Abstract
Aims
The aim of this study was to describe variation in hip fracture treatment in Norway expressed as adherence to international and national evidence-based treatment guidelines, to study factors influencing deviation from guidelines, and to analyze consequences of non-adherence.
Methods
International and national guidelines were identified and treatment recommendations extracted. All 43 hospitals routinely treating hip fractures in Norway were characterized. From the Norwegian Hip Fracture Register (NHFR), hip fracture patients aged > 65 years and operated in the period January 2014 to December 2018 for fractures with conclusive treatment guidelines were included (n = 29,613: femoral neck fractures (n = 21,325), stable trochanteric fractures (n = 5,546), inter- and subtrochanteric fractures (n = 2,742)). Adherence to treatment recommendations and a composite indicator of best practice were analyzed. Patient survival and reoperations were evaluated for each recommendation.
Results
Median age of the patients was 84 (IQR 77 to 89) years and 69% (20,427/29,613) were women. Overall, 79% (23,390/29,613) were treated within 48 hours, and 80% (23,635/29,613) by a surgeon with more than three years’ experience. Adherence to guidelines varied substantially but was markedly better in 2018 than in 2014. Having a dedicated hip fracture unit (OR 1.06, 95%CI 1.01 to 1.11) and a hospital hip fracture programme (OR 1.16, 95% CI 1.06 to 1.27) increased the probability of treatment according to best practice. Surgery after 48 hours increased one-year mortality significantly (OR 1.13, 95% CI 1.05 to 1.22; p = 0.001). Alternative treatment to arthroplasty for displaced femoral neck fractures (FNFs) increased mortality after 30 days (OR 1.29, 95% CI 1.03 to 1.62)) and one year (OR 1.45, 95% CI 1.22 to 1.72), and also increased the number of reoperations (OR 4.61, 95% CI 3.73 to 5.71). An uncemented stem increased the risk of reoperation significantly (OR 1.23, 95% CI 1.02 to 1.48; p = 0.030).
Conclusion
Our study demonstrates a substantial variation between hospitals in adherence to evidence-based guidelines for treatment of hip fractures in Norway. Non-adherence can be ascribed to in-hospital factors. Poor adherence has significant negative consequences for patients in the form of increased mortality rates at 30 and 365 days post-treatment and in reoperation rates.
Cite this article: Bone Joint Open 2020;1-10:644–653.
Take home message
Substantial variation in hip fracture treatment in Norway, despite established evidence-based guidelines.
Deviation from best practice has negative consequences for patient outcomes.
Dissemination of information on best practice through guidelines is challenging.
Introduction
Hip fractures in older people represent a devastating injury for the individual, and treatment is followed by elevated mortality, reduced quality of life and disability.1 Surgery is the only effective treatment, and with the increasing longevity of the population hip fractures represent a steadily growing and substantial burden for hospitals and social services in our societies.2
The concept of variation in health care treatment was pioneered by John Wennberg.3 Annual reports from the Norwegian Hip Fracture Register (NHFR) have shown significant variations in the treatment of hip fractures in Norway.4 We know that patient preferences can affect variation.3 However, for a surgical emergency such as a hip fracture, patients have little or no influence on the choice of treatment. Unwarranted variation in hip fracture treatment, therefore, depends mostly on the preference of the provider (surgeon and hospital). Treatment guidelines have been introduced to give patients the best evidence-based treatment, thereby reducing unwarranted variation.5-9 Guidelines are also tools to reduce inequity by providing care of equal quality.
The main aim of this paper was, in a national setting, to describe compliance with international and national treatment guidelines and variation in hip fracture treatment based on data from the NHFR. Further aims are to analyze relevant factors explaining deviation from the guidelines and to determine consequences of non-adherence.
Methods
The Norwegian Hip Fracture Register
This is a population-based (5.3 million inhabitants in 2018) national prospective study based on data from the NHFR. The term "hip fracture" denotes patients with femoral neck fractures (FNFs: ICD10 code S72.0), trochanteric (ICD10 code S72.1) and subtrochanteric (ICD10 code S72.2) fractures. The NHFR has collected data on all hip fracture patients admitted to hospitals in Norway since 2005. The NHFR receives a form with information on patients, primary operations, and subsequent reoperations. Information on patients receiving total hip arthroplasty (THA) is primarily registered in the Norwegian Arthroplasty Register (NAR) and subsequently imported to the NHFR.10
Completeness of reporting to the NHFR is evaluated regularly by comparing registry data with the national administrative database (Norwegian Patient Registry) operated by the Norwegian Directorate of Health. Completeness in 2015 to 2016 was 88.2% for osteosynthesis, 94.5% for hemiarthroplasties, and 87.8% for total hip arthroplasties.4
Data from all patients registered with a hip fracture in the NHFR in the five-year period (January 2014 to December 2018) admitted to all 43 hospitals in Norway routinely treating hip fractures were included. Data on patient characteristics (age, sex, American Society of Anesthesiologists grade11 ), fracture type, and treatment information (time from injury to surgery, type of treatment, experience level of the surgeon, and reoperations) were extracted. Information on time from injury to operation, fracture type, and experience level of the surgeon were unavailable for hip fracture patients treated with THA, since this is not recorded in the NAR.
Follow-up
The patients were followed in the NHFR until time of reoperation. Patients without reoperations were censored at time of death or on 31 December 2019. Data on death was provided to NHFR by the Norwegian National Population Register.
Characteristics of Norwegian acute care hospitals/hospital trusts
We performed an online survey of the characteristics of all 43 hospitals (23 hospital trusts) in Norway that routinely treat hip fracture patients. The hospitals varied from small community hospitals with a catchment area of fewer than 30,000 inhabitants to large regional and university hospitals.12 Information was collected on the organization of hip fracture care, presence of hospital treatment policies/guidelines, dedicated unit for hip fracture patients, interdisciplinary care including an orthogeriatric unit, number of beds in the orthopaedic ward(s), number of orthopaedic consultants and specialist registrars/residents, and whether the hospital had 24/7 service for hip fracture patients. We ranked the hospitals by treatment volume (low to high) and then divided them into four volume groups with an equal number of hospitals in each group.
