of 25,730 patients undergoing CABG surgery under 30 surgeons over eight years. Heart2007;93:744–748.CrossrefPubMed Google Scholar
8 Michaëlsson K . Surgeon volume and early complications after primary total hip arthroplasty. BMJ2014;348:3433.CrossrefPubMed Google Scholar
9 No authors listed. National Joint Registry. http://www.njrsurgeonhospitalprofile.org.uk (date last accessed 30 November 2014). Google Scholar
10 Kynaston-Pearson F , AshmoreAM, MalakTT, et al.Primary hip replacement prostheses and their evidence base: systematic review of literature. BMJ2013;347:6956.CrossrefPubMed Google Scholar
11 Mäkelä KT , MatilainenM, PulkkinenP, et al.Failure rate of cemented and uncemented total hip replacements: register study of combined Nordic database of four nations. BMJ2014;348:7592.CrossrefPubMed Google Scholar
12 No authors listed Australian Orthopaedic Association: National Joint Replacement Registry; Annual Report, 2013. https://aoanjrr.dmac.adelaide.edu.au/annual-reports-2013 (date last accessed 12 January 2015). Google Scholar
13 Cohen D . How a fake hip showed up failings in European device regulation. BMJ2012;345:7090.CrossrefPubMed Google Scholar
14 Phillips JR , JamesP. Orthopaedics in the UK is ahead of proposed regulations for incremental innovation in medical devices. BMJ2014;349:5894.CrossrefPubMed Google Scholar
15 Jameson SS , MasonJ, BakerP, et al.A comparison of surgical approaches for primary hip arthroplasty: a cohort study of patient reported outcome measures (PROMs) and early revision using linked national databases. J Arthroplasty2014;29:1248–1255.CrossrefPubMed Google Scholar
16 Lindgren JV , WretenbergP, KärrholmJ, GarellickG, RolfsonO. Patient-reported outcome is influenced by surgical approach in total hip replacement: a study of the Swedish Hip Arthroplasty Register including 42,233 patients. Bone Joint J2014;96-B:590–596.CrossrefPubMed Google Scholar
17 Amlie E , HavelinLI, FurnesO, et al.Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty. A cross-sectional questionnaire study of 1,476 patients 1-3 years after surgery. Acta Orthop2014;85:463–469.CrossrefPubMed Google Scholar
18 Hunt LP , Ben-ShlomoY, ClarkEM, et al.90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet2013;382:1097–1104.CrossrefPubMed Google Scholar
19 Müller DA , ZinggPO, DoraC. Anterior minimally invasive approach for total hip replacement: five-year survivorship and learning curve. Hip Int2014;24:277–283.CrossrefPubMed Google Scholar
20 Masonis J , ThompsonC, OdumS. Safe and accurate: learning the direct anterior total hip arthroplasty. Orthopedics2008;31(12Suppl2).:.PubMed Google Scholar
21 Poehling-Monaghan KL, Kamath AF, Taunton MJ, Pagnano MW. Direct Anterior versus Miniposterior THA With the Same Advanced Perioperative Protocols: Surprising Early Clinical Results. Clin Orthop Relat Res 2014;(Epub ahead of print) PMID : 19298019. Google Scholar
22 Christensen CP , KarthikeyanT, JacobsCA. Greater prevalence of wound complications requiring reoperation with direct anterior approach total hip arthroplasty. J Arthroplasty2014;29:1839–1841.CrossrefPubMed Google Scholar
23 Ogonda L , WilsonR, ArchboldP, et al.A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg [Am]2005;87-A:701–710. Google Scholar
24 Woolson ST , MowCS, SyquiaJF, LanninJV, SchurmanDJ. Comparison of primary total hip replacements performed with a standard incision or a mini-incision. J Bone Joint Surg [Am]2004;86-A:1353–1358. Google Scholar