Evidence-based hip fracture guidelines
Guidelines were identified from the Guidelines International Network (GIN),13 using the search terms “hip fracture” and “hip fracture treatment”. We also searched for evidence-based guidelines in BMJ Best Practice and PubMed. We identified six relevant guidelines of high quality. We excluded a Finnish and a German guideline published in their respective native languages. We also added a consensus-based Norwegian guideline.5,14
From international guidelines6-9 we extracted treatment recommendations. They largely coincide with the Norwegian interdisciplinary guideline, which is based on the critical literature review and evidence base published by National Institute for Health and Care Excellence (NICE) in the UK.9 Three of the five guidelines (American Academy of Orthopaedic Surgeons (AAOS), Scottish Intercollegiate Guidelines Network (SIGN), Norwegian Orthopaedic Association (NOF)) address hip fracture treatment in the elderly. The guideline recommendations are summarized in Table I, which also outlines treatment-related and outcome variables where the NHFR could provide information. Guideline summaries were extracted by two experienced orthopaedic surgeons (CK, J-EG).
Table I.
Summary of guideline reccomendations for treatment of hip fractures. The arrow in the final column indicates the direction of effect if the guideline is followed.
| Evidence based guidelines | Concensus based guidelines | ||||||
|---|---|---|---|---|---|---|---|
| Variable | SIGN 20099 | NICE 20117 | AAOS 20148 | ANZ 20146 | NOF 20185,14 | Recommendations and outcomes | |
| Fracture type independent | |||||||
| Experienced surgeon | + | + | N/A | + | + | + | ↓REOP* |
| Timing of surgery | Same or next day | < 24 h | < 48 h | Same or next day | < 24 h | < 48 h | ↓MORT,* ↑PROM* |
| < 48 h | Daytime | ||||||
| Fracture type dependent | |||||||
| Femoral neck | |||||||
| Garden15 1 to 2 (undisplaced) | |||||||
| Screw fixation | + | N/A | + | N/A | + | + | ↓LOS, ↓MORT,* ↑PROM* |
| Garden 3 to 4 (displaced) | |||||||
| Arthroplasty | + | + | + | + | + | + | ↓MORT |
| Cemented stem | + | + | + | + | + | + | ↓REOP,* ↑PROM* |
| Trochanteric | |||||||
| AO/OTA16 A1 | |||||||
| Sliding hip screw | + | + | = | = | + | + | ↓MORT,* ↓REOP,* ↓LOS, ↓OT |
| AO/OTA A2 | |||||||
| Sliding hip screw | + | + | = | = | = | = | |
| Intramedullary nail | = | = | = | = | = | = | |
| Intertrochanteric | |||||||
| AO/OTA A3 incl reverse oblique | |||||||
| Intramedullary nail | + | N/A | + | + | + | + | ↓REOP* |
| Subtrochanteric | |||||||
| Intramedullary nail | + | + | + | + | + | + | ↓REOP* |
-
*
Data available in the NHFR.
-
+, positive effect; =, equipoise; AAOS, American Academy of Ortopaedic Surgeons; ANZ, Australian and New Zealand Hip Fracture Registry; LOS, length of stay; MORT, mortality; N/A, not applicable; NICE, National Institute of Care of Excellence; NOF, Norwegian Orthopaedic Association; OT, operating time; OTA, Orthopaedic Trauma Association; PROM, Patient Related Outcome Measure; REOP, reoperations; SIGN, Scottish Intercollegiate Guidelines Network.
Recommendations independent of type of fracture included data on the time of treatment within 48 hours after injury and on surgeon competence, in the NHFR defined as more than three years of experience with fracture surgery. Fracture type-dependent treatment recommendations included treatment of undisplaced (Garden types 1 and 215) femoral neck fractures (FNFs) with screw fixation (two or three screws or pins), treatment of displaced FNFs (Garden types 3 and 4) with arthroplasty (hemi- or total hip arthroplasty) and use of a cemented stem.
For trochanteric fractures type AO/Orthopaedic Trauma Association (AO/OTA) A1,16 the guidelines recommend a sliding hip screw (SHS) rather than an intramedullary nail (IMN). For intertrochanteric fractures, type AO/OTA A3, and subtrochanteric fractures, the guidelines recommend IMN. For trochanteric fractures, type AO/OTA A2, there is equipoise between SHS and IMN. These fractures were therefore not included in the analysis.
We estimated the proportion of patients receiving treatment fulfilling the guideline recommendations described in Table I, i.e. treatment within 48 hours; y a surgeon with more than three years’ of experience; and using fracture-specific recommended treatment. This composite best practice indicator, reflecting and summarizing adherence to guideline recommendations, was calculated for each fracture-specific group. We also estimated best practice for all hip fractures as a group, i.e. practice that fulfilled the guideline criteria for all fracture types.
The NHFR contained data on 41,699 patients treated for a hip fracture in the five-year period between January 2014 and December 2018 (Figure 1). We excluded in sequential order patients with pathological fractures (treatment based on surgeon discretion), patients younger than 65 years (the focus was on elderly patients), patients with ASA grade 5 (moribund patients at operation), or with missing information on ASA grade. Similarly, patients with fracture types with equal recommendations in the guidelines (basocervical fractures and multifragmented trochanteric fractures, type AO/OTA A2), combined fracture types and those in whom fracture type was missing were excluded. Subsequently, 29,613 patients were included in the study: 21,325 FNF, 5,546 trochanteric and 2,742 sub- or intertrochanteric fractures (Figure 1). We included 20,427 women and 9,186 men, with median age 84 years (interquartile range (IQR) 78 to 89) and 83 years (IQR 75 to 88) respectively. Patient characteristics and fracture types are outlined in Table II.
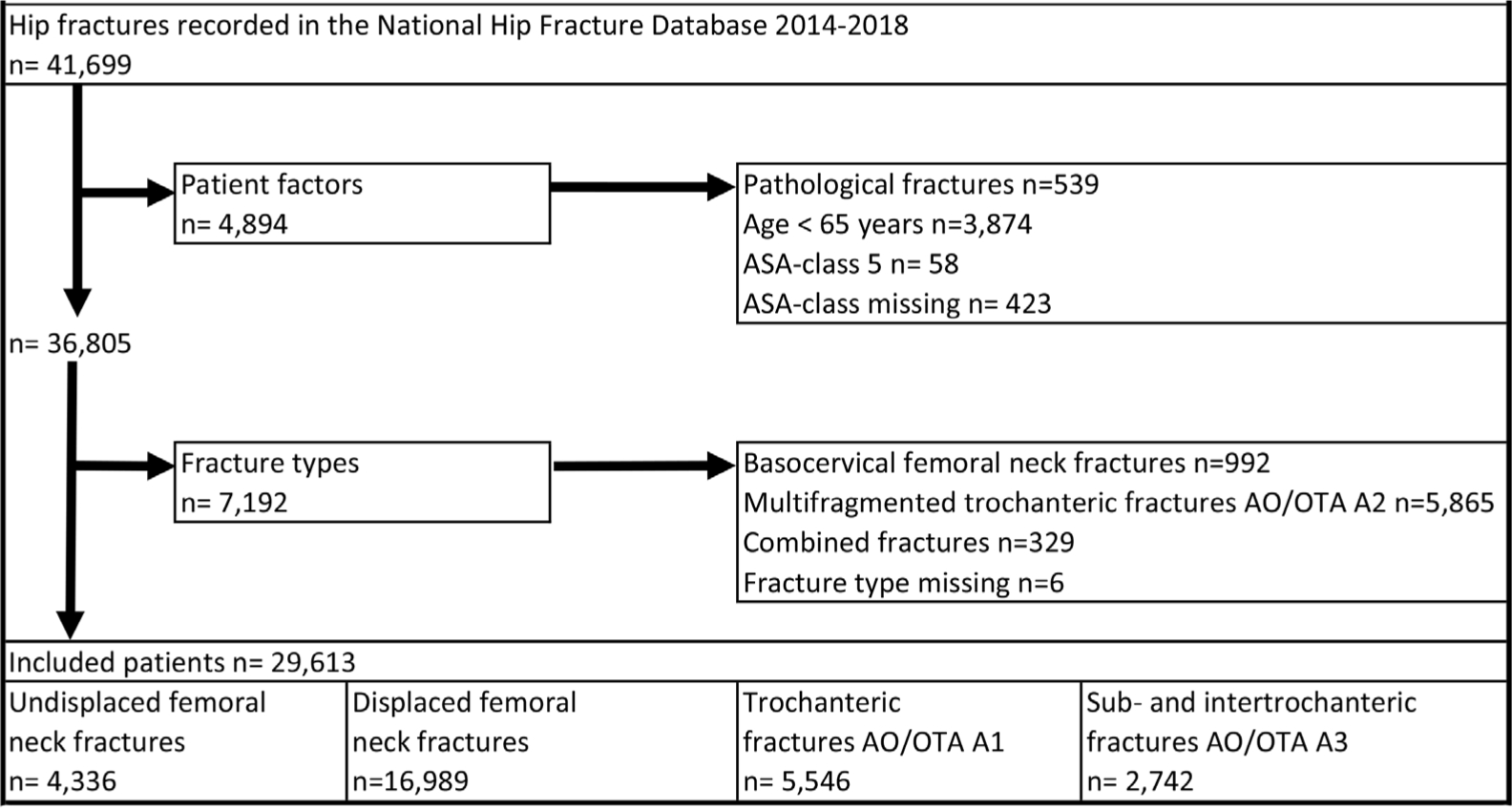
Fig. 1
Patient selection-study population. OTA, Orthopaedic Trauma Association; ASA, American Society of Anesthesiologists.
Statistical analysis
The analysis was performed using SAS/STAT for Windows v. 7.1 (SAS Institute, Cary, North Carolina, USA). Continuous variables are presented as medians and ranges for patients and hospital characteristics. Treatment distribution is presented in numbers and percentages. Adherence to guideline recommendations was calculated as a mean of annual proportions of patients treated according to the recommendations described. This was performed for each hospital over the study period and adjusted for age and sex. We used logistic regression (LR) models to measure the effect of the predictors of adherence and results are presented as odds ratios (ORs). All analyses were adjusted for age, sex, and ASA class. For all LR analyses, a 95% confidence interval (CI) was calculated and p-values below 0.05 were considered statistically significant.
Ethics, funding and conflict of interest
The project was approved by the Northern Norway Regional Committee for Medical and Health Research Ethics and was exempted from the duty of confidentiality (REK 2018/1955). A data protection integrity assessment was compiled according to the EU General Data Protection Regulation (GDPR). The project was funded by the Northern Norway Regional Health Authority (HNF1482-19). No competing interests were declared.
The NHFR is authorized by the Norwegian Data Protection Authority to collect and store data on hip fracture patients (authorisation issued 3 January 2005; reference number 2004/1658 to 2 SVE/-). The NHFR required patients to sign a written, informed consent declaration, and when unable to understand or sign, a family member could sign the consent form on their behalf. The NHFR is financed by the Western Norway Regional Health Authority.
Results
Patient and treatment characteristics
Overall, two-thirds of the patients had severe comorbidity (ASA class 3 to 4; n = 19,682). A majority of the patients were treated within 48 hours of injury and by an experienced surgeon (79%; n = 23,390). FNFs were most prevalent (72%; n = 21,325). Fracture treatment is outlined in Table III. Most (86%; n = 3,747) undisplaced FNFs were treated with screw fixation, whereas almost all (96%; n = 16,219) displaced FNFs were treated with arthroplasty. In all, 68% of trochanteric fractures received SHS (n = 3783) while IMN was used in 76% (n = 2,084) of inter- and subtrochanteric fractures.
Table II.
Population characteristics.
| Variable | n (%) |
|---|---|
| Study population | 29,613 |
| Women | 20,427 (69.0) |
| Men | 9,186 (31.0) |
| Median age, yrs (IQR) | 84 (77 to 89) |
| ASA grade | |
| 1 | 538 (1.8) |
| 2 | 9,393 (31.7) |
| 3 | 17,251 (58.3) |
| 4 | 2,431 (8.2) |
| Surgeon experience in fracture surgery | |
| < 3 years | 4,686 (15.8) |
| > 3 years | 23,635 (79.8) |
| Missing | 1,292 (4.4) |
| Time of surgery after injury | |
| < 48 hours | 23,390 (79.0) |
| > 48 hours | 4,931 (16.6) |
| Missing | 1,292 (4.4) |
| Fracture type | |
| Undisplaced femoral neck (Garden 1 to 2) | 4,336 (14.6) |
| Displaced femoral neck (Garden 3 to 4) | 16,989 (57.4) |
| Trochanteric AO/OTA A1 | 5,546 (18.7) |
| Intertrochanteric AO/OTA A3 | 879 (3.0) |
| Subtrochanteric | 1,863 (6.3) |
-
ASA, American Society of Anaesthesiologists; IQR, interquartile range; OTA, Orthopaedic Trauma Association.