25 Duncan WW , HubbleMJW, HowellJR, et al.Revision of the cemented femoral stem using a cement-in-cement technique: a five- to 15-year review. J Bone Joint Surg [Br]2009;91-B:577–582.CrossrefPubMed Google Scholar
26 Ahmad R , SharmaV, SandhuH, BishayM. Leg length discrepancy in total hip arthroplasty with the use of cemented and uncemented femoral stems. A prospective radiological study. Hip Int2009;19:264–267.CrossrefPubMed Google Scholar
27 Su EP , BarrackRL. Cementless femoral fixation: not all stems are created equally. Bone Joint J2013;95-B(11SupplA):53–56. Google Scholar
28 Whittingham-Jones P , WilliamsD, RajaS, BridleS, BircherM. Negligence claims in UK total hip arthroplasty: a series of 167 consecutive cases. Med Leg J2012;80(Pt4):157–161.CrossrefPubMed Google Scholar
29 Prynne M, Knapton S. The Telegraph, 2014. http://www.telegraph.co.uk/health/nhs/10896853/Toxic-NHS-hip-implants-blamed-for-more-than-40-deaths.html (date last accessed 12 January 2015). Google Scholar
30 30. Borland S. The Daily Mail. http://www.dailymail.co.uk/health/article-2656762/Alert-killer-cement-used-hip-replacements-41-patients-die-operating-table-seven-years-warns-study.html (date last accessed 12 January 2015). Google Scholar
31 McMinn DJ , SnellKI, DanielJ, et al.Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ2012;344:3319.CrossrefPubMed Google Scholar
32 Parvizi J , JohnsonBG, RowlandC, ErethMH, LewallenDG. Thirty-day mortality after elective total hip arthroplasty. J Bone Joint Surg [Am]2001;83-A:1524–1528.CrossrefPubMed Google Scholar
33 Griffiths EJ , StevensonD, PorteousMJ. Cost savings of using a cemented total hip replacement: an analysis of the National Joint Registry data. J Bone Joint Surg [Br]2012;94-B:1032–1035.CrossrefPubMed Google Scholar
34 Pennington M , GrieveR, SekhonJS, et al.Cemented, cementless, and hybrid prostheses for total hip replacement: cost effectiveness analysis. BMJ2013;346:1026.CrossrefPubMed Google Scholar
35 Pennington M , GrieveR, BlackN, van der MeulenJH. Functional outcome, revision rates and mortality after primary total hip replacement--a national comparison of nine prosthesis brands in England. PLoS One2013;8:73228.CrossrefPubMed Google Scholar
36 Krishnan H , KrishnanSP, BlunnG, SkinnerJA, HartAJ. Modular neck femoral stems. Bone Joint J2013;95-B:1011–1021.CrossrefPubMed Google Scholar
37 Barrack RL , RuhEL, WilliamsBM, et al.Patient specific cutting blocks are currently of no proven value. J Bone Joint Surg [Br]2012;94-B(supplA):95–99.CrossrefPubMed Google Scholar
38 Krishnan SP , DawoodA, RichardsR, HenckelJ, HartAJ. A review of rapid prototyped surgical guides for patient-specific total knee replacement. J Bone Joint Surg [Br]2012;94-B:1457–1461.CrossrefPubMed Google Scholar
39 Voleti PB , HamulaMJ, BaldwinKD, Lee G-C. Current data do not support routine use of patient-specific instrumentation in total knee arthroplasty. J Arthroplasty2014;29:1709–1712. Google Scholar
40 Small T , KrebsV, MolloyR, et al.Comparison of acetabular shell position using patient specific instruments vs. standard surgical instruments: a randomized clinical trial. J Arthroplasty2014;29:1030–1037.CrossrefPubMed Google Scholar
41 Lass R , KubistaB, OlischarB, et al.Total hip arthroplasty using imageless computer-assisted hip navigation: a prospective randomized study. J Arthroplasty2014;29:786–791.CrossrefPubMed Google Scholar
42 Licini DJ , BurnikelDJ, MeneghiniRM, OchsnerJL. Comparison of limb-length discrepancy after THA: with and without computer navigation. Orthopedics2013;36:543–547.CrossrefPubMed Google Scholar