Table III.
Treatment distribution in 29,613 patients with a hip fracture.
| Category, n (%) | Total | Screw fixation | Arthroplasty | SHS | IMN | Other |
|---|---|---|---|---|---|---|
| Undisplaced FNF (Garden 1 to 2) | 4,336 | 3,747 (86.4) | 463 (10.7) | 90 (2.1) | 11 (0.3) | 25 (0.6) |
| Displaced FNF (Garden 3 to 4) | 16,989 | 605 (3.6) | 16,219 (95.5) | 76 (0.4) | 20 (0.1) | 69 (0.4) |
| Trochanteric fracture AO/OTA A1 | 5,546 | 4 ( < 0.1) | 10 (0.2) | 3,783 (68.2) | 1,651 (29.8) | 98 (1.8) |
| Intertrochanteric fracture AO/OTA A3 | 1,863 | 3 (0.2) | 1 ( < 0.1) | 335 (18.0) | 1,518 (81.5) | 6 (0.3) |
| Subtrochanteric | 879 | 0 | 8 (0.9) | 308 (35.0) | 554 (63.0) | 9 (1.0) |
-
FNF, femoral neck fracture; IMN, intramedullary nail; OTA, Orthopaedic Trauma Association; SHS, sliding hip screw.
Hospital characteristics
Treatment volume and organization of orthopaedic services are given in Table IV. The majority of hospitals (74%; n = 32)) reported having a separate orthopaedic ward, a hospital hip fracture programme (86%; n = 37)) and 24/7 service for hip fracture patients (86%; n = 37)). A dedicated hip fracture unit was present in 26% of the hospitals (n = 11), while an orthogeriatric service was present in 33% (n = 14). The hospitals had a median of seven orthopaedic consultants (IQR 5 to 17) and seven specialist registrars/residents (IQR 3 to 9) in orthopaedic surgery. In the study period, the median hospital patient volume was 553 (IQR 309 to 892).
Table IV.
Hospital characteristics (2018 data).
| Variable | Total | Median (IQR) |
|---|---|---|
| Population base in catchment area | 5,300,000 | 82,000 (42,000 to 140,000) |
| Orthopaedic consultants | 481 | 7 (5 to 17) |
| Orthopeadic specialist registrar/resident | 284 | 7 (3 to 9) |
| Orthopaedic beds in hospital | 1,053 | 21 (12 to 30) |
| Hip fracture volume, 2014 to 2018 (total) | 41,699 | 777 (444 to 1,238) |
| Hip fracture volume, 2014 to 2018 (included in study) | 29,613 | 553 (309 to 892) |
| Low (11 hospitals) | 2,213 | 238 (83 to 276) |
| Intermediate low (11 hospitals) | 5,331 | 480 (450 to 533) |
| Intermediate high (11 hospitals) | 8,030 | 696 (615 to 862) |
| High (10 hospitals) | 14,039 | 1,327 (1,018 to 1,809) |
| Hospitals routinely treating hip fractures, n (%) | 43 (100) | |
| Separate orthopaedic ward, n (%) | 32 (74) | |
| Dedicated hip fracture unit, n (%) | 11 (26) | |
| Orthogeriatric service, n (%) | 14 (33) | |
| Hospital hip fracture programme, n (%) | 37 (86) | |
| 24/7 service for hip fracture patients, n (%) | 37 (86) |
Hospital adherence to guidelines
Variation in adherence to guideline recommendations (described in Table I) related to hospital category (volume groups) has also been estimated and is illustrated in Figure 2.
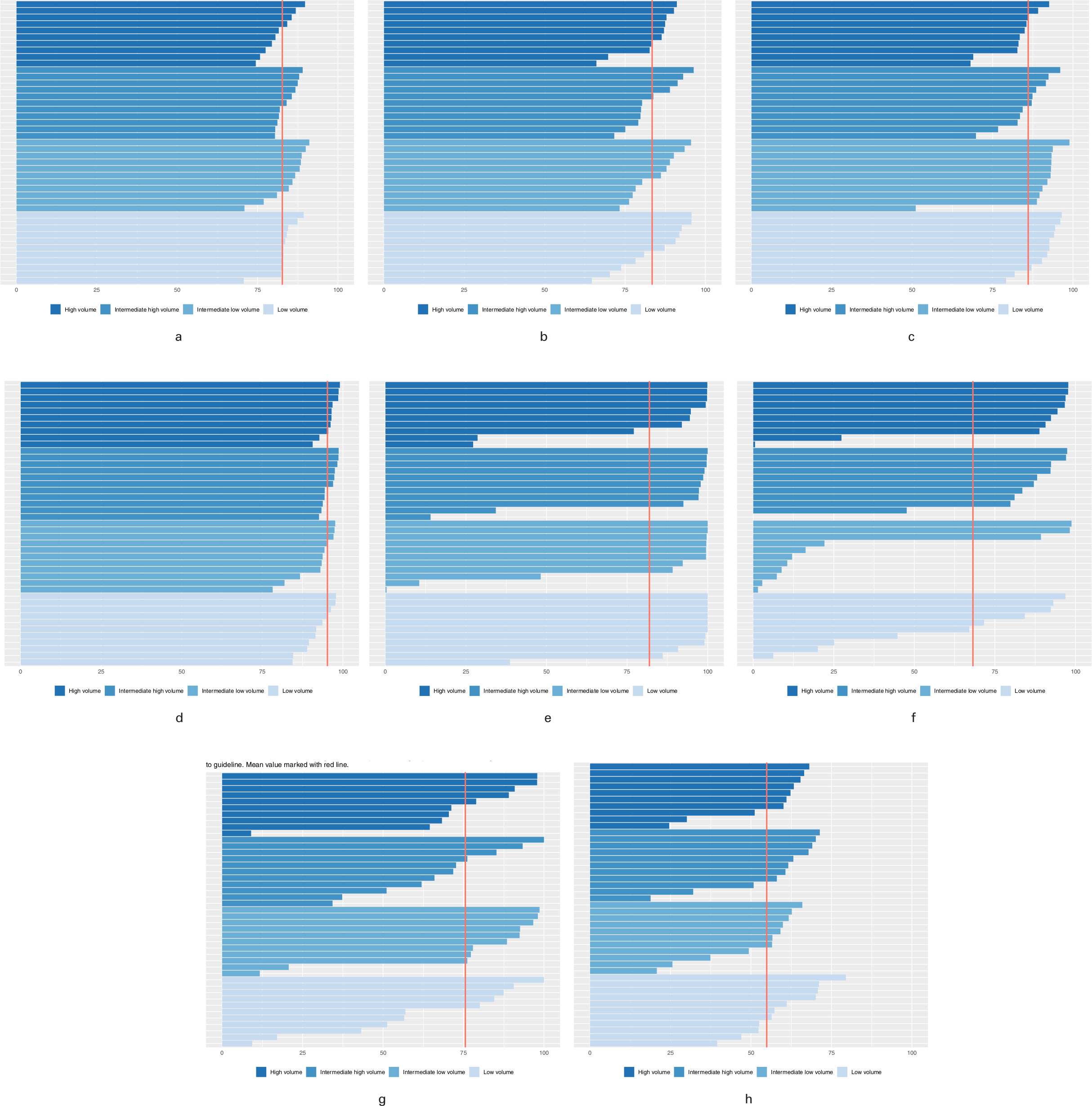
Fig. 2
a) Surgery within 48 hours. b) Surgeon with more than three years of fracture surgery experience. c) Undisplaced femoral neck fractures (FNFs) treated with screw fixation. d) Displaced FNFs treated with arthroplasty. e) Arthroplasties with cemented stem. f) Trochanteric AO/OTA A1 fractures treated with sliding hip screw (SHS). g) Intertrochanteric AO/OTA A3 and subtrochanteric fractures treated with intramedullary nail (IMN). h) Best practice 2014 to 2018 mean values.
A mean 83% of patients (71% to 91%) was treated within 48 hours (Figure 2a) and 83% of patients (65% to 96%) were treated by an experienced surgeon (Figure 2b). For undisplaced FNFs screw fixation was used in 86% of patients (51% to 99%; Figure 2c).
The majority of patients (mean 96% (79% to 99%)) with a displaced FNF received an arthroplasty (Figure 2d), and a mean 80% of these patients (0.3% to 100%) had a cemented stem. Seven of the 43 hospitals used a cemented prosthetic stem in fewer than 40% of the arthroplasties in contrast to five hospitals that used bone cement in all patients (100%; Figure 2e).
In trochanteric fractures the mean proportion receiving guideline-recommended treatment with a SHS was 68% (0% to 99%; Figure 2f). In inter- and subtrochanteric fractures, the mean proportion of patients treated with the recommended IMN was 76% (9% to 100%). In 14 hospitals (33%) the mean proportion receiving IMN for such fractures was below 30%, while 16 hospitals used IMN in more than 90% of patients (Figure 2g).
The mean composite best practice indicator for the group of hip fractures in January 2014 to December 2018 was 55% (Figure 2h).
During the five-year study period, adherence improved for all fracture types, except for trochanteric fractures (Figure 3); the mean composite "best practice indicator" increased from 50% (2014) to 59% (2018).

Fig. 3
Fracture specific adherence to best practice January 2014 to December 2018. Values given as mean percent adherence to fracture specific guideline recommendation.FNF, femoral neck fracture,OTA, Orthopaedic Trauma Association.
Predictors for adherence to guidelines
Adherence to guidelines, expressed by the composite measure of best practice calculated for all hip fractures, is shown in Table V. Hospitals with a dedicated hip fracture unit adhered more often to guidelines than those without such a unit (OR 1.06 (95% CI 1.01 to 1.11); p = 0.025). Furthermore, hospitals with a hip fracture programme were more compliant in following guidelines compared to hospitals without such a programme (OR 1.16 (95% CI 1.06 to 1.27); p = 0.002). The effect of hospital treatment volume on adherence to guideline recommendations expressed by the term "best practice" varied significantly; with high volume hospitals as reference, both intermediate-high and low volume hospitals adhered significantly better to best practice (OR 1.08 (95% CI 1.02 to 1.14); p = 0.010, and OR 1.19 (95% CI 1.08 to 1.31); p < 0.001 respectively), whereas intermediate low volume hospitals underperformed (OR 0.82 (95% CI 0.76 to 0.87); p < 0.001). Table V also shows a gradual improvement in adherence to guidelines over the period studied.
Table V.
Factors influencing best practice.
| Factor | Patients, n | Best practice, n (%) | OR (95% CI) | p-value |
|---|---|---|---|---|
| Orthogeriatric service | ||||
| Yes | 12,340 | 6,779 (54.9) | 1.01 (0.96 to 1.06) | 0.740 |
| No | 15,981 | 8,759 (54.8) | Reference | |
| Dedicated hip fracture unit | ||||
| Yes | 10,925 | 6,089 (55.7) | 1.06 (1.01 to 1.11) | 0.025 |
| No | 17,396 | 9,449 (54.3) | Reference | |
| Separate orthopaedic ward | ||||
| Yes | 24,777 | 13,542 (51.5) | 0.94 (0.88 to 1.01) | 0.086 |
| No | 3,544 | 1,996 (56.3) | Reference | |
| Hospital hip fracture programme | ||||
| Yes | 26,323 | 14,509 (55.1) | 1.16 (1.06 to 1.27) | 0.002 |
| No | 1,998 | 1,029 (51.5) | Reference | |
| Total hip fracture volume of hospital 2014 to 2018 | ||||
| High (868 to 2,025) | 13,388 | 7,366 (55.0) | Reference | |
| Intermediate high (551 to 839) | 7,754 | 4,402 (56.8) | 1.08 (1.02 to 1.14) | 0.010 |
| Intermediate low (373 to 541) | 5,100 | 2,540 (49.8) | 0.82 (0.76 to 0.87) | < 0.001 |
| Low volume (66 to 296) | 2,079 | 1,230 (59.2) | 1.19 (1.08 to 1.31) | < 0.001 |
| Year of surgery | ||||
| 2014 | 5,635 | 2,850 (50.6) | Reference | |
| 2015 | 5,742 | 3,036 (52.9) | 1.10 (1.02 to 1.18) | 0.013 |
| 2016 | 5,806 | 3,085 (53.1) | 1.11 (1.04 to 1.20) | 0.004 |
| 2017 | 5,618 | 3,276 (58.3) | 1.38 (1.28 to 1.49) | < 0.001 |
| 2018 | 5,52 | 3,291 (59.6) | 1.45 (1.35 to 1.57) | < 0.001 |
| RHA | ||||
| South-Eastern Norway | 16,347 | 8,692 (53.2) | Reference | |
| Western Norway | 5,194 | 2,877 (55.4) | 1.09 (1.03 to 1.16) | 0.006 |
| Central Norway | 4,150 | 2,594 (62.5) | 1.50 (1.39 to 1.60) | < 0.001 |
| Northern Norway | 2,630 | 1,375 (52.3) | 0.97 (0.89 to 1.06) | 0.488 |
-
CI, confidence interval; OR, odds ratio; RHA, regional health authority.