43 Benum P , AamodtA. Uncemented custom femoral components in hip arthroplasty. A prospective clinical study of 191 hips followed for at least 7 years. Acta Orthop2010;81:427–435.CrossrefPubMed Google Scholar
44 Muirhead-Allwood S , SandifordNA, SkinnerJA, et al.Uncemented computer-assisted design-computer-assisted manufacture femoral components in revision total hip replacement: a minimum follow-up of ten years. J Bone Joint Surg [Br]2010;92-B:1370–1375.CrossrefPubMed Google Scholar
45 Langton DJ , JamesonSS, JoyceTJ, et al.Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg [Br]2010;92-B:38–46.CrossrefPubMed Google Scholar
46 Kurtz SM , GawelHA, PatelJD. History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res2011;469:2262–2277.CrossrefPubMed Google Scholar
47 Walter WL , O’tooleGC, WalterWK, EllisA, ZicatBA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty2007;22:496–503.CrossrefPubMed Google Scholar
48 Owen DH , RussellNC, SmithPN, WalterWL. An estimation of the incidence of squeaking and revision surgery for squeaking in ceramic-on-ceramic total hip replacement: a meta-analysis and report from the Australian Orthopaedic Association National Joint Registry. Bone Joint J2014;96-B:181–187.CrossrefPubMed Google Scholar
49 Wyatt MC , JesaniS, FramptonC, DevaneP, HorneJG. Noise from total hip replacements: a case-controlled study. Bone Joint Res2014;3:183–186.CrossrefPubMed Google Scholar
50 Baker DA , HastingsRS, PruittL. Study of fatigue resistance of chemical and radiation crosslinked medical grade ultrahigh molecular weight polyethylene. J Biomed Mater Res1999;46:573–581.CrossrefPubMed Google Scholar
51 Rajpura A , KendoffD, BoardTN. The current state of bearing surfaces in total hip replacement. Bone Joint J2014;96-B:147–156.CrossrefPubMed Google Scholar
52 Kuzyk PRT , SacconeM, SpragueS, et al.Cross-linked versus conventional polyethylene for total hip replacement: a meta-analysis of randomised controlled trials. J Bone Joint Surg [Br]2011;93-B:593–600.CrossrefPubMed Google Scholar
53 Bragdon CR , DoernerM, MartellJ, et al.The 2012 John Charnley Award: Clinical multicentre studies of the wear performance of highjly crosslinked remelted polyethylene in THA. Clin Orthop Relat Res2013;471:393–402. Google Scholar
54 Babovic N , TrousdaleRT. Total hip arthroplasty using highly cross-linked polyethylene in patients younger than 50 years with minimum 10-year follow-up. J Arthroplasty2013;28:815–817.CrossrefPubMed Google Scholar
55 Rowell SL , OralE, MuratogluOK. Comparative oxidative stability of α-tocopherol blended and diffused UHMWPEs at 3 years of real-time aging. J Orthop Res2011;29:773–780.CrossrefPubMed Google Scholar
56 Baker RP , PollardTCB, Eastaugh-WaringSJ, BannisterGC. A medium-term comparison of hybrid hip replacement and Birmingham hip resurfacing in active young patients. J Bone Joint Surg [Br]2011;93-B:158–163.CrossrefPubMed Google Scholar
57 Daniel J , PradhanC, ZiaeeH, PynsentPB, McMinnDJW. Results of Birmingham hip resurfacing at 12 to 15 years: a single-surgeon series. Bone Joint J2014;96-B:1298–1306.CrossrefPubMed Google Scholar
58 Matharu GS , McBrydeCW, PynsentWB, PynsentPB, TreacyRBC. The outcome of the Birmingham Hip Resurfacing in patients aged < 50 years up to 14 years post-operatively. Bone Joint J2013;95-B:1172–1177. Google Scholar
59 Murray DW , GrammatopoulosG, PanditH, et al.The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg [Br]2012;94-B:1180–1186.CrossrefPubMed Google Scholar
60 Feyen H , ShimminAJ. Is the length of the femoral component important in primary total hip replacement?Bone Joint J2014;96-B:442–448.CrossrefPubMed Google Scholar