There were also significant differences between the four regional health authorities (RHAs). With the most populated region (South-Eastern Norway RHA) as reference, Western Norway RHA and Central Norway RHA adhered significantly better to best practice (OR 1.50 (95% CI 1.39 to 1.60); p < 0.001, and OR 1.09 (95% CI 1.03 to 1.16); p = 0.006 respectively), whereas Northern Norway RHA did not differ significantly.
Consequences of deviation from guidelines
Guideline-recommended treatment and subsequent outcomes are presented in Table VI. Delayed surgery exceeding the recommended 48 hours increased 365 day mortality (OR 1.13 (95% CI 1.05 to 1.22); p = 0.001). Years of experience of surgeons did not affect any of the three outcome measures. For undisplaced FNFs, non-adherence to the recommended screw fixation reduced the risk of reoperation substantially (OR 0.34 (95% CI 0.21 to 0.55); p < 0.001). Patients with displaced FNF receiving treatment alternatives other than the recommended arthroplasty had a statistically significantly higher 30 day mortality rate (OR 1.29 (95% CI 1.03 to 1.62); p = 0.030), a higher 365 day mortality rate (OR 1.45 (95% CI 1.22 to 1.72); p < 0.001) and a higher 365 day reoperation rate (OR 4.61 (95% CI 3.73 to 5.71); p < 0.001). Patients treated with arthroplasty without the recommended cemented stem had a statistically significant higher 365 day reoperation rate (OR 1.23 (95% CI 1.02 to 1.48); p = 0.030). Patients with trochanteric fractures not treated with the recommended SHS had a significantly lower 365 day mortality rate (OR 0.85 (95% CI 0.75 to 0.98); p = 0.023). For inter- and subtrochanteric fractures the risk of reoperation increased significantly if recommended treatment with IMN was not employed (OR 1.54 (95% CI 1.10 to 2.16); p = 0.012).
Table VI.
Treatment outcome according to seven guideline recommendations and according to the best practice.
| Mortality 30 days | Mortality 365 days | Revision 365 days | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Total | n (%) | OR (95% CI) |
p-value | n (%) | OR (95% CI) |
p-value | n (%) | OR (95% CI) |
p-value |
| Surgery within 48 hours | ||||||||||
| Yes | 23,390 | 1,969 (8.4) | Reference | 5,860 (25.1) | Reference | 1,168 (5.0) | Reference | |||
| No | 4,931 | 477 (9.7) | 1.04 (0.93 to 1.16) | 0.499 | 1,427 (28.9) | 1.13 (1.05 to 1.22) | 0.001 | 262 (5.3) | 1.06 (0.92 to 1.22) | 0.405 |
| Surgeon has > 3 years experience | ||||||||||
| Yes | 23,815 | 2065 (8.7) | Reference | 6,091(25.8) | Reference | 1,171 (5.0) | Reference | |||
| No | 4,686 | 381 (8.1) | 0.97 (0.86 to 1.09) | 0.573 | 1,196 (25.5) | 1.04 (0.96 to 1.12) | 0.380 | 259 (5.5) | 1.12 (0.98 to 1.29) | 0.100 |
| Screw fixation (Garden 1 to 2) | ||||||||||
| Yes | 3,747 | 224 (6.0) | Reference | 846 (22.6) | Reference | 338 (9.0) | Reference | |||
| No | 589 | 46 (7.8) | 1.09 (0.77 to 1.55) | 0.619 | 160 (27.2 ) | 1.05 (0.84 to 1.29) | 0.687 | 19 (3.2) | 0.34 (0.21 to 0.55) | <0.001 |
| Arthroplasty (Garden 3 to 4) | ||||||||||
| Yes | 16,219 | 1,328 (8.2) | Reference | 3,805 (23.5) | Reference | 678 (4,2) | Reference | |||
| No | 770 | 111 (14.4) | 1.29 (1.03 to 1.62) | 0.030 | 276 (35.8) | 1.45 (1.22 to 1.72) | <0.001 | 124 (16,1) | 4.61 (3.73 to 5.71) | <0.001 |
| Cemented stem if arthroplasty | ||||||||||
| Yes | 13,017 | 1,097 (8.4) | Reference | 3,128 (24.0) | Reference | 523 (4.0) | Reference | |||
| No | 3,202 | 231 (7.2) | 0.90 (0.77 to 1.05) | 0.184 | 677 (21.1) | 0.91 (0.83 to 1.01) | 0.082 | 155 (4.8) | 1.23 (1.02 to 1.48) | 0.030 |
| SHS (Trochanteric AO/OTA A1) | ||||||||||
| Yes | 3,783 | 348 (9.2) | Reference | 1,091 (28.8) | Reference | 96 (2.5) | Reference | |||
| No | 1,763 | 167 (9.5) | 1.04 (0.85 to 1.27) | 0.701 | 462 (26.2) | 0.85 (0.75 to 0.98) | 0.023 | 43 (2.4) | 0.96 (0.67 to 1.39) | 0.842 |
| IMN (Intertrochanteric AO/OTA A3+ Subtrochanteric) | ||||||||||
| Yes | 2,072 | 173 (8.4) | Reference | 506 (24.4) | Reference | 113 (5.5) | Reference | |||
| No | 670 | 67 (10.0) | 1.14 (0.84 to 1.56) | 0.400 | 189 (28.2) | 1.17 (0.95 to 1.45) | 0.139 | 54 (8.1) | 1.54 (1.10 to 2.16) | 0.012 |
-
*
Logistic regression analysis.
-
CI, confidence interval; IMN, intramedullary nail; OR, odds ratio; OTA, Orthopaedic Trauma Association; SHS, sliding hip screw.
Discussion
Our study demonstrates substantial hospital variation in adherence to evidence-based guidelines used for treatment of hip fractures in Norway. Further findings are that best practice can be ascribed to in-hospital factors and that the variation has significant negative consequences for patients in the form of increased mortality rates at 30- and 365-day post-treatment and in reoperation rates. On the other hand, adherence, expressed by the term best practice, improved significantly over the five-year study period for all fracture types except for trochanteric fractures. Treatment variation and non-adherence were notable although 86% of hospitals (n = 37) reported that they had a local, hospital-based, hip fracture programme.
We acknowledge that it is good medical practice to deviate from guidelines in specific clinical settings, if deviation can be substantiated. However, although the non-adherence rates demonstrated in this study may appear not to be substantial, deviation still represents a significant number of patients receiving less-than-optimal treatment. As an example, an adherence rate of 80% in the use of a cemented hip prosthesis means that more than 3,000 patients in Norway in the five year study period did not receive optimal care. We argue that deviation cannot be explained by rational clinical judgment alone, particularly because we have excluded combined (complex) fractures where variation and treatment according to surgeon discretion could be expected.
Evidence-based guidelines are in principle valid at the time of publication and must be revised when significant new scientific data have accrued. An example of this is that the SIGN guideline has now been withdrawn for revision. We would argue that there has been no paradigm shift in hip fracture treatment policies over the five-year study period, which may explain the relatively high non-adherence rates.
A striking feature is that individual hospitals did comply with guidelines for some items (time of surgery, competence) and fracture types, but at the same time demonstrated significant non-adherence and deviation for others. This explains the relatively low adherence rate when all hip fractures were evaluated as a group. Further, some hospitals were at odds with long-established and scientifically strong evidence. An example of this is the use of uncemented prosthesis stems.17
Non-adherence to guidelines is not a unique Norwegian phenomenon. A Dutch study showed that 74% of treatment for FNF complied with established national guidelines.18 They did not study structural components of care nor geographical variation in adherence. Data from the British National Hip Fracture Database also have shown wide disparities and poor adherence to guidelines in the use of total hip arthroplasty for hip fractures.19 Inconsistent compliance with guidelines poses a significant risk of inequality in treatment and poor outcomes.
Consequently, our findings strongly suggest that the observed variation mostly depends on providers and their hospital-specific, probably unwritten, treatment preferences. A hospital “surgical signature”, as described by Birkmeyer et al,20 probably reflects hospital-specific traditions due to regional training and surgeon-specific attitudes and beliefs as to treatment policy, which override established scientific evidence and formal national guidelines. Bhandari and Swiontkowski2 have also shown that surgeons disagree on the optimal treatment principle (arthroplasty or internal fixation) in patients aged 60 to 80 years with FNF and that surgeons' personal preferences and beliefs probably have a major impact on the choice of treatment.
It is a challenge to explain the treatment volume and regional effects on adherence to best practice in a logical or clinical context. Some of the effects may be explained by an uneven distribution of hospitals favouring a non-cemented prosthesis stem in volume groups and regional categories. Certain structural elements of the hospitals may also contribute. Considering all information as a whole, we conclude that treatment practice in individual hospitals is the main cause of non-adherence.
Grove et al21 have explored different drivers of variation in orthopaedic surgery. They argued that formal codified knowledge such as evidence-based guidelines has a little influence on decision-making. They concluded that treatment decisions are more driven by socialized knowledge spread between colleagues, particularly influenced by professional meetings and conferences.21 Timmermans22 also emphasizes the importance of clinical autonomy, which takes precedence over guidelines. Surgeon autonomy and informal paths of knowledge may partly explain the marked variation in adherence.
The main strength of this study is that it is population-based with a high inclusion rate and a high degree of completeness of the data from the NHFR. Reports to the registry are completed directly after surgery, which ensures high accuracy of the information. Subsequently, the NHFR provides high-quality information on hip fracture treatment in Norway.
A limitation is that there has been an underreporting of reoperations in the NHFR.4 Reporting of reoperations probably does not differ between fracture groups. Therefore, more complete data would probably have supported and strengthened our findings, particularly the effects on outcomes (Table VI). We also acknowledge that the use of the ASA grade to express preoperative physical status may not fully characterize health status of this patient group. On the other hand, we argue that adjustment for health status of the patients using the ASA grade is far better than no adjustment at all. There may also be factors other than the variables included in this study that may influence the choice of treatment, and that may legitimize a treatment deviating from guideline recommendations.We acknowledge that concluding summary treatment recommendations based on five evidence-based guidelines might be challenged. However, we would argue that the recommendations summarized in Table I were homogeneous across the guidelines and that the discrepancies we encountered were of minor importance.
There is substantial variation in the treatment of hip fractures in Norway. Adherence to guidelines has gradually improved over the five-year study period, but in 2018 only 59% of patients received best practice treatment. Non-adherence had a negative effect on patient outcomes. Steps must be taken to disseminate knowledge on best practice and consequences of non-adherence, and to improve non-compliance and reduce the importance of surgeons’ personal preferences in treatment decisions.
References
1. Johansen A , Mansor M , Beck S , Mahoney H , Thomas S . Outcome following hip fracture: post-discharge residence and long-term mortality . Age Ageing . 2010 ; 39 ( 5 ): 653 – 656 . Crossref PubMed Google Scholar
2. Bhandari M , Swiontkowski M . Management of acute hip fracture . N Engl J Med . 2017 ; 377 ( 21 ): 2053 – 2062 . Crossref PubMed Google Scholar
3. Wennberg John E . Tracking Medicine: A Researcher’s Quest to Understand Health Care . 170819 : Oxford University Press , 2010 . Google Scholar
4. Furnes O , Gjertsen JE , Hallan G , et al. Annual report 2019: Norwegian Advisory unit on arthroplasty and hip fractures . 2019 . http://nrlweb.ihelse.net/eng/Rapporter/Report2019_english.pdf Google Scholar
5. Norwegian guidelines for interdisiplinary care of hip fractures . Norwegian orthopaedic association, Norwegian geriatric Society, Norwegian Anaestesiological Society . 2018 . https://www.legeforeningen.no/contentassets/7f4bec178c34464489d83240608fb9ee/norske-retningslinjer-for-tverrfaglig-behandling-av-hoftebrudd.pdf (date last accessed 26 Sep 2019 ). Google Scholar
6. Australian and New Zealand Hip Fracture Registry (ANZHFR) . Australian and New Zealand guideline for hip fracture care . 2014 . https://anzhfr.org/wp-content/uploads/2016/07/ANZ-Guideline-for-Hip-Fracture-Care.pdf (date last accessed 03 Sep 19 ). Google Scholar
7. National Institute of Health and Care Excellence . National Institute of health and care excellence clinical guideline CG124 – the care of hip fracture in adults 2011 . 2011 . www.nice.org.uk/guidance/cg124 (date last accessed 01 Sep 2019 ). Google Scholar
8. American Academy of Orthopaedic Surgeons . Management of hip fractures in the elderly. AAOS . 2014 . https://www.aaos.org/cc_files/aaosorg/research/guidelines/hipfxguideline.pdf (date last accessed 3 October 2019 ). Google Scholar
9. Scottish Intercollegiate Guidelines Network . Management of hip fracture in older people -A national clinical guideline,: Scottish Intercollegiate guidelines network . 2009 . https://www.sign.ac.uk/assets/sign111.pdf (date last accessed 01 Oct 2019 ). Google Scholar
10. Bartels S , Gjertsen J-E , Frihagen F , Rogmark C , Utvåg SE . High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years . Acta Orthop . 2018 ; 89 ( 1 ): 53 – 58 . Crossref PubMed Google Scholar
11. Saklad M . Grading of patients for surgical procedures . Anesthesiology . 1941 ; 2 ( 3 ): 281 – 284 . Google Scholar
12. Ministry of Health and Care Services Norway . National health and hospital plan. Ministry of health and care services . 2015 . https://www.regjeringen.no/contentassets/7b6ad7e0ef1a403d97958bcb34478609/no/pdfs/stm201520160011000dddpdfs.pdf (date last accessed 14 Oct 2019 ). Google Scholar
13. GIN . Guidelines International Network . 2020 . https://g-i-n.net (date last accessed 15 Jul 2019 ). Crossref PubMed Google Scholar
14. Ranhoff AH , Saltvedt I , Frihagen F , Raeder J , Maini S , Sletvold O . Interdisciplinary care of hip fractures.: Orthogeriatric models, alternative models, interdisciplinary teamwork . Best Pract Res Clin Rheumatol . 2019 ; 33 ( 2 ): 205 – 226 . Crossref PubMed Google Scholar
15. Kazley JM , Banerjee S , Abousayed MM , Rosenbaum AJ . Classifications in brief . Clin Orthop Relat Res . 2018 ; 476 ( 2 ): 441 – 445 . Crossref PubMed Google Scholar
16. Meinberg EG , Agel J , Roberts CS , Karam MD , Kellam JF . Fracture and dislocation classification Compendium-2018 . J Orthop Trauma . 2018 ; 32 Suppl 1 : S1 – S10 . Crossref PubMed Google Scholar
17. Veldman HD , Heyligers IC , Grimm B , Boymans TAEJ . Cemented versus cementless hemiarthroplasty for a displaced fracture of the femoral neck: a systematic review and meta-analysis of current generation hip stems . Bone Joint J . 2017 ; 99-B ( 4 ): 421 – 431 . Crossref PubMed Google Scholar
18. Zielinski SM , Meeuwis MA , Heetveld MJ , et al. Adherence to a femoral neck fracture treatment guideline . Int Orthop . 2013 ; 37 ( 7 ): 1327 – 1334 . Crossref PubMed Google Scholar
19. Perry DC , Metcalfe D , Griffin XL , Costa ML . Inequalities in use of total hip arthroplasty for hip fracture: population based study . BMJ ; 2016 ( 353 ): i2021 . Crossref PubMed Google Scholar
20. Birkmeyer JD , Reames BN , McCulloch P , Carr AJ , Campbell WB , Wennberg JE . Understanding of regional variation in the use of surgery . The Lancet . 2013 ; 382 ( 9898 ): 1121 – 1129 . Crossref PubMed Google Scholar
21. Grove A , Johnson RE , Clarke A , Currie G . Evidence and the drivers of variation in orthopaedic surgical work: a mixed method systematic review . Health Policy and Policy Research . 2016 ; 3 : 1 . Google Scholar
22. Timmermans S . From autonomy to accountability: the role of clinical practice guidelines in professional power . Perspect Biol Med . 2005 ; 48 ( 4 ): 490 – 501 . Crossref PubMed Google Scholar
Acknowledgements
We are most grateful to the Director of SKDE, Professor Barthold Vonen, for initiating this project and for his continuing support; to Beate Hauglann, PhD, Senior Scientist at SKDE, for crucial help in the conceptual phase of the project and in facilitating the formal application processes required; to Heidi Talsethagen, Senior Legal Advisor at SKDE, for valuable help in transferring GDPR regulations to the application; to Frank Olsen, cand.polit, Analyst at SKDE for his command of the SAS Enterprise Guide and for making the programme understandable; and to Mai-Helen Walsnes, user representative, for inspiring interest of our research and useful comments during the project.
Author contributions
C. Kjærvik: Devised the research program and protocol, Designed the study, Acquired, analyzed, and interpreted the data, Drafted, critically edited, and revised the manuscript.
E. Stensland: Devised the research program and protocol, Designed the study, Drafted, critically edited, and revised the manuscript.
H. S. Byhring: Acquired, analyzed, and interpreted the data.
J. E. Gjertsen: Designed the study, Acquired, analyzed, and interpreted the data, Drafted, critically edited, and revised the manuscript.
E. Dybvik: Acquired, analyzed, and interpreted the data, Critically edited and revised the manuscript.
O. Søreide: Devised the research program and protocol, Designed the study, Acquired, analyzed, and interpreted the data, Drafted, critically edited, and revised the manuscript.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical review statement
The project was approved by the Northern Norway Regional Committee for Medical and Health Research Ethics and was exempted from the duty of confidentiality (REK 2018/1955). A data protection integrity assessment was compiled according to the EU General Data Protection Regulation (GDPR).
Follow C. Kjærvik @doktorknokkel
© 2020 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attributions licence (CC-BY-NC-ND), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/.









